Submitted:
09 September 2024
Posted:
10 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Obarski, P.; Włodarczyk, J. Diagnosis and Management of Gastrointestinal Chemical Burns and Post-Burn Oesophageal Stenosis. Kardiochir Torakochirurgia Pol 2021, 18, 252–259. [Google Scholar] [CrossRef]
- Arnold; Marion; Alp Numanoglu. Caustic Ingestion in Children—a Review. Seminars in Pediatric Surgery 2017, 26, 95–104. [Google Scholar] [CrossRef]
- Sari; Desi Rahmah; Ismi Dian Meiliana; Sakti, D. ; Kinasih, S.; Kurniasari, H.; Rejeki, P.S. Hyperbaric Oxygen Therapy as an Adjuvant Treatment in Hydrochloric Acid Poisoning: A Literature Review. Biomorphology J. 2023, 33, 52–58. [Google Scholar]
- Schröder, W.; Brunner, S.; Bruns, C.J. Caustic Ingestion of the Upper Gastrointestinal Tract. Chirurg 2022, 93, 202–203. [Google Scholar] [CrossRef]
- Oliva, S.; Romano, C.; De Angelis, P.; Isoldi, S.; Mantegazza, C.; Felici, E.; Dabizzi, E.; Fava, G.; Renzo, S.; Strisciuglio, C.; et al. Foreign body and caustic ingestions in children: A clinical practice guideline. Dig. Liver Dis. 2020, 52, 1266–1281. [Google Scholar] [CrossRef]
- Dilawari, J.B.; Singh, S.; Rao, P.N.; Anand, B.S. Corrosive acid ingestion in man - a clinical and endoscopic study. Gut 1984, 25, 183–187. [Google Scholar] [CrossRef]
- Gill, M.; Tee, D.; Chinnaratha, M.A. Caustic Ingestion: Has the Role of the Gastroenterologist Burnt Out? Emerg Med Australas 2019, 31, 479–482. [Google Scholar] [CrossRef]
- Agarwal, A.; Srivastava, D.N.; Madhusudhan, K.S. Corrosive injury of the upper gastrointestinal tract: the evolving role of a radiologist. Br. J. Radiol. 2020, 93. [Google Scholar] [CrossRef]
- Kaewlai, R.; Noppakunsomboon, N.; Tongsai, S.; Tamrakar, B.; Kumthong, N.; Teerasamit, W.; Kongkaewpaisan, N.; Pisanuwongse, A.; Amornsitthiwat, R.; Maitriwong, W.; et al. Performance of computed tomography and its reliability for the diagnosis of transmural gastrointestional necrosis in a setting of acute ingestion of predominantly strong acid substances in adults. Clin. Toxicol. 2023, 61, 346–354. [Google Scholar] [CrossRef]
- Cutaia, G.; Messina, M.; Rubino, S.; Reitano, E.; Salvaggio, L.; Costanza, I.; Agnello, F.; La Grutta, L.; Midiri, M.; Salvaggio, G.; et al. Caustic ingestion: CT findings of esophageal injuries and thoracic complications. Emerg. Radiol. 2021, 28, 845–856. [Google Scholar] [CrossRef]
- Saito, K.; Goto, F.; Sekine, M.; Yamamoto, H.; Kaneda, S.; Sakai, A.; Ebisumoto, K.; Maki, D.; Iijima, H.; Yamauchi, M.; et al. Computed Tomography to Diagnose Paranasal Sinus Chemical Burns and Tissue Damage: A Case Report. Laryngoscope 2021, 131, E2490–E2493. [Google Scholar] [CrossRef]
- Gupta, V.; Shah, J.; Yadav, T.D.; Kumar, P.; Wig, J.D.; Kochhar, R. Emergency surgical intervention in acute corrosive ingestion: single-center experience from India. ANZ J. Surg. 2023, 93, 2864–2869. [Google Scholar] [CrossRef]
- Rasbach, E.; Schölch, S.; Reissfelder, C.; Rahbari, N.N. Successful treatment of gastric necrosis after ingestion of hydrochloric acid: a two-stage minimally invasive surgical procedure. BMJ Case Rep. 2019, 12, e231879. [Google Scholar] [CrossRef]
- Wijeratne, T.; Ratnatunga, C.; Dharrmapala, A.; Samarasinghe, T.; University of Sri Jayewardenepura; LK About T Department of Surgery; Faculty of Medical Sciences X close T Wijeratne; Peradeniya, T. H.; Ratnatunga, L.A.T.S.U.X.C.C.; LK About C Department of Surgery; et al. Corrosive acid injury of the stomach. Ceylon Med J. 2015, 60, 25. [Google Scholar] [CrossRef]
- Frank, D.B.; Fumanti, B.J.; Grossman, M.D.; Mendez, A. Suicidal ingestion of household bleach resulting in total gastrectomy. Clin. Toxicol. 2019, 58, 300–301. [Google Scholar] [CrossRef]
- Ushio, M. A case of early gastric necrosis due to ingestion of an acidic toilet cleaner. Clin. Case Rep. 2023, 11, e7481. [Google Scholar] [CrossRef]
- Furlano, E.R.; Wu, G.P.; Vosburgh, B.; Waldman, C.R.; Noonan, J.; Bracey, A. Man Presenting After Hydrochloric Acid Ingestion. Clin. Pr. Cases Emerg. Med. 2023, 8, 77–79. [Google Scholar] [CrossRef]
- Kumar, C.B.; Chowdhury, S.D.; Ghatak, S.K.; Sreekar, D.; Kurien, R.T.; David, D.; Dutta, A.K.; Simon, E.G.; Joseph, A.J. Immediate and long-term outcome of corrosive ingestion. Indian J. Gastroenterol. 2019, 38, 356–361. [Google Scholar] [CrossRef]
- Chirica, M.; Bonavina, L.; Kelly, M.D.; Sarfati, E.; Cattan, P. Caustic Ingestion. Lancet 2017, 389, 2041–2052. [Google Scholar] [CrossRef]
- Hoffman, R.S.; Burns, M.M.; Gosselin, S. Ingestion of Caustic Substances. New Engl. J. Med. 2020, 382, 1739–1748. [Google Scholar] [CrossRef]
- Singh, H.; Dhibar, D.P.; Naidu, G.S.R.S.N.K. Life-threatening corrosive injury with hepato-renal-pulmonary failure in boric acid poisoning. Postgrad. Med J. 2020, 98, 70–71. [Google Scholar] [CrossRef]
- Picciariello, A.; Papagni, V.; Martines, G.; Palasciano, N.; Altomare, D. The management of esophago-gastric necrosis due to caustics ingestion: Anastomotic reinforcement with Cyanoacrylate glue and damage control with Vacuum Assisted Closure Therapy—A case report. Int. J. Surg. Case Rep. 2019, 60, 327–330. [Google Scholar] [CrossRef]
- Huscher, C.G.; Mingoli, A.; Mereu, A.; Sgarzini, G. Laparoscopy can be Very Effective in Reducing Mortality Rate for Caustic Ingestion in Suicide Attempt. World J. Surg. 2011, 35, 2363–2364. [Google Scholar] [CrossRef]
- Yeh, I.J.; Liu, K.T. St Segment Elevation Associated with Hydrochloric Acid Ingestion: A Case Report. Medicine (Baltimore) 2017, 96, e8819. [Google Scholar] [CrossRef]
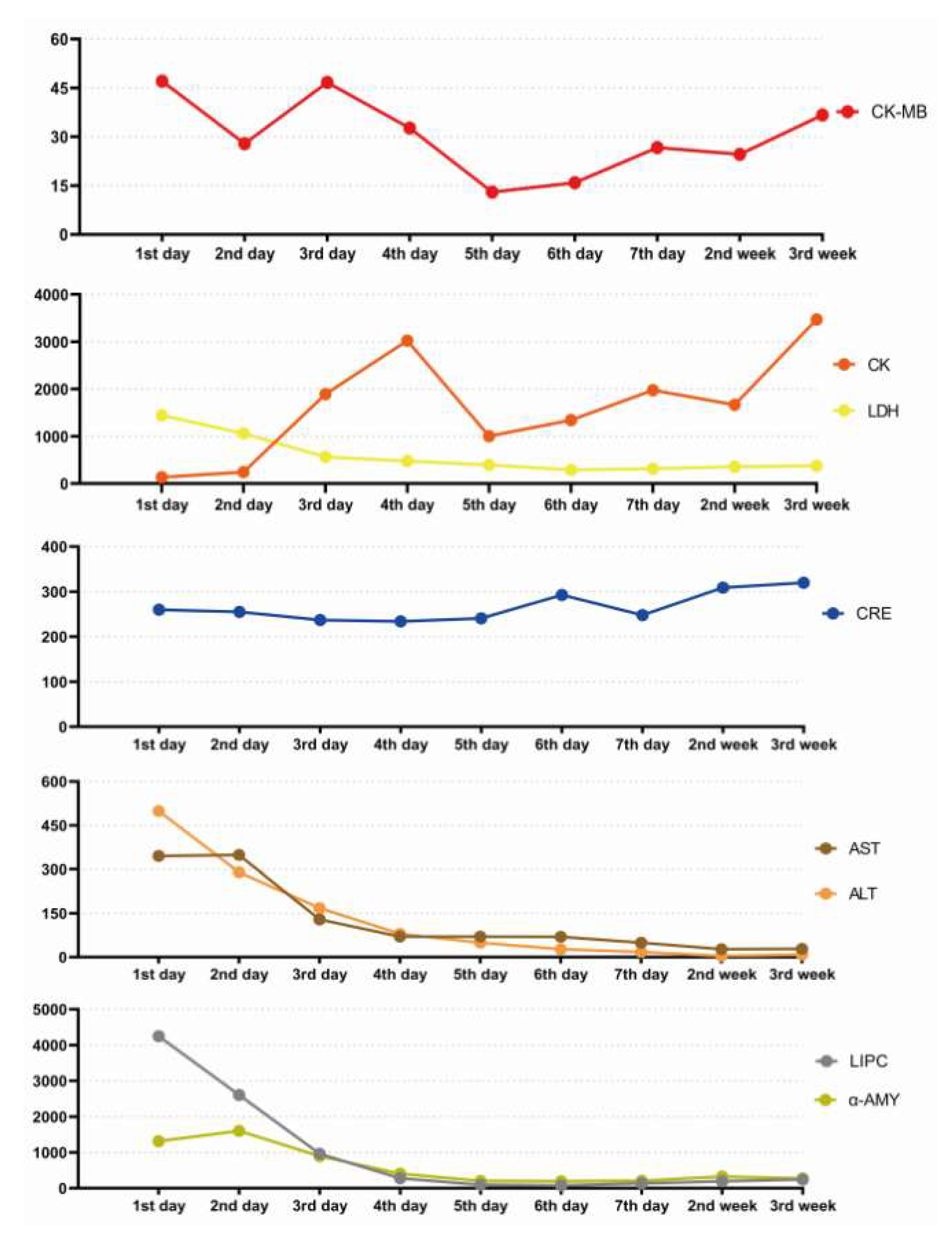
| Index | Normal range | 1st day | 2nd day | 3rd day | 4th day | 5th day | 6th day | 7th day | 2nd week | 3rd week |
|---|---|---|---|---|---|---|---|---|---|---|
| WBC | 5-12×109 | 24.69 | 10.22 | 7.77 | 6.17 | 6.20 | 10.1 | 13.61 | 12.5 | 27.86 |
| NEUT% | 40-75% | 90.6 | 87.3 | 85.8 | 89.3 | 81.1 | 88.9 | 90.2 | 84.6 | 77.2 |
| HGB | 105-145g/L | 143 | 118 | 101 | 75 | 65 | 64 | 65 | 52 | 20 |
| PLT | 140-440×109/L | 126 | 119 | 70 | 47 | 47 | 76 | 129 | 232 | 96 |
| CRE | 35-73μmol/L | 260 | 255 | 237 | 234 | 241 | 293 | 248 | 309 | 320 |
| CRP | 0-6mg/L | 61.45 | 220.80 | 330.36 | 383.12 | 361 | 193.03 | 139.82 | 218.3 | 255.09 |
| CK | 40-310u/L | 133 | 243 | 1894 | 3023 | 1004 | 1342 | 1975 | 1667 | 3472 |
| CK-MB | 0-25u/L | 47.1 | 27.9 | 46.7 | 32.7 | 13.0 | 15.9 | 26.7 | 24.6 | 36.7 |
| LDH | 120-250u/L | 1445 | 1062 | 563 | 476 | 393 | 290 | 313 | 355 | 374 |
| AST | 7-40u/L | 345.2 | 349.0 | 129.3 | 70.1 | 70.6 | 69.8 | 49.5 | 27.3 | 28.3 |
| ALT | 7-40u/L | 499.1 | 290.1 | 168 | 80.2 | 49.2 | 27.2 | 17.8 | 4.3 | 8.7 |
| LIPC | 1-63U/L | 4250.0 | 2608.2 | 961.6 | 280.1 | 94.7 | 78.9 | 135.3 | 194.6 | 245.5 |
| α-AMY | 20-90u/L | 1315.0 | 1604.1 | 898.2 | 409.1 | 206.1 | 195.4 | 208.9 | 328.2 | 273.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





