1. Background
Cardiac and pulmonary diseases are among the top five most prevalent and burdensome health conditions globally, accounting for more than 20% of the world’s disability and more than 3.5 million global fatalities annually [
1]. Deaths from these diseases have recently declined in high income countries due to more effective primary treatment options [
2,
3]. Improved survival rates mean, however, that more people than ever are living longer while managing these chronic diseases. People living with cardiac and pulmonary diseases have an increased likelihood of poor physical health, mental health, and low quality of life [
4,
5]. Effective management strategies are needed to ensure that people with cardiac and pulmonary disease live long, healthy, and happy lives.
Physical activity is essential for quality and longevity of life [
6], particularly for people with cardiac or pulmonary diseases [
7,
8]. For example, regular physical activity reduces the risk of all-cause mortality by 12–14% for those with heart disease and 30% for those with chronic lung disease [
9,
10]. Physical activity can also offset the negative impacts of cardiac and pulmonary disease on quality of life [
11,
12]. Effective long-term management of cardiac and pulmonary diseases requires engagement in regular physical activity.
Following cardiac or pulmonary health events, patients are often referred to exercise rehabilitation programs. Exercise rehabilitation programs are typically short-term (6-12 weeks), comprised of weekly in-clinic exercise sessions designed to improve mobility, functional capacity, and fitness [
13,
14]. A wealth of evidence demonstrates positive health outcomes of exercise rehabilitation in cardiac and pulmonary patients, including improved physical and mental health, quality of life, and fitness [
15,
16,
17,
18]. Unsurprisingly, patients’ physical activity levels increase when enrolled in these programs [
14,
19]. Some evidence suggests that people compensate for the exercise engaged in during rehabilitation with less lifestyle physical activity [
20,
21], although the findings are mixed [
22,
23]. If cardiac and pulmonary rehabilitation patients are replacing their lifestyle physical activity with rehabilitation exercise, it may put their activity levels at risk once rehabilitation programs cease.
Understanding motivation for long-term engagement in regular physical activity is essential for increasing the longevity of the benefits of cardiac and pulmonary exercise rehabilitation. Self-determination, intention, and habit have been theorised as key predictors of physical activity, especially for the long-term maintenance of changes in physical activity behaviour [
24]. Self-determination theory proposes that people are innately driven to behave in ways that lead to autonomous, or self-determined, motivation which enhances individuals’ overall growth and wellbeing [
25,
26]. The quality of motivation is proposed to vary across a continuum of self-determination, from purely self-determined or
intrinsic regulation (i.e., internal drives based on core values and interests) to non-self-determined, wholly
extrinsic regulation (i.e., drives to behave based on external pressures). Evidence has consistently shown that people with more self-determined physical activity motivation tend to be more strongly motivated overall [
27], are more likely to act on their motivation [
28], and are more likely to maintain physical activity over the long-term [
29,
30]. Previous research amongst cardiac rehabilitation patients supports the importance of self-determined motivation for long-term maintenance of physical activity [
31,
32].
Retaining positive physical activity intentions is also important for motivation of regular engagement in physical activity over the long-term. Intentions are proposed to represent the summation of all conscious, deliberative influences on behaviour – such as outcome expectancies, social norm beliefs, and perceptions of behavioural control [
33,
34] – and are positioned as the most proximal determinant of behaviour [
35]. Intentions have been shown to be an important predictor of exercise and physical activity in cardiac exercise rehabilitation patients [
36,
37].
Habit is a core mechanism for long-term engagement in physical activity [
38]. Habit can be defined as a non-conscious process through which an association between a cue (e.g., waking up) and a behavioural response (e.g., going for a walk), learned through repetition, automatically triggers impulses to act when the cue is encountered [
39]. Habit is thought to sustain action even when people have little conscious motivation to act [
40,
41]. Evidence on the value of habit for improving physical activity in cardiac and pulmonary rehabilitation patients is promising [
42,
43].
Perhaps owing to the dichotomization of long-term behaviour change into discrete ‘initiation’ and ‘maintenance’ stages [
38], behaviour maintenance is tacitly conceived of as a single, stable action phase. This overlooks the potential that physical activity motivation may change over time throughout either or both the initiation and maintenance stages. For example, the extent to which a behaviour is self-motivated can change over time: through praise and mastery experiences, initially, extrinsically motivated behaviours may become internalized [
29], and conversely, providing extrinsic rewards for an intrinsically motivated behaviour can foster external motivation [
44]. Similarly, intention strength will likely change as new barriers and facilitators of physical activity emerge [
45], and the strength of newly formed positive habits can dip over the long-term [
46,
47]. Decreases in the strength of self-determined motivation, intention or habit is likely to precede a decline in physical activity [
24]. Understanding how motivation for physical activity changes over time both during and after exercise rehabilitation may aid the development of interventions to support long-term physical activity maintenance among cardiac and pulmonary rehabilitation patients.
2. The Present Study
Exercise rehabilitation programs are crucial aides for providing guided advice and support for safe and healthy engagement in exercise. However, little is known about change in cardiac and pulmonary patients’ physical activity behaviour and motivation during and after exercise rehabilitation. This study was undertaken among community-based cardiac and pulmonary disease patients to investigate how rehabilitation exercise, lifestyle physical activity, self-determined motivation and habit and intention changed during and after participating in a rehabilitation exercise program.
3. Methods
3.1. Study Design & Procedure
This repeated measures study was conducted over six months, with six once-monthly survey assessments. Participants were tracked throughout their individual journeys of the community-based rehabilitation programs, so weeks in rehabilitation and time of completion/drop-out was tracked for each individual. As such, the time in the study and time to and since completing rehabilitation differed for each individual.
3.2. Participants & Recruitment
Following a heart or lung disease diagnosis or surgery, patients were medically referred to a local community-based clinical rehabilitation program based in a regional city in Australia (Bundaberg, Queensland), as part of usual care. Regular engagement in this particular rehabilitation program consisted of eight weeks of one-hour clinically-based, supervised exercise sessions conducted twice a week (16 exercise sessions in total). Patients were provided with information regarding the research and invited to participate during clinical consultation. Where patients met the eligibility criteria (≥18 years of age and had been referred to the rehabilitation program) and were interested in participating in the research, a face-to-face appointment was scheduled. At this point, participants' informed consent, preferred survey method (paper or electronic) and baseline self-reported survey data were collected. All participants who provided informed consent opted for a posted hard-copy (paper) survey to their home addresses. Following the initial face-to-face research appointment, participants were posted a paper self-report survey each month for the following four months. In month six, each patient was invited for a second face-to-face appointment and completed their final (sixth) self-report survey. After the second appointment, each participant was given an AU$50 gift card. All procedures were approved by the associated University’s Human Research Ethics Committee (#20840).
3.3. Measures
In each of the six surveys, participants were asked about physical activity engaged in outside of the clinical sessions (i.e., ‘lifestyle physical activity’) and exercise engaged in during rehabilitation sessions (‘rehabilitation exercise’). Measures were scored using the R
psych package [
48].
3.3.1. Lifestyle Physical Activity
Lifestyle physical activity was measured using the International Physical Activity Questionnaire—Short Form [IPAQ-SF; 49]. The IPAQ-SF consists of seven items requiring participants to reflect on the past seven days and report the number of days and average time (hours and minutes) spent performing vigorous, moderate and walking activities (e.g., “During the last 7 days, on how many days did you do vigorous physical activities like heavy lifting, digging, aerobics or fast bicycling?”; “How much time did you usually spend doing vigorous physical activities on one of those days?”). Before each item, participants were reminded not to include rehabilitation exercises. As per validated scoring procedures [
49], scores were calculated for estimated metabolic equivalents (METs) per week and categories of low, moderate or high physical activity levels.
3.3.2. Rehabilitation Exercise
Rehabilitation exercise was scored using a second set of the IPAQ-SF items [
49], worded to reflect the rehabilitation-based exercise and activity sessions (e.g., “During the last 7 days, on how many days did you do vigorous exercise for at least 10 minutes at a time, during rehabilitation sessions?”). Scoring calculations were the same as for lifestyle physical activity.
3.3.3. Self-Determined Motivation
Two versions of the Behavioural Regulation in Exercise Questionnaire [BREQ-2; [
50]] were used, one for lifestyle physical activity and one for rehabilitation exercise. The BREQ-2 uses a 5-point Likert scale (0= “Not true for me” – 4= “Very true for me”) with items such as “I exercise because it’s fun”, and “I feel like a failure when I haven’t exercised”. Scores were calculated as subscales of intrinsic (4 items), identified (4 items), introjected (3 items), and external (4 items) regulation as well as an overall relative autonomy index score. Interitem reliabilities ranged from α = 0.61 to α = 0.93.
3.3.4. Intention Strength
Intentions to engage in lifestyle physical activity and rehabilitation exercise were separately measured using single items (“Over the next month, to what extent do you intend to exercise outside or rehabilitation”, “Over the next month, to what extent do you intend on attending rehabilitation sessions”). Response scales ranged from 1 =
Not at all to 7 =
A lot [
51].
3.3.5. Habit Strength
Habit strength was measured about lifestyle physical activity and exercise rehabilitation separately via the validated 4-item Self-Report Behavioural Automaticity Index [SRBAI; [
52]], which is a subscale of the Self-Report Habit Index [SRHI; [
53]]. Response options varied on 7-point Likert-style scales (1=
Strongly disagree to 7=
Strongly agree) to two sets of four items, which followed the stems “Attending rehabilitation sessions is something I do…” and “Exercise is something I do…”. The items were: “…automatically”, “…without having to consciously remember”, “…without thinking”, and “…I start doing before I realize I’m doing it”. Interitem reliability was α = 0.98 for lifestyle physical activity habit strength and α = 0.90 for exercise rehabilitation habit strength.
3.4. Data Management and Analyses
Statistical analyses were performed in R version 3.6.2 [
54]. Descriptive statistics (
M,
SD, intraclass correlations [ICC]) were calculated for all variables. Linear regression models were conducted to test for overall associations between maintenance determinants and behaviour for exercise rehabilitation and lifestyle physical activity during and following rehabilitation. During assumption testing, it became clear that there was the risk of undue influence from outliers of the self-reported physical activity measure, so the variable was truncated to the 75% interquartile range value for analyses. Following transformation, all model assumptions were met.
To test for differences of physical activity behaviour and motivation between rehabilitation exercise, lifestyle physical activity during rehabilitation, and lifestyle physical activity following rehabilitation, random effects models and estimated marginal means were calculated for pairwise comparisons with Tukey’s
p-value adjustment for multiple corrections and the Kenward-Roger method for degrees of freedom [
55,
56]. To test for change over time during and after exercise rehabilitation, random effects models were estimated with time modelled linearly as month in study, separately for during and post-exercise rehabilitation. Effect sizes were estimated as marginal R-squared estimates [
57], interpretable as pseudo-R
2 (i.e., the proportion of variability explained by the effect). Post-hoc power calculation established that the study was powered to detect medium effects (
d = 0.49, 1 – β = 80%, α = 0.05) at the within-person level, and large effects (
d = 0.68, 1 – β = 80%, α = 0.05) at the between-person level [
58,
59].
4. Results
4.1. Sample Characteristics
Thirty-one participants (cardiac patients
n = 15, pulmonary patients
n = 16) participated in the study. A detailed summary of participant demographic characteristics is presented in
Table 1. Most patients were male (71%), and Caucasian (96.8%), with a
M age of 71.5 years (
SD = 9.4, range = 36 – 84 years).
4.1.1. Change in Physical Activity Behaviour
The ICC for lifestyle physical activity behaviour was 71.9%, representing less change over time compared to between-person differences, in that about two-thirds of variability was accounted for by between-person differences. There was far more within-person variability in exercise rehabilitation physical activity (ICC of 39.1%), with only about one-third of variability accounted for by differences between people.
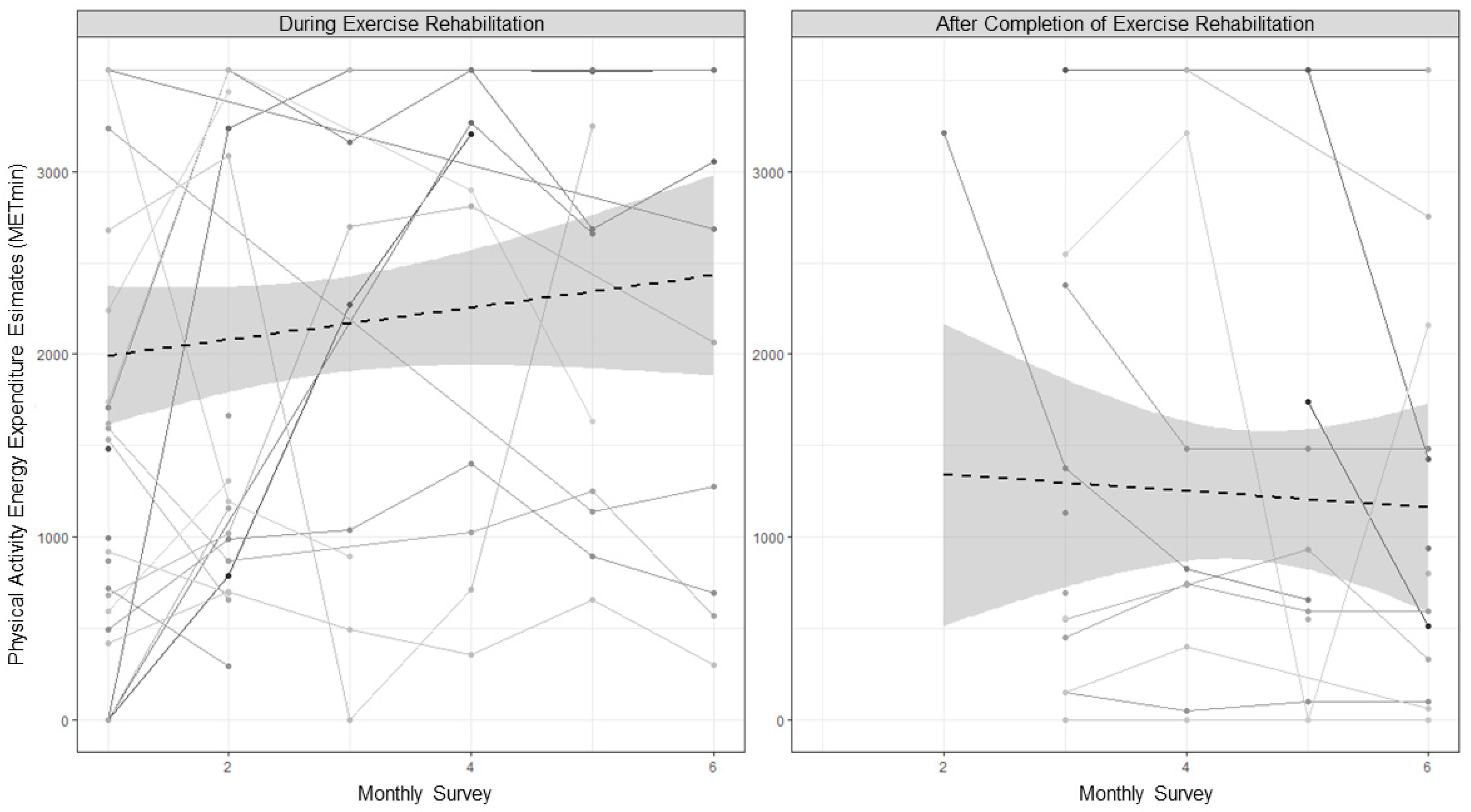
Descriptive statistics and the results of the estimated means difference tests are presented in
Table 2. Overall, physical activity decreased after exercise rehabilitation, but this is largely due to the ceasing of the rehabilitation exercise rather than a decline in lifestyle physical activity. As shown in
Table 3 and
Figure 1, total physical activity behaviour (i.e., the sum of rehabilitation exercise and lifestyle physical activity) did not significantly increase during exercise rehabilitation but declined steadily once exercise rehabilitation was completed, with an estimated 3% of the variability in physical activity accounted for by the decrease across time. Lifestyle physical activity did not significantly change from during to following rehabilitation.
4.1.2. Physical Activity Behaviour and Motivation
Overall associations between physical activity motivation variables and rehabilitation exercise and lifestyle physical activity are shown in
Table 4. Rehabilitation exercise was not significantly associated with any motivation variable. During the months that participants were in exercise rehabilitation, lifestyle physical activity was significantly associated with identified regulation (
Adj. R2 = 11%), intention strength (
Adj. R2 = 23%), and lifestyle activity habit strength (
Adj. R2 = 14%). After exercise rehabilitation was complete, lifestyle physical activity was associated with intrinsic regulation (
Adj. R2 = 17%), identified regulation (
Adj. R2 = 36%), individuals’ relative autonomy index scores (
Adj. R2 = 19%), intention strength (
Adj. R2 = 45%), and lifestyle activity habit strength (
Adj. R2 = 40%).
Note. Outcome is physical activity reported in estimated energy expenditure per week. *p < .05.
4.1.3. Self-Determined Motivation
All forms of regulation for rehabilitation exercise had ICCs between 26.6% and 43.4%, indicating that between-person differences only accounted for about one-third of the variability in regulation. So, most variability was accounted for by within-person change across the study. Comparatively, the ICCs for regulation of lifestyle physical activity were far more stable, with ICCs between 73.2% and 78.1%, indicating that most variability was due to between-person differences rather than changes over the study period.
Descriptive statistics and the results of the estimated means differences for lifestyle physical activity, rehabilitation exercise, and self-determined motivation are presented in
Table 3. Intrinsic and identified regulations were stronger for rehabilitation exercise than for lifestyle physical activity both during and following rehabilitation. There were no differences in introjected or external regulation for exercise rehabilitation and lifestyle physical activity either during or following rehabilitation. There were no significant changes in any form of regulation for lifestyle physical activity from during to following rehabilitation. Overall, relative autonomy indexes were higher for rehabilitation exercise than for lifestyle physical activity both during and following rehabilitation.
When considering change over time both during and following exercise rehabilitation (
Table 4), no specific form of regulation for lifestyle physical activity changed during exercise rehabilitation. However, an increase in the relative autonomy index suggested that people became more self-determined for lifestyle physical activity over time during rehabilitation. This increase over time explained 2% of variability in the relative autonomy index. Following completion of rehabilitation, there were no significant changes in the more self-determined forms of motivation (intrinsic, introjected, and identified); however, external regulation decreased over time, with less than 1% of variability in external regulation explained by change across time.
4.1.4. Intention
Intention strength for rehabilitation exercise had an ICC of 4.2% (95% CI = -14.2% to 28.6%), indicating very low between-person differences in intention strength (with most having quite strong intentions). Comparatively, the stability of intention strength for lifestyle physical activity was much less, with an ICC of 45.3%, indicating that about half of the variability was from between-person differences and half from within-person change. Participants reported stronger intentions for rehabilitation exercise than for lifestyle physical activity during and following rehabilitation. There were no changes in lifestyle physical activity or exercise rehabilitation intention strength from during to following rehabilitation and no changes across time for rehabilitation exercise either during or following rehabilitation (
Table 3 and
Table 4).
4.1.5. Habit Strength
Habit strength for rehabilitation exercise had an ICC of 27.1%, reflecting considerable change across time. However, habit strength for lifestyle physical activity had an ICC of 76.5%, indicating minimal change across the study, with most variability accountable at the between-person level. Participants reported stronger habits for rehabilitation exercise than for lifestyle physical activity during or following rehabilitation. There were no significant changes in lifestyle physical activity habit strength from during to following rehabilitation, though trends indicated that habit strength tended to decrease (
Table 3). There were no changes across time either during or following rehabilitation (
Table 4).
5. Discussion
This repeated measures study tracked physical activity behaviour and motivation during and after a community-based cardiac and pulmonary exercise rehabilitation program. Overall, physical activity levels decreased following rehabilitation as a result of the ceasing of rehabilitation exercise and no added gain in lifestyle physical activity. Uniquely, this study provided insight into the dynamics of motivation for both lifestyle physical activity (engaged in outside rehabilitation sessions) and exercise rehabilitation (done within rehabilitation sessions), revealing that the processes underlying adherence to exercise rehabilitation differs from those for lifestyle physical activity. Unless more is done to enhance motivation for lifestyle physical activity post-rehabilitation, the benefits of exercise rehabilitation will be short-lived.
Patients’ lifestyle physical activity changed very little across the study, demonstrating that engaging in rehabilitation exercise did not replace their other physical activity behaviour. This finding adds to the evidence that not all exercise rehabilitation sessions lead to a compensatory effect of less physical activity outside of rehabilitation [
22,
23]. Given the conflicting evidence on this phenomenon, more is needed to understand what factors influence whether a person does or does not compensate for rehabilitation exercise with less lifestyle physical activity. Some evidence suggests that compensation may be more likely with older populations or when mixed aerobic and resistance training is used, but even these findings are not reliable across all studies [
22]. When patients enrol in exercise rehabilitation programs, care is needed for encouraging rehabilitation exercise and lifestyle physical activity throughout program participation.
Support for lifestyle physical activity becomes even more essential in the transition that follows completion of exercise rehabilitation programs. In our study, when including rehabilitation exercise, patients’ overall physical activity levels increased during program enrolment, echoing evidence showing an increase of physical activity during such programs [
14,
19]. Notably, however, patients did not increase their lifestyle physical activity behaviour once their rehabilitation exercise program ended. The substantial health and wellbeing outcomes gained from participating in exercise rehabilitation [e.g., 15,17] are unlikely to continue beyond the time of the rehabilitation program unless changes are made to enhance motivation for lifestyle physical activity amidst and following the rehabilitation program. These study findings highlight the need for a focus on motivation intervention and boosters within exercise rehabilitation programs, in line with contemporary guidelines which advocate for self-management rather than a reliance on clinical management of chronic diseases (Grady & Gough, 2014).
One of the novel elements of this study was the separate investigation of motivation for rehabilitation exercise vs lifestyle physical activity, and the results show large differences in these motivational processes. Overall, patients’ motivation for lifestyle physical activity and rehabilitation exercise was generally high, with self-determination, intention strength, and habit strength for exercise rehabilitation were rated consistently higher than for lifestyle physical activity. That patients were so strongly motivated for exercise rehabilitation is encouraging, given the evidenced benefits of such programs [
14,
19]. However, this motivation did not necessarily translate into more physical activity.
For lifestyle physical activity, more self-determined motivation, stronger intentions, and stronger habits were associated with greater behavioural engagement. This aligns with theory and evidence that these aspects of motivation are important in influencing physical activity behaviour, e.g., [
60,
61,
62,
63]. However, in contrast to theory and evidence, none of these motivation variables were associated with rehabilitation exercise behaviour. The lack of motivation-behaviour associations found for rehabilitation exercise could be the byproduct of a lack of variability in motivation resulting in a ceiling effect or of measurement artefact. Energy expenditure was self-reported based on estimated time spent in different intensities of activity during sessions, which is likely prone to error. It may be that motivation would be associated with less subjective measures of exercise energy expenditure such as accelerometer monitors or physiological trackers. Future research is needed to test the replicability of our findings for clarity on the motivational processes of rehabilitation exercise.
If our findings of rehabilitation exercise behaviour not being associated with intentions, habit, or self-determined motivation for rehabilitation exercise are found to be reproducible, it has important implications for clinical practice. The aspects of motivation that influence lifestyle physical activity may be distinct from those for exercise behaviour within rehabilitation programs. Most research has considered motivation for adherence to rehabilitation exercise [
64] or motivation for lifestyle physical activity following rehabilitation, e.g., [
65]. More research is needed that tracks motivation for these two different types of activity as people transition into the post-rehabilitation phase.
Our findings add to the limited understanding of what happens to physical activity motivation across the transition of having regular exercise rehabilitation to the program ceasing. We found that there was very little change in people’s motivation for lifestyle physical activity either during or following patients’ involvement in exercise rehabilitation. This finding aligns with other evidence of a lack of change in motivation for physical activity across rehabilitation programs [
66]. It seems that patients maintain their levels of self-determination, intention, and habit strength for physical activity during and beyond the completion of exercise rehabilitation. For those who have strong habits, intentions, and self-determination for lifestyle physical activity, this finding is encouraging in that their motivation is unlikely to decline due to rehabilitation. However, for patients with low motivation, it may be a missed opportunity to improve people’s motivation for lifestyle physical activity [
67].
Most exercise rehabilitation programs focus on in-gym exercise training with less focus on motivation and behaviour change strategies [
68]. If exercise rehabilitation were to include motivational training and support for safely enhancing physical activity levels beyond exercise rehabilitation, the physical and mental health benefits of exercise rehabilitation could have long-lasting benefits for patients at-risk of inactivity following exercise rehabilitation. Simple planning aides have been shown to be effective in enhancing physical activity habit strength and in turning strong intentions into physical activity behaviour [
69,
70]. For example, one study found that an exercise rehabilitation program with planning intervention elements that helped people specify when, where, and how they will engage in physical activity (action plans), as well as how to deal with anticipated barriers (coping plans), led to increases in physical activity 2 months following discharge [
71]. When applied in the incremental distribution with telephone-based boosters, planning aides can enhance motivation for physical activity and physical activity habit strength for more than a year following exercise rehabilitation programs [
72]. Further exploration is needed for how to effectively implement these and other potential effective approaches for utilising the time clinicians have with exercise rehabilitation patients to enhance patients’ physical activity motivation.
5.1. Conclusions
Physical activity is a cost-effective way to enhance cardiac and pulmonary patients’ quality and longevity of life [
7,
8], and exercise rehabilitation plays an important role in helping people engage in physical activity that is safe and beneficial. Our findings show that once rehabilitation programs end, patients’ physical activity levels decline, and their motivation for lifestyle physical activity does not improve. To ensure the longevity of the benefits of exercise rehabilitation for this important and widely prevalent at-risk population, more work is needed to enhance lifestyle physical activity motivation and behaviour amidst and following cardiac and pulmonary rehabilitation programs.
5.2. Future Directions
Future research efforts are needed to test the replicability and generalisability of our findings, with consideration of the limitations of our study. As a result of the intensive, rich person-level focus of the study, the data were from a small sample of relatively demographically homogenous patients from one exercise rehabilitation clinic. Geographical location, socio-demographic factors, and clinic-specific variables may have systematically impacted results. Future research is needed to test replicability using data from different locations, communities, and clinics. Our study focused on patients with any cardiac and pulmonary condition. Future research might tease out whether there are different patterns of physical activity behaviour or motivation between patients living with different cardiac or pulmonary diseases. Consideration is also needed to ensure such research is person-focused rather than condition-focused, given that physical and mental health conditions are oftentimes comorbid [
73].
Author Contributions
Conceptualization, K.L.A., B.G., J.J., C.D.A., C.V., & A.L.R.; methodology, K.L.A., B.G., J.J., C.D.A., & A.L.R.; formal analysis, K.L.A. & A.L.R; investigation, K.L.A., & A.L.R; resources, K.L.A., J.J., C.V., & A.L.R; data curation, K.L.A. & A.L.R; writing—original draft preparation, K.L.A., & A.L.R.; writing—review and editing, K.L.A., B.G., J.J., C.D.A., C.V., & A.L.R; supervision, K.L.A., J.J., C.V., & A.L.R; project administration, K.L.A.; funding acquisition, K.L.A., B.G., J.J., C.D.A., C.V., & A.L.R; All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Central Queensland University & Bundaberg Health Promotions LTD.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Central Queensland University (project number: 20840).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to restrictions from ethics committee to reduce risk of participant loss of confidentiality.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- World Health Organization. The Top 10 Causes of Death; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Nowbar, A.N.; Gitto, M.; Howard, J.P.; Francis, D.P.; Al-Lamee, R. Mortality from Ischemic Heart Disease. Circulation: Cardiovascular Quality and Outcomes 2019, 12, e005375. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Cao, X.; Guo, M.; Xie, M.; Liu, X. Trends and Risk Factors of Mortality and Disability Adjusted Life Years for Chronic Respiratory Diseases from 1990 to 2017: Systematic Analysis for the Global Burden of Disease Study 2017. BMJ 2020, 368, m234. [Google Scholar] [CrossRef] [PubMed]
- Bahall, M.; Legall, G.; Khan, K. Quality of Life among Patients with Cardiac Disease: The Impact of Comorbid Depression. Health Qual Life Outcomes 2020, 18, 189. [Google Scholar] [CrossRef] [PubMed]
- Blakemore, A.; Dickens, C.; Guthrie, E.; Bower, P.; Kontopantelis, E.; Afzal, C.; Coventry, P.A. Depression and Anxiety Predict Health-Related Quality of Life in Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. International Journal of Chronic Obstructive Pulmonary Disease 2014, 9, 501–512. [Google Scholar] [CrossRef]
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical Activity Level and Health-Related Quality of Life in the General Adult Population: A Systematic Review. Preventive Medicine 2007, 45, 401–415. [Google Scholar] [CrossRef]
- Winzer, E.B.; Woitek, F.; Linke, A. Physical Activity in the Prevention and Treatment of Coronary Artery Disease. Journal of the American Heart Association 2018, 7, e007725. [Google Scholar] [CrossRef]
- Salcedo, P.A.; Lindheimer, J.B.; Klein-Adams, J.C.; Sotolongo, A.M.; Falvo, M.J. Effects of Exercise Training on Pulmonary Function in Adults with Chronic Lung Disease: A Meta-Analysis of Randomized Controlled Trials. Archives of Physical Medicine and Rehabilitation 2018, 99, 2561–2569.e7. [Google Scholar] [CrossRef]
- Jeong, S.-W.; Kim, S.-H.; Kang, S.-H.; Kim, H.-J.; Yoon, C.-H.; Youn, T.-J.; Chae, I.-H. Mortality Reduction with Physical Activity in Patients with and without Cardiovascular Disease. European Heart Journal 2019, 40, 3547–3555. [Google Scholar] [CrossRef]
- Geidl, W.; Schlesinger, S.; Mino, E.; Miranda, L.; Pfeifer, K. Dose–Response Relationship between Physical Activity and Mortality in Adults with Noncommunicable Diseases: A Systematic Review and Meta-Analysis of Prospective Observational Studies. International Journal of Behavioral Nutrition and Physical Activity 2020, 17, e109. [Google Scholar] [CrossRef]
- Ostman, C.; Jewiss, D.; Smart, N.A. The Effect of Exercise Training Intensity on Quality of Life in Heart Failure Patients: A Systematic Review and Meta-Analysis. CRD 2017, 136, 79–89. [Google Scholar] [CrossRef]
- Driver, C.N.; Novotny, P.J.; Benzo, R.P. Differences in Sedentary Time, Light Physical Activity, and Steps Associated with Better COPD Quality of Life. Chronic Obstr Pulm Dis 2021, 9, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V. Effects of Cardiac Rehabilitation, Exercise Training, and Weight Reduction on Exercise Capacity, Coronary Risk Factors, Behavioral Characteristics, and Quality of Life in Obese Coronary Patients. The American Journal of Cardiology 1997, 79, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Pitta, F.; Troosters, T.; Probst, V.S.; Langer, D.; Decramer, M.; Gosselink, R. Are Patients with COPD More Active after Pulmonary Rehabilitation? Chest 2008, 134, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Chatziefstratiou, A.A.; Giakoumidakis, K.; Brokalaki, H. Cardiac Rehabilitation Outcomes: Modifiable Risk Factors. Br J Nurs 2013, 22, 200–207. [Google Scholar] [CrossRef]
- Hamburg, N.M.; Balady, G.J. Exercise Rehabilitation in Peripheral Artery Disease: Functional Impact and Mechanisms of Benefits. Circulation 2011, 123, 87–97. [Google Scholar] [CrossRef]
- McDermott, M.M. Exercise Rehabilitation for Peripheral Artery Disease: A Review. Journal of cardiopulmonary rehabilitation and prevention 2018, 38, 63–69. [Google Scholar] [CrossRef]
- Rochester, C.L. Exercise Training in Chronic Obstructive Pulmonary Disease. Journal of rehabilitation research and development 2003, 40, 59–80. [Google Scholar] [CrossRef]
- Dibben, G.O.; Dalal, H.M.; Taylor, R.S.; Doherty, P.; Tang, L.H.; Hillsdon, M. Cardiac Rehabilitation and Physical Activity: Systematic Review and Meta-Analysis. Heart 2018, 104, 1394–1402. [Google Scholar] [CrossRef]
- Ayabe, M.; Brubaker, P.H.; Dobrosielski, D.; Miller, H.S.; Ishi, K.; Yahiro, T.; Kiyonaga, A.; Shindo, M.; Tanaka, H. The Physical Activity Patterns of Cardiac Rehabilitation Program Participants. Journal of Cardiopulmonary Rehabilitation and Prevention 2004, 24, 80–86. [Google Scholar] [CrossRef]
- Gray, P.; Murphy, M.; Gallagher, A.; Simpson, E.E.A. A Qualitative Investigation of Physical Activity Compensation among Older Adults. Br J Health Psychol 2018, 23, 208–224. [Google Scholar] [CrossRef]
- Gomersall, S.R.; Rowlands, A.V.; English, C.; Maher, C.; Olds, T.S. The Activitystat Hypothesis. Sports Med 2013, 43, 135–149. [Google Scholar] [CrossRef] [PubMed]
- Gomersall, S.R.; Maher, C.; English, C.; Rowlands, A.V.; Dollman, J.; Norton, K.; Olds, T. Testing the Activitystat Hypothesis: A Randomised Controlled Trial. BMC Public Health 2016, 16, e900. [Google Scholar] [CrossRef] [PubMed]
- Kwasnicka, D.; Dombrowski, S.U.; White, M.; Sniehotta, F. Theoretical Explanations for Maintenance of Behaviour Change: A Systematic Review of Behaviour Theories. Health Psychology Review 2016, 10, 277–296. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Self-Determination Theory: When Mind Mediates Behavior. The Journal of Mind and Behavior 1980, 1, 33–43. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory and the Facilitation of Intrinsic Motivation, Social Development, and Well-Being. American Psychologist 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Biddle, S.; Soos, I.; Chatzisarantis, N. Predicting Physical Activity Intentions Using Goal Perspectives and Self-Determination Theory Approaches. European Psychologist 1999, 4, 83–89. [Google Scholar] [CrossRef]
- Chatzisarantis, N.L.D.; Biddle, S.J.H.; Meek, G.A. A Self-Determination Theory Approach to the Study of Intentions and the Intention–Behaviour Relationship in Children’s Physical Activity. British Journal of Health Psychology 1997, 2, 343–360. [Google Scholar] [CrossRef]
- Daley, A.J.; Duda, J.L. Self-Determination, Stage of Readiness to Change for Exercise, and Frequency of Physical Activity in Young People. European Journal of Sport Science 2006, 6, 231–243. [Google Scholar] [CrossRef]
- Gardner, B.; Lally, P. Does Intrinsic Motivation Strengthen Physical Activity Habit? Modeling Relationships between Self-Determination, Past Behaviour, and Habit Strength. Journal of Behavioral Medicine 2013, 36, 488–497. [Google Scholar] [CrossRef]
- Sweet, S.N.; Tulloch, H.; Fortier, M.S.; Pipe, A.L.; Reid, R.D. Patterns of Motivation and Ongoing Exercise Activity in Cardiac Rehabilitation Settings: A 24-Month Exploration from the TEACH Study. Annals of Behavioral Medicine 2011, 42, 55–63. [Google Scholar] [CrossRef]
- Russell, K.L.; Bray, S.R. Self-Determined Motivation Predicts Independent, Home-Based Exercise Following Cardiac Rehabilitation. Rehabilitation Psychology 2009, 54, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The Theory of Planned Behavior. Organizational Behavior and Human Decision Processes 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Triandis, H.C. Interpersonal Behavior; Brooks/Cole Publishing Company: Monterey, CA, 1977. [Google Scholar]
- Fishbein, M.; Ajzen, I. Predicting and Changing Behavior: The Reasoned Action Approach. Taylor & Francis, 2011; ISBN 978-1-136-87473-4. [Google Scholar]
- Blanchard, C.M.; Courneya, K.S.; Rodgers, W.M.; Daub, B.; Knapik, G. Determinants of Exercise Intention and Behavior during and after Phase 2 Cardiac Rehabilitation: An Application of the Theory of Planned Behavior. Rehabilitation Psychology 2002, 47, 308–323. [Google Scholar] [CrossRef]
- Blanchard, C.M.; Courneya, K.S.; Rodgers, W.M.; Fraser, S.N.; Murray, T.C.; Daub, B.; Black, B. Is the Theory of Planned Behavior a Useful Framework for Understanding Exercise Adherence during Phase II Cardiac Rehabilitation? Journal of Cardiopulmonary Rehabilitation and Prevention 2003, 23, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Rothman, A.J.; Sheeran, P.; Wood, W. Reflective and Automatic Processes in the Initiation and Maintenance of Dietary Change. Annals of Behavioral Medicine 2009, 38, s4–s17. [Google Scholar] [CrossRef]
- Gardner, B. A Review and Analysis of the Use of ‘Habit’ in Understanding, Predicting and Influencing Health-Related Behaviour. Health Psychology Review 2015, 9, 277–295. [Google Scholar] [CrossRef]
- Gardner, B.; Lally, P.; Rebar, A.L. Does Habit Weaken the Relationship between Intention and Behaviour? Revisiting the Habit-Intention Interaction Hypothesis. Social and Personality Psychology Compass 2020, 14, e12553. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Baranova, M.; Christian, H.; Westgarth, C. Increasing Physical Activity by Four Legs Rather than Two: Systematic Review of Dog-Facilitated Physical Activity Interventions. Br J Sports Med 2020, 54, 1202–1207. [Google Scholar] [CrossRef]
- Fleig, L.; Lippke, S.; Pomp, S.; Schwarzer, R. Intervention Effects of Exercise Self-Regulation on Physical Exercise and Eating Fruits and Vegetables: A Longitudinal Study in Orthopedic and Cardiac Rehabilitation. Preventive Medicine 2011, 53, 182–187. [Google Scholar] [CrossRef]
- Kaushal, N.; Payer, M.; Bérubé, B.; Juneau, M.; Bherer, L. Facilitating Exercise Habit Formation among Cardiac Rehabilitation Patients: A Randomized Controlled Pilot Trial. International Journal of Environmental Research and Public Health 2021, 18, 6440. [Google Scholar] [CrossRef]
- Deci, E.L.; Koestner, R.; Ryan, R.M. A Meta-Analytic Review of Experiments Examining the Effects of Extrinsic Rewards on Intrinsic Motivation. Psychological Bulletin 1999, 125, 627–668. [Google Scholar] [CrossRef] [PubMed]
- Rebar, A.L.; Rosenbaum, S.; Maher, J.P. Responsiveness to Change of the Psychological Determinants and Outcomes of Physical Activity and Sedentary Behavior. Psychology of Sport and Exercise 2020, 49, e101706. [Google Scholar] [CrossRef]
- Keller, J.; Kwasnicka, D.; Klaiber, P.; Sichert, L.; Lally, P.; Fleig, L. Habit Formation Following Routine-Based versus Time-Based Cue Planning: A Randomized Controlled Trial. British Journal of Health Psychology 2021, 26, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Judah, G.; Gardner, B.; Aunger, R. Forming a Flossing Habit: An Exploratory Study of the Psychological Determinants of Habit Formation. British journal of health psychology 2013, 18, 338–353. [Google Scholar] [CrossRef]
- Revelle, W. Psych: Procedures for Personality and Psychological Research 2021.
- Craig, C.L.; Marshall, A.L.; Sjorstrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.F.; Yngve, A.; Sallis, J.F. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Medicine and science in sports and exercise 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Markland, D.; Tobin, V. A Modification to the Behavioural Regulation in Exercise Questionnaire to Include an Assessment of Amotivation. Journal of Sport and Exercise Psychology 2004, 26, 191–196. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Rebar, A.L. Conceptualizing and Defining the Intention Construct for Future Physical Activity Research. Exercise and Sport Sciences Reviews 2017, 45, 209–216. [Google Scholar] [CrossRef]
- Gardner, B.; Abraham, C.; Lally, P.; de Bruijn, G.-J. Towards Parsimony in Habit Measurement: Testing the Convergent and Predictive Validity of an Automaticity Subscale of the Self-Report Habit Index. International Journal of Behavioral Nutrition and Physical Activity 2012, 9, 102–113. [Google Scholar] [CrossRef]
- Verplanken, B.; Orbell, S. Reflections on Past Behavior: A Self-Report Index of Habit Strength. Journal of Applied Social Psychology 2003, 33, 1313–1330. [Google Scholar] [CrossRef]
- R Core Team R: A Language and Environment for Statistical Computing 2023.
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. Journal of Statistical Software 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Lenth, R. Emmeans: Estimated Marginal Means, Aka Least-Squares Means 2022.
- Bartoń, K. MuMIn: Multi-Model Inference 2023.
- Arend, M.G.; Schäfer, T. Statistical Power in Two-Level Models: A Tutorial Based on Monte Carlo Simulation. Psychological Methods 2019, 24, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Snijders, T.A.B. Power and Sample Size in Multilevel Modeling. In Encyclopedia of statistics in behavioral science; Everitt, B.S., Howell, D.C., Eds.; Wiley: Chicester, 2005; Volume 3, pp. 1570–1573. [Google Scholar]
- McEachan, R.R.C.; Taylor, N.; Harrison, R.; Lawton, R.; Gardner, P.; Conner, M. Meta-Analysis of the Reasoned Action Approach (RAA) to Understanding Health Behaviors. Annals of Behavioral Medicine 2016, 50, 592–612. [Google Scholar] [CrossRef] [PubMed]
- Rebar, A.L.; Dimmock, J.A.; Jackson, B.; Rhodes, R.E.; Kates, A.; Starling, J.; Vandelanotte, C. A Systematic Review of the Effects of Non-Conscious Regulatory Processes in Physical Activity. Health Psychology Review 2016, 10, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Rebar, A.L.; Rhodes, R.E. Progression of Motivation Models in Exercise Science: Where We Have Been and Where We Are Heading. In The handbook of sport psychology; Tenenbaum, G., Eklund, R.C., Eds.; John Wiley & Sons, Inc.: Hoboken, New Jersey, USA, 2019; Volume 4, p. 63. [Google Scholar]
- Teixeira, P.J.; Carraça, E.V.; Markland, D.; Silva, M.N.; Ryan, R.M. Exercise, Physical Activity, and Self-Determination Theory: A Systematic Review. International Journal of Behavioral Nutrition and Physical Activity 2012, 9, 78–107. [Google Scholar] [CrossRef]
- Teo, J.L.; Zheng, Z.; Bird, S.R. Identifying the Factors Affecting ‘Patient Engagement’ in Exercise Rehabilitation. BMC Sports Science, Medicine and Rehabilitation 2022, 14, 18–28. [Google Scholar] [CrossRef]
- Schwarzer, R.; Luszczynska, A.; Ziegelmann, J.P.; Scholz, U.; Lippke, S. Social-Cognitive Predictors of Physical Exercise Adherence: Three Longitudinal Studies in Rehabilitation. Health Psychology 2008, 27, S54–S63. [Google Scholar] [CrossRef]
- Rahman, R.J.; Hudson, J.; Thøgersen-Ntoumani, C.; Doust, J.H. Motivational Processes and Well-Being in Cardiac Rehabilitation: A Self-Determination Theory Perspective. Psychology, Health & Medicine 2015, 20, 518–529. [Google Scholar] [CrossRef]
- Barbour, K.A.; Miller, N.H. Adherence to Exercise Training in Heart Failure: A Review. Heart Fail Rev 2008, 13, 81–89. [Google Scholar] [CrossRef]
- McGregor, G.; Powell, R.; Finnegan, S.; Nichols, S.; Underwood, M. Exercise Rehabilitation Programmes for Pulmonary Hypertension: A Systematic Review of Intervention Components and Reporting Quality. BMJ Open Sport & Exercise Medicine 2018, 4, e000400. [Google Scholar] [CrossRef]
- Fleig, L.; Pomp, S.; Parschau, L.; Barz, M.; Lange, D.; Schwarzer, R.; Lippke, S. From Intentions via Planning and Behavior to Physical Exercise Habits. Psychology of Sport and Exercise 2013, 14, 632–639. [Google Scholar] [CrossRef]
- Arnautovska, U.; Fleig, L.; O’Callaghan, F.; Hamilton, K. A Longitudinal Investigation of Older Adults’ Physical Activity: Testing an Integrated Dual-Process Model. Psychology & Health 2017, 32, 166–185. [Google Scholar] [CrossRef]
- Sniehotta, F.F.; Scholz, U.; Schwarzer, R. Action Plans and Coping Plans for Physical Exercise: A Longitudinal Intervention Study in Cardiac Rehabilitation. British Journal of Health Psychology 2006, 11, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Fleig, L.; Pomp, S.; Schwarzer, R.; Lippke, S. Promoting Exercise Maintenance: How Interventions with Booster Sessions Improve Long-Term Rehabilitation Outcomes. Rehabilitation Psychology 2013, 58, 323–333. [Google Scholar] [CrossRef]
- Carter, P.; Lagan, J.; Fortune, C.; Bhatt, D.L.; Vestbo, J.; Niven, R.; Chaudhuri, N.; Schelbert, E.B.; Potluri, R.; Miller, C.A. Association of Cardiovascular Disease with Respiratory Disease. Journal of the American College of Cardiology 2019, 73, 2166–2177. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).