Submitted:
16 September 2024
Posted:
17 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Data and Methods
2.1. Data Source
2.2. Methodology
3. Results and Discussion
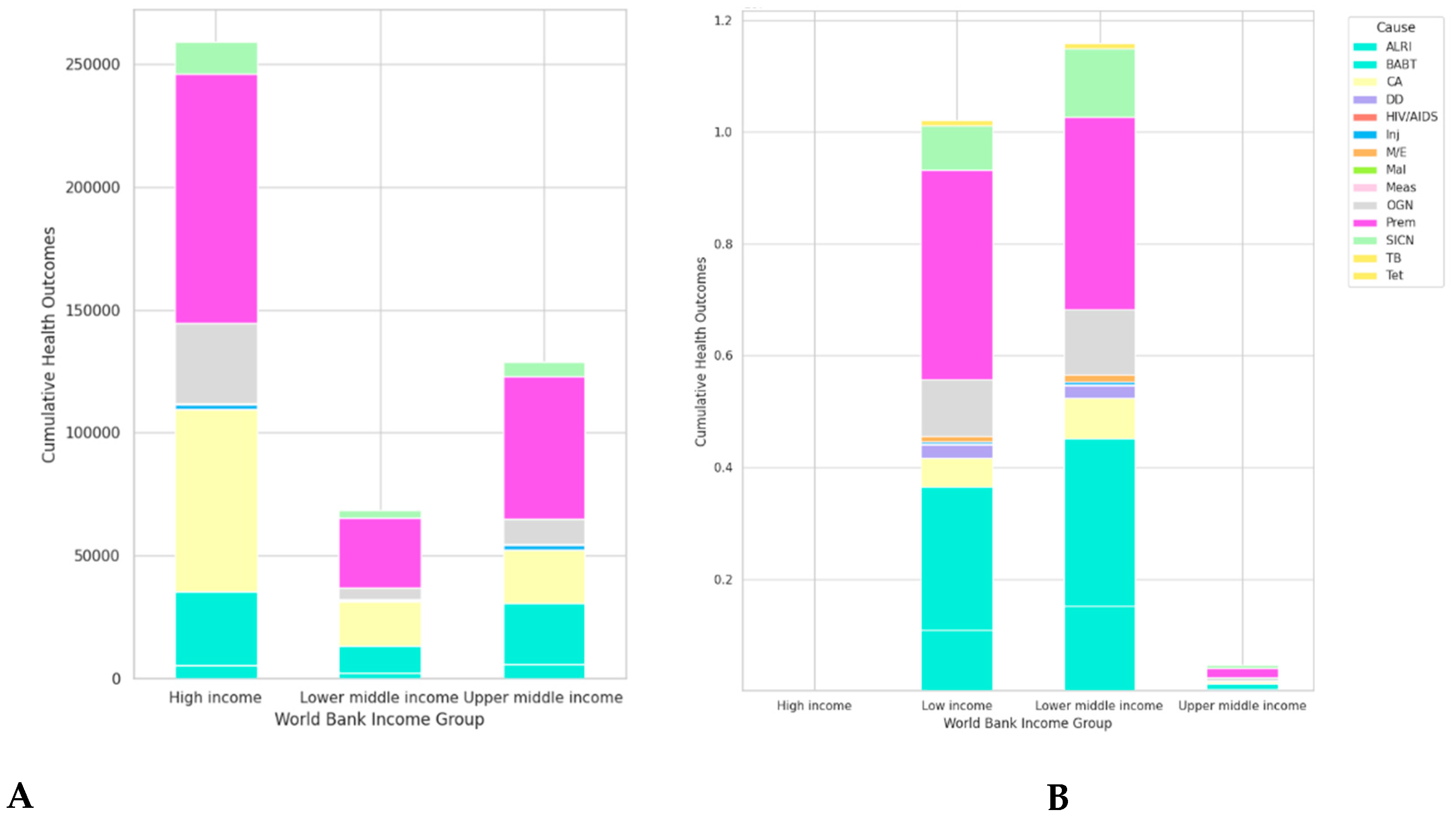
3.1. Health Outcomes by Cause and Income Group in European and African Countries
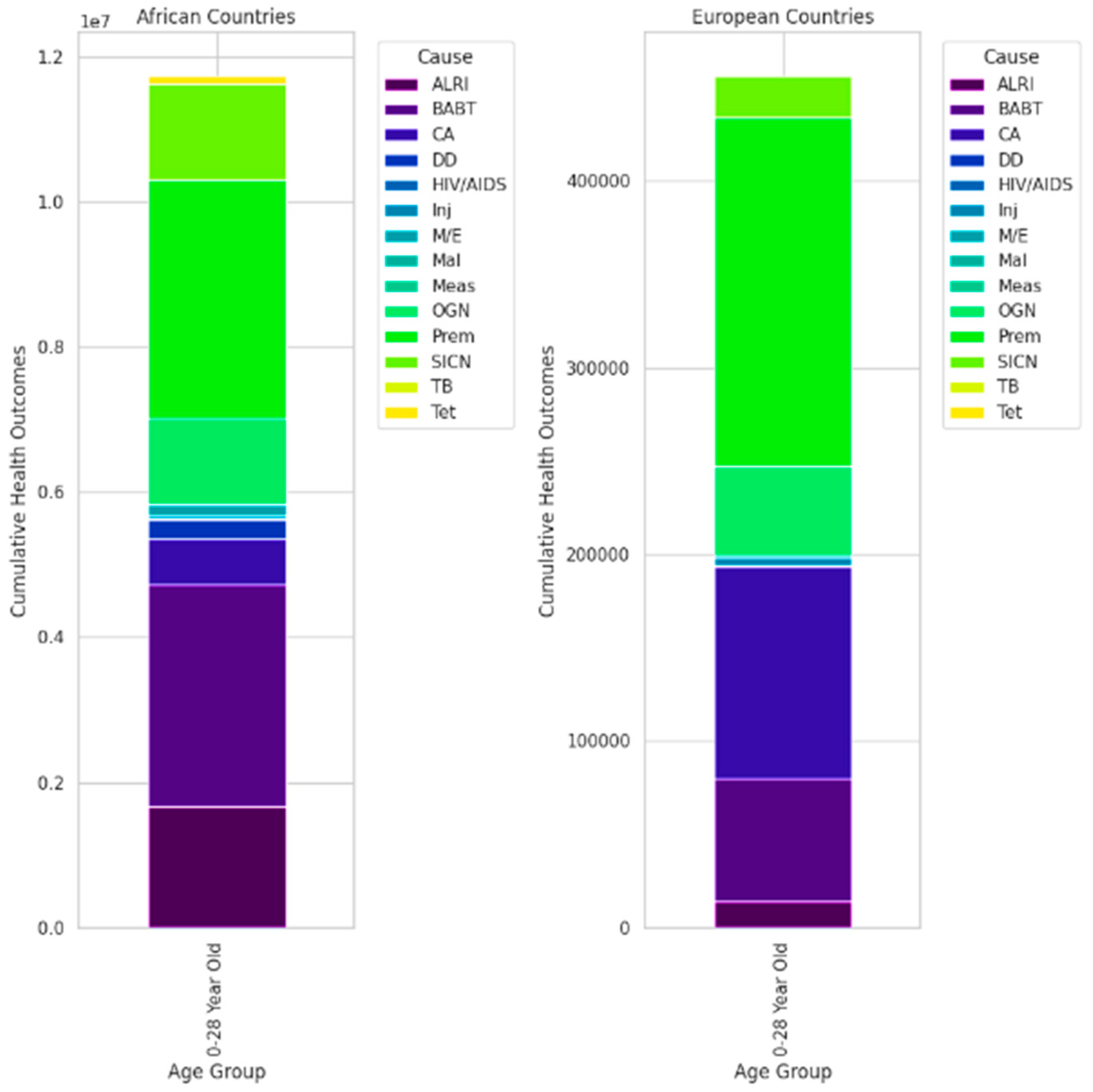
3.2. Age-Specific Health Conditions in European and African Countries
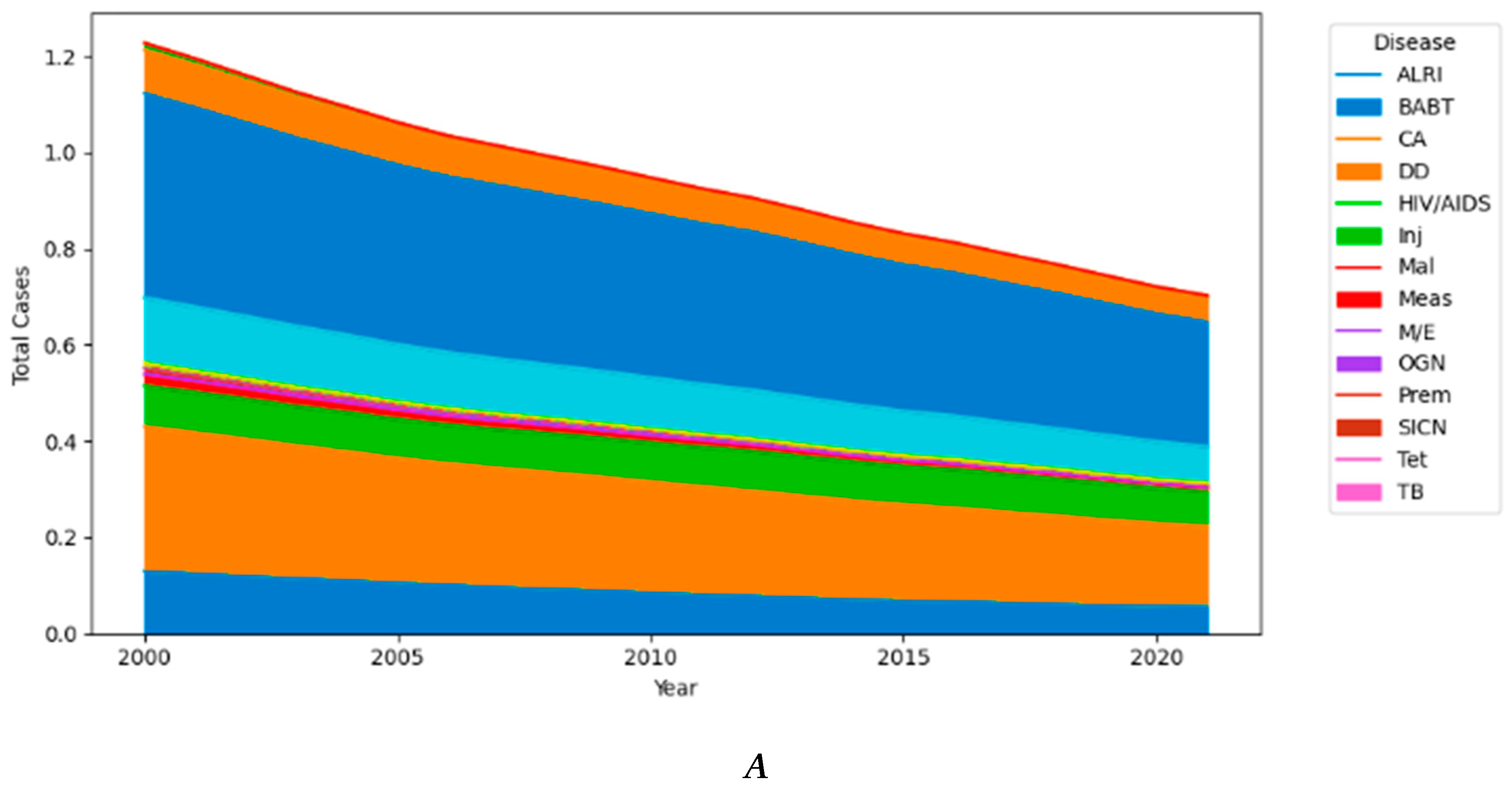
3.3. Trend of Diseases Over Time in European Countries
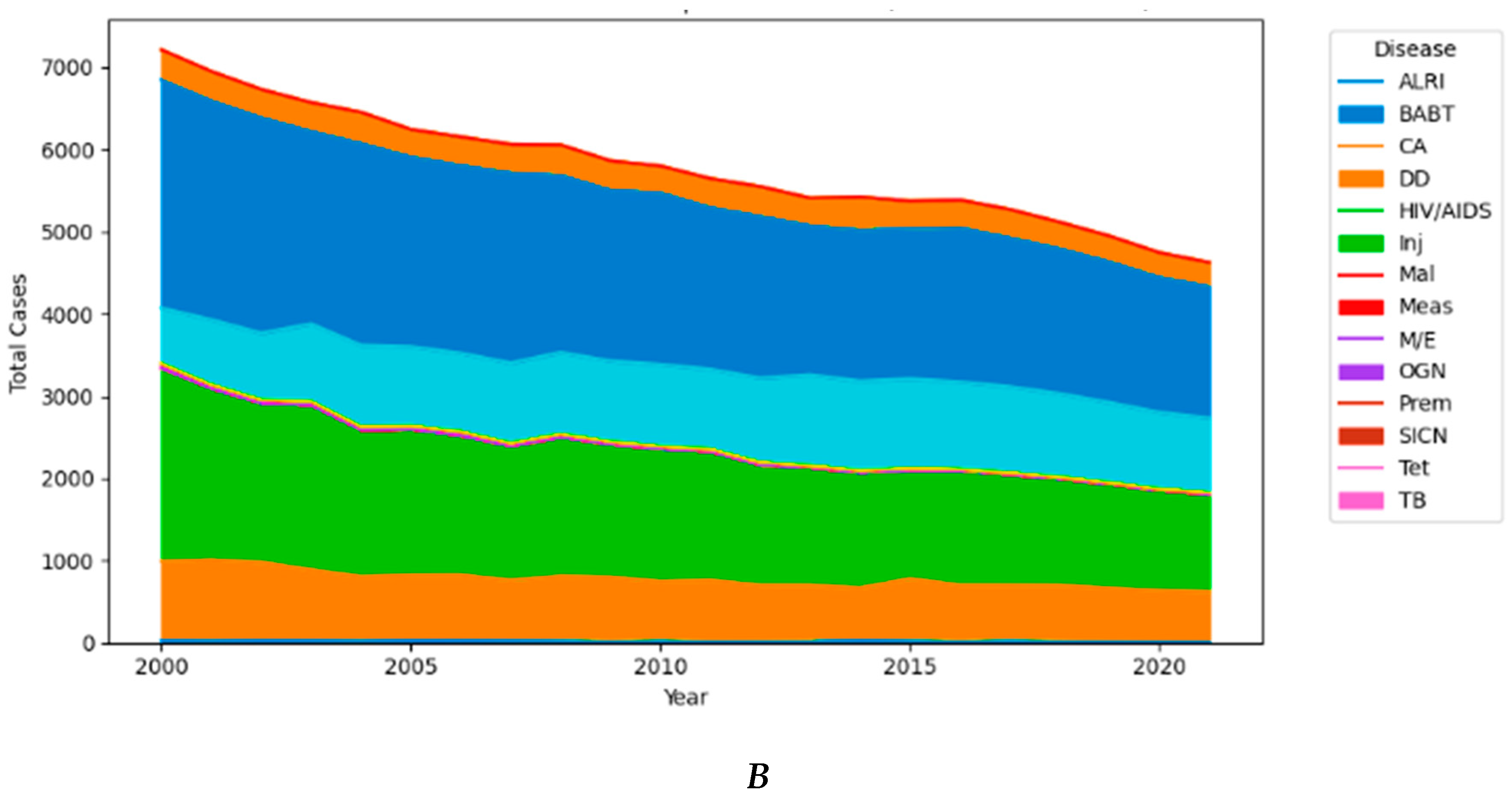
3.4. Contrasting Health Profiles between Africa vs. Europe
4. Conclusion
Author Contributions
Funding
Data Availability
Ethics Approval
Consent to Participate
Consent for Publication
Competing Interests
References
- Abbott, L. and Williams, C. (2015). Influences of social determinants of health on african americans living with hiv in the rural southeast: a qualitative meta-synthesis. Journal of the Association of Nurses in Aids Care, 26(4), 340-356. [CrossRef]
- Aborode, A., David, K., Uwishema, O., Nathaniel, A., Imisioluwa, J., Onigbinde, S., … & Farooq, F. (2021). Fighting covid-19 at the expense of malaria in africa: the consequences and policy options. American Journal of Tropical Medicine and Hygiene, 104(1), 26-29. [CrossRef]
- Abuzerr, S., Nasseri, S., Yunesian, M., Mirfazaelian, H., Mahvi, A., Nabizadeh, R., … & Mustafa, A. (2019). Prevalence of diarrheal illness and healthcare-seeking behavior by age-group and sex among the population of gaza strip: a community-based cross-sectional study. BMC Public Health, 19(1). [CrossRef]
- Adam, M., Wang, J., Enan, K., Shen, H., Wang, H., Hussein, A., … & Ma, X. (2018). Molecular survey of viral and bacterial causes of childhood diarrhea in khartoum state, sudan. Frontiers in Microbiology, 9. [CrossRef]
- Adeboyejo, T., Matamale, L., & Kharidza, S. (2012). Impact of climate change on children’s health in limpopo province, south africa. International Journal of Environmental Research and Public Health, 9(3), 831-854. [CrossRef]
- Adler, N. and Newman, K. (2002). Socioeconomic disparities in health: pathways and policies. Health Affairs, 21(2), 60-76. [CrossRef]
- Alexander, K., Carzolio, M., Goodin, D., & Vance, E. (2013). Climate change is likely to worsen the public health threat of diarrheal disease in botswana. International Journal of Environmental Research and Public Health, 10(4), 1202-1230. [CrossRef]
- Anderson, D., Rees, D., & Wang, T. (2020). The phenomenon of summer diarrhea and its waning, 1910-1930. Explorations in Economic History, 78, 101341. [CrossRef]
- Armah, G., Pringle, K., Enweronu-Laryea, C., Ansong, D., Mwenda, J., Diamenu, S., … & Lopman, B. (2016). Impact and effectiveness of monovalent rotavirus vaccine against severe rotavirus diarrhea in ghana. Clinical Infectious Diseases, 62(suppl 2), S200-S207. [CrossRef]
- Asefa, A., Qanche, Q., Asaye, Z., & Abebe, L. (2020). <p>determinants of delayed treatment-seeking for childhood diarrheal diseases in southwest ethiopia: a case–control study</p>. Pediatric Health Medicine and Therapeutics, Volume 11, 171-178. [CrossRef]
- Baryarama, F., Mugisha, J., & Luboobi, L. (2006). Mathematical model for hiv/aids with complacency in a population with declining prevalence. Computational and Mathematical Methods in Medicine, 7(1), 27-35. [CrossRef]
- Battle, K. E., Lucas, T. C. D., Nguyen, M., Howes, R. E., Nandi, A. K., Twohig, K. A., Pfeffer, D. A., Cameron, E., Rao, P. C., Casey, D., Gibson, H. S., Rozier, J. A., Dalrymple, U., Keddie, S. H., Collins, E. L., Harris, J. R., Guerra, C. A., Thorn, M. P., Bisanzio, D.,... Gething, P. W. (2019). Mapping the global endemicity and clinical burden of Plasmodium vivax, 2000–17: a spatial and temporal modelling study. Lancet, 394(10195), 332–343. [CrossRef]
- Bayero, S., Safiyanu, B., & Gurin, I. (2022). The impact of health expenditure on maternal and child mortality in african countries. International Review of Social Sciences Research, 2(3), 20-36. [CrossRef]
- Beckman, A., Herrin, J., Nasir, K., Desai, N., & Spatz, E. (2017). Trends in cardiovascular health of us adults by income, 2005-2014. Jama Cardiology, 2(7), 814. [CrossRef]
- Bekele, M., Urgessa, M., Kumsa, K., & Sinba, E. (2023). Contributing factors of delay in seeking treatment for childhood diarrheal diseases in berbere woreda, ethiopia: an unmatched case–control study. Journal of Health Population and Nutrition, 42(1). [CrossRef]
- Berry, M., Nickerson, N., & Odum, A. (2017). Delay discounting as an index of sustainable behavior: devaluation of future air quality and implications for public health. International Journal of Environmental Research and Public Health, 14(9), 997. [CrossRef]
- Boniol, M., Kunjumen, T., Nair, T., Siyam, A., Campbell, J., & Diallo, K. (2022). The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage?. BMJ Global Health, 7(6), e009316. [CrossRef]
- Braveman, P. and Gottlieb, L. (2014). The social determinants of health: it's time to consider the causes of the causes. Public Health Reports, 129(1_suppl2), 19-31. [CrossRef]
- Braveman, P., Cubbin, C., Egerter, S., Chideya, S., Marchi, K., Metzler, M., … & Posner, S. (2005). Socioeconomic status in health research. Jama, 294(22), 2879. [CrossRef]
- Canturk, S., Qaddoumi, I., Khetan, V., Ma, Z., Furmanchuk, A., Antoneli, C., … & Chantada, G. (2010). Survival of retinoblastoma in less-developed countries impact of socioeconomic and health-related indicators. British Journal of Ophthalmology, 94(11), 1432-1436. [CrossRef]
- Cappuccio, F. and Miller, M. (2016). Cardiovascular disease and hypertension in sub-saharan africa: burden, risk and interventions. Internal and Emergency Medicine, 11(3), 299-305. [CrossRef]
- Carter, E., Bryce, J., Perin, J., & Newby, H. (2015). Harmful practices in the management of childhood diarrhea in low- and middle-income countries: a systematic review. BMC Public Health, 15(1). [CrossRef]
- Degefa, G., Gebreslassie, M., Meles, K. G., & Jackson, R. (2018). Determinants of delay in timely treatment seeking for diarrheal diseases among mothers with under-five children in central Ethiopia: A case control study. PloS One, 13(3), e0193035. [CrossRef]
- Deguen, S. and Zmirou-Navier, D. (2010). Social inequalities resulting from health risks related to ambient air quality--a european review. European Journal of Public Health, 20(1), 27-35. [CrossRef]
- Dockery, D. (2009). Health effects of particulate air pollution. Annals of Epidemiology, 19(4), 257-263. [CrossRef]
- Dzianach, P., Rumisha, S., Lubinda, J., Saddler, A., Berg, M., Gelaw, Y., … & Weiss, D. (2023). Evaluating covid-19-related disruptions to effective malaria case management in 2020–2021 and its potential effects on malaria burden in sub-saharan africa. Tropical Medicine and Infectious Disease, 8(4), 216. [CrossRef]
- Ezeh, A., Izugbara, C., Kabiru, C., Fonn, S., Kahn, K., Manderson, L., … & Thorogood, M. (2010). Building capacity for public and population health research in africa: the consortium for advanced research training in africa (carta) model. Global Health Action, 3(1), 5693. [CrossRef]
- Fisher, J., Mello, M., Patel, V., Rahman, A., Tran, T., Holton, S., … & Holmes, W. (2011). Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization, 90(2), 139-149H. [CrossRef]
- Galan, D., Kim, S., & Graham, J. (2013). Exploring changes in open defecation prevalence in sub-saharan africa based on national level indices. BMC Public Health, 13(1). [CrossRef]
- Getachew, A., Guadu, T., Tadie, A., Gizaw, Z., Gebrehiwot, M., Cherkos, D., … & Gebrecherkos, T. (2018). Diarrhea prevalence and sociodemographic factors among under-five children in rural areas of north gondar zone, northwest ethiopia. International Journal of Pediatrics, 2018, 1-8. [CrossRef]
- Gething, P., Battle, K., Bhatt, S., Smith, D., Eisele, T., Cibulskis, R., … & Hay, S. (2014). Declining malaria in africa: improving the measurement of progress. Malaria Journal, 13(1). [CrossRef]
- Gouda, H., Charlson, F., Sorsdahl, K., Ahmadzada, S., Ferrari, A., Erskine, H., … & Whiteford, H. (2019). Burden of non-communicable diseases in sub-saharan africa, 1990–2017: results from the global burden of disease study 2017. The Lancet Global Health, 7(10), e1375-e1387. [CrossRef]
- Guo, J., Hernandez, I., Dickson, S., Tang, S., Essien, U., Mair, C., … & Berenbrok, L. (2022). Income disparities in driving distance to health care infrastructure in the united states: a geographic information systems analysis. BMC Research Notes, 15(1). [CrossRef]
- Harerimana, J., Nyirazinyoye, L., Thomson, D., & Ntaganira, J. (2016). Social, economic and environmental risk factors for acute lower respiratory infections among children under five years of age in rwanda. Archives of Public Health, 74(1). [CrossRef]
- Haverkos, H., Chung, R., & Perez, L. (2003). Is there an epidemic of hiv/aids among heterosexuals in the usa?. Postgraduate Medical Journal, 79(934), 444-448. [CrossRef]
- He, G., Pan, Y., & Tanaka, T. (2020). The short-term impacts of covid-19 lockdown on urban air pollution in china. Nature Sustainability, 3(12), 1005-1011. [CrossRef]
- He, Z. (2023). Diarrhea as a disease of poverty among under-five children in sub-saharan africa: a cross-sectional study. Inquiry the Journal of Health Care Organization Provision and Financing, 60. [CrossRef]
- Heaney, A., Shaman, J., & Alexander, K. (2019). El niño-southern oscillation and under-5 diarrhea in botswana. Nature Communications, 10(1). [CrossRef]
- Hedt-Gauthier, B., Jeufack, H., Neufeld, N., Alem, A., Sauer, S., Odhiambo, J., … & Volmink, J. (2019). Stuck in the middle: a systematic review of authorship in collaborative health research in africa, 2014–2016. BMJ Global Health, 4(5), e001853. [CrossRef]
- Irabor, D. (2017). Emergence of colorectal cancer in west africa: accepting the inevitable. Nigerian Medical Journal, 58(3), 87. [CrossRef]
- Isaxon, C., Abera, A., Asfaw, A., Bililign, S., Eriksson, A., Malmqvist, E., … & Roba, K. (2022). A call for action: air pollution, a serious health and economic hazard suffocating africa. Clean Air Journal, 32(2). [CrossRef]
- K., V. (2023). Enhancing logistic support during chemotherapy to nonlocal children with cancer and their families through home away from home program. Indian Journal of Medical and Paediatric Oncology, 45(02), 173-175. [CrossRef]
- Karamagi, H., Charif, A., Kidane, S., Yohanes, T., Kariuki, D., Titus, M., … & Droti, B. (2022). Investments for effective functionality of health systems towards universal health coverage in africa: a scoping review. Plos Global Public Health, 2(9), e0001076. [CrossRef]
- Lal, A., Erondu, N., Heymann, D., Gitahi, G., & Yates, R. (2021). Fragmented health systems in covid-19: rectifying the misalignment between global health security and universal health coverage. The Lancet, 397(10268), 61-67. [CrossRef]
- Lauritano, D., Moreo, G., Campanella, V., Vella, F., & Petruzzi, M. (2021). Oral health status among migrants from middle- and low-income countries to europe: a systematic review. International Journal of Environmental Research and Public Health, 18(22), 12203. [CrossRef]
- Lekana-Douki, S. E., Behillil, S., Enouf, V., Leroy, E. M., & Berthet, N. (2018). Detection of human bocavirus-1 in both nasal and stool specimens from children under 5 years old with influenza-like illnesses or diarrhea in Gabon. BMC Research Notes, 11(1). [CrossRef]
- Levine, M., Kotloff, K., Nataro, J., & Muhsen, K. (2012). The global enteric multicenter study (gems): impetus, rationale, and genesis. Clinical Infectious Diseases, 55(suppl 4), S215-S224. [CrossRef]
- Lopez-Carmen, V. (2022). The “elephants in the room” in u.s. global health: indigenous nations and white settler colonialism. Plos Global Public Health, 2(7), e0000719. [CrossRef]
- Maphumulo, W. and Bhengu, B. (2019). Challenges of quality improvement in the healthcare of south africa post-apartheid: a critical review. Curationis, 42(1). [CrossRef]
- Masiira, B., Antara, S., Kazoora, H., Namusisi, O., Gombe, N., Magazani, A., … & Tshimanga, M. (2020). Building a new platform to support public health emergency response in africa: the afenet corps of disease detectives, 2018–2019. BMJ Global Health, 5(10), e002874. [CrossRef]
- McKone, E., Ariti, C., Jackson, A., Zolin, A., Carr, S., Orenti, A., … & Naehrlich, L. (2021). Survival estimates in european cystic fibrosis patients and the impact of socioeconomic factors: a retrospective registry cohort study. European Respiratory Journal, 58(3), 2002288. [CrossRef]
- Moran, A., Forouzanfar, M., Sampson, U., Chugh, S., Feigin, V., & Mensah, G. (2013). The epidemiology of cardiovascular diseases in sub-saharan africa: the global burden of diseases, injuries and risk factors 2010 study. Progress in Cardiovascular Diseases, 56(3), 234-239. [CrossRef]
- Moshammer, H. and Wallner, P. (2011). Air quality as respiratory health indicator — a critical review. International Journal of Occupational Medicine and Environmental Health, 24(3). [CrossRef]
- Mwenda, J., Ntoto, K., Abebe, A., Enweronu-Laryea, C., Ismail, A., Mchomvu, J., … & Steele, A. (2010). Burden and epidemiology of rotavirus diarrhea in selected african countries: preliminary results from the african rotavirus surveillance network. The Journal of Infectious Diseases, 202(S1), S5-S11. [CrossRef]
- Nkumama, I., O’Meara, W., & Osier, F. (2017). Changes in malaria epidemiology in africa and new challenges for elimination. Trends in Parasitology, 33(2), 128-140. [CrossRef]
- Novignon, J., Olakojo, S., & Nonvignon, J. (2012). The effects of public and private health care expenditure on health status in sub-saharan africa: new evidence from panel data analysis. Health Economics Review, 2(1). [CrossRef]
- Ogunbodede, E., Kida, I., Madjapa, H., Amedari, M., Ehizele, A., Mutave, R., … & Okoye, L. (2015). Oral health inequalities between rural and urban populations of the african and middle east region. Advances in Dental Research, 27(1), 18-25. [CrossRef]
- Okeke, I. (2009). Diarrheagenic escherichia coli in sub-saharan africa: status, uncertainties and necessities. The Journal of Infection in Developing Countries, 3(11), 817-842. [CrossRef]
- Pacheco, A., Saraceni, V., Tuboi, S., Lauria, L., Moulton, L., Faulhaber, J., … & Schechter, M. (2011). Estimating the extent of underreporting of mortality among hiv-infected individuals in rio de janeiro, brazil. Aids Research and Human Retroviruses, 27(1), 25-28. [CrossRef]
- Page, A., Hustache, S., Luquero, F., Djibo, A., Manzo, M., & Grais, R. (2011). Health care seeking behavior for diarrhea in children under 5 in rural niger: results of a cross-sectional survey. BMC Public Health, 11(1). [CrossRef]
- Pop, M., Walker, A., Paulson, J., Lindsay, B., Antonio, M., Hossain, M., … & Stine, O. (2014). Diarrhea in young children from low-income countries leads to large-scale alterations in intestinal microbiota composition. Genome Biology, 15(6), R76. [CrossRef]
- Rohner, E., Bütikofer, L., Schmidlin, K., Sengayi, M., Maskew, M., Giddy, J., … & Bohlius, J. (2019). Cervical cancer risk in women living with hiv across four continents: a multicohort study. International Journal of Cancer, 146(3), 601-609. [CrossRef]
- Rojas-López, M., Monterio, R., Pizza, M., Desvaux, M., & Rosini, R. (2018). Intestinal pathogenic escherichia coli: insights for vaccine development. Frontiers in Microbiology, 9. [CrossRef]
- Simo, F., Bigna, J., Kenmoe, S., Ndangang, M., Temfack, E., Moundipa, P., … & Demanou, M. (2019). Dengue virus infection in people residing in africa: a systematic review and meta-analysis of prevalence studies. Scientific Reports, 9(1). [CrossRef]
- Souza, J., Hunt, B., Asirwa, F., Adebamowo, C., & Lopes, G. (2016). Global health equity: cancer care outcome disparities in high-, middle-, and low-income countries. Journal of Clinical Oncology, 34(1), 6-13. [CrossRef]
- Steele, A., Armah, G., Mwenda, J., & Kirkwood, C. (2023). The full impact of rotavirus vaccines in africa has yet to be realized. Clinical Infectious Diseases, 76(Supplement_1), S1-S4. [CrossRef]
- Tafa, B., Gebrewold, L., Mekuria, W., & Assefa, N. (2023). Molecular epidemiology of respiratory syncytial virus in children with acute respiratory illnesses in africa: a systematic review and meta-analysis. Journal of Global Health, 13. [CrossRef]
- Tafere, Y., Abate, B., Enyew, H., & Mekonnen, A. (2020). Diarrheal diseases in under-five children and associated factors among farta district rural community, amhara regional state, north central ethiopia: a comparative cross-sectional study. Journal of Environmental and Public Health, 2020, 1-7. [CrossRef]
- Tamir, T. (2024). Prevalence of childhood stunting and determinants in low and lower-middle income african countries: evidence from standard demographic and health survey. Plos One, 19(4), e0302212. [CrossRef]
- Tareke, A., Enyew, E., & Takele, B. (2022). Pooled prevalence and associated factors of diarrhea among under-five years children in east africa: a multilevel logistic regression analysis. Plos One, 17(4), e0264559. [CrossRef]
- Vanderpuye, V., Hammad, N., Martei, Y., Hopman, W., Fundytus, A., Sullivan, R., … & Booth, C. (2019). Cancer care workforce in africa: perspectives from a global survey. Infectious Agents and Cancer, 14(1). [CrossRef]
- Vasco, G., Trueba, G., Atherton, R., Calvopiña, M., Cevallos, W., Andrade, T., … & Eisenberg, J. (2014). Identifying etiological agents causing diarrhea in low income ecuadorian communities. American Journal of Tropical Medicine and Hygiene, 91(3), 563-569. [CrossRef]
- Vlismas, K., Stavrinos, V., & Panagiotakos, D. (2009). Socio-economic status, dietary habits and health-related outcomes in various parts of the world: a review. Central European Journal of Public Health, 17(2), 55-63. [CrossRef]
- Wong, E., Choy, R., Zhang, Y., Chu, W., Chen, L., Pang, C., … & Yam, J. (2022). Global retinoblastoma survival and globe preservation: a systematic review and meta-analysis of associations with socioeconomic and health-care factors. The Lancet Global Health, 10(3), e380-e389. [CrossRef]
- Yaya, S., Hudani, A., Udenigwe, O., Shah, V., Ekholuenetale, M., & Bishwajit, G. (2018). Improving water, sanitation and hygiene practices, and housing quality to prevent diarrhea among under-five children in nigeria. Tropical Medicine and Infectious Disease, 3(2), 41. [CrossRef]
- Yuyun, M., Sliwa, K., Kengne, A., Mocumbi, A., & Bukhman, G. (2020). Cardiovascular diseases in sub-saharan africa compared to high-income countries: an epidemiological perspective. Global Heart, 15(1), 15. [CrossRef]
- Boschi-Pinto, C. (2008). Estimating child mortality due to diarrhoea in developing countries. Bulletin of the World Health Organization, 86(9), 710–717. [CrossRef]
- Braveman, P., & Gottlieb, L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports, 129(1_suppl2), 19–31. [CrossRef]
- Denkyira, S. A., Adesola, R. O., Idris, I., Yelarge, K., Asaaseasa, K. T., Danquah, C. A., & Opuni, E. (2022). Marburg virus in Ghana: A public health threat to Ghanaians and to Africans. Public Health Challenges, 1(4). [CrossRef]
- Dhefer, I. H. (2021). Liver damage during infections with coronavirus. Journal of Techniques, 3(2), 79–85. [CrossRef]
- Ferkol, T., & Schraufnagel, D. (2014). The global burden of respiratory disease. Annals of the American Thoracic Society, 11(3), 404–406. [CrossRef]
- Gelband, H., Bogoch, I. I., Rodriguez, P. S., Ngai, M., Peer, N., Watson, L. K., & Jha, P. (2020). Is Malaria an Important Cause of Death among Adults? ˜the œAmerican Journal of Tropical Medicine and Hygiene, 103(1), 41–47. [CrossRef]
- Groves, H. E., Piché-Renaud, P., Peci, A., Farrar, D. S., Buckrell, S., Bancej, C., Sevenhuysen, C., Campigotto, A., Gubbay, J. B., & Morris, S. K. (2021). The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. ˜the œLancet Regional Health. Americas, 1, 100015. [CrossRef]
- Gussow, A. B., Auslander, N., Faure, G., Wolf, Y. I., Zhang, F., & Koonin, E. V. (2020). Genomic determinants of pathogenicity in SARS-CoV-2 and other human coronaviruses. Proceedings of the National Academy of Sciences of the United States of America, 117(26), 15193–15199. [CrossRef]
- Ha, L. T. (2022). Effects of digitalization on financialization: Empirical evidence from European countries. Technology in Society, 68, 101851. [CrossRef]
- Hamdi, Y., Zass, L., Othman, H., Radouani, F., Allali, I., Hanachi, M., Okeke, C. J., Chaouch, M., Tendwa, M. B., Samtal, C., Sallam, R. M., Alsayed, N., Turkson, M., Ahmed, S., Benkahla, A., Romdhane, L., Souiai, O., Bishop, Ö. T., Ghedira, K.,... Kassim, S. K. (2021). Human OMICs and Computational Biology research in Africa: Current challenges and prospects. Omics, 25(4), 213–233. [CrossRef]
- Jaddaoui, I. E., Allali, I., Sehli, S., Ouldim, K., Hamdi, S., Idrissi, N. A., Nejjari, C., Amzazi, S., Bakri, Y., & Ghazal, H. (2020). Cancer omics in Africa: present and prospects. Frontiers in Oncology, 10. [CrossRef]
- Lukamba, R. M., Yao, J. A., Kabesha, T. A., Budiongo, A. N., Monga, B. B., Mwembo, A. T., Bey, P., Chenge, G. B., Desjardins, L., Luboya, O. N., Doz, F., & Stefan, C. D. (2018). Retinoblastoma in Sub-Saharan Africa: Case Studies of the Republic of Côte d’Ivoire and the Democratic Republic of the Congo. Journal of Global Oncology, 4, 1–8. [CrossRef]
- Lukšić, I., Mulić, R., Falconer, R., Orban, M., Sidhu, S., & Rudan, I. (2013). Estimating global and regional morbidity from acute bacterial meningitis in children: assessment of the evidence. Croatian Medical Journal, 54(6), 510–518. [CrossRef]
- Oduoye, M. O., Fatima, E., Muzammil, M. A., Dave, T., Irfan, H., Fariha, F. N. U., Marbell, A., Ubechu, S. C., Scott, G. Y., & Elebesunu, E. E. (2024). Impacts of the advancement in artificial intelligence on laboratory medicine in low- and middle-income countries: Challenges and recommendations—A literature review. Health Science Reports, 7(1). [CrossRef]
- Pennington, B. F., McGrath, L. M., & Peterson, R. L. (2020). Diagnosing Learning Disorders, third edition: From Science to Practice. Guilford Publications.
- Pillay, J. (2022). Difficulties experienced by South African adolescents during COVID-19 lockdown: implications for early mental health interventions. South African Journal of Psychology, 53(2), 211–224. [CrossRef]
- Verhein, K. C., Vellers, H. L., & Kleeberger, S. R. (2018). Inter-individual variation in health and disease associated with pulmonary infectious agents. Mammalian Genome, 29(1–2), 38–47. [CrossRef]
- He, X., Lau, E. H. Y., Wu, P., Deng, X., Wang, J., Hao, X., Lau, Y. C., Wong, J. Y., Guan, Y., Tan, X., Mo, X., Chen, Y., Liao, B., Chen, W., Hu, F., Zhang, Q., Zhong, M., Wu, Y., Zhao, L.,... Leung, G. M. (2020). Temporal dynamics in viral shedding and transmissibility of COVID-19. Nature Medicine, 26(5), 672–675. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




