1. Introduction
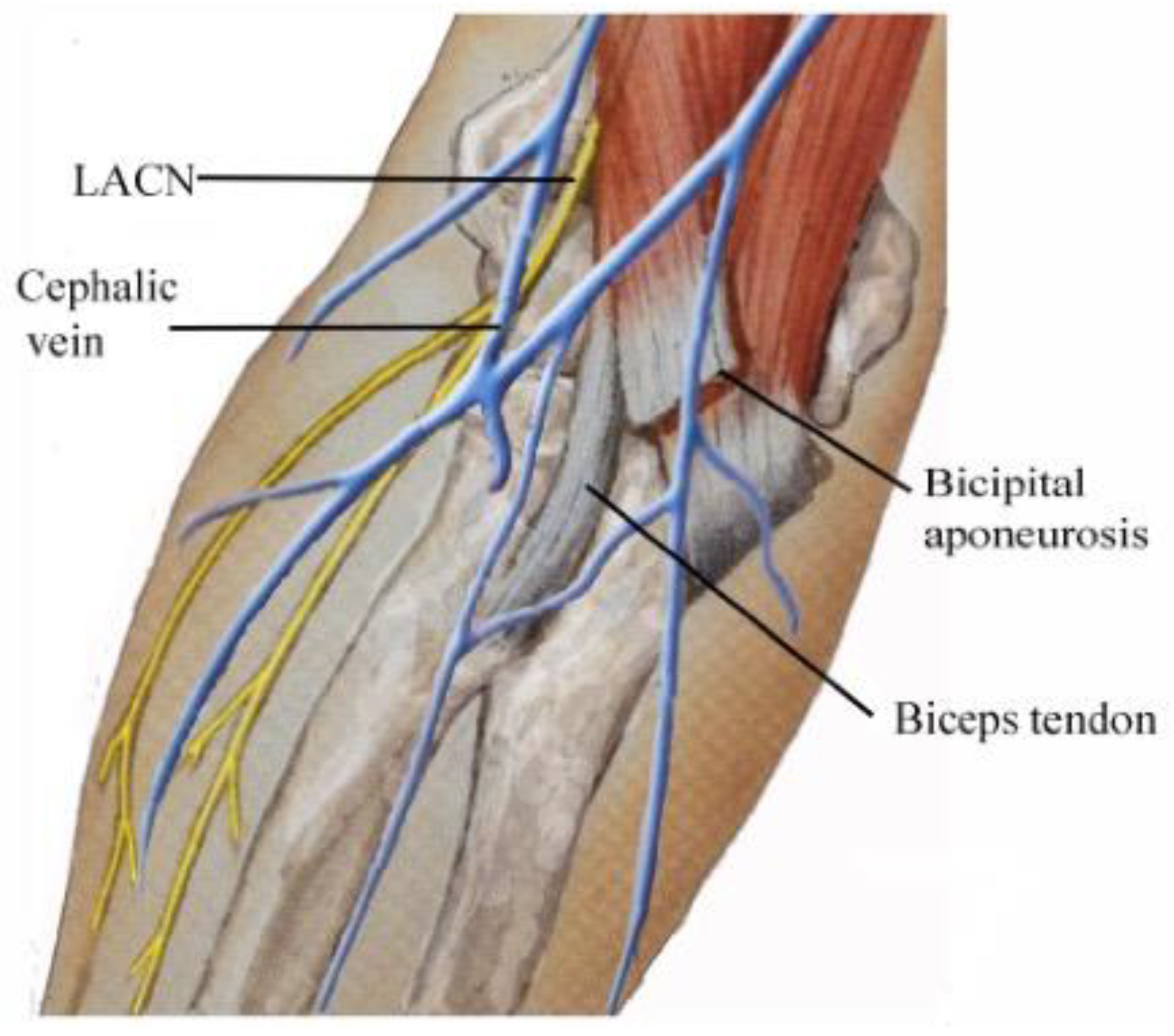
The lateral antebrachial cutaneous nerve (LACN) is the distal sensory termination of the musculocutaneous nerve in the lateral aspect of the forearm [
1,
2,
3,
4,
5]. Due to its anatomical proximity to the biceps brachii tendon, lateral epicondyle, antebrachial vein, and cephalic vein (
Figure 1), the LACN is prone to iatrogenic injuries during repair of the biceps tendon [
4,
6,
7,
8,
9,
10], phlebotomy [
4,
11,
12,
13,
14,
15], prolonged use of retractors by surgical assistants [
16], positional pressure during prolonged surgery [
17], and steroid injection at the lateral epicondyle [
18]. Entrapment neuropathy of the LACN may occur at the lateral margin of the biceps tendon/bicipital aponeurosis or at the site of emergence of the nerve through the deep fascia [
1,
2,
3,
4,
5,
16,
19,
20,
21,
22,
23,
24].
Dynamic compression at potential entrapment sites of the LACN during activities that require forcible elbow flexion/extension or forearm pronation has been postulated as an etiology of LACN neuropathy [
1,
2]. This condition has been associated with a variety of physical activities causing stretch injuries, occurring in high-level pitchers [
25], throwing athletes [
26], windsurfers [
27], swimmers (backstroke) [
28], tennis players (forceful overhead tennis stroke with the forearm pronated) [
28], racquetball (backhand stroke) [
28], restaurant servers from pressure on the lateral bicipital tendon by edges of heavy trays [
29], boxers (following a punch in forceful elbow extension and forearm pronation) [
30], basketball players (slam-dunking basketball and hanging on the rim) [
28], repetitive forearm use while gardening [
4], and photographers carrying a camera bag with the strap draped over the antecubital fossa for prolonged period of time (“handbag paresthesia”) [
31].
Electrodiagnostic (EDX) studies are a valuable diagnostic tool in the evaluation of patients with pain and/or paresthesia of the forearm in sensory nerve abnormalities. Characteristic findings of LACN neuropathy in the symptomatic forearm include sensory nerve action potentials (SNAPs) that are either absent, have a prolonged distal latency, or have a decreased amplitude compared to the asymptomatic side [
2,
18,
29].
While there are many anecdotal reports of LACN neuropathy, there are few large series, leading to insufficient data regarding the causes of LACN neuropathy. The study of EDX confirmed cases of LACN neuropathy is a valuable source of insight into this rare focal neuropathy of upper extremity. In this report, the clinical and EDX findings of 49 patients with LACN neuropathy confirmed by EDX studies are described with discussion focusing on the etiology.
2. Materials and Methods
2.1. Electrodiagnostic Studies
Under an Institutional Review Board (IRB)-approved protocol, we performed a 13-year (2/8/2010-6/22/2023) retrospective analysis of patients with pain and/or paresthesia of the forearm referred for EDX studies. The patients underwent a focused neurological examination of the upper extremities followed by nerve conduction velocity (NCV) and needle EMG studies. The EDX studies were performed in our American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM)-accredited facility. The LACN nerve conduction studies (NCS) were conducted according to the technique described by Buschbacher and colleagues [
32].
2.2. Inclusion and Exclusion Criteria
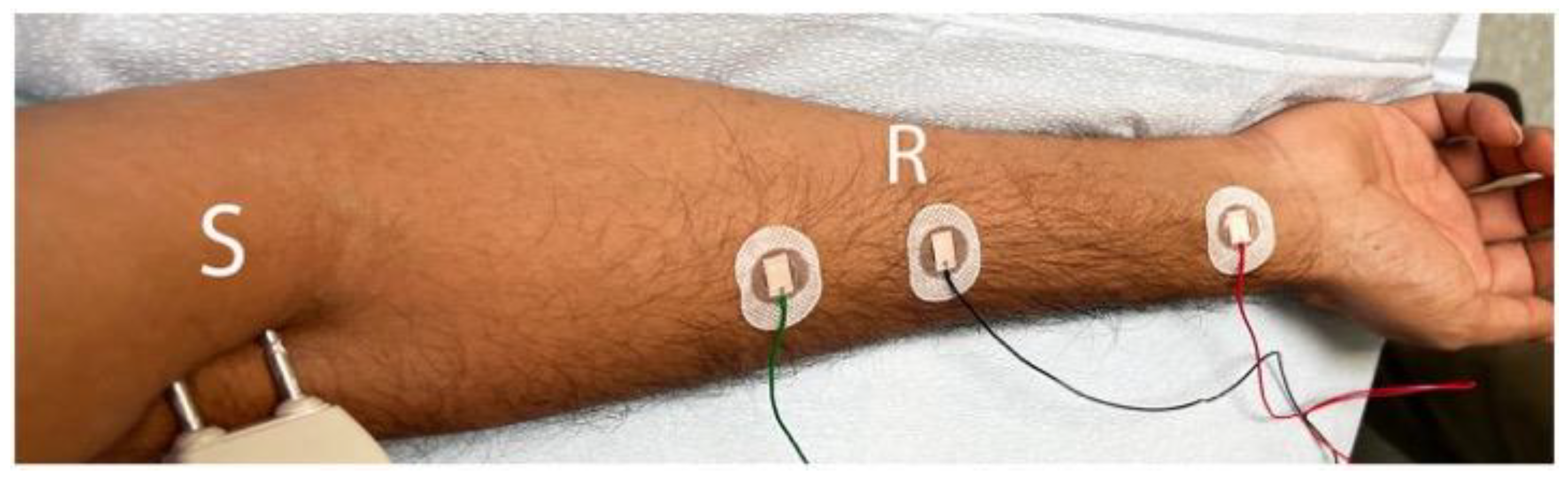
Inclusion criteria were: (1) sensory disturbance (pain/paresthesia/hypoesthesia/allodynia) in the lateral aspect of the forearm and (2) NCS show absence of sensory nerve action potentials (SNAPs) over the LACN; peak to peak amplitude less than 50% of the unaffected side; or peak latency which is twice or more than that of the unaffected side. The nerve was stimulated at the distal upper arm just lateral to the biceps tendon (S), and the recording electrode (R) was placed 10 cm distally on a line to the radial pulse (
Figure 2). A peak latency ≥ 2.6 ms and peak to peak amplitude of ≤ 3 μV were considered abnormal [
32]. The asymptomatic side was studied for comparison. Median, ulnar, superficial radial, and medial antebrachial cutaneous nerves were also studied along with needle EMG of the upper extremity muscles to confirm or rule out brachial plexopathy/cervical radiculopathy.
Several metrics were collected including the patients’ gender and age, laterality (left/right), symptom onset (acute/chronic), symptoms (pain/paresthesia/numbness) and signs (hypoesthesia/dysesthesia) in the distribution of the LACN, SNAP findings (absent/decreased amplitude/increased latency), and clues to the etiology of the LACN neuropathy.
2.3. Institutional Review Board Approval of Research
Informed consent was obtained from all patients. The IRB determined that our study was exempt under 45 CFR 46.104(d)(4). The IRB number is 23-N0146. The IRB approval date was July 25, 2024.
3. Results
3.1. Demographics
A total of 49 patients were diagnosed with LACN neuropathy based on clinical and EDX findings (
Table 1). The mean age was 48.4 years (range: 16-81 years), and the majority (31 [63.3%]) of patients were male. The LACN neuropathy was more common on the right side (28 [57.1%]). Forty-three (87.8%) patients were right hand dominant, 3 (6.1%) were left hand dominant, and 3 (6.1%) were ambidextrous. The symptomatic side corresponded to hand dominance in 8 (57.1%) patients. A total of 44 (89.8%) patients had an acute onset of symptoms, while 5 (10.2%) experienced a gradual onset.
3.2. Etiologies
The most common etiology of LACN neuropathy was iatrogenic injury in 30 (61.2%) patients, primarily due to biceps tendon repair at the elbow (11 [36.7%]) and phlebotomy (5 [16.7%] (
Table 1). Two patients underwent intense physical therapy several weeks following shoulder replacement surgery which created symptoms of LACN neuropathy. Fifteen (30.6%) patients experienced non-iatrogenic injury at the proximal forearm/elbow, with 6 (40.0%) sustaining a laceration injury and 5 (33.3%) incurring a stretch injury. Patients with stretch injuries gave a history of prolonged pronation with flexion/extension of the elbow prior to symptom onset and consisted of the following: (1) driving with the upper extremity in a prolonged elbow flexion/pronation position; (2) prolonged forcible stretching of the elbow; (3) practicing the violin for several hours a day (severe pain and paresthesia after keeping the bow hand flexed at the elbow with the forearm pronated); and (4) prolonged deep sleep from medication overuse (the hand was in a tightly flexed and pronated position for several hours). Four (8.2%) patients comprised the “other” etiology category. Two of these patients had mass lesions (a cystic lesion and a lipoma) at the volar aspect of the elbow/distal upper arm causing compression of the LACN. The other two did not have a discernable cause and presumably represent entrapment neuropathies.
3.3. Signs and Symptoms of LACN Neuropathy
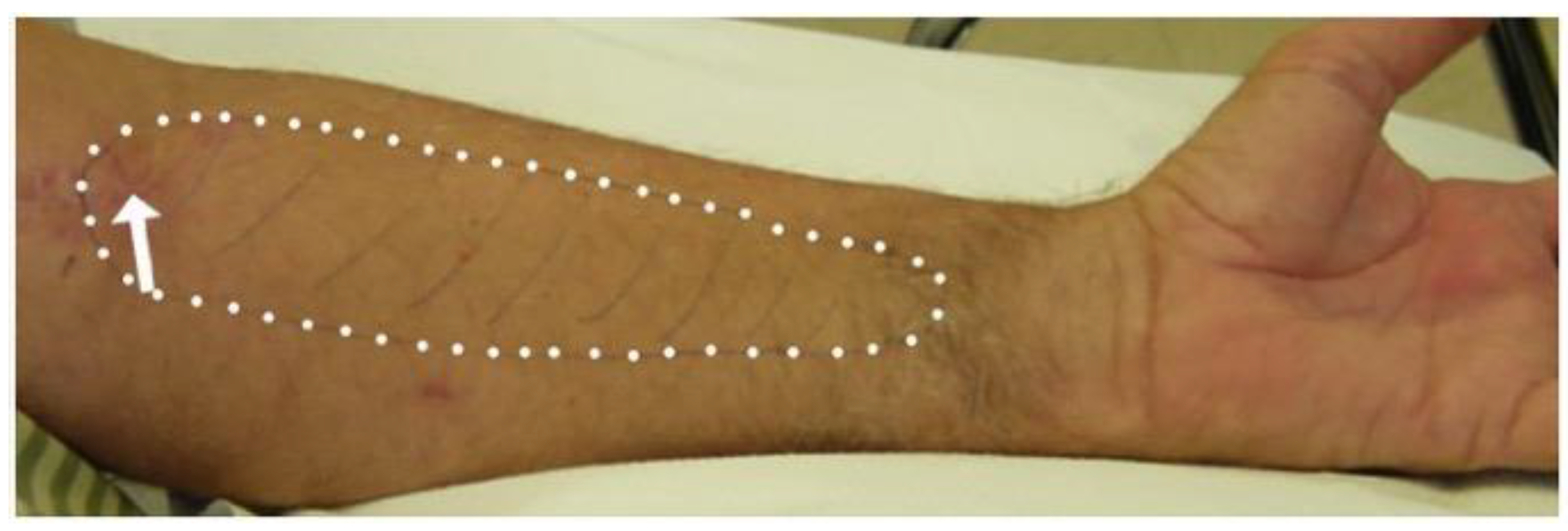
At presentation, pain, paresthesia, and/or numbness in the distribution of the LACN were reported in 33 (67.3%), 27 (55.1%), and 23 (46.9%) patients, respectively (
Table 1) (
Figure 3). Hypoesthesia was detected in 45 (91.8%) patients, and dysesthesia was noted in 7 (14.3%).
3.4. Electrodiagnostic Studies
The SNAPs of the LACN on the symptomatic side were absent in 44 (89.8%) patients (
Table 1). Of the 5 patients whose SNAPs of the LACN were detected, all had a decreased amplitude and 2 had an increased latency.
3.5. Illustrative Cases
Patient 1
A 57-year-old male complained of numbness of the skin in the left forearm soon after undergoing repair of a ruptured distal biceps tendon by single incision technique under regional block anesthesia. Decreased pinprick and light touch over the volar lateral aspect of the forearm were noted. EDX revealed absent SNAP over the left LACN. The clinical picture suggested iatrogenic injury to the LACN. The symptoms gradually improved over 6 months.
Patient 2
A 28-year-old male complained of paresthesia and pain involving the lateral aspect of the right forearm. The description was a “shock in my right forearm after playing the violin for extended periods of time.” The symptoms were noted primarily when straightening the elbow after keeping it in a flexed and pronated position while holding the bow. A decrease in pinprick sensation over the lateral aspect of the forearm was noted, and no SNAP over the right LACN were detected. Corticosteroid injections in the antecubital fossa lateral to the biceps brachii tendon and limiting the number of hours on the violin led to significant improvement within 2 weeks.
Patient 3
A 40-year-old female underwent a surgical procedure in the proximal forearm to remove a mass which caused pain along the lateral aspect of the forearm and the thumb. Biopsy of the mass revealed a granular cell tumor. The mass was resected along with the brachioradialis muscle into which it had grown. The patient was referred to our Neurodiagnostic Center 6 months postoperatively for numbness of the left forearm and thumb. EDX demonstrated absent SNAP of the left LACN, and the superficial radial nerve confirming nerve injury. The etiology was considered to be iatrogenic injury during tumor excision.
Patient 4
An 81-year-old female reported a 2-month history of pain and paresthesia of the elbow and lateral aspect of the right forearm and a “painful knot” in the distal upper arm above the elbow. Neurological examination revealed decreased pinprick sensation over the anterolateral aspect of the right forearm and a tender nodular swelling over the distal right upper arm. Tinel sign was positive over the swelling which caused a “shock-like” sensation over the lateral forearm. The SNAP was absent over the right LACN. A cystic lesion was detected by US in the distal lateral upper arm. The patient refused surgical intervention.
Patient 5
A 37-year-old female complained of painful paresthesia of the lateral aspect of left forearm after venipuncture at the antecubital fossa. The patient experienced severe sharp pain and electric shock-like sensation in the forearm during the procedure. An area of allodynia in the volar lateral aspect of the left forearm was noted. SNAP was absent over the left LACN. Following treatment with gabapentin, the symptoms resolved after 3-4 months without the need for surgical intervention.
4. Discussion
4.1. Iatrogenic Injuries
Iatrogenic LACN injury has been reported as a complication of distal biceps tendon repair, with the complication rate varying depending upon the surgical technique [
7,
8,
9]. The complication is higher after a single-incision procedure compared to a double-incision technique [
7,
9]. In Amin and colleagues’ meta-analysis of single-incision versus double-incision surgical techniques for distal biceps tendon repair, LACN neuropraxia was the most common complication in the single-incision group (77 of 785 cases [9.9%]) [
7]. LACN neuropraxia occurred in 11 (2.2%) cases in the double-incision group, with a statistically significant difference (< 0.001) between the two incision groups. In Dunphy and colleagues’ study of 784 surgical repairs of distal biceps tendon ruptures, the most common nerve complication involved the LACN (162 [20.7%] patients), with a significantly higher number following a single-incision repair compared to a double-incision repair (24.4% vs. 4.1%, p < 0.001) [
9]. In Carroll and colleagues’ study of neurologic complications of distal biceps tendon repair with a single-incision endo button fixation in 50 patients, LACN injury was the most frequent nerve injury [
8]. These authors reported additional posterior interosseous nerve (PIN), anterior interosseous nerve (AIN), and superficial radial nerve involvement in 4% of patients [
8]. All patients in our series had a single-incision surgery. Of the 11 patients who sustained an iatrogenic injury of the LACN during biceps tendon repair, additional injuries were noted of the superficial radial nerve in 8 (72.3%) patients, PIN in 2 (18.2%), and AIN in 1 (9.1%) by EDX studies. Studies have been conducted to find the optimum trajectory for drilling and placement of the button to avoid injury to the PIN [
33].
LACN injuries are known to complicate phlebotomy, either during routine venipuncture or blood donation [
4,
11,
12,
13,
14,
15,
34]. Due to the close proximity of the LACN to the cephalic and median cubital veins, it is vulnerable to injury during phlebotomy. Injuries of the LACN are likely underrecognized and underreported since this nerve is purely sensory and unaccompanied by motor abnormalities [
13]. It has been suggested that areas immediately lateral to the biceps tendon and medial to the brachioradialis muscle should be avoided during routine antecubital phlebotomy or be performed superficially in this location [
12].
4.2. Non-Iatrogenic Injuries
Non-iatrogenic trauma due to laceration injuries of the volar aspect of the forearm accounted for 6 cases in our study. These injuries occurred in a younger age group compared to the mean age of the entire cohort (32.3 vs. 48.4 years). Compression of the LACN may be result from direct compression or intense physical exertion [
16]. Neuropraxia may develop from compression from the biceps brachii during prolonged positional application [
16]. The mechanism of LACN injury in this setting involves strenuous elbow extension combined with forearm pronation.
4.3. Large Series of LACN Neuropathy in the Literature
Few large series of LACN neuropathy have been reported in the literature (
Table 2) [
1,
4,
5]. In Memon and colleagues’ study of 15 patients with LACN neuropathy, a postsurgical etiology was most common (7 patients) during orthopedic surgeries [
4]. Two of these patients sustained direct surgical trauma, while 5 developed symptoms secondary to arm positioning during shoulder (4 patients) and knee (1 patient) surgeries. Antecubital fossa phlebotomy and intravenous placement were the next most frequent etiologies (4 patients). EDX studies revealed absent or reduced sensory amplitudes in 13 (86.7%) patients. In Naam and colleagues’ study of 23 patients with LACN neuropathy, 8 (34.8%) sustained elbow trauma and 17 (73.9%) were Workers’ compensation cases [
5]. All had positive nerve conduction study findings consistent with LACN dysfunction, without specific details provided. In Davidson and colleagues’ study of 15 patients with LACN neuropathy, neither the etiology nor EDX findings were reported [
1]. The dominant arm was involved in 12 (80%) patients, and 10 (66.7%) had symptoms longer than 6 months in duration. These findings differ from our study that had a lower percentage (57.1%) of patients with dominant arm involvement and a higher percentage (89.8%) with acute symptom onset. Our study concurs with that of Memon et al. with respect to iatrogenic injury during orthopedic surgeries as the leading etiology of LACN neuropathy, followed by injuries during phlebotomy. Both studies also reveal SNAP abnormalities, with 13 (86.7%) patients with absent or reduced sensory amplitude in the Memon et al. study and absent SNAP in 44 (89.8%) patients in the present study.
4.4. Electrodiagnostic Studies
Elbow pain and paresthesia of the forearm are common reasons for referral for EDX studies. The clinical evaluation can provide important clues to the diagnosis, but poor objectivity of the sensory examination can lead to errors. When the paresthesia involves primarily the lateral aspect of the forearm, the differential diagnosis includes a cervical radiculopathy (C5, C6), brachial plexus injury (lateral cord, upper trunk), pronator teres syndrome, biceps tendonitis, radial tunnel syndrome, Parsonage-Turner syndrome, radial and median nerve neuropathies at the level of the elbow, and LACN neuropathy [
4,
5,
27]. EDX studies are often useful in clarifying the correct diagnosis.
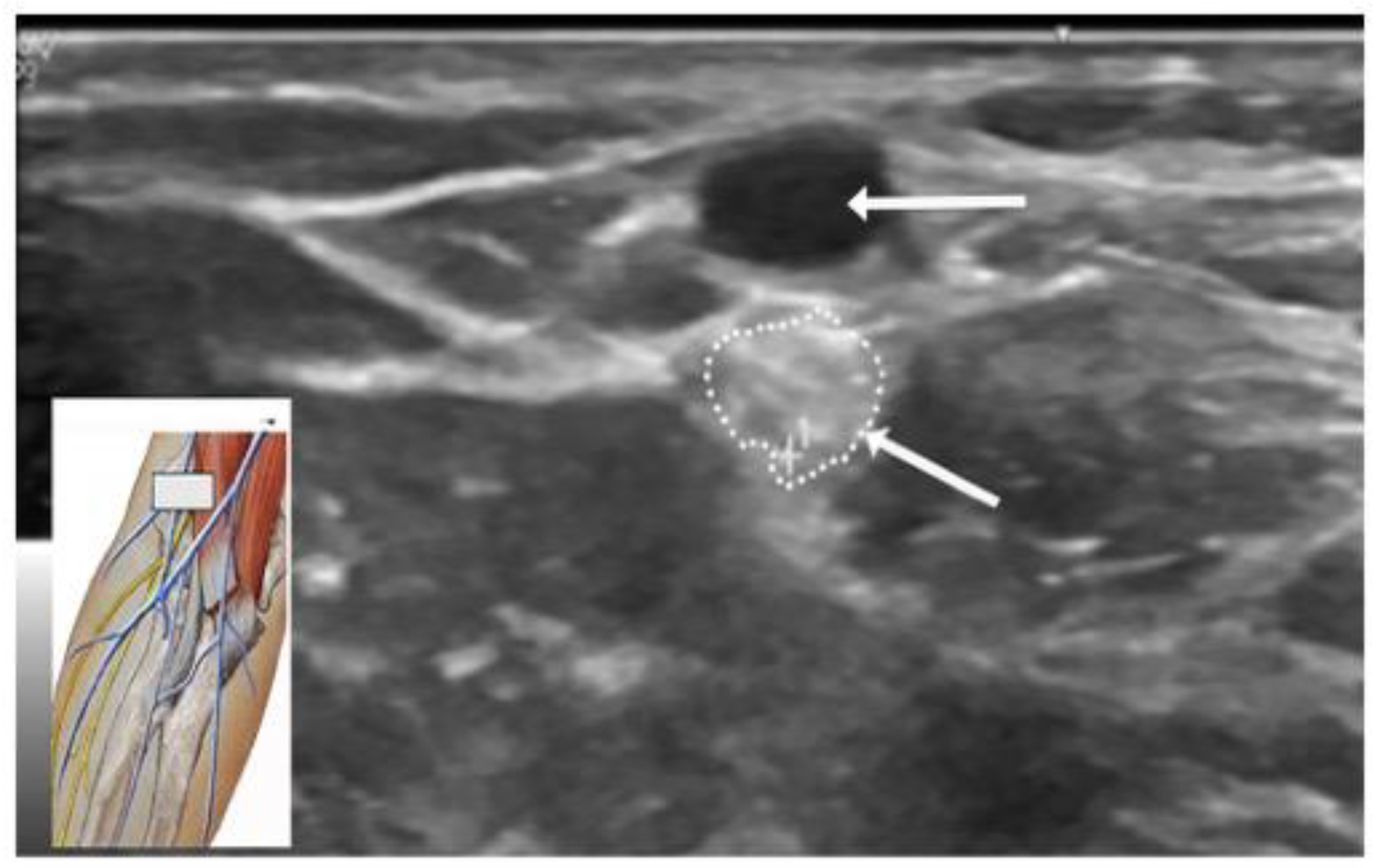
4.5. Ultrasound Studies
US studies may assist in the diagnostic evaluation of LACN neuropathy by differentiating various conditions with symptoms involving the upper arm, elbow, forearm, and wrist [
35]. US has important role in the localization and determining the etiology of LACN neuropathy. In Chiavaras and colleagues’ study of US of the LACN with MRI and anatomic correlation in 13 patients with LACN neuropathy, the symptomatic LACN demonstrated fusiform enlargement, increased echogenicity, and loss of the normal fascicular echotexture [
35]. The mean cross-sectional area of the symptomatic LACN was 12.0 mm
2 compared to 3.3 mm
2 at the same level in the contralateral normal side. While only 7 patients in our series underwent an US study, it was valuable in providing details of the masses in the upper extremity compressing the LACN.
Figure 4 depicts the US study involving injury to the LACN from phlebotomy.
4.6. Strengths and Limitations
The strength of the current study is that it consists of the largest number of patients with LACN neuropathy in the literature, confirmed by EDX studies. By determining the etiology of all patients with LACN neuropathy, prophylactic measures can be instituted to avoid injury to the nerve as well as the most effective treatment course can be pursued. Limitations of the present study include its retrospective nature and lack of follow-up after the EDX studies as most patients were evaluated only once at our Neurodiagnostic Center.
5. Conclusion
LACN neuropathy should be considered in the differential diagnosis of patients presenting with pain, paresthesia, or numbness of the forearm, especially after surgical procedures such as biceps tendon repair or activities involving prolonged flexion/extension at the elbow and pronation of the forearm. Without a high index of clinical suspicion and performance of nerve conduction studies of the LACN, such cases may be missed. Protecting the LACN during surgical procedures at the elbow and upper arm may avoid perioperative injury.
Author Contributions
Conceptualization, V.I. and L.S.; Methodology, V.I. and L.S.; Software, V.I., L.S., Y.Z.; Validation, V.I., L.S., Y.Z., and C.S.; Formal Analysis, V.I., L.S. Y.Z., and C.S.; Investigation, V.I., L.S., Y.Z., and C.S.; Resources, V.I., L.S., Y.Z., and C.S.; Data Curation, V.I., L.S., Y.Z., and C.S.; Writing – Original Draft Preparation, V.I.; Writing – Review & Editing, V.I., L.S. Y.Z., and C.S.; Visualization, V.I., L.S., Y.Z., and C.S.; Supervision, V.I., L.S., and C.S.; Project Administration, V.I., L.S., and C.S.; Funding Acquisition, This research received no external funding.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the WCG The IRB determined that our study was exempt under 45 CFR 46.104(d)(4). The IRB number is 23-N0146. The IRB approval date was July 25, 2024.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All of the data for this study is included in the current article.
Acknowledgments
We acknowledge Norton Healthcare for their continued support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Davidson, J.J.; Bassett, F.H.; Nunley, J.A. Musculocutaneous nerve entrapment revisited. J. Shoulder Elbow Surg. 1998, 7, 250–5. [Google Scholar] [CrossRef] [PubMed]
- Felsenthal, G.; Mondell, D.L.; Reischer, M.A.; Mack, R.H. Forearm pain secondary to compression syndrome of the lateral cutaneous nerve of the forearm. Arch. Phys. Med. Rehabil. 1984, 65, 139–41. [Google Scholar] [PubMed]
- Khadanovich, A.; Benes, M.; Kaiser, R.; Herma, T.; Kachlik, D. Clinical anatomy of the lateral antebrachial cutaneous nerve: is there any safe zone for interventional approach? Ann. Anat. 2024, 252, 152202. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.B.; Mahmood, S.; Waseem, F.; Sherburn, F.; Nardone, A.; Ahmad, B.K. Lateral antebrachial cutaneous neuropathy: a review of 15 cases. Cureus. 2022, 14, e25203. [Google Scholar] [CrossRef] [PubMed]
- Naam, N.H.; Massoud, H.A. Painful entrapment of the lateral antebrachial cutaneous nerve at the elbow. J. Hand. Surg. Am. 2004, 29, 1148–53. [Google Scholar] [CrossRef]
- Amarasooriya, M.; Bain, G.I.; Roper, T.; Bryant, K.; Iqbal, K.; Phadnis, J. Complications after distal biceps tendon repair: a systematic review. Am. J. Sports. Med. 2020, 48, 3103–11. [Google Scholar] [CrossRef]
- Amin, N.H.; Volpi, A.; Lynch, T.S.; Patel, R.M.; Cerynik, D.L.; Schickendantz, M.S.; Jones, M.H. Complications of distal biceps tendon repair: a meta-analysis of single-incision versus double-incision surgical technique. Orthop. J. Sports. Med. 2016, 4, 2325967116668137. [Google Scholar] [CrossRef]
- Carroll, M.J.; DaCambra, M.P.; Hildebrand, K.A. Neurologic complications of distal biceps tendon repair with 1-incision endobutton fixation. Am. J. Orthop. 2014, 43, E159–E162. [Google Scholar]
- Dunphy, T.R.; Hudson, J.; Batech, M.; Acevedo, D.C.; Mirzayan, R. Surgical treatment of distal biceps tendon ruptures: an analysis of complications in 784 surgical repairs. Am. J. Sports Med. 2017, 45, 3020–9. [Google Scholar] [CrossRef]
- Ly, T.; Pasternak, I.; Meuli-Simmen, C.; Mauler, F. Iatrogenic rerouting of the lateral antebrachial cutaneous nerve during distal biceps tendon repair: a case report. JSES Open Access. 2017, 1, 139–40. [Google Scholar] [CrossRef] [PubMed]
- Ramos, J.A. Venipuncture-related lateral antebrachial cutaneous nerve injury: what to know? Braz. J. Anesthesiol. 2014, 64, 131–3. [Google Scholar] [CrossRef] [PubMed]
- Rayegani, S.M.; Azadi, A. Lateral antebrachial cutaneous nerve injury induced by phlebotomy. J. Brachial. Plex. Peripher. Nerve Inj. 2007, 2, 6. [Google Scholar] [CrossRef]
- Sander, H.W.; Conigliari, M.F.; Masdeu, J.C. Antecubital phlebotomy complicated by lateral antebrachial cutaneous neuropathy. N. Engl. J. Med. 1998, 339, 2024. [Google Scholar] [CrossRef] [PubMed]
- Stitik, T.P.; Foye, P.M.; Nadler, S.F.; Brachman, G.O. Phlebotomy-related lateral antebrachial cutaneous nerve injury. Am. J. Phys. Med. Rehabil. 2001, 80, 230–4. [Google Scholar] [CrossRef]
- Yuan, R.T.; Cohen, M.J. Lateral antebrachial cutaneous nerve injury as a complication of phlebotomy. Plast. Reconstr. Surg. 1985, 76, 299–300. [Google Scholar] [CrossRef]
- Seoighe, D.M.; Baker, J.F.; Mulhall, K.J. Surgical trainees neuropraxia? An unusual case of compression of the lateral cutaneous nerve of the forearm. Orthop. Traumatol. Surg. Res. 2010, 96, 603–5. [Google Scholar] [CrossRef] [PubMed]
- Judge, A.; Fecho, K. Lateral antebrachial cutaneous neuropathy as a result of positioning while under general anesthesia. Anesth. Analg. 2010, 110, 122–4. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, S.H. Lateral antebrachial cutaneous neuropathy after steroid injection at lateral epicondyle. J. Back Musculoskelet. Rehabil. 2015, 28, 419–22. [Google Scholar] [CrossRef]
- Allen, D.M.; Nunley, J.A. Lateral antebrachial cutaneous neuroapthy. Oper. Techn. Sport Med. 2001, 9, 222–4. [Google Scholar] [CrossRef]
- Bassett, F.H.; Nunley, J.A. Compression of the musculocutaneous nerve at the elbow. J, Bone Joint Surg. Am. 1982, 64, 1050–2. [Google Scholar] [CrossRef]
- Belzile, E.; Cloutier, D. Entrapment of the lateral antebrachial cutaneous nerve exiting through the forearm fascia. J. Hand Surg. Am. 2001, 26, 64–7. [Google Scholar] [CrossRef]
- Dailiana, Z.H.; Roulot, E.; Le, V.D. Surgical treatment of compression of the lateral antebrachial cutaneous nerve. J. Bone Joint Surg. Br. 2000, 82, 420–3. [Google Scholar] [CrossRef] [PubMed]
- Gillingham, B.L.; Mack, G.R. Compression of the lateral antebrachial cutaneous nerve by the biceps tendon. J. Shoulder Elbow Surg. 1996, 5, 330–2. [Google Scholar] [CrossRef] [PubMed]
- Narasanagi, S.S. Compression of lateral cutaneous nerve of forearm. Neurol. India 1972, 20, 224–5. [Google Scholar]
- von Bergen, T.N.; Lourie, G.M. Etiology, diagnosis, and treatment of dynamic nerve compression syndromes of the elbow among high-level pitchers: a review of 7 cases. Orthop. J. Sports Med. 2018, 6, 2325967118807131. [Google Scholar] [CrossRef]
- Alberta, F.G.; Elattrache, N.S. Diagnosis and treatment of distal biceps and anterior elbow pain in throwing athletes. Sports Med. Arthrosc. Rev. 2008, 16, 118–23. [Google Scholar] [CrossRef]
- Jablecki, C.K. Lateral antebrachial cutaneous neuropathy in a windsurfer. Muscle Nerve. 1999, 22, 944–5. [Google Scholar] [CrossRef]
- Giannoulis, F.; Papoulidis, N.G.; Krexi, A.V. Lateral antebrachial nerve entrapment in compressive neuropathies of the upper extremity. In Compressive Neuropathies of the Upper Extremity: A Comprehensive Guide to Treatment, 1st ed.; Sotereanos, D.G., Papatheodorou, L.K., Eds.; Springer: Cham, Switzerland, 2020; pp. 217–223. [Google Scholar]
- Patel, C.; Vishnubhakat, S. Compression of lateral antebrachial cutaneous nerve in waitresses. J. Clin. Neuromuscul. Dis. 2015, 16, 121–4. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Bassini, L.; Magill, R. Compression neuropathy of the lateral antebracheal cutaneous nerve. Orthopedics. 1991, 14, 173–4. [Google Scholar] [CrossRef]
- Hale, B.R. Handbag paraesthesia. Lancet. 1976, 2, 470. [Google Scholar] [CrossRef]
- Buschbacher, R.; Koch, J.; Emsley, C.; Katz, B. Electrodiagnostic reference values for the lateral antebrachial cutaneous nerve: standardization of a 10-cm distance. Arch. Phys. Med. Rehabil. 2000, 81, 1563–6. [Google Scholar] [CrossRef] [PubMed]
- Mwaturura, T.; Peters, M.J.; Glaris, Z.; Goetz, T.J. Safe drill trajectory for anatomic repair of distal biceps tendon through a single incision: a cadaveric study. J. Hand Surg. Am. 2023, 48, 1160. [Google Scholar] [CrossRef] [PubMed]
- Stevens, R.J.; Mahadevan, V.; Moss, A.L. Injury to the lateral cutaneous nerve of forearm after venous cannulation: a case report and literature review. Clin. Anat. 2012, 25, 659–62. [Google Scholar] [CrossRef] [PubMed]
- Chiavaras, M.M.; Jacobson, J.A.; Billone, L.; Lawton, J.M.; Lawton, J. Sonography of the lateral antebrachial cutaneous nerve with magnetic resonance imaging and anatomic correlation. J. Ultrasound Med. 2014, 33, 1475–83. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).