1. Introduction
Transesophageal echocardiography (TEE) is an invaluable diagnostic tool for structural heart diseases, offering high-quality images suitable for routine echocardiographic examinations [
1,
2,
3]. Its significance extends to transcatheter interventions, where it plays a pivotal role from pre-operative planning to intra-operative guidance and final result assessment [
4,
5,
6,
7]. Effective collaboration between the imager and interventionist is crucial, with real-time demonstration of procedural steps facilitated by two and three-dimensional (3D) echocardiographic images [
8,
9]. Notably, 3D echocardiography enables precise device sizing, exhibiting a strong correlation with other imaging modalities such as cardiac computed tomography (CT) [
10].
Despite the generally favorable safety profile of adult TEE probes, they may cause minimal complications, including oropharyngeal trauma, esophageal lesions, and post-examination symptoms such as throat hoarseness or chest pain [
11,
12,
13]. These complications are related to the thickness of the adult TEE probe, the manipulations of the probe during the examination, and probe-generated heat. The standard adult TEE probes are often poorly tolerated in non-sedated patients, limiting their prolonged use. While routine TEE examinations typically last 10-15 minutes and do not necessitate deep sedation, transcatheter interventions last longer, necessitating general anesthesia (GA) as standard practice in order to mitigate patient discomfort. However, GA requires the presence of an anesthesiologist and results in extended procedural and hospitalization times, along with an increased risk of anesthesia-related complications.
Intracardiac echocardiography (ICE) is as a potential solution to the limitations of adult TEE probes [
14]. However, ICE is an invasive tool requiring additional venous access and has additional substantial costs. Another alternative, the Micro-TEE probe (10T-D GE Healthcare), lacks support for three-dimensional imaging, which is imperative for most transcatheter procedures [
15,
16,
17].
The objective of this study is to assess the feasibility of employing the new 4D mini-TEE probe for both routine examinations and guidance of transcatheter procedures, while evaluating the quality of the obtained images.
2. Materials and Methods
This is a multi-center prospective registry that assessed the feasibility of (1) using the 4D mini-TEE probe in everyday practice and (2) guiding transcatheter interventions. Our cohort consisted of 30 consecutive patients who either visited the echocardiography department or were scheduled for a transcatheter procedure. Interbalkan Medical center and the University Hospital of Rennes participated in the study and the registry was approved by their local ethics and scientific committees. All TEE examinations were conducted by experienced imaging specialists with the new 9VT-D, 4D mini-TEE probe that has recently been commercially available. All examinations were done with the Vivid E95 machine and were stored and post-processed in EchoPAC workstations. Standard 2D/4D examination protocols were acquired for complete assessment of the patients, for pre-operative planning and intra-operative guidance. For qualitative assessment of the images, a 5-point score was used (1-non-interpretable images, 2-poor quality but interpretable, 3-average quality, 4-good quality, 5-excellent quality) that was answered immediately after the end of the TEE.
Comparison between mini-TEE and standard adult TEE probe
To assess the image quality of the mini-TEE probe and ensure the accuracy of findings, a limited number of patients were selected for examination using both the adult 6VT-D and pediatric mini-TEE 9VT-D probes. Prior to the examination, patients were duly informed about the procedure and provided their consent. The protocol dictated the initial examination with the adult probe followed by the insertion and utilization of the pediatric probe to capture identical images. To increase patient comfort during probe insertion, mild sedation with midazolam and local application of lidocaine to the oropharynx were administered.
Echocardiography department transesophageal echocardiography
For routine TEE examinations, the anesthesia protocol comprised the local application of lidocaine at the posterior oropharynx, coupled, for some, with minimal sedation using 1-2mg of midazolam to ensure patients remained calm yet awake throughout the procedure. In instances where patients exhibited intolerance to the probe, higher doses of midazolam (5-10mg) were administered based on individual response levels.
Probe insertion into the esophagus involved the utilization of an endocavity probe-cover coated with lubricant gel at the tip, aiming to preventing artifacts from partial attachment of the mini probe to the esophageal wall. To assess probe tolerance, a 5-point scoring system was employed, with patients completing a questionnaire following the examination. Scores ranged from 1 (indicating probe intolerance necessitating termination of the examination) to 5 (signifying no discomfort experienced during or after the TEE procedure). (1-non-tolerable probe/termination of examination, 2-major discomfort during TEE, 3-major discomfort immediately after TEE with chest pain/bleeding, 4-minor discomfort, 5-no discomfort during or post-TEE).
Intra-procedural transesophageal echocardiography
For transcatheter procedures, the preferred approach involved sedation without the need for general anesthesia or intubation. This decision was contingent upon factors such as the duration of the procedure, patient tolerance of the probe, and their ability to remain still during the operation, thereby assisting the interventionist in completing the procedure effectively. During the insertion of the probe into the esophagus for transcatheter procedures, an endocavity probe-cover coated with lubricant gel was once again utilized. Unlike routine TEE examinations where patients typically lie in the decubitus position, for transcatheter procedures, all patients were positioned supinely to facilitate probe insertion. Probe tolerance was assessed at the conclusion of the procedure through a straightforward inquiry regarding the patient’s level of cooperation or necessity for intubation.
3. Results
Comparison between mini-TEE and standard adult TEE probe
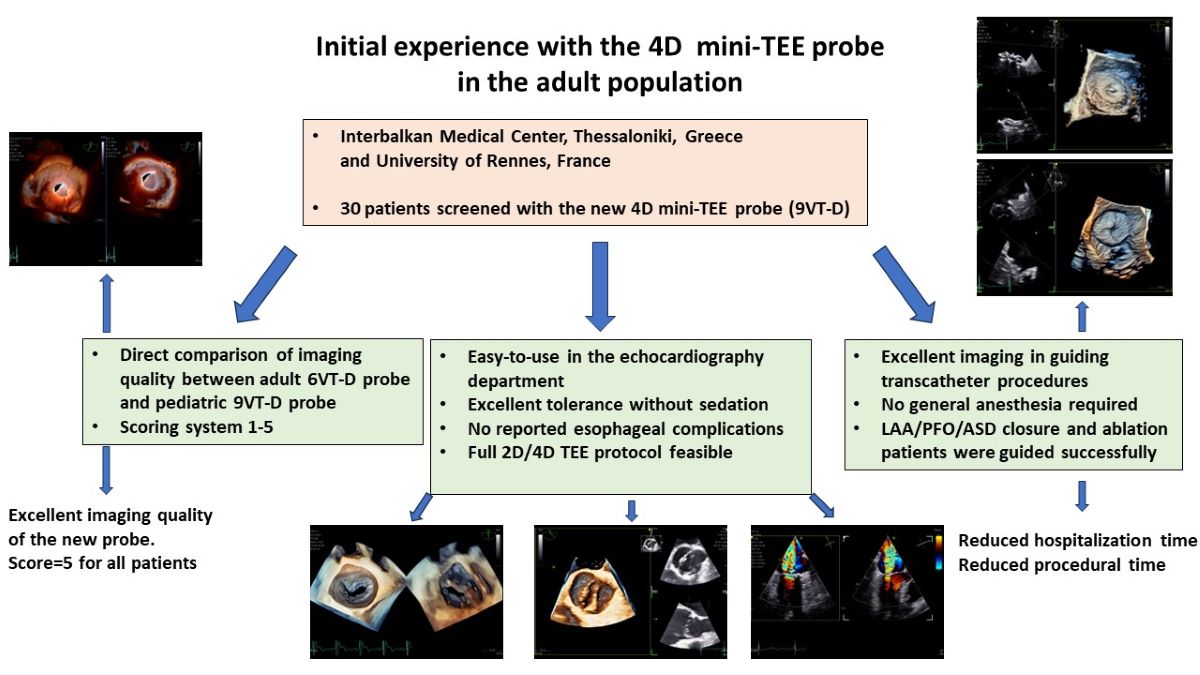
The quality of images obtained with the 9VT-D pediatric probe and the accuracy of findings were assessed through examination of the first three patients. Each patient underwent a comprehensive TEE protocol using both the pediatric 9VT-D and adult 6VT-D probes, allowing for direct comparison of findings and image quality. Throughout the procedure, patients received local oropharyngeal lidocaine and mild sedation with midazolam to ensure tolerance.
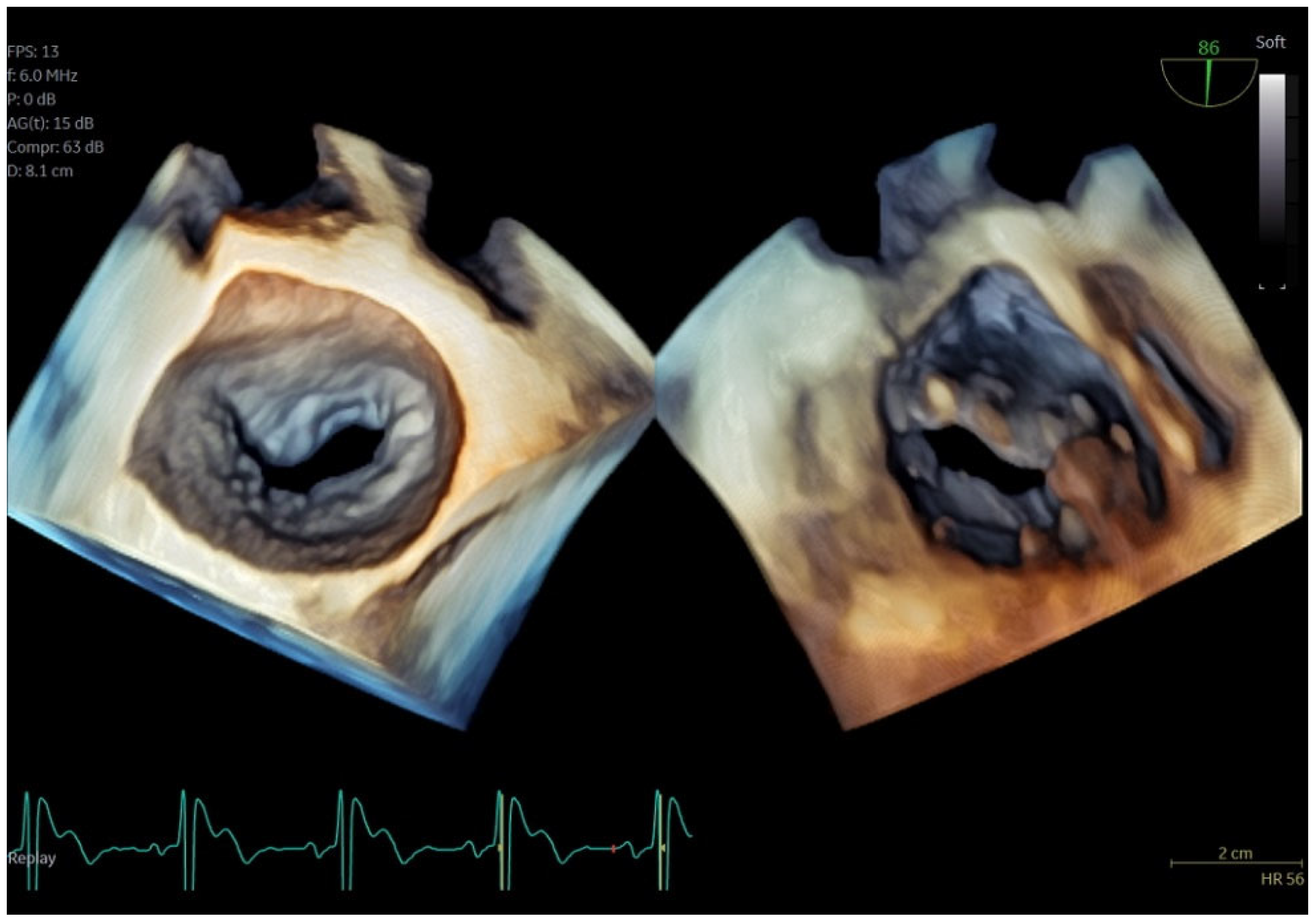
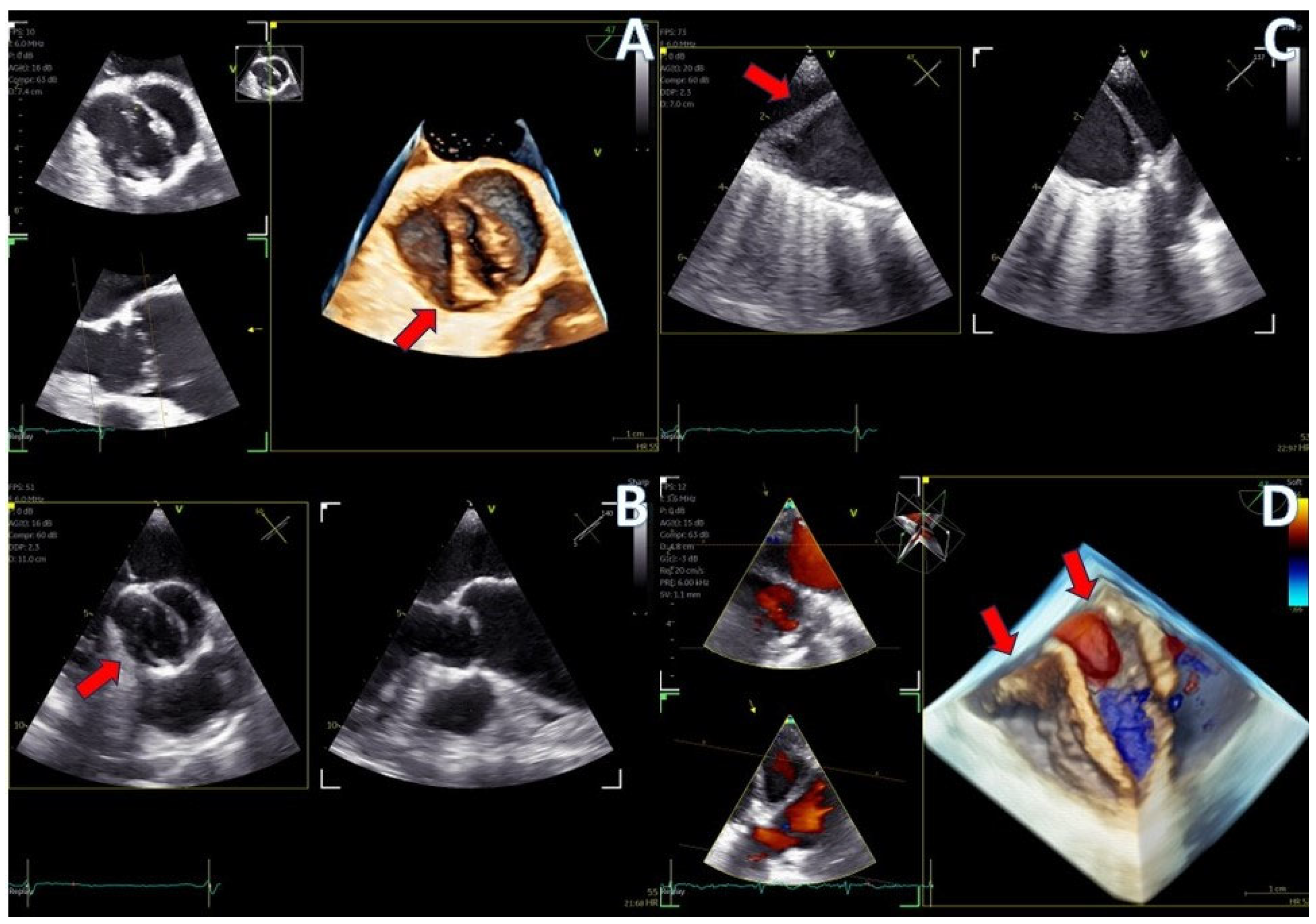
The adult probe was initially inserted for complete 2D/4D image acquisition, followed by the insertion of the pediatric probe while the patient remained under sedation. Remarkably, insertion of the pediatric probe was effortless in all cases, requiring no additional sedation. Despite encountering challenging diagnostic scenarios in all three cases (1st patient: combined severe aortic stenosis and severe mitral regurgitation (MR) due to P1 scallop prolapse, 2nd patient: malfunction of metallic mitral valve prosthesis with an occluded disk, 3rd patient: bioprosthetic aortic valve with paravalvular leak and significant MR in previously MV repair with a complete ring), the pediatric probe consistently provided high-quality images comparable to those obtained with the standard adult probe (
Figure 1 and
Figure 2). Notably, there was no compromise in 2D and 4D spatial and temporal resolution, with only minor differences observed compared to the adult 6VT-D probe. Evaluation using the 5-point scoring system consistently yielded a score of 5 for all three cases, indicating excellent image quality.
Figure 1.
Direct comparison of 3D volume-rendered “en face” images of a metallic prosthetic mitral valve with occluded disk. Left image corresponds to 6VT-D adult probe and right image corresponds to 9VT-D pediatric probe.
Figure 1.
Direct comparison of 3D volume-rendered “en face” images of a metallic prosthetic mitral valve with occluded disk. Left image corresponds to 6VT-D adult probe and right image corresponds to 9VT-D pediatric probe.
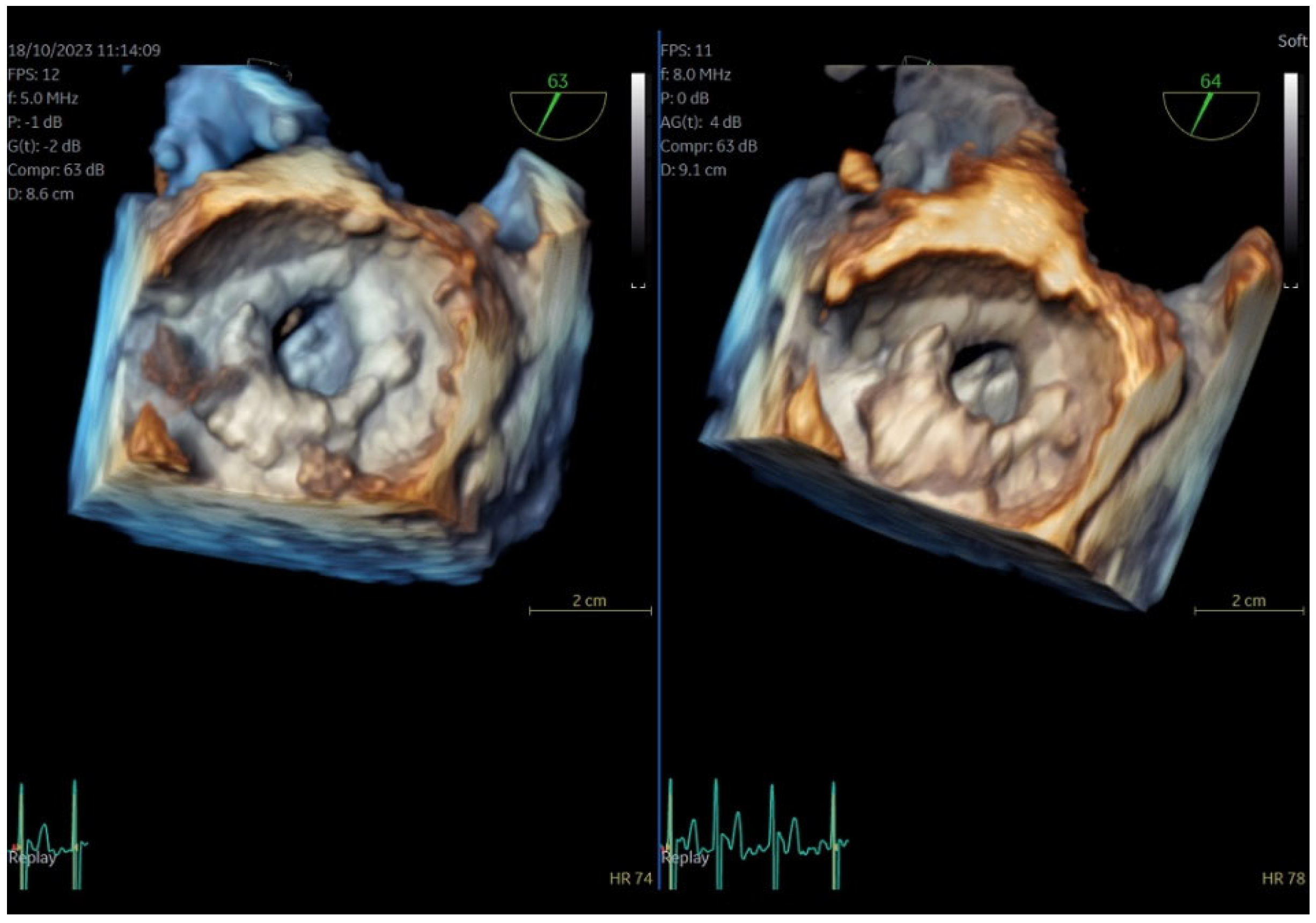
Figure 2.
Direct comparison of 3D volume-rendered “en face” images of a metallic prosthetic mitral valve with occluded disk. Left image corresponds to 6VT-D adult probe and right image corresponds to 9VT-D pediatric probe. Images enhanced with “photorealistic method” with Flexilight application (GE Healthcare).
Figure 2.
Direct comparison of 3D volume-rendered “en face” images of a metallic prosthetic mitral valve with occluded disk. Left image corresponds to 6VT-D adult probe and right image corresponds to 9VT-D pediatric probe. Images enhanced with “photorealistic method” with Flexilight application (GE Healthcare).
Echocardiography department transesophageal echocardiography
Following the initial comparison between the pediatric and adult probes, where confidence in the accuracy of the 9VT-D probe was established, the rest of the consecutive patients underwent the TEE protocol solely with the pediatric probe. Most patients received local anesthesia of the posterior pharynx with lidocaine and a few of them minimal doses of midazolam (1-2mg) to ensure they remained cooperative throughout the procedure. With the exception of one patient who experienced intense pharyngeal reflex and required sedation with 5mg of midazolam, all patients tolerated the mini-TEE probe well.
Our initial experience further showed that left lateral decubitus position was suboptimal for the introduction of the probe. The introduction was much easier in patients in the sitting position that were asked to swallow the probe by themselves with a very limited implication of the physician or the nurse. Local anesthesia could also be unnecessary for a significant number of patients.
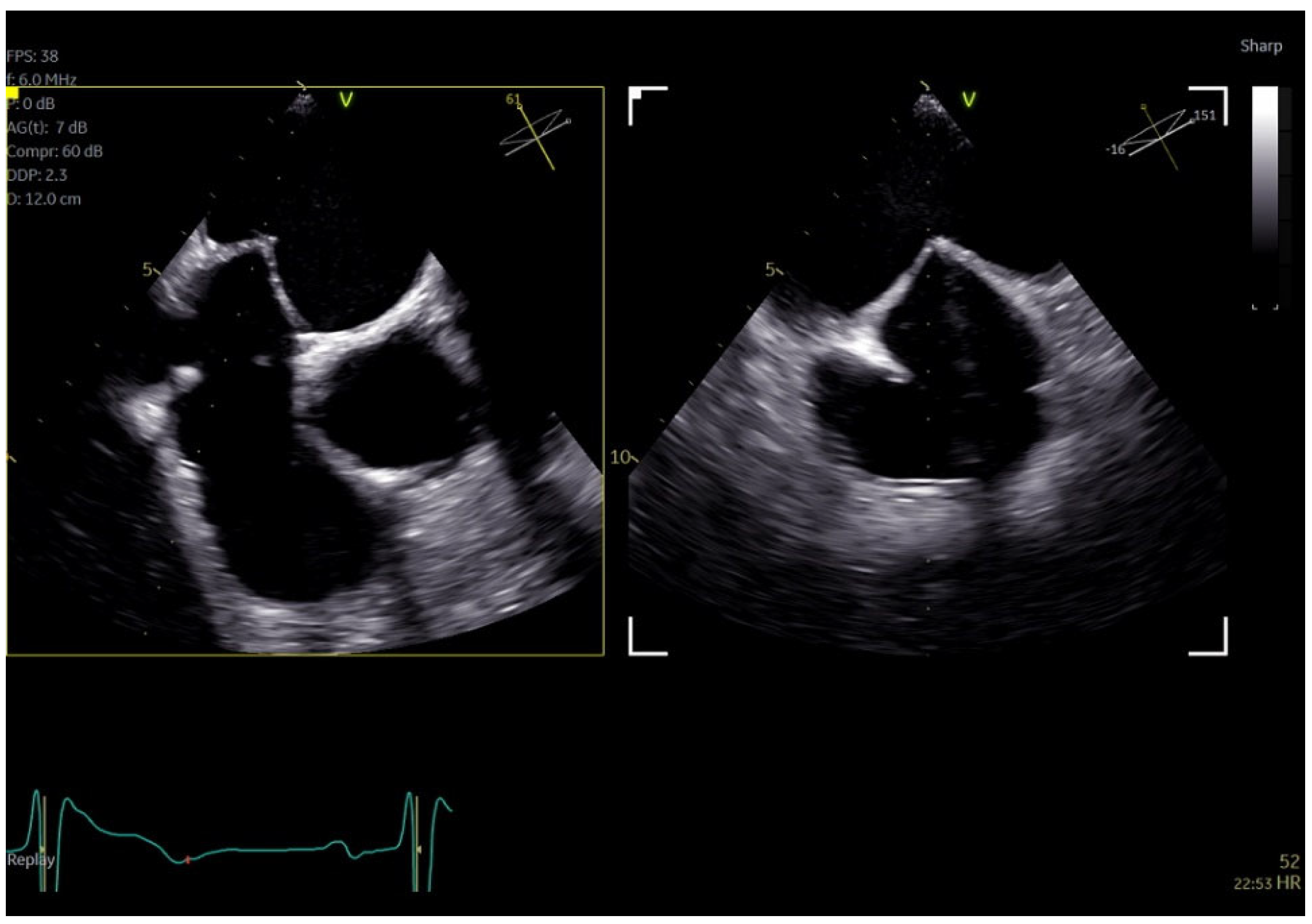
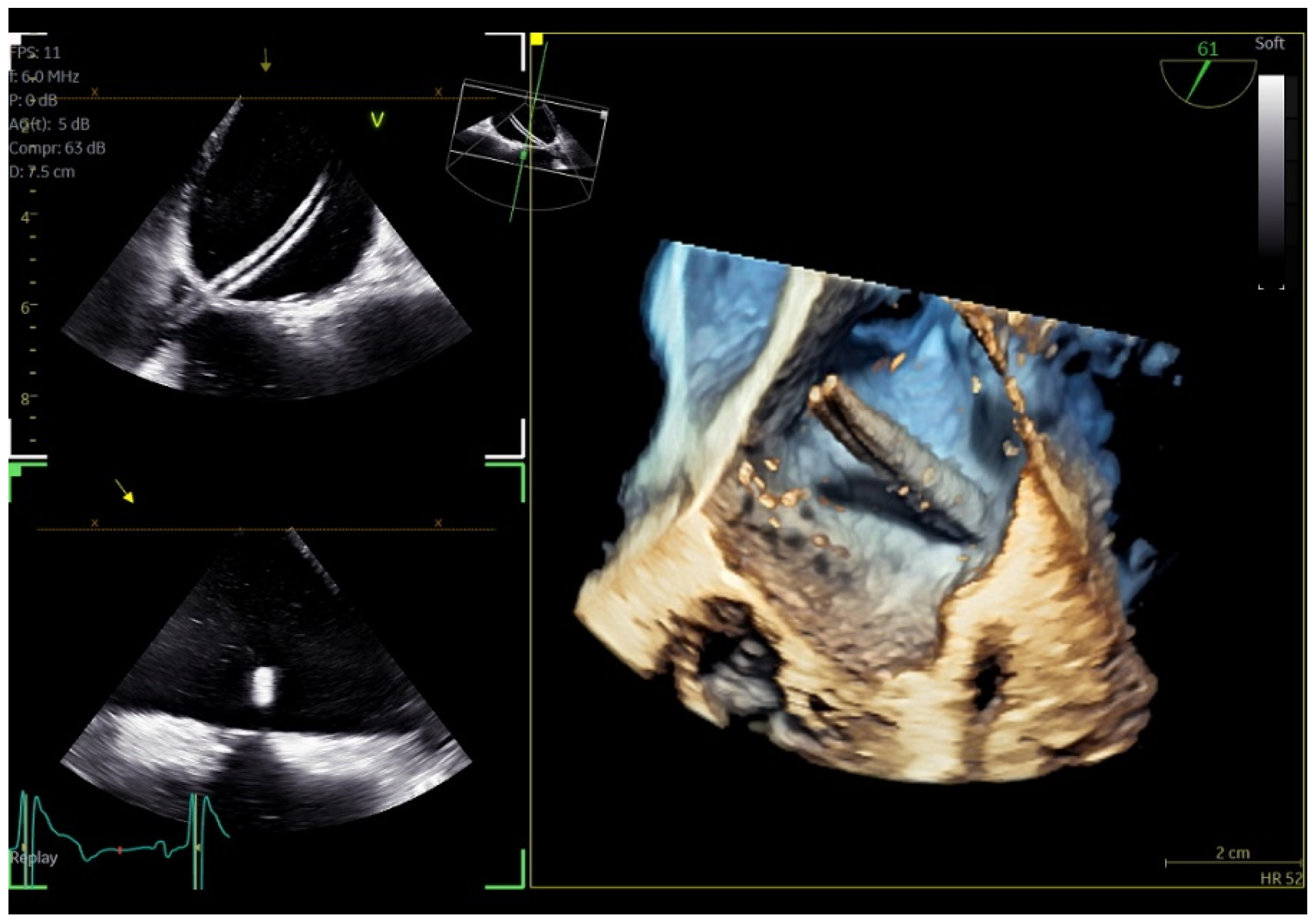
Regarding imaging quality, all patients exhibited excellent images without any compromise in resolution, obviating the need to confirm findings using the standard TEE probe (
Figure 3 and
Figure 4). Despite the one patient requiring additional sedation due to intense pharyngeal reflex, the quality of images obtained remained consistent across all cases.
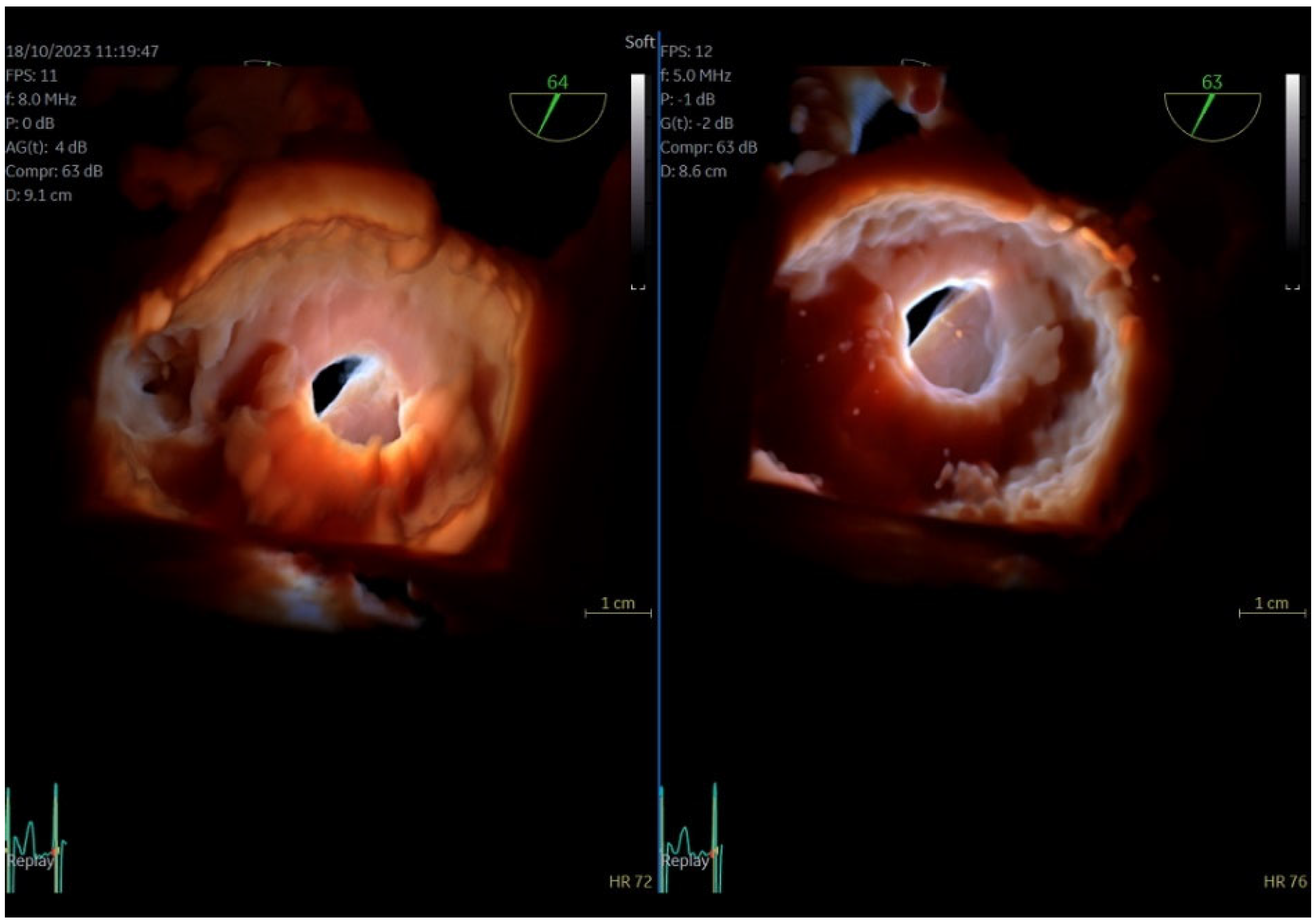
Figure 3.
Dual crop 3D volume-rendered atrial (left) and ventricular (right) views of normal mitral valve.
Figure 3.
Dual crop 3D volume-rendered atrial (left) and ventricular (right) views of normal mitral valve.
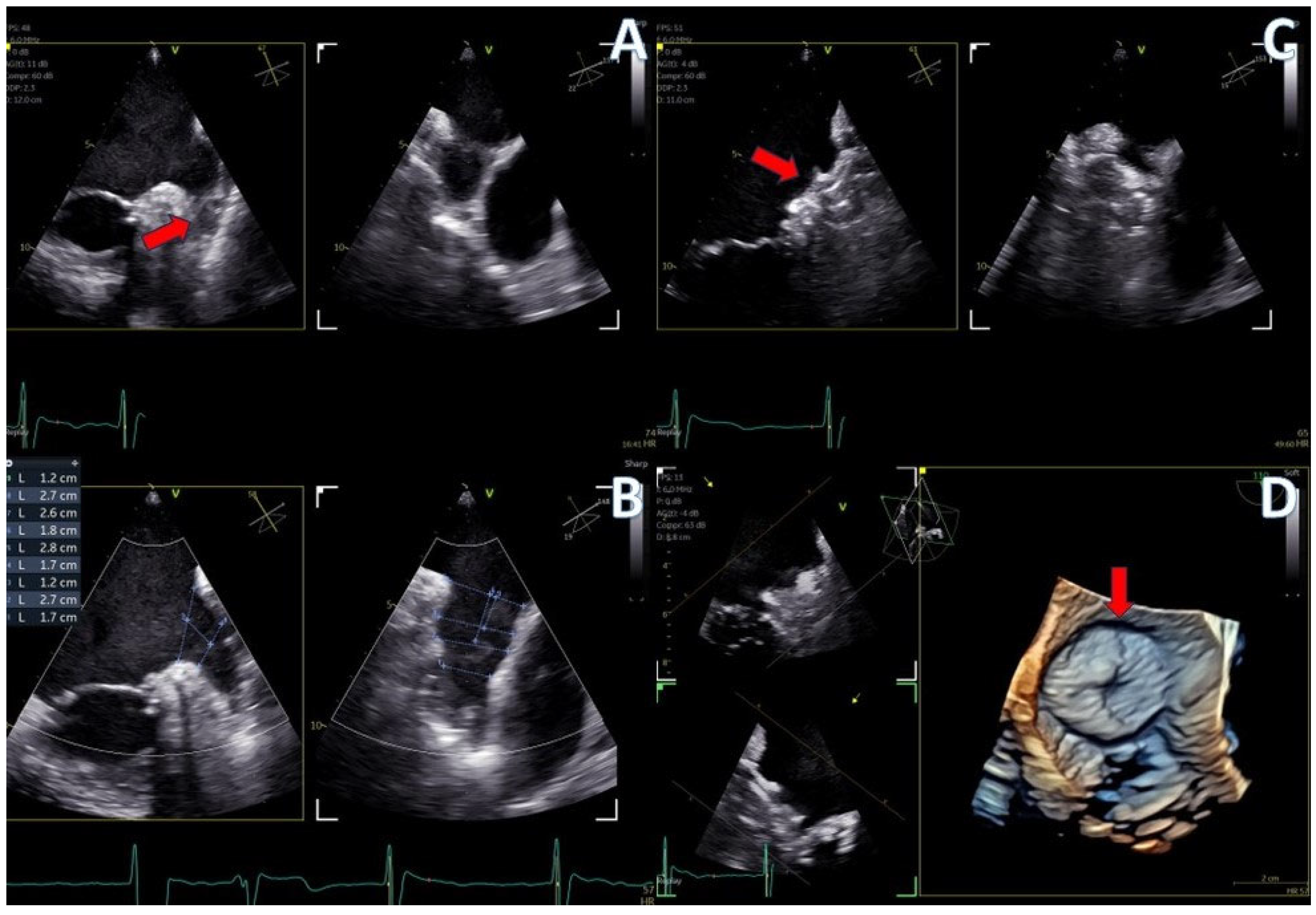
Figure 4.
A) 4D demonstration of a true-bicuspid aortic valve (red arrow), B) Biplane 2D demonstration of a true-bicuspid aortic valve (red arrow), C) Chronic dissection of descending aorta, (red arrow showing the wall of the true lumen), D) 3D volume rendered color doppler image showing the true (right arrow) and the false lumen (left arrow).
Figure 4.
A) 4D demonstration of a true-bicuspid aortic valve (red arrow), B) Biplane 2D demonstration of a true-bicuspid aortic valve (red arrow), C) Chronic dissection of descending aorta, (red arrow showing the wall of the true lumen), D) 3D volume rendered color doppler image showing the true (right arrow) and the false lumen (left arrow).
Intra-procedural transesophageal echocardiography
The new 4D mini-TEE probe was utilized in 8 consecutive patients undergoing transcatheter procedures at our clinic. Among them, 4 patients underwent cryo-ablation for atrial fibrillation, 2 underwent patent foramen ovale (PFO) closure, 1 underwent atrial septal defect (ASD ostium secundum) closure, and 1 underwent left atrial appendage (LAA) closure.
Despite the protocol recommending minimal sedation and avoidance of intubation, two of the “ablation” patients were unable to tolerate the probe, necessitating intubation and administration of general anesthesia. Additionally, the patient scheduled for LAA closure required general anesthesia due to the detection of thrombus formation at the distal part of the appendage at the onset of the procedure, posing safety concerns for the interventionist. The decision to proceed under general anesthesia was made to minimize risk and ensure patient safety. Conversely, the remaining “ablation” patients, as well as those undergoing ASD and PFO closure, tolerated the mini-TEE probe well and completed the intervention with mild sedation only. The average duration of probe insertion into the esophagus for all procedures was 29 minutes (range 20-32min). None of the patients reported post-operative discomfort, and no esophageal trauma was observed. The anesthesiologist noted that while it was easier to awaken patients who did not receive general anesthesia, maintaining sufficient sedation for the duration of the procedure was more demanding. Despite the challenges encountered, there were no anesthesia-related complications, and all patients adhered to the standard 24-hour post-procedural hospitalization protocol. However, same-day discharge could be considered for patients who do not require intubation, offering an attractive and cost-effective option.
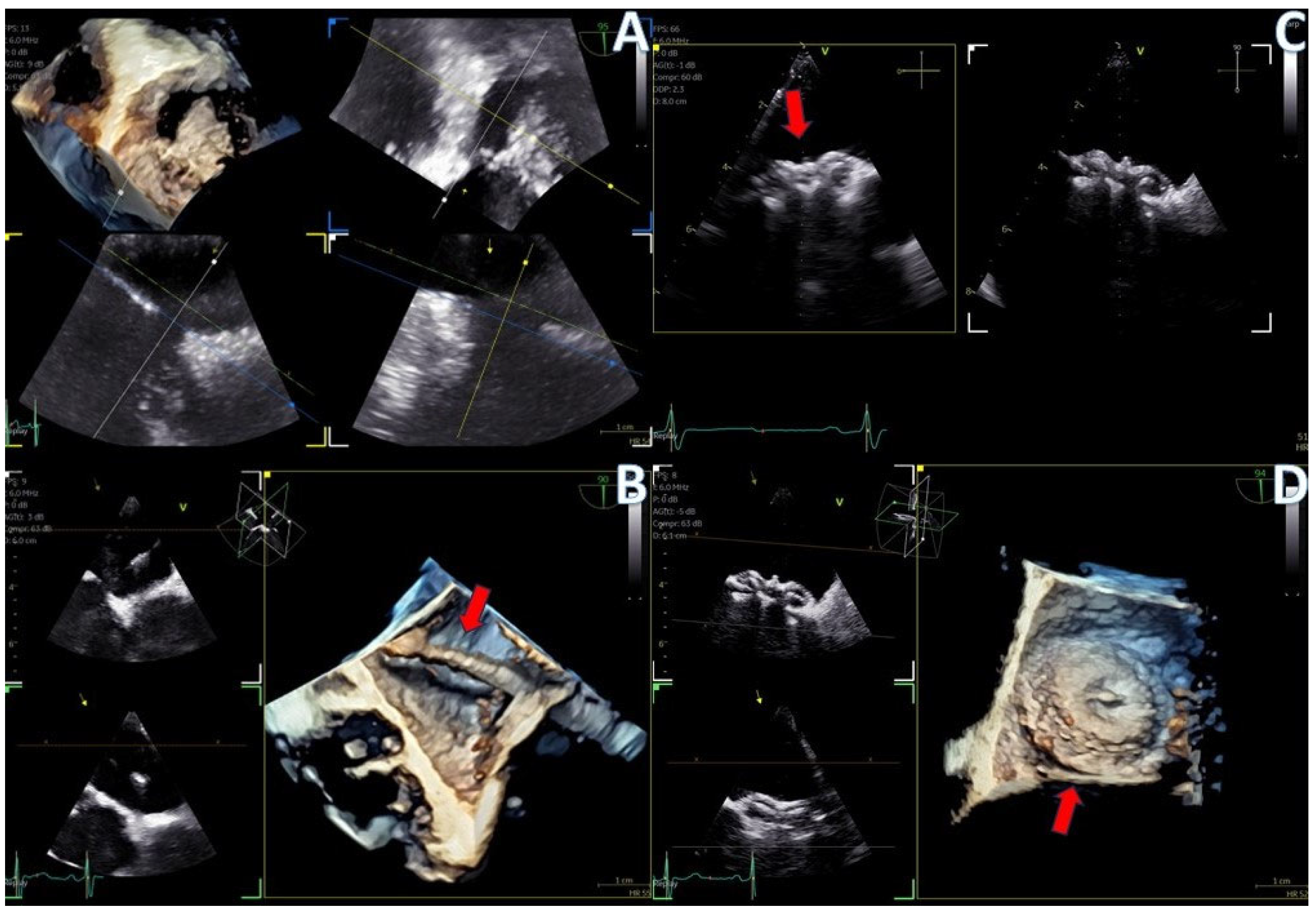
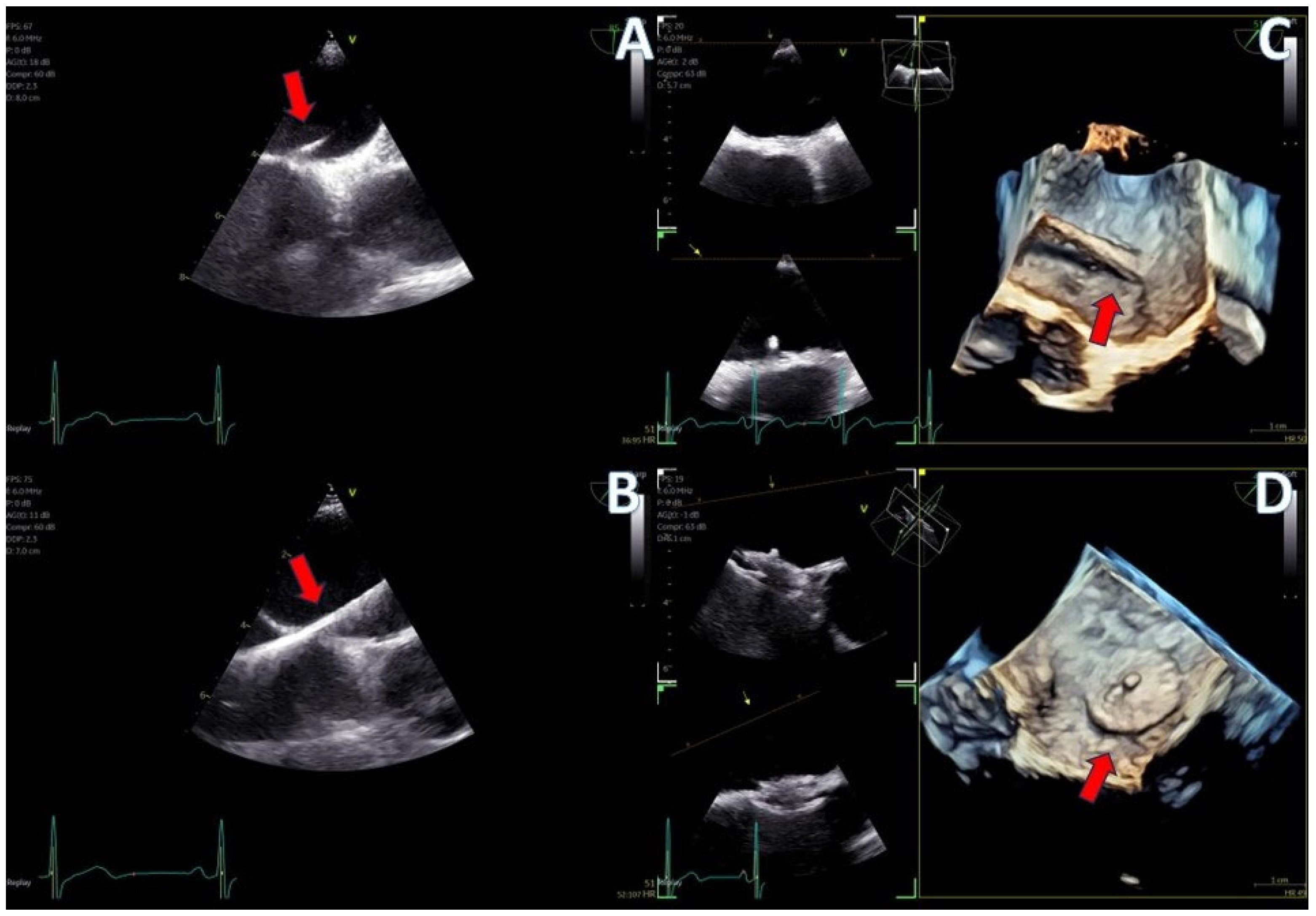
The imaging capabilities of the 4D mini-TEE probe were consistently excellent across all procedures (
Figure 5,
Figure 6,
Figure 7,
Figure 8 and
Figure 9). Trans-septal puncture in ablation cases was facilitated by bi-plane imaging (
Figure 5), demonstrating a nice tending of the septum. For the guidance of wires to the pulmonary veins, both 2D and 4D volume-rendered images were utilized (
Figure 5 and
Figure 6), expediting the procedure. The TEE probe was removed after the insertion of the cryo-ablation catheter into the LA.
In the case of LAA closure (
Figure 8), 3D tools (MPR-flexislice) aided in accurate sizing of the ostium and the landing zone (important for AMULET device), particularly in the presence of distal thrombus where contrast infusion was contraindicated. The final result was satisfactory, with no leakage observed and a stable device placement confirmed with a tug test.
PFO closure cases (
Figure 9) benefited from the probe’s excellent imaging, enabling precise wire insertion and providing anatomical criteria for device sizing. Bubbles study was performed at the beginning and at the end of the procedure for any remaining shunt. The stability of the device was confirmed with a wiggle test. Similarly, in the ASD case (
Figure 7), the probe facilitated visualization of all defect rims, accurate sizing of the oval-shaped defect (with MPR) confirmed with balloon sizing and stop-flow technique and ensured a successful outcome with no residual shunt observed.
Overall, the 4D mini-TEE probe demonstrated exceptional imaging capabilities and played a pivotal role in guiding transcatheter interventions with precision and efficacy.
4. Discussion
Our study represents a pioneering effort in evaluating the new 4D mini-TEE probe (9VT-D GE Healthcare) across diverse patient populations, encompassing both routine TEE examinations and transcatheter procedures. Dr. Sanchis et al. have recently published their experience with this particular probe in a small number of LAA occlusion cases with excellent feedback in terms of patient’s tolerance and imaging quality [
18]. While previous studies have included procedures using miniaturized TEE probes [
15,
16,
17,
19,
20], ours is unique by the fact that this is the first commercially available probe boasting full 3D options and capable of supporting all TEE examinations and transcatheter procedures. The added value of 3D echocardiography lies in its capacity for precise device sizing and improved comprehension of cardiac anatomy. Notably, bi-plane imaging facilitates trans-septal puncture, thereby reducing procedural time. Multi-planar reconstruction (Flexislice method) serves as a vital tool for sizing in cases such as secundum ASDs and LAAs, where precise structural dimensions are imperative [
4].
Traditionally, the standard practice has involved the use of adult, thick, and rigid probes for all TEE examinations. While these probes offer comprehensive 2D and 3D applications and possess an overall safe profile, they are frequently associated with esophageal lesions and patient discomfort due to probe manipulation and heat generation [
11,
12,
13]. In routine TEE examinations, mild sedation is sometimes employed to enhance probe tolerance, whereas, in transcatheter interventions, general anesthesia and intubation are commonly utilized due to the poor tolerance of the adult thick probe and the longer duration of these procedures.
Our study demonstrates that the new 4D mini-TEE 9VT-D probe effectively addresses the limitations of the adult TEE probe. The introduction of the probe requires less effort, especially in non-sedated patients that are asked to swallow it, under the physician’s supervision. The role of the physician continues with the manipulation of the probe with the patient lying down on a left decubitus position. Direct comparison of images between the pediatric and adult probes confirmed the exceptional imaging quality achievable with the mini probe. The inclusion of 3D tools facilitates both routine examinations and transcatheter interventions, rendering this probe superior to previous mini-TEE/micro-TEE 2D probes and intracardiac echocardiography (ICE). While ICE may emerge as an attractive alternative option in the future, its current limitations in terms of cost and image resolution preclude it from matching the 3D imaging capabilities of the 9VT-D probe [
14].
Moreover, the thin and flexible nature of the 9VT-D probe ensures good tolerability even in non-sedated patients, enabling routine TEE examinations to proceed potentially without local anesthesia. It is probably a tool that will become necessary for large tertiary centers where frail patients are often referred for diagnosis that could be accessible to a percutaneous treatment. The greatest benefit is observed in transcatheter procedures, where the full array of 3D options can be leveraged without requiring intubation and general anesthesia. This results in reduced procedural time, avoidance of anesthesia-related complications, and the potential for same-day discharge, particularly advantageous for high-surgical-risk patients undergoing transcatheter procedures. Notably, our study revealed no complications from the esophagus or the administered anesthesia.
In summary, our study underscores the remarkable clinical utility and patient benefits afforded by the 4D mini-TEE 9VT-D probe, positioning it as a valuable tool in contemporary echocardiography practice, particularly in the era of transcatheter interventions.
Limitations
While our experience with the mini-TEE probe in routine practice has generally been favorable, there are certain issues that warrant mention. Unlike the standard adult probe, which is thick and rigid, facilitating its advancement through the tongue and posterior pharynx, the mini-TEE probe is thin and flexible. This can result in instances where the probe curls into the oral cavity, resembling a naso-gastric Levin tube. In one intubated patient, the anesthesiologist had to utilize a laryngoscope to aid in probe insertion into the esophagus. Additionally, in one awake patient who exhibited poor tolerance to the probe, standard doses of sedation were necessary to complete the examination.
Another limitation is the current cost of the mini-TEE probe which is 1.5 times higher than the standard adult 4D probe (6VT-D). Our pilot experience provides convincing evidence in favor of the use of the mini-TEE despite its higher cost. Future studies will have to further investigate the clinical advantages and the long-term benefits of this adult probe by targeting a larger population
5. Conclusions
The introduction of the new 4D mini-TEE probe represents a significant advancement in echocardiography, offering excellent imaging capabilities and encompassing all the essential 2D/4D options required for a comprehensive TEE protocol and guidance of transcatheter interventions. Notably, the utilization of this probe might lead to a reduction in esophageal and anesthesia-related complications. Further validations are needed.
Our initial experience with the mini-TEE probe has been satisfying and holds promise for even further improvements in future iterations of such probes. The potential for enhanced versions of mini-TEE probes in the future presents exciting opportunities for continued advancement in cardiac imaging and intervention.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1,
Video S1: atrial septal defect closure case,
Video S2: patent foramen ovale closure case,
Video S3: left atrial appendage closure case,
Video S4: Metallic mitral valve assessment,
Video S5: Bicuspid aortic valve with chronic descending aortic dissection.
Author Contributions
Conceptualization, K.P., I.I., E.D.; methodology, K.P., I.I., O.O.K., M.V., E.D.; formal analysis, K.P., I.I., A.T., E.D.; investigation, K.P., A.C., A.T., N.F., A.A.; writing—original draft preparation, K.P., A.C., O.O.K., A.T., N.F., A.A., M.A., E.D.; writing—review and editing, K.P., I.I., A.C., O.O.K., A.T., N.F., M.V., E.D.; supervision, K.P., E.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of INTERBALKAN MEDICAL CENTER (protocol code 2338, 11th of September 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data supporting this article are available upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964. [CrossRef]
- Nicoara A, Skubas N, Ad N, et al. Guidelines for the Use of Transesophageal Echocardiography to Assist with Surgical Decision-Making in the Operating Room: A Surgery-Based Approach: From the American Society of Echocardiography in Collaboration with the Society of Cardiovascular Anesthesiologists and the Society of Thoracic Surgeons [published correction appears in J Am Soc Echocardiogr. 2020 Nov;33(11):1426]. J Am Soc Echocardiogr. 2020;33(6):692-734. [CrossRef]
- Papadopoulos CH, Kadoglou NPE, Theodosis-Georgilas A, et al. Practical guidance and clinical applications of transoesophageal echocardiography. A position paper of the working group of echocardiography of the Hellenic Society of Cardiology. Curr Probl Cardiol. 2024;49(8):102634. [CrossRef]
- Faletra FF, Saric M, Saw J, Lempereur M, Hanke T, Vannan MA. Imaging for Patient’s Selection and Guidance of LAA and ASD Percutaneous and Surgical Closure. JACC Cardiovasc Imaging. 2021;14(1):3-21. [CrossRef]
- Silvestry FE, Rodriguez LL, Herrmann HC, et al. Echocardiographic guidance and assessment of percutaneous repair for mitral regurgitation with the Evalve MitraClip: lessons learned from EVEREST I. J Am Soc Echocardiogr. 2007;20(10):1131-1140. [CrossRef]
- Khalique OK, Hahn RT. Role of Echocardiography in Transcatheter Valvular Heart Disease Interventions. Curr Cardiol Rep. 2017;19(12):128. Published 2017 Oct 27. [CrossRef]
- Papadopoulos CH, Kadoglou NPE, Theodosis-Georgilas A, et al. Transoesophageal echocardiography beyond the echo-laboratory. An expert consensus paper of the working group of echocardiography of the hellenic society of cardiology. Hellenic J Cardiol. Published online June 18, 2024. [CrossRef]
- Bushari LI, Reeder GS, Eleid MF, et al. Percutaneous Transcatheter Edge-to-Edge MitraClip Technique: A Practical “Step-by-Step” 3-Dimensional Transesophageal Echocardiography Guide. Mayo Clin Proc. 2019;94(1):89-102. [CrossRef]
- Lang RM, Tsang W, Weinert L, Mor-Avi V, Chandra S. Valvular heart disease. The value of 3-dimensional echocardiography. J Am Coll Cardiol. 2011;58(19):1933-1944. [CrossRef]
- Coisne A, Pontana F, Aghezzaf S, et al. Utility of Three-Dimensional Transesophageal Echocardiography for Mitral Annular Sizing in Transcatheter Mitral Valve Replacement Procedures: A Cardiac Computed Tomographic Comparative Study. J Am Soc Echocardiogr. 2020;33(10):1245-1252.e2. [CrossRef]
- O’Shea JP, Southern JF, D’Ambra MN, et al. Effects of prolonged transesophageal echocardiographic imaging and probe manipulation on the esophagus--an echocardiographic-pathologic study. J Am Coll Cardiol. 1991;17(6):1426-1429. [CrossRef]
- Freitas-Ferraz AB, Bernier M, Vaillancourt R, et al. Safety of Transesophageal Echocardiography to Guide Structural Cardiac Interventions. J Am Coll Cardiol. 2020;75(25):3164-3173. [CrossRef]
- Ruf TF, Heidrich FM, Sveric KM, et al. ELMSTREET (Esophageal Lesions during MitraClip uSing TRansEsophageal Echocardiography Trial). EuroIntervention. 2017;13(12):e1444-e1451. Published 2017 Dec 8. [CrossRef]
- Alkhouli M, Hijazi ZM, Holmes DR Jr, Rihal CS, Wiegers SE. Intracardiac Echocardiography in Structural Heart Disease Interventions. JACC Cardiovasc Interv. 2018;11(21):2133-2147. [CrossRef]
- Stec S, Zaborska B, Sikora-Frac M, Kryński T, Kułakowski P. First experience with microprobe transoesophageal echocardiography in non-sedated adults undergoing atrial fibrillation ablation: feasibility study and comparison with intracardiac echocardiography. Europace. 2011;13(1):51-56. [CrossRef]
- Jiménez Brítez G, Sanchis L, Regueiro A, Sabate M, Sitges M, Freixa X. Minimally-invasive Transesophageal Echocardiography for Left Atrial Appendage Occlusion With a Latest-generation Microprobe. Initial Experience. Rev Esp Cardiol (Engl Ed). 2019;72(6):511-512. [CrossRef]
- Nijenhuis VJ, Alipour A, Wunderlich NC, et al. Feasibility of multiplane microtransoesophageal echocardiographic guidance in structural heart disease transcatheter interventions in adults. Neth Heart J. 2017;25(12):669-674. [CrossRef]
- Sanchis L, Regueiro A, Cepas-Guillén P, Sitges M, Freixa X. First experience of left atrial appendage occlusion using a 3D mini transoesophageal echocardiographic probe with conscious sedation. EuroIntervention. 2023;18(17):1460-1461. [CrossRef]
- Maarse M, Wintgens LIS, Klaver MN, Rensing BJWM, Swaans MJ, Boersma LVA. Transoesophageal echocardiography guidance with paediatric probes in adults undergoing left atrial appendage occlusion. EuroIntervention. 2021;17(1):93-96. [CrossRef]
- Aminian A, Leduc N, Freixa X, et al. Left Atrial Appendage Occlusion Under Miniaturized Transesophageal Echocardiographic Guidance and Conscious Sedation: Multicenter European Experience. JACC Cardiovasc Interv. 2023;16(15):1889-1898. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).