1. Introduction
Post COVID-19 syndrome, or Long Covid (LC) is defined as the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting at least 2 months with no other explanation [
1]. It is estimated that there are approximately 1.9 million people in England experiencing symptoms following COVID-19 in the UK, with 1.1 million experiencing these symptoms for over 12 months and 762,00 (41%) at least 2 years previously (persistent LC) [
2].
Patients experience debilitating and wide ranging symptoms across multiple organ systems [
3,
4], with symptoms such as fatigue, ‘brain fog’, pain, and shortness of breath being reported for months after infection [
5]. Disability rates are high within this population with >20% of people reporting their symptoms limited their ability to perform their normal activities ‘a lot’ [
2]. Symptom burden and disability in Long Covid have been found to be worse than that reported in the literature for Diabetes Mellitus, COPD, Heart Failure and Multiple Sclerosis [
6].
The prevalence of self-reported Long Covid in the UK is greatest amongst people aged 35-69 [
2], many reporting the symptoms having an impact on their ability to work and remain in employment. In a survey by the Trade Union Congress in March 2023 one in seven respondents (14 per cent) had lost their job because of reasons connected to Long COVID [
7] and one in four employers now include Long COVID among their main causes of long-term sickness absence [
8].
With symptoms lasting for years [
5,
6,
9] there is emerging evidence that LC should now be considered for some patients as a Long Term Condition (LTC). One UK evaluation showed no improvement in EQ-5D-5L at 6 month follow up, and concluded that for most patients in this evaluation, LC had evidently become a long-term condition, causing disability and significant deterioration of their overall health status even 18 months post infection [
6]. Persistent symptoms have been found in 38% of non-hospitalised patients as long as 23 months after onset [
10], with fatigue, breathlessness, difficulty concentrating, memory problems and pain being the most common reported symptoms [
5,
11,
12,
13,
14]
Significant fluctuations in symptoms have been demonstrated by assessing the same patients at different time points in their journey [
15], with up to 93% of patients reporting symptoms fluctuating over time [
7]. Symptoms of fatigue and breathlessness were found to increase in one group of patients from 5 months after LC onset to 12 months [
11], with other symptoms such as hair loss decreasing. This relapsing nature of LC has been further observed with symptoms increasing at 30 days post onset, decreasing at 60 days and then increasing again after 90 days [
16]. Suggesting that the unknown trajectory of this condition may be difficult to predict and that patients may need to access services as and when their symptoms deteriorate.
The Leeds Long Covid Community Rehabilitation Service (LLCRS) was developed in response to NHS England’s commissioning guidance (2023) for a broad based multi-disciplinary team to provide holistic, symptom-led rehabilitation for those whose symptoms were having a significant impact on their daily activities and particularly, with the largest number coming from people of working age to support them to remain in work or return to work in a vocational rehabilitation programme. The multidisciplinary team in Leeds consists of Occupational therapists, Physiotherapists, Dietitians, Psychology professionals, rehabilitation assistants, a GP with a special interest and consultants in specialities in rehabilitation medicine, respiratory medicine and cardiology [
17].
The debilitating nature of LC with its effects on so many organ systems and its fluctuating and protracted nature in some, is well known. We, however, lack knowledge of the long-term health effects of this novel condition. We wanted to know whether those being discharged from our service fully recover to their pre-COVID status or whether they continue to have lingering symptoms. The aim of this study was to evaluate the long-term health outcomes in a sample of patients discharged from the service. We wanted to know the status of their LC symptoms, whether they are accessing any other services, what support they continue to require and how has LC impacted on their ability to live, work and interact within society.
2. Materials and Methods
This service evaluation study was approved locally by the service lead, Leeds Community Healthcare NHS Trust. The Health Authority (HRA) toolkit was completed and confirmed as not needing any further ethical approvals to undertake this service evaluation. A standard follow-up questionnaire with usual service Patient Reported Outcome Measures (PROMs) were sent to patients who had been discharged from the service and had consented to be contacted for service evaluation purposes.
Participant Identification
Participants were identified by using an electronic patient record database for all patients who had been managed for LC in the LLCRS and discharged for more than 3 months. Inclusion criteria for the service evaluation were: confirmed diagnosis of LC (as per NICE guidelines)[
1], consented to service evaluation and research, initial EQ-5D-5L completed and documented in record and evidence of ‘engagement’ with the service. ‘Engagement’ was set as a minimum of at least one consultation with a therapist documented on their clinical record. This criteria was applied to the list of discharged patients and postal questionnaires sent, along with information about the service evaluation study. Participation was voluntary and participants were free to withdraw at any point without having to give a reason for withdrawal. Deceased patients and those without adequate information were excluded from the study.
The questionnaires included were the standard PROMs used in the service, i.e., Modified C19-YRS, EQ-5D-5L, ME/CFS screening and a qualitative questionnaire to capture the patient’s perception of their health state. These were agreed by the LLCRS Patient Carer and Public Involvement (PCPI) group.
Patient Reported Outcome Measures (PROMs)
C19-YRS
The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) was literature’s first condition specific PROM developed to measure the symptoms, functioning and disability associated with COVID-19. C19-YRSm is a modified version of the original C19-YRS with 17 items and four sub-scales. Each item has a 4-point response category: 0, no problem to 3, severe problem [
18] . The subscales (range) are: Symptom Severity (0-30), Functional Disability (0-15), Other Symptoms (0-25), and Overall Health (0-10). The evaluation of psychometric properties of C19-YRSm revealed it is a valid, reliable and responsive measure [
19]. The Minimal Clinical Important Difference (MCID) has been estimated to be 4 points for the Symptom Severity subscale and 4 points for the Functional Disability subscales.
EQ-5D-5L
The EuroQol EQ-5D-5L is a health-related quality of life measure with five domains: Mobility, Usual Activities, Selfcare, Pain / Discomfort, and Anxiety / Depression. Each item has five response categories ranging from 1 (no problems) to 5 (severe problems). Responses to each item are collated into a profile score which is converted into a health utility or index score using a country-specific algorithm (tariff or value set). The utility score reflects societal preference for health state and is measured on a metric from 0 (dead) to 1 (perfect health). The EQ-5D-5L scores are mapped onto the EQ-5D-3L (an alternative version of the instrument with 3 response categories advocated by the National Institute for Health and Care Excellence, NICE) using a standard mapping crosswalk algorithm to derive UK utility values [
20].
3. Results
A total of 2124 patients had been discharged from LLCRS since its opening in September 2021. The inclusion criteria for this service evaluation study were met by 460 patients who were sent the agreed questionnaires. Completed questionnaires were returned by 118 patients. Six participants did not re-confirm their consent for the study and hence a final dataset of 112 participants were included in the analysis. Demographics for the participants are shown in
Table 1.
Participants had LC for an average of 37.6 months and were 9.7 months post-discharge from LLCRS. There were a greater number of females in the sample (62%), predominantly white (75%) and an average age of 58.5 years.
The average C19-YRSm and EQ-5D-5L scores at the different time points are shown in
Table 2.
Of the 112 respondents, only 11 participants reported that they had returned to pre-COVID-19 health (9.8%) with 90.2% of participants continuing to experience symptoms of LC (
Table 3). However, 64.2% of these participants reported their symptoms are the same or have improved since discharge from LLCRS. Almost equal numbers of participants were in employment at follow up, with no changes to their role since their COVID-19 illness (45%) and those who had had some sort of change to their job or role experienced (43%), the largest group of which is 20% of participants who either had to retire or change their job.
There was a total of 52 new referrals to NHS services reported after discharge from LLCRS reported by participants excluding visits to General Practitioners.
Table 4.
Other health services accessed since discharge from LLCRS.
Table 4.
Other health services accessed since discharge from LLCRS.
| |
Number of patients
(n=112) |
% |
| Participants accessing any other health service since discharge |
48 |
43 |
Participants with at least 1 NHS referral for LC management since discharge
(excluding GP)
|
31 |
28 |
| 1 NHS referral since dc |
16 |
14.2 |
| 2 NHS referrals since dc |
13 |
12 |
| 4 NHS referrals since dc |
1 |
0.9 |
| 6 NHS referrals since dc |
1 |
0.9 |
The private and NHS services accessed by participants after Discharge from LLCRS include GP, physiotherapy, psychology, pain management, exercise class, neurology, respiratory, rheumatology, hearing services, reflexology, massage therapist, cardiology, gastroenterology, ENT, dietitian, orthopaedics, meditation, yoga, hypnotherapy, Nuffield Long Covid programme, personal trainer, peer support group, CUCs, shared harmonies (online singing course for breathing control), haematology, hospital admission, access to work, endocrinology, asthma nurse, hepatology, chiropractor and acupuncture.
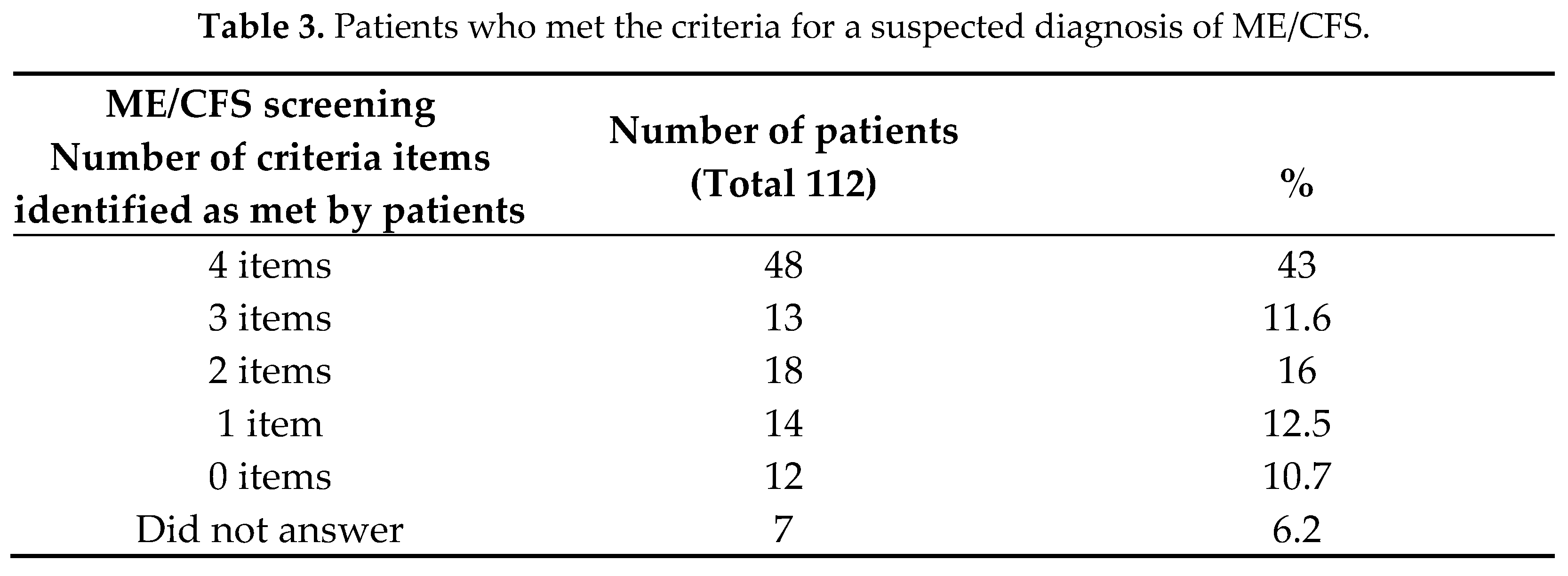
A total of 48 patients (43% of the sample) met the NICE diagnostic criteria for suspected ME/CFS.
4. Discussion
The principal findings of this service evaluation study are that 90.2% patients who have been discharged from the LLCRS are still exhibiting significant symptom burden and functional disability from LC (at 3 years post-infection) and have not recovered to their pre-COVID heath state. A very small proportion of patients who have engaged with the LLCRS made a full recovery to their previous heath state prior to COVID-19 infection (9.8%). The mean EQ-5D-5L index value at post discharge follow up was 0.53, which is comparable to the mean EQ-5D-5L Index scores of several other LTCs such as COPD, Heart Failure and Multiple Sclerosis (see Table 9).
We believe that this is one of the first studies to measure outcomes of LC patients at different time points along their journey after being referred to a specialist Long Covid Clinic, specifically at discharge and 3-years post discharge. One study reported mean EQ-5D-5L Index scores of 0.54 in patients referred to an NHS community Long Covid clinic at assessment [
13]. Our mean EQ-5D-5L index score of 0.52 at entry to the service compares well to these findings suggesting a similar population, however we are unable to make comparisons in terms of improvement whilst in the service as no other study has assessed outcomes at discharge or beyond. Other studies amongst the general population self-reporting LC have found average EQ-5D-5L Index scores of 0.49 [
14] and 0.75 [
22] but these may include a range of respondents and will not be made up entirely of patients referred for rehabilitation.
There is a general trend in the literature of reported recovery from LC within the general population over time [12 ,23], one study reported only 6% of patients with mild to moderate COVID-19 still having symptoms at 24 months [
5] whilst another found 17.2% had not fully recovered at 24 months [
24]. Furthermore, another study reported that average EQ-5D-5L Index scores recovered (mean 0.84) to pre-covid levels (mean 0.82) amongst a group of 300 non-hospitalised patients, some with self reported LC, over a 2 year period [
25]. This is a very different picture to our findings of 90.2% reporting not fully recovering, amongst a population of patients who have received specialist rehabilitation however our sample will likely be biased towards those with persistent symptoms and thus overrepresented, but representing a specific group of patients for whom this is likely to be a long-term condition.
Findings in this study add weight to this emerging picture of Persistent LC (PLC) as a long-term condition with clear evidence that even after being treated in a specialist LC service the majority of patients continue to face overwhelming and debilitating symptoms for as long as 3 years.
Table 9.
Comparison of EQ5D-5L Index Scores in this population with LC and other chronic long-term conditions.
Table 9.
Comparison of EQ5D-5L Index Scores in this population with LC and other chronic long-term conditions.
| Condition |
EQ-5D Index (SD) |
| Healthy population |
0.92 (0.17) |
| COPD |
0.68 (0.24) |
| Heart Failure |
0.60 (0.25) |
| Multiple Sclerosis |
0.59 (0.29) |
| Long Covid (this service evaluation study) |
0.53 (0.29) |
PROMs assessed during participants time with LLCRS all show improvements from initial assessment to the point of discharge. Using a MCID of 4 [
19], symptom severity improves significantly from a mean of 18.4 at initial assessment to 13 at discharge. Mean Functional Disability scores decrease during a participant’s time within the LLCRS from 6.7 to 5.9 but this does not reach clinical significance. Overall health scores also improve from a mean of 4.9 to 6 at discharge but this does not quite return to the pre-covid average of 7.3.
EQ-5D-5L Index scores improved indicating a significant change in quality of life from entering the service (0.52) to discharge (0.65) by a mean EQ-5D-5L Index score of 0.13, which is above the smallest clinically meaningful change of 0.08 [
31]. Furthermore, there was a clinically significant improvement in EQ-5D-5L VAS mean score of 13.1 (MCID value 7.5 [
32]) between initial assessment and discharge from the service. This demonstrates that targeted interventions used within the LLCRS were effective in reducing symptom burden and improving the functional levels of individuals who engaged with clinicians. However, with a mean EQ-5D-5L Index value of 0.65 at discharge is still well below that of the healthy population at 0.92. This suggests the service is getting patients to a level of self-management and stability in the condition rather than full recovery. This also reflects on the nature of this novel condition.
Outcomes are seen to deteriorate after discharge in both the EQ-5D-5L and the C19-YRSm with average symptom severity increasing significantly from 13 to 15.1 after discharge [
19]. Average EQ-5D-5L index scores after discharge drop below initial EQ-5D-5L index scores by 0.12 representing a significant deterioration in functional levels. Furthermore EQ-5D-5L VAS scores deteriorate between discharge and follow up, reducing by 7.3, but not quite making the clinical significance of 7.5 from 65 to 57.7, indicating that participants are experiencing a substantial drop in functional ability once they have been discharged. This highlights the value of the service in stabilising the long-term condition and the need for the service to continue to provide regular input to avoid any such deterioration in health state. This is also reflected in the fact that there were significant referrals to other services after discharge to manage the flare ups of LC which we know is a fluctuating condition.
The employment status in this cohort was adversely affected in 43% patients. Other national studies have reported that this change can be as much as 62% [
6] and indeed findings from local data show that in 75% of patients at entrance to the LLCRS there has been a negative change to their working situation. It may be that as we follow participants further down the line some who were off sick in the initial weeks and months of their diagnosis have been able to return to work and indeed some who had their hours temporarily reduced were able to return to their usual hours with the support and guidance from the specialists within LLCRS. This highlights the crucial role that specialist services for Long Covid play in Vocational Rehabilitation and supporting with reasonable adjustments within the workplace to keep as many people and support people back into roles as possible.
The magnitude of the symptom burden experienced by participants at follow up is clearly illustrated in the very low symptom burden and Functional Disability score at pre-covid assessment compared to an average symptom severity of 15 at follow up and with 40% reporting more than 3 other significant health problems. Fit and well individuals have now developed further health conditions as a result of their ongoing LC symptoms. This reiterates a new-onset long-term condition of LC in most of these individuals with a significant burden to the healthcare system (as evidenced by healthcare services referrals they have had since discharge) and economy.
As many as 43% of participants with ongoing Long Covid symptoms continue to experience symptoms which may fit with a suspected ME/CFS diagnosis and would warrant further assessment, reporting significant ongoing symptoms for more than 3 months of debilitating fatigue, post exertional malaise, unrefreshed sleep and cognitive difficulties as described by NICE (2021) [
21]. This is generally in keeping with the high prevalence of ME/CFS within Long Covid populations in the literature with studies reporting 45.2% - 58% of LC patients fitting this criteria [
33,
34].
The NICE guidelines criteria for ME/CFS (2021) [
21] were used in this study however we found the wording of the first question confusing and unclear to participants and it was discovered that although many participants had fatigue scored on other PROMs they had not selected the first item on debilitating fatigue in the NICE ME/CFS criteria. Whilst recent studies have used the IOM or the CCC criteria to identify the prevalence of ME/CFS in those with Long Covid, we used the UK NICE Guidelines criteria as these are more widely used within our local services [
35,
36]. We were also mindful of the time taken to complete additional long questionnaire particularly in this population with fatigue and cognitive difficulties as their most frequent challenges.
5. Conclusions
With a recent move towards reduction of specialist Long Covid services with clinicians who have developed expertise in managing Long Covid, this study highlights the huge gap between unmet need and resources being planned for this patient group. These patients need holistic multidisciplinary care including optimising medical management, therapy input, Vocational Rehabilitation and long-term continuous input given the Long Term Condition (LTC) nature of the condition. Otherwise, it is likely these patients will then present to services where there is little understanding of the complexities of LC and any experience of how to provide appropriate support and rehabilitation, leading to further decline in functional status, increased health needs and further burden on the NHS along with greater dependence on social care or productivity loss.
This study has several limitations
. As this is a self-selected sample (24% response rate), it is likely that those patients who are still struggling with PLC have responded. However, this is similar to all questionnaire surveys and does highlight that there is a proportion of patients who have been worse since discharge and essentially have developed a LTC. The actual proportion of LC patients who end up with an LTC needs further prospective research. Studies such as LOCOMOTION are ideally placed to undertake such work on larger datasets [
37]. Using the NICE criteria for ME/CFS was a limitation as discussed above and adding few other criteria such as Institute of Medicine (IOM) or Centre for Disease Control and Prevention (CDC) would have added value to understanding the overlap between the conditions. This area needs further prospective research as it determines how the services for these conditions could consider integration (combined services) to provide a robust clinical and research active service that moves this area of medicine forward.
Author Contributions
R.B., J.G., B.G., S.W., J.S., R.T. and M.S contributed towards conceptualization, methodology, investigation, writing, review and editing, M.S.; supervision, R.B and H.T. retrieved and formulated the data, R.B. formal analysis, data curation and original draft preparation. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The NHS HRA tool was completed. NHS Ethical review and approval were not required for this service evaluation. Approval was granted locally by the Service Lead, Leeds Community Healthcare Trust.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the service evaluation.
Data Availability Statement
Anonymised data can be obtained by contacting the corresponding author.
Acknowledgments
The authors would like to acknowledge assistance received from the LLCRS administrative team, specifically Iqra Iqbal who supported this service evaluation significantly.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef] [PubMed]
- Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK – Office for National Statistics. Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/30march2023 (Accessed 9 April 2024).
- Davis, H.E.; Assaf, G.S.; Mccorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. Eclinicalmedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Robineau, O.; Zins, M.; Touvier, M.; Wiernik, E.; Lemogne, C.; De Lamballerie, X.; Blanché, H.; Deleuze, J.; Villarroel, P.; Dorival, C.; Nicol, J.; Gomes-Rima, R.; Correia, E.; Coeuret-Pellicer, M.; Druesne-Pecollo, N.; Esseddik, Y.; Ribet, C.; Goldberg, M.; Severi, G.; Carrat, F. Long-lasting Symptoms After an Acute COVID-19 Infection and Factors Associated With Their Resolution. JAMA Netw. Open. 2022, 5, 11. [Google Scholar] [CrossRef]
- Demko, Z.O.; Yu, T.; Mullapudi, S.K.; Varela Heslin, M.G.; Dorsey, C.A.; Payton, C.B.; Blair, P.W.; Mehta, S.H.; Thomas, D.L.; Manabe, Y.C.; Antar, A.A.R. Two-Year Longitudinal Study Reveals That Long COVID Symptoms Peak and Quality of Life Nadirs at 6–12 Months Postinfection. Open Forum Infect.Dis 2024, 11, 1–8. [Google Scholar] [CrossRef]
- Sivan, M.; Greenwood, D.; Smith, A.; Rocha Lawrence, R.; Osborne, T.; Goodwin, M. A national evaluation of outcomes in Long COVID services using digital PROM data from the ELAROS platform. LOCOMOTION and ELAROS, Published by NHS England, 2023. Available online: https://locomotion.leeds.ac.uk/wp-content/uploads/sites/74/2023/10/National-Evaluation-of-LC-Service-Outcomes-using-ELAROS-Data-09-10-23.pdf.
- Joint report by TUC and Long Covid Support, March 2023. Available online: https://www.tuc.org.uk/research-analysis/reports/workers-experience-long-covid (accessed on 23rd April 2024).
- CIPD Report: Health and wellbeing at work. Available online: https://www.cipd.org/uk/knowledge/reports/health-well-being-work (accessed on 23rd April 2024).
- Demko, Z.O.; Yu, T.; Mullapudi, S.K.; Heslin, M.G.V.; Dorsey, C.A.; Payton, C.B.; Tornheim, J. A.; Blair, P. W.; Mehta, S. H.; Thomas, D. L.; Manabe, Y. C.; Antar, A. A. R. Post-acute sequelae of SARS-CoV-2 (PASC) impact quality of life at 6, 12 and 18 months post-infection. medRxiv 2022, Aug 9. [CrossRef]
- Helmsdal, G.; Hanusson, K.D.; Kristiansen, M.F.; Foldbo, B.M.; Danielsen, M.E; Steig, B.Á.; Gaini, S.; Strom, M.; Weihe, P.; Petersen, M.S. Long COVID in the Long Run—23-Month Follow-up Study of Persistent Symptoms. Open Forum Infect. Dis. 2024, 9. [Google Scholar] [CrossRef] [PubMed]
- Seeßle, J.; Waterboer, T.; Hippchen, T.; Simon, J.; Kirchner, M.; Lim, A.; Merle, U. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin. Infect. Dis. 2021; 74, 1191–1198. [Google Scholar] [CrossRef]
- Cai, M.; Xie, Y.; Topol, E.J.; Al-Aly, Z. Three-year outcomes of post-acute sequelae of COVID-19. Nat. Med. 2024, 30, 1564–1573. [Google Scholar] [CrossRef]
- Walker, S.; Goodfellow, H.; Pookarnjanamorakot, P.; Murray, E.; Bindman, J.; Blandford, A.; Bradbury, K.; Cooper, B.; Hamilton, F.; Hurst, J.R.; Hylton, H.; Linke, S.; Pfeffer, P.; Ricketts, W.; Robson, C.; Stevenson, F.A.; Sunkersing, D.; Wang, J.; Gomes, M.; Henley, W. Impact of fatigue as the primary determinant of functional limitations among patients with post-COVID-19 syndrome: a cross-sectional observational study. BMJ Open 2023, 13, e069217. [Google Scholar] [CrossRef] [PubMed]
- Carlile, O.; Briggs, A.; Henderson, A.D.; Butler-Cole, B.F.C.; Tazare, J.; Tomlinson, L.A.; Marks, M.; Jit, M.; Lin, L-Y.; Bates, C.; Parry, J.; Bacon, S.C.J.; Dillingham, I.; Dennison, W.; Costello, R.E.; Walker, A.J.; Hulme, W.; Goldacre, B.; Mehrkar, A.; Mackenna, B. Impact of long COVID on health-related quality-of-life: an OpenSAFELY population cohort study using patient-reported outcome measures (OpenPROMPT). Lancet 2024, 40, 100908. [CrossRef]
- Huang, L.; Li, X.; Gu, X.; Zhang, H.; Ren, L.; Guo, L.; Liu, M.; Wang, Y.; Cui, D.; Wang, Y.; Zhang, X.; Shang, L.; Zhong, J.; Wang, X.; Wang, J.; Cao, B. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir. Med. 2022; 10, 863–876. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Florencio, L.L.; Cuadrado, M.L.; Plaza-Manzano, G.; Navarro-Santanna, M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur. J. Int. Med. 2021, 92, 55–70. [Google Scholar] [CrossRef]
- Parkin, A.; Davison, J.; Tarrant, R.; Ross, D.; Halpin, S.; Simms, A.; Salman, R.; Sivan, M. A Multidisciplinary NHS COVID-19 Service to Manage Post-COVID-19 Syndrome in the Community. J. prim. Care. Comm. Health 2021, 12, 1–9. [Google Scholar] [CrossRef]
- Sivan, M.; Preston, N.; Parkin, A.; Makower, S.; Gee, J.; Ross, D.; Tarrant, R.; Davison, J.; Halpin, S.; O’Connor, R.; Horton, M. The modified COVID-19 Yorkshire Rehabilitation Scale (C19-YRSm) patient-reported outcome measure for Long Covid or Post-COVID-19 syndrome. J. Med. Virol. 2022, 94, 4253–4269. [Google Scholar] [CrossRef]
- Smith, A.; Greenwood, D.; Horton, M.; Osborne, T.; Goodwin, M.; Lawrence, R.R.; Winch, D.; Williams, P.; Milne, R.; Sivan, M. Psychometric analysis of the modified COVID-19 Yorkshire Rehabilitation Scale (C19-YRSm) in a prospective multicentre study. BMJ Open Respir. Res. 2024, 11, e002271. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, B.; Janssen, M.F.; Feng, Y.-S.; Kohlmann, T.; Busschbach, J.; Golicki, D.; Lloyd, A.; Scalone, L.; Kind, P.; Pikard, S. Interim Scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L Value Sets. Value Health 2012, 15, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Overview | Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management | Guidance | NICE. Available online: https://www.nice.org.uk/guidance/ng206 (accessed on 23rd April 2024).
- Atchison, C.J.; Davies, B.; Cooper, E.; Lound, A.; Whitaker, M.; Hampshire, A.; Azor, A.; Donnelly, A.A.; Chadeau-Hyam, M.; Cooke, G.S.; Ward, H.; Elliot, P. Long-term health impacts of COVID-19 among 242,712 adults in England. Nat. Commun. 2023, 14, 6588. [Google Scholar] [CrossRef]
- Bowe, B.; Xie, Y.; Al-Aly, Z. Postacute sequelae of COVID-19 at 2 years. Nat. Med. 2023, 29, 2347–2357. [Google Scholar] [CrossRef]
- Ballouz, T.; Menges, D.; Anagnostopoulos, A.; Domenghino, A.; Aschmann, H.E.; Frei, A.; Fehr, J.S.; Puhan, M.A. Recovery and symptom trajectories up to two years after SARS-CoV-2 infection: population based, longitudinal cohort study. BMJ 2023, 381, e074425. [Google Scholar] [CrossRef]
- Soare, I.-A.; Ansari, W.; Nguyen, J.L.; Mendes, D.; Ahmed, W.; Atkinson, J.; Scott, A.; Atwell, J.E.; Longworth, L.; Becker, F. Health-related quality of life in mild-to-moderate COVID-19 in the UK: a cross-sectional study from pre- to post-infection. HQOL 2024, 22, 12. [Google Scholar] [CrossRef] [PubMed]
- Squire, I.; Glover, J.; Corp, J.; Haroun, R.; Kuzan, D.; Gielen, V. Impact of HF on HRQoL in patients and their caregivers in England: results from the ASSESS study. Br. J. Cardiol 2017, 30–34. [Google Scholar] [CrossRef]
- Carney, P.; O’boyle, D.; Larkin, A.; Mcguigan, C.; O’rourke, K. Societal costs of multiple sclerosis in Ireland. J. Med. Econ. 2018, 21, 425–437. [Google Scholar] [CrossRef]
- Nolan, C.M.; Longworth, L.; Lord, J.; Canavan, J.L.; Jones, S.E.; Kon, S.S.C.; Man, W.D.-C. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax 2016, 71, 493–500. [Google Scholar] [CrossRef]
- Glasziou, P.; Alexander, J.; Beller, E.; Clarke, P. Which health-related quality of life score? A comparison of alternative utility measures in patients with Type 2 diabetes in the ADVANCE trial. HQOL 2007, 5, 21. [Google Scholar] [CrossRef]
- Janssen, M.F.; Pickard, A.S.; Shaw, J.W. General population normative data for the EQ-5D-3L in the five largest European economies. Eur. J. Health Econ. 2021, 22, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Luo, N.; Johnson, J.A.; Coons, S.J. Using Instrument-Defined Health State Transitions to Estimate Minimally Important Differences for Four Preference-Based Health-Related Quality of Life Instruments. Med. Care. 2010, 48, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Navarro-Santana, M.J.; Fernández-De-Las-Peñas, C.; López-De-Uralde-Villanueva, I. Minimal Clinically Important Differences in EQ-5D-5L Index and VAS after a Respiratory Muscle Training Program in Individuals Experiencing Long-Term Post-COVID-19 Symptoms. Biomedicines 2023, 11, 2522. [Google Scholar] [CrossRef] [PubMed]
- Kedor, C.; Freitag, H.; Meyer-Arndt, L.; Wittke, K.; Hanitsch, L.G.; Zoller, T.; Steinbeis, F.; Haffke, M.; Rudolf, G.; Heidecker, B.; Bobbert, T.; Spranger, J.; Volk, H-D.; Skurk, C.; Konietschke, F.; Paul, F.; Behrends, U.; Bellmann-Strobl, J. & Scheibenbogen, C. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat. Commun. 2022, 13, 1, 5104. [CrossRef]
- Jason, L.A.; Dorri, J.A. ME/CFS and Post-Exertional Malaise among Patients with Long COVID. Neurol. Int. 2023, 15, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Tokumasu, K.; Honda, H.; Sunada, N.; Sakurada, Y.; Matsuda, Y.; Yamamoto, K.; Kakono, Y.; Hasegawa, T.; Yamamoto, Y.; Otsuka, Y.; Hagiya, H.; Kataoka, H.; Ueda, K.; Otsuka, F. Clinical Characteristics of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Diagnosed in Patients with Long COVID. Medicina 2022, 7, 850. [Google Scholar] [CrossRef] [PubMed]
- González-Hermosillo, J. A.; Martínez-López, J. P.; Carrillo-Lampón, S. A.; Ruiz-Ojeda, D.; Herrera-Ramírez, S.; Amezcua-Guerra, L. M.; Martínez-Alvarado, M. D. R. Post-Acute COVID-19 Symptoms, a Potential Link with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A 6-Month Survey in a Mexican Cohort. Brain sci. 2021, 11, 760. [Google Scholar] [CrossRef]
- Sivan, M.; Greenhalgh, T.; Darbyshire, J.L.; Mir, G.; O’Connor, R.J.; Dawes, H.; Greenwood, D.; O’Connor, D.; Horton, M.; Petrou, S.; de Lusignan, S.; Curcin, V.; Mayer, E.; Casson, A.; Milne, R.; Rayner, C.; Smith, N.; Parkin, A.; Preston, N.; Delaney, B. LOng COvid Multidisciplinary consortium Optimising Treatments and servIces acrOss the NHS (LOCOMOTION): protocol for a mixed-methods study in the UK. BMJ Open 2022, 12, e063505. [Google Scholar] [CrossRef]
Table 1.
Sociodemographic characteristics for all participants included in the study.
Table 1.
Sociodemographic characteristics for all participants included in the study.
| Demographics |
Number |
% |
| Total Number of responses |
112
58.5 (22-81) |
| Median age (range) |
Sex
Male |
42 |
37.5 |
| Female |
70 |
62.5 |
| Ethnicity |
|
|
| White |
84 |
75 |
| Mixed |
0 |
|
| Asian or Asian British |
2 |
1.8 |
| Black or Black British |
1 |
0.9 |
| Other ethnic groups |
0 |
|
| Unknown |
25 |
22.3 |
| Employment |
|
|
| Employed – no change |
50 |
45 |
| Had to retire/change jobs |
22 |
20 |
| Reduced working hours |
15 |
13.4 |
| Changes to job/role |
7 |
6.3 |
| Missing/unknown |
7 |
6.3 |
| Lost job |
3 |
2.7 |
| Disability |
3 |
2.7 |
| Unemployed |
3 |
2.7 |
| Sick Leave |
1 |
0.9 |
| Body Mass Index |
|
|
| Median (range) |
28.7 |
(14.8 – 47.4) |
| Underweight |
1 |
1 |
| Healthy weight |
19 |
17 |
| Overweight |
32 |
29 |
| Obese |
36 |
32 |
| Unknown |
24 |
21 |
Co-morbidities (>3
significant co-morbidities) |
40 |
35.7 |
Duration of LC –
Median (range) |
37.06 months (15.08 – 49.51)
9.7 months (3.9 – 26.5) |
|
Time since discharge from the service – median (range) |
Table 2.
PROM values at different time points of the service evaluation.
Table 2.
PROM values at different time points of the service evaluation.
| PROM (SD) |
Pre-COVID
Mean (SD) |
Initial
Mean (SD) |
Interim
Mean (SD) |
At discharge
Mean (SD) |
Post-discharge
Mean (SD) |
C19 – YRSm
SS |
4 |
18.4 |
17.3 |
13 |
15.1 |
| (4.59) |
(4.94) |
(5.31) |
(7.54) |
(6.06) |
C19-YRSm
FD |
1.2 |
6.7 |
6.2 |
6 |
5.9 |
| (2.47) |
(3.32) |
(2.65) |
(3.6) |
(4.48) |
C19-YRSm
OH |
7.3 |
4.9 |
5.5 |
6 |
5.2 |
| (2.76) |
(1.77) |
(1.98) |
(2.03) |
(2.21) |
EQ-5D-5L
Index Value |
- |
0.52 |
0.52 |
0.65 |
0.53 |
| - |
(0.27) |
(0.25) |
(0.23) |
(0.29) |
EQ-5D-5L
VAS |
- |
51.9 |
53.11 |
65 |
57.67 |
| - |
(20.84) |
(16.51) |
(20.46) |
(20.19) |
Table 3.
Reported changes since discharge from LLCRS.
Table 3.
Reported changes since discharge from LLCRS.
| Change since Discharge from LLCRS |
No. of patients (n=112) |
% |
| Back to pre-covid health |
11 |
9.8 |
| Greatly improved |
16 |
14.2 |
| Some improvement |
31 |
28 |
| Same as when discharged |
25 |
22 |
| Somewhat worse |
21 |
19 |
| A lot worse |
7 |
6.2 |
| Unanswered |
1 |
0.8 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).