Submitted:
11 September 2024
Posted:
11 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Literature Review
2.1. Health Services
2.2. The Paradox of Dynamic Equilibrium
2.3. Telemedicine
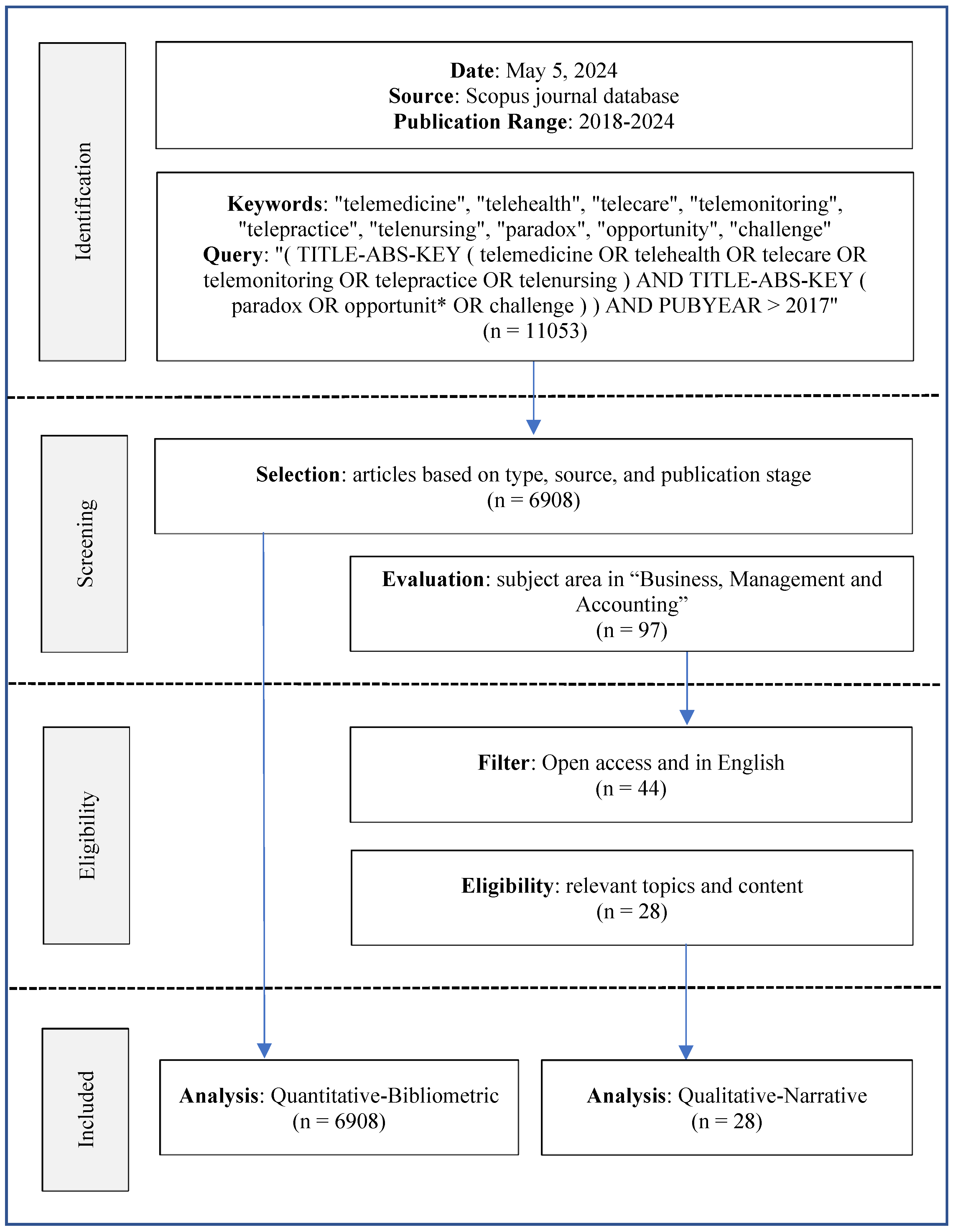
3. Methods
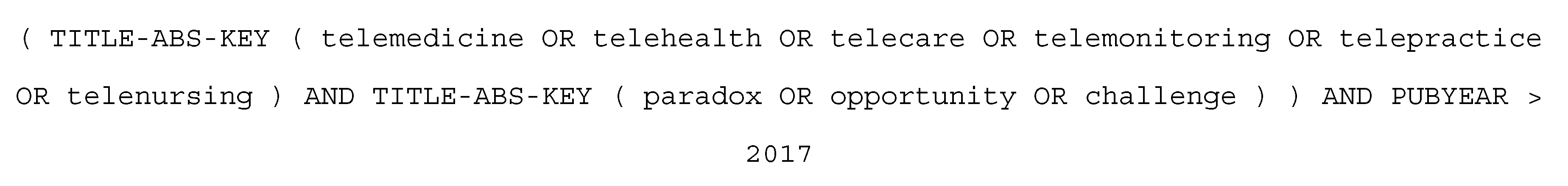
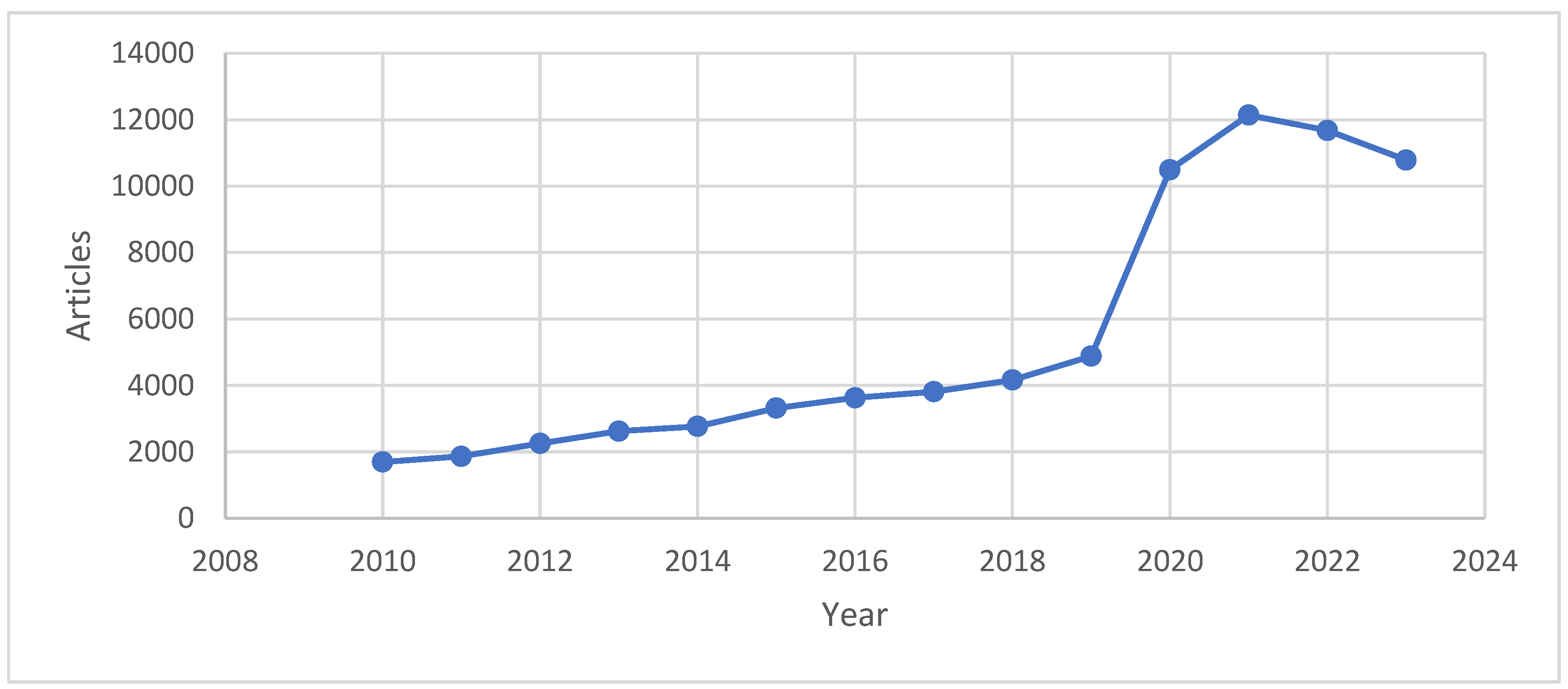
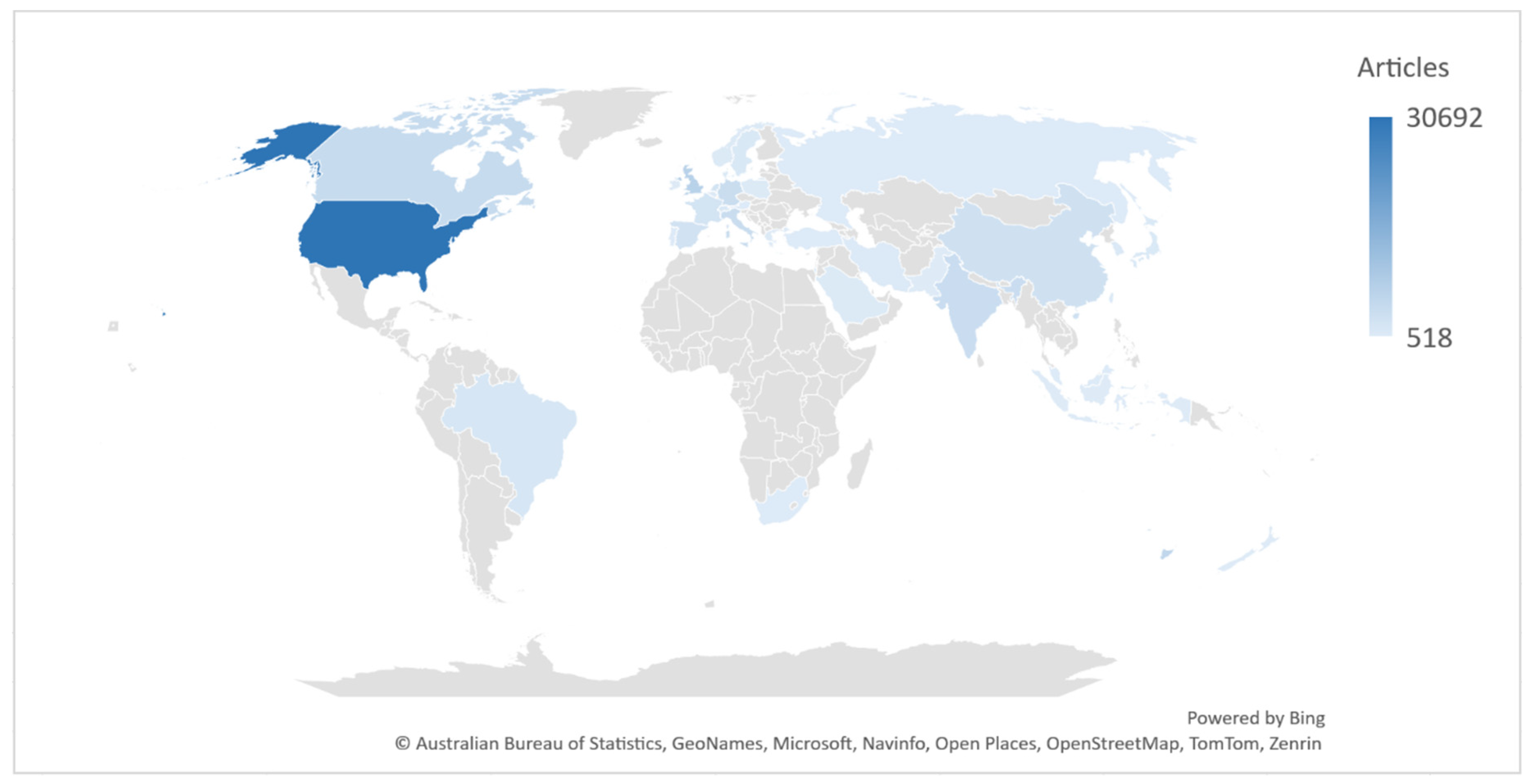
4. Results
4.1. Quantitative Data
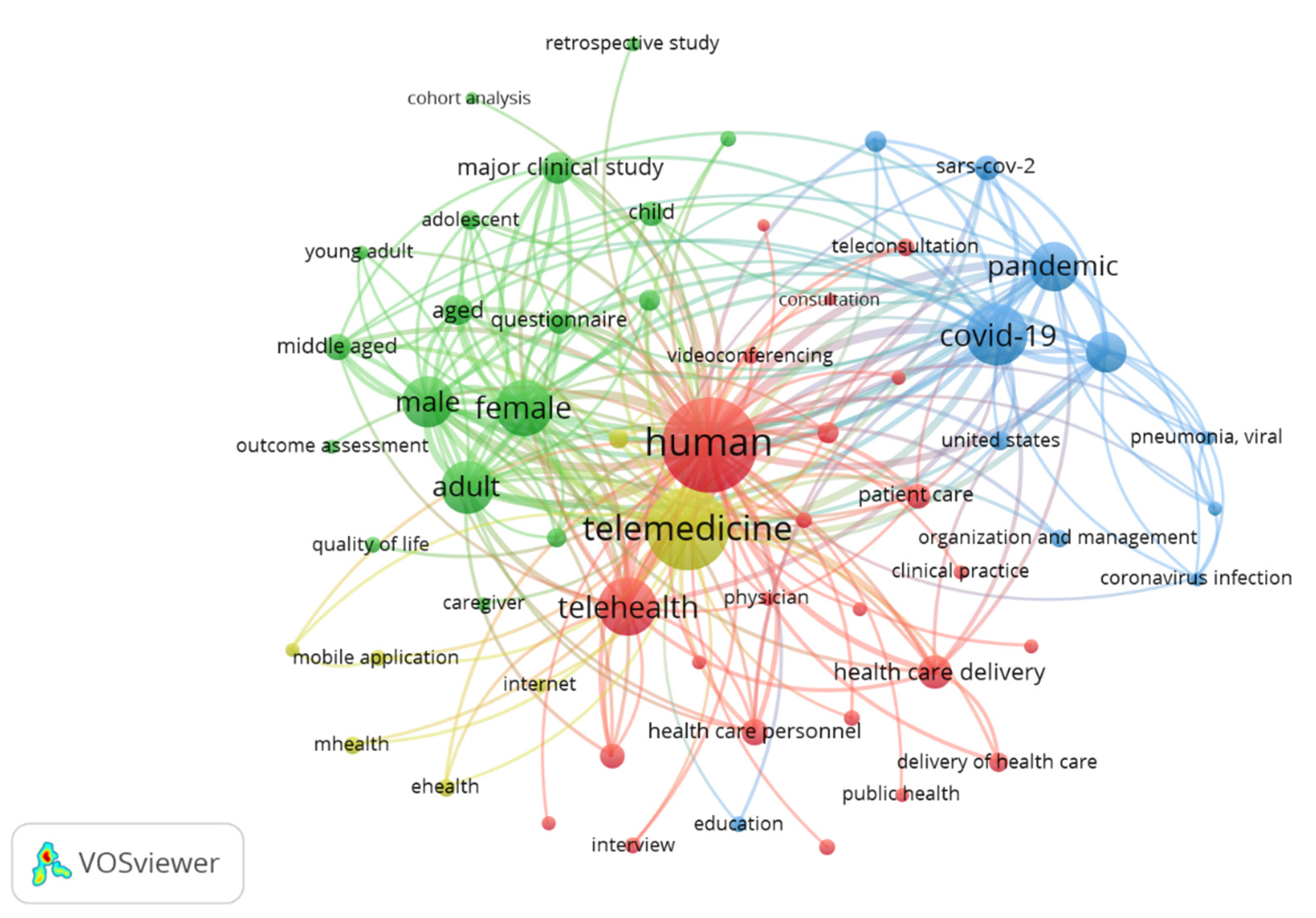
- Cluster 1 (red): Health services. This cluster consists of keywords related to aspects of public health and primary health services, such as "health care access", "health care delivery", "primary health care", and "public health". The nodes in this cluster demonstrate the importance of health service accessibility, health service delivery, and the role of primary health care in the context of telemedicine.
- Cluster 2 (green): Health quality. This cluster includes keywords related to mental health and quality of life, such as "mental health", "quality of life", and "patient satisfaction". This shows the focus of research on the psychological aspects and quality of life of patients when using telemedicine.
- Cluster 3 (blue): COVID-19 pandemic. This cluster includes keywords related to the COVID-19 pandemic and viral infections, such as "COVID-19", "coronavirus infection", "pandemic", and "virus pneumonia". This shows that the COVID-19 pandemic has been an important factor driving research on the use of telemedicine in managing the pandemic and treating patients infected with the virus.
- Cluster 4 (yellow): Technology. This cluster consists of keywords related to telemedicine technology and its applications, such as "telemedicine", "eHealth", "mhealth", and "telehealth". The nodes in this cluster represent research on various technical aspects of telemedicine, including technology platforms, mobile applications, and remote consultations.
4.2. Qualitative Data
4.2.1. Pre-COVID Telemedicine Services Articles
4.2.2. Post-COVID Telemedicine Services Article
5. Discussion
5.1. Pre- and Post-COVID Telemedicine
5.2. Telemedicine Paradox Cluster
5.2.1. Health Services
5.2.2. Health Quality
5.2.3. COVID-19 Pandemic
5.2.4. Technology
5.3. Telemedicine Research Perspective in the Dynamic Equilibrium Model
6. Conclusion
7. Implications
8. Limitations and Further Research
Sources of Financial and Non-Financial Support
Declaration of competing interest
References
- LR Koenig, A. Becker, J. Ko, and UD Upadhyay, “The Role of Telehealth in Promoting Equitable Abortion Access in the United States: Spatial Analysis.,” JMIR Public Heal. Surveillance. , vol. 9, p. e45671, Nov. 2023. [CrossRef]
- S. Kolluri, TS Stead, RK Mangal, RLJ Coffee, J. Littell, and L. Ganti, “Telehealth in Response to the Rural Health Disparity.,” Heal. Psychol. Res. , vol. 10, no. 3, p. 37445, 2022. [CrossRef]
- SN Gajarawala and JN Pelkowski, “Telehealth Benefits and Barriers.,” J. Nurse Pract. , vol. 17, no. 2, pp. 218–221, Feb. 2021. [CrossRef]
- DD Payán, JL Frehn, L. Garcia, AA Tierney, and HP Rodriguez, “Telemedicine implementation and use in community health centers during COVID-19: Clinic personnel and patient perspectives,” SSM - Qual. Res. Heal. , vol. 2, p. 100054, 2022. [CrossRef]
- JR Abbatemarco et al., “Providing Person-Centered Care via Telemedicine in the Era of COVID-19 in Multiple Sclerosis,” J. Patient Exp. , vol. 8, p. 2374373520981474, Jan. 2021. [CrossRef]
- DI Atefeh Farzindar, Natural Language Processing for Social Media, 1st ed. Switzerland: Springer Cham, 2015.
- F. Binsar and N. Legowo, "Design of Cloud Computing Outpatient Registration Model Through SMS Messages at Hospitals using TOGAF ADM," Int. J. Recent Technol. Eng. , vol. 8, no. 5, pp. 3857–3865, 2020. [CrossRef]
- Chakraborty, S. Edirippulige, and P. Vigneswara Ilavarasan, “The role of telehealth startups in healthcare service delivery: A systematic review,” Int. J. Med. Inform. , vol. 174, p. 105048, 2023. [CrossRef]
- RMA van der Boon et al., “Risks and benefits of sharing patient information on social media: a digital dilemma,” Eur. Listen. J. - Digits. Heal. , p. ztae009, Feb. 2024. [CrossRef]
- R.-A. Hardie et al., “Telehealth-based diagnostic testing in general practice during the COVID-19 pandemic: an observational study.,” BJGP open, vol. 6, no. 1, March. 2022. [CrossRef]
- B. Hofmann, “The paradox of health care,” Heal. Anal Care. , vol. 9, no. 4, pp. 369–386, 2001. [CrossRef]
- D. Kabel, J. Martin, and M. Elg, “Paradoxical tensions during industry 4.0 integration within health care: managing tensions for quality improvement,” Int. J. Lean Six Sigma, 2024.
- N. Singh, M. Jain, MM Kamal, R. Bodhi, and B. Gupta, “Technological paradoxes and artificial intelligence implementation in healthcare. An application of paradox theory,” Technol. Forecast. Soc. Change, vol. 198, no. November 2023, p. 122967, 2024. [CrossRef]
- Kokshagina and S. Schneider, “The Digital Workplace: Navigating in a Jungle of Paradoxical Tensions,” Calif. Manage. Rev., vol. 65, no. 2, pp. 129–155, 2023. [CrossRef]
- M. Abdel-Wahab, E. Rosenblatt, B. Prajogi, E. Zubizarretta, and M. Mikhail, “Opportunities in Telemedicine, Lessons Learned After COVID-19 and the Way Into the Future,” Int. J. Radiat. Oncol. Biol. Phys. , vol. 108, no. 2, pp. 438–443, 2020. [CrossRef]
- E. Tenggono, BW Soetjipto, and L. Sudhartio, "Navigating institutional pressure: Role of dynamic managerial capabilities and strategic agility in healthcare organizations' renewal," Int. J. Health c. Manag. , 2024. [CrossRef]
- Y. Mahendradhata et al., The Republic of Indonesia Health System Review, vol. 7, no. 1. Asia Pacific Observatory on Health Systems and Policies, 2017.
- KR Gallardo, D. Santa Maria, S. Narendorf, CM Markham, MD Swartz, and CM Batiste, “Access to healthcare among youth experiencing homelessness: Perspectives from healthcare and social service providers,” Child. Youth Serv. Rev., vol. 115, p. 105094, 2020. [CrossRef]
- J. Choi and J. Xavier, Digitalization of Public Service Delivery in Asia, First edit. Tokyo: Asian Productivity Organization, 2021.
- JH Vojtěch Máca, Milan Ščasný, Iva Zvěřinová, Michal Jakob, “Incentivizing Commuter Cycling by Financial and Non-Financial Rewards,” Int. J. Environment Res. public Heal. , vol. 17, no. 17, p. 6033, 20AD. [CrossRef]
- L. Emanuel et al., “What Exactly Is Patient Safety?,” J. Med. Regular. , vol. 95, no. 1, pp. 13–24, 2009.
- Kuek and S. Hakkennes, “Healthcare staff digital literacy levels and their attitudes towards information systems,” Health Informatics J., vol. 26, no. 1, pp. 592–612, Apr. 2019. [CrossRef]
- J.L. Sánchez, S. Savin, and V. Vasileva, “Key Success Factors in Implementing Electronic Medical Records in University Hospital of Rennes,” L'Ecole Natl. la Santé Publique Natl. Sch. Public Heal. Rennes Rennes Fr. , no. January 2005, pp. 1–59, 2005.
- B.M. Esch, F. Marian, A. Busato, and P. Heusser, "Patient satisfaction with primary care: an observational study comparing anthroposophic and conventional care," Heal. Qual. Life Outcomes, vol. 6, no. 74, pp. 1–15, 2008. [CrossRef]
- G. of Ireland, Building a Culture of Patient Safety. Dublin, Ireland: Brunswick Press Ltd, 2008.
- C. Vincent, Patient Safety, 2nd Editio. London, UK: Wiley-Blackwell, 2010.
- MU Chelladurai, DS Pandian, and DK Ramasamy, "A blockchain-based patient-centric electronic health record storage and integrity management for e-Health systems," Heal. Policy Technol. , vol. 10, no. 4, 2021. [CrossRef]
- D. Diaz, “Digital literacy in healthcare,” University of Sunderland, 2021. [Online]. Available: https://online.sunderland.ac.uk/digital-literacy-in-healthcare/. [Accessed: 10-Sep-2023].
- WHO, World, Delivering quality health services: a global imperative for universal health coverage, no. July. Geneva, 2018.
- J. Schad, M.W. Lewis, S. Raisch, and W.K. Smith, “Paradox Research in Management Science: Looking Back to Move Forward,” Acad. Manag. Ann. , vol. 10, no. 1, pp. 5–64, 2016. [CrossRef]
- D. Miller, "Icarus paradox: How exceptional companies bring about their downfall," IEEE Eng. Manag. Rev., vol. 21, no. 2, pp. 80–88, 1992.
- MP e Cunha and LL Putnam, “Paradox theory and the paradox of success,” Strateg. Organ. , vol. 17, no. 1, pp. 95–106, Oct. 2017. [CrossRef]
- Ella Miron-Spektor, “Embracing the Paradoxes of Leadership,” INSEAD Knowl. , pp. 1–3, 2019.
- MM Sulphey, “How the Icarus Paradox Doomed Kingfisher Airlines,” Vision, vol. 24, no. 1, pp. 118–124, 2020. [CrossRef]
- W. Smith and M. Lewis, “Toward a theory of paradox: A dynamic equilibrium model of organizing,” Acad. Manag. Rev., vol. 36, no. 2, pp. 381–403, 2011. [CrossRef]
- J. Grady, “Telehealth: A case study in disruptive innovation,” Am. J. Nurs. , vol. 114, no. 4, pp. 38–45, 2014. [CrossRef]
- M. Chen, S. Xu, L. Husain, and G. Galea, “Digital health interventions for COVID-19 in China: a retrospective analysis,” Intell. Med., no. April, 2021. [CrossRef]
- R. Wasim, K. Salah, R. Jayaraman, I. Yaqoob, S. Ellahham, and M. Omar, “The role of blockchain technology in telehealth and telemedicine,” Int. J. Med. Inform. , vol. 148, no. 2021, pp. 1–10, 2021. [CrossRef]
- J. Gaughan, L. Siciliani, H. Gravelle, and G. Moscelli, “Do small hospitals have lower quality? Evidence from the English NHS,” Soc. Sci. Med., vol. 265, p. 113500, 2020. [CrossRef]
- RS Weinstein et al., “Telemedicine, Telehealth, and Mobile Health Applications That Work: Opportunities and Barriers,” Am. J. Med. , vol. 127, no. 3, pp. 183–187, 2014. [CrossRef]
- D. Greene et al., “Creating training opportunities for public health practitioners,” Am. J. Prev. Med., vol. 16, no. 3 SUPPL., pp. 80–85, 1999. [CrossRef]
- RA Scheepers, H. Emke, RM Epstein, and KMJMH Lombarts, “The impact of mindfulness-based interventions on doctors' well-being and performance: A systematic review,” Med. Educ. , vol. 54, no. 2, pp. 138–149, 2020. [CrossRef]
- Kirby, “Exploratory Bibliometrics: Using VOSviewer as a Preliminary Research Tool,” Publications, vol. 11, no. 1. 2023. [CrossRef]
- N. Donthu, S. Kumar, D. Mukherjee, N. Pandey, and WM Lim, “How to conduct a bibliometric analysis: An overview and guidelines,” J. Bus. Res. , vol. 133, pp. 285–296, 2021. [CrossRef]
- Y. Qiang, X. Tao, X. Gou, Z. Lang, and H. Liu, “Towards a Bibliometric Mapping of Network Public Opinion Studies,” Information, vol. 13, no. 1. 2022. [CrossRef]
- H. Tiirinki et al., “COVID-19 pandemic in Finland – Preliminary analysis on health system response and economic consequences,” Heal. Policy Technol. , vol. 9, no. 4, pp. 649–662, 2020. [CrossRef]
- M. Hamsal and M. Ichsan, “The COVID-19 Pandemic and Telemedicine Adoption: Challenges and Opportunities,” Proc. First Int. Conf. Econ. Bus. Entrep. ICEBE 2020 , p. 324, 2020. [CrossRef]
- C. Standing, S. Standing, M. L. McDermott, R. Gururajan, and R. Kiani Mavi, “The Paradoxes of Telehealth: a Review of the Literature 2000–2015,” Syst. Res. Behav. Sci. , vol. 35, no. 1, pp. 90–101, 2018. [CrossRef]
- X. Sheng, Y. Martirosyan, KS Hossain, R. Felix, and A. Singh, “Unpacking the influencing factors of telehealth usage among older consumers,” Health Mark. Q. , vol. 41, no. 1, pp. 95–111, 2024. [CrossRef]
- Patnaik and KK Prasad, “Secure Authentication and Data Transmission for Patients Healthcare Data in the Internet of Medical Things,” Int. J. Math. Eng. Manag. Sci. , vol. 8, no. 5, pp. 1006–1023, 2023. [CrossRef]
- R. Pitchai, S. Anjanayya, and M. Maravarman, “Cloud computing based generic medicine recommendation system for advanced E-Healthcare,” Mater. Today Proc. , 2021. [CrossRef]
- KM Zobair, L. Sanzogni, and K. Sandhu, “Telemedicine healthcare service adoption barriers in rural Bangladesh,” Australas. J. Inf. Syst. , vol. 24, pp. 1–24, 2020. [CrossRef]
- AA Khafizova, AM Galimov, SR Kharisova, LY Grebenshchikova, RI Yagudina, and LM Smirnova, “The impact of healthcare digitalization on the medical education curricula and programs: Points of convergence and divergence,” Contemp. Educ. Technol. , vol. 15, no. 4, 2023. [CrossRef]
- SSM Sadrul and N. Noushin, “Alternative Modes of Health Service Delivery,” Sustain. Future. , vol. 3, p. 100055, 2021. [CrossRef]
- Y. Wang, N. Yi, H.M. Ericksen, and W. Zhang, “Case report: Self-performed orthopedic examinations in telehealth treatment of a youth athlete with acute rotator cuff strain,” Front. Sport. Act. Living, vol. 5, no. May, pp. 1–6, 2023. [CrossRef]
- Y. Siriwardhana, C. De Alwis, G. Gur, M. Ylianttila, and M. Liyanage, “The Fight against the COVID-19 Pandemic with 5G Technologies,” IEEE Eng. Manag. Rev., vol. 48, no. 3, pp. 72–84, 2020. [CrossRef]
- Chowdhury, A. Hafeez-Baig, R. Gururajan, A. McCubbin, M.A. Sharif, and S.J. Miah, “The Role of Image Quality in Telehealth: Adoption Challenges in the Subcontinent,” Pacific Asia J. Assoc. Inf. Syst. , vol. 13, no. 3, pp. 131–145, 2021. [CrossRef]
| Code | Authors | Year | Purpose | Findings | |
|---|---|---|---|---|---|
| Opportunities | Challenges | ||||
| B1 | Nielsen K.D.; Langstrup H. | 2018 | Exploring how patients express their participation in various ways through e-health technologies. |
|
The implementation to involve is unpredictable. |
| B2 | Standing C.; Standing S.; McDermott M.-L.; Gururajan R.; Kiani Mavi R. | 2018 | Analyzes telehealth literature from 2000 to 2015 focusing on paradoxes. | Growth in telehealth literature, opportunities for the development of more advanced telehealth technologies. | Disadvantages of telehealth operational models in capturing value. |
| B3 | Samerski S. | 2018 | Investigate how digital epidemiology and eHealth together become a solid health surveillance system, changing current concepts about the body and health. |
|
Patients are considered a risk profile and are encouraged to perceive and manage themselves as a collection of health and safety risks. |
| B4 | Dash M.; Shadangi PY; Kar S.; Prusty R. | 2019 | Analyze the factors influencing the adoption of telemedicine services by doctors in India. |
|
|
| B5 | Samerski S.; Müller H. | 2019 | To examine the perspectives and status of stakeholders in the German health system and to develop the concept of digital health literacy. |
|
|
| B6 | Eklund C.; Elfström ML; Eriksson Y.; Soderlund A. | 2019 |
|
|
|
| Code | Authors | Year | Purpose | Findings | ||
|---|---|---|---|---|---|---|
| Opportunities | Challenges | |||||
| P1 | Lupiáñez-Villanueva F.; Folkvord F.; Abeele MV | 2020 | Investigate mobile health (mHealth) application business model factors that influence adoption rates and user willingness to pay revenue models, data protection models, recommendation models, and provider models. |
|
|
|
| P2 | Siriwardhana Y.; De Alwis C.; Gur G.; Ylianttila M.; Liyanage M. | 2020 | To show how 5G and Internet of Things (IoT) technology can be used and developed to fight the COVID-19 pandemic. |
|
|
|
| P3 | Rhodes A.; Martin S.; Guarna J.; Vowles K.; Allen T. | 2020 | Development of a behavioral-contextual perspective on the treatment of patients with chronic pain during the COVID-19 pandemic. | Telehealth can provide easier access for chronic pain patients during periods of mandatory physical distancing. |
|
|
| P 4 | Zobair KM; Sanzogni L.; Sandhu K. | 2020 | Investigating barriers to telemedicine adoption in centers hosted by public hospitals in rural Bangladesh. | Telemedicine adoption improves access and quality of health services in rural Bangladesh. |
|
|
| P5 | Müller SD; Wehner DL; Konzag H.; Vesterby M.; Høybye MT | 2021 | Investigating the paradoxical success of the telehealth platform project "My Pathway" in Denmark to reduce the duration of patient hospitalization while maintaining patient satisfaction. |
|
|
|
| P6 | Shah A.; Guessi M.; Wali S.; Ware P.; McDonald M.; O'Sullivan M.; Posada JD; Ross H.; Seto E. | 2021 | Understanding the experience of using virtual cardiac care during the COVID-19 pandemic at Toronto General Hospital, Canada. |
|
|
|
| P7 | Guarcello C.; Raupp E. | 2021 | Analyzing the impact of the pandemic on innovation in the health sector and proposing an end-to-end innovation adoption model. |
|
|
|
| P8 | Chowdhury A.; Hafeez-Baig A.; Gururajan R.; McCubbin A.; Sharif MA; Miah SJ | 2021 | Investigates the challenges of the telehealth environment in India and Pakistan that hinder the transmission of high-quality images between patients and healthcare professionals. |
|
|
|
| P 9 | Sadrul SSM; Noushin N. | 2021 | Explores the role of telemedicine in providing adequate health services, especially during the COVID-19 pandemic, to reach communities in rural areas of Bangladesh. |
|
Inequality in the health system between urban and rural areas, with most highly qualified doctors providing services only in urban areas. | |
| P10 | Koinig I.; Diehl S. | 2022 |
|
|
|
|
| P11 | Frenert S.; Petersson L.; Muhic M.; Rydelfält C.; Nymberg VM; Ekman B.; Erlingsdottir G. | 2022 | Explores how eHealth mediates the experiences of health professionals, with a focus on the influence of solution materiality. |
|
|
|
| P12 | van Kessel R.; Hrzic R.; O'Nuallain E.; Weir E.; Wong BLH; Anderson M.; Baron-Cohen S.; Mossialos E. | 2022 | Exploring the benefits of digital health technologies for the global population, particularly those with disabilities, |
|
|
|
| P13 | Ghasemzadeh K.; Escobar O.; Yordanova Z.; Villasalero M. | 2022 | Application of user innovation (UI) in the e-health sector, as a step to discuss potential, trends, managerial gaps, and future research opportunities. |
|
|
|
| P 14 | Kark SM; Worthington MA; Christie RH; Masino AJ | 2023 | To identify the challenges psychiatrists face in treating patients with major depressive disorder (MDD), with a focus on the problem of misdiagnosis of bipolar disorder (BD). |
|
|
|
| P15 | Dreisoerner A.; Ferrandina C.; Schulz P.; Nater UM; Junker NM | 2023 | Explore the possibility of improving self-compassion through a novel, intense, and accessible intervention using online group-based interactive video teleconferencing. |
|
There remains great unexplored potential to improve other resources that improve mental health | |
| P16 | Alviani R.; Purwandari B.; Eitiveni I.; Purwaningsih M. | 2023 | Research and enrich knowledge about telemedicine adoption in Indonesia. |
|
|
|
| P17 | Khafizova AA; Galimov AM; Kharisova SR; Grebenshchikova LY; Yagudina RI; Smirnova LM | 2023 | Analyze how medical education programs are evolving to address the digital transformation in health care. |
|
|
|
| P18 | Patnaik A.; Prasad KK | 2023 | Protect sensitive medical data in the cloud by leveraging cloud computing facilities. |
|
|
|
| P19 | Wang Y.; Yi N.; Ericksen HM; Zhang W. | 2023 | Exploration of the possibility of self-administered orthopedic examination in telehealth treatment of a young athlete |
|
|
|
| P20 | Kuen L.; Schürmann F.; Westmattelmann D.; Hartwig S.; Tzafrir S.; Schewe G. | 2023 | Exploration of the interaction of various trust references (physician, technology, medication) and risk dimensions (performance, privacy, time, psychological) in patient adoption of telemedicine, taking physical and mental considerations into account. |
|
|
|
| P21 | Sheng X.; Martirosyan Y.; Hossain KS; Felix R.; Singh A. | 2024 | Exploration of challenges and motivations for telehealth use among older consumers, an under-researched population in the telehealth literature. |
|
|
|
| P22 | Aji PT; Ramadani L. | 2024 | Assessing the influence of user dimensions, technological aspects, and socio-cultural elements on intention to adopt telemedicine services. |
|
|
|
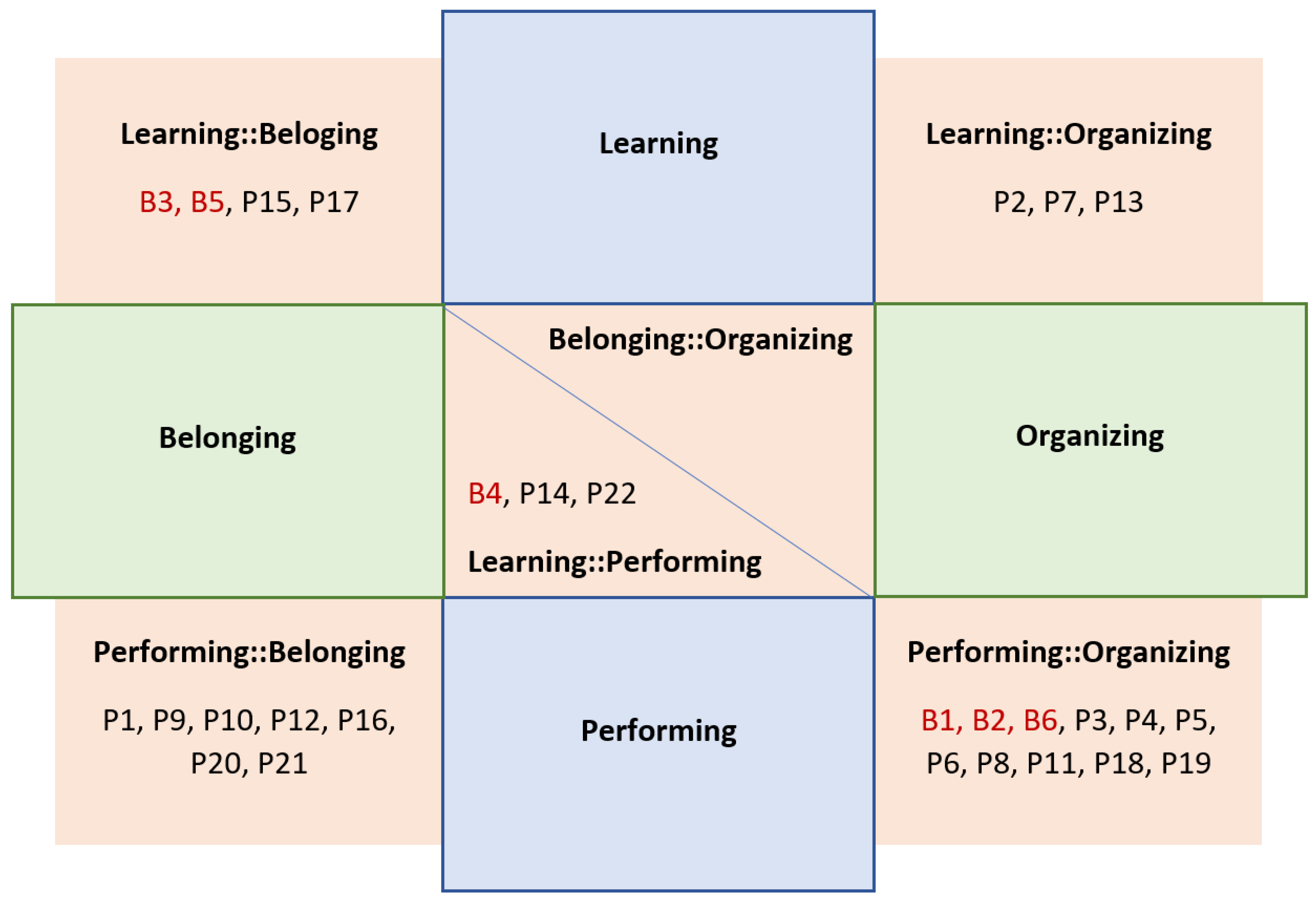
| Code | Year | Opportunities | Challenges |
|---|---|---|---|
| B1 | 2018 | Performing | Organizing |
| B2 | 2018 | Performing | Organizing |
| B3 | 2018 | Learning | Belonging |
| B4 | 2019 | Performing | Learning |
| B5 | 2019 | Belonging | Learning |
| B6 | 2019 | Performing | Organizing |
| Code | Year | Opportunities | Challenges |
|---|---|---|---|
| P1 | 2020 | Belonging | Performing |
| P2 | 2020 | Learning | Organizing |
| P3 | 2020 | Performing | Organizing |
| P4 | 2020 | Performing | Organizing |
| P5 | 2021 | Performing | Organizing |
| P6 | 2021 | Performing | Organizing |
| P7 | 2021 | Learning | Organizing |
| P8 | 2021 | Performing | Organizing |
| P9 | 2021 | Performing | Belonging |
| P10 | 2022 | Performing | Belonging |
| P11 | 2022 | Belonging | Organizing |
| P12 | 2022 | Performing | Belonging |
| P13 | 2022 | Learning | Organizing |
| P14 | 2023 | Performing | Learning |
| P15 | 2023 | Belonging | Learning |
| P16 | 2023 | Performing | Belonging |
| P17 | 2023 | Learning | Belonging |
| P18 | 2023 | Performing | Organizing |
| P19 | 2023 | Performing | Organizing |
| P20 | 2023 | Performing | Belonging |
| P21 | 2024 | Performing | Belonging |
| P22 | 2024 | Learning | Performing |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





