1. Background
Antimicrobial resistance (AMR) is a persistent global health challenge resulting in approximately 700,000 deaths each year worldwide [
1]. AMR is a problem both in high-income countries (HICs) and low- and middle-income countries (LMICs); however, its effect is more pronounced in the latter. The challenges in LMICs include higher rates of infectious diseases, limited access to new antibiotics, and significant misuse of antibiotics, contributing to a higher prevalence of AMR [
2]. In these regions, the misuse and overuse of antibiotics, coupled with inadequate sanitation and infection control practices, have accelerated the spread of resistant strains leading to increased morbidity and mortality rates. This contributes to a substantial financial burden on already strained healthcare systems [
3,
4].
HICs, while better equipped to manage AMR, are not immune to its effects. For example, ineffective prescribing practices and inefficient waste management systems have increased the burden of AMR [
5]. Without effective interventions, it is projected that AMR could cause up to 10 million deaths annually [
2,
3], and 4.1 million deaths annually in Africa alone by 2050 if current trends continue unchecked [
1,
6] Additionally, the availability of antimicrobial stewardship (AMS) programs and infection prevention and control measures is significantly lower in LMICs compared to HICs. For instance, only 42% of LMIC healthcare facilities have formal AMS programs, compared to 76% in HICs [
6]. AMR is not only a health crisis but also poses a severe economic threat. It is projected to cause a 2% reduction in global GDP to 3.5% by 2050, potentially resulting in a loss of between
$60 trillion and
$100 trillion in economic output if not addressed [
7]. The rise in treatment costs is due to poor antibiotic prescribing practices, rendering commonly used, accessible antibiotics ineffective, resulting in the need for more costly and vigorous treatments, extended hospital stay, and the increased need for isolation beds [
8]. This underscores the urgent need for effective AMS programs and global collaboration to mitigate its impact across all socio-ecological levels.
To manage this ongoing crisis, many countries have developed AMS programs to optimise the use of antimicrobial medications, encourage justifiable use of antibiotics and reduce healthcare costs with the rational use of antimicrobial medications [
9]. Common AMS strategies used globally to tackle AMR include: setting up an AMS working group or committee, consisting of physicians, nurses and pharmacists; developing, publishing and utilising national or local antimicrobial guidelines; developing and delivering Continuous Professional Development (CPD) courses and education and training to raise awareness of AMR, best practice recommendations for antimicrobial prescribing, use and surveillance [
10].
Implementing AMS interventions in LMICs is accompanied with several significant barriers that impede their effectiveness. A primary challenge is the limited availability and high cost of antimicrobials, which complicates access to essential medications and undermines stewardship efforts [
11]. Additionally, there is often resistance among healthcare providers to alter established prescribing practices, largely due to insufficient awareness and education regarding AMR and AMS principles. The lack of access to diagnostic tools and laboratory services for a high proportion of healthcare facilities and where these do exist, accurate and timely results are challenged by capacity / skilled personnel further exacerbates the situation. Systemic issues, such as inadequate healthcare infrastructure, limited human resources, and insufficient funding for healthcare initiatives, also hinder the establishment and sustainability of stewardship programs[
12]. Moreover, cultural and contextual factors, including the prevailing clinical environment and healthcare system dynamics, often deprioritize AMS [
11]. Addressing these barriers requires a comprehensive approach that encompasses improving access to affordable antimicrobials, enhancing diagnostic capabilities, increasing provider education, and strengthening healthcare infrastructure. Collaborative efforts among healthcare teams and institutions are essential to overcome these challenges and implement effective AMS interventions in LMICs [
10,
13].
A hub-and-spoke model (HSM) involves a central “hub”, usually a centre of excellence which provides guidance, resources, and expertise to smaller, peripheral facilities, or “spokes”. The HSM is frequently used in HICs to improve access and service provision [
14,
15] and has been particularly effective in addressing healthcare inequities. Various applications of the HSM have been reported, such as tele-oncology within the Veterans Health Administration, where it has improved access to specialised cancer care and reduced travel for patients [
15]. In Sicily, the HSM has been successfully implemented in neurorehabilitation, leading to increased admissions and improved care, resulting in reducing unnecessary patient transfers across regions [
16]. In the context of LMIC’s the HSM has been extensively applied to enhance service delivery and improve patient outcomes [
17,
18]. This model is well-suited to resource-limited health systems, as it connects well-equipped central facilities (hubs) with peripheral facilities (spokes) to provide technical assistance, expertise, and resources, including learning materials and trained healthcare professionals [
18]. For example, in South Africa’s Northern Cape province, the Cancer ECHO (Extension of Community Healthcare Outcomes) Model was implemented to address disparities in cancer care; a central hub at a tertiary cancer centre provided training and mentorship to healthcare workers in rural district hospitals, improving access to cancer diagnosis and treatment in these underserved areas [
19]. In India, the HSM was used during the COVID-19 pandemic to deliver online cancer screening training programs for healthcare providers [
20]. Additionally, another study from India employed the HSM to deliver super-specialty medical teleconsultations to remote areas, enhancing access to specialised care through telemedicine platforms [
21]. These initiatives illustrate the model’s effectiveness in expanding specialised healthcare and improving outcomes in HICs and LMICs.
Although individual studies have highlighted the application and utility of the HSM, there is limited evidence of its evaluation in the AMS context. The primary aim of this scoping review was to explore the application of the HSM and review the barriers and facilitators in AMS.
2. Methods
The review was undertaken with reference to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-ScR) to ensure that essential reporting items were included [
22].
2.1. Search Strategy
The search strategy was designed in line with the following research questions:
How many studies has the HSM been applied to deliver AMS programs?
What has been the efficacy of the HSM in the AMS context?
What are the barriers and facilitators experienced with the application of HSM in the AMS context?
Keywords such as ‘hub-and-spoke model’, ‘antimicrobial stewardship’, ‘barriers’ and ‘facilitators’ were included in the search strategy. The full list of keywords used is included in Appendix 1.
2.2. Identification of Relevant Studies
Searches were performed by two authors (AI, YK) using four databases and electronic search tools: PubMed, Cochrane Library, ScienceDirect and Google Scholar, which were expected to have studies from healthcare and AMS. All articles were transferred to Rayyan®, as a comma-separated values (CSV) file. Duplicates were identified and removed using the software’s ‘detect duplicates’ feature. The search for articles was limited to peer-reviewed, full text articles published in English. No research design or publication date specific search limits were applied; studies using qualitative, quantitative and mixed methods were included.
2.3. Selection of Relevant Studies
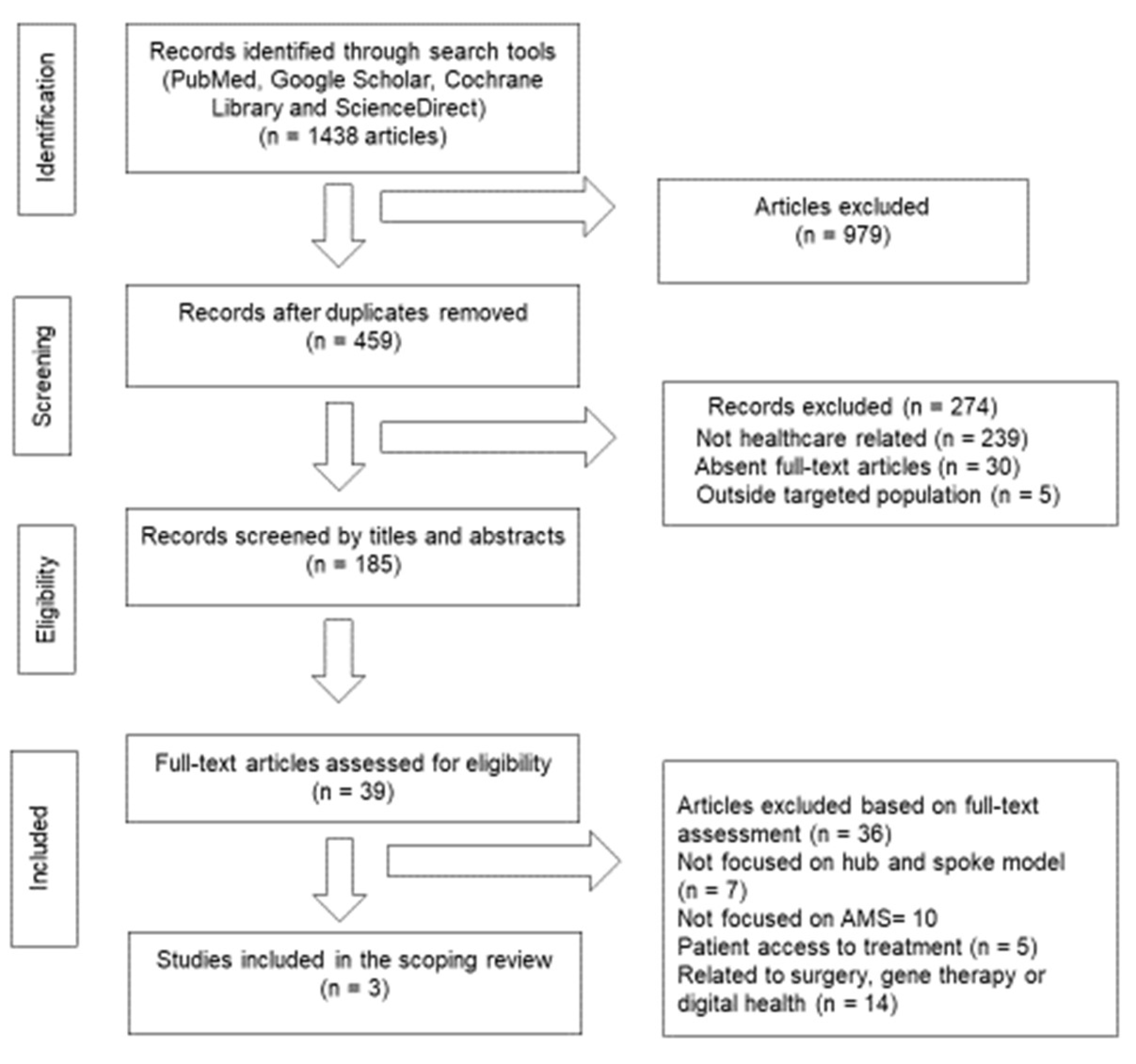
Article titles and abstracts were screened by three authors (AI, YK, GG) according to the eligibility criteria as shown in
Table 1; a fourth author (HR) resolved the conflicts. Articles with insufficient or inadequate information on the application of HSM, and studies emphasising patients’ access to treatment or discussing healthcare models other than HSM were excluded (
Figure 1).
2.4. Data Extraction and Reporting of Findings
The following data were recorded in a data collection form specifically designed for this study: title of article, year of publication, online link to the full-text article, number of hub and spokes, type or structure of the HSM, study design (e.g., quantitative, qualitative or mixed methods), data collection methods, analysis of data, outcomes measured, challenges encountered during the implementation of HSM. The extracted data was narratively synthesised into two subsections: outcomes of the interventions and implementation evaluation.
3. Results
A total of 1,438 articles were retrieved from the search: PubMed: 588, Cochrane Library: 0, ScienceDirect: 379, Google Scholar: 471. . After removing duplicates, 459 articles were left to be screened. The titles and abstracts’ screening stage led to a total of 39 full-text articles to be assessed for eligibility. By the end of the screening process, three articles specifically related to the application of HSM in AMS and/or AMR were included in the scoping review as shown in
Figure 1.
3.1. Characteristics of the Included Studies
Geographically, two of the included studies were from Asia-Pacific regions and one from North America. One study was conducted in a HIC (Canada) while the remaining two studies focused on a LMIC (India). Training healthcare professionals was a common intervention across all studies, while additional interventions delivered through the HSM model are detailed in
Table 2.
Our literature search retrieved three articles - Zacchaeus et al. (2023) [
23], Nakamachi et al. (2015) [
24] and Agarwal et al. (2022) [
25] - demonstrating the efficacy of the HSM to contribute to AMS interventions and initiatives. In the study by Agarwal et al. (2022), the HSM facilitated the implementation of a case-based e-learning initiative to enhance the knowledge and skills of healthcare providers managing Tuberculosis - Human Immunodeficiency Virus (TB-HIV) co-infection. This initiative proved highly effective, with 59 learning sessions conducted, engaging an average of 152 participants per session. The program significantly improved self-efficacy, technical knowledge retention, and clinical practices, leading to better patient outcomes, such as increased TB screening and treatment initiation rates. Similarly, the study by Zacchaeus et al. (2023) highlighted the success of the HSM in implementing AMS programs in secondary-care hospitals in India. The model led to a significant reduction in antimicrobial usage. Additionally, there was a marked increase in antibiotic de-escalation, indicating improved antibiotic management practices. In the study conducted by Nakamachi et al. (2015), the pattern of antibiotic use was prospectively audited at the intensive care units (ICU) of the two participating health science centres. They demonstrated the scalability and standardisation potential of the HSM by expanding AMS programs from well-resourced academic centres to community hospitals. More details about HSM efficacy with respect to focused categories are provided as follows:
3.1.1. Clinical Outcomes
The effectiveness of the HSM was established in two studies, by Zacchaeus et al. (2023) and Agarwal et al. (2022). Before initiating a series of interventions, both studies observed antimicrobial prescribing practices to understand trends. In the former study, a significant reduction in antimicrobial usage and improved antibiotic management was achieved. The primary outcome was a notable decrease in days on antimicrobial therapy per 1,000 patient days, a fall from 1,952.63 at baseline to 1,483.06 in the post-intervention phase (P = 0.001). This reduction suggested a more efficient use of antibiotics. Additionally, there was a marked decrease in the use of specific antibiotics, including quinolones, macrolides, cephalosporins, clindamycin, and nitroimidazoles. The rate of antibiotic de-escalation also increased significantly, from 12.5% at baseline to 44% in the post-intervention phase, reflecting better management and adjustment of antibiotic therapies. HSM efficacy to deliver interventions was also reported in Agarwal et al. (2022). The AMS interventions and initiatives led to an increase in TB screening (4.2%), TB diagnosis (2.7%), antiretroviral therapy centre initiation (4.3%), and TB preventive treatment completion (5.2%).
In the study by Nakamachi et al. (2015) there were no clinical outcomes reported; however, they conducted their programmatic evaluation on-site, three months after the implementation of the project, and demonstrated significant success in standardisation and scalability of the AMS programmes in both academic and community hospitals.
3.1.2. Training and Knowledge of Healthcare Professionals
Training of healthcare professionals on the appropriate use of antibiotics was the only common intervention in all three studies, as shown in
Table 2. Nakamachi et al. (2015) had identified that healthcare professionals were proficient in treating rare or complicated infections but lacked opportunities to apply their knowledge to managing common infectious diseases. To address these knowledge gaps, training modules were developed focusing on various infections of bodily systems, early diagnosis, appropriate antimicrobial treatment, and infection prevention and control. This initiative resulted in mentoring and developing new experts and leaders, particularly in community hospitals without in-house infectious diseases specialists, thereby improving workforce skills.
Agarwal et al. (2022) had a different baseline focus as the research team emphasised on e-learning. The evaluation of the e-learning program revealed positive outcomes in terms of feasibility, acceptability, and impact on knowledge and skills. Participants showed significant improvements in perceived knowledge, skills, and competencies, with an 8.6% increase in self-efficacy and an 18.3% increase in technical knowledge retention from baseline. Specific improvements included a 9.8% increase in the ability to identify TB symptoms in people living with HIV, an 11.4% improvement in diagnosing and treating complicated HIV-TB cases, and an 8.9% enhancement in managing other comorbidities. Furthermore, technical knowledge retention improved, with short-term retention increasing by 16.2% and long-term retention showing an 18.3% improvement from baseline, highlighting the program’s effectiveness in enhancing both immediate and sustained learning outcomes. Feedback on e-learning sessions indicated high levels of satisfaction, with 81% of sessions receiving agreement from at least 80% of respondents that their specific queries were addressed. Additionally, 95% of sessions were rated as having relevant and clear topics, while 88% of sessions were deemed to have an appropriate duration. Expert feedback further supported these findings, with unanimous agreement on the effectiveness of e-learning for capacity building in the AMS context.
Zacchaeus et al. (2023) implemented a blended, customised distance education program designed to equip physicians with the skills necessary to implement and sustain AMS programs. A distinctive aspect of their study from the other two studies was the training of laboratory personnel at the hub site, Christian Medical College, Vellore, to ensure accurate and timely microbial diagnostics. This training focused on cultivating proper sample collection and testing methods, which helped reduce the empirical use of antibiotics and allowed for modifications in pharmacotherapy based on the pathogens’ susceptibility.
3.1.3. Establishment of AMS Programs
AMS programs were established at the spoke sites involved in the studies by Zacchaeus et al. (2023) and Nakamachi et al. (2015). Both studies highlight the importance of tailored strategies and interdisciplinary collaboration in establishing effective AMS programs, with Zacchaeus et al. (2023) focusing on local training and feedback, while Nakamachi et al. (2015) emphasised institutional support and scalability.
In the study by Zacchaeus et al. (2023), the program involved training participating physicians from the spoke sites alongside either a pharmacist or a nurse. This collaborative training aimed to establish and implement the AMS program effectively. The trained physicians were then responsible for providing interventions, which resulted in improved clinical outcomes. In contrast, the study by Nakamachi et al. (2015) initiated the AMS program within academic health science centres before expanding it to five ICUs within these centres. The successful practices from these initial implementations were then leveraged to expand the program to 14 academic hospital ICUs and, eventually, to community hospitals that lacked in-house infectious diseases specialists. An infectious diseases physician and a pharmacist were appointed as subject experts and leads for the AMS program. The hospital’s Vice Presidents were designated as champions for the AMS project, ensuring that spoke sites received coaching throughout the planning, implementation, and evaluation stages.
3.1.4. Development of Antibiograms
Both Nakamachi et al. (2015) and Zacchaeus et al. (2023) developed antibiograms, but they employed contrasting approaches. In the study by Zacchaeus et al. (2023), the spoke centres recorded results from culture and sensitivity tests conducted on urine, sputum, pus, and blood samples starting in July 2019. Additionally, they collected similar data retrospectively from health records dating back one to three years. These sites utilised WHO-net to create antibiograms, benefiting from the expertise and assistance provided by the hub site.
In contrast, the team in Ontario adopted a more technical approach to develop an antimicrobial measure aimed at monitoring antimicrobial usage and resistance. The study did not specify data utilisation for antibiogram development. Leveraging an existing system that collected real-time patient data, they collaborated with Critical Care Services Ontario and CritiCall (the organisation maintaining the information system), to expand their data fields. This expansion included tracking days of antibacterial therapy, days of antifungal therapy, and ICU-onset Clostridium difficile. The comprehensive data collection facilitated the establishment of a framework that was instrumental in creating antimicrobial guidelines and policies tailored to the local context.
3.1.5. Development of Antimicrobial Guidelines and Resources
Antimicrobial guidelines were developed in two studies. Upon receiving adequate data, the hub-and-spoke team in the Zacchaeus et al. (2023) study gained a clear understanding of the necessary content to create facility-specific guidelines. These guidelines addressed several key areas: the availability of antibiotics, commonly used antimicrobials, prophylactic measures for various surgeries, and the management of common post-surgical infections. Furthermore, the team established criteria for healthcare-acquired infections (HAI) by adhering to the guidelines provided by the Centres for Disease Control and Prevention (CDC). In the study by Agarwal et al. (2022), a curriculum was developed based on national TB prevention and management guidelines for people living with HIV. This curriculum was created alongside input from subject matter experts from both the National AIDS Control Programme (NACP) and the National Tuberculosis Elimination Programme (NTEP). This e-learning content provided guidance to healthcare providers enabling them to apply their learning directly to patient care scenarios, thereby improving the quality of care provided to patients with TB-HIV co-infection.
3.2. Intervention Implementation Facilitators
The studies by Agarwal et al. (2022), Zacchaeus et al. (2023), and Nakamachi et al. (2015) each highlight unique facilitators at different socio-ecological levels, contributing to the success of AMS programs. The following text provides an overview of facilitators collectively contributing to the success of each initiative by enhancing AMS through tailored education, collaboration, strategic planning, and data utilisation at various levels of the healthcare system.
3.2.1. Facilitators Targeting Individual Level Factors
At the individual level, Agarwal et al. (2022) emphasised the role of an interactive e-learning platform in enhancing healthcare providers’ knowledge and self-efficacy, leading to increased professional satisfaction as a facilitator to engage and sustain AMS initiatives. Similarly, Zacchaeus et al. (2023) focused on tailored training and education to build confidence and competence among healthcare staff that improved compliance with the AMS programs. Nakamachi et al. (2015) highlighted the importance of strong leadership skills and accountability of dedicated leaders towards successful implementation of AMS programs. Adequate remuneration was key to maintaining the leaders’ motivation and commitment to the programme.
3.2.2. Facilitators Targeting Interpersonal Level Factors
Agarwal et al. (2022) leveraged the HSM platform to foster connections among healthcare providers, enhancing collaborative learning. Zacchaeus et al. (2023) implemented systems for prospective review and feedback to encourage continuous engagement and improvement, while Nakamachi et al. (2015) showcased the power of mentorship and the engagement of respected clinicians as leaders to expand the program’s outreach contributing to success.
3.2.3. Facilitators Targeting Organisational Level Factors
The studies by Agarwal et al. (2022), Zacchaeus et al. (2023), and Nakamachi et al. (2015) each employed distinct organisational level strategies to enhance AMS within healthcare settings. Agarwal et al. (2022) focused on building organisational communities of practice, which facilitated the sharing of experiences and best practices among healthcare providers, thereby strengthening organisational capacity. This approach enabled providers to learn from one another and fostered a collaborative environment that supported continuous improvement in managing TB-HIV co-infections. In contrast, Zacchaeus et al. (2023) developed effective communication and infrastructure to utilise the hub’s centralised resources and expertise and allowed for efficient dissemination of knowledge and best practices, ensuring that even hospitals with limited resources could benefit from centralised expertise. Nakamachi et al. (2015) leveraged evidence-based organisational change management practices such as strong dedicated senior leadership, clear accountability, and reliable data to facilitate the expansion of their program from academic centres to community hospitals.
3.2.4. Facilitators Targeting System Level Factors
Zacchaeus et al. (2023) focused on developing antibiograms and hospital-specific antibiotic policies, which tailored antimicrobial use to the unique antimicrobial resistance patterns of each facility. This customization improved system-wide management by ensuring that antibiotic prescribing was both effective and targeted. Meanwhile, in the study by Nakamachi et al. (2015) collaboration with a major stakeholder-the Ontario’s Critical Care Information centre was a huge facilitator. This allowed them to employ a data-driven decision-making approach, integrating standardised data fields into the provincial critical care information system. This initiative allowed for consistent monitoring and evaluation of antimicrobial use, setting a robust framework for system-wide stewardship. By leveraging reliable data, the stakeholders could make informed decisions and track progress across multiple hospitals, ultimately enhancing the overall effectiveness of AMS efforts. The project’s scale and expansion were further strengthened by a dedicated grant, which overcame financial constraints and enabled the payment of salaries for site champions.
3.3. Intervention Implementation Barriers
3.3.1. Barriers Targeting Individual Level Factors
In the study by Nakamachi et al. (2015), several leadership challenges were identified. The absence of a physician leader posed significant obstacles, emphasising the importance of having a multidisciplinary leadership team to ensure the success of AMS programs. Similarly, Zacchaeus et al. (2023) identified significant training and knowledge gaps among healthcare providers regarding appropriate antimicrobial use. Their study also reported resistance to change from healthcare providers which hindered the adoption of new stewardship practices and the modification of existing prescribing habits. This was also reported in the study by Agarwal et al., (2022) where healthcare providers demonstrated resistance to adopting new learning methods especially those who were accustomed to traditional training approaches. This resistance posed a barrier to the implementation of e-learning interventions designed to enhance AMS.
3.3.2. Barriers Targeting Interpersonal Factors
Nakamachi et al. (2015) study, reported that assigning a pharmacist as the main, solitary leader had posed significant challenges, e.g., due to the heavy reliance on a single individual which then had to be supported by having co-leaders amongst a cohort of respected clinicians.
3.3.3. Barriers Targeting Organisational Level Factors
At the organisational level, the studies by Nakamachi et al. (2015), Zacchaeus et al. (2023), and Agarwal et al. (2022) each highlight significant barriers impacting the implementation and sustainability of AMS programs. Nakamachi et al. (2015) pointed out the lack of institutional investment in data systems and personnel with the expertise to manage these systems as a major challenge. Many hospital systems were not designed to easily capture and retrieve accurate data, which is essential for monitoring and evaluating AMS programs. This would require additional investment in IT infrastructure and skilled personnel to ensure timely and reliable data retrieval. In addition, a lack of organisational structure to outline clear accountability was deemed as challenging post-implementation.
In the study by Zacchaeus et al. (2023), resource limitations in secondary-care hospitals posed significant barriers to the implementation of AMS programs. These hospitals often lacked the necessary infrastructure and resources, such as diagnostic tools and trained personnel, to effectively develop, implement and sustain AMS programs. Limited diagnostic capabilities made it challenging to accurately identify infections and tailor antimicrobial therapy accordingly. This scarcity of resources impeded the ability to enforce hospital-specific antibiotic policies, highlighting the need for targeted resource allocation and capacity-building efforts to overcome these challenges and ensure successful AMS programs implementation in resource-constrained settings. In the study by Agarwal et al. (2022), the author(s) noted that limited resources, including time and personnel, were significant challenges to fully implementing and sustaining e-learning interventions within organisations.
3.3.4. Barriers Targeting System Level Factors
At the system level, all studies revealed significant barriers impacting the implementation of intervention across spokes. Nakamachi et al. (2015) identified data challenges as a major obstacle, noting that many hospital systems were not designed to easily capture and retrieve accurate data, necessitating substantial IT support and institutional investment for timely data retrieval. This limitation underscores the foundational role of clinical information systems in system-wide stewardship efforts. Zacchaeus et al. (2023) highlighted diagnostic limitations within hospitals, which made it difficult to accurately identify infections and tailor antimicrobial therapy, significantly impacting system-wide management. Resource limitations in secondary-care hospitals further exacerbated these challenges, as these facilities often lacked the necessary infrastructure and resources to support comprehensive AMS programs. Agarwal et al. (2022) faced technological challenges, such as limited access to digital devices and reliable internet connectivity, which were barriers to implementing e-learning initiatives designed to support AMS programs, particularly in low-resource settings. These studies collectively illustrate the interconnected nature of data, diagnostic capabilities, personnel/capacity and technological infrastructure in supporting system-level AMS programs implementation.
4. Discussion
The application of the HSM in the AMS context presents a promising approach to managing AMR across various healthcare settings. To the best of our knowledge this is the first review to systematically assess the effectiveness and implementation evaluation of the HSM in the AMS context.
The scoping review highlights the potential of the HSM in improving health system capacities and patient outcomes. The findings from the studies included in this review also provide critical insights into both the facilitators and challenges associated with the implementation of the HSM in AMS programs.
4.1. Comparative Effectiveness of HSM in AMS Programs
The effectiveness of the HSM in AMS programs is highlighted through several key outcomes from the included studies. These outcomes provide evidence that the HSM can significantly contribute to optimising antimicrobial use, improving clinical outcomes, and enhancing the knowledge and skills of healthcare professionals. All three studies Zacchaeus et al. (2023), Agarwal et al. (2022) and Nakamachi et al. (2015) demonstrated that HSM significantly reduced antimicrobial usage and improved antibiotic management, with notable decreases in days on antimicrobial therapy and increases in antibiotic de-escalation rates, together with improved rates of TB screening, diagnosis, and treatment. They also showcase successful scalability of AMS capacity from academic centres to community hospitals. This is critical since a larger proportion (approximately 80%) of antimicrobial use for human health is used within the community settings [
26]. These findings align with broader research, which shows that the HSM is effective in improving access to specialised care, optimising medication use, and promoting best practices consistently across diverse healthcare settings. The model’s centralised expertise, structured training, and scalability make it a valuable tool for enhancing AMS efforts [
27,
28].
4.2. Comparative Effectiveness of HSM in Various Healthcare Contexts
Similar to our findings, the HSM has proven to be an effective organisational model across diverse healthcare settings for the management of other conditions. The effectiveness of the HSM in enhancing access to specialised care and improving patient outcomes has been documented in various settings, such as the Willis-Knighton Health System, where it facilitated advanced oncology treatments and neuro-rehabilitation services by centralising resources and expertise at the hub [
29]. Moreover, the HSM has been applied in diverse diseases and conditions beyond oncology and neuro-rehabilitation. Studies have highlighted its successful implementation in areas such as dental services, and gastrointestinal tumour boards, demonstrating its versatility and effectiveness in providing sustainable specialty care to remote regions [
30,
31]. In the Veterans Affairs (VA) TelePain program, the HSM facilitated specialised pain management services across multiple sites, improving access and standardising care for chronic pain patients. This model effectively addressed the challenges of providing specialised care in remote areas by leveraging telehealth technologies [
31].
4.3. Barriers to HSM Implementation
The implementation of the HSM in AMS programs encountered various barriers across individual, interpersonal, organisational, and system levels. Understanding these challenges is essential for developing strategies to mitigate them and enhance the effectiveness of HSM in combating AMR. At the individual level, leadership challenges and resistance to change among healthcare providers are significant obstacles. Resistance to change is often driven by a lack of awareness or understanding of stewardship principles, which underscores the importance of targeted education and leadership to overcome these obstacles. Similarly, a review by Pulcini et al. (2017) [
32] highlights the challenge of leadership in AMS programs, noting that the absence of strong leadership often results in poor adherence to stewardship guidelines and inconsistent implementation across different healthcare settings.
Interpersonal barriers often stem from the dynamics within healthcare teams. One notable challenge is the reliance on a single leader, such as a pharmacist, to drive the program. This approach can create significant difficulties, particularly if the leader lacks the necessary support from other clinicians or fails to engage them effectively. This finding is corroborated by the work of Dellit et al. (2007) [
33] who argue that successful AMS programs require a multidisciplinary approach, with shared leadership among physicians, pharmacists, and nurses to ensure comprehensive and sustained antimicrobial stewardship efforts.
Organisational barriers are perhaps the most pronounced in the implementation of HSM in AMS programs. A major challenge identified is the lack of institutional investment in robust data systems and personnel to monitor antimicrobial use and resistance patterns accurately. Baur et al. (2017) [
34] discusses the importance of adequate IT infrastructure for real-time data collection and analysis, which is essential for monitoring antimicrobial use and resistance patterns. Additionally, the challenge of resource limitations, as noted in the review, aligns with findings from a study by Hulscher et al. (2010) [
35], which emphasises that insufficient resources, including lack of trained personnel and diagnostic tools, are major obstacles to the success of AMS programmes, particularly in LMICs. Furthermore, the lack of clear organisational structures and accountability can impede the post-implementation success of these initiatives [
36]. Without well-defined roles and responsibilities, it becomes challenging to maintain the momentum of the program and ensure its long-term sustainability.
System-level barriers are equally impactful, particularly in terms of data management and technological infrastructure that can capture and retrieve accurate information on antimicrobial use across different healthcare settings. A study by Cox et al. (2018) [
37] highlights the foundational role of robust data systems in supporting antimicrobial stewardship, noting that many healthcare facilities, especially in low-resource settings, lack the necessary technology to capture and analyze data effectively. Furthermore, technological challenges such as limited access to digital devices and unreliable internet connectivity, as discussed in this study, are also identified as critical barriers in a study by Dyar et al. (2017) [
38]. These challenges not only impede the adoption of e-learning interventions designed to enhance AMS programs but also limit the overall reach and impact of the program.
4.4. Facilitators of Successful Implementation
The successful implementation of the HSM in AMS programs can be influenced by several facilitators that operate across different levels of the healthcare system. These facilitators enhance the effectiveness of the HSM by addressing the specific needs of healthcare providers, fostering collaboration, and leveraging organisational and system-level resources.
Findings show that the enhancement of healthcare providers’ knowledge and skills was a critical facilitator to improving buy-in with AMS initiatives resulting in improved outcomes. This is in congruence with findings from another study, which emphasises the importance of ongoing education and training in improving antimicrobial prescribing practices [
39]. Additionally, strong leadership skills and the accountability of dedicated leaders played a crucial role in driving the success of AMS programs by maintaining motivation and commitment among healthcare providers.
Interpersonal facilitators revolve around fostering collaboration and mentorship within healthcare teams. The HSM platform effectively facilitated connections among healthcare providers, enhancing collaborative learning and knowledge sharing. This collaborative environment can be essential for sustaining AMS initiatives and ensuring continuous improvement. Collaborative learning and mentorship have been repeatedly identified as effective strategies for enhancing healthcare outcomes [
40]. Mentorship by experienced clinicians significantly contributes to the successful adoption and implementation of stewardship practices, particularly in settings where expertise is limited [
41].
At the organisational level, strategies such as building communities of practice and developing effective communication channels are identified as key to strengthening organisational capacity and ensuring that even resource-limited hospitals can benefit from centralised expertise. The importance of organisational support in the success of AMS programmes is echoed in several studies [
34,
42,
43] . For instance, the study by Baur et al. (2017) [
34] emphasises the need for strong institutional commitment, including the establishment of AMS committees and the provision of resources such as data systems and personnel. The concept of building communities of practice, as discussed in the current review, aligns with Wenger’s (1998) [
44] theory of communities of practice, which states that these groups are essential for knowledge sharing and professional development within organisations. By fostering these communities, organisations can enhance the dissemination of best practices and support continuous learning among healthcare providers.
System-level facilitators focus on the importance of developing tailored antimicrobial guidelines and integrating data-driven decision-making into healthcare systems. The development of tailored antimicrobial guidelines is supported by research from Howard et al. (2015) [
45], which demonstrates that guidelines tailored to local microbial resistance patterns significantly improve the appropriateness of antimicrobial therapy. Moreover, the importance of securing dedicated financial resources for sustaining AMS programmes is reinforced by a study from Dyar et al. (2017) [
38], which found that financial constraints are a major barrier to the implementation and expansion of AMS, particularly in low-resource settings.
Strengths and Limitations
This review applied a systematic search strategy which allowed the retrieval of relevant articles. To the best of our knowledge, this scoping review is the first available review on the application of hub and spoke model in AMS programmes. With the limited number of papers available on the application of HSM to manage AMR, its impact and feasibility could not be explored in greater detail. It should also be noted that two articles with the absence of minor details such as the number of hubs and spokes were included in the review due to the depth of information available. It is to be noted that none of the studies did a formal implementation evaluation of these interventions, and the findings have been synthesised based on informal data within the studies.
5. Conclusions
The review highlights the HSM’s effectiveness in managing AMR through AMS initiatives and programs. By facilitating resource sharing between larger “hub” facilities and smaller “spoke” facilities, the HSM enhances capacity building, particularly in resource-limited settings, and enables the delivery of multi-faceted AMS initiatives across diverse healthcare environments. However, there is a notable gap in the literature regarding the application of the HSM in AMS programs. To address this, future research should focus on evaluating the model’s effectiveness in improving antimicrobial prescribing practices, assessing its feasibility in various healthcare contexts, and analysing its cost-effectiveness compared to traditional AMS approaches. Additionally, studies should explore the HSM’s adaptability to different geographic and socioeconomic settings and examine the long-term sustainability of HSM-based AMS programs. By conducting more peer-reviewed studies, the healthcare community can provide evidence-based guidance for policymakers and administrators, identify best practices for implementation, and ultimately leverage the HSM to combat AMR and enhance antimicrobial stewardship efforts globally.
Implications for Future Research and Practice
Despite the growing interest in the HSM across various healthcare settings, there remains a significant gap in the literature concerning robust evaluations of its impact, particularly in AMS. It is well documented / there are best practice recommendations which suggest what elements should be in place for a “good” AMS programme. However, this study addresses a critical gap in understanding how the HSM can be a useful model and provides a resource sharing and improved capability for resource limited settings. This model has the potential to reduce government health spending while ensuring effective service provision, making it a promising avenue for developing more budget-friendly healthcare policies and initiatives. Moreover, while studies have explored the benefits of the HSM in various healthcare contexts, including telehealth and medication treatment for opioid use disorders, there is a notable absence of research that specifically investigates the integration of the HSM in AMS initiatives. Understanding how the HSM can be tailored and optimised to support AMS efforts, improve antibiotic prescribing practices, and enhance infection control measures is essential for advancing antimicrobial stewardship strategies and combating antimicrobial resistance effectively. Therefore, the research gap in the literature pertains to the limited exploration of the application, challenges, and outcomes of implementing the HSM within AMS programs. Future studies should focus on evaluating the effectiveness, feasibility, and impact of integrating the HSM into AMS initiatives to strengthen AMS practices and mitigate the growing threat of antimicrobial resistance.
The findings from this scoping review highlight both the potential benefits and the significant challenges associated with HSM implementation. These insights offer several important implications for future research and practice that can guide the development and refinement of HSM in the context of AMS. The implications for future research and practice emphasise the need for comprehensive, context-specific studies to evaluate the HSM in diverse healthcare settings, particularly in LMICs. Research should focus on developing tailored interventions such as increasing the delivery of structured education and training initiatives, strengthening leadership and interprofessional collaboration, and improving data systems and technological infrastructure. Additionally, securing sustainable funding and addressing behavioural and cultural barriers are crucial for the successful implementation of AMS programs. By focusing on these areas, healthcare institutions can optimise the effectiveness of AMS programs and contribute to the global effort to combat AMR.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org.
Author Contributions
Conceptualization: AI, GG, HR; Methodology: AI, YK; Software: AI, YK, GG, HR; Validation: MN, CB, HR; Formal Analysis: AI, YK, GG; Investigation: All authors; Resources: AI, YK, GG, HR; Data Curation: AI, YK; Writing – Original Draft Preparation: AI, YK, GG; Writing – Review & Editing: AI, GG, HR, VR, CB, FG; Visualization: AI, YK; Supervision: HR, VR, FG; Project Administration: MN; Funding Acquisition: VR, FG, MN.
Funding Information
This research was funded by Funding the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) managed by the Tropical Health and Education Trust (THET) and Commonwealth Pharmacists Association (CPA). CwPAMS is a global health partnership programme funded by the Fleming Fund using UK aid funding. The Fleming Fund is a UK aid programme supporting up to 25 countries across Sub-Saharan Africa and Asia to tackle antimicrobial resistance. The Fund is managed by the UK Department of Health and Social Care and invests in strengthening surveillance systems through a portfolio of country and regional grants, global projects and fellowship schemes. The views expressed in this publication are those of the authors and not necessarily those of the UK Department of Health and Social Care, the National Health System (NHS) and represented NHS Trusts.
Conflicts of Interest
The authors declare no conflict of interest.
Ethics Statements
Formal ethics approval was not required since this study was classified as a scoping review.
References
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. The lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Otaigbe, I.I.; Elikwu, C.J. Drivers of Inappropriate Antibiotic Use in Low-and Middle-Income Countries. JAC-Antimicrobial Resistance 2023, 5, dlad062. [Google Scholar] [CrossRef]
- Porter, S.B.; Glasgow, A.E.; Yao, X.; Habermann, E.B. Association of Florida House Bill 21 With Postoperative Opioid Prescribing for Acute Pain at a Single Institution. JAMA Surg 2020, 155, 263–264. [Google Scholar] [CrossRef]
- Sulis, G.; Sayood, S.; Gandra, S. Antimicrobial Resistance in Low-and Middle-Income Countries: Current Status and Future Directions. Expert review of anti-infective therapy 2022, 20, 147–160. [Google Scholar] [CrossRef] [PubMed]
- Bell, B.G.; Schellevis, F.; Stobberingh, E.; Goossens, H.; Pringle, M. A Systematic Review and Meta-Analysis of the Effects of Antibiotic Consumption on Antibiotic Resistance. BMC infectious diseases 2014, 14, 1–25. [Google Scholar] [CrossRef]
- Villanueva, P.; Coffin, S.E.; Mekasha, A.; McMullan, B.; Cotton, M.F.; Bryant, P.A. Comparison of Antimicrobial Stewardship and Infection Prevention and Control Activities and Resources between Low-/Middle-and High-Income Countries. The Pediatric Infectious Disease Journal 2022, 41, S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Ab, U. Impact of Antimicrobial Resistance in Health and Economic Outcomes: A Review. Advances in Pharmacology and Clinical Trials 2024. [CrossRef]
- Friedman, N.D.; Temkin, E.; Carmeli, Y. The Negative Impact of Antibiotic Resistance. Clinical microbiology and infection 2016, 22, 416–422. [Google Scholar] [CrossRef]
- Morris, A.M. Antimicrobial Stewardship Programs: Appropriate Measures and Metrics to Study Their Impact. Current treatment options in infectious diseases 2014, 6, 101–112. [Google Scholar] [CrossRef]
- Kamere, N.; Garwe, S.T.; Akinwotu, O.O.; Tuck, C.; Krockow, E.M.; Yadav, S.; Olawale, A.G.; Diyaolu, A.H.; Munkombwe, D.; Muringu, E. Scoping Review of National Antimicrobial Stewardship Activities in Eight African Countries and Adaptable Recommendations. Antibiotics 2022, 11, 1149. [Google Scholar] [CrossRef]
- Rolfe, R.; Kwobah, C.; Muro, F.; Ruwanpathirana, A.; Lyamuya, F.; Bodinayake, C.; Nagahawatte, A.; Piyasiri, B.; Sheng, T.; Bollinger, J. Barriers to Implementing Antimicrobial Stewardship Programs in Three Low-and Middle-Income Country Tertiary Care Settings: Findings from a Multi-Site Qualitative Study. Antimicrobial Resistance & Infection Control 2021, 10, 1–11. [Google Scholar]
- Collignon, P.; Beggs, J.J.; Walsh, T.R.; Gandra, S.; Laxminarayan, R. Anthropological and Socioeconomic Factors Contributing to Global Antimicrobial Resistance: A Univariate and Multivariable Analysis. The Lancet Planetary Health 2018, 2, e398–e405. [Google Scholar] [CrossRef] [PubMed]
- Foxlee, N.D.; Townell, N.; Heney, C.; McIver, L.; Lau, C.L. Strategies Used for Implementing and Promoting Adherence to Antibiotic Guidelines in Low-and Lower-Middle-Income Countries: A Systematic Review. Tropical Medicine and Infectious Disease 2021, 6, 166. [Google Scholar] [CrossRef]
- Barbara, A.M.; MacDougall, D. Hub-and-Spoke Models of Care for Chronic Pain. Canadian Journal of Health Technologies 2022, 2. [Google Scholar] [CrossRef]
- Parikh, D.A.; Rodgers, T.D.; Passero, V.A.; Chang, J.C.; Tisdale, R.; Kelley, M.J.; Das, M. Teleoncology in the Veterans Health Administration: Models of Care and the Veteran Experience. American Society of Clinical Oncology Educational Book 2024, 44, e100042. [Google Scholar] [CrossRef]
- De Cola, M.C.; Ielo, A.; Lo Buono, V.; Quartarone, A.; Calabrò, R.S. Toward Social-Health Integration in Sicily: Description of the First Hub and Spoke Model to Improve the Diagnostic Therapeutic Care Paths for Neurorehabilitation. Frontiers in Public Health 2023, 11, 1141581. [Google Scholar] [CrossRef] [PubMed]
- Effah, K.; Attivor, E.K.; Atuguba, B.H.; Adaletey, D.D.; Ofori, D.A.; Diame, P.; Tekpor, E.; Wormenor, C.M.; Gedzah, I.; Agyiri, D. Application of the Hub and Spokes Model in Improving Access to Cervical Cancer Screening in Ghana. Ghana Medical Journal 2022, 56, 134–140. [Google Scholar] [CrossRef]
- Srivastava, S.; Datta, V.; Garde, R.; Singh, M.; Sooden, A.; Pemde, H.; Jain, M.; Shivkumar, P.; Bang, A.; Kumari, P.; et al. Development of a Hub and Spoke Model for Quality Improvement in Rural and Urban Healthcare Settings in India: A Pilot Study. BMJ open qual. 2020, 9. [Google Scholar] [CrossRef]
- Osei-Fofie, D. Effective Innovative Models of Health Care Delivery in the Era of the COVID-19 Pandemic to Reduce Disparities in Cancer Care and for Cancer Control in Low-Middle Income Countries—South African Experience of the Cancer ECHO Model. 2022.
- Dhanasekaran, K.; Hariprasad, R.; Singh, M.; Jain, S.; Nethan, S.T.; Singh, S. Impact of the COVID-19 Pandemic on an Online Cancer Screening Training Programme for Healthcare Providers in the Public Sector in India: Learnings from a Hub and Spoke Model Perspective. ecancermedicalscience 2023, 17. [Google Scholar] [CrossRef]
- Jain, S.; Arora, S.; Chauhan, A.; Agarwal, A.; Saikia, B.; Singh, M. Super-Specialty Medical Teleconsultations to Remote Areas of Ladakh, India via E-Sanjeevani under Hub-and-Spoke Model: A Pilot Study. Telehealth and Medicine Today 2024. [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of internal medicine 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Zacchaeus, N.G.P.; Palanikumar, P.; Alexander, H.; Webster, J.; Nair, I.K.; Sadanshiv, M.; Thomas, R.M.; Deodhar, D.; Samuel, P.; Rupali, P. Establishing an Effective Antimicrobial Stewardship Program at Four Secondary-Care Hospitals in India Using a Hub-and-Spoke Model. Antimicrob Steward Healthc Epidemiol 2023, 3, e99. [Google Scholar] [CrossRef] [PubMed]
- Nakamachi, Y.; West, S.; Dresser, L.; Morris, A. Antimicrobial Stewardship: Developing and Expanding Hospital Antimicrobial Stewardship: The Ontario Experience. Canada Communicable Disease Report 2015, 41, 14. [Google Scholar] [PubMed]
- Agarwal, R.; Agarwal, U.; Das, C.; Reddy, R.A.; Pant, R.; Ho, C.; Kumar, B.R.; Dabla, V.; Moonan, P.K.; Nyendak, M.; et al. Building Communities of Practice through Case-Based e-Learning to Prevent and Manage TB among People Living with HIV-India. BMC Infect Dis 2022, 22, 967. [Google Scholar] [CrossRef]
- Gelband, H.; Miller, P., Molly; Pant, S.; Gandra, S.; Levinson, J.; Barter, D.; White, A.; Laxminarayan, R. The State of the World’s Antibiotics 2015. Wound healing southern africa 2015, 8, 30–34. [Google Scholar]
- Davey, P.; Brown, E.; Charani, E.; Fenelon, L.; Gould, I.M.; Holmes, A.; Ramsay, C.R.; Wiffen, P.J.; Wilcox, M. Interventions to Improve Antibiotic Prescribing Practices for Hospital Inpatients. Cochrane database of systematic reviews 2013.
- Schuts, E.C.; Hulscher, M.E.; Mouton, J.W.; Verduin, C.M.; Stuart, J.W.C.; Overdiek, H.W.; van der Linden, P.D.; Natsch, S.; Hertogh, C.M.; Wolfs, T.F. Current Evidence on Hospital Antimicrobial Stewardship Objectives: A Systematic Review and Meta-Analysis. The Lancet infectious diseases 2016, 16, 847–856. [Google Scholar]
- Elrod, J.K.; Fortenberry, J.L. The Hub-and-Spoke Organization Design: An Avenue for Serving Patients Well. BMC health services research 2017, 17, 25–33. [Google Scholar]
- Dyson, K.; Kruger, E.; Tennant, M. Networked Remote Area Dental Services: A Viable, Sustainable Approach to Oral Health Care in Challenging Environments. Australian Journal of Rural Health 2012, 20, 334–338. [Google Scholar] [CrossRef]
- Subramaniam, S.; Chen, J.; Wilkerson, T.-L.; Stevenson, L.; Kincaid, C.; Firestone, C.; Ball, S.L. Refining the Implementation of a Hub-and-Spoke Model for Telepain through Qualitative Inquiry. Journal of Technology in Behavioral Science 2023, 8, 295–305. [Google Scholar] [CrossRef]
- Pulcini, C.; Morel, C.; Tacconelli, E.; Beovic, B.; Goossens, H.; Harbarth, S.; Holmes, A.; Howard, P.; Morris, A.; Nathwani, D. Human Resources Estimates and Funding for Antibiotic Stewardship Teams Are Urgently Needed. Clinical Microbiology and Infection 2017, 23, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Dellit, T.H.; Owens, R.C.; McGowan, J.E.; Gerding, D.N.; Weinstein, R.A.; Burke, J.P.; Huskins, W.C.; Paterson, D.L.; Fishman, N.O.; Carpenter, C.F. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clinical infectious diseases 2007, 44, 159–177. [Google Scholar] [CrossRef] [PubMed]
- Baur, D.; Gladstone, B.P.; Burkert, F.; Carrara, E.; Foschi, F.; Döbele, S.; Tacconelli, E. Effect of Antibiotic Stewardship on the Incidence of Infection and Colonisation with Antibiotic-Resistant Bacteria and Clostridium Difficile Infection: A Systematic Review and Meta-Analysis. The Lancet Infectious Diseases 2017, 17, 990–1001. [Google Scholar] [CrossRef] [PubMed]
- Hulscher, M.E.; Grol, R.P.; Van Der Meer, J.W. Antibiotic Prescribing in Hospitals: A Social and Behavioural Scientific Approach. The Lancet infectious diseases 2010, 10, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Houston, S.M.; Bove, L.A.; Houston, S.M.; Bove, L.A. Applying the Project Management Process in Healthcare Informatics. Project Management for Healthcare Informatics 2007, 69–77. [Google Scholar]
- Cox, N.; Tak, C.R.; Cochella, S.E.; Leishman, E.; Gunning, K. Impact of Pharmacist Previsit Input to Providers on Chronic Opioid Prescribing Safety. J Am Board Fam Med 2018, 31, 105–112. [Google Scholar] [CrossRef]
- Dyar, O.; Huttner, B.; Schouten, J.; Pulcini, C. What Is Antimicrobial Stewardship? Clinical microbiology and infection 2017, 23, 793–798. [Google Scholar] [CrossRef]
- Giamarellou, H.; Galani, L.; Karavasilis, T.; Ioannidis, K.; Karaiskos, I. Antimicrobial Stewardship in the Hospital Setting: A Narrative Review. Antibiotics 2023, 12, 1557. [Google Scholar] [CrossRef]
- Wallen, G.R.; Mitchell, S.A.; Melnyk, B.; Fineout-Overholt, E.; Miller-Davis, C.; Yates, J.; Hastings, C. Implementing Evidence-based Practice: Effectiveness of a Structured Multifaceted Mentorship Programme. Journal of advanced nursing 2010, 66, 2761–2771. [Google Scholar] [CrossRef]
- McAlearney, A.S. Leadership Development in Healthcare: A Qualitative Study. Journal of Organizational Behavior: The International Journal of Industrial, Occupational and Organizational Psychology and Behavior 2006, 27, 967–982. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Nabiryo, M.; Zengeni, L.; Kamere, N.; Makotose, A.; Olaoye, O.; Townsend, W.; Waddingham, B.; Matuluko, A.; Nambatya, W. Tackling Antimicrobial Resistance: Developing and Implementing Antimicrobial Stewardship Interventions in Four African Commonwealth Countries through a Health Partnership Model. Journal of Public Health in Africa 2023, 14. [Google Scholar] [CrossRef] [PubMed]
- Pakyz, A.L.; Moczygemba, L.R.; VanderWielen, L.M.; Edmond, M.B.; Stevens, M.P.; Kuzel, A.J. Facilitators and Barriers to Implementing Antimicrobial Stewardship Strategies: Results from a Qualitative Study. American journal of infection control 2014, 42, S257–S263. [Google Scholar] [CrossRef] [PubMed]
- Wenger, E. Communities of Practice: Learning, Meaning, and Identity; Cambridge university press, 1999; ISBN 0-521-66363-6.
- Howard, P.; Pulcini, C.; Levy Hara, G.; West, R.; Gould, I.; Harbarth, S.; Nathwani, D. An International Cross-Sectional Survey of Antimicrobial Stewardship Programmes in Hospitals. Journal of Antimicrobial Chemotherapy 2015, 70, 1245–1255. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).