Submitted:
04 September 2024
Posted:
05 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
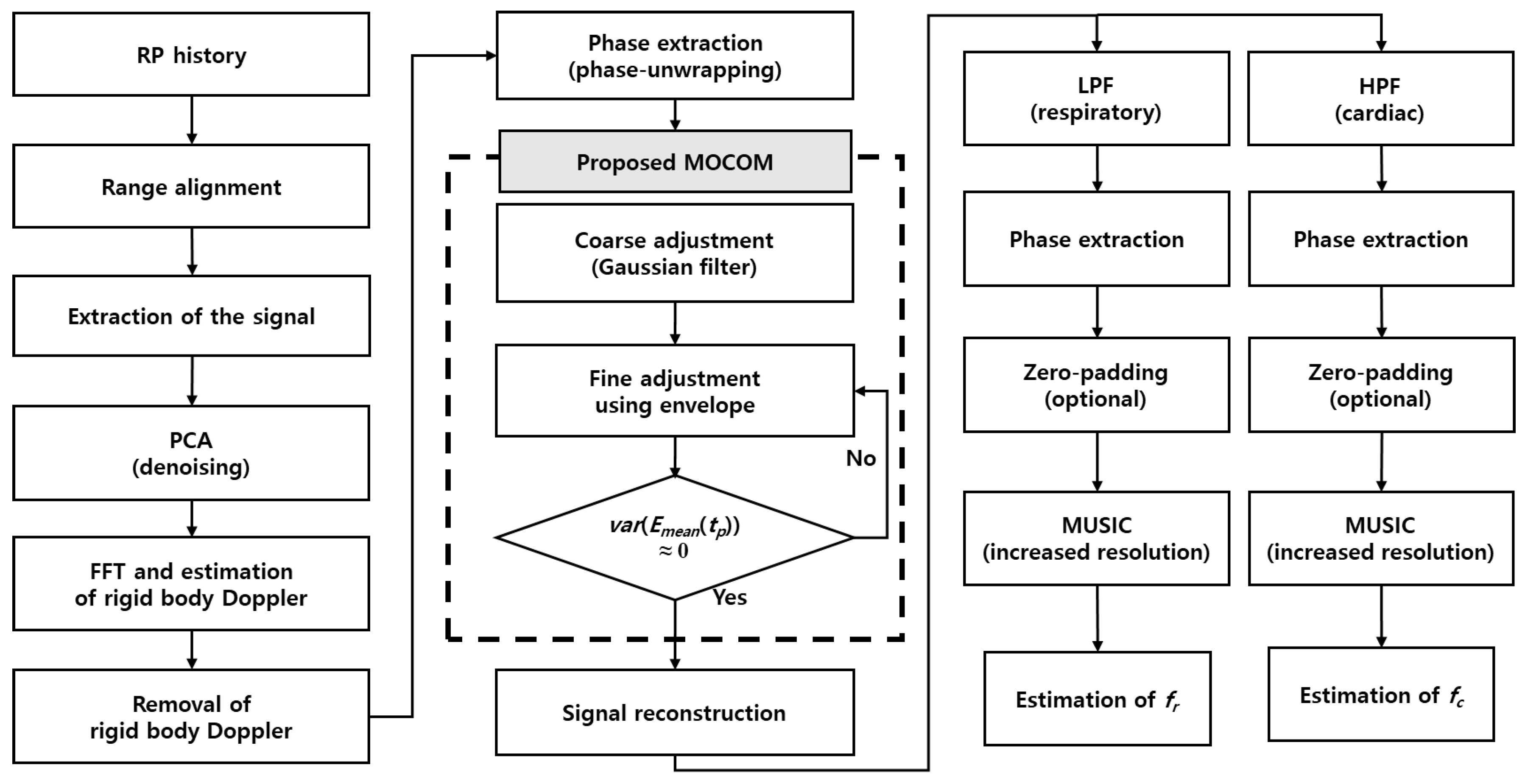
- Denoising and signal separation: The radar signal is denoised using principal component analysis (PCA).
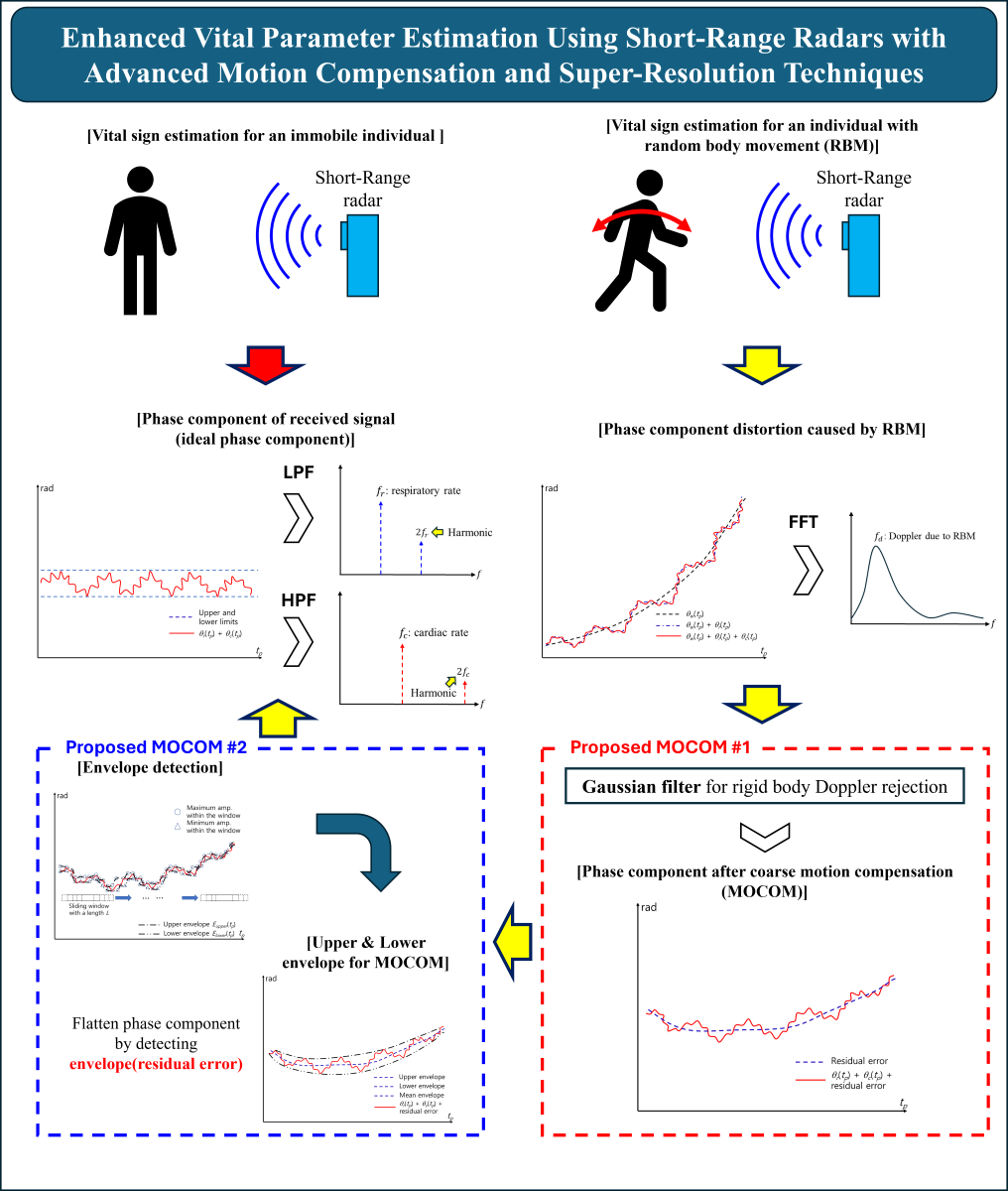
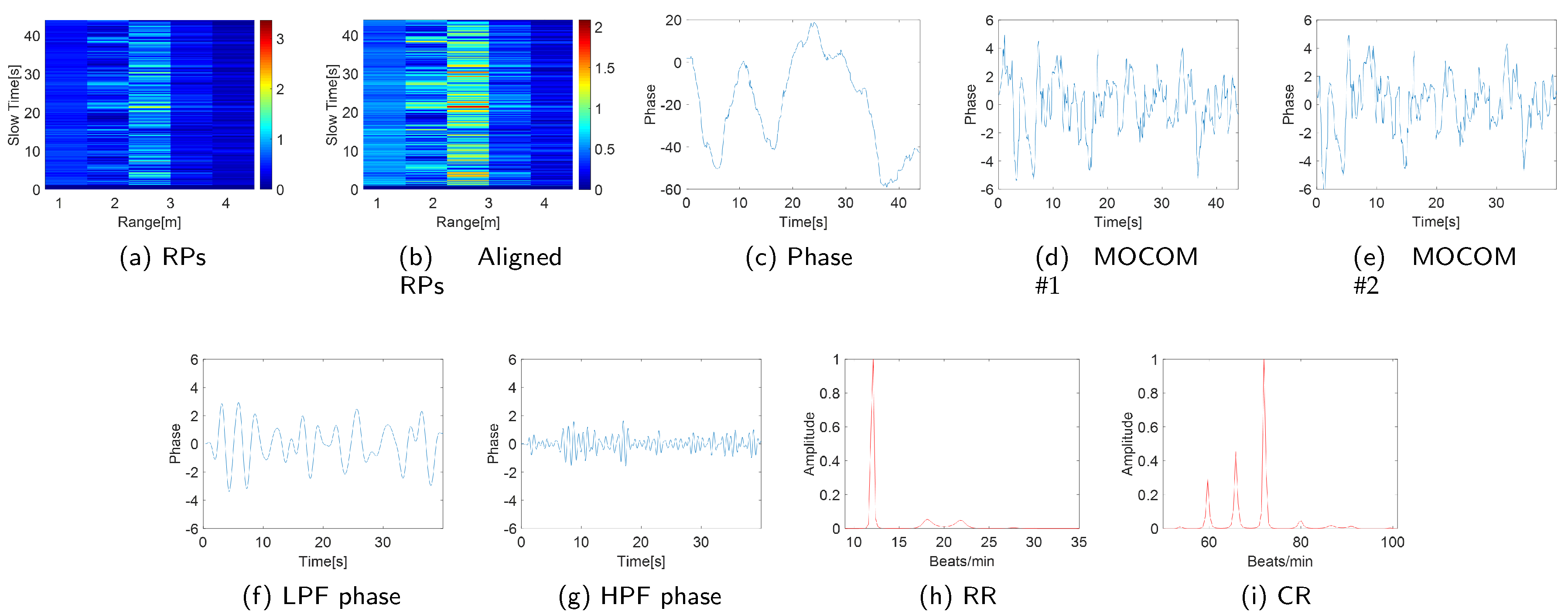
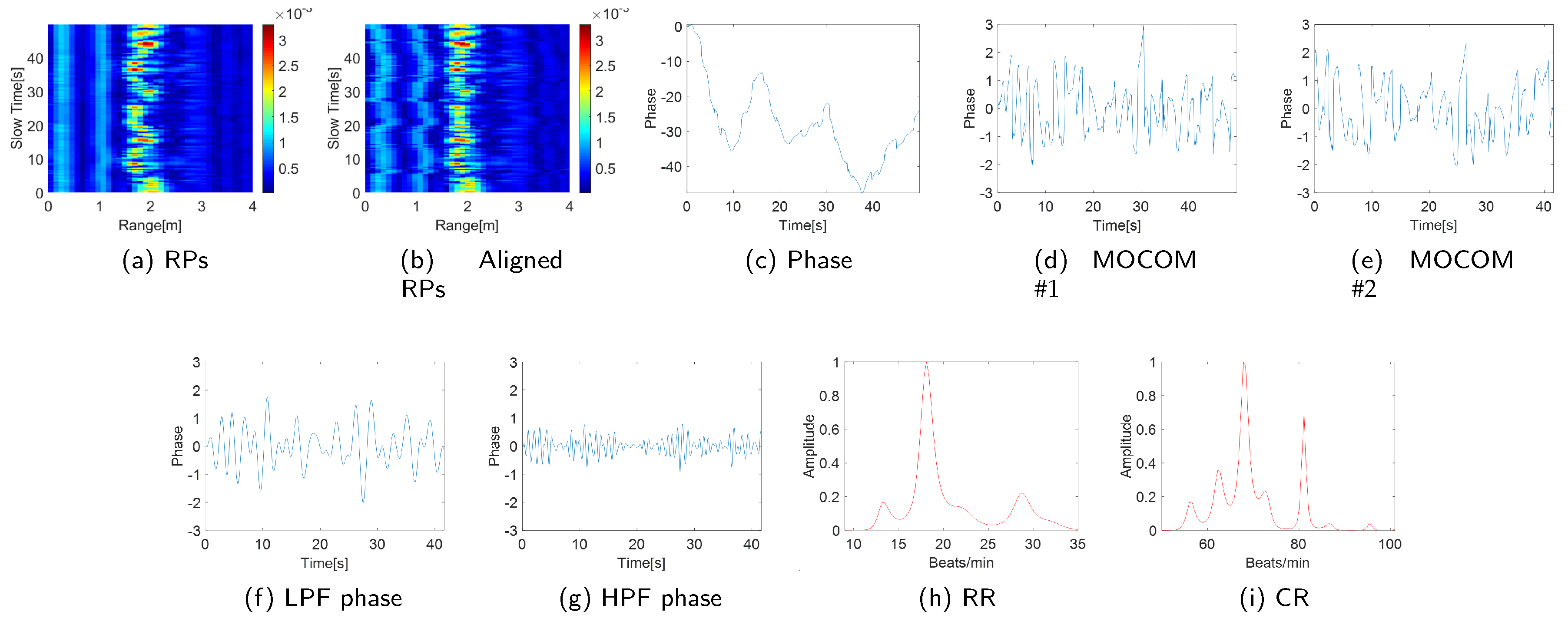
- Motion compensation (MOCOM): Based on an analysis of the phase components of the echo signal, two efficient MOCOM methods, MOCOM and MOCOM , are introduced.
- Noise reduction and auto-focusing: To further reduce noise and enhance resolution, the respiratory and cardiac signals are separated again and auto-focused.
- Super-resolution spectrum estimation: The multiple signal classification (MUSIC) method [26], a super-resolution technique, is used to obtain the spectra of the separated signals with very high resolution.
2. Signal Model and Problem Analysis
2.1. Radar Signal Model
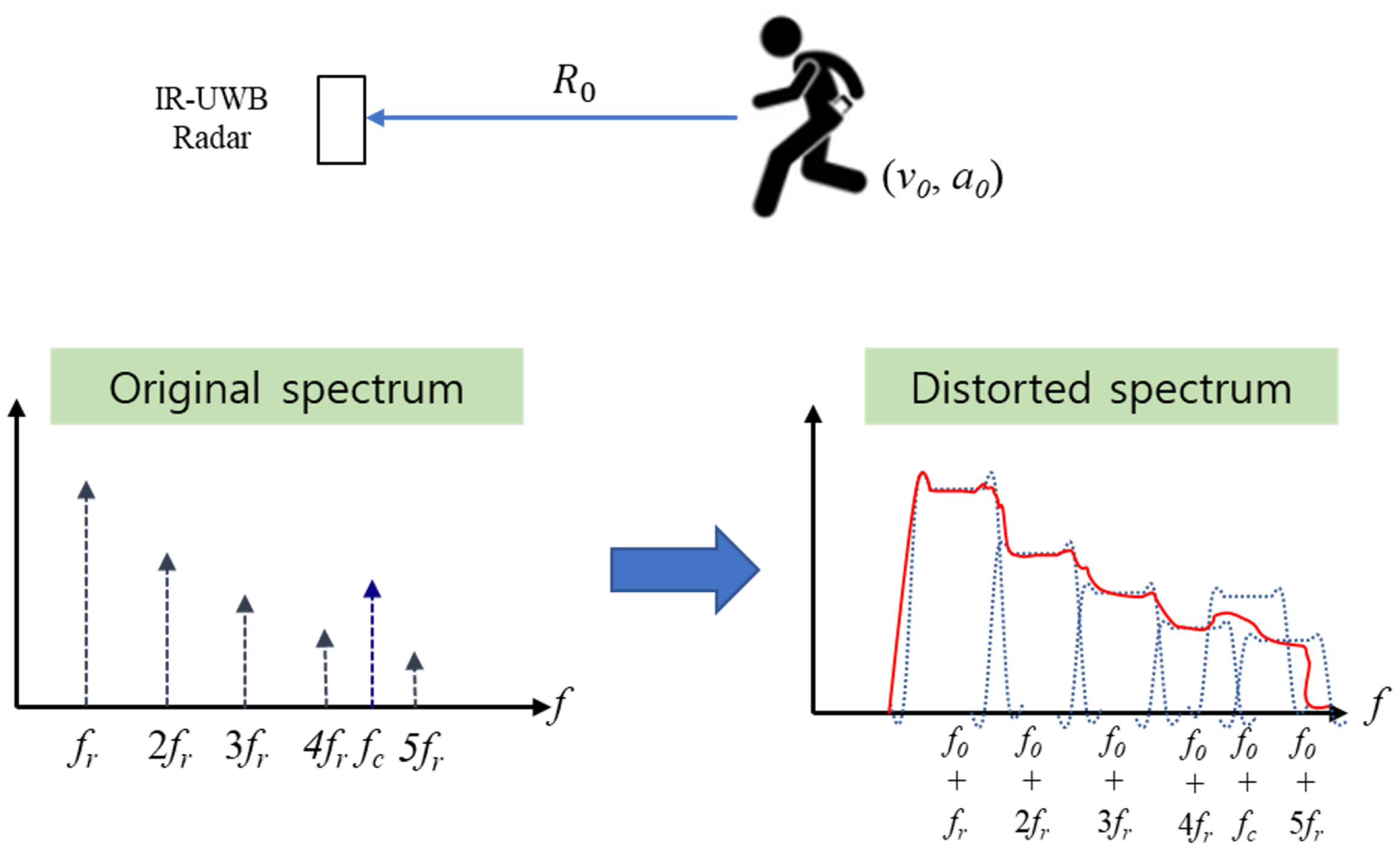
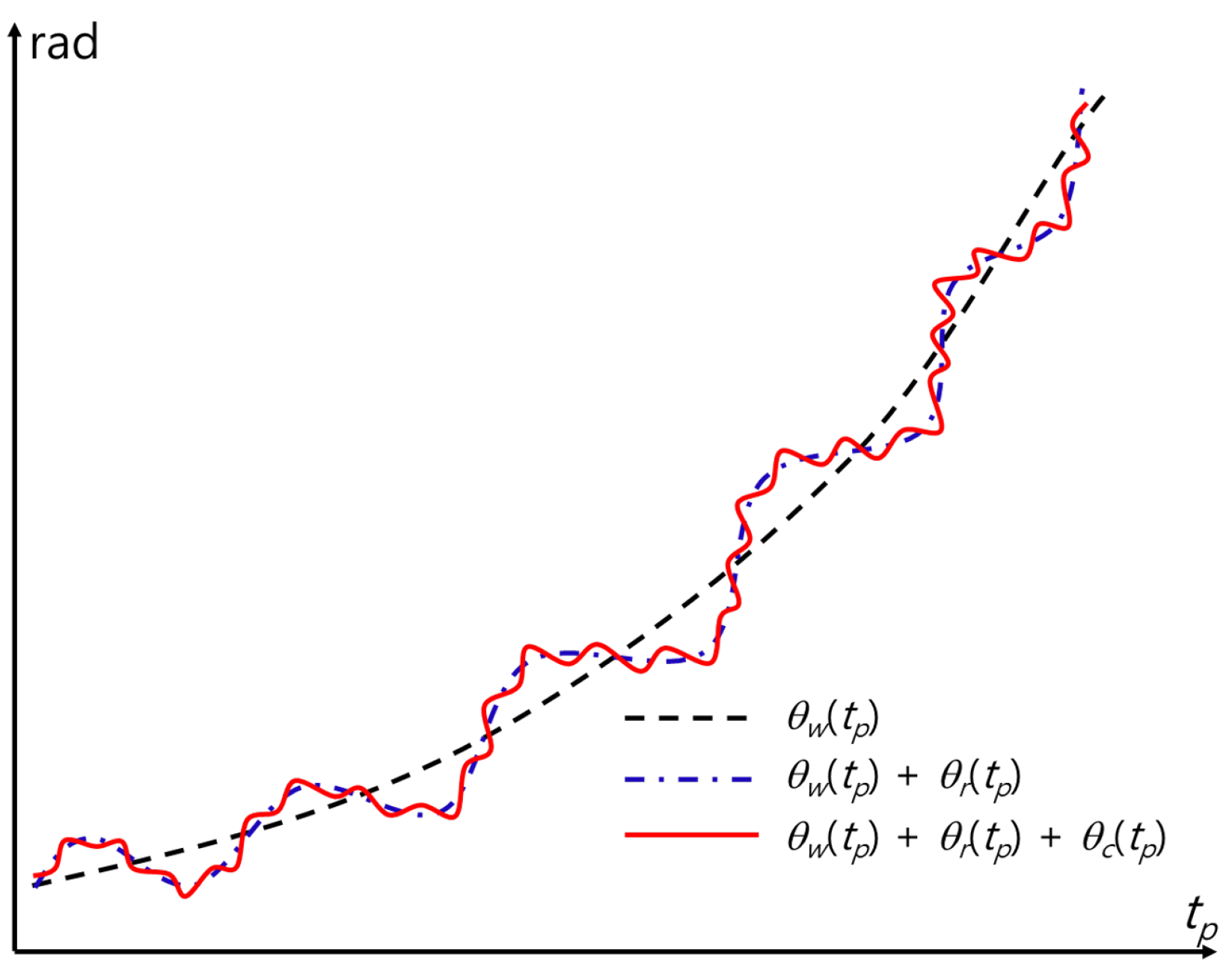
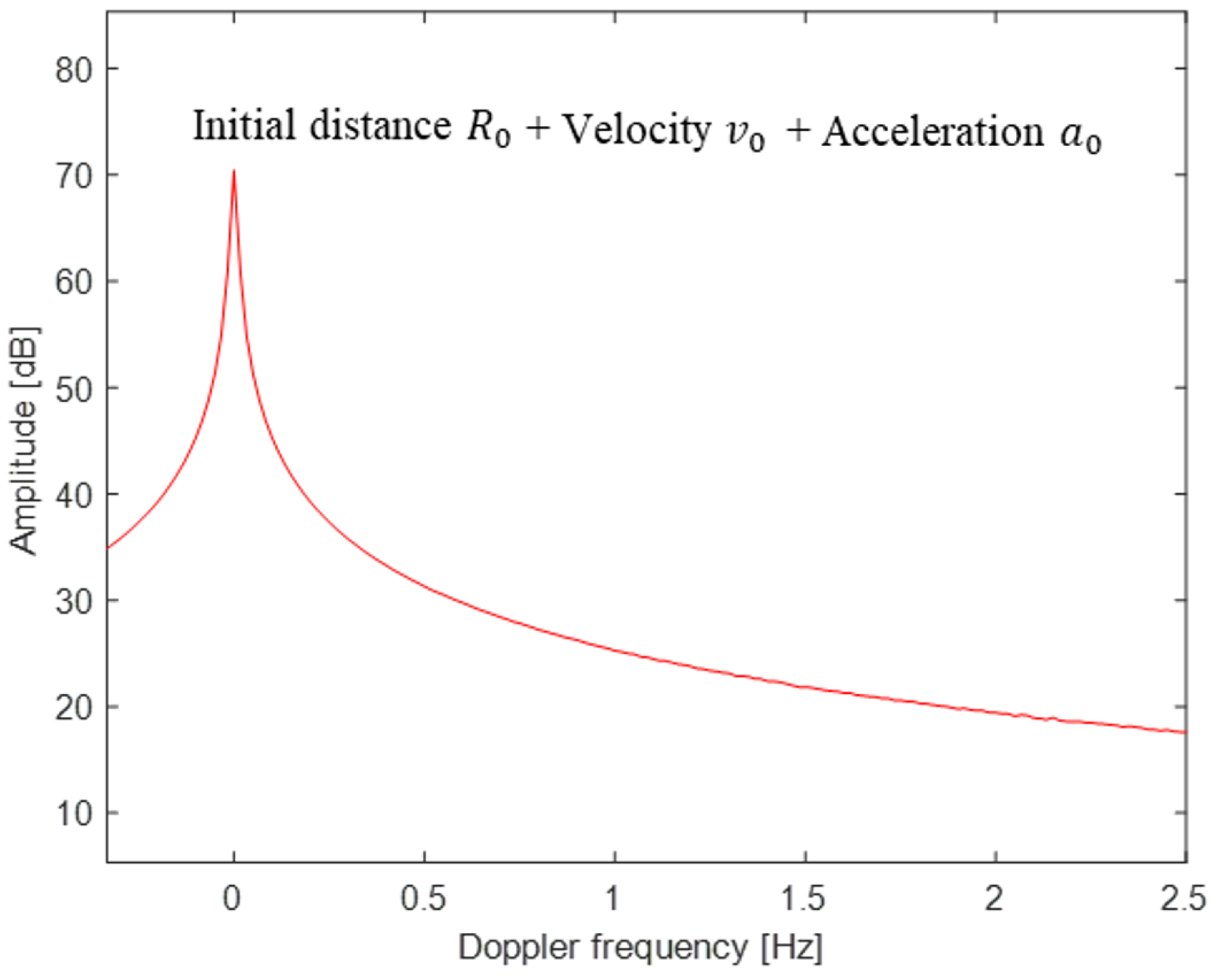
2.2. Effect of the Motion of the Rigid Body
3. Proposed Method
3.1. Summary of the Proposed Method
- ➀
- Align the range profile (RP) history of the received radar signal to position the scatterer in an identical location during the coherent processing interval, thereby removing range migration due to movement.
- ➁
- Clip the radar signal around the range bin with the maximum energy to estimate the vital parameters.
- ➂
- Apply PCA to denoise the radar signal and extract the torso and vital signals.
- ➃
- Estimate the rigid-body Doppler frequency using a fast Fourier transform (FFT) and remove the corresponding velocity.
- ➄
- Extract the phase history using a phase unwrapping technique.
- ➅
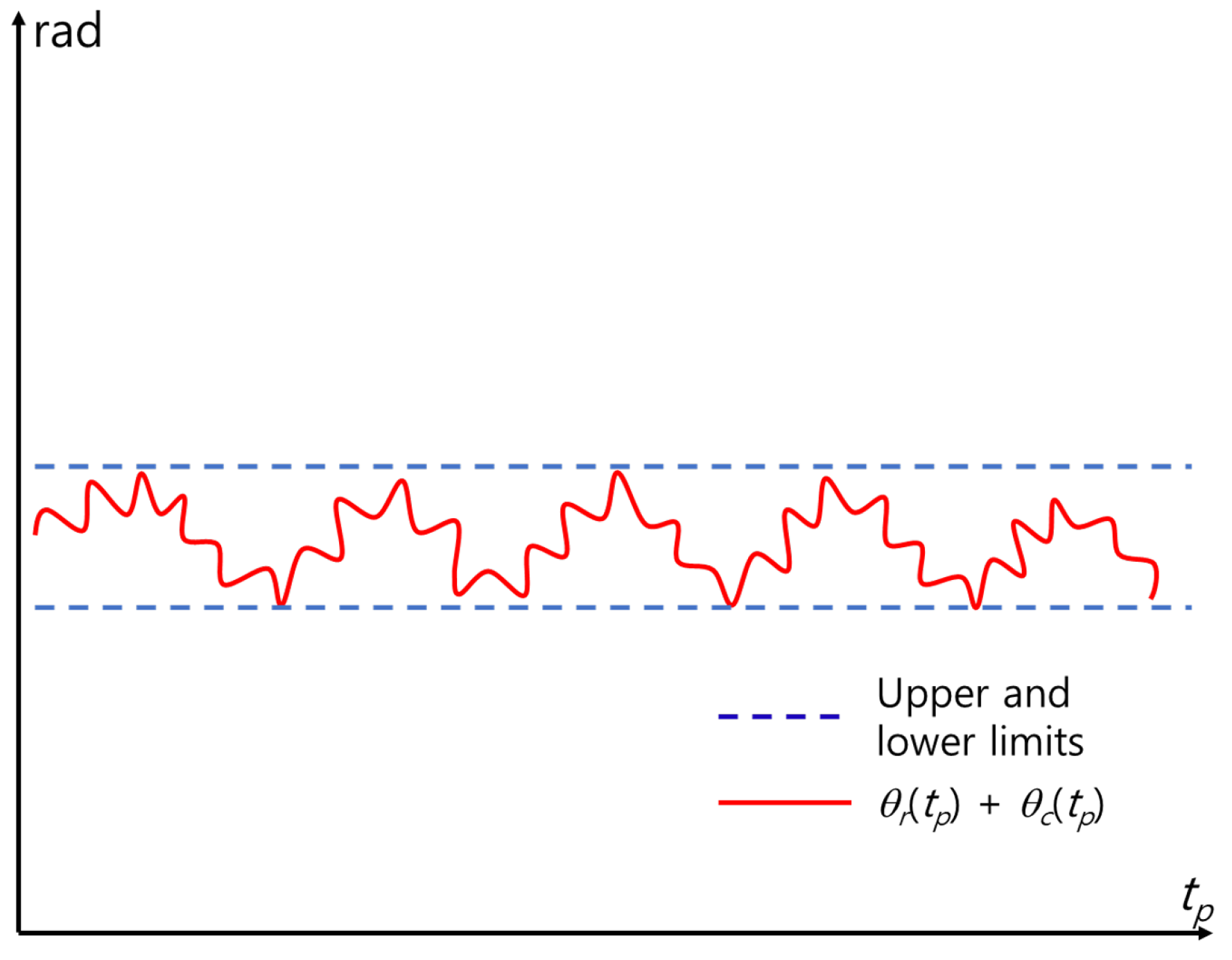
- Coarsely estimate the phase history via Gaussian filtering of the unwrapped phase and remove phase errors using the filtered phase history (MOCOM ).
- ➆
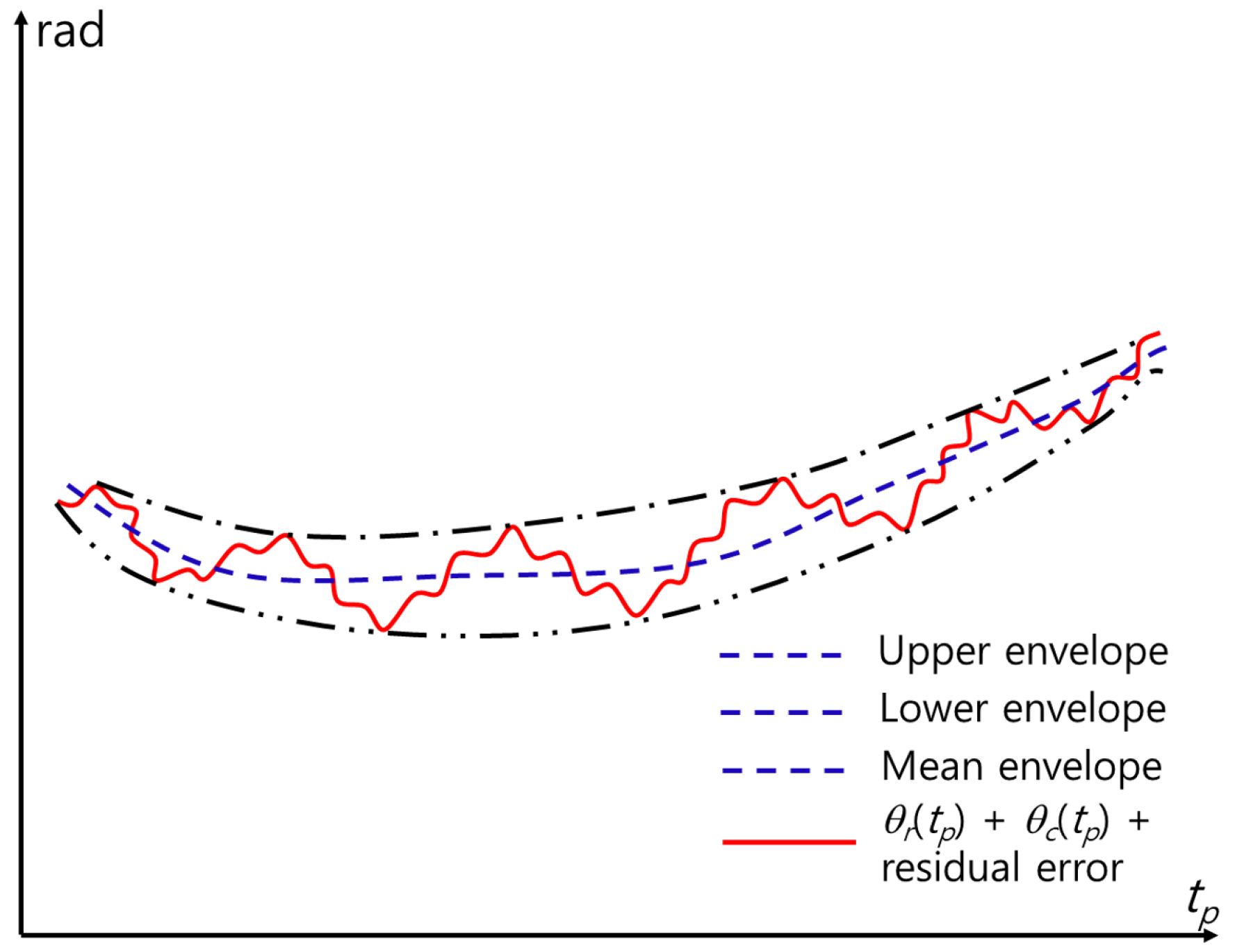
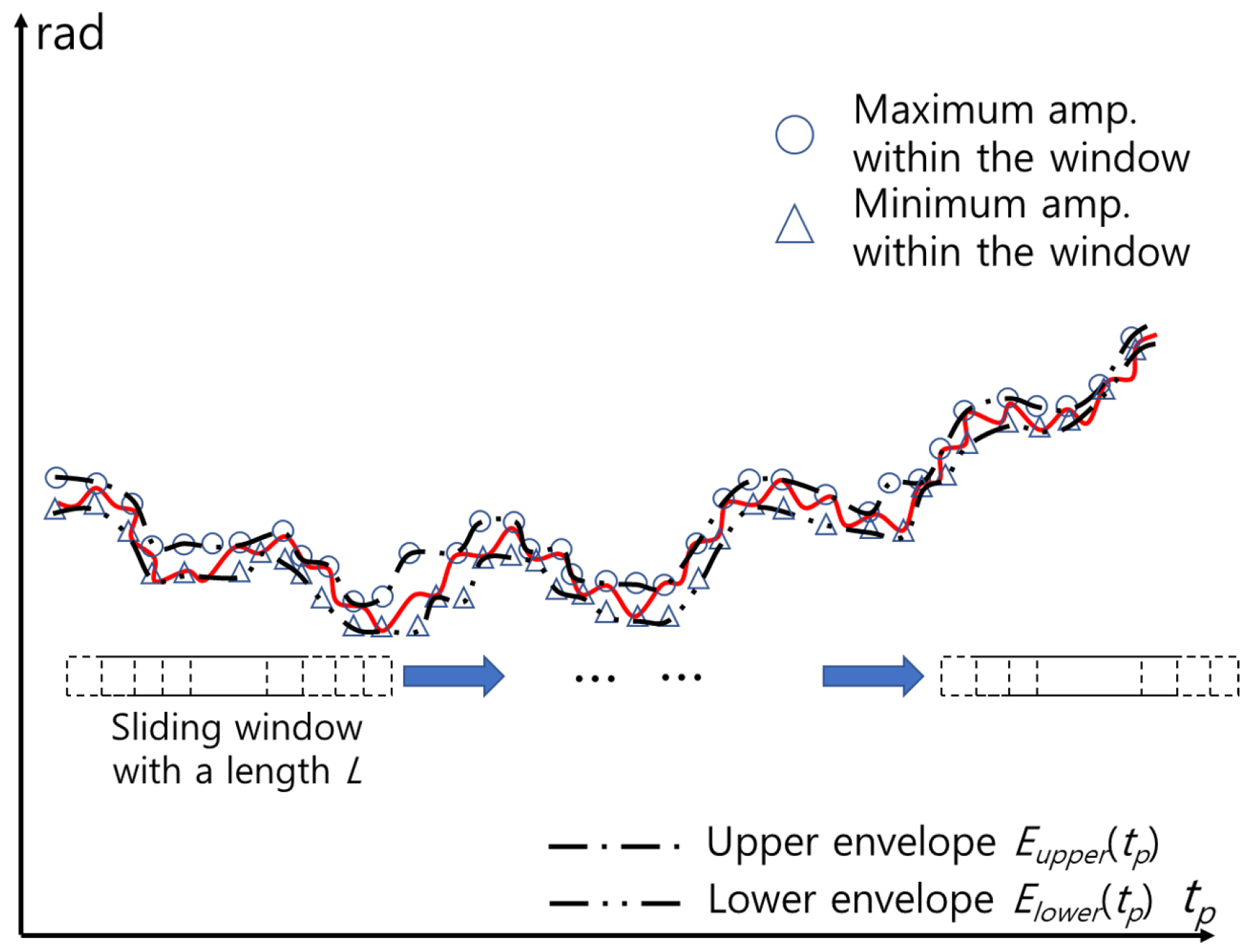
- Remove residual errors using the envelope (MOCOM ).
- ➇
- Reconstruct the complex signal using amplitude- and motion-compensated phases.
- ➈
- Further suppress noise and obtain super-resolution by separating the respiratory and cardiac signals using a low-pass filter (LPF) and high-pass filter (HPF).
- ➉
- Remove residual phase errors using a phase-adjustment technique for each of the separated signals.
- ⑪
- Optionally apply zero padding and then use the MUSIC algorithm to obtain the super-resolution spectrum of the separated signals.
- ⑫
- Estimate fr and fc by identifying the maximum peaks in each super-resolution spectrum.
3.2. Main Idea of the Proposed Method
3.2.1. Range Alignment
3.2.2. Extraction of Vital Signals and Denosing Using PCA
3.2.3. Estimation and Removal of the Rigid-Body Doppler
3.2.4. MOCOM
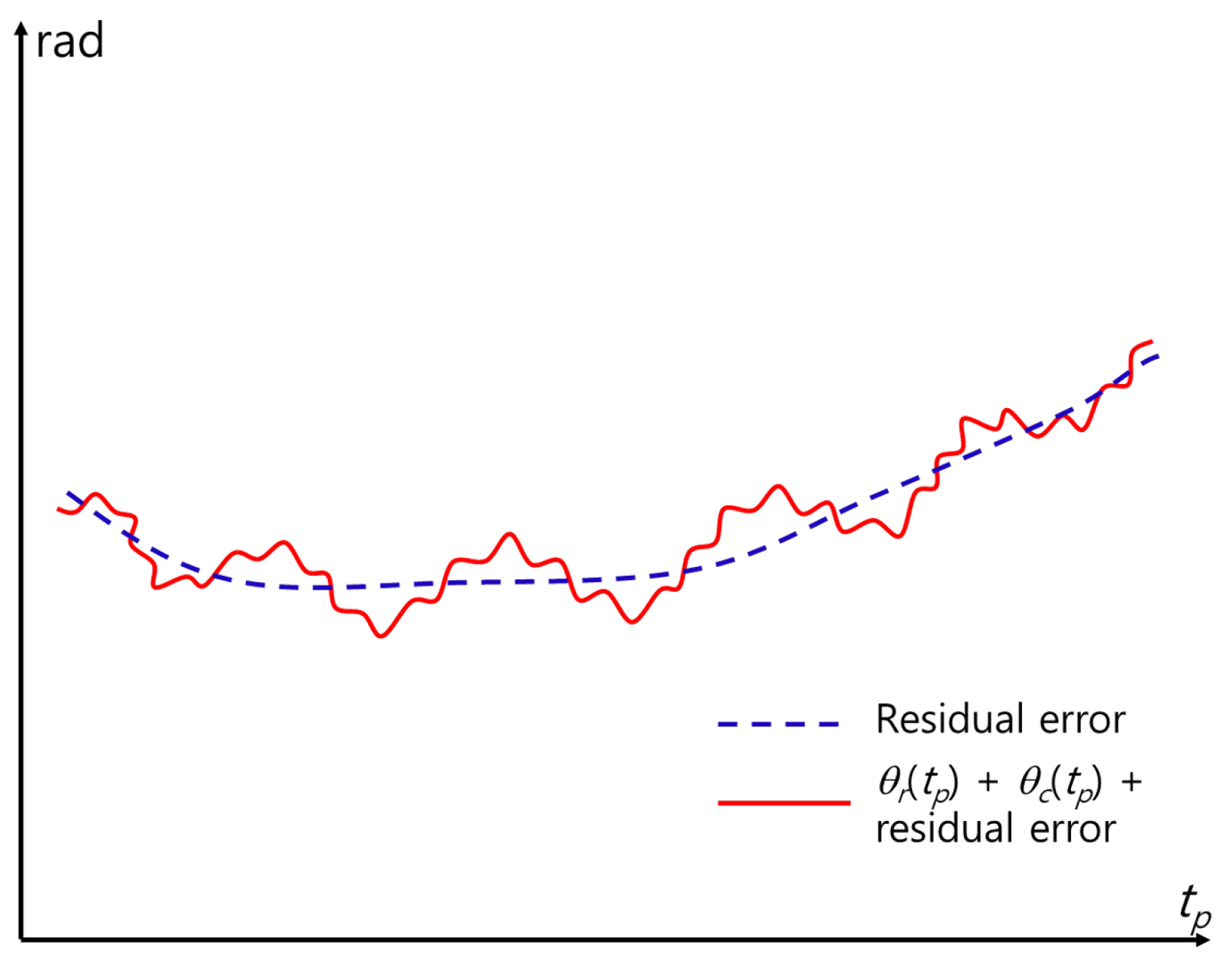
3.2.5. MOCOM
3.2.6. Reconstruction of Signals and Separation of Vital Signals Using LPF and HPF
3.2.7. Phase Adjustment
3.2.8. Zero-Padding and Application of MUSIC
4. Experimental Results
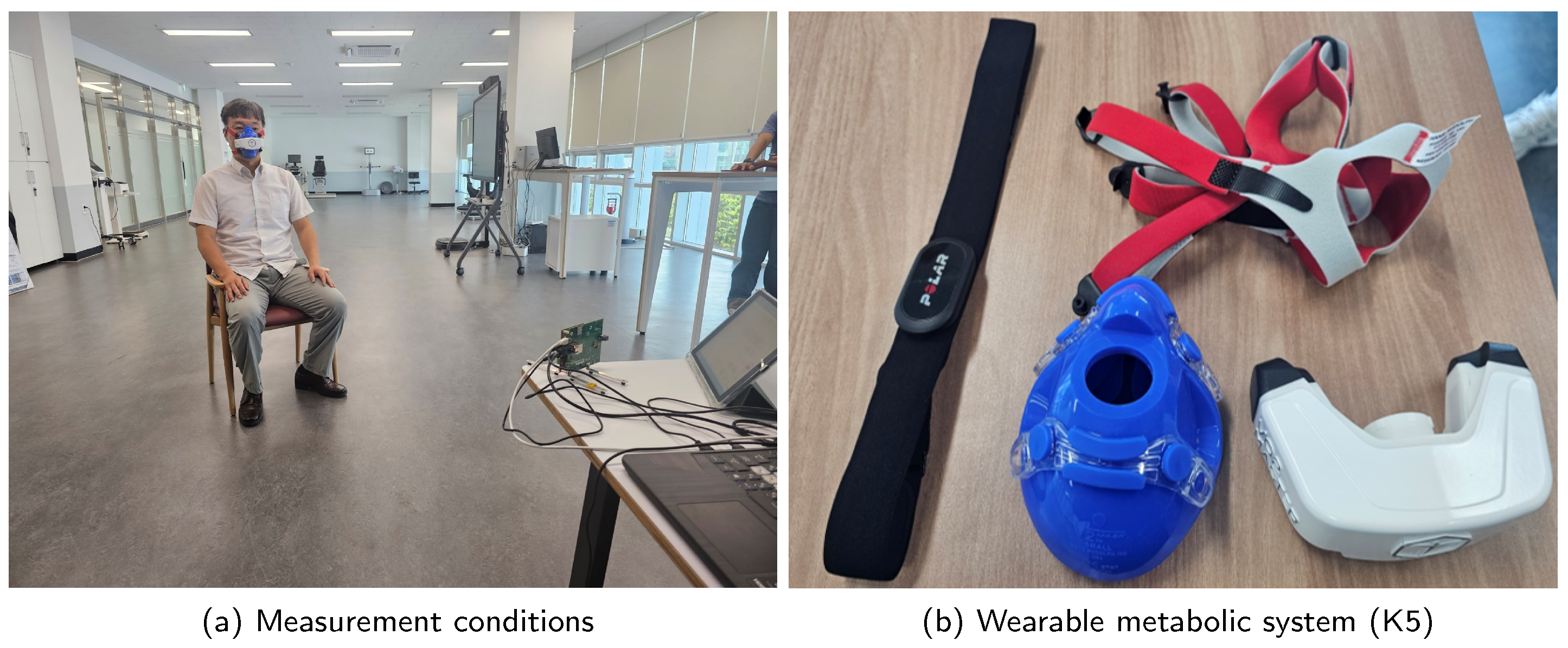
4.1. Experimental Condition
- The method in [16] compensated for phase error by detecting constant Doppler shift due to random body movement.
- The conventional method in [20] used a fuzzy rule to mitigate the effects of random movement.
- The method in [25] employed empirical mode decomposition (EMD).
- The method in [35] used VMD to detect vital signs.
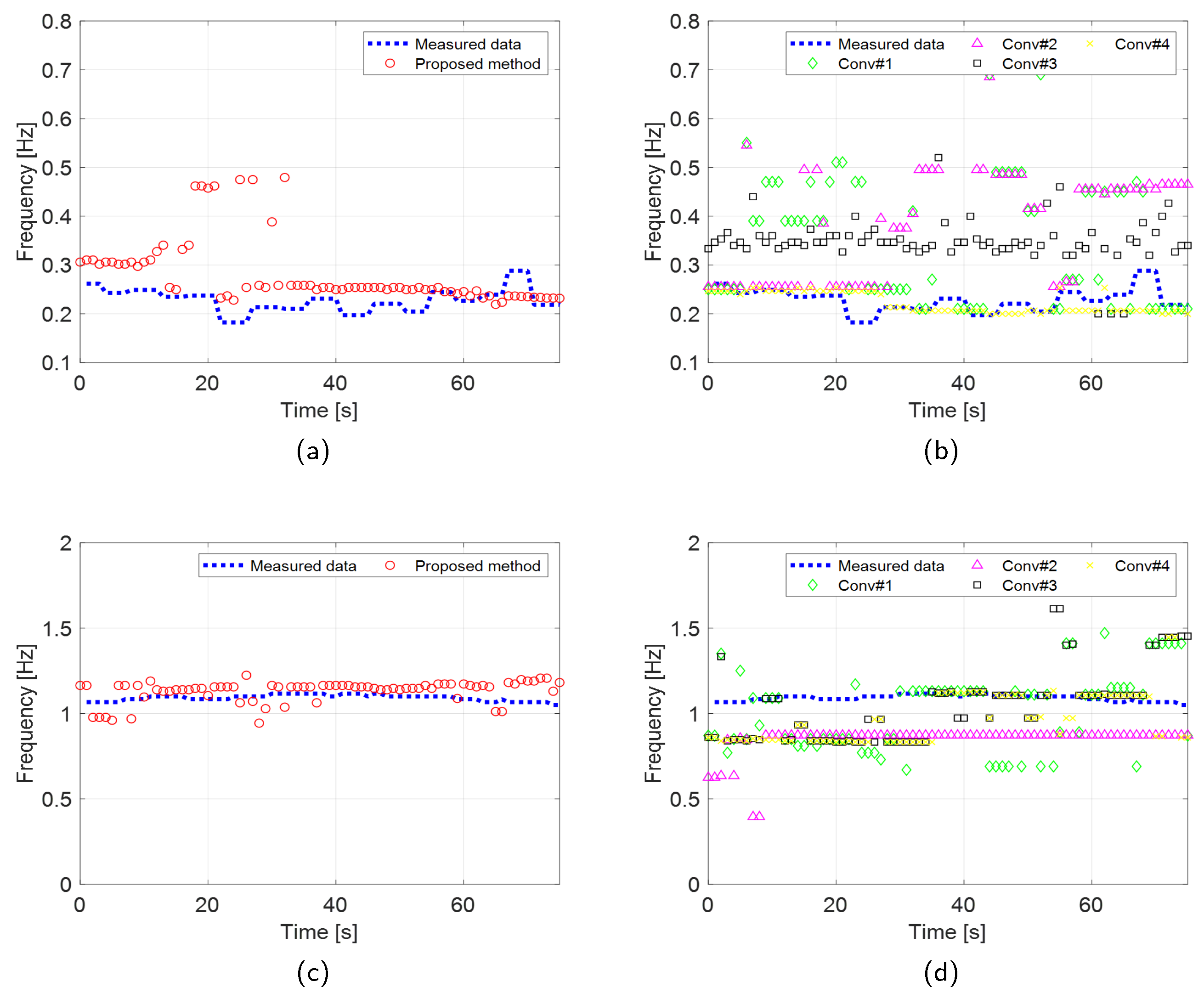
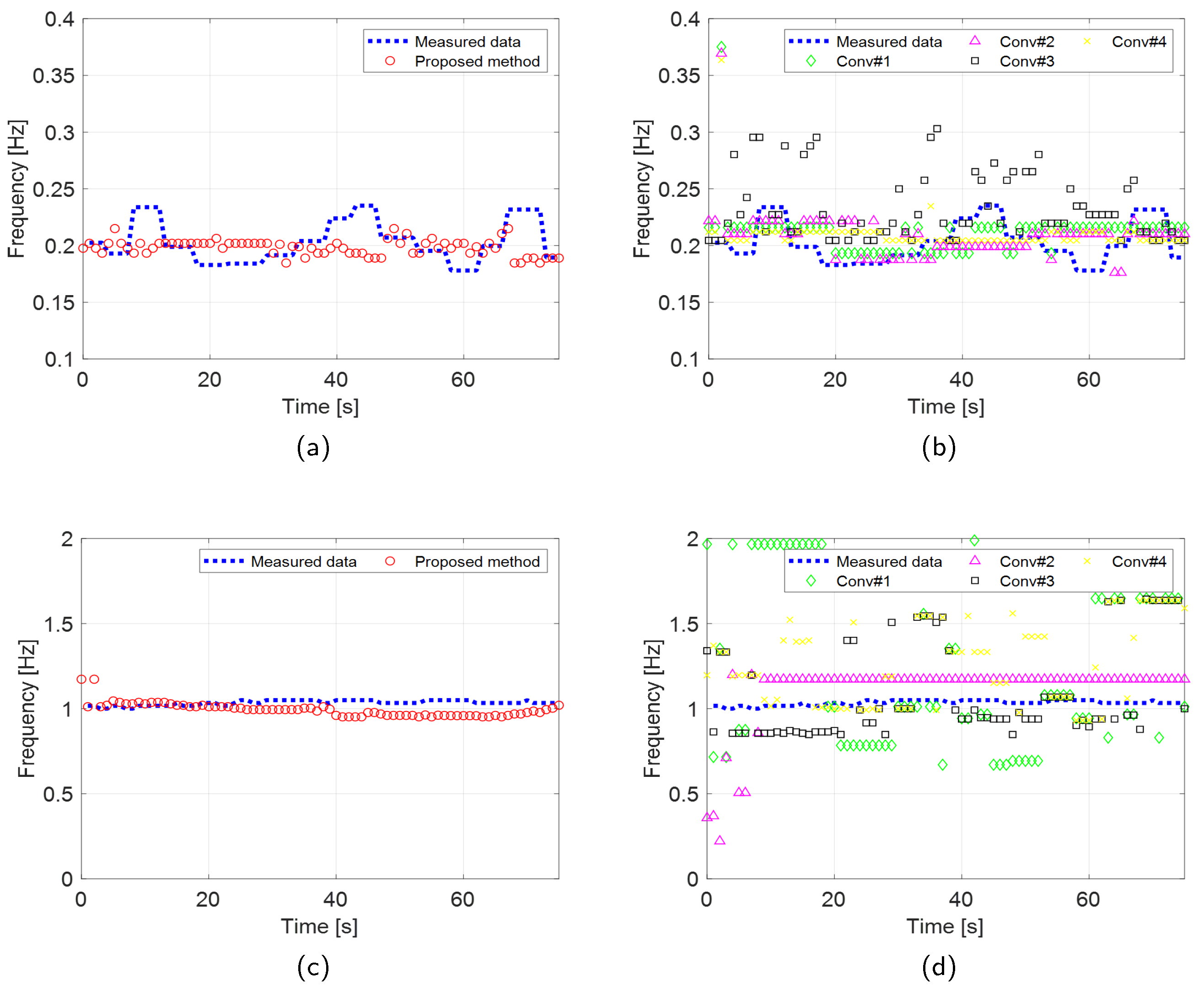
4.2. Estimation Accuracy and Robustness of the Proposed Scheme
5. Conclusions
References
- Staderini, E. UWB radars in medicine. IEEE Aerosp. Electron. Syst. Mag. 2002, 17, 13–18. [Google Scholar] [CrossRef]
- Droitcour, A.; Boric-Lubecke, O.; Lubecke, V.; Lin, J.; Kovacs, G. Range correlation and I/Q performance benefits in single-chip silicon Doppler radars for noncontact cardiopulmonary monitoring. IEEE Trans. Microw. Theory Techn. 2004, 52, 838–848. [Google Scholar] [CrossRef]
- Gu, C.; Li, R.; Zhang, H.; Fung, A.Y.C.; Torres, C.; Jiang, S.B.; Li, C. Accurate Respiration Measurement Using DC-Coupled Continuous-Wave Radar Sensor for Motion-Adaptive Cancer Radiotherapy. IEEE Trans. Biomed. Eng. 2012, 59, 3117–3123. [Google Scholar] [CrossRef]
- Hu, W.; Zhao, Z.; Wang, Y.; Zhang, H.; Lin, F. Noncontact Accurate Measurement of Cardiopulmonary Activity Using a Compact Quadrature Doppler Radar Sensor. IEEE Trans. Biomed. Eng. 2014, 61, 725–735. [Google Scholar] [CrossRef]
- An, Y.J.; Yun, G.H.; Yook, J.G. Sensitivity Enhanced Vital Sign Detection Based on Antenna Reflection Coefficient Variation. IEEE Trans. Biomed. Circuits Syst. 2016, 10, 319–327. [Google Scholar] [CrossRef]
- Li, C.; Peng, Z.; Huang, T.Y.; Fan, T.; Wang, F.K.; Horng, T.S.; Muñoz-Ferreras, J.M.; Gómez-García, R.; Ran, L.; Lin, J. A Review on Recent Progress of Portable Short-Range Noncontact Microwave Radar Systems. IEEE Trans. Microw. Theory Techn. 2017, 65, 1692–1706. [Google Scholar] [CrossRef]
- Park, J.K.; Hong, Y.; Lee, H.; Jang, C.; Yun, G.H.; Lee, H.J.; Yook, J.G. Noncontact RF Vital Sign Sensor for Continuous Monitoring of Driver Status. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 493–502. [Google Scholar] [CrossRef]
- Zhang, Y.; Qi, F.; Lv, H.; Liang, F.; Wang, J. Bioradar Technology: Recent Research and Advancements. IEEE Microw. Mag. 2019, 20, 58–73. [Google Scholar] [CrossRef]
- Lee, H.; Kim, B.H.; Park, J.K.; Kim, S.W.; Yook, J.G. A Resolution Enhancement Technique for Remote Monitoring of the Vital Signs of Multiple Subjects Using a 24 Ghz Bandwidth-Limited FMCW Radar. IEEE Access 2020, 8, 1240–1248. [Google Scholar] [CrossRef]
- LAZARO, A.; Girbau, D.; Villariono, R. Analysis of vital signs monitoring using an IR-UWB radar. Prog. Electromagn. Res. 2010, 1, 100. [Google Scholar] [CrossRef]
- Nezirovic, A.; Yarovoy, A.G.; Ligthart, L.P. Signal Processing for Improved Detection of Trapped Victims Using UWB Radar. IEEE Trans. Geosci. Remote Sens. 2010, 48, 2005–2014. [Google Scholar] [CrossRef]
- Sachs, A. Handbook of Ultra-wideband Short-range Sensing: Theory Sensors Applications; John Wiley and Sons, 2013.
- Lazaro, A.; Girbau, D.; Villarino, R.M. Techniques for Clutter Suppression in the Presence of Body Movements during the Detection of Respiratory Activity through UWB Radars. Sensors 2014, 14, 2595–2618. [Google Scholar] [CrossRef] [PubMed]
- Jürgen, S.; Herrmann, R. M-sequence-based ultra-wideband sensor network for vitality monitoring of elders at home. IET Radar, Sonar Navigation 2015, 9, 125–137. [Google Scholar] [CrossRef]
- Adib, F.; Mao, H.; Kabelac, Z.; Katabi, D.; Miller, R.C. Smart Homes that Monitor Breathing and Heart Rate. Proceedings of the CHI Conference on Human Factors in Computing Systems; Association for Computing Machinery: New York, NY, USA, 2015. [Google Scholar] [CrossRef]
- Tu, J.; Hwang, T.; Lin, J. Respiration Rate Measurement Under 1-D Body Motion Using Single Continuous-Wave Doppler Radar Vital Sign Detection System. IEEE Trans. Microw. Theory Techn. 2016, 64, 1937–1946. [Google Scholar] [CrossRef]
- Li, C.; Lin, J. Random Body Movement Cancellation in Doppler Radar Vital Sign Detection. IEEE Trans. Microw. Theory Techn. 2008, 56, 3143–3152. [Google Scholar] [CrossRef]
- Schires, E.; Georgiou, P.; Lande, T.S. Vital Sign Monitoring Through the Back Using an UWB Impulse Radar With Body Coupled Antennas. IEEE Trans Biomed. Circuits Syst. 2018, 12, 292–302. [Google Scholar] [CrossRef]
- Xiang, M.; Ren, W.; Li, W.; Xue, Z.; Jiang, X. High-Precision Vital Signs Monitoring Method Using a FMCW Millimeter-Wave Sensor. Sensors 2022, 22, 7543. [Google Scholar] [CrossRef]
- Choi, I.; Kim, M.; Choi, J.; Park, J.; Park, S.; Kim, K. Robust Cardiac Rate Estimation of an Individual. IEEE Sens. 2021, 21, 15053–15064. [Google Scholar] [CrossRef]
- Liu, T.H.; Hsu, M.L.; Tsai, Z.M. High Ranging Accuracy and Wide Detection Range Interferometry Based on Frequency-Sweeping Technique With Vital Sign Sensing Function. IEEE Trans. Microw. Theory Techn. 2018, 66, 4242–4251. [Google Scholar] [CrossRef]
- Gu, C.; Peng, Z.; Li, C. High-Precision Motion Detection Using Low-Complexity Doppler Radar With Digital Post-Distortion Technique. IEEE Trans. Microw. Theory Techn. 2016, 64, 961–971. [Google Scholar] [CrossRef]
- Yavari, E.; Boric-Lubecke, O. Channel Imbalance Effects and Compensation for Doppler Radar Physiological Measurements. IEEE Trans. Microw. Theory Techn. 2015, 63, 3834–3842. [Google Scholar] [CrossRef]
- He, M.; Nian, Y.; Liu, B. Noncontact heart beat signal extraction based on wavelet transform. 2015 8th International Conference on Biomedical Engineering and Informatics (BMEI), 2015, pp. 209–213. [CrossRef]
- Feng, J.C.; Pan, S.Y. Extraction algorithm of vital signals based on empirical mode decomposition. J. South China Univ. Technol. 2010, 38, 1–6. [Google Scholar] [CrossRef]
- Kim, K.T.; Seo, D.K.; Kim, H.T. Efficient radar target recognition using the MUSIC algorithm and invariant features. IEEE Trans. Antennas and Propag. 2002, 50, 325–337. [Google Scholar] [CrossRef]
- Yoon, S.; Kim, S.; Jung, J.; Cha, S.; Baek, Y.; Koo, B.; Choi, I.; Park, S. Efficient Protocol to Use FMCW Radar and CNN to Distinguish Micro-Doppler Signatures of Multiple Drones and Birds. IEEE Access 2022, 10, 26033–26044. [Google Scholar] [CrossRef]
- Mahuza, B. Radar Systems Analysis and Design Using MATLAB, 4th ed.; CRC Press, 2022.
- Soumekh, M. Synthetic Aperture Radar Signal Processing with MATLAB Algorithms, 1st ed.; Wiley, 1999.
- Zheng, J.; Liu, H.; Liao, G.; Su, T.; Liu, Z.; Liu, Q.H. ISAR Imaging of Targets With Complex Motions Based on a Noise-Resistant Parameter Estimation Algorithm Without Nonuniform Axis. IEEE Sens. 2016, 16, 2509–2518. [Google Scholar] [CrossRef]
- V., A.; Ranjith, M.R.; M., R.; Sowmyah, N.; L., V. V., A.; Ranjith, M.R.; M., R.; Sowmyah, N.; L., V. Comparison of curve fitting methods for synthetic generation of PPG. 2023 IEEE 20th India Council International Conference (INDICON), 2023, pp. 447–451. [CrossRef]
- Pozar, D.M. Microwave Engineering; Wiley, 2012.
- Faires, J.D.; Burden, R.L. Numerical Methods; Brooks Cole, 2002.
- Wang, J.; Kasilingam, D.; Liu, X.; Zhou, Z. ISAR minimum-entropy phase adjustment. Proceedings of the 2004 IEEE Radar Conference (IEEE Cat. No.04CH37509), 2004, pp. 197–200. [CrossRef]
- Ding, C.; Yan, J.; Zhang, L.; Zhao, H.; Hong, H.; Zhu, X. Noncontact multiple targets vital sign detection based on VMD algorithm. 2017 IEEE Radar Conference (RadarConf), 2017, pp. 0727–0730. [CrossRef]
| Paremater | X4M03 | Distance2GoL |
|---|---|---|
| Center frequency () | 7.29 GHz | 24 GHz |
| Bandwidth (B) | 1.5 GHz | 200 MHz |
| Maximum range | 10 m | 10 m |
| Frame time () | 40 s | 40 s |
| Pulse repetition time () | 0.0417 s | 0.02 s |
| No. of samples per frame | 960 | 2000 |
| Frame time interval | 1 s | 1 s |
| Observation time | 115 s | 115 s |
| Distance to target | 2 m | 2 m |
| Proposed | |||||
|---|---|---|---|---|---|
| RR(IR-UWB) | 0.091 | 0.2675 | 0.3129 | 0.1315 | 0.0298 |
| CR(IR-UWB) | 0.0772 | 0.2427 | 0.26 | 0.2203 | 0.1898 |
| RR(FMCW) | 0.0219 | 0.028 | 0.0288 | 0.043 | 0.0273 |
| CR(FMCW) | 0.064 | 0.5084 | 0.2102 | 0.2759 | 0.3319 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).