Introduction
Air temperature alone is seldom regarded as the best indicator for measuring the amount of heat stress on humans caused by excessive levels of atmospheric temperature [
1]. Relative humidity, defined as the amount of moisture in the air compared to what the air can hold at that temperature may affect heat stress [
2]. Since the conditions of heat exchange between the human body and the surrounding thermal environment is quite complex, thermal indices, mostly involving two parameters, have been developed. For tropical countries, such indices frequently combine dry-bulb temperature and different measures of humidity [
1,
3]. One such index for thermal-stress assessment that is widely used by various national and local weather services is known as the Heat Index (HI). The HI is an index that measures perceived temperature in the human body by combining air temperature with relative humidity to determine the apparent temperature.
With global climate change, significant upward trends of HI have been reported in many humid regions across the globe including United States, Southeast Asia, India and Northern Australia [
4,
5]. This index can therefore be an alternative indicator of temperature and could better reflect the exposure-response relationship between temperature and health in an era of climate change. Adverse health consequences have been associated with periods of very high HI [
4].
Diarrhoea occurs when more than three loose, watery stools are passed within 24 hours. Although the exact prevalence and incidence of diarrhoea are not available, diarrhoea is endemic and a major cause of morbidity and mortality in Bangladesh [
6]. With notable improvements in diarrhoea care, Bangladesh has achieved significant success in reducing diarrhoea mortality in the recent years [
7,
8]. However, diarrhoea outbreaks and hyper-endemicity continue to plague the nation despite notable improvements in socio-economic conditions as well as in water and sanitation infrastructure [
9]. The impact of environmental temperature on diarrhoeal diseases have been studied extensively. However, the combined impact of various meteorological parameters such as HI on diarrhoea remains relatively less explored [
10,
11]. While the potential impact of HI on diarrhoea is currently underexplored, it is well-established that both temperature and relative humidity can directly affect the replication of diarrhoeal pathogens including bacteria and protozoa as well as enhance the survival of enteroviruses [
12,
13,
14,
15]. The HI may serve as an important exposure for determining the combined impact of environmental temperature and humidity on diarrhoea in the context of climate change.
Given that no previous study has attempted to assess the effect of the HI on diarrhoea hospitalisation, this study aimed to identify the relationship between HI and hospitalisations for diarrhoea, examine the impacts of extreme HI, and elucidate the modifying effects of age, gender, and season in Dhaka Bangladesh. Although it is acknowledged that correlations uncovered do not necessarily imply direct causation, such indicators may support understanding of the effects of climate parameters on diarrhoeal disease morbidity thereby aiding further research to elicit linkages between climate change and gastrointestinal health.
Materials and Methods
Study Setting
Dhaka, the capital of Bangladesh, is located at 23°42′N 90°22′E, on the eastern banks of the Buriganga River. The low-lying coastal city surrounded by five major rivers and 50 water channels is at risk of flooding from rising sea levels [
16]. Several dykes and embankments and interim boundaries created to protect Dhaka from flooding together with inadequate drainage and water pumping systems frequently result in water logging of the protected city area during the rainy monsoon season [
17,
18]. With over 20 million residents, the rapidly expanding, resource-constrained megacity faces a number of challenges including inadequate water and sanitation and hygiene infrastructure [
18,
19]. Given these challenges, the impacts of meteorological parameters on diarrhoea could be particularly concerning for Dhaka where diarrhoea is already highly prevalent [
6].
Diarrhoea Data
Daily data on total number of patients seeking care for diarrhoea (defined as the passage of ≥3 loose stools per 24 hours due to any cause) by age group and gender between 1 January 1981 and 31 December 2010 were collected from the Dhaka Hospital of the International Centre for Diarrhoeal Diseases Research, Bangladesh (icddr,b) on 7 October 2020. Since reliable records of the total number of patients admitted per day and the illness onset dates were not available for the study period, we collected data from icddr,b’s Diarrheal Disease Surveillance System (DDSS) to estimate the total number of diarrhoea patients per day. The DDSS is a robust surveillance system that was established in 1979 to collect information from a systematic sub-sample of patients attending the Dhaka Hospital. During 1979 and 1995, every 25th patient (4% of the sample) and during 1996-2010, every 50th patient (2% of the sample) was enrolled into the DDSS. Surveillance patients were seen by the regular hospital staff with emergency cases treated on a priority basis. All patients were first treated in an outpatient area; those requiring further care were admitted to an intravenous treatment centre or a hospital ward. After initial examination and care by a nurse or doctor, a trained health assistant sought verbal informed consent from the surveillance patient or an adult guardian prior to interview. Using a structured questionnaire, the trained health assistant interviewed patients and/or their caregivers and collected and recorded relevant information from diarrhoeal patients presenting to the icddr,b Dhaka Hospital. No personal identifying information were accessed for this study. The well-known diarrhoeal disease hospital in Dhaka served a population of approximately 3.5 million in 1981, 6.6 million in 1990 and 14.6 million in 2010 predominantly from urban Dhaka [
23]. Additional information on health data is provided in the supporting information (S1 Appendix).
Calculating the Heat Index (HI)
For this study, the HI was calculated using the formula described in a 1990 National Weather Service (NWS) Technical Attachment (SR 90-23) [
20].
Heat Index (HI) = − 42.379 + (2.04901523 × Tf) + (10.14333127 × RH) − (0.22475541 × Tf × RH) − (6.83783 × 10 −3 × Tf2) − (5.481717 × 10−2 × RH2 ) + (1.22874 × 10−3) Tf 2(RH) + (8.5282 × 10−4 × Tf × RH2 ) − (1.99 × 10−6) Tf2 RH2
Where:
Tf average air temperature in degrees Fahrenheit
RH relative humidity in whole number
Statistical Analysis
A descriptive analysis was performed to understand the daily time-series characteristics of diarrhoea and HI over the study period. Each data series was checked for stationarity, autocorrelation, long-term trends, seasonality, possible outliers, normality, homoscedasticity and volatility using established methods [
21,
22,
23,
24,
25]. The HI data series was pre-whitened using autoregressive integrated moving average (ARIMA) models to achieve stationarity before checking cross-correlation between diarrhoea hospitalisation and HI.
A time-series adjusted generalised linear model (GLM) with negative binomial regression distribution was used to assess the association between acute effects of HI and extreme HI on diarrhoea hospitalisations [
24]. The negative binomial distribution was used to allow for the overdispersion/extra variation detected in the response variable [
26]. Since past studies have identified atmospheric pressure, day of the week, long-term time and seasonal trends, and rainfall as potential confounders on the relationship between HI and human health, the model was adjusted for these potential confounding factors [
27]. To examine the effect of season, an indicator variable for season was incorporated into the model. The months of November to February was defined as the winter, March to June as the summer and July to October as the rainy monsoon season that reflected the seasonality of Bangladesh [
28]. We initially investigated individual and distributed lag effects for 28 days. As statistically significant relationship between diarrhoea and HI was found at lag zero only, lag effects were not considered in the model. A series of flexible spline functions of time were used to flexibly model underlying trends and seasonal patterns in the health data unrelated to climatic factors [
21]. The Bayesian Information Criterion (BIC) and analysis of residuals were used to evaluate model fit and inform the choice of degrees of freedom for flexible splines. Model residuals were lagged by one day to adjust for significant residual autocorrelation associated with the day before. For all statistical tests, values of p<0.05 were considered statistically significant. The relative risk of hospitalisation for diarrhoea per unit change in HI was calculated from equation (1) as incidence rate ratio (IRR).
The model to investigate the effects of HI on diarrhoea took the following form:
Yt ~ Negative Binomial (µt, θ)
log[E(Yt)]= β0 + β1HI1t + β2Rain2t + β3ATPress3t + γ1dow1t + γ2Season2t + θ1(LS Time, 8 D.F.)1t………………….……………………………………………………………………………..(1)
where E(Yt) denotes expected daily diarrhoea count at time t, log[E(Yt)] is the natural logarithm of the expected count (log link function), β0 is the intercept term, HI1t denotes heat index at time t, Raint and ATPresst denote the cumulative rainfall and daily atmospheric pressure at time t. To control for long-term trends and seasonality, a flexible linear spline LS with 8 degrees of freedom per year was incorporated into the model. Season is the categorical variable denoting the three seasons and dowt is the categorical day of the week with a reference day of Friday.
To explore the impacts of extreme HI on diarrhoea, three categories of HI were generated. The heat indices above the 75th, 95th and 99th percentiles during the study period were defined as high HI, very high HI and extremely high HI, respectively. To examine the effect of extreme HI on diarrhoea, different models were generated using the three categories of extreme HI.
In addition, we used a generalised linear model to study the effects of temperature and relative humidity on diarrhoea hospitalisation. The model is as follows:
log[E(Yt)]= β0 + β1Temp1t + β2Hum2t + β3Rain3t + β4ATPress4t + γ1dow1t + γ2Season2t + θ1(LS Time, 8 D.F.)1t ………………………………………….....……..(2)
where E(Yt) denotes expected daily diarrhoea count at time t, log[E(Yt)] is the natural logarithm of the expected count (log link function), β0 is the intercept term, Temp1t and Hum2t denote mean temperature and relative humidity at time t respectively, Raint and ATPresst denote the cumulative rainfall and daily atmospheric pressure at time t. LS is a flexible linear spline with 8 degrees, Season is the categorical variable representing the three seasons and dowt is the categorical day of the week with a reference day of Friday.
The estimation of relative risks can change significantly with changing model specifications [
27,
29]. As a result, the analyses were repeated using linear splines of 1–14 degrees of freedom per year and by fitting a natural cubic spline with 3–7 D.F. to control for long-term trend and seasonality instead of linear splines. In addition, sensitivity analyses were conducted removing atmospheric pressure from the covariates and including interaction terms in the temperature humidity models. We reran the analyses using the number of patients enrolled into the icddr,b’s DDSS as the outcome instead of the total estimated diarrhoea hospitalisation per day. We used Stata/SE 18.0 (StataCorp LLC) for data analyses in this study.
Ethics Approval
This study was granted approval by the Research Review Committee (RRC) and Ethical Review Committee (ERC) of the International Centre for Diarrhoeal Diseases Research, Bangladesh (icddr,b) (Protocol number: PR-19097). The study used secondary data and did not involve primary data collection from human participants. The study was also approved by the University College London’s Research Ethics Committee (UCL REC).
Results
Approximately 29,83,850 diarrhoea patients sought care from the icddr,b Dhaka Hospital during the 30-year study period.
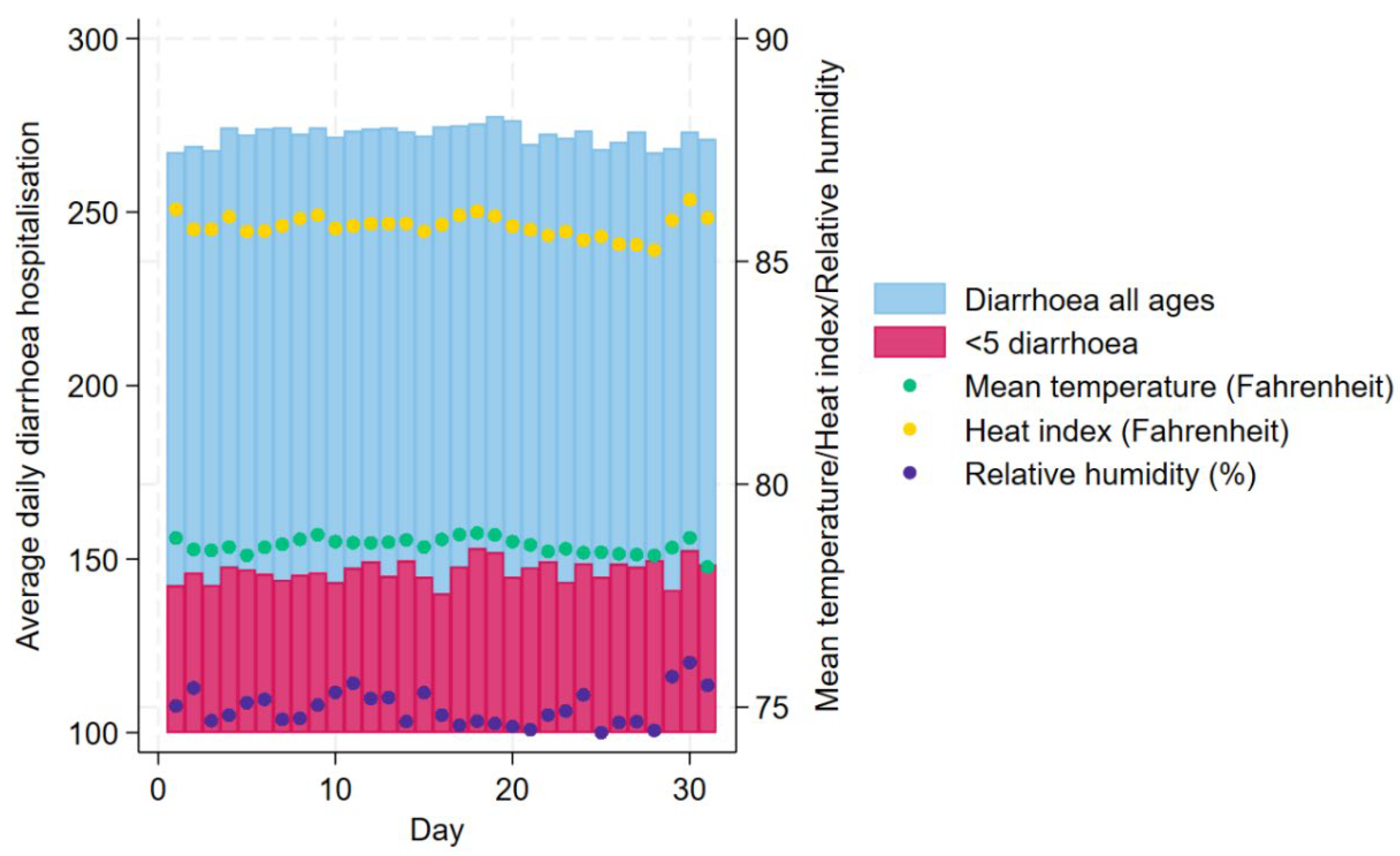
Figure 1 shows the daily distributions of diarrhoea hospitalisations for all ages and <5 children and mean temperature (°F), HI (°F) and relative humidity (%) in Dhaka averaged across the years 1981 – 2010.
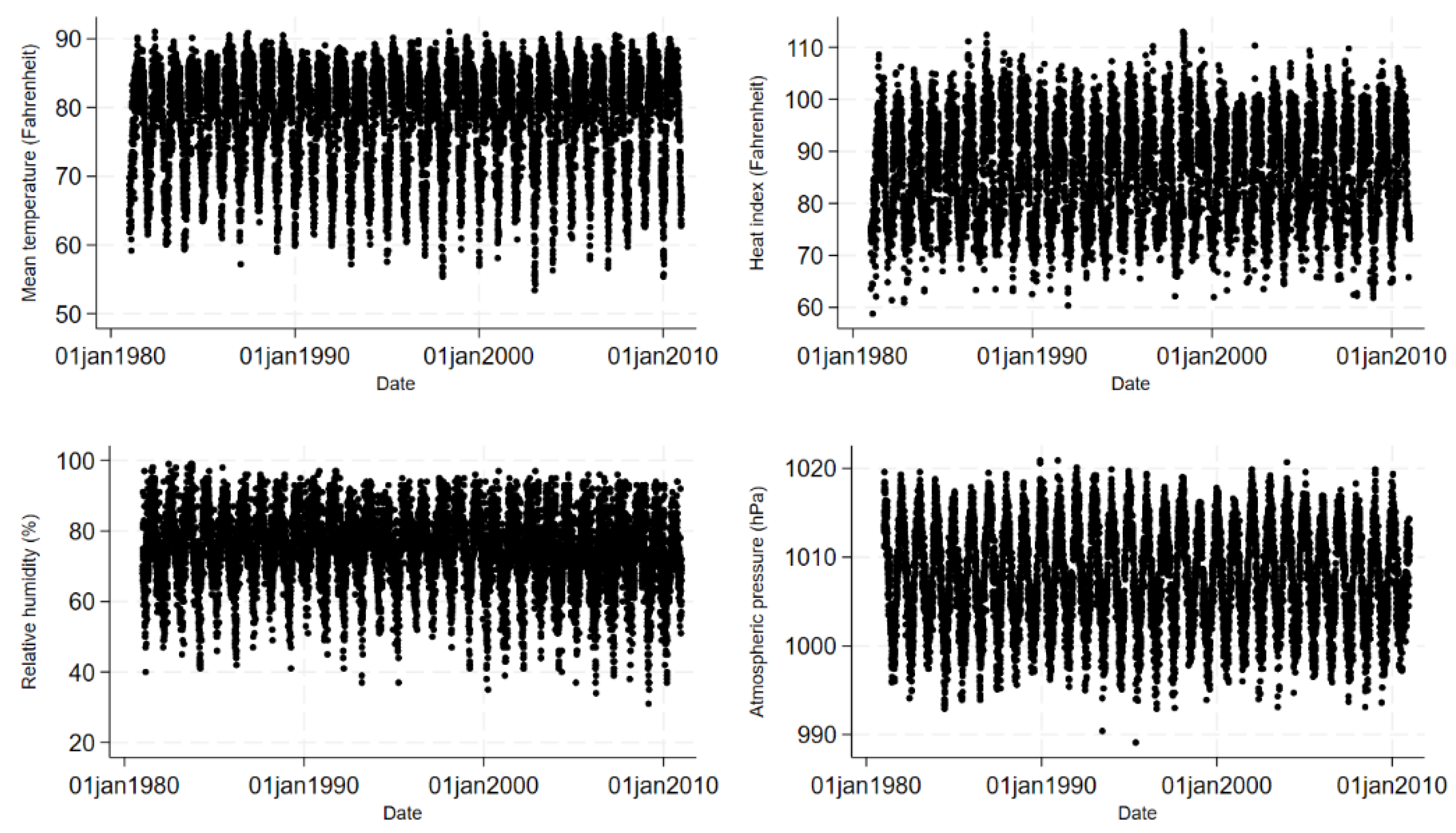
Figure 2 shows the daily and
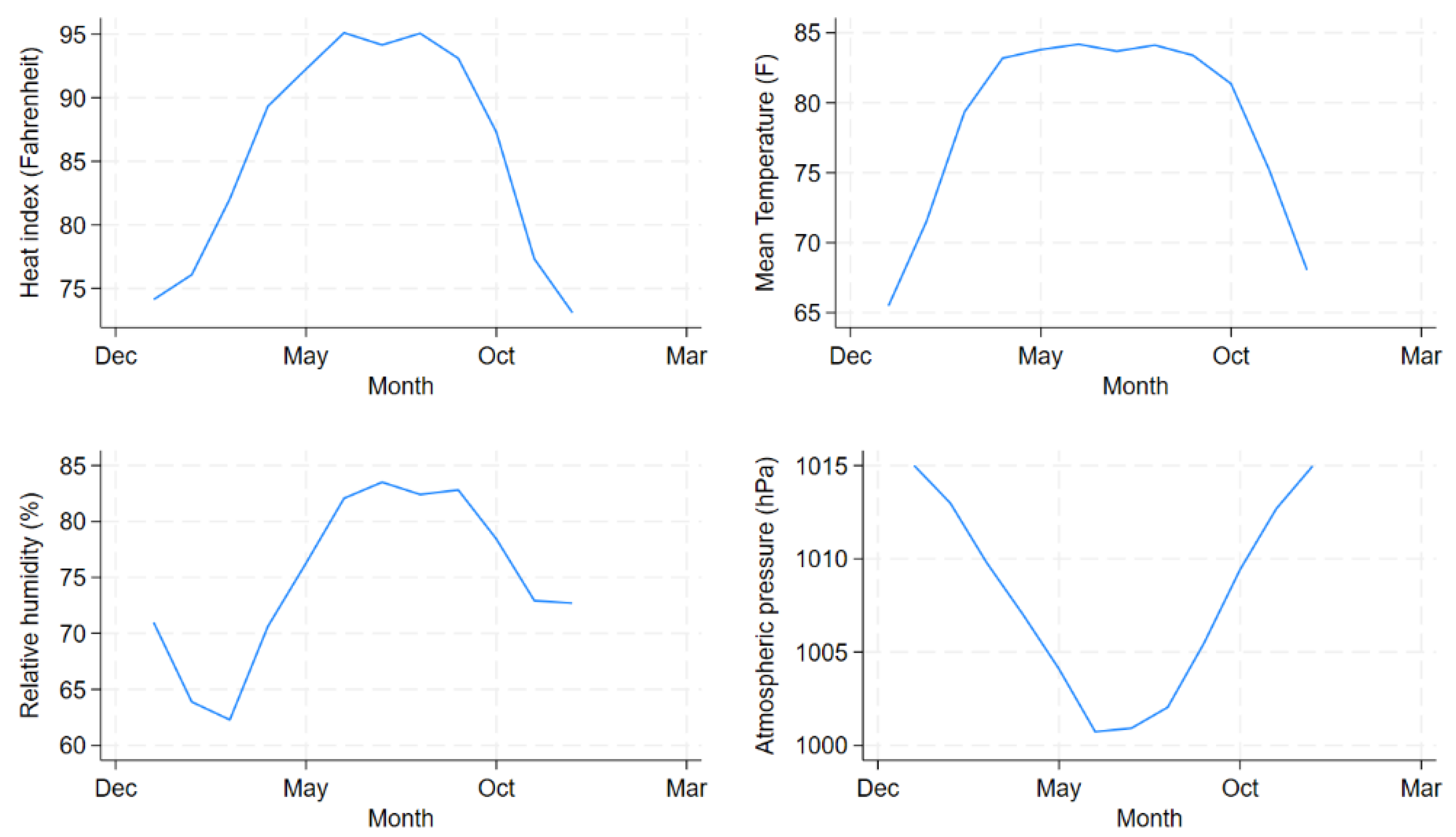
Figure 3 shows the monthly distributions of meteorological factors in Dhaka Bangladesh revealing distinct seasonal patterns. HI remained high from April to September peaking during June and August before lowering down from October. The figure suggests that HI was lower during the months of December to February which corresponds roughly to the winter season in Bangladesh.
Table 1 shows the summary statistics for HI, mean temperature, relative humidity, atmospheric pressure and diarrhoea hospitalisations. During the study period, the median HI was 86.2°F, median temperature was 81.1°F and the median relative humidity was 76.0%. The median number of daily diarrhoea admission in all ages for the period was 250. Only 25 out of 10,957 (0.2%) days during the study period had a relative humidity lower than 40%.
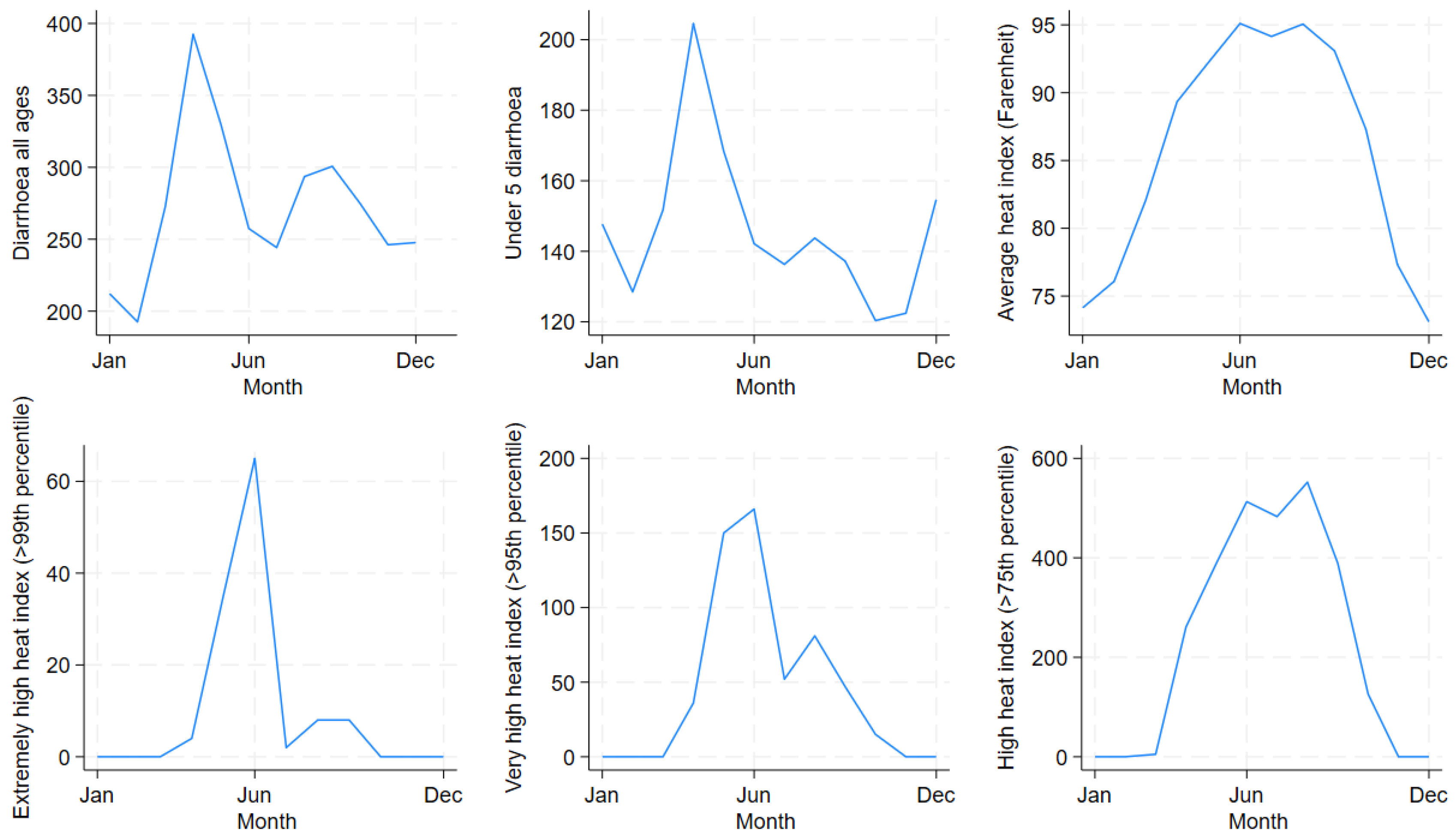
Figure 4 shows the temporal distribution of diarrhoea hospitalisation in all ages and in <5 children and the extreme HI indicators by months. Diarrhoea hospitalisation in all ages and <5 children peaked in April. Most extreme HI days were concentrated during the summer months. Extremely high (>99th percentile) and very high HI (>95th percentile) peaked in June whereas high HI (>75th percentile) peaked in September.
Table 2 shows a decreasing trend of extreme HIs across decades. However, the residents of Dhaka were still exposed to considerable number of large HIs during the 30-year study period.
As highlighted
Table 3, a 1°F rise in HI, high, very high and extremely high HI were associated with a 0.84% (95% CI: 0.76% – 0.91%), 7.7% (95% CI: 6.7% – 8.8%), 7.3% (95% CI: 5.5% – 9.0%) and 8.8% (95% CI: 5.3% – 12.4%) increase in diarrhoea, respectively. The overall impact of HI varied slightly by gender (1.1% in males versus 1.0% in females). The effects were greatest in children under 5 years of age.
Using equation (2), 1°F increase in mean temperature was associated with 1.4% (1.3 – 1.5), 1.8% (1.4 – 2.1), 1.1% (0.9 – 1.3) and 1.0% (0.7 – 1.3) increase diarrhoea hospitalisation in all ages, under 5 children, males, and females, respectively. The results of the sensitivity analyses changed the results very little (S2 File). Acceptable model fit was achieved for the models in the various subgroups. Partial autocorrelation plots of the deviance residuals show that for all sub-groups, the heat index models had negligible deviance residuals (S2 File).
Discussion
This study examined the effects of HI on diarrhoea in all ages and found small but significant non-linear positive relationship between HI and diarrhoea after controlling for the confounding effects of atmospheric pressure, heavy rainfall, day of the week, long-term time trend and seasonality. A unit (1°F) increase in HI was associated with 0.8% - 0.9% increase in the risk of hospitalisation for diarrhoea. While no previous study has investigated the effects of HI on diarrhoeal disease morbidity, a few past studies examining the impact of HI on mortality and cardiovascular diseases have reported non-linear relationship between HI and health outcomes [
27,
30].
In this study, the effects of relatively large HI were found to be much more pronounced than average HI. Between 1981 and 2010, the population in Dhaka were exposed to high (>94.3°F), very high (>100.7°F) and extremely high (>105°F) HI for 2,718, 547 and 122 days, respectively. High, very high and extremely high HI were associated with approximately 8%, 7% and 9% increase in the risk of diarrhoea in all ages, respectively. The results of this study support the hypothesis that large HI poses greater risk to human health including diarrhoea.
With ongoing climate change, the HIs are likely to become more and more variable. As pointed out by several past investigations, the effects of increased HI on health outcomes including diarrhoea are likely to become more severe with global climate change [
4,
27]. Although the dose-response relationship between exposure to various levels of HI and diarrhoeal disease morbidity was not investigated in the past, US National Weather Service generates different heat alerts according to the level of exposure to HI and heat illnesses [
31]. The result of this study underscores the importance of raising awareness of patients, caregivers, medical, public health and allied staff of the particular high risk posed by relatively large HI on diarrhoeal disease morbidity among the residents of Dhaka. Based on the impact of extreme HI on morbidity, similar heat alerts could be generated not only for heat related illnesses but also for other morbidity including diarrhoea that likely impacts people even within the indoor settings in addition to outdoors.
In this study, children under 5 years of age were observed to suffer greater impacts of relatively large HIs compared to all ages. Unit increase in very high and extremely high HIs were associated with approximately 18% increase in diarrhoea hospitalisations among children under 5 years of age. While the exact mechanism by which exposure to large HIs influence the risk of diarrhoea in young children remain largely unknown, immune system in children are likely to be immature and children are likely to have low self-care capacity [
32,
33,
34].
In addition to young children, males were found to be at a slightly higher risk of diarrhoea due to extremely high (14.2% vs 10.4%) and high HI (10.1% vs 8.4%) compared to females. However, compared to males, females were found to be at slightly higher risk for very high HI (10.2% vs 10.8%). A few studies that have investigated the impact of HI on cardiovascular disease mortality have reported greater vulnerability of females to the effects of HI owing to their patho-physiological responses to heat stress [
27,
35,
36]. The inconsistency noted in this study suggest that additional factors including social and living conditions [
37], social behaviour, amount of time spent outdoor versus indoor and healthcare seeking behaviour likely also modify the effect of HI on diarrhoea hospitalisation. Future studies focused on identifying vulnerable groups based on the impacts of HI on specific morbidities could shed further light on the modifying role of gender.
Although forecasting heat index may not be as straightforward as temperature forecast, the negligible deviance residuals in the heat index models in this study suggest that heat index may perform similarly to temperature as an indicator to measure the effects of meteorological factors on diarrhoeal diseases in Dhaka, Bangladesh. This finding is consistent with a previous study that examined the utility of various measures of temperature to identify the best predictor of mortality and found no single measure to be superior over the others [
30]. However, this finding is inconsistent with the finding of a study conducted by Yin and Wang in 2018 in China where the heat index performed better than mean temperature to measure the effects of meteorological parameters on CVD mortality [
27]. While the exact mechanism how temperature and relative humidity together affect diarrhoea occurrence is yet to be elicited, temperature and relative humidity likely affect host immunity, host susceptibility, pathogen transmission and pathogen survival thereby indirectly affecting diarrhoeal disease morbidity [
11]. On the other hand, meteorological parameters exert direct effect on CVD mortality by compromising the body’s capacity to lose heat and control core body temperature via sweat evaporation [
38]. As a result, the observed difference in HI effect could result from the difference in the way temperature and relative humidity affect the causation of infectious diarrhoea as opposed to CVD mortality.
While this study used established statistical techniques to quantify the effects of HI and extreme HI on diarrhoea and further examined the variations of HI impact by gender and age groups, this study has several limitations. Diarrhoea occurrence and hospitalisation are determined not only by meteorological factors including temperature and relative humidity, but also by other individual and socioeconomic factors such as nutritional status, educational level, water and sanitation infrastructure, poverty and healthcare seeking behaviour, which may vary among cities. These additional factors should be taken into consideration when comparing results from different areas. In addition, the study period consisted of 25 days of observation with relative humidity below 40%. The HI in this study was derived from the formula proposed by Rothfusz, which is known to work better at relative humidity of ≥40% [
20]. This may have introduced some bias into the results. Given that only 0.2% of the data points represented such malformation, relative humidity of less than 40% was unlikely to deviate the result significantly. Furthermore, sensitivity analysis conducted by replacing the 25 data points with mean relative humidity did not change the result. Huang et al. (2011) adapted the heat index formula for Beijing, China that was not only suitable for the climatic condition of that country but also applicable to relative humidity below 40% [
27]. Future studies can compare the utility of both formulae for analysing the relationship of HI and health outcomes in the Bangladeshi context.
Conclusions
In an era of climate change, the effects of HI on diarrhoea are likely to become more pronounced, particularly among children under 5 years of age. This underscores the importance of conducting research to elucidate the impacts of HI on diarrhoea as well as to develop targeted health policies and programs to mitigate the risks. Using the comprehensive meteorological index, the heat index, to analyse the combined effects of temperature and relative humidity on diarrhoeal diseases, this study advances knowledge of how to measure morbidity risk using alternative weather indicators.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. S1 File. Description of the health data. S2 File. Findings from the sensitivity analyses and model diagnostics
Author Contributions
Conceptualization, Farhana Haque; Data curation, Farhana Haque, S.M. Hasan, A. S. G. Faruque and Shamim Jubayer; Formal analysis, Farhana Haque; Methodology, Farhana Haque, Fiona Lampe, Shakoor Hajat and Ilan Kelman; Project administration, Shamim Jubayer; Resources, Farhana Haque, Katerina Stavrianaki, S.M. Hasan, A. S. G. Faruque, Tahmeed Ahmed and Shamim Jubayer; Supervision, Fiona Lampe, Shakoor Hajat, Katerina Stavrianaki, Tahmeed Ahmed and Ilan Kelman; Validation, Farhana Haque; Visualization, Farhana Haque; Writing – original draft, Farhana Haque; Writing – review & editing, Farhana Haque, Fiona Lampe, Shakoor Hajat and Ilan Kelman.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Research Review Committee (RRC) and Ethical Review Committee (ERC) of the International Centre for Diarrhoeal Diseases Research, Bangladesh (icddr,b) (Protocol number: PR-19097). The study used secondary data and did not involve primary data collection from human participants. The study was also approved by the University College London’s Research Ethics Committee (UCL REC).
Informed consent Statement
Patient consent was waived due to no individual data being collected.
Data Availability Statement
The datasets presented in this article are not readily available because according to the institutional data policy of the icddr,b (International Centre for Diarrhoeal Disease Research, Bangladesh), only summary of data can be publicly displayed or can be made publicly accessible. To protect intellectual property rights of primary data, icddr,b cannot make primary data publicly available. However, upon request, Institutional Data Access Committee of icddr,b can provide access to primary data to any individual, upon reviewing the nature and potential use of the data. Requests to access the datasets should be directed to Ms. Armana Ahmed, Head, Research Administration, icddr,b, Dhaka, Bangladesh, Email: aahmed@icddrb.org, Phone: +88 02 9827001-10 (ext. 3200).
Acknowledgements
This study was completed as a part of a PhD thesis by FH. The authors would like to thank the Commonwealth Scholarship Commission for funding the PhD study. The authors would also like to thank members of the Research Administration team of icddr,b, National Health Foundation and Research Institute (NHF&RI) and Bangladesh Meteorological Department (BMD) for their support to data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- McGregor, G.R.; Bessemoulin, P.; Ebi, K.; Menne, B. , editors. Heatwaves and Health: Guidance on Warning-System Development Geneva, Switzerland World Meteorological Organization and World Health Organization; 2015.
- Chen, X.; Li, N.; Liu, J.; Zhang, Z.; Liu, Y. Global Heat Wave Hazard Considering Humidity Effects during the 21st Century. Int. J. Environ. Res. Public Heal. 2019, 16, 1513. [Google Scholar] [CrossRef]
- Blazejczyk, K.; Epstein, Y.; Jendritzky, G.; Staiger, H.; Tinz, B. Comparison of UTCI to selected thermal indices. Int. J. Biometeorol. 2012, 56, 515–535. [Google Scholar] [CrossRef]
- Delworth, T.L.; Mahlman, J.D.; Knutson, T.R. Changes in Heat Index Associated with CO2-Induced Global Warming. Clim. Chang. 1999, 43, 369–386. [Google Scholar] [CrossRef]
- Rajib, M.A.; Mortuza, M.R.; Selmi, S.; Ankur, A.K.; Rahman, M.M. Increase of Heat Index over Bangladesh: Impact of Climate Change. International Journal of Civil and Environmental Engineering 2011, 5. [Google Scholar]
- Collaborators GBDDD. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017, 17, 909–948. [Google Scholar] [CrossRef]
- Billah, S.M.; Raihana, S.; Ali, N.B.; Iqbal, A.; Rahman, M.M.; Khan, A.N.S.; Karim, F.; Karim, M.A.; Hassan, A.; Jackson, B.; et al. Bangladesh: a success case in combating childhood diarrhoea. J. Glob. Heal. 2019, 9, 020803. [Google Scholar] [CrossRef] [PubMed]
- Black, R.; Fontaine, O.; Lamberti, L.; Bhan, M.; Huicho, L.; El Arifeen, S.; Masanja, H.; Walker, C.F.; Mengestu, T.K.; Pearson, L.; et al. Drivers of the reduction in childhood diarrhea mortality 1980-2015 and interventions to eliminate preventable diarrhea deaths by 2030. J. Glob. Heal. 2019, 9, 020801. [Google Scholar] [CrossRef]
- Haque, F.; Hossain, M.J.; Kundu, S.K.; Naser, A.M.; Rahman, M.; Luby, S.P. Cholera Outbreaks in Urban Bangladesh In 2011. Epidemiology 2013, 3. [Google Scholar] [CrossRef]
- Levy, K.; Smith, S.M.; Carlton, E.J. Climate Change Impacts on Waterborne Diseases: Moving Toward Designing Interventions. Curr. Environ. Heal. Rep. 2018, 5, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.; Woster, A.P.; Goldstein, R.S.; Carlton, E.J. Untangling the Impacts of Climate Change on Waterborne Diseases: a Systematic Review of Relationships between Diarrheal Diseases and Temperature, Rainfall, Flooding, and Drought. Environ. Sci. Technol. 2016, 50, 4905–4922. [Google Scholar] [CrossRef]
- Feldacker CB, editor Environmental influences on cholera outbreaks in Bangladesh and Vietnam: implications for prevention and prediction. APHA 135th Meeting and Expo; 2007 November 3-7; Washington, DC.
- Hashizume, M.; Ben Armstrong, B.; Hajat, S.; Wagatsuma, Y.; Faruque, A.S.; Hayashi, T.; Sack, D.A. Association between climate variability and hospital visits for non-cholera diarrhoea in Bangladesh: effects and vulnerable groups. Leuk. Res. 2007, 36, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, M.; Armstrong, B.; Wagatsuma, Y.; Faruque, A.S.G.; Hayashi, T.; Sack, D.A. Rotavirus infections and climate variability in Dhaka, Bangladesh: a time-series analysis. Epidemiology Infect. 2007, 136, 1281–1289. [Google Scholar] [CrossRef]
- Huq, A.; Sack, R.B.; Nizam, A.; Longini, I.M.; Nair, G.B.; Ali, A.; Morris, J.G.; Khan, M.N.H.; Siddique, A.K.; Yunus, M.; et al. Critical Factors Influencing the Occurrence of Vibrio cholerae in the Environment of Bangladesh. Appl. Environ. Microbiol. 2005, 71, 4645–4654. [Google Scholar] [CrossRef] [PubMed]
- UN-Habitat. State of the World’s Cities 2008/2009—Harmonious Cities. London, UK and Sterling, VA, USA: United Nations Human Settlements Programme; 2008. Report No.: ISBN: 978-1-84407-696-3.
- Mowla, Q.; Islam, M. Natural Drainage System and Water Logging in Dhaka: Measures to address the Problems. J Bangladesh Inst Plan. 2013, 6, 23–33. [Google Scholar]
- Swapan, M.S.H.; Zaman, A.U.; Ahsan, T.; Ahmed, F. Transforming Urban Dichotomies and Challenges of South Asian Megacities: Rethinking Sustainable Growth of Dhaka, Bangladesh. Urban Sci. 2017, 1, 31. [Google Scholar] [CrossRef]
- Hassan, M.M.; Southworth, J. Analyzing Land Cover Change and Urban Growth Trajectories of the Mega-Urban Region of Dhaka Using Remotely Sensed Data and an Ensemble Classifier. Sustainability 2018, 10, 10. [Google Scholar] [CrossRef]
- Rothfusz, LP. The Heat Index “Equation” (or, More Than You Ever Wanted to Know About Heat Index). Fort Worth, TX: NWS Southern Region Headquarters; 1990. Contract No.: SR 90-23.
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef]
- Chandler RE, Scottt EM, editors. Statistical Methods for Trend Detection and Analysis in the Environmental Sciences. First ed. United Kingdom John Wiley & Sons, Ltd.; 2011.
- Imai, C.; Armstrong, B.; Chalabi, Z.; Mangtani, P.; Hashizume, M. Time series regression model for infectious disease and weather. Environ. Res. 2015, 142, 319–327. [Google Scholar] [CrossRef]
- Hardin JW, Hilbe JM, editors. Generalized Linear Models and Extensions 2nd ed. Texas 77845: Stata Press; 2007.
- Shumway RH, Stoffer DS, editors. Time Series Analysis and Its Applications Fourth ed. Switzerland Springer International Publishing AG; 2017.
- Warton, D.I.; Lyons, M.; Stoklosa, J.; Ives, A.R. Three points to consider when choosing a LM or GLM test for count data. Methods in Ecology and Evolution 2016, 7, 882–890. [Google Scholar] [CrossRef]
- Yin, Q.; Wang, J. A better indicator to measure the effects of meteorological factors on cardiovascular mortality: heat index. Environ Sci Pollut Res Int. 2018, 25, 22842–22849. [Google Scholar] [CrossRef]
- Nissan, H.; Burkart, K.; Perez ECd Aalst, M.V.; Mason, S. Defining and Predicting Heat Waves in Bangladesh. Journal of Applied Meteorology and Climatology 2017, 56. [Google Scholar] [CrossRef]
- Touloumi, G.; Atkinson, R.; Le Tertre, A.; Samoli, E.; Schwartz, J.; Schindler, C.; Vonk, J.M.; Rossi, G.; Saez, M.; Rabszenko, D.; et al. Analysis of health outcome time series data in epidemiological studies. Environmetrics 2004, 15, 101–117. [Google Scholar] [CrossRef]
- Barnet, A.G.; Tong, S.; Clements, A.C.A. What measure of temperature is the best predictor of mortality? Environmental Research 2010, 110, 604–611. [Google Scholar] [CrossRef] [PubMed]
- NWS. What is the heat index? Amarillo, TX: National Weather Service; 2021. Available online: https://www.weather.gov/ama/heatindex.
- Gerba, C.P.; Rose, J.B.; Haas, C.N. Sensitive populations: who is at the greatest risk? Int J Food Microbiol. 1996, 30, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Etzel, R.A.; Su, H.; Huang, C.; Guo, Y.; Tong, S. Impact of ambient temperature on children's health: A systematic review. Environ. Res. 2012, 117, 120–131. [Google Scholar] [CrossRef]
- Xu Z, Huang C, Turner LR, Su H, Qiao Z, Tong S. Is diurnal temperature range a risk factor for childhood diarrhea? PLoS One. 2013;8(5):e64713.
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef]
- Stafoggia M, Forastiere F, Agostini D, Biggeri A, Bisanti L, Cadum E, et al. Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology. 2006;17(3):315-23.
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: who is at risk? Occup Environ Med. 2007, 64, 93–100. [Google Scholar] [CrossRef]
- Liu, C.; Yavar, Z.; Sun, Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Circ. Physiol. 2015, 309, H1793–H1812. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).