1. Introduction
Temporomandibular joint disorders (TMDs) are group of complex and diversified clinical conditions impairing physiological functioning of the masticatory system. American Academy of Orofacial Pain classifies TMDs as group of disorders involving the masticatory muscles, the temporomandibular joint (TMJ) and the associated structures. These may be caused by abnormal biomechanical forces in the TMJ, injuries, acquired or congenital deformations, lack of lubrication, degenerative articular disorder, malocclusion, joint hypermobility, weakness or laxity of the TMJ ligament and joint capsule. [
1,
2]. Recently, short sleep has been discussed as an another possible causal factor of TMDs. [
3] Genetic factors, such as polymorphisms in genes related to pain perception, inflammation,
bone metabolism, and
neurotransmission, and their significance in the onset and development of TMDs are still being investigated. [
4]
In clinical conditions, common complaints among patients are
myalgia involving masticatory muscle pain with or without complications, and
arthralgia associated with
TMJ pain, headaches. This may lead to sequela of unfavorable consequences. If left untreated, TMDs may contribute to limitation of jaw functionality and hence, oral health and quality of life. [
5] Patients with temporomandibular disorders were proven to be exhibit causal association with depression. [
6] Moreover, it may lead to sleep deprivation, oral parafunction, stress, anxiety and somatization. [
7]
Current treatment protocols assume interdisciplinary approach. Depending on severity of joint dysfunction, it may be limited to conservative approach such as rehabilitation supplemented with dental treatment, of splints, orthodontics, physical therapy and psychological approaches. [
8] More advanced techniques assume use of nerve blocks and surgical procedures. Arthrocentesis of the temporomandibular joints has been firstly described by Nitzan et al. in 1991. [
9] From that moment there were many modifications described, mostly comparing original Nitzan’s double needle technique with single- puncture needle or other modifications. [
10,
11] Arthrocentesis has been proven to be a bridging gap between conservative and surgical approach of TMDs treatment protocol.
Additional use of intracapsular injection of medicines was analyzed and compared in many studies. [
12,
13,
14] Nevertheless, arthrocentesis may decrease the TMDs severity and limit the necessity of more invasive treatment such as arthroscopy, open disc repositioning or total arthroplasty with use of TMJ prosthesis. The aim of this study was to evaluate the efficiency of arthrocentesis in the cohort of patients suffering from TMDs, evaluation which technique is more efficient, justification of additional medicine injection into the joints and their impact on overall treatment outcome.
2. Materials and Methods
Retrospective clinical control study of the patients who attended for TMJ arthrocentesis due to diagnosed TMD in the Department of Cranio-Maxillofacial Surgery, Oral Surgery and Implantology, Medical University of Warsaw, Poland was performed. All patients were diagnosed clinically and radiographically with informed consent prior to the procedure. The study was performed in accordance with Declaration of Helsinki and Approval of the ethics committee was obtained for the study.
The patents who met the following criteria were selected for the study: clinical presentation of pain in TMJ region on movement of mandible, restriction of mouth opening, clicking during mandibular movements, pain, deviation of mandible on opening the mouth, regular check ups and completed 6 sessions of arthrocentesis.
The patents who did not meet the following criteria were excluded from the study: lack of informed consent, patients who suffered muscular pain without diagnosis of TMDs, indications for arthroscopy or other invasive surgical treatment, medically compromised patients, incomplete documentation or less than 6 sessions of TMJ arthrocentesis performed.
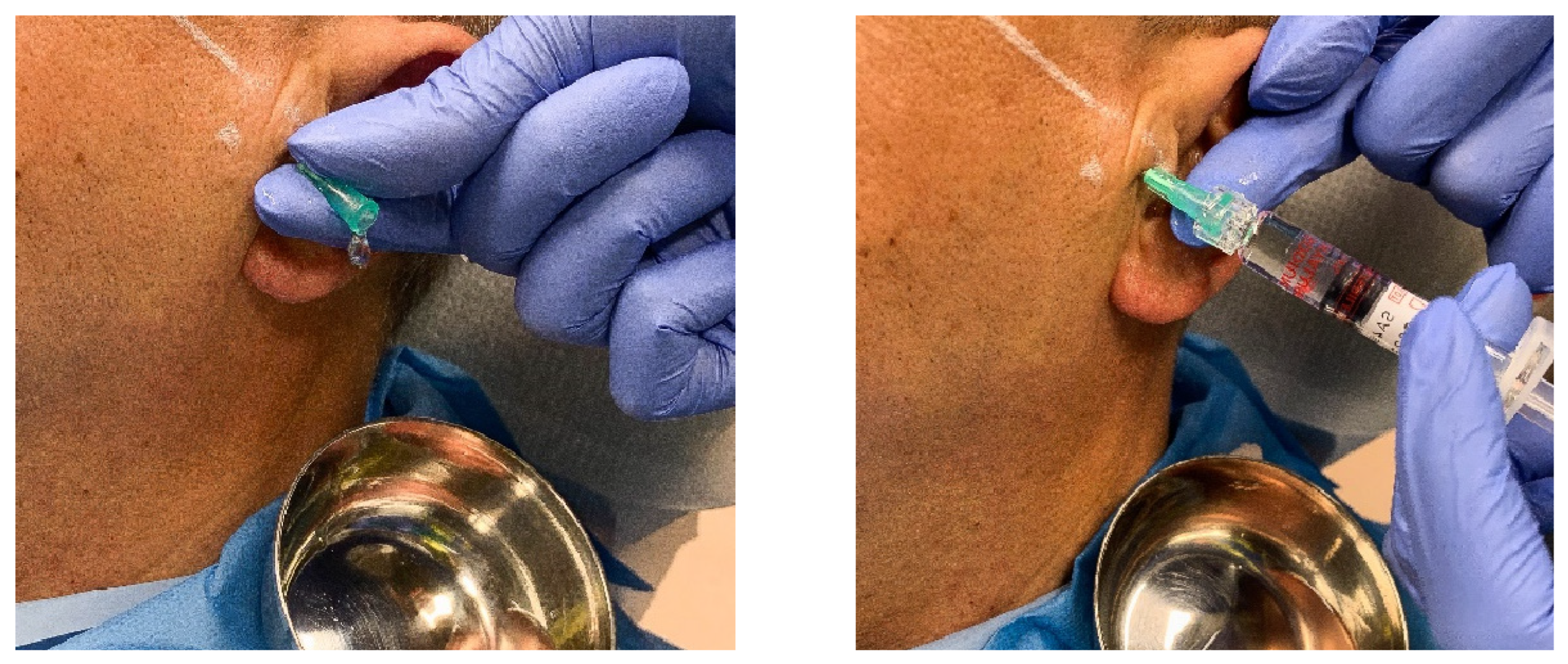
The two- needle arthrocentesis procedure was performed accordingly to the original technique described by Nitzan. [
15]Patient was seated inclined at 45° angle with head turned towards the unaffected side to provide approach to the joint to be treated. A line was drawn from the middle of the tragus to the outer canthus. The points of insertion were marked on the skin accordingly to McCain points used in arthroscopy. [
16] The posterior entrance point was located along the canthotragal line, 10 mm from the middle of the tragus and 2 mm below the line (
Figure 1). The anterior point of entry was placed 10 mm farther along the line and 10 mm below it. These markings over the skin indicate the location of the articular fossa and the eminence of the TMJ (Figure). In the single- needle puncture technique only posterior access point was used for joint lavage accordingly to technique described by Murakami et al. (1987). [
11]
After arthrocentesis through posterior access 1ml of hyaluronic acid () or platelet- rich plasma (PRF) was injected into the upper compartment of the TMJ. Pain assessment was done using visual analog scale (VAS), rated 1-10. The mouth opening was measured using caliper.
The success rate of treatment was graded as good, acceptable, or failure in accordance with
Table 1 as previously described. [
17,
18]
The data obtained in the study were analysed using IBM SPSS Statistics for Windows, Version 22.0 IBM Corp. A significance level with a p-value < 0.05 was considered statistically significant.
3. Results
96 patients who attended for TMJ arthrocentesis were enrolled into the study. 48 patients were diagnosed with established osteoarthritis (OA) (50%) and 48 with TMJ internal de-arrangement (disc displacement- DD). All individuals underwent TMJ arthrocentesis with either 1- needle or 2- needle technique performed every 4 weeks during a 6 month treatment period. Intracapsular application of the medicine (PRP or HA) was performed in 81 individuals. 15 patient refused intracapsular injection. (
Table 1)
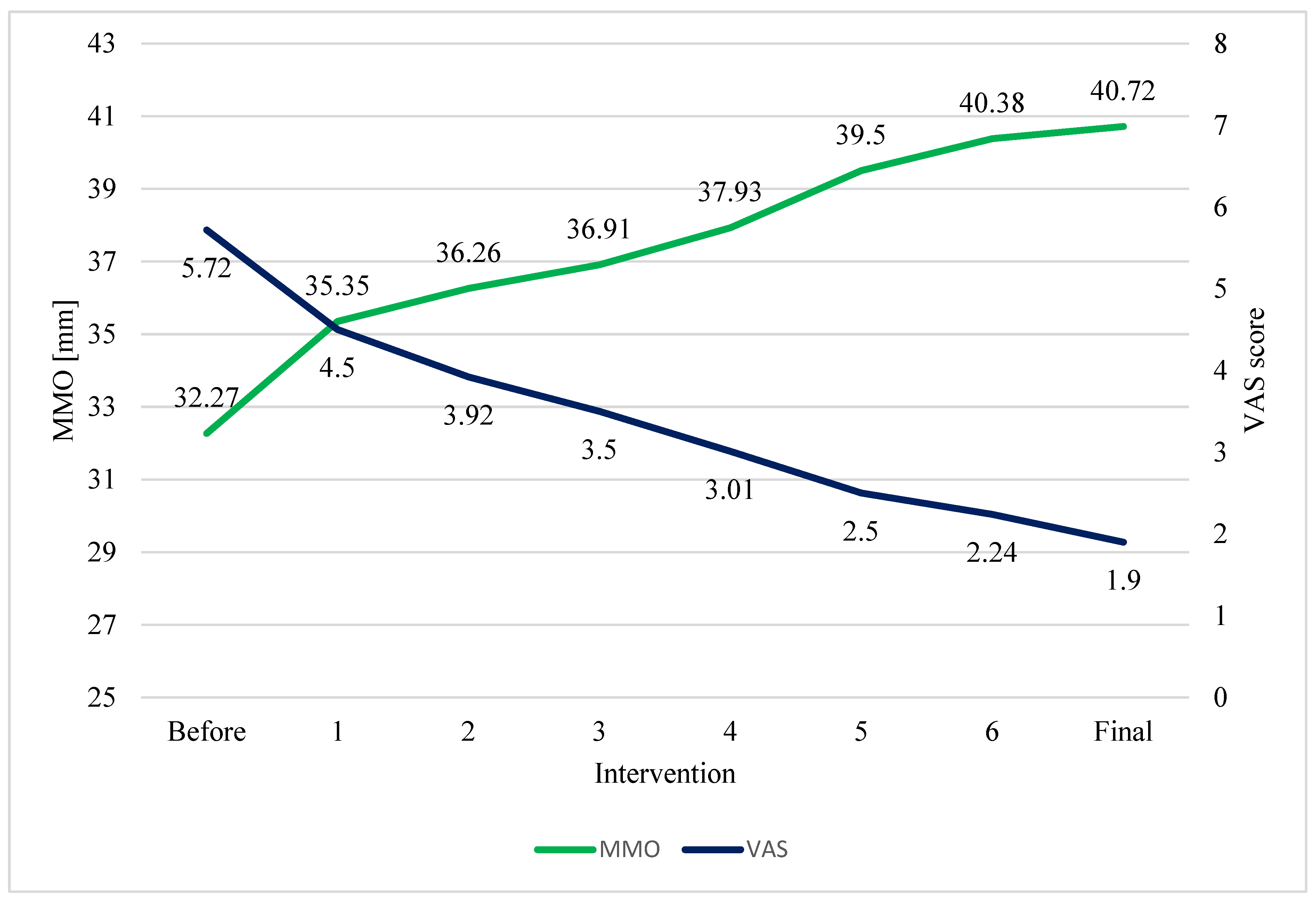
Patients, who underwent 6 cycles of arthrocentesis exhibited statistically significant pain reduction and increased mouth opening at the endpoint of the study in paired t- tests (
Table 2) (
Figure 2).
Table 2.
Main characteristics of the studied sample, N=96.
Table 2.
Main characteristics of the studied sample, N=96.
Figure 2.
Change in mean VAS and MMO scores, N=96. A one-way analysis of variance (ANOVA) with repeated measures showed a significant difference between the variables, F = 205.36, p-value = <0.001 for VAS decrease and F = 91.54, p-value = <0.001 for increase of MMO before and after the treatment.
Figure 2.
Change in mean VAS and MMO scores, N=96. A one-way analysis of variance (ANOVA) with repeated measures showed a significant difference between the variables, F = 205.36, p-value = <0.001 for VAS decrease and F = 91.54, p-value = <0.001 for increase of MMO before and after the treatment.
Table 3.
Average values and standard deviations of the characteristics of the studied sample, N=96.
Table 3.
Average values and standard deviations of the characteristics of the studied sample, N=96.
Single- puncture technique provided similar pain reduction as two needle approach. VAS decrease of mean 3.65±1,25 in single- needle and 4.11±1.21 in two- needle technique were observed without statistically significant differences in paired t- tests (p= .008). However, single- puncture technique provided better results in maximum mouth opening of 9.98±6.52 (p<0,001). Two needle technique provided 4.97± 3.97 mm improvement (suppl. Table 7).
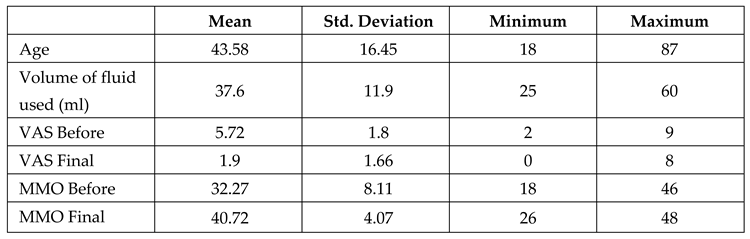
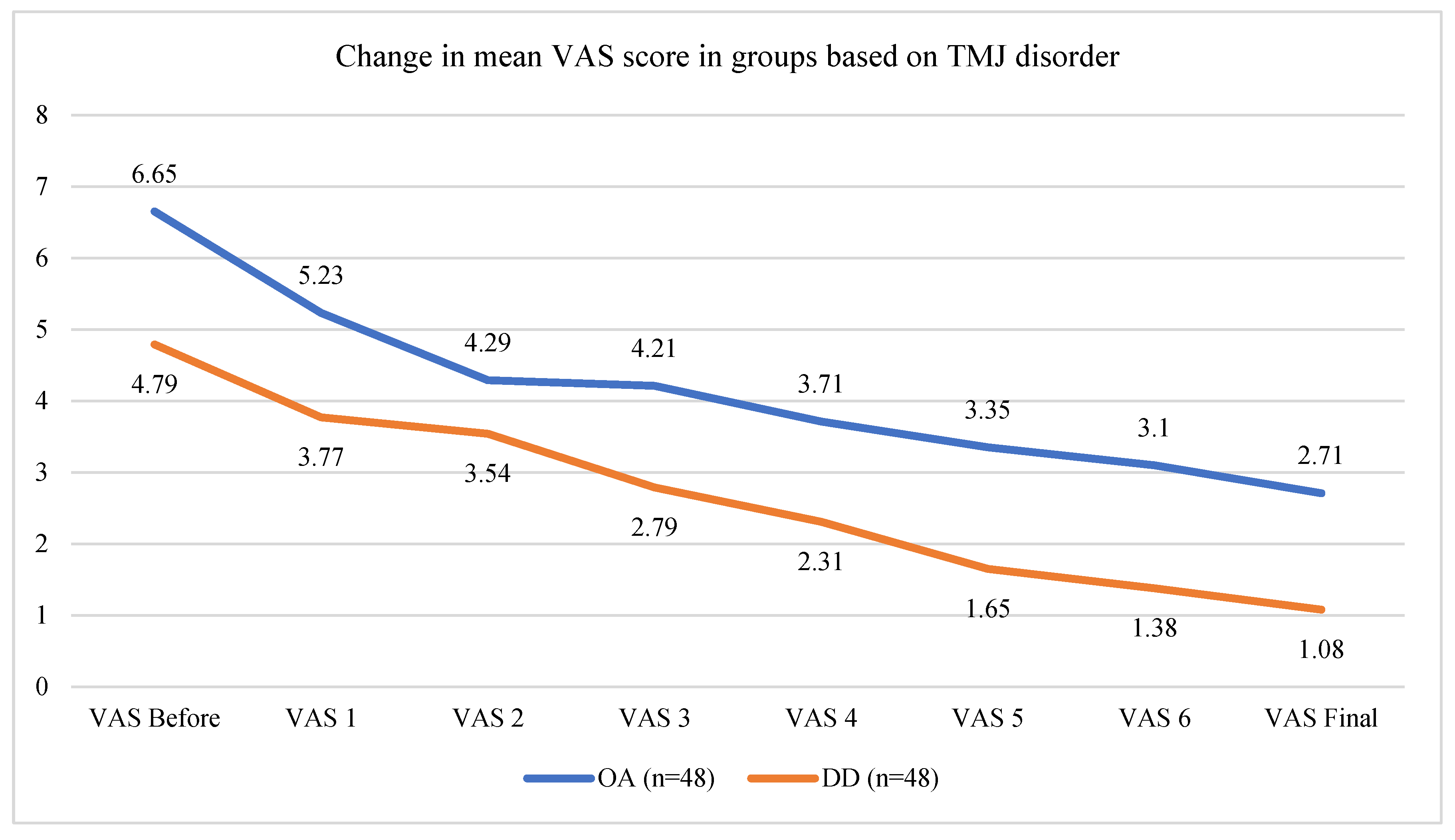
Patients with osteoarthritis (OA group) exhibited higher VAS scores and more limited mouth opening than patients with disc displacement (DD group) before the treatment. (suppl. Table 5). OA group mean age was 56.46±11.93 years old, whereas DD group was characterized by younger individuals (mean age of 30.71±8.13). Both groups exhibited statistically significant pain reduction and increased mouth opening at the endpoint of the study. (
Figure 2) Reduction of the pain was similar when comparing between the groups (p= 0.371). However patients with DD reached significantly better mouth opening than OA group at the endpoint of the study in paired t- tests (increase of 12.75±4.65mm VS increase of 3.46±3.39) (p<0.001) (suppl. Table 5) (
Figure 3).
Figure 3.
Graph showing gradual decrease of pain between each treatments in OA and DD cohorts.
Figure 3.
Graph showing gradual decrease of pain between each treatments in OA and DD cohorts.
Figure 4.
Graph showing gradual increase of maximal mouth opening between each treatments in OA and DD cohorts.
Figure 4.
Graph showing gradual increase of maximal mouth opening between each treatments in OA and DD cohorts.
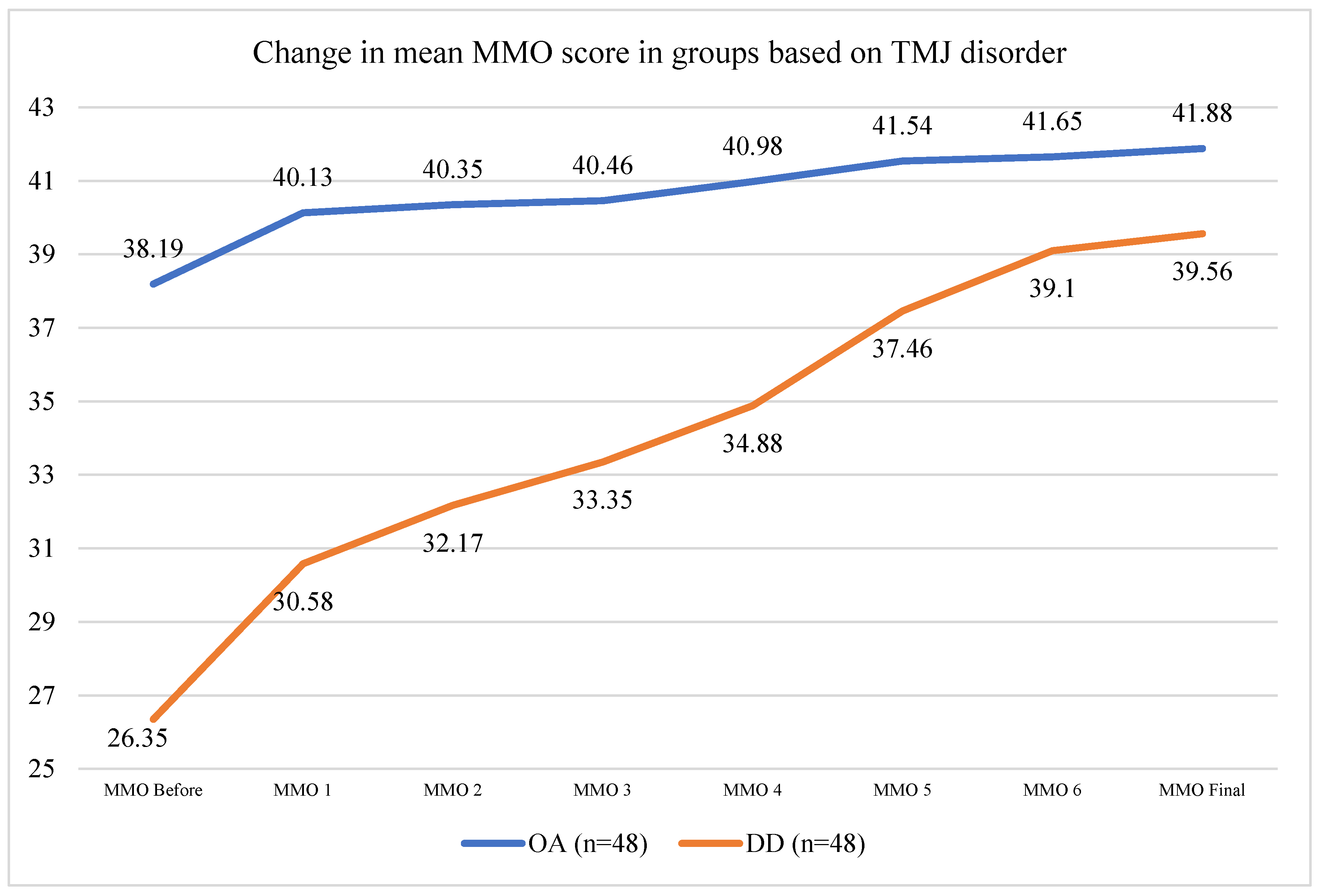
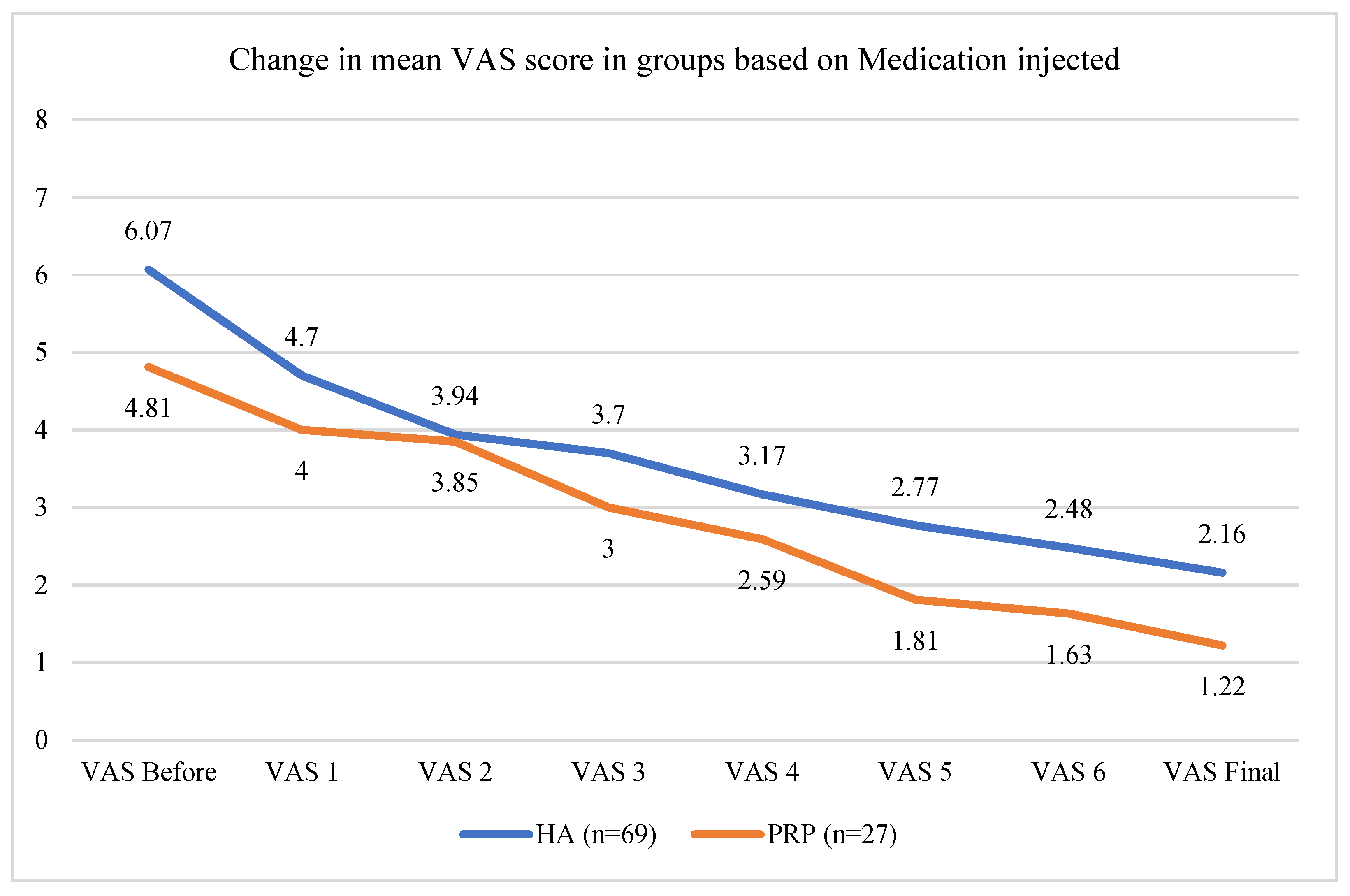
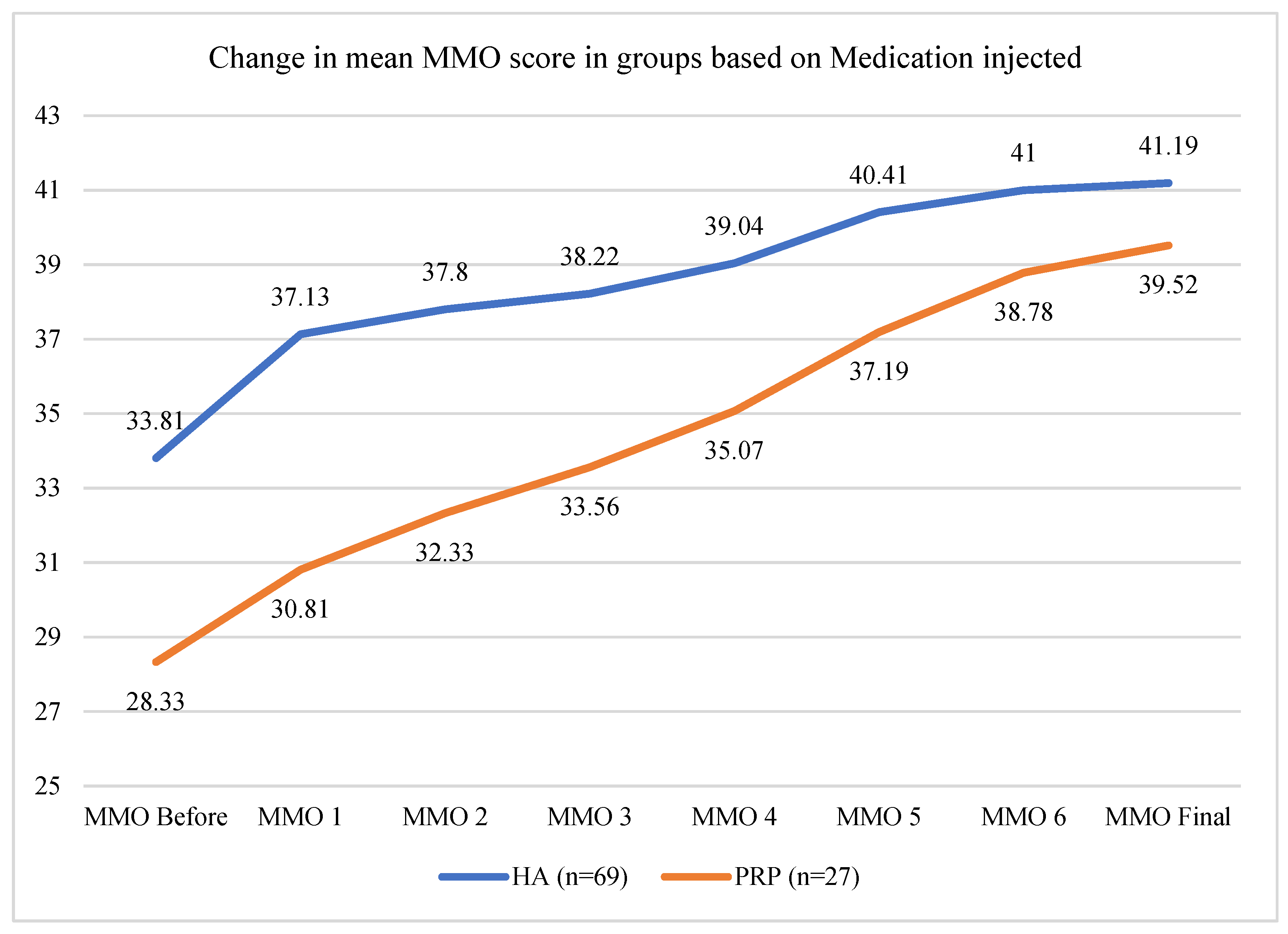
Intracapsular application of medication contributed to decrease of pain in both HA and PRP cohorts. Mean VAS decrease at the endpoint of the study was 3.91±1.21 for HA and 3.59± 1.34mm for PRP groups respectively showing similar impact on pain reduction associated with TMDs (DD or OA) without statistically significant difference in paired t- tests (p=.026). Mouth opening at the endpoint of the study was improved in both cohorts. However, PRP injection was significantly more efficient than HA (p=0,019). Mean final increase of maximal mouth opening in PRP cohort was improved by 10.44±5.18 mm whereas in HA cohort by 7.19± 6.33 mm.
Figure 5.
Graph showing gradual decrease of pain between each treatments in HA and PRP cohorts.
Figure 5.
Graph showing gradual decrease of pain between each treatments in HA and PRP cohorts.
Figure 6.
Graph showing gradual increase of maximal mouth opening between each treatments in in HA and PRP cohorts.
Figure 6.
Graph showing gradual increase of maximal mouth opening between each treatments in in HA and PRP cohorts.
Despite overall success of the arthrocentesis, regardless of its type or medication applicated accordingly to
Table 1, 20 patients were classified as treatment “failure” accordingly to Angleo et al. 2024 and Eriksson& Westersson 2001 and were qualified for further more invasive surgical treatment arthroscopy. [
17,
18] In this cohort, mean VAS level after completion of 6 cycles of arthrocentesis remained at level of mean 3.55±1.88 showing constant or moderate pain despite statistically significant VAS decrease from mean 6.55 ± 1.79. This cohort also exhibited worse MMO increase from mean 31,65 mm ± 7.8 mm to 37.1 ± 4.94 mm which gave mean 5.35± 6.07 mm of improvement. 76 patients were classified as “good” or “acceptable” treatment results (79,16%). In this cohort mean VAS of 1,46 ± 1.29 and mean MMO 41.67 ± 3.22 mm were reported at the endpoint of the study showing significant clinical improvement (suppl. Table 9).
4. Discussion
Arthrocentesis is a procedure performed to collect synovial fluid from joint spaces for the identification of a disease process or the relief of painful or bothersome symptoms.[
19] Arthrocentesis of the temporomandibular joints has been widely established as a tool in minimally- invasive treatment of joint disorders since its introduction by Nitzan et al. in 1991. [
9] The aim of a treatment is to reduce pain and increase mouth opening as these are the most morbid factors associated with temporomandibular disorders (TMDs). Currently, there are two main techniques established. One, originally described by Nitzan et al. (1991) where TMJ is lavaged through two- needle approach and second technique introduced by Sing & Varghese (2013) where single needle is applied. Both techniques have been compared with regards to decrease of pain and mouth opening increase. Also, until now different modifications and approaches has been reported by many authors so far including joint lavage techniques, volumes of the fluid used, application of different medications into the capsular space, amount of sessions and their intervals and more. Moreover, these studies are characterized by significant heterogeneity, bias in randomization, allocation concealment and blinding make the literature seems inconclusive. [
20,
21,
22,
23,
24,
25]
However, data pulled from recent extensive systematic reviews with meta-analysis showed that both techniques (single puncture or double- needle) provided comparable results in pain decrease and mouth opening increase. [
26,
27,
28]
Navaneetham et al. (2023) also indicated that since there were no statistically significant differences between single- or double- needle techniques in terms of clinical improvement, authors suggest using single- puncture approach due to shorter duration to perform, easier execution and less invasive than two- needle approach due to reduced risk of nerve damage. [
29]Similar observations were described in other study of Nagori et al. (2020) and Grossman& Poluha (2022). [
30,
31] In our study however, single- puncture technique provided better maximal mouth opening than two- needle technique. This could be a result of pressure- generated distension of the upper compartment of the TMJ and better impact of fluid- generated enlargement of the joint space, increased intra-articular pressure, removal of adhesions and adherences, and alterations to the synovial fluid viscosity. [
20]
Multiple sessions of arthrocentesis were proven to be more effective in clinical outcome in extensive systematic review by Guarda-Nardini et al. (2021). This was also confirmed within this study as gradual improvement between six consecutive monthly sessions was observed until the endpoint of the study. However, less than 25% remained as symptomatic and were referred for additional treatment such as arthroscopy which is consistent with congruent literature. [
20]
Basing on the results described within this article as well as recent updates in TMJ treatments concepts, arthrocentesis with or without injection of the medicine into the capsular space should be considered as soon as possible when conservative approach does show a clear benefit. It offers significant pain reduction and enables wider mouth opening in more than 70% of the patients with diagnosed OA or DD.
5. Conclusions
TMJ arthrocentesis is a nonarthroscopic lavage of the joint. It may be performed either by two- needle technique or single puncture approach. Both techniques are equally efficient in reduction of pain, however single- puncture approach proved to be more effective in increasing mouth opening. Multiple sessions of arthrocentesis are advised, as clinical improvement is not linear. Intracapsular injection of PRP or HA has similarly beneficial effect on pain reduction. In this study PRP appeared to be superior in increase of maximal mouth opening.
Author Contributions
Conceptualization, M.S. and R.P.; methodology, M.S.; software, R.P.; validation, Z.S. and R.P.; formal analysis, P.Z.; investigation, M.S.; resources, R.P.; data curation, Z.S.; writing—original draft preparation, M.S..; writing—review and editing, R.P.; visualization, R.P.; supervision, Z.S.; project administration, P.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by the Ethics Committee of the Warsaw Medical University, Warsaw, Poland; (ID KB/210.2020; date of approval: 14.12.2020) and was conducted in accordance with the Declaration of Helsinki of the World Medical Association concerning ethical procedures for medical studies involving human participants.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- D. Manfredini, “Etiopathogenesis of disk displacement of the temporomandibular joint: a review of the mechanisms,” Indian J Dent Res, vol. 20, no. 2, pp. 212–221, Apr. 2009. [CrossRef]
- R. L. Poluha, G. De La Torre Canales, Y. M. Costa, E. Grossmann, L. R. Bonjardim, and P. C. R. Conti, “Temporomandibular joint disc displacement with reduction: a review of mechanisms and clinical presentation,” Journal of Applied Oral Science, vol. 27, 2019. [CrossRef]
- C. Xu, X. Ren, P. Lin, S. Jin, and Z. Zhang, “Exploring the causal effects of sleep characteristics on TMD-related pain: a two-sample Mendelian randomization study,” Clin Oral Investig, vol. 28, no. 7, Jul. 2024. [CrossRef]
- A. Alshahrani et al., “The association between genetic factors and temporomandibular disorders: A systematic literature review,” Arch Oral Biol, vol. 166, p. 106032, Oct. 2024. [CrossRef]
- U. Yap, J. Lei, C. Liu, and K. Y. Fu, “Characteristics of painful temporomandibular disorders and their influence on jaw functional limitation and oral health-related quality of life,” J Oral Rehabil, vol. 51, no. 9, Sep. 2024. [CrossRef]
- H. Que, Q. Zhang, S. Xu, T. Chu, L. Xu, and Y. Wang, “Bi-directional two-sample Mendelian randomization identifies causal association of depression with temporomandibular disorders,” J Oral Rehabil, vol. 51, no. 9, Sep. 2024. [CrossRef]
- J. Warzocha, J. Gadomska-Krasny, and J. Mrowiec, “Etiologic Factors of Temporomandibular Disorders: A Systematic Review of Literature Containing Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) and Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) from 2018 to 2022,” Healthcare 2024, Vol. 12, Page 575, vol. 12, no. 5, p. 575, Feb. 2024. [CrossRef]
- Asadauskas, M. M. Luedi, R. D. Urman, and L. Andereggen, “Modern Approaches to the Treatment of Acute Facial Pain,” Curr Pain Headache Rep, vol. 28, no. 8, Aug. 2024. [CrossRef]
- D. W. Nitzan, M. Franklin Dolwick, and G. A. Martinez, “Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening,” J Oral Maxillofac Surg, vol. 49, no. 11, pp. 1163–1167, 1991. [CrossRef]
- S. Singh and D. Varghese, “Single puncture arthrocentesis of temporomandibular joint; introducing a novel device: A pilot study,” Natl J Maxillofac Surg, vol. 4, no. 2, p. 193, 2013. [CrossRef]
- K. I. Murakami, M. Matsuki, T. Iizuka, and T. Ono, “Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint,” Cranio, vol. 5, no. 1, p. 17, 1987. [CrossRef]
- G. B. Giraddi, A. Siddaraju, A. Kumar, and T. Jain, “Comparison Between Betamethasone and Sodium Hyaluronate Combination with Betamethasone Alone After Arthrocentesis in the Treatment of Internal Derangement of TMJ-Using Single Puncture Technique: A Preliminary Study,” J Maxillofac Oral Surg, vol. 14, no. 2, pp. 403–409, Jun. 2015. [CrossRef]
- E. H. Shinohara, S. C. Pardo-Kaba, M. Z. Martini, and F. K. Horikawa, “Single puncture for TMJ arthrocentesis: An effective technique for hydraulic distention of the superior joint space,” Natl J Maxillofac Surg, vol. 3, no. 1, p. 96, 2012. [CrossRef]
- Sharma, A. S. Rana, G. Jain, P. Kalra, D. Gupta, and S. Sharma, “Evaluation of efficacy of arthrocentesis (with normal saline) with or without sodium hyaluronate in treatment of internal derangement of TMJ – A prospective randomized study in 20 patients,” J Oral Biol Craniofac Res, vol. 3, no. 3, p. 112, Sep. 2013. [CrossRef]
- D. W. Nitzan, “Arthrocentesis--incentives for using this minimally invasive approach for temporomandibular disorders,” Oral Maxillofac Surg Clin North Am, vol. 18, no. 3, pp. 311–328, Aug. 2006. [CrossRef]
- J. P. McCain, “Arthroscopy of the human temporomandibular joint,” J Oral Maxillofac Surg, vol. 46, no. 8, pp. 648–655, 1988. [CrossRef]
- L. Eriksson and P. L. Westesson, “Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up,” J Oral Maxillofac Surg, vol. 59, no. 7, pp. 750–758, 2001. [CrossRef]
- D. F. Ângelo et al., “Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study,” J Clin Med, vol. 13, no. 3, Feb. 2024. [CrossRef]
- J. Houck, S. S. Patel, and B. K. Desai, “Arthrocentesis,” Atlas of Emergency Medicine Procedures, Second Edition, pp. 555–559, Jul. 2023,. [CrossRef]
- E. Grossmann, P. Guilherme Vargas Pasqual, R. L. Poluha, L. C. V. Iwaki, L. Iwaki Filho, and Ê. T. Setogutti, “Single-Needle Arthrocentesis with Upper Compartment Distension versus Conventional Two-Needle Arthrocentesis: Randomized Clinical Trial,” Pain Res Manag, vol. 2017, 2017. [CrossRef]
- C. W. Kim et al., “Effect of arthrocentesis on the clinical outcome of various treatment methods for temporomandibular joint disorders,” Maxillofac Plast Reconstr Surg, vol. 41, no. 1, Dec. 2019. [CrossRef]
- M. Santagata et al., “Arthrocentesis and sodium hyaluronate infiltration in temporomandibular disorders treatment. Clinical and MRI evaluation,” J Funct Morphol Kinesiol, vol. 5, no. 1, 2020. [CrossRef]
- R. Rossini, E. Grossmann, R. L. Poluha, Ê. T. Setogutti, and M. F. Dos Santos, “Double-Needle Arthrocentesis with Viscosupplementation in Patients with Temporomandibular Joint Disc Displacement without Reduction,” Clinics, vol. 76, 2021. [CrossRef]
- J. Sequeira, B. H. S. Rao, and P. R. Kedia, “Efficacy of Sodium Hyaluronate for Temporomandibular Joint Disorder by Single-Puncture Arthrocentesis,” J Maxillofac Oral Surg, vol. 18, no. 1, p. 88, Mar. 2019. [CrossRef]
- J. L. G. C. Monteiro, J. A. Almeida de Arruda, E. Dias de Oliveira e Silva, and B. Cavalcanti do Egito Vasconcelos, “Is Single-Puncture TMJ Arthrocentesis Superior to the Double-Puncture Technique for the Improvement of Outcomes in Patients With TMDs?,” J Oral Maxillofac Surg, vol. 78, no. 8, pp. 1319.e1-1319.e15, Aug. 2020. [CrossRef]
- M. Siewert-Gutowska, R. Pokrowiecki, A. Kamiński, P. Zawadzki, and Z. Stopa, “State of the Art in Temporomandibular Joint Arthrocentesis—A Systematic Review,” J Clin Med, vol. 12, no. 13, p. 4439, Jul. 2023. [CrossRef]
- L. Guarda-Nardini, A. De Almeida, and D. Manfredini, “Arthrocentesis of the Temporomandibular Joint: Systematic Review and Clinical Implications of Research Findings,” J Oral Facial Pain Headache, vol. 35, no. 1, pp. 17–29, Feb. 2021. [CrossRef]
- S. A. Nagori, S. K. Roy Chowdhury, H. Thukral, A. Jose, and A. Roychoudhury, “Single puncture versus standard double needle arthrocentesis for the management of temporomandibular joint disorders: A systematic review,” J Oral Rehabil, vol. 45, no. 10, pp. 810–818, Oct. 2018,. [CrossRef]
- R. Navaneetham, A. Navaneetham, V. Nagaraj, N. Gnapika, and G. Sankarnarayan, “Single-Puncture Versus Double-Puncture Technique Arthrocentesis in the Treatment of Internal Derangement of TM Joint-A Comparative Clinical Study,” J Maxillofac Oral Surg, vol. 22, no. 4, pp. 1060–1065, Dec. 2023. [CrossRef]
- S. A. Nagori, A. Jose, and A. Roychoudhury, “Comparison of intraoperative outcomes with single and double puncture techniques of arthrocentesis of the temporomandibular joint,” Br J Oral Maxillofac Surg, vol. 58, no. 8, pp. 928–932, Oct. 2020. [CrossRef]
- E. Grossmann and R. L. Poluha, “Double-Puncture Versus Single-Puncture Arthrocentesis: A Randomized Controlled Trial with 3 Years of Follow-Up,” J Oral Facial Pain Headache, vol. 36, no. 2, pp. 141–146, May 2022. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).