Submitted:
13 September 2024
Posted:
13 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. TEER Procedure
2.3. Definition of the Variables
2.4. Study Objectives
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Procedural Results
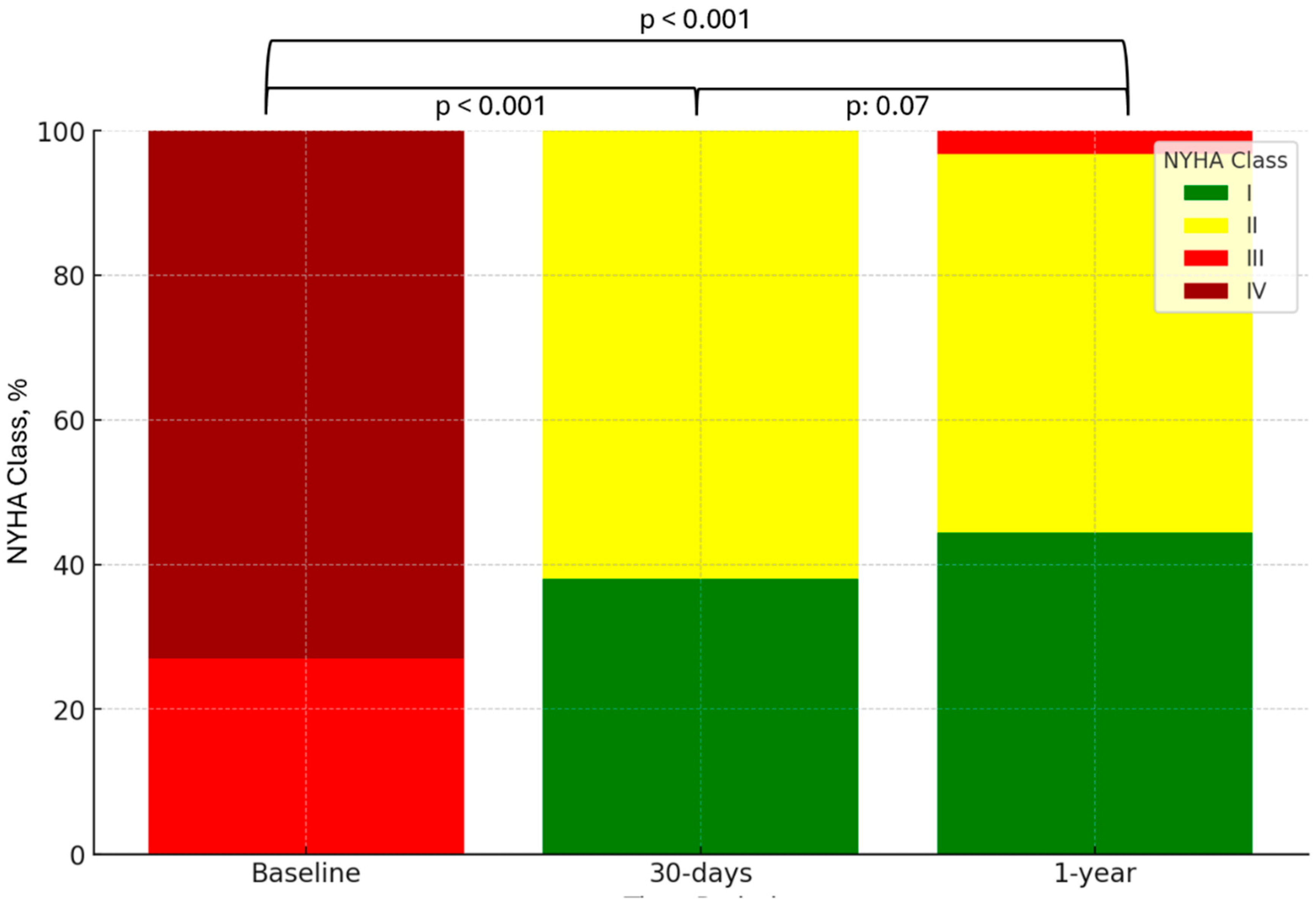
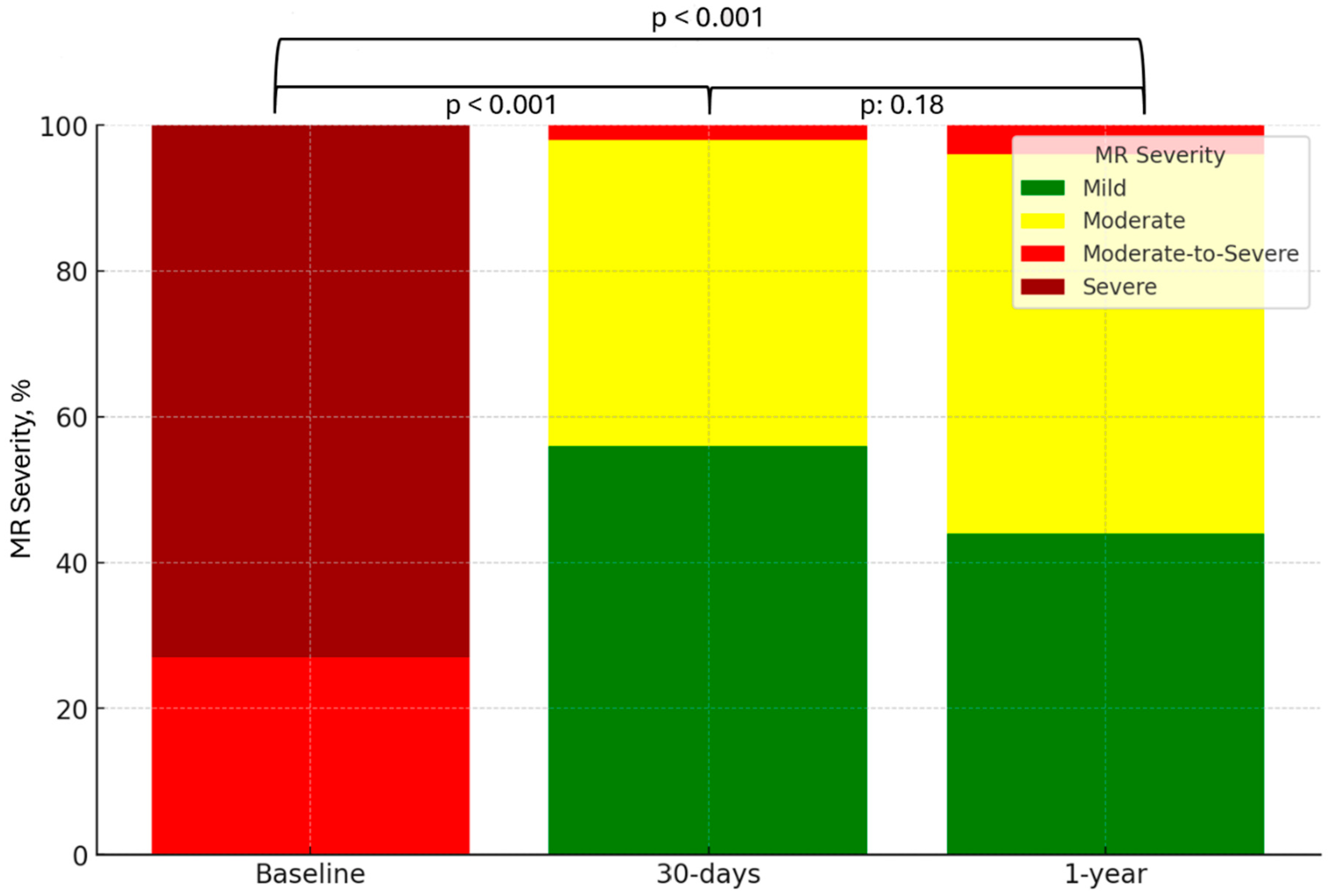
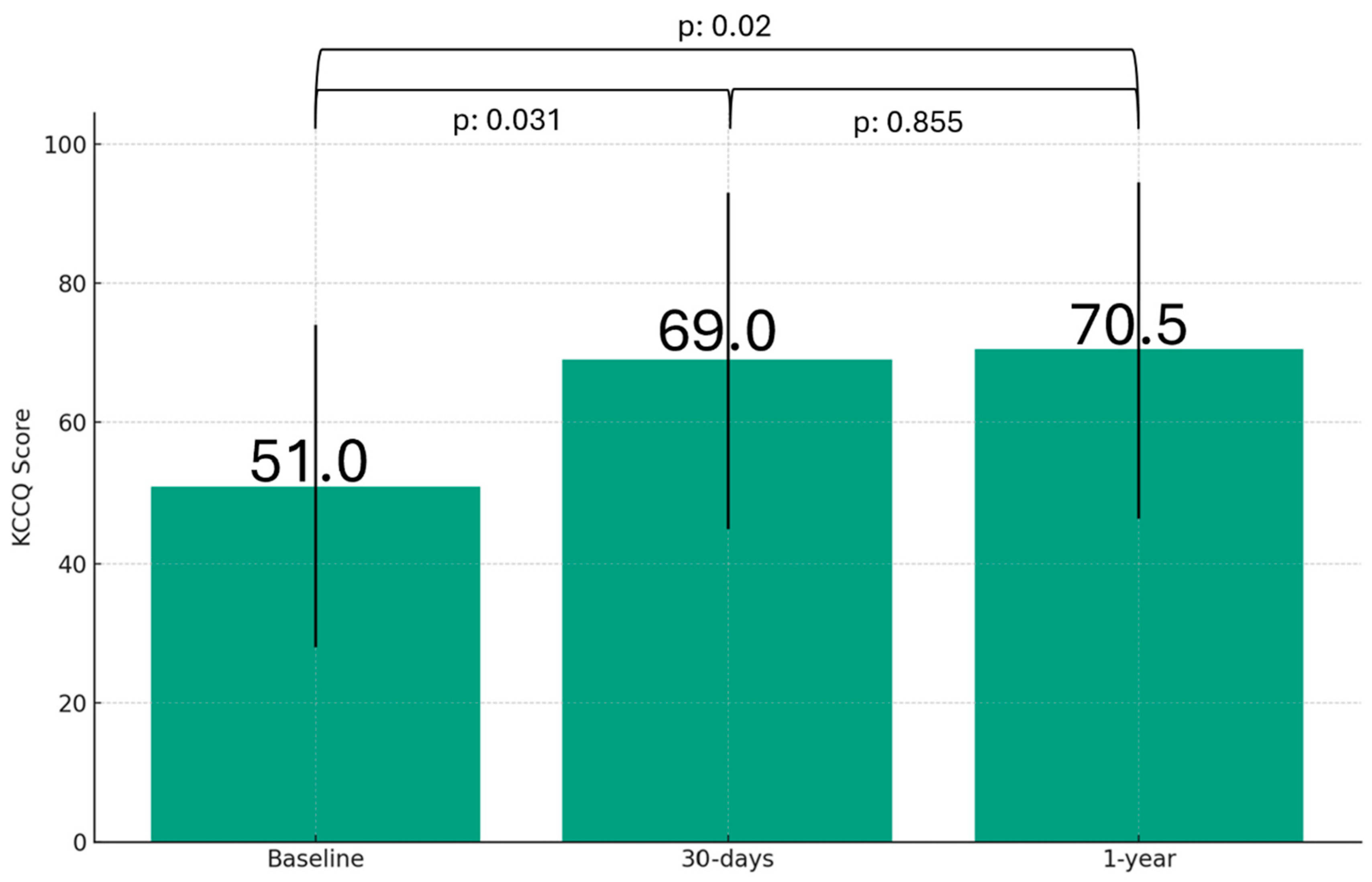
3.2. One-Year Outcomes
3.3. NYHA Class I Prognostic Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agricola, E.; Ielasi, A.; Oppizzi, M.; Faggiano, P.; Ferri, L.; Calabrese, A.; Vizzardi, E.; Alfieri, O.; Margonato, A. Long-term prognosis of medically treated patients with functional mitral regurgitation and left ventricular dysfunction. European Journal of Heart Failure 2009, 11, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Sarano, M.; Akins, C.W.; Vahanian, A. Mitral regurgitation. The Lancet 2009, 373, 1382–1394. [Google Scholar] [CrossRef]
- Nkomo, V.T.; Gardin, J.M.; Skelton, T.N.; Gottdiener, J.S.; Scott, C.G.; Enriquez-Sarano, M. Burden of valvular heart diseases: a population-based study. The Lancet 2006, 368, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Dini, F.L.; Faggiano, P.; Agricola, E.; Cicoira, M.; Frattini, S.; Simioniuc, A.; Gullace, M.; Ghio, S.; Enriquez-Sarano, M.; Temporelli, P.L. Independent prognostic value of functional mitral regurgitation in patients with heart failure. A quantitative analysis of 1256 patients with ischaemic and non-ischaemic dilated cardiomyopathy. Heart 2011, 97, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Taramasso, M.; Buzzatti, N.; La Canna, G.; Colombo, A.; Alfieri, O.; Maisano, F. Interventional vs. surgical mitral valve therapy. Which technique for which patient? Herz 2013, 38, 460–6. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Foster, E.; Glower, D.D.; Kar, S.; Rinaldi, M.J.; Fail, P.S.; Smalling, R.W.; Siegel, R.; Rose, G.A.; Engeron, E.; Loghin, C.; Trento, A.; Skipper, E.R.; Fudge, T.; Letsou, G.V.; Massaro, J.M.; Mauri, L. Percutaneous Repair or Surgery for Mitral Regurgitation. New England Journal of Medicine 2011, 364, 1395–1406. [Google Scholar] [CrossRef] [PubMed]
- Mauri, L.; Foster, E.; Glower, D.D.; Apruzzese, P.; Massaro, J.M.; Herrmann, H.C.; Hermiller, J.; Gray, W.; Wang, A.; Pedersen, W.R.; Bajwa, T.; Lasala, J.; Low, R.; Grayburn, P.; Feldman, T. 4-Year Results of a Randomized Controlled Trial of Percutaneous Repair Versus Surgery for Mitral Regurgitation. Journal of the American College of Cardiology 2013, 62, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Obadia, J.-F.; Messika-Zeitoun, D.; Leurent, G.; Iung, B.; Bonnet, G.; Piriou, N.; Lefèvre, T.; Piot, C.; Rouleau, F.; Carrié, D.; Nejjari, M.; Ohlmann, P.; Leclercq, F.; Etienne, C.S.; Teiger, E.; Leroux, L.; Karam, N.; Michel, N.; Gilard, M.; Donal, E.; Trochu, J.-N.; Cormier, B.; Armoiry, X.; Boutitie, F.; Maucort-Boulch, D.; Barnel, C.; Samson, G.; Guerin, P.; Vahanian, A.; Mewton, N. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. New England Journal of Medicine 2018, 379, 2297–2306. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; Whisenant, B.; Grayburn, P.A.; Rinaldi, M.; Kapadia, S.R.; Rajagopal, V.; Sarembock, I.J.; Brieke, A.; Marx, S.O.; Cohen, D.J.; Weissman, N.J.; Mack, M.J. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. New England Journal of Medicine 2018, 379, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Bardeleben, R.S. v.; Mahoney, P.; Morse, M.A.; Price, M.J.; Denti, P.; Maisano, F.; Rogers, J.H.; Rinaldi, M.; Marco, F.D.; Rollefson, W.; Chehab, B.; Williams, M.; Leurent, G.; Asch, F.M.; Rodriguez, E. 1-Year Outcomes With Fourth-Generation Mitral Valve Transcatheter Edge-to-Edge Repair From the EXPAND G4 Study. JACC: Cardiovascular Interventions 2023, 16, 2600–2610. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Friede, T.; Bardeleben, R.-S. v.; Butler, J.; Khan, M.-S.; Diek, M.; Heinrich, J.; Geyer, M.; Placzek, M.; Ferrari, R.; Abraham, W.T.; Alfieri, O.; Auricchio, A.; Bayes-Genis, A.; Cleland, J.G.F.; Filippatos, G.; Gustafsson, F.; Haverkamp, W.; Kelm, M.; Kuck, K.-H.; Landmesser, U.; Maggioni, A.P.; Metra, M.; Ninios, V.; Petrie, M.C.; Rassaf, T.; Ruschitzka, F.; Schäfer, U.; Schulze, P.C.; Spargias, K.; Vahanian, A.; Zamorano, J.L.; Zeiher, A.; Karakas, M.; Koehler, F.; Lainscak, M.; Öner, A.; Mezilis, N.; Theofilogiannakos, E.K.; Ninios, I.; Chrissoheris, M.; Kourkoveli, P.; Papadopoulos, K.; Smolka, G.; Wojakowski, W.; Reczuch, K.; Pinto, F.J.; Wiewiórka, Ł.; Kalarus, Z.; Adamo, M.; Santiago-Vacas, E.; Ruf, T.F.; Gross, M.; Tongers, J.; Hasenfuss, G.; Schillinger, W.; Ponikowski, P. Transcatheter Valve Repair in Heart Failure with Moderate to Severe Mitral Regurgitation. New England Journal of Medicine, ahead of print. 2024. [Google Scholar]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; Delgado, V.; Freemantle, N.; Gilard, M.; Haugaa, K.H.; Jeppsson, A.; Jüni, P.; Pierard, L.; Prendergast, B.D.; Sádaba, J.R.; Tribouilloy, C.; Wojakowski, W.; Group, E.E.S.D.; Societies, E.N.C. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal 2021, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Kubo, S.; Izumo, M.; Mizuno, S.; Shirai, S. MitraClip Treatment of Moderate-to-Severe and Severe Mitral Regurgitation in High Surgical Risk Patients—Real-World 1-Year Outcomes From Japan. Circ J 2022, 86, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.; von Bardeleben, R.S.; Rottbauer, W.; Mahoney, P.; Price, M.J.; Grasso, C.; Williams, M.; Lurz, P.; Ahmed, M.; Hausleiter, J.; Chehab, B.; Zamorano, J.L.; Asch, F.M.; Maisano, F. Contemporary Outcomes Following Transcatheter Edge-to-Edge Repair: 1-Year Results From the EXPAND Study. JACC Cardiovasc Interv 2023, 16, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Kubo, S.; Yamamoto, M.; Saji, M.; Asami, M.; Enta, Y.; Nakashima, M.; Shirai, S.; Izumo, M.; Mizuno, S.; Watanabe, Y.; Amaki, M.; Kodama, K.; Yamaguchi, J.; Nakajima, Y.; Naganuma, T.; Bota, H.; Ohno, Y.; Yamawaki, M.; Ueno, H.; Mizutani, K.; Adachi, Y.; Otsuka, T.; Hayashida, K.; Hayashida, K.; Adachi, Y.; Yamamoto, M.; Yamamoto, M.; Shirai, S.; Watanabe, Y.; Naganuma, T.; Yamawaki, M.; Enta, Y.; Nakashima, M.; Mizuno, S.; Ueno, H.; Ohno, Y.; Nakajima, Y.; Izumo, M.; Bota, H.; Kodama, K.; Yamaguchi, J.; Kubo, S.; Amaki, M.; Asami, M.; Saji, M.; Mizutani, K. One-year outcomes and their relationship to residual mitral regurgitation after transcatheter edge-to-edge repair with MitraClip device: Insights from the OCEAN-Mitral registry. Journal of the American Heart Association 2023, 12, e030747. [Google Scholar] [CrossRef] [PubMed]
- Puls, M.; Lubos, E.; Boekstegers, P.; von Bardeleben, R.S.; Ouarrak, T.; Butter, C.; Zuern, C.S.; Bekeredjian, R.; Sievert, H.; Nickenig, G.; Eggebrecht, H.; Senges, J.; Schillinger, W. One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German transcatheter mitral valve interventions registry. Eur Heart J 2016, 37, 703–12. [Google Scholar] [CrossRef] [PubMed]
- Sorajja, P.; Vemulapalli, S.; Feldman, T.; Mack, M.; Holmes, D.R., Jr.; Stebbins, A.; Kar, S.; Thourani, V.; Ailawadi, G. Outcomes With Transcatheter Mitral Valve Repair in the United States: An STS/ACC TVT Registry Report. J Am Coll Cardiol 2017, 70, 2315–2327. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Overall, N = 831 | DMR, N = 24 | FMR, N = 59 | p-value2 |
| Age, years | 76 (11) | 79 (9) | 75 (11) | 0.2 |
| Male sex | 55 / 83 (66) | 16 / 24 (67) | 39 / 59 (66) | >0.9 |
| NYHA class | >0.9 | |||
| III | 22 / 83 (27) | 6 / 24 (25) | 16 / 59 (27) | |
| IV | 61 / 83 (73) | 18 / 24 (75) | 41 / 59 (73) | |
| Euroscore II, % | 0.07 (0.06) | 0.06 (0.03) | 0.08 (0.07) | 0.074 |
| eGFR, mL/min/1.73 m² | 48 (30) | 59 (25) | 45 (30) | 0.12 |
| NT-proBNP, pg/mL | 2,755 (3,351) | 1,788 (3,786) | 2,876 (3,375) | 0.072 |
| HF hospitalization | 57 / 83 (69) | 17 / 24 (71) | 40 / 59 (68) | 0.8 |
| MI | 23 / 83 (28) | 1 / 24 (4.2) | 22 / 59 (37) | 0.002 |
| AF | 54 / 83 (65) | 13 / 24 (54) | 41 / 59 (69) | 0.2 |
| PPM | 12 / 83 (14) | 0 / 24 (0) | 12 / 59 (20) | 0.015 |
| COPD | 31 / 83 (37) | 10 / 24 (42) | 21 / 59 (36) | 0.6 |
| Diabetes | 15 / 83 (18) | 5 / 24 (21) | 10 / 59 (17) | 0.8 |
| ICD / CRT | 0.023 | |||
| None | 61 / 83 (73) | 22 / 24 (92) | 39 / 59 (66) | |
| ICD | 11 / 83 (13) | 2 / 24 (8.3) | 9 / 59 (15) | |
| CRT | 11 / 83 (13) | 0 / 24 (0) | 11 / 59 (19) | |
| Echocardiography | ||||
| Severe (4+) MR | 73 / 83 (88) | 21 / 24 (88) | 52 / 59 (88) | >0.9 |
| ERO, mm | 42 (11) | 52 (17) | 41 (9) | <0.001 |
| LVEF, % | <0.001 | |||
| < 40 | 36 / 83 (43) | 3 / 24 (13) | 33 / 59 (56) | |
| 41-49 | 30 / 83 (36) | 8 / 24 (33) | 22 / 59 (37) | |
| ≥ 50 | 17 / 83 (20) | 13 / 24 (54) | 4 / 59 (6.8) | |
| LVDD, cm | 6.10 (1.20) | 5.30 (0.75) | 6.20 (0.85) | <0.001 |
| Hemodynamics | ||||
| CI, mL/min/m2 | 1.90 (0.60) | 2.05 (0.53) | 1.80 (0.60) | 0.027 |
| PASP, mmHg | 55 (15) | 53 (20) | 55 (15) | 0.6 |
| mPAP, mmHg | 33 (11) | 33 (11) | 33 (14) | 0.4 |
| PCWP, mmHg | 24 (11) | 24 (11) | 24 (10) | 0.4 |
| mRAP, mmHg | 10.0 (5.0) | 9.5 (6.3) | 10.0 (6.8) | 0.4 |
| Procedural results | ||||
| Procedural success | 83 / 83 (100) | 24 / 24 (100) | 59 / 59 (100) | >0.9 |
| Implantation time, mins | 26 (8) | 30 (10) | 25 (5) | <0.001 |
| Procedural time, mins | 55 (11) | 63 (10) | 52 (7) | <0.001 |
| Number of clips implanted | 0.060 | |||
| 1 | 57 / 83 (69) | 15 / 24 (63) | 42 / 59 (71) | |
| 2 | 23 / 83 (28) | 6 / 24 (25) | 17 / 59 (29) | |
| 3 | 2 / 83 (2.4) | 2 / 24 (8.3) | 0 / 59 (0) | |
| 4 | 1 / 83 (1.2) | 1 / 24 (4.2) | 0 / 59 (0) | |
| MR severity at discharge | >0.9 | |||
| 1+ (mild) | 6 / 83 (7.2) | 1 / 24 (4.2) | 5 / 59 (8.5) | |
| 2+ (moderate) | 46 / 83 (55) | 13 / 24 (54) | 33 / 59 (56) | |
| 3+ (moderate-to-severe) | 28 / 83 (34) | 9 / 24 (38) | 19 / 59 (32) | |
| 4+ (severe) | 3 / 83 (3.6) | 1 / 24 (4.2) | 2 / 59 (3.4) | |
| Transmitral gradient, mmHg | 3.53 (1.2) | 3.82 (1.3) | 3.47 (1.2) | 0.3 |
| Hospital length of stay, days | 3 (1) | 3 (1) | 3 (1) | >0.9 |
| Univariate | Multivariate | ||||||
| Characteristic | N | HR1 | 95% CI1 | p-value | HR1 | 95% CI1 | p-value |
| Age | 83 | 1.0 | 0.96, 1.03 | 0.7 | |||
| Male sex | 83 | 0.91 | 0.44, 1.90 | 0.8 | |||
| Euroscore II2 | 83 | 0.50 | 0.28, 0.88 | 0.017 | 0.64 | 0.35, 1.14 | 0.13 |
| eGFR | 83 | 1.01 | 0.99, 1.03 | 0.4 | |||
| NT-proBNP2 | 83 | 0.55 | 0.37, 0.82 | 0.003 | 0.63 | 0.41, 0.95 | 0.030 |
| HF Hospitalization | 83 | 0.56 | 0.27, 1.14 | 0.11 | |||
| MI | 83 | 0.57 | 0.23, 1.38 | 0.2 | |||
| AF | 83 | 0.82 | 0.40, 1.68 | 0.6 | |||
| PPM | 83 | 0.35 | 0.08, 1.47 | 0.2 | |||
| COPD | 83 | 1.77 | 0.87, 3.58 | 0.11 | |||
| Diabetes | 83 | 0.84 | 0.32, 2.20 | 0.7 | |||
| ICD / CRT | 83 | 0.90 | 0.54, 1.50 | 0.7 | |||
| MR etiology | 83 | ||||||
| DMR | — | — | — | — | |||
| FMR | 0.48 | 0.23, 0.98 | 0.044 | 0.66 | 0.31, 1.41 | 0.3 | |
| Number of clips implanted | 83 | ||||||
| 1 | — | — | |||||
| 2 | 1.34 | 0.63, 2.86 | 0.5 | ||||
| 3 | 5.02 | 0.67, 37.7 | 0.12 | ||||
| MR severity at 30 days | 83 | ||||||
| 1+ | — | — | |||||
| 2+ | 1.22 | 0.59, 2.51 | 0.6 | ||||
| 3+ | 1.60 | 0.21, 12.0 | 0.6 | ||||
| MR severity at 1 year | 83 | ||||||
| 1+ | — | — | |||||
| 2+ | 1.14 | 0.40, 3.29 | 0.8 | ||||
| 3+ | 0.00 | 0.00, Inf | >0.9 | ||||
| Hospital stay | 83 | 0.72 | 0.37, 1.40 | 0.3 | |||
| Echocardiography | |||||||
| LVEF | 83 | 5.37 | 0.16, 182 | 0.4 | |||
| LVDD | 83 | 0.72 | 0.42, 1.24 | 0.2 | |||
| ERO | 83 | 1.00 | 0.97, 1.03 | >0.9 | |||
| Hemodynamics | |||||||
| PASP | 83 | 0.99 | 0.96, 1.03 | 0.6 | |||
| PCWP | 83 | 0.98 | 0.93, 1.03 | 0.4 | |||
| mRAP | 83 | 0.98 | 0.91, 1.05 | 0.5 | |||
| mPAP | 83 | 0.97 | 0.93, 1.02 | 0.3 | |||
| CI | 83 | 2.21 | 1.07, 4.59 | 0.033 | |||
| Univariate | Multivariate | ||||||
| Characteristic | N | HR1 | 95% CI1 | p-value | HR1 | 95% CI1 | p-value |
| Age | 83 | 0.98 | 0.95, 1.01 | 0.12 | |||
| Male sex | 83 | 0.92 | 0.45, 1.85 | 0.8 | |||
| Euroscore II2 | 83 | 0.40 | 0.23, 0.69 | 0.001 | 0.50 | 0.28, 0.89 | 0.019 |
| eGFR | 83 | 1.02 | 1.00, 1.04 | 0.025 | |||
| NT-proBNP2 | 83 | 0.58 | 0.40, 0.85 | 0.004 | 0.67 | 0.44, 0.99 | 0.049 |
| HF hospitalization | 83 | 0.49 | 0.25, 0.96 | 0.037 | 0.64 | 0.32, 1.26 | 0.2 |
| MI | 83 | 0.49 | 0.20, 1.18 | 0.11 | |||
| AF | 83 | 0.61 | 0.31, 1.19 | 0.15 | |||
| PPM | 83 | 0.51 | 0.16, 1.66 | 0.3 | |||
| COPD | 83 | 1.44 | 0.73, 2.83 | 0.3 | |||
| Diabetes | 83 | 0.96 | 0.40, 2.33 | >0.9 | |||
| ICD/CRT | 83 | 0.89 | 0.55, 1.46 | 0.6 | |||
| MR etiology | 83 | ||||||
| DMR | — | — | |||||
| FMR | 0.49 | 0.25, 0.97 | 0.040 | ||||
| Number of clips implanted | 83 | ||||||
| 1 | — | — | |||||
| 2 | 0.98 | 0.46, 2.13 | >0.9 | ||||
| 3 | 4.24 | 0.57, 31.6 | 0.2 | ||||
| MR severity at 30 days | 83 | ||||||
| 1+ | — | — | |||||
| 2+ | 1.47 | 0.73, 2.94 | 0.3 | ||||
| 3+ | 1.60 | 0.21, 12.0 | 0.6 | ||||
| MR severity at 1 year | 83 | ||||||
| 1+ | — | — | |||||
| 2+ | 0.93 | 0.36, 2.42 | 0.9 | ||||
| 3+ | 0.00 | 0.00, Inf | >0.9 | ||||
| Hospital stay | 83 | 0.77 | 0.40, 1.46 | 0.4 | |||
| Echocardiography | |||||||
| LVEF | 83 | 4.44 | 0.15, 131 | 0.4 | |||
| LVDD | 83 | 0.79 | 0.47, 1.32 | 0.4 | |||
| ERO | 83 | 1.00 | 0.97, 1.03 | 0.9 | |||
| Hemodynamics | |||||||
| PASP | 83 | 0.99 | 0.96, 1.02 | 0.5 | |||
| PCWP | 83 | 0.98 | 0.93, 1.02 | 0.3 | |||
| mRAP | 83 | 0.95 | 0.88, 1.02 | 0.14 | |||
| mPAP | 83 | 0.97 | 0.93, 1.02 | 0.2 | |||
| CI | 83 | 1.73 | 0.87, 3.45 | 0.12 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





