Submitted:
13 September 2024
Posted:
14 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
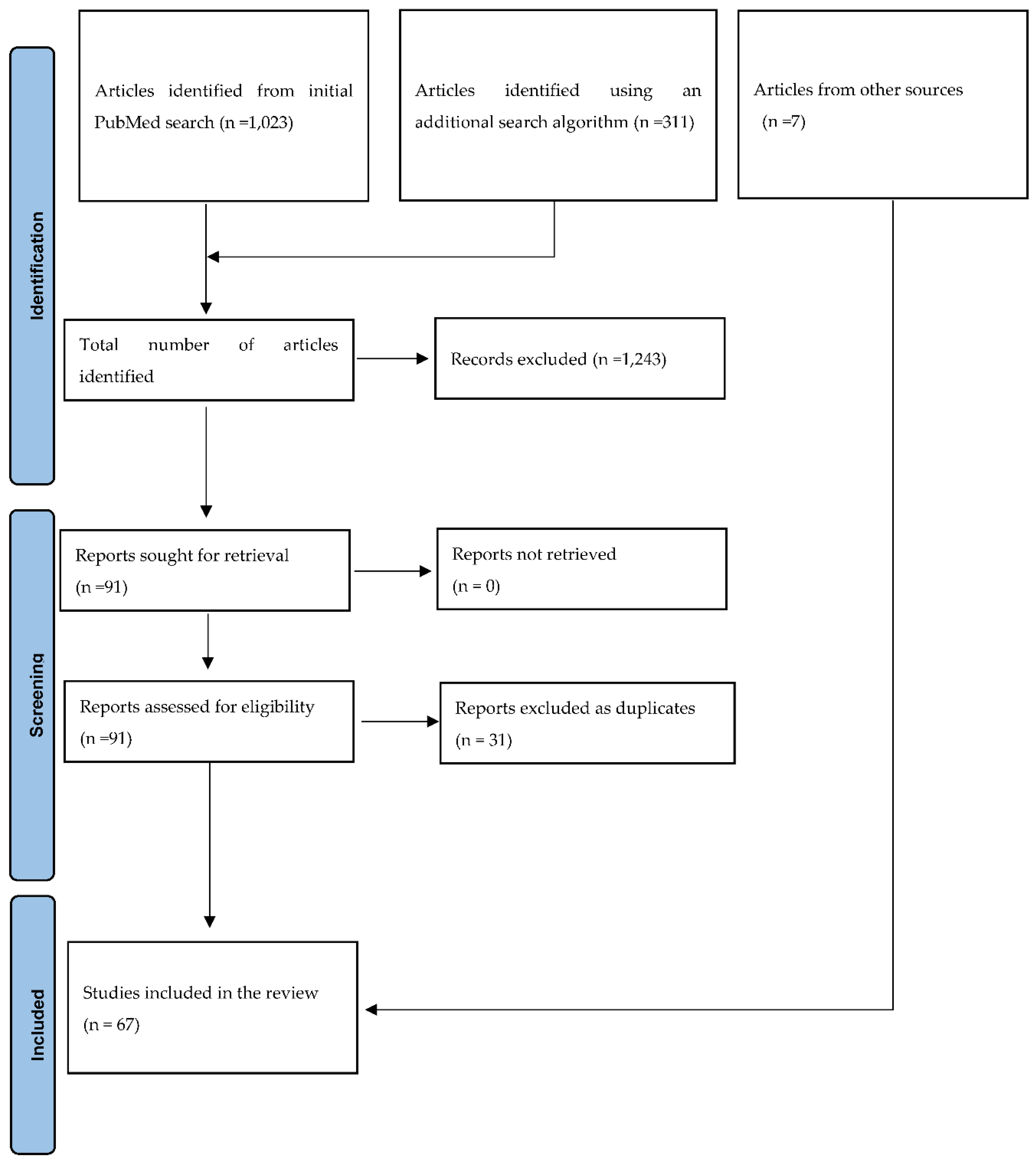
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Selection Process
2.5. Data Extraction
3. Results
3.1. Search Results
3.2. Demographics
3.3. Study Designs
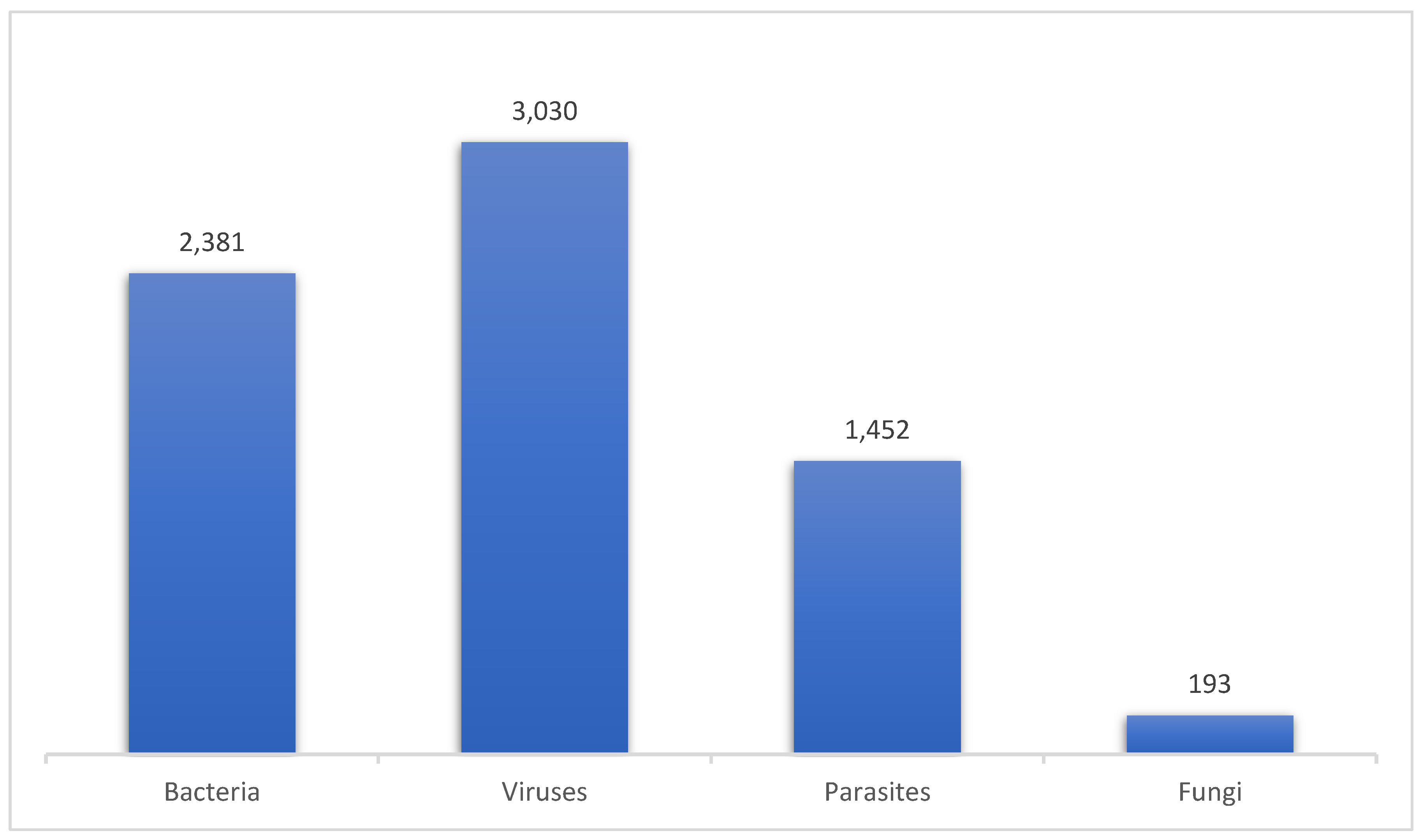
3.4. Pathogens
4. Discussion
4.1. Viral Infection
4.2. Bacterial Infection
4.3. Parasitic Infection
4.4. Fungal Infection
4.5. Susceptibility Testing of Pathogens
4.6. Clinical Outcomes and Treatment Relapse
5. Limitations
6. Conclusion
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- André B, Measuring the Burden of Severe Acute Malnutrition: Current Challenges. Global Nutrition Report 2022. Available at https://globalnutritionreport.org/blog/measuring-burden-severe-acute-malnutrition-current-challenges/. Assessed :10th August 2024.
- United Nations Children’s Fund (UNICEF), Stunting has declined steadily since 2000 – but faster progress is needed to reach the 2030 target. Wasting persists at alarming rates and overweight will require a reversal in trajectory if the 2030 target is to be achieved. Unicef,2023. Available: https://data.unicef.org/topic/nutrition/malnutrition/. Accessed :10th August 2024.
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013; 382(9890): 427-451. [CrossRef]
- Madhumita Paul .Nearly 282 million people in Africa were undernourished in 2022: UN https://www.downtoearth.org.in/news/africa/nearly-282-million-people-in-africa-were-undernourished-in-2022-un-93345.Accessed 25/5/24.
- UNICEF, WHO & World Bank Group (2018) Levels and Trends in Child Malnutrition. Geneva: World Health Organization; available at https://www.who.int/nutgrowthdb/2018-jme-brochure.pdf (accessed May 2024).
- Moyer JD, Bohl DK, Petry C, Scott A, Solórzano JR, Kuhn R. The persistent global burden of severe acute malnutrition: Cross-country estimates, models and forecasts. Global Transitions. 2020;2:167-79. [CrossRef]
- Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect Dis. 2018;31(3):231-236. [CrossRef]
- Otiti MI, Allen SJ. Severe acute malnutrition in low-and middle-income countries. Paediatrics and Child Health. 2021;31(8):301-7. [CrossRef]
- Nigussie J, Girma B, Molla A, Mareg M, Mihretu E. Under-nutrition and associated factors among children infected with human immunodeficiency virus in sub-Saharan Africa: a systematic review and meta-analysis. Arch Public Health. 2022;80(1):19. [CrossRef]
- Fergusson P, Tomkins A. HIV prevalence and mortality among children undergoing treatment for severe acute malnutrition in sub-Saharan Africa: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2009;103(6):541-8. [CrossRef]
- Desyibelew HD, Bayih MT, Baraki AG, Dadi AF. The recovery rate from severe acute malnutrition among under-five years of children remains low in sub-Saharan Africa. A systematic review and meta-analysis of observational studies. PLoS One. 2020;15(3):e0229698. [CrossRef]
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018,169(7):467-473.
- De Maayer T, Saloojee H. Clinical outcomes of severe malnutrition in a high tuberculosis and HIV setting. Arch Dis Child. 2011;96(6):560-4. [CrossRef]
- Girum T, Kote M, Tariku B, Bekele H. Survival status and predictors of mortality among severely acute malnourished children< 5 years of age admitted to stabilization centers in Gedeo Zone: a retrospective cohort study. Therapeutics and clinical risk management. 2017:101-10. [CrossRef]
- Ide LE. Prevalence of tuberculosis among children with severe acute malnutrition at Ola during Children’s Hospital in Freetown Sierra Leone. J Adv Med Med Res. 2019;30(3):1-7. [CrossRef]
- Kasonka L, Munthali G, Rehman AM, Chisenga M, Wells S, Wells JCK, et al. Anthropometry, body composition and chronic disease risk factors among Zambian school-aged children who experienced severe malnutrition in early childhood. Br J Nutr. 2022;128(3):453-460. [CrossRef]
- Osório DV, Munyangaju I, Muhiwa A, Nacarapa E, Nhangave AV, Ramos JM. Lipoarabinomannan Antigen Assay (TB-LAM) for Diagnosing Pulmonary Tuberculosis in Children with Severe Acute Malnutrition in Mozambique. J Trop Pediatr. 2021;67(3):fmaa072. [CrossRef]
- Gavhi F, Kuonza L, Musekiwa A, Motaze NV. Factors associated with mortality in children under five years old hospitalized for Severe Acute Malnutrition in Limpopo province, South Africa, 2014-2018: A cross-sectional analytic study. PLoS One. 2020;15(5):e0232838. [CrossRef]
- Musiime V, Rujumba J, Kakooza L, Namisanvu H, Atuhaire L, Naguti E, et al. HIV prevalence among children admitted with severe acute malnutrition and associated factors with mother-to-child HIV transmission at Mulago Hospital, Uganda: A mixed methods study. PLoS One. 2024;19(4):e0301887. [CrossRef]
- Bwakura-Dangarembizi M, Dumbura C, Amadi B, Ngosa D, Majo FD, Nathoo KJ, et al. Risk factors for postdischarge mortality following hospitalization for severe acute malnutrition in Zimbabwe and Zambia. Am J Clin Nutr. 2021;113(3):665-674. [CrossRef]
- Chinkhumba J, Tomkins A, Banda T, Mkangama C, Fergusson P. The impact of HIV on mortality during in-patient rehabilitation of severely malnourished children in Malawi. Trans R Soc Trop Med Hyg. 2008;102(7):639-44. [CrossRef]
- Page AL, de Rekeneire N, Sayadi S, Aberrane S, Janssens AC, Rieux C, et al. Infections in children admitted with complicated severe acute malnutrition in Niger. PLoS One. 2013;8(7):e68699. [CrossRef]
- Calgaro S, Isidoris V, Girotto C, Chhaganlal K, Moiane J, Putoto G, et al. Children's Nutritional Rehabilitation Program in Beira, Mozambique: A Retrospective Study. Am J Trop Med Hyg. 2021;105(6):1631-1637.
- Teshale EB, Nigatu YD, Delbiso TD. Relapse of severe acute malnutrition among children discharged from outpatient therapeutic program in western Ethiopia. BMC Pediatr. 2023;23(1):441. [CrossRef]
- Yohannes T, Laelago T, Ayele M, Tamrat T. Mortality and morbidity trends and predictors of mortality in under-five children with severe acute malnutrition in Hadiya zone, South Ethiopia: a four-year retrospective review of hospital-based records (2012-2015). BMC Nutr. 2017;3:18. [CrossRef]
- CossaMoiane I, Roucher C, Campos-Ponce M, Doak C, Bauhofer A, Chissaque A, et al. Profile of Children with Undernutrition Admitted in Two Secondary-Level Hospitals in Maputo City, Mozambique. Nutrients. 2024;16(7):1056. [CrossRef]
- Amadi B, Imikendu M, Sakala M, Banda R, Kelly P. Integration of HIV care into community management of acute childhood malnutrition permits good outcomes: retrospective analysis of three years of a programme in Lusaka. PLoS One. 2016;11(3):e0149218. [CrossRef]
- Heydenrych N, De Maayer T, Nel M, van den Berg L. A retrospective cohort analysis of factors associated with the development of refeeding syndrome in children 0-59 months diagnosed with severe acute malnutrition in a South African setting. Heliyon. 2024;10(9):e30091. [CrossRef]
- Asafo-Agyei SB, Antwi S, Nguah SB. HIV infection in severely malnourished children in Kumasi, Ghana: a cross-sectional prospective study. BMC Pediatr. 2013;13:181. [CrossRef]
- Wondim A, Tigabu B, Kelkay MM. Time to Recovery from Severe Acute Malnutrition and Its Predictors among Admitted Children Aged 6-59 Months at the Therapeutic Feeding Center of Pawi General Hospital, Northwest Ethiopia: A Retrospective Follow-Up Study. Int J Pediatr. 2020;2020:8406597. [CrossRef]
- Oumer A, Mesfin L, Tesfahun E, Ale A. Predictors of Death from Complicated Severe Acute Malnutrition in East Ethiopia: Survival Analysis. Int J Gen Med. 2021; 14:8763-8773. [CrossRef]
- Bilal JA, Eltahir HG, Al-Nafeesah A, Al-Wutayd O, Adam I. Acute severe malnutrition treatment outcomes in children ages 6–59 months admitted to Singa Hospital, Sudan. Trans R Soc Trop Med Hyg. 2020;114(8):612-7. [CrossRef]
- Talbert A, Thuo N, Karisa J, Chesaro C, Ohuma E, Ignas J, et al. Diarrhoea complicating severe acute malnutrition in Kenyan children: a prospective descriptive study of risk factors and outcome. PloS one. 2012;7(6):e38321. [CrossRef]
- LaCourse SM, Chester FM, Preidis G, McCrary LM, Arscott-Mills T, Maliwichi M, et al. Use of Xpert for the diagnosis of pulmonary tuberculosis in severely malnourished hospitalized Malawian children. Pediatr Infect Dis J. 2014;33(11):1200-2. [CrossRef]
- Sunguya B. Effects of infections on severely malnourished children in Kilifi-Mombasa and Dar es Salaam: a comparative study. Dar Es Salaam Medical Students' Journal. 2006;14(1):27-35. [CrossRef]
- Schramm B, Nganaboy RC, Uwiragiye P, Mukeba D, Abdoubara A, Abdou I, et al.. Potential value of urine lateral-flow lipoarabinomannan (LAM) test for diagnosing tuberculosis among severely acute malnourished children. PLoS One. 2021;16(5):e0250933. [CrossRef]
- Bachou H, Tylleskär T, Downing R, Tumwine JK. Severe malnutrition with and without HIV-1 infection in hospitalised children in Kampala, Uganda: differences in clinical features, haematological findings and CD4+ cell counts. Nutrition journal. 2006;5:1-7. [CrossRef]
- Moramarco S, Amerio G, Ciarlantini C, Chipoma JK, Simpungwe MK, Nielsen-Saines K, et al. Community-Based Management of Child Malnutrition in Zambia: HIV/AIDS Infection and Other Risk Factors on Child Survival. Int J Environ Res Public Health. 2016;13(7):666. [CrossRef]
- Sudawa A, Ahmad AA, Adeleke S, Umar L, Rogo LD. HIV Infection among Under-Five Malnourished Children in Kano State. World Journal of AIDS. 2013;3(04):350. [CrossRef]
- Atalell KA, Haile RN, Techane MA. Magnitude of tuberculosis and its associated factors among under-five children admitted with severe acute malnutrition to public hospitals in the city of Dire Dawa, Eastern Ethiopia, 2021: multi-center cross-sectional study. IJID regions. 2022;3:256-60. [CrossRef]
- Muzigaba M, Puoane T, Sartorius B, Sanders D. Independent and interactive effects of HIV infection, clinical stage and other comorbidities on survival of children treated for severe malnutrition in rural South Africa: A retrospective multicohort study. South African Journal of Child Health. 2017;11(1):46-53.
- Baraki AG, Akalu TY, Wolde HF, Takele WW, Mamo WN, Derseh B, et al. Time to recovery from severe acute malnutrition and its predictors: a multicentre retrospective follow-up study in Amhara region, north-west Ethiopia. BMJ Open. 2020;10(2):e034583. [CrossRef]
- Kambale RM, Ngaboyeka GA, Ntagazibwa JN, Bisimwa MI, Kasole LY, Habiyambere V, et al. Severe acute malnutrition in children admitted in an Intensive Therapeutic and Feeding Centre of South Kivu, Eastern Democratic Republic of Congo: Why do our patients die? PLoS One. 2020;15(7):e0236022. [CrossRef]
- Bitew ZW, Alebel A, Worku T, Alemu A. Recovery rate and its predictors among children with severe acute malnutrition in Addis Ababa, Ethiopia: A retrospective cohort study. PLoS One. 2020;15(7):e0235259. [CrossRef]
- Mena MB, Dedefo MG, Billoro BB. Treatment Outcome of Severe Acute Malnutrition and Its Determinants among Pediatric Patients in West Ethiopia. Int J Pediatr. 2018;2018:8686501. [CrossRef]
- Kabeta A, Bekele G. Factors associated with treatment outcomes of under-five children with severe acute malnutrition admitted to therapeutic feeding unit of Yirgalem hospital. Clinics Mother Child Health. 2017;14(261):2.
- Banga D, Baren M, Ssonko NV, Sikakulya FK, Tibamwenda Y, Banga C, et al. Comorbidities and Factors Associated with Mortality among Children under Five Years Admitted with Severe Acute Malnutrition in the Nutritional Unit of Jinja Regional Referral Hospital, Eastern Uganda. Int J Pediatr. 2020;2020:7809412. [CrossRef]
- Fikrie A, Alemayehu A, Gebremedhin S. Treatment outcomes and factors affecting time-to-recovery from severe acute malnutrition in 6-59 months old children admitted to a stabilization center in Southern Ethiopia: A retrospective cohort study. Ital J Pediatr. 2019;45(1):46. [CrossRef]
- Abeje AT, Gudayu TW, Malefia YD, Befftu BB. Analysis of hospital records on treatment outcome of severe acute malnutrition: the case of Gondar University Tertiary Hospital. Pediatrics & Therapeutics. 2016;6(2):2161-0665.
- Desta K. Survival status and predictors of mortality among children aged 0–59 months with severe acute malnutrition admitted to stabilization center at Sekota Hospital Waghemra Zone. J Nutr Disord Ther. 2015;5(2):1-1.
- Negussie AS, Tadesse AW. Predictors of undesirable treatment outcomes of severe acute malnutrition among inpatient children in Addis Ababa, Ethiopia: a retrospective cohort study. BMC Public Health. 2020;20(1):1532. [CrossRef]
- Ikobah JM, Uhegbu K, Akpan F, Muoneke L, Ekanem E. Predictors of In-Patient Mortality of Severe Acute Malnutrition of Hospitalised Children in a Tertiary Facility in Southern Nigeria. Cureus. 2022;14(4):e24195. [CrossRef]
- Mekuria G, Derese T, Hailu G. Treatment outcome and associated factors of severe acute malnutrition among 6-59 months old children in Debre Markos and Finote Selam hospitals, Northwest Ethiopia: a retrospective cohort study. BMC Nutr. 2017;3:42.
- Nabukeera-Barungi N, Grenov B, Lanyero B, Namusoke H, Mupere E, Christensen VB, et al. Predictors of mortality among hospitalized children with severe acute malnutrition: a prospective study from Uganda. Pediatric research. 2018;84(1):92-8. [CrossRef]
- Desyibelew HD, Fekadu A, Woldie H. Recovery rate and associated factors of children age 6 to 59 months admitted with severe acute malnutrition at inpatient unit of Bahir Dar Felege Hiwot Referral hospital therapeutic feeding unite, northwest Ethiopia. PLoS One. 2017;12(2):e0171020. [CrossRef]
- Chiabi A, Malangue B, Nguefack S, Dongmo FN, Fru F, Takou V, et al. The clinical spectrum of severe acute malnutrition in children in Cameroon: a hospital-based study in Yaounde, Cameroon. Transl Pediatr. 2017;6(1):32-39. [CrossRef]
- Ba A, Thiongane A, Niang B, Keïta Y, Ly F, Ndongo AA, et al. Outcome after Discharge from Hospital of Children with Complicated Severe Acute Malnutrition and Predictors Factors of Non-Response during Outpatient Treatment, in Senegal. Open Journal of Pediatrics. 2023;13(4):473-83. [CrossRef]
- Asiimwe O, Ndezi G, Nduwimana M, Namukasa F, Mutisya CM, Abdirahman SH, et al. Prevalence, radio-clinical patterns and factors associated with pulmonary tuberculosis among children with severe acute malnutrition: A crossectional study in Uganda.
- Girma T, Kæstel P, Mølgaard C, Michaelsen KF, Hother AL, Friis H. Predictors of oedema among children hospitalized with severe acute malnutrition in Jimma University Hospital, Ethiopia: a cross-sectional study. BMC pediatrics. 2013;13:1-8. [CrossRef]
- Bizuneh FK, Tolossa T, Bekonjo NE, Wakuma B. Time to recovery from severe acute malnutrition and its predictors among children aged 6-59 months at Asosa general hospital, Northwest Ethiopia. A retrospective follow up study. PLoS One. 2022;17(8):e0272930.
- Abate BB, Tilahun BD, Kassie AM, Kassaw MW. Treatment outcome of Severe Acute Malnutrition and associated factors among under-five children in outpatient therapeutics unit in Gubalafto Wereda, North Wollo Zone, Ethiopia, 2019. PLoS One. 2020;15(9):e0238231. [CrossRef]
- Archary M, Adler H, La Russa P, Mahabeer P, Bobat RA. Bacterial infections in HIV-infected children admitted with severe acute malnutrition in Durban, South Africa. Paediatr Int Child Health. 2017;37(1):6-13. [CrossRef]
- Aye A, Amare F, Sosengo T. Treatment outcomes and associated factors among children with severe acute malnutrition at Hiwot Fana Specialized University Hospital, Harar, Eastern Ethiopia: a retrospective cohort study. Sudan J Paediatr. 2023;23(1):32-41. [CrossRef]
- Adem F, Edessa D, Bayissa B, Mohammed Hassen M, Mohammed MA. Treatment Outcomes and Associated Factors in Hospitalised Children with Severe Acute Malnutrition: A Prospective Cohort Study. Pediatric Health Med Ther. 2020;11:235-243. [CrossRef]
- Mody A, Bartz S, Hornik CP, Kiyimba T, Bain J, Muehlbauer M, et al. Effects of HIV infection on the metabolic and hormonal status of children with severe acute malnutrition. PLoS One. 2014;9(7):e102233. [CrossRef]
- Hussen Kabthymer R, Gizaw G, Belachew T. Time to Cure and Predictors of Recovery Among Children Aged 6-59 Months with Severe Acute Malnutrition Admitted in Jimma University Medical Center, Southwest Ethiopia: A Retrospective Cohort Study. Clin Epidemiol. 2020;12:1149-1159. [CrossRef]
- Vonasek BJ, Kumwenda T, Gumulira J, Nyirongo M, Heller T, Palmer M, et al. Point-of-Care Ultrasound for Tuberculosis in Young Children with Severe Acute Malnutrition. Pediatr Infect Dis J. 2024;43(2):e65-e67. [CrossRef]
- Wake AD. Survival Status and Predictors of Tuberculosis Development Among Under 5 Children Admitted With Severe Acute Malnutrition in Ethiopia: A Retrospective Cohort Study. Glob Pediatr Health. 2024;11:2333794X231226071. [CrossRef]
- Kassaw A, Amare D, Birhanu M, Tesfaw A, Zeleke S, Arage G, et al. Survival and predictors of mortality among severe acute malnourished under-five children admitted at Felege-Hiwot comprehensive specialized hospital, northwest, Ethiopia: a retrospective cohort study. BMC Pediatr. 2021;21(1):176. [CrossRef]
- Nduhukire T, Atwine D, Rachel L, Byonanebye JE. Predictors of in-hospital mortality among under-five children with severe acute malnutrition in South-Western Uganda. PLoS One. 2020;15(6):e0234343. [CrossRef]
- Ngari MM, Obiero C, Mwangome MK, Nyaguara A, Mturi N, Murunga S, et al. Mortality during and following hospital admission among school-aged children: a cohort study. Wellcome Open Res. 2021;5:234.
- Amadi B, Kelly P, Mwiya M, Mulwazi E, Sianongo S, Changwe F, et al. Intestinal and systemic infection, HIV, and mortality in Zambian children with persistent diarrhea and malnutrition. J Pediatr Gastroenterol Nutr. 2001;32(5):550-4.
- Nalwanga D, Musiime V, Kizito S, Kiggundu JB, Batte A, Musoke P, et al. Mortality among children under five years admitted for routine care of severe acute malnutrition: a prospective cohort study from Kampala, Uganda. BMC Pediatr. 2020;20(1):182. [CrossRef]
- Suliman OS, Salih MA, Karrar ZA, Mohammed AO, Helsing C. Infection and immunoglobulin levels in Sudanese children with severe protein-energy malnutrition. Sudan J Paediatr. 2011;11(2):32-42.
- Rytter MJ, Babirekere-Iriso E, Namusoke H, Christensen VB, Michaelsen KF, Ritz C, et al. Risk factors for death in children during inpatient treatment of severe acute malnutrition: a prospective cohort study. Am J Clin Nutr. 2017;105(2):494-502. [CrossRef]
- Ahmed JA, Yusuf N, Wilfong T, Tukeni KN, Berhanu H, Roba KT. Treatment outcomes among children admitted stabilization centers in Eastern Ethiopia: retrospective study. Front Public Health. 2023;11:1165858. [CrossRef]
- Asare H, Carboo J, Nel ED, Dolman RC, Conradie C, Lombard MJ, et al. Mortality in relation to profiles of clinical features in Ghanaian severely undernourished children aged 0-59 months: an observational study. Br J Nutr. 2021;125(10):1157-1165. [CrossRef]
- Irena AH, Mwambazi M, Mulenga V. Diarrhea is a major killer of children with severe acute malnutrition admitted to inpatient set-up in Lusaka, Zambia. Nutr J. 2011;10:110. [CrossRef]
- Muwanguzi E, Oboi JE, Nabbamba A, Wanyama R. Treatment outcome and associated factors for severely malnourished children (1-5 years) admitted to Lacor Hospital and Gulu Regional Referral Hospital in Uganda. J Nutr Sci. 2021;10:e33. [CrossRef]
- Bourke CD, Berkley JA, Prendergast AJ. Immune Dysfunction as a Cause and Consequence of Malnutrition. Trends Immunol. 2016;37(6):386-398. [CrossRef]
- Schaible UE, Kaufmann SH. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med. 2007;4(5):e115.
- Mwene-Batu P, Bisimwa G, Baguma M, Chabwine J, Bapolisi A, Chimanuka C, et al. Long-term effects of severe acute malnutrition during childhood on adult cognitive, academic and behavioural development in African fragile countries: The Lwiro cohort study in Democratic Republic of the Congo. PLoS One. 2020;15(12):e0244486. [CrossRef]
- Toska E, Laurenzi CA, Roberts KJ, Cluver L, Sherr L. Adolescent mothers affected by HIV and their children: A scoping review of evidence and experiences from sub-Saharan Africa. Glob Public Health. 2020;15(11):1655-1673. [CrossRef]
- Chilaka VN, Konje JC. HIV in pregnancy - An update. Eur J Obstet Gynecol Reprod Biol. 2021;256:484-491.
- Transactional sex and HIV risk: from analysis to action. Geneva: Joint United Nations Programme on HIV/AIDS and STRIVE; 2018.
- Rezazadeh L, Ostadrahimi A, Tutunchi H, Naemi Kermanshahi M, Pourmoradian S. Nutrition interventions to address nutritional problems in HIV-positive patients: translating knowledge into practice. J Health Popul Nutr. 2023;42(1):94. [CrossRef]
- Vonasek BJ, Radtke KK, Vaz P, Buck WC, Chabala C, McCollum ED, et al. Tuberculosis in children with severe acute malnutrition. Expert Rev Respir Med. 2022;16(3):273-284. [CrossRef]
- Sinha P, Davis J, Saag L, Wanke C, Salgame P, Mesick J, et al. Undernutrition and Tuberculosis: Public Health Implications. J Infect Dis. 2019;219(9):1356-1363. [CrossRef]
- Lönnroth K, Castro KG, Chakaya JM, Chauhan LS, Floyd K, Glaziou P, et al. Tuberculosis control and elimination 2010-50: cure, care, and social development. Lancet. 2010;375(9728):1814-29.
- Franco JV, Bongaerts B, Metzendorf MI, Risso A, Guo Y, Peña Silva L, et al. Undernutrition as a risk factor for tuberculosis disease. Cochrane Database Syst Rev. 2024;6(6):CD015890.
- Denning DW. Global incidence and mortality of severe fungal disease. Lancet Infect Dis. 2024;24(7):e428-e438. [CrossRef]
| Location/ Country |
Type of Study | HB/CB/ OTP |
Study period | Study population | Sample size (n) | Age range or Median age | Number of Pathogens/Infection cases (n) | Fatality rates | Authors/Year of publication | No. of reference | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| South Africa | Prospective, observational study | HB | NS | SAM | 113 | < 5 years | HIV (n=58), TB (n=27) | 11.5% (n=13) | De Maayer et al 2011 | [13] | |||||||
| aEthiopia | Retrospective cohort study | HB | 2013 to 2015 | SAM | 545 | < 5 years | Malaria (n=37), TB (n=41) |
9.3% (n=51) | Girum et al 2017 | [14] | |||||||
| Sierra Leone | Descriptive cross-sectional study | HB | Over 6 months in 2018 | SAM | 74 | Median age of 11 months | TB (n=20) | - | Ide et al, 2019 | [15] | |||||||
| Zambia | Retrospective study | HB | 2009 to 2013 | SAM | 9,450 | 0 to 59 months | TB (n=151) | 56% (n=84) | Munthali et al 2017 | [16] | |||||||
| Mozambique | Retrospective study | HB | February to August 2018 | SAM | 45 | 0 to 59 months | TB (n=17) | - | Osorio et al. 2020 | [17] | |||||||
| aSouth Africa | Cross-sectional study | HB | 2014 – 2018 | SAM | 956 | Children under 5 years | HIV (n=181) TB (n=127) Malaria (n=4) |
25.9% (n=248) | Gavhi et al.2019(2020) | [18] | |||||||
| Uganda | Cross-sectional study | HB | June 2021 to December 2022 | SAM | 797 | 1 month to 5 years | HIV (n=76) | - | Musiime et al. 2024 | [19] | |||||||
|
bZambia/ Zimbabwe |
Prospective cohort study | HB | July 2016 and March 2019 | SAM | 649 | 1 to 59 months | HIV (n=130) | 8.5% (n=55) | Bwakura-Dangarembizi et al, 2021 | [20] | |||||||
| Malawi | Prospective cohort study | HB | NS | SAM | 454 | 6 to 59 months | HIV (n=79) | 14.8% (n=67) | Chinkhumba et al, 2008 | [21] | |||||||
| aNiger | Prospective study | HB | November 2007 to July 2008 | Complicated SAM | 311 | 6 to 59 months | Bacteremia, n=79, malaria parasite, n=44, enteric pathogens isolated from stool (bacteria, n=36, viruses, n=23, intestinal parasites, n=6), TB (n=4), pathogens isolated from the urinary tract (bacteria, n=48), pathogens identified from nasal swabs (viruses, n=5) | 9% (n=29) | Page et al, 2013 | [22] | |||||||
| Mozambique | Retrospective observational study | HB | March 2016 to February 2017 | SAM | 1,231 | 0 to 5 years | HIV (n=157) | - | Calgaro et al, 2021 | [23] | |||||||
| Ethiopia | Cross-sectional study | HB | April – June 2020 | SAM | 208 | 6 to 59 | HIV (n=11) | - | Teshale et al, 2023 | [24] | |||||||
| aEthiopia | Retrospective cohort study | HB | January 2012 to December 2015 | SAM | 500 | Under 5 years | TB (n=15) | 7% (NS) | Yohannes et al, 2017 | [25] | |||||||
| aMozambique | Cross-sectional study | HB | January 2018 to March 2020 | Undernourished children | 449 | 1 to 14 years | HIV (n=120), malaria (n=12), intestinal parasitic infections (n=90) | - | Cossa-Moiane et al, 2024 | [26] | |||||||
| Zambia | Retrospective study | CB | October 2009 and September 2012 | SAM (n=1,195) MAM (n=664) | 1,859 | Median age of 16 months | HIV in children with SAM (n=134) HIV in children with MAM (n=51) |
2.9% (n=53) | Amadi et al, 2016 | [27] | |||||||
| aSouth Africa | Retrospective cohort study | HB | October 2014 to December 2018. | SAM | 126 | 0 to 59 months | HIV (n=23), TB (n=17) | 15.1 % (n=19) | Heydenrych et al, 2024 | [28] | |||||||
| aGhana | Cross-sectional prospective study | HB | February 2010 to October 2010 | SAM | 246 | 3 months to 13 years | HIV (n=67), TB (n=23), malaria (n=34), bacteremia (n=85) | 17.5% (n=43) | Asafo-Agyei et al 2013 | [29] | |||||||
| aEthiopia | Retrospective follow-up study | HB | March to April, 2018 | SAM | 398 | 6 to 59 months | HIV (n=1), malaria (n=76), TB (n=27) | - | Wondim et al, 2020 | [30] | |||||||
| aEthiopia | Retrospective cohort study | HB | September 2017 to March 2020. | Complicated SAM | 665 | 0 to 59 months | HIV (n=5), TB (n=23), malaria (n=2) | 9% (60) | Oumer et al, 2021 | [31] | |||||||
| Sudan | Prospective hospital-based study | HB | April to October 2018 | SAM | 376 | 6 to 59 months | Malaria (n=131), intestinal parasites (n=24) | 3.7% (n=14) | Bilal et al, 2020 | [32] | |||||||
| Kenya | Prospective descriptive study | HB | June 2005 to June 2009 | SAM | 1,206 | 6 to 12 years | HIV (n=229), malaria parasitemia (n=227), bacteremia (n=86) | 16% (194) | Talbert et al, 2012 | [33] | |||||||
| Malawi | Cross-sectional observational study | HB | February to May 2012 | SAM | 300 | 6 to 60 months | HIV (n=52), TB (n=2) | 9.7% (n=29) | LaCourse et al. 2014 | [34] | |||||||
| bKenya/Tanzania | A retrospective study | HB | 2004 to 2005 | SAM | 1121 | NS | Malaria (n=404), candidiasis (n=119), TB (n=293) | 19% (n=64) 28% (n=222) |
Sunguya et al, 2006 | [35] | |||||||
| Niger | Cross-sectional study | HB | 2016 to 2017 | SAM | 202 | < 5 years | TB (n=90) | 19.6% (n=20) | Schramm et al. 2021 | [36] | |||||||
| aUganda | Prospective study | HB | September-November 2003 and September-December 2004 | SAM | 450 | < 60 months | HIV (n=151), bacteremia (n=76) | 28.9% (n=22) | Bachou et al, 2006 | [37] | |||||||
| Zambia | Retrospective | CB | 2012 to 2014 | SAM | 858 | 6 to 59 months | HIV (n=63), malaria (n=7) | 5.6% (n=48) | Moramarco et al, 2016 | [38] | |||||||
| Nigeria | Cross-sectional study | HB | - | SAM | 400 | < 5 years | HIV (n=31) | - | Sudawa et al, 2013 | [39] | |||||||
| aEthiopia | Retrospective cross-sectional study | HB | 2018 – 2020 | SAM | 414 | < 5 years | Malaria (n=7), HIV (n=20), TB (n=43) | - | Atalell et al, 2021 | [40] | |||||||
| aSouth Africa | A retrospective multicohort study | HB | 2009 – 2013 | SAM | 454 | 6 to 60 months | HIV (n=196) | 24.4% (n=108) | Muzigaba et al, 2017 | [41] | |||||||
| aEthiopia | Retrospective | HB | 2012 - 2016 | SAM | 1690 | The majority of the participants were < 2 years | TB (n=107), HIV (n=54) | - | Baraki et al, 2020 | [42] | |||||||
| aDemocratic Republic of Congo | Retrospective | HB | 2017 - 2018 | SAM | 633 | 1 month to 18 years | HIV (n=14), malaria (n=33), bacteremia (n=38) | 9.2% (n=58) | Kambale et al, 2020 | [43] | |||||||
| aEthiopia | Retrospective cohort study | HB | 2012 – 2019, (may to June 2019) | SAM | 515 | Majority were < 24 months | TB (n=71) | 9% (n=46) | Bitew et al, 2020 | [44] | |||||||
| aEthiopia | Retrospective cross-sectional study | HB | 2015 - 2017 | SAM | 205 | 1 month – 14 years | HIV (n=21), TB (n=16), malaria (n=30) | 4.4% (n=9) | Mena et al, 2018 | [45] | |||||||
| aEthiopia | Retrospective study | HB | 2013 - 2015 | SAM | 196 | Median age: 12+8.5 months. | TB (n=27), malaria (n=2) | 16% (NS) | Kabeta et al, 2017 | [46] | |||||||
| aUganda | Analytical and Descriptive Prospective Cohort Study | HB | July to September 2019 | SAM | 338 | < 5 years | Malaria (n=72), bacteremia (n=23), HIV (n=20), TB (n=17) | 14.5% (49) | Banga et al, 2020 | [47] | |||||||
| aEthiopia | Retrospective cohort study | HB | 2015 to 2017 | SAM | 420 | 6 to 59 months | HIV (n=3), TB (n=87), malaria (n=10) | 10.8% (n=41) | Fikrie et al, 2019 | [48] | |||||||
| aEthiopia | Cross-sectional study | HB | 2010 to 2012 | SAM | 298 | 2 to 59 months | HIV (n=5) | 11.7% (n=35) | Abeje et al 2016 | [49] | |||||||
| aEthiopia | A Retrospective Cohort Study | HB | 2011 to 2013 | SAM | 415 | 0 to 59 months | TB (n=9), HIV (n=17), malaria (n=77) | 28.7% (n=119) | Desta et al, 2015 | [50] | |||||||
| aEthiopia | A Retrospective Cohort Study | HB | 2013 to 2016 | Complicated SAM | 259 | 6 to 59 months | TB (n=18), HIV (n=11) | 12.2% (n=37) | Negussie et al, 2020 | [51] | |||||||
| aNigeria | Prospective cohort study | HB | 2017 to 2019 | SAM | 100 | Mean age: 14.28 ± 14.04 months | HIV (n=81), TB (n=79) | 7.7% (NS) | Ikobah et al, 2022 | [52] | |||||||
| aEthiopia | Retrospective cohort study | HB | 2014 to 2016 | SAM | 253 | 6 to 59 months | TB (n=19) | 5.5% (n=14) | Mekuria et al, 2017 | [53] | |||||||
| aUganda | Prospective cohort study | HB | 2014 to 2015 | SAM | 400 | 6 to 59 months | HIV (n=43) | 9.8% (39) | Nabukeera-Barungi et al, 2017 | [54] | |||||||
| aEthiopia | Cross-sectional study | HB | 2012 to 2016 | SAM | 401 | 6 to 59 months | TB (n=37), HIV (n=26), malaria (n=13) | 8.5% (n=34) | Desyibelew et al 2017 | [55] | |||||||
| aCameroon | Retrospective study | HB | 2006 to 2015 | SAM | 179 | < 15 years | Malaria (n=27) | 15% (n=27) | Chiabi et al, 2016 | [56] | |||||||
| aSenegal | Descriptive and analytical cross-sectional study | HB | March to November, 2021 | Complicated SAM | 103 | 6 to 59 months | TB (n=2), HIV (n=6) | 2.9% (n=3) | Ba et al, 2023 | [57] | |||||||
| Uganda | Cross sectional study | HB | 2023 - 2024 | SAM | 137 | 6-59 months | TB (n=32) | - | Asiimwe et al, 2024 | [58] | |||||||
| aEthiopia | Cross sectional study | HB | Not stated | SAM | 351 | 0.5-14 years | HIV (n=9), TB (n=17), malaria (n=9) | - | Girma et al 2013 | [59] | |||||||
| aEthiopia | Retrospective study | HB | 2015 - 2019 | SAM | 454 | 6 – 59 months | HIV (n=15), TB (n=35) | - | Bizuneh et al 2022 | [60] | |||||||
| aEthiopia | Retrospective cohort study | OTP | 2016 - 2019 | SAM | 600 | Birth to 59 months | HIV (n=12), TB (n=12) | 2.0% (n=12) | Abate et al 2020 | [61] | |||||||
| South Africa | Prospective | HB | 2012 - 2015 | SAM | 82 | 1 month to 10.6 years | HIV (n=82), Bacteria (n=51) | - | Archary et al, 2016 | [62] | |||||||
| aEthiopia | A retrospective cohort study | HB | January to February, 2021 | SAM | 162 | 6 – 59 months | Malaria (n=9), HIV (n=12) | 6.8% (n=11) | Aye et al, 2023 | [63] | |||||||
| aEthiopia | A prospective cohort study | HB | March to July, 2018 | SAM | 133 | 6 – 59 months | TB (n=24), HIV (n=3), malaria (n=3) | 3.8% (NS) | Adem et al, 2020 | [64] | |||||||
| Uganda | A prospective cohort study | HB | 2010 - 2011 | SAM | 74 | 6 months – 5 years | HIV (n=18), malaria (n=7) | 12% (n=9) | Mody et all, 2014 | [65] | |||||||
| Ethiopia | A Retrospective Cohort Study | HB | 2015 – 2017 | SAM | 375 | 6 – 59 months | HIV (n=15), TB (n=54), malaria (n=21) | 12.3% (n=43) | Kabthymer et al, 2020 | [66] | |||||||
| Malawi | Prospective observational study | HB | 2021 - 2022 | Complicated SAM | 131 | 6 – 59 months | TB (n=4) | - | Vonasek et al, 2024 | [67] | |||||||
| Ethiopia | Retrospective cohort study | HB | 2018 - 2022 | SAM | 247 | < 5 years | TB (n=24) | - | Wake et al, 2024 | [68] | |||||||
| aEthiopia | Retrospective, Cohort study | HB | 2016 to 2019 | SAM | 476 | < 5 years | HIV (n=31) TB (n=61) |
11.3% (n=54) | Kassaw et al 2021 | [69] | |||||||
| Uganda | Prospective cohort study | HB | June to August 2015 | SAM | 122 | Children under 5 years | HIV (n=9) Malaria (n=25) |
- | Nduhukire et al.2020 | [70] | |||||||
| Kenya | Retrospective cohort study | HB | 2007-2016 | SAM | 3090 | 5-12yrs | HIV (n=197) | 3.4% (n=132) | Ngari et al, 2021 | [71] | |||||||
| Zambia | Cross-sectional study | HB | 19982000 | SAM | 200 | 6 to 24months | HIV (n=106), TB (n=27), bacteremia (n=26), Intesstinal infection [Cryptosporidium parvum (n=47), Isospora belli (n=4), Giardia intestinalis (n=11), Blastocystis hominis (n=4), Microsporidia (n=1), Salmonella spp. (n=35), Shigella spp.(n=4), Vibrio cholerae (n=6), Hookworm (n=3), Ascaris lumbricoides (n=10), Yeast cells (n=74) | 19.5% (39) | Amadi et al, 2001 | [72] | |||||||
| Uganda | Prospective cohort study | HB | November 2007 to July 2008 | SAM | 270 | <5yrs | HIV (n=33) | 25% (n=67) | Nwalanga et al 2020 | [73] | |||||||
| aSudan | Case control study | HB | 1992-1993 | SAM | 81 | 0 to 5 years | TB (n=8), intestinal parasitic infection (n=24), UTI [(E. coli, (n=6), Proteus species (n=2), Klebsiella species (n=2)] | - | Suliman et al, 2011 | [74] | |||||||
| aUganda | Prospective observational study | HB | 2012 - 2013 | SAM | 120 | 6 – 59 months | HIV (n=20) | 14% (n=17) | Rytter et al, 2017 | [75] | |||||||
| aEthiopia | Retrospective cohort study | HB | December 10-30, 2021 | SAM | 712 | 6 months to 59 months | TB (n=43), HIV (n=3) |
5.9% | Ahmed et al, 2023 | [76] | |||||||
| aGhana | Prospective observational study | HB | 2013 to 2018 | SAM | 601 | 0 to 59 months | HIV (54), TB (n=32), malaria(n=110) | 16.5% (n=99) | Asare et al, 2021 | [77] | |||||||
| Zambia | Cohort study | HB | August - December 2009 | Complicated SAM | 430 | 6 months to 59 months | HIV (n=161) TB (n=6) |
40.5% (n=174) | Irena et al 2013 | [78] | |||||||
| Uganda | Retrospective observational study | HB | January to December 2017 | Complicated SAM | 330 | 1-5yrs | HIV (n=86) | 22% (70) | Muwanguzi et al, 2021 | [79] | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





