Submitted:
06 September 2024
Posted:
06 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. CT Scanning
2.3. CT Image Evaluation
2.4. Statistical Analysis
3. Results
3.1. Clinical Information
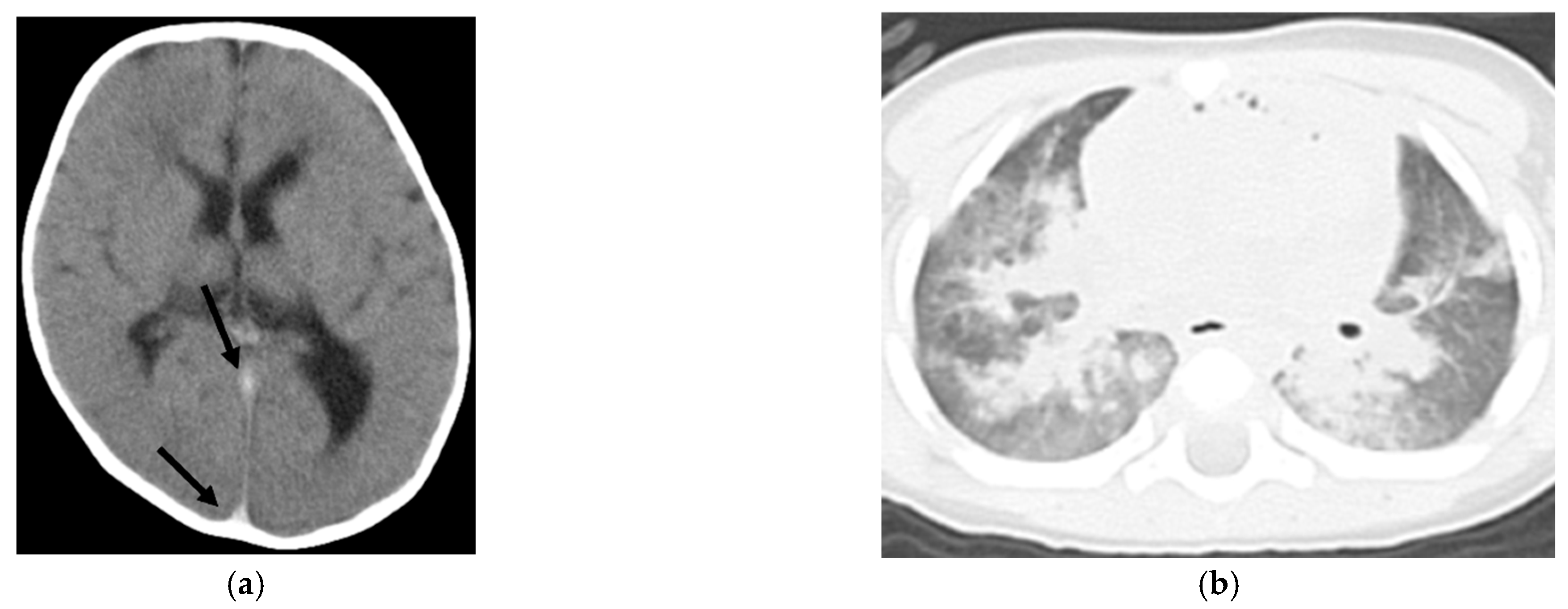
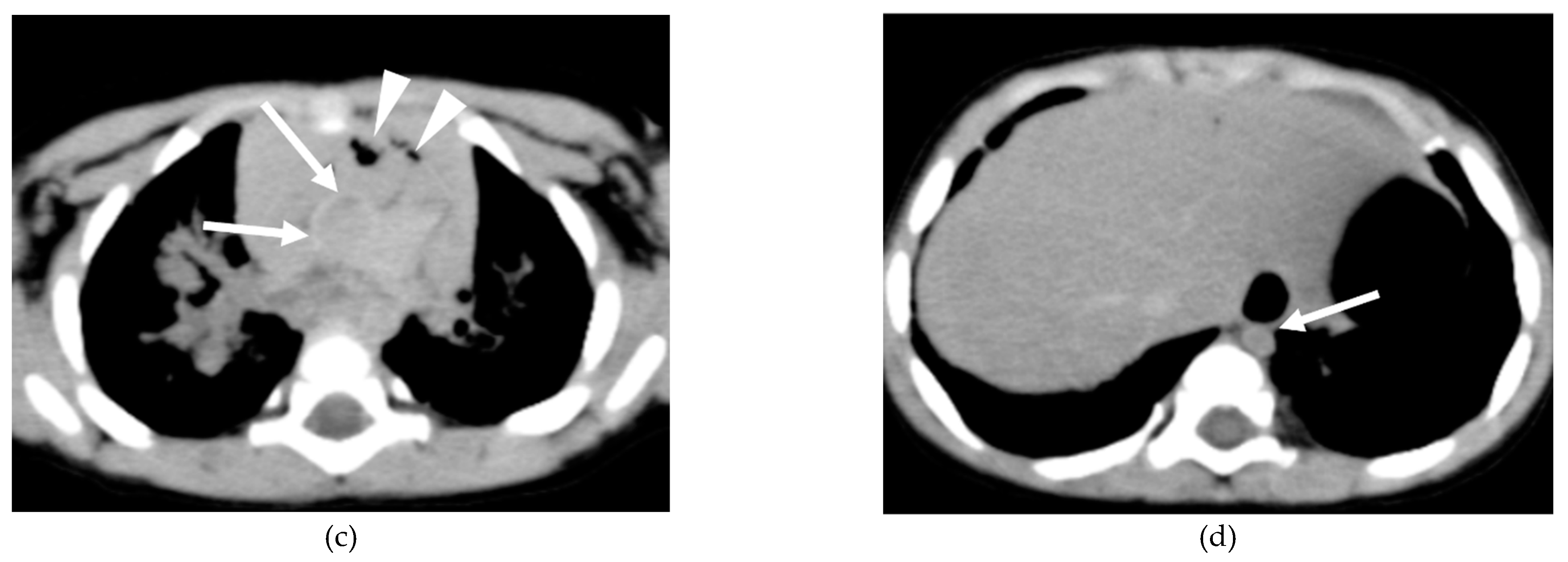
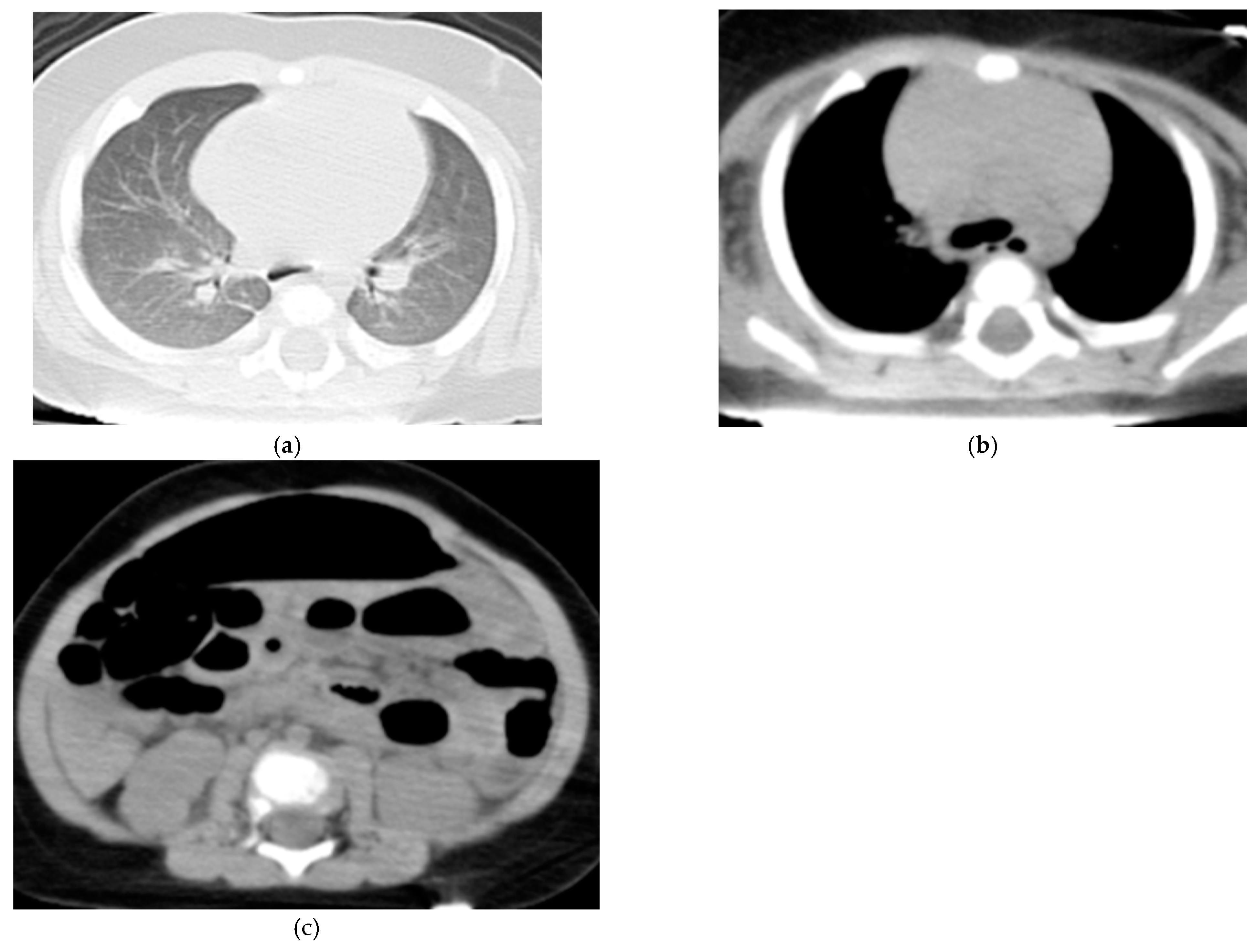
3.2. Evaluation of WBCT Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tokyo Households and Population (by town/village and age) by Basic Resident Ledger; Statistics Division, Bureau of General Affairs, Tokyo Metropolitan Government, 2024. Available online: https://www.toukei.metro.tokyo.lg.jp/juukiy/2024/jy24qf0001.pdf.
- Current status of emergency services 2022; Tokyo Fire Department, 2023. Available online: https://www.tfd.metro.tokyo.lg.jp/hp-kyuukanka/katudojitai/data/pdf/R2_2.pdf.
- Numaguchi, A.; Mizoguchi, F.; Aoki, Y.; An, B.; Ishikura, A.; Ichikawa, K.; Ito, Y.; Uchida, Y.; Umemoto, M.; Ogawa, Y.; et al. Epidemiology of child mortality and challenges in child death review in Japan: the Committee on Child Death Review: A Committee Report: The Committee on Child Death Review: a Committee Report. Pediatr Int 2022, 64, e15068. [CrossRef]
- Survey on the search for causes of pediatric out-of-hospital cardiac arrest (in Japanese); Japan Pediatric Association. Available online: https://www.jpeds.or.jp/uploads/files/20240729_ingai_hokoku.pdf.
- Adel, J.; Akin, M.; Garcheva, V.; Vogel-Claussen, J.; Bauersachs, J.; Napp, L.C.; Schäfer, A. Computed-tomography as first-line diagnostic procedure in patients with out-of-hospital cardiac arrest. Front Cardiovasc Med 2022, 9, 799446. [CrossRef]
- Chelly, J.; Mongardon, N.; Dumas, F.; Varenne, O.; Spaulding, C.; Vignaux, O.; Carli, P.; Charpentier, J.; Pène, F.; Chiche, J.D.; et al. Benefit of an early and systematic imaging procedure after cardiac arrest: insights from the PROCAT (Parisian RegionOut of Hospital Cardiac Arrest) registry. Resuscitation 2012, 83, 1444–1450. [CrossRef]
- Christ, M.; von Auenmueller, K.I.; Noelke, J.P.; Sasko, B.; Amirie, S.; Trappe, H.J. Early computed tomography in victims of non-traumatic out-of-hospital cardiac arrest. Intern Emerg Med 2016, 11, 237–243. [CrossRef]
- Viniol, S.; Thomas, R.P.; König, A.M.; Betz, S.; Mahnken, A.H. Early whole-body CT for treatment guidance in patients with return of spontaneous circulation after cardiac arrest. Emerg Radiol 2020, 27, 23–29. [CrossRef]
- Ishida, M.; Gonoi, W.; Okuma, H.; Shirota, G.; Shintani, Y.; Abe, H.; Takazawa, Y.; Fukayama, M.; Ohtomo, K. Common postmortem computed tomography findings following atraumatic death: differentiation between normal postmortem changes and pathologic lesions. Korean J Radiol 2015, 16, 798–809. [CrossRef]
- Ishida, M.; Gonoi, W.; Abe, H.; Ushiku, T.; Abe, O. Essence of postmortem computed tomography for in-hospital deaths: what clinical radiologists should know. Jpn J Radiol 2023, 41, 1039–1050. [CrossRef]
- Shiotani, S.; Kohno, M.; Ohashi, N.; Yamazaki, K.; Nakayama, H.; Ito, Y.; Kaga, K.; Ebashi, T.; Itai, Y. Hyperattenuating aortic wall on postmortem computed tomography (PMCT). Radiat Med 2002, 20, 201–206.
- Takahashi, N.; Higuchi, T.; Hirose, Y.; Yamanouchi, H.; Takatsuka, H.; Funayama, K. Changes in aortic shape and diameters after death: comparison of early postmortem computed tomography with antemortem computed tomography. Forensic Sci Int 2013, 225, 27–31. [CrossRef]
- Shirota, G.; Gonoi, W.; Ishida, M.; Okuma, H.; Shintani, Y.; Abe, H.; Takazawa, Y.; Ikemura, M.; Fukayama, M.; Ohtomo, K. Brain swelling and loss of gray and white matter differentiation in human postmortem cases by computed tomography. PLOS ONE 2015, 10, e0143848. [CrossRef]
- Shiotani, S.; Kohno, M.; Ohashi, N.; Atake, S.; Yamazaki, K.; Nakayama, H. Cardiovascular gas on non-traumatic postmortem computed tomography (PMCT): the influence of cardiopulmonary resuscitation. Radiat Med 2005, 23, 225–229.
- Ishida, M.; Gonoi, W.; Hagiwara, K.; Takazawa, Y.; Akahane, M.; Fukayama, M.; Ohtomo, K. Intravascular gas distribution in the upper abdomen of non-traumatic in-hospital death cases on postmortem computed tomography. Leg Med (Tokyo) 2011, 13, 174–179. [CrossRef]
- Yamaki, T.; Ando, S.; Ohta, K.; Kubota, T.; Kawasaki, K.; Hirama, M. CT demonstration of massive cerebral air embolism from pulmonary barotrauma due to cardiopulmonary resuscitation. J Comput Assist Tomogr 1989, 13, 313–315. [CrossRef]
- Barber, J.L.; Kiho, L.; Sebire, N.J.; Arthurs, O.J. Interpretation of intravascular gas on postmortem CT in children. J Forensic Radiol Imaging 2015, 3, 174–179. [CrossRef]
- Takahashi, N.; Satou, C.; Higuchi, T.; et al. Quantitative analysis of intracranial hypostasis: comparison of early postmortem and antemortem CT findings. AJR 2010, 195, 388–393.
- Gould, S.W.; Harty, M.P.; Givler, N.E.; Christensen, T.E.; Curtin, R.N.; Harcke, H.T. Pediatric postmortem computed tomography: initial experience at a Children’s Hospital in The United States. Pediatr Radiol 2019, 49, 1113–1129. [CrossRef]
- Krentz, B.V.; Alamo, L.; Grimm, J.; Dédouit, F.; Bruguier, C.; Chevallier, C.; Egger, C.; Da Silva, L.F.F.; Grabherr, S. Performance of post-mortem CT compared to autopsy in children. Int J Legal Med 2016, 130, 1089–1099. [CrossRef]
- Oyake, Y.; Aoki, T.; Shiotani, S.; Kohno, M.; Ohashi, N.; Akutsu, H.; Yamazaki, K. Postmortem computed tomography for detecting causes of sudden death in infants and children: retrospective review of cases. Radiat Med 2006, 24, 493–502. [CrossRef]
- van Rijn, R.R.; Beek, E.J.; van de Putte, E.M.; Teeuw, A.H.; Nikkels, P.G.J.; Duijst, W.L.J.M.; Nievelstein, R.A.; Dutch NODO Group. The value of postmortem computed tomography in paediatric natural cause of death: a Dutch observational study. Pediatr Radiol 2017, 47, 1514–1522. [CrossRef]
- Speelman, A.C.; Engel-Hills, P.C.; Martin, L.J.; van Rijn, R.R.; Offiah, A.C. Postmortem computed tomography plus forensic autopsy for determining the cause of death in child fatalities. Pediatr Radiol 2022, 52, 2620–2629. [CrossRef]
- Sieswerda-Hoogendoorn, T.; Soerdjbalie-Maikoe, V.; de Bakker, H.; van Rijn, R.R. Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 2014, 128, 957–965. [CrossRef]
- Proisy, M.; Marchand, A.J.; Loget, P.; Bouvet, R.; Roussey, M.; Pelé, F.; Rozel, C.; Treguier, C.; Darnault, P.; Bruneau, B. Whole-body post mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 2013, 23, 1711–1719. [CrossRef]
- Noda, Y.; Yoshimura, K.; Tsuji, S.; Ohashi, A.; Kawasaki, H.; Kaneko, K.; Ikeda, S.; Kurokawa, H.; Tanigawa, N. Postmortem computed tomography imaging in the investigation of nontraumatic death in infants and children. BioMed Res Int 2013, 2013, 327903. [CrossRef]
- Ishida, M.; Gonoi, W.; Shirota, G.; Abe, H.; Shintani-Domoto, Y.; Ikemura, M.; Ushiku, T.; Abe, O. Utility of unenhanced postmortem computed tomography for investigation of in-hospital nontraumatic death in children up to 3 years of age at a single Japanese tertiary care hospital. Med (Baltim) 2020, 99, e20130. [CrossRef]
- Garstang, J.; Griffiths, F.; Sidebotham, P. What do bereaved parents want from professionals after the sudden death of their child: a systematic review of the literature. BMC Pediatr 2014, 14, 269. [CrossRef]
| non-ROSC (n=19) | ROSC (n=8) | p (Mann–Whitney U test) | |
|---|---|---|---|
| Age (mean month, range) | 13.2 (1–108) | 14.3 (0.4–166) | 0.735 |
| Sex (m:f) | 10:9 | 4:4 | 0.938 |
| Past history (-:+) | 13:6 | 7:1 | 0.449 |
| Whether or not the home of the place of discovery (-:+) | 18:1 | 5:3 | 0.198 |
| Whether found after bedtime (-:+) | 18:1 | 1:7 | < .001 |
| Estimated time from the last sighting to discovery (mean minutes, range) | 254.8 (0–560) | 17.3 (0–115) | < .001 |
| Bystander CPR (+:-) | 7:12 | 3:5 | 0.979 |
| Number of positive cases | |||
| CT findings | non-ROSC (n=19) | ROSC (n=8) | p (Fisher’s exact test) |
| Head | |||
| Brain swelling | 16 | 1 | <0.001 |
| Loss of cerebral gray-white matter differentiation | 14 | 3 | 0.033 |
| Hyperdense intracranial venous sinus | 6 | 0 | 0.136 |
| Lung | |||
| Symmetrical consolidation/ground-glass opacity | 18 | 4 | 0.017 |
| Asymmetrical consolidation/ground-glass opacity | 2 | 2 | 0.558 |
| Mediastinum | |||
| Cardiomegaly | 16 | 2 | 0.006 |
| Pericardial effusion | 0 | 0 | n/a |
| Hyperdense aortic wall | 16 | 0 | <0.001 |
| Narrowed aorta | 19 | 0 | <0.001 |
| Gas in the cardiac cavity, aorta, and superior vena cava | 15 | 0 | <0.001 |
| Abdomen and pelvis | |||
| Hepatomegaly | 15 | 1 | 0.002 |
| Dilated inferior vena cava | 3 | 2 | 0.616 |
| Dilated gastrointestinal tract | 17 | 5 | 0.136 |
| Gas in the upper abdominal organs | 8 | 0 | 0.061 |
| Soft tissue | |||
| Subcutaneous fatty edema | 0 | 0 | n/a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





