Submitted:
13 September 2024
Posted:
15 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
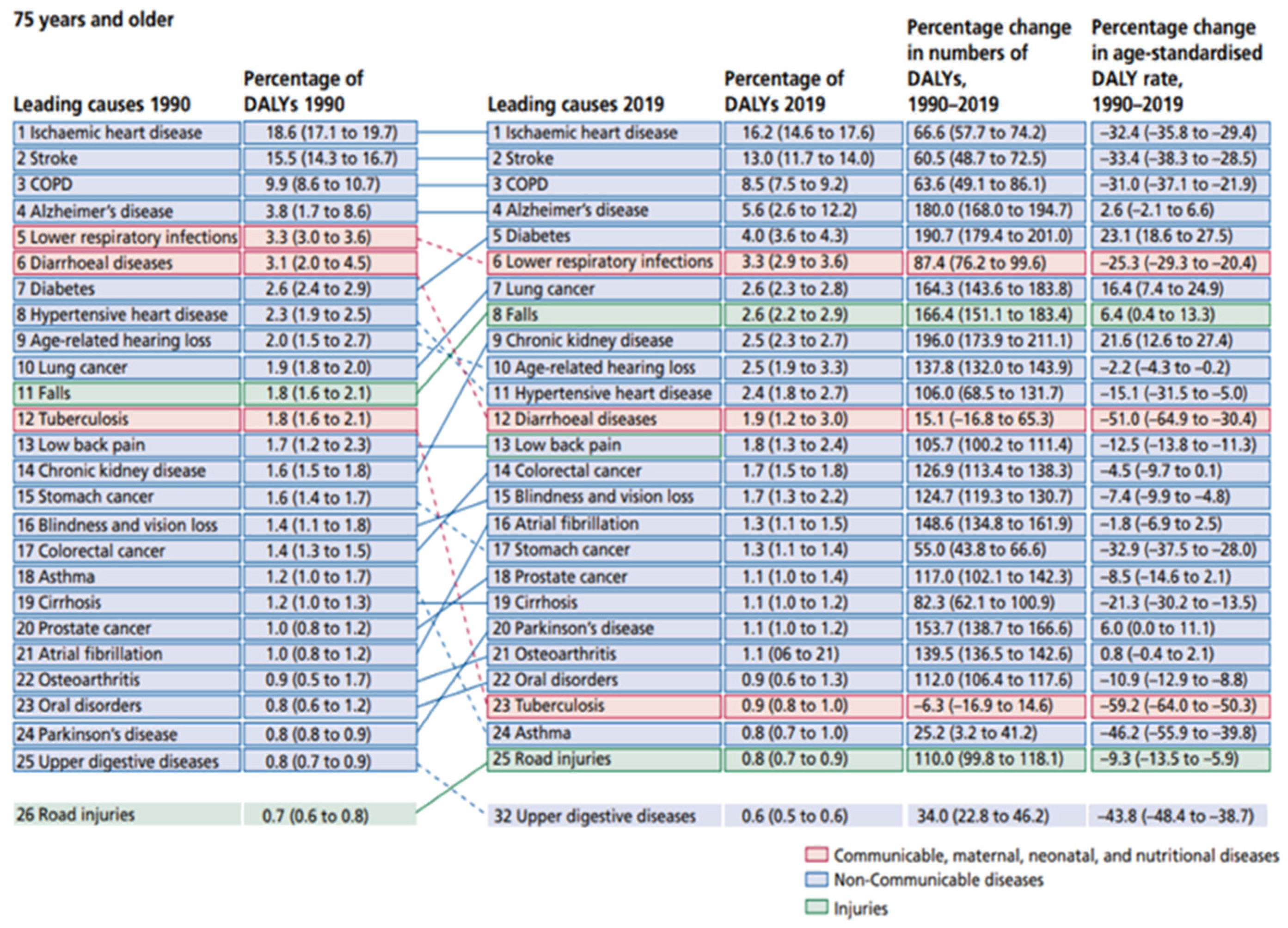
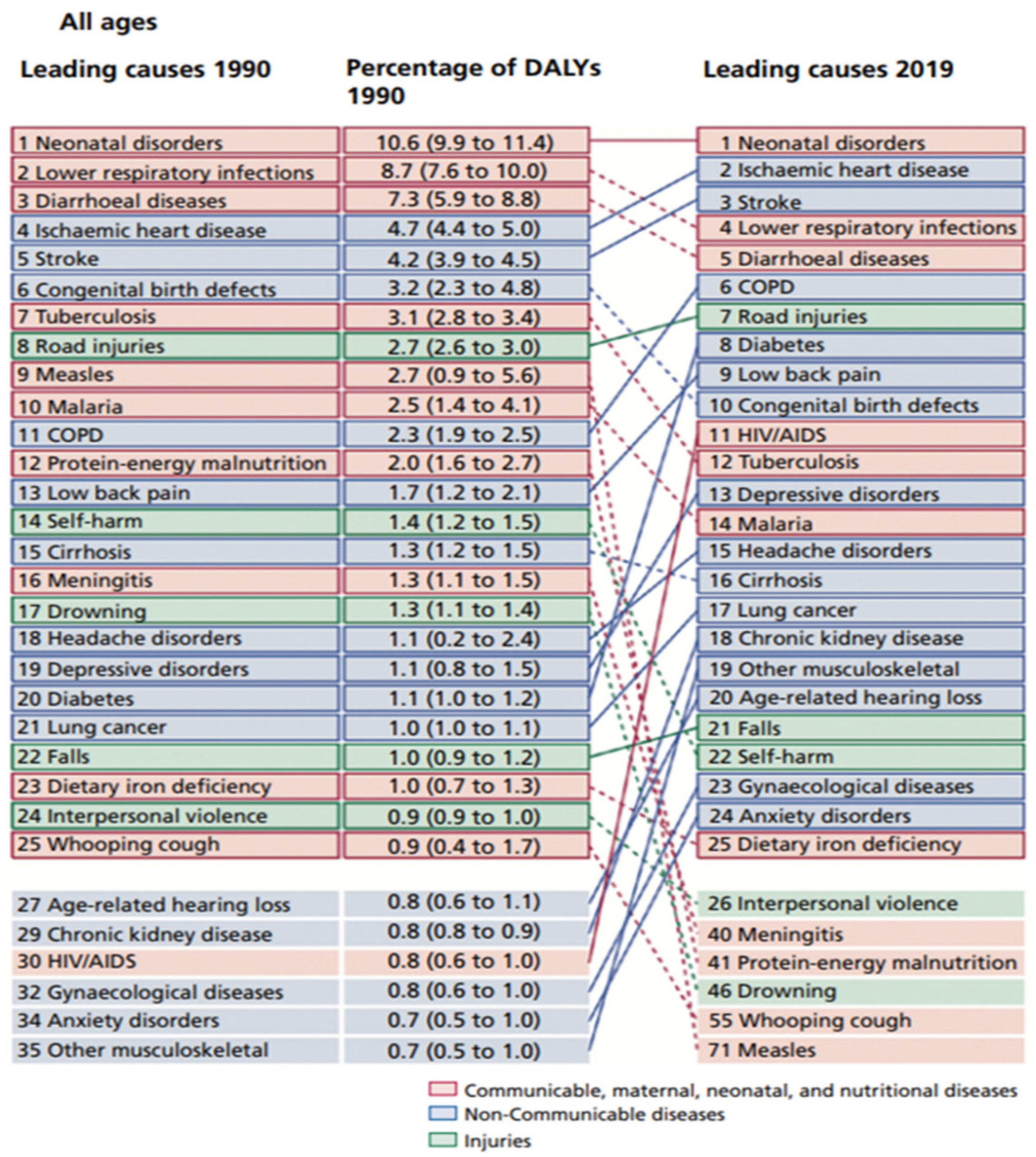
- The Global Burden of Disease
- The Rise of Non-Communicable Diseases
1.2. The Double Burden of Disease
1.3. The Impact of Urbanization and Aging
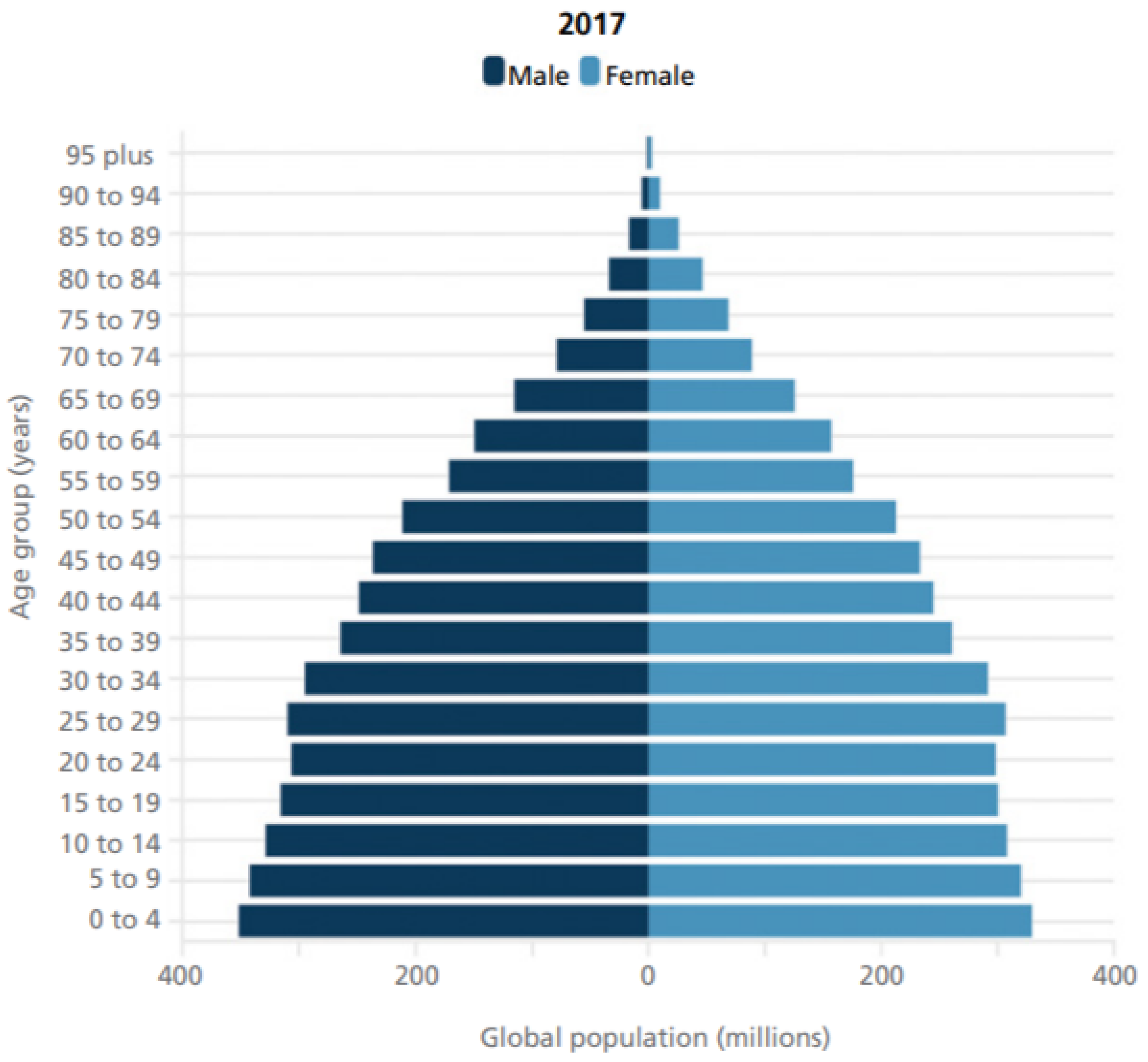
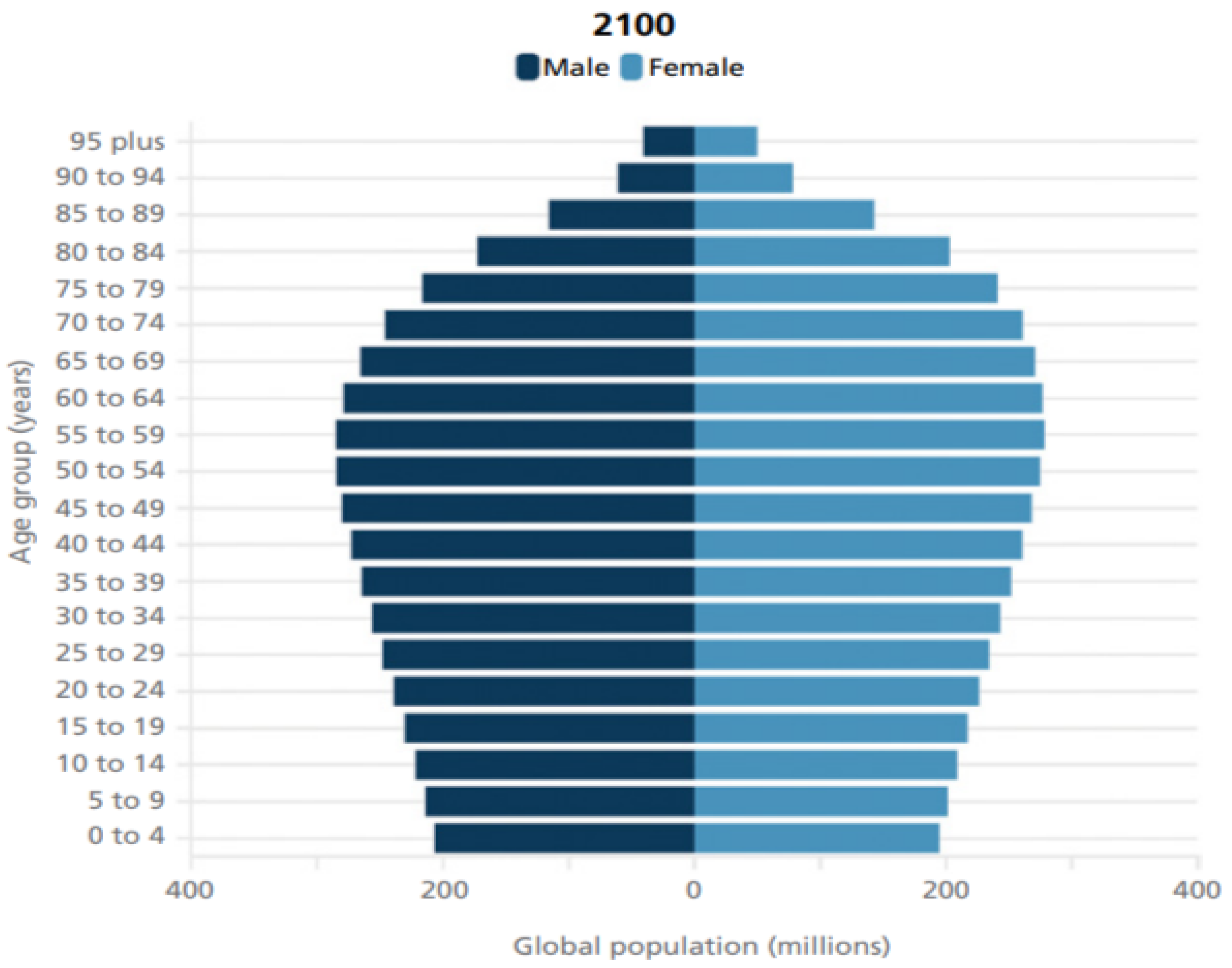
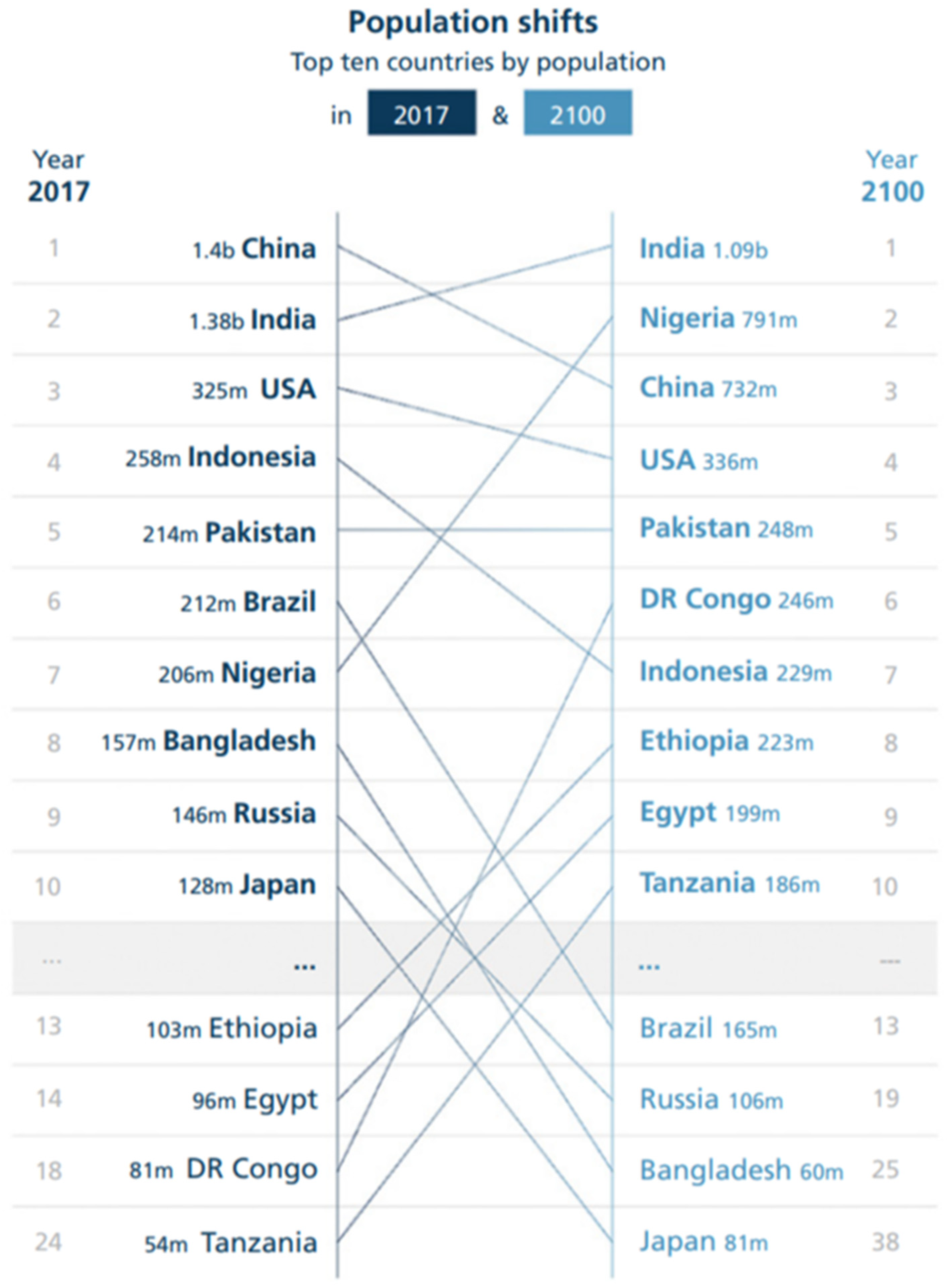
- Aging Population
2. Discussion
2.1. Global Health Initiatives and Policies
- National and Regional Efforts
- Research and Innovation
2.3. The Alarming Tendencies of Non-Communicable Diseases and the Role of Artificial Intelligence
- Regional Disparities in NCD Burden
- High-Income Countries
- Explanation:
- High Income Countries
- Low- and Middle-Income Countries (LMICs)
2.4. The Growing Burden of Neurological Diseases
- Alzheimer's Disease and Other Dementias
- High-Income Countries
- Low and Middle Income Countries
- Parkinson's Disease
2.5. The Rise of Obesity
2.6. Potential Solutions to Mitigate NCD Burden
- Public Health Policies, Interventions and the Crucial Role of AI
- Implementing strict tobacco control measures, including taxation, advertising bans, and smoking cessation programs, can reduce smoking rates and associated NCDs (World Health Organization [WHO], 2020).
- Nutrition and Physical Activity: Promoting healthy diets and regular physical activity through public health campaigns, school programs, and community initiatives can help combat obesity and related diseases (World Health Organization [WHO], 2021).
- Healthcare Access: Ensuring access to healthcare services, particularly in LMICs, is essential for early detection and treatment of NCDs. This includes improving primary care services and ensuring the availability of essential medicines (World Health Organization [WHO], 2013).
- Technological innovations, particularly in the field of artificial intelligence (AI), hold great promise for addressing NCDs. AI will enhance early diagnosis, personalize treatment plans, and improve healthcare delivery.
- Early Diagnosis and Screening: AI-driven diagnostic tools can improve the early detection of NCDs, including neurological diseases and cancers. Machine learning algorithms are already been used to analyze medical images, genomic data, and patient records to identify patterns and predict disease risk.
- Cancer Screening: AI algorithms have demonstrated the ability to detect cancers, such as breast and lung cancer, at earlier stages through the analysis of imaging data (McKinney et al., 2020).
- Neurological Diseases: AI can assist in the early diagnosis of Alzheimer's disease by analyzing neuroimaging data and identifying subtle changes in the brain that indicate the onset of the disease (Ding et al., 2020).
- Personalized Medicine: AI enables the development of personalized treatment plans based on individual patient data, including genetics, lifestyle, and environmental factors. This approach can improve treatment outcomes and reduce adverse effects.
- Precision Medicine: AI can identify the most effective treatments for individual patients, such as selecting the optimal chemotherapy regimen for cancer patients based on genetic profiles (Topol, 2019).
- Chronic Disease Management: AI-powered applications can help manage chronic conditions like diabetes by providing real-time monitoring, personalized recommendations, and alerts for healthcare providers (Krittanawong et al., 2017).
- Healthcare Delivery and Management: AI can streamline healthcare delivery and improve resource allocation, particularly in resource-constrained settings.
- Telemedicine: AI-powered telemedicine platforms can provide remote consultations, monitor patient health, and deliver care to underserved populations (Dorsey et al., 2020). It´s already a source of knowledge for large startct of the world population, a fact that may contribute to decrease medical-patient information bias (Montgomery, 2023).
- Resource Allocation: AI can optimize resource allocation in hospitals and healthcare systems by predicting patient admissions, managing bed capacity, and reducing wait times (Yoon et al., 2020). This optimization is already happening in several countries like Brazil and USA, with drastic cuts in costs and faster attending to urgent diseased patients.
2.7. Exponential Growth of Artificial Intelligence
- Current Capabilities and Limitations
- Data Quality and Availability
- Interpretability and Trust
- Projected Developments in the Next Five Years
- Bias and Fairness
3. Conclusion
Conflicts of Interest
References
- Alzheimer's Association. (2020). 2020 Alzheimer's disease facts and figures. Alzheimer's & Dementia, 16(3), 391-460.
- Beaglehole, R., Bonita, R., Horton, R., Adams, C., Alleyne, G., Asaria, P.,... & Watt, J. (2011). Priority actions for the non-communicable disease crisis. The Lancet, 377(9775), 1438-1447.
- Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W., Carson, A. P.,... & Virani, S. S. (2019). Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation, 139(10), e56-e528.
- Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W., Carson, A. P.,... & Virani, S. S. (2019). Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation, 139(10), e56-e528.
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 68(6), 394-424.
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 68(6), 394-424.
- Centers for Disease Control and Prevention (CDC). (2020). National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention.
- Chen, J. H., & Asch, S. M. (2017). Machine learning and prediction in medicine—precision medicine or blunt instruments? New England Journal of Medicine, 376(23), 2211-2213.
- Cho, N. H., Shaw, J. E., Karuranga, S., Huang, Y., da Rocha Fernandes, J. D., Ohlrogge, A. W., & Malanda, B. (2018). IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice, 138, 271-281.
- Daneault, J. F., Gagnon, J. F., Duval, C., Desautels, A., Gosselin, N., Tampieri, D.,... & Montplaisir, J. (2019). Diagnostic accuracy of a deep learning model for the prediction of Parkinson's disease using clinical data. Movement Disorders, 34(8), 1149-1158.
- Demiris, G., Rantz, M., Aud, M., Marek, K. D., Tyrer, H. W., & Stahl, S. M. (2018). Older adults' attitudes towards smart home technologies: Implications for research and practice. Journal of Telemedicine and Telecare, 13(4), 232-234.
- Ding, Y., Zhou, X., He, Z., & Zeng, J. (2020). Deep learning for Alzheimer's disease: a systematic review. Frontiers in Neuroscience, 14, 887.
- Dorsey, E. R., Achey, M. A., Beck, C. A., Beran, D. B., Biglan, K. M., Boyd, C. M.,... & Sherer, T. (2018). National randomized controlled trial of virtual house calls for Parkinson disease. Neurology, 90(15), e1278-e1285.
- Dorsey, E. R., Glidden, A. M., Holloway, M. R., Birbeck, G. L., & Schwamm, L. H. (2020). Teleneurology and mobile technologies: access, equity, and cost. Annals of Neurology, 87(5), 655-665.
- Ezzati, M., Lopez, A. D., Rodgers, A., Hoorn, S. V., & Murray, C. J. (2005). Selected major risk factors and global and regional burden of disease. The Lancet, 360(9343), 1347-1360.
- Ferlay, J., Ervik, M., Lam, F., Colombet, M., Mery, L., Pincon, A.,... & Bray, F. (2020). Global Cancer Observatory: Cancer Today. International Agency for Research on Cancer.
- Forouzanfar, M. H., Liu, P., Roth, G. A., Ng, M., Biryukov, S., Marczak, L.,... & Murray, C. J. (2017). Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA, 317(2), 165-182.
- Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, 360, 1-8.
- Hssayeni, M. D., Jimenez, S., Shaikh, M. F., & Ghoraani, B. (2020). A deep learning approach for prediction of freezing of gait in Parkinson’s disease. IEEE Journal of Biomedical and Health Informatics, 24(5), 1470-1478.
- Kowal, P., Dowd, J. E., & Chatterji, S. (2016). Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Global Health Action, 9(1), 29405.
- Lozano, R., Naghavi, M., Foreman, K., Lim, S., Shibuya, K., Aboyans, V.,... & AlMazroa, M. A. (2013). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2095-2128.
- Marmot, M., Friel, S., Bell, R., Houweling, T. A., Taylor, S., & Commission on Social Determinants of Health. (2008). Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet, 372(9650), 1661-1669.
- Montgomery, R. M.; Aprahamian, I. (2018). Thesis: Fragilidade e Doença de Parkinson. (2018). University of São Paulo. [CrossRef]
- (Montgomery, R. M. 2024). The Shift from Aerobic to Anaerobic Strength Training A Paradigm Change in Preventing Frailty, Morbidity, and Mortality in Older Adults. (2024). [CrossRef]
- (Montgomery, R. M. 2024). A Comparative Analysis of Mortality Rates in Public vs. Private Healthcare Systems Worldwide"(2024). [CrossRef]
- Murray, C. J., Aravkin, A. Y., Zheng, P., Abbafati, C., Abbas, K. M., Abbasi-Kangevari, M.,... & Vos, T. (2020). Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1223-1249.
- Nugent, R., Bertram, M. Y., Jan, S., Niessen, L. W., Sassi, F., Jamison, D. T.,... & Zheng, Y. (2018). Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. The Lancet, 392(10152), 1036-1038.
- Nutbeam, D. (2000). Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259-267.
- United Nations. (2015). Transforming our world: the 2030 Agenda for Sustainable Development. United Nations.
- Vos, T., Lim, S. S., Abbafati, C., Abbas, K. M., Abbasi, M., Abbasi-Kangevari, M.,... & Murray, C. J. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204-1222.
- World Health Organization. (2013). Global action plan for the prevention and control of noncommunicable diseases 2013-2020. World Health Organization.
- World Health Organization. (2020). Tobacco. World Health Organization.
- World Health Organization. (2021). Cardiovascular diseases (CVDs). World Health Organization.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



