1. Introduction
Nigeria has historically low rates of utilization of antenatal care (ANC) [
1,
2]. Analysis of the Nigeria 2018 Demographic and Health Survey (DHS) showed only 67% ANC use among women 15-49 with some states in the northwest having a non-utilization rate of over 50% [
2]. This was more pronounced in rural areas with non-utilization rate of 33.8%compared to 10.1% in urban areas. Facility births were lowest in the northwest at 16% compared to 82% in the southeast [
2,
3]. Having no contact with ANC has been observed in up to 25% of women in Nigeria [
3]. Literacy level, living distance to health facility, healthcare experience, and gender relations are among the factors that influence utilization of ANC and contraceptive uptake [
4].
Previous studies had demonstrated the effectiveness of group antenatal care (gANC) in low-and-middle- income countries (LMICs). Group ANC is a concept that involves enable peer-to-peer discussions and sharing of experiences [
5,
6]. This approach seeks to address quality of care and coverage gaps prevalent in conventional individual person-doctor antenatal sessions driven by poor communications and limited counselling time [
5]. In a pre-post quasi-experimental study of over 1,600 women in Kenya, knowledge of three or more danger signals of pregnancy rose to 26% following completion of gANC, more than three times the 7.1% observed at baseline [
5]. This was also true for many other quality of care parameters. Women participating in gANC were more likely to discuss reproductive health issues including family planning and HIV testing with their partners compared to those in conventional ANC in a randomized controlled trial in Malawi and Tanzania [
6]. In a study in Nigeria and Kenya, women receiving gANC were more likely than their counterparts in individual care to attend not less than 4 ANC visits
(Nigeria: aOR 13.30, CI 7.69-22.99, p<0.001; Kenya: aOR 7.12, CI 3.91-12.97, p<0.001), receive good quality care
(Nigeria: aOR 5.8, CI 1.98-17.21, p<0.001; Kenya: aOR 5.08, CI 2.31-11.16, p<0.001), and deliver in a health facility (Nigeria:
aOR 2.30, CI 1.51-3.49) [
7]. In another study, Senegalese adolescents attending gANC indicated preference for utilization of gANC over individual ANC in their next pregnancies [
8]. Open communication and supportive relationships have also been associated with gANC [
9].
Failure to detect significant difference in the impact of gANC on pregnancy outcomes compared to individual ANC has also been described in literature. In a cluster-randomized controlled trial to determine the effect of gANC on gestational length in a large sample of pregnant women (4752 intervention, 4091 control) in Rwanda, there was no significant difference in gestational length or other secondary outcomes except for postnatal visits which was more common in the control group [
10]. The authors noted that low dose of exposure to the intervention at only 4 antenatal visits might have influenced this observation [
10]. In the qualitative component of the same trial, participants of gANC reported knowledge gain, support from peers, and improved relationship with their healthcare providers following the intervention [
10]. However, these were pre- and post-test data from a study that did not include a comparison group.
The World Health Organization (WHO) recommends group antenatal care (gANC) as an effective model to improve maternal and newborn health outcomes [
11]. In Nigeria, the Federal Ministry of Health (FMOH) has endorsed gANC as a strategy to increase the quality and coverage of ANC services. However, the adoption and adaptation of gANC in Nigeria has been limited. This study seeks to demonstrate the effectiveness of Antenatal Care (ANC)/Postnatal Care (PNC) packages and scale proven implementation packages; this has only been done in a limited number of countries. It will catalyze scaling platforms to advance Primary Health Care (PHC) as well as scale contextual proven intervention BOWs. This study will help answer questions about the effectiveness of gANC in different settings as well as how gANC can be designed to be successful in different settings. It will provide governments of participating states the data they need to inform effective scaling of the intervention in their states. Findings from the baseline phase of the study will be compared with follow up data to be collected at two future time points are presented in this paper.
Study Objectives: This phase of the study sought to estimate baseline parameters on antenatal history and behavior, delivery preparedness, and perception of contraception among pregnant women attending gANC in health facilities in Kaduna and Kano States of Nigeria. It also elicited baseline data on the quality of ANC experienced by participants attending gANC in these health facilities.
2. Materials and Methods
2.1. Conceptual Model and Approach
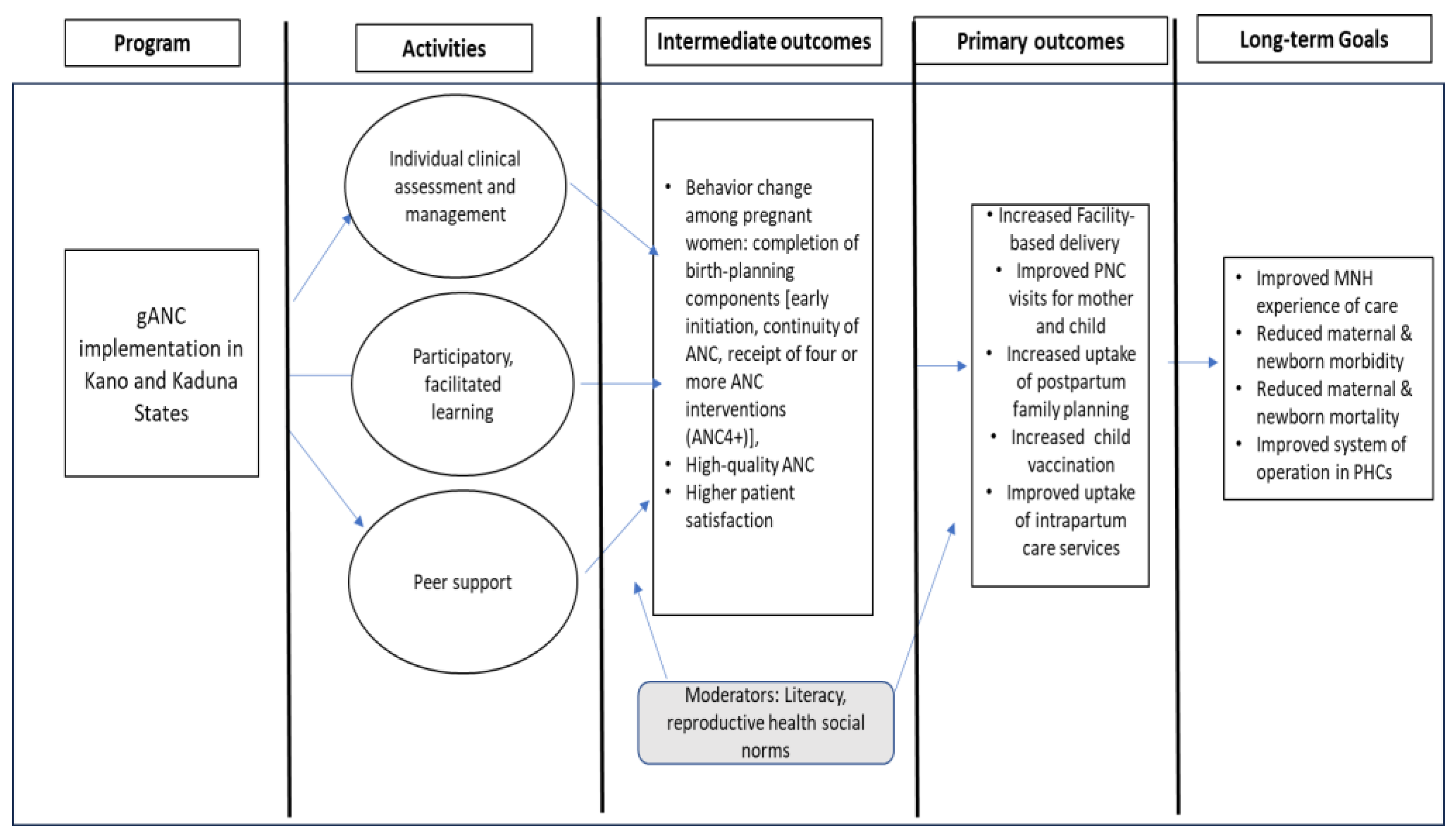
This implementation research is underpinned by the Diffusion of Innovation theory that explores how gANC is adopted and becomes a standard of care in northern Nigeria [
12]. This model provides a basis for the conceptual framework of the program, which posits that ANC utilization can be influenced to promote the adoption of change, which in this case is the gANC intervention [
13]. Observing the implementation of gANC in real life can provide important insight into facilitators and barriers that should be considered in planning for the scaling of the intervention in the States.
Figure 1 provides the theory of change from the implementation of project activities to the observation of specific intermediate, primary and long-term outcomes.
2.2. Study Design
The overall evaluation includes both quantitative and qualitative components, with the quantitative component being a three-wave longitudinal study of pregnant women enrolled in gANC at health facilities in Kaduna and Kano states. This paper focuses on the quantitative component of the overall study. Baseline data from that longitudinal study are the focus of the current report. Subsequent waves will include measures of uptake of, services received in, and satisfaction with care for gANC services over the course of the pregnancy, as well as perinatal outcomes including facility delivery, completion of postnatal health checks, postpartum family planning use, and uptake of recommended child immunizations.
2.3. Study Setting
Kaduna and Kano States are in the northwest geopolitical zone of Nigeria with a projected 2022 population size of about 9.02 million and 15.46 million respectively. Kaduna State has 23 local government areas (LGAs) spread across 3 senatorial districts in a land space of 45,061 KM
2 and with a population density of over 200/KM
2. Kano State has a smaller land mass of about 20,230 KM
2 and a population density of 764.3/KM
2 with 44 LGAs in 3 senatorial districts [
14,
15]. Nigeria’s2006 census showed gender distribution of 53% males and 47% females for Kano State with about 50% of the population in the 15-64 years age category. Kaduna State had over 51% of the population within the age of 15-64 years with 51% males and 49% females gender distribution [
14].Islam is the predominant religion in both States but with a higher proportion in Kano State. In Kaduna State the total number of health facilities offering the gANC program is 486 and in Kano Stater, 523.
2.4. Study Population and Sample Size
Pregnant women enrolled in the gANC program in the participating health facilities in Kaduna and Kano States of Nigeria. In order to be eligible for the program, women needed to have visited one of the facilities offering gANC in Kaduna and Kano states that were selected for the study sample. We calculated that a sample of 1,200 participants per state (2,400 total) ) would be sufficient to provide statistical power of at least 0.80 in the planned propensity score analyses. Key assumptions in that calculation were (a) that the marginal correlation between number of gANC sessions attended and the probability of facility delivery net of covariates that will be used to obtain the propensity scores, will be 0.10; and that no more than 30% of enrolled participants will be lost to follow-up between baseline and subsequent waves of the longitudinal study.
2.5. Sampling & Recruitment Strategy
Statistical power calculation was 1,200 per state (2,400 total), based upon the plan to conduct PSM analysis to isolate the cause-and-effect relationship between number of gANC meetings attended and the probability of delivering in a health facility. A stratified, three-stage cluster sampling design was used. In the first stage, the local government areas (LGAs) in each state were stratified by senatorial district, of which there are three in each state, and we randomly sampled two LGAs per senatorial district with equal probability, for a total sample of 12 LGAs. At this stage, some LGAs were removed from the sampling frame because the security situation would make data collection there unsafe for study personnel. In the second stage, we randomly sampled eight health facilities within each sampled LGA, again with equal probability, yielding a total of 96 sampled facilities. In the final stage, we planned to sample 25 eligible women per sampled facility. Some sampled facilities, however, were excluded because of security concerns, because they had insufficient enrollment, or because they were not implementing gANC at the time of baseline data collection. To compensate for this, we sampled more than 25 women from the remaining facilities in LGAs in which some facilities were excluded, in order to achieve a sample of 200 women in each LGA. Pregnant women aged 15-49 years attending gANC who consented to participate were recruited for the study.
2.6. Data Collection
Baseline data collection for this study was conducted in Kaduna and Kano States in March and April of 2024. This initial phase of the study included both qualitative and quantitative baseline components. A 72-item Questionnaire was used for the quantitative survey. The survey tool was pilot-tested prior to implementation. Data collection was conducted during 15 days of fieldwork in March2024. Eligible women (age 15 – 49 years at 12 - 20 weeks GA) were recruited from randomly selected sample of facilities in each state. In each state, the quantitative survey composed of three broad teams of interviewers and supervisors, one team per senatorial district. In each senatorial district, 10 interviewers and two supervisors conducted fieldwork.
2.7. Data Analysis
For the baseline data, initial data quality and consistency checks were conducted, and data cleaning done before analyses. Frequencies, descriptive statistics, cross-tabulations for the baseline data were developed overall and by state. This covered multiple domains such as sociodemographic background, prior pregnancies and births, current pregnancy and gANC use, services received, quality of care and satisfaction with care. All analyses were carried out in Stata SE v18.
3. Results
A total of 1,269 and 1,200 participants were recruited from the sampled facilities in the six sampled LGAs of Kaduna State and Kano State, respectively.
3.1. Socio-Demographics of Participants
The sociodemographic composition of the sample is shown, overall and by state, in
Table 1. Participants in both states were mostly between ages 19- 31 years, married or living with a partner, and identified as Muslim. Over 62% and 34% had completed secondary or higher-level education in Kaduna and Kano States respectively. In both states, just over half of the participants have their own business. Nearly 60% and over 80% live in an urban area in Kaduna and Kano States respectively. Only about 27% of the study participants in Kaduna State and 22% in Kano State never gave birth before (
Table 1). Up to 71% had 3 or more living children with 10% having up to6 or more children in Kaduna State. In Kano State
, 61% had 3 or more living children with about 20% having six or more children.
3.2. Obstetric History
3.2.1. Previous Pregnancies
Table 2 summarizes information about prior pregnancies among the subset of participants who reported having at least one prior birth. In Kaduna State, among those who reported at least one previous pregnancy and birth, nearly 65% of participants’ last delivery was in a facility, over 70% had a skilled birth assistance, and nearly 70% reported no problems with previous pregnancies. About 88% had postnatal care appointments, and 83% had a postnatal check within one week of delivery. In Kano, 61% of participants’ with at least one prior pregnancy and birth reported that their last delivery was at home, up to 42% had no skilled birth assistance, while 64% reported no problems with previous pregnancies. Up to 82% had postnatal care appointments, and 80% had a postnatal check within one week of delivery.
3.2.2. Current Pregnancies
As shown in
Table 3, in both States, about two-thirds of the participants had a first ANC visit by18 weeks gestational age and had at least two visits.
3.3. Quality of Care
When asked about their most recent ANC visit, in both states, over 90% of participants reported receiving at least 4 services, and over 75% reported receiving not less than 9. Discussing Iron Folic Acid (IFA) side effects with the provider was the least common service received at just over 20%. Other services not commonly provided included estimation of delivery dates, height measurement, and asking about blood group (see
Figures S1 and S2 for findings). In both States, nearly all participants expressed satisfaction with the antenatal care they received with over 95% planning to continue ANC at the same facility.
3.4. Measures of Birth Readiness
In Kaduna State, nearly 90% of participants had identified a delivery facility, and among those, over 70% had made a transport plan. Over 35% of participants reported it took 30 minutes or more to reach a facility. Nearly 70% of participants reported having a cash plan for emergency care, and 90% had made arrangements for a companion. In Kano, over 50% of participants had identified a delivery facility, and among those, nearly 80% had made a transport plan. A third of the participants reported it took 30 minutes or more to reach a facility. Nearly 80% of the participants reported having a cash plan for emergency care, and nearly all had arrangements for a companion (
Table S1). More than 85% of participants plan to be at home during pregnancy and after birth.
3.5. Family Planning Behavior
About half of participants in Kaduna State had not previously used family planning methods, and over three-quarters of those who had used said it was joint decision between them and their husbands/partners. More than half reported they could ask their partner to use a condom, over 90% said they would delay future pregnancy and said there were advantages to spacing births. In Kano State, over 60% of the participants had previously used family planning, and 65% said it was mainly a joint decision. Nearly half reported they could not ask their partner to use a condom, over 3/4 said they would delay future pregnancy, and over 90% said there were advantages to spacing births.
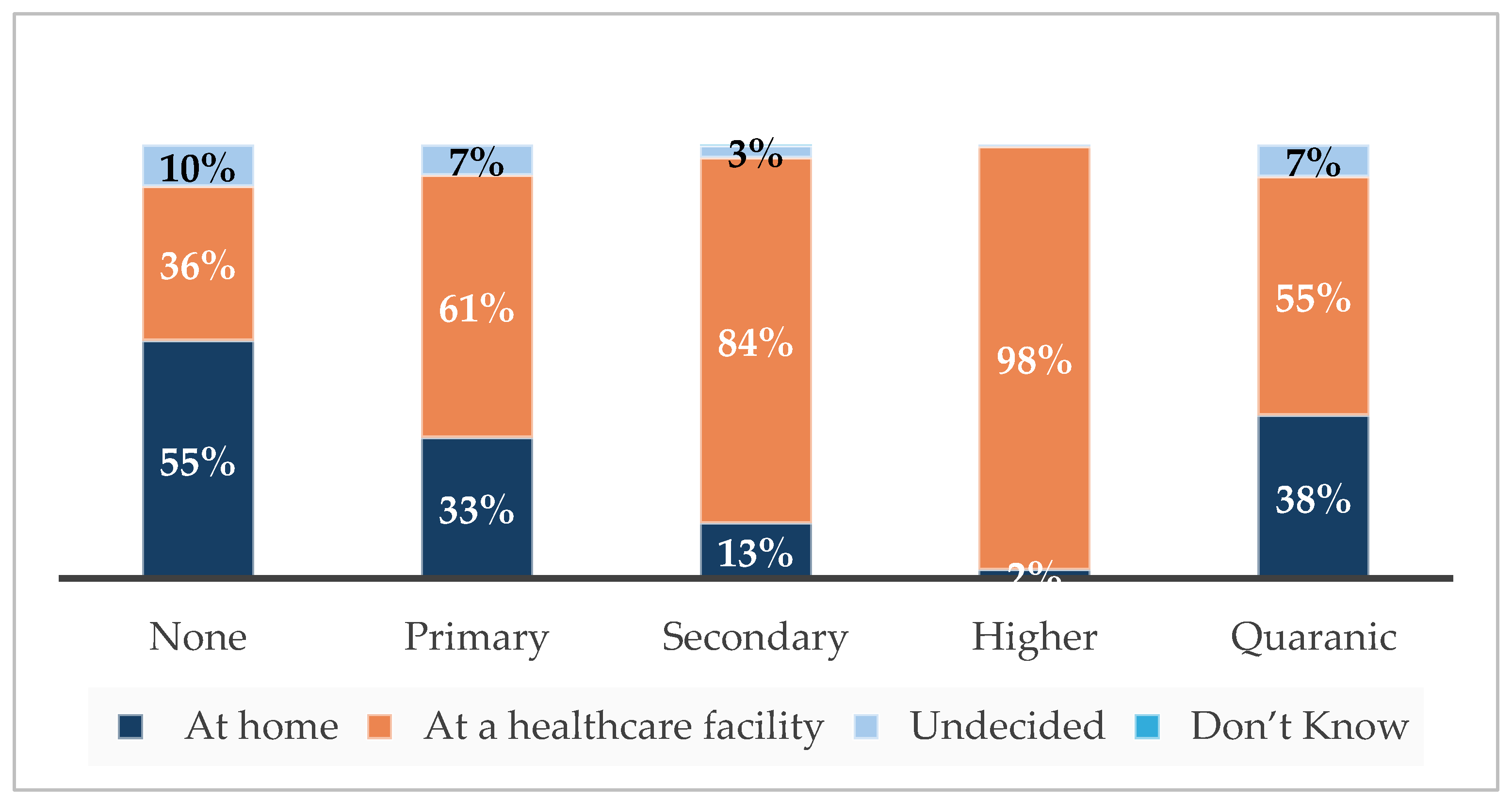
3.6. Pregnancy Knowledge and Behavior by Education Status
Across education levels, there was agreement that spacing pregnancies is advantageous. This perception tended to be higher among participants with higher education levels. Reported ability to ask for condom use was also higher among participants with higher education levels (
Table S2). There are high levels of awareness of warning signs, and this also tends to be higher among participants with higher education levels. Most participants had made transport plans, and this was slightly higher among participants with higher education levels. Most participants across education levels had had 1-3 ANC visits (
Figure S3). Plans to deliver at a facility were higher among participants with higher education levels (
Figure 2).
4. Discussion
This study has provided baseline data in the first step in a multi-year process to evaluate the implementation of the gANC program in Nigeria. Although inferences about the impacts of gANC utilization cannot be made from the data at this phase, some important observations from baseline are noted in comparison with data from literature. The experience and findings from this initial implementation evaluation provide context and insights for the planned longitudinal follow-up and data analysis for this project.
In both states, over 95% of the participants expressed satisfaction with the individual antenatal care (ANC) they had received in previous pregnancies from the same facility. Considering that gANC is a novel approach and most participants had received minimal doses at baseline, it is not surprising that they consider the status quo standard and satisfactory, not having a higher quality experience to compare with. Social desirability bias is also not unlikely, where participants inaccurately provide desirable response to maintain a positive impression and not displease the interviewer [
16]. High level of satisfaction with ANC had been observed by other studies in this region. In a survey of 1336 mothers in northern Nigeria, 90% of the respondents expressed satisfaction with the ANC services and this was associated with responsive treatment, communication, staff being empathetic, ease of access to treatment, and other quality-related factors [
17]. Triangulating qualitative data in this study could provide more insight into the perception of satisfaction and related factors, and provide basis for subsequent comparisons.
Over 40% of the participants in Kano State had their last delivery at home with no skilled birth attendant. This is not an unusual finding in this part of Nigeria. This seems to contradict the high response of satisfaction expressed in ANC. It is possible that experience at ANC differs from that during childbirth in health facilities. This was the observation in an earlier study in Kano State where women quit ANC to deliver at home due to the attitude of maternity staff and the presence of male staff during deliveries [
18]. Facility-based delivery was observed to be higher among women who participated in gANC compared to their ANC counterparts in a
facility-based, pragmatic, cluster-randomized controlled trial of Nigerian women in Nasarawa state, northcentral Nigeria [
7]. Quality of antenatal care received in gANC could have been responsible for this positive effect in the choice of health facility delivery. In another study, a strong correlation was found between ANC attendance and the use of skilled birth attendant (r=0.706, p<0.001) in a secondary analysis of the 2018 Nigerian National Nutrition and Health Survey, further confirming that antenatal care experience could influence delivery behavior choices [
19]. The positive effect of gANC on delivery behavior choices is anticipated in this present implementation study that has facility-based delivery as a primary outcome.
One in four participants in Kano state commenced ANC at ≥23 weeks gestational age. This is similar to the findings from the national survey where up to 63% of women started ANC during the second semester [
3]. In Kaduna, women were more likely to commence ANC during the first semester. Timely initiation of ANC has been associated with better health outcomes among pregnant women in sub-Saharan Africa [
20]. Factors that influence decision on when to commence ANC would be good to explore as this could guide targeted interventions to improve health outcomes among pregnant women in Nigeria.
The level of birth preparedness among women in both states was generally high with most having identified delivery health facility, made transportation and cash plans for emergency, and identified a companion. Preparedness was reported more by those with higher levels of education, including intention to deliver in a health facility. This is not surprising as education is known to influence health literacy which in turn leads to adoption of health promoting behavior [
21]. This was also the case in the observed higher proportions of those with higher levels of education perceiving child spacing as advantageous and being able to ask their husbands to use condom. Up to half the participants in Kano State expressed their inability to ask their husbands to use condom. Interventions that improve health literacy are therefore recommended for better reproductive health behavior and outcomes. This has been proposed as a life-course strategy that can be implemented in many settings, including informal learning settings [
22]. It is hoped that the peer-to-peer learning from gANC will support health literacy and improve pregnancy outcomes among the participants.
4.1. Limitations
This is a baseline study and report on the methodology used in the gANC implementation evaluation. As such, we cannot draw conclusions at this point about the impact of the program. Future longitudinal data collection using PSM analysis to create a matched comparison group will enable us to make inferences about program effectiveness. While PSM is a sound quasi-experimental methodology, and the best available analytic method given that the gANC program was being implemented in Kaduna and Kano before the evaluation began, it is not a randomized controlled design. The quality of the PSM method will depend on having sufficient matching data, and on potential loss to follow-up in the longitudinal sample, which will be determined in the next phase of the project.
4.2. Future Research
We will continue with midline data collection in late 2024, and endline data collection in 2025. Longitudinal data collection and efforts to maximize participant retention and minimize loss to follow-up will be the key next steps. Once follow up data are available, we will use PSM to create comparison groups (treatment and comparison) based on matching of demographic characteristics. The PSM analysis will be based on several socio-demographic variables including location, gender, religion, education, employment, and other co-variates in a multivariable logistic regression procedure to compare participants who received more gANC services (attendance at meetings) during the implementation period to those who participated in fewer or no intervention services [23]. This procedure will be used to create two matched groups for subsequent multivariate impact analysis where the independent variables will be participation in gANC meetings, and the dependent variables will be giving birth at a facility (primary) as well as additional secondary outcomes [24].
Future studies should include evaluating gANC in other settings within Nigeria and other low-and middle-income countries that have low utilization of ANC in healthcare facilities. Studies should examine approaches to improving the quality of care following the WHO guidelines [
11]. Such studies may examine programs designed to reduce the risk of stillbirths and pregnancy complications and give women a positive pregnancy experience, following WHO recommendations. Use of novel methods to promote ANC utilization, including reducing barriers such as transportation and cost, and exploring telehealth solutions and mobile health technologies should also be examined.
5. Conclusion
An evidence-based gANC program is being implemented across two states in northern Nigeria. An implementation evaluation has been successfully launched and has collected data from 2,469 women receiving care at facilities delivering the gANC program. Longitudinal data collection will continue at two future time points and utilize a PSM analysis methodology to identify potential impacts of the gANC program.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1, Figure S1: Antenatal clinic services received at most recent visit in Kaduna; Figure S2: Antenatal services received in the most recent visit in Kano; Figure S3: Antenatal visits by education level; Table S1: Responses to delivery planning questions among participants who had identified a facility for delivery; and Table S2: Perception of pregnancy and family planning by education level.
Author Contributions
Conceptualization, WDE, MA; methodology, WDE, JBB, SBA; software, JBB, CLO; validation, WDE, JBB, CLO.; formal analysis, WDE, JBB, CLO; investigation, WDE, SBA, FAD, SAG; resources, SBA, FAD, SAG; data curation, SG, JBB; writing—original draft preparation, WDE, CLO.; writing—review and editing, WDE, JBB, CLO; visualization, JBB, CLO; supervision, WDE, SBA, SAG; project administration, WDE, SBA, SAG; funding acquisition, WDE. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Bill & Melinda Gates Foundation grant number INV-043363.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the George Washington University and the Nigeria’s National Health Research Ethics Committee (NHREC/01/01/2007-12/01/2024 on 12 January 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
We acknowledge support from the Bill & Melinda Gates Foundation Nigeria country office.
Conflicts of Interest
The authors declare no conflicts of interest. The final author is the program officer for this project at the Bill & Melinda Gates Foundation. He contributed to the conceptualization of the project, but had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Salami, K.; Yusuf, O.; Akinyemi, J.; Morhason-Bello, I.; Eyelade, R.; Ilori, T.; Aderinto, A.; Alarape, K.; Alada, A.; Jegede, A.; Fawole, O.; Kana, I.; Solanke, O.; Suleiman, J.; Okara, D.; Adebiyi, A.; Abdullahi, A.; Ejiade, OO.; Adewole, IF. Individual and Ecological Analyses of Antenatal Care: Prospects for Delivery Assistance and Use of Modern Family Planning in Nigeria. Afr J Reprod Health 2022, 26, 69–76. [Google Scholar] [PubMed]
- National Population Commission (NPC) [Nigeria] and ICF. Nigeria Demographic and Health Survey 2018; Abuja: Nigeria and Rockville, MA, USA, 2019. [Google Scholar]
- Fagbamigbe, A. F.; Olaseinde, O.; Setlhare, V. Sub-National Analysis and Determinants of Numbers of Antenatal Care Contacts in Nigeria: Assessing the Compliance with the WHO Recommended Standard Guidelines. BMC Pregnancy Childbirth 2021, 21, 1–19. [Google Scholar] [CrossRef]
- Adewoyin, Y.; Odimegwu, C. O. Gender Relations and the Utilization of Contraceptives and Antenatal Care Services in Kenya, Namibia and Nigeria. Afr J Reprod Health 2022, 26, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Somji, A.; Ramsey, K.; Dryer, S.; Makokha, F.; Ambasa, C.; Aryeh, B.; Booth, K.; Xueref, S.; Moore, S.; Mwenesi, R.; Rashid, S. “Taking Care of Your Pregnancy”: A Mixed-Methods Study of Group Antenatal Care in Kakamega County, Kenya. BMC Health Serv Res 2022, 22, 969. [Google Scholar] [CrossRef]
- Jeremiah, R. D.; Patel, D. R.; Chirwa, E.; Kapito, E.; Mei, X.; McCreary, L. L.; Norr, K. F.; Liu, L.; Patil, C. L. A Randomized Group Antenatal Care Pilot Showed Increased Partner Communication and Partner HIV Testing during Pregnancy in Malawi and Tanzania. BMC Pregnancy Childbirth 2021, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Grenier, L.; Suhowatsky, S.; Kabue, M. M.; Noguchi, L. M.; Mohan, D.; Karnad, S. R.; Onguti, B.; Omanga, E.; Gichangi, A.; Wambua, J.; Waka, C.; Oyetunji, J.; Smith, J. M. Impact of Group Antenatal Care (G-ANC) versus Individual Antenatal Care (ANC) on Quality of Care, ANC Attendance and Facility-Based Delivery: A Pragmatic Cluster-Randomized Controlled Trial in Kenya and Nigeria. PLoS One 2019, 14, e0222177. [Google Scholar] [CrossRef]
- Vandermorris, A.; McKinnon, B.; Sall, M.; Witol, A.; Traoré, M.; Lamesse-Diedhiou, F.; Bassani, D. G. Adolescents’ Experiences with Group Antenatal Care: Insights from a Mixed-Methods Study in Senegal. Trop Med Int Health 2021, 26, 1700–1708. [Google Scholar] [CrossRef] [PubMed]
- Grenier, L.; Onguti, B.; Whiting-Collins, L. J.; Omanga, E.; Suhowatsky, S.; Winch, P. J. Transforming Women’s and Providers’ Experience of Care for Improved Outcomes: A Theory of Change for Group Antenatal Care in Kenya and Nigeria. PLoS One 2022, 17. [Google Scholar] [CrossRef] [PubMed]
- Sayinzoga, F.; Lundeen, T.; Musange, S. F.; Butrick, E.; Nzeyimana, D.; Murindahabi, N.; Azman-Firdaus, H.; Sloan, N. L.; Benitez, A.; Phillips, B.; Ghosh, R.; Walker, D. Assessing the Impact of Group Antenatal Care on Gestational Length in Rwanda: A Cluster-Randomized Trial. PLoS One 2021, 16. [Google Scholar] [CrossRef]
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience.
- Dearing, J.; Cox, J. Diffusion Of Innovations Theory, Principles, And Practice. Health Aff 2018, 37, 183–190. [Google Scholar] [CrossRef]
- Carpenter, D.; Hassell, S.; Mardon, R.; Fair, S.; Johnson, M.; Siegel, S.; Nix, M. Using Learning Communities to Support Adoption of Health Care Innovations. Jt Comm J Qual Patient Saf 2018, 44, 566–573. [Google Scholar] [CrossRef] [PubMed]
- City Population. Kano (State, Nigeria) - Population Statistics, Charts, Map and Location. Available online: https://citypopulation.de/en/nigeria/admin/NGA020__kano/ (accessed on 17 June 2024).
- Kaduna State Bureau of Statistics. 2018 BOOK. Kaduna State Government Planning & Budget Commission.
- Latkin, C. A.; Edwards, C.; Davey-Rothwell, M. A.; Tobin, K. E. The Relationship between Social Desirability Bias and Self-Reports of Health, Substance Use, and Social Network Factors among Urban Substance Users in Baltimore, Maryland. Addictive behaviors 2017, 73, 133. [Google Scholar] [CrossRef] [PubMed]
- Onyeajam, D. J.; Xirasagar, S.; Khan, M. M.; Hardin, J. W.; Odutolu, O. Antenatal Care Satisfaction in a Developing Country: A Cross-Sectional Study from Nigeria. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, S.; Adamu, D.; Hamza, R.; Galadima, J. Determinants of Home Delivery among Women Attending Antenatal Care in Bagwa...: EBSCOhost. Afr J Reprod Health 2017, 21, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Salami, K.; Yusuf, O.; Akinyemi, J.; Morhason-Bello, I.; Eyelade, R.; Ilori, T.; Aderinto, A.; Alarape, K.; Alada, A.; Jegede, A.; Fawole, O.; Kana, I.; Solanke, O.; Suleiman, J.; Okara, D.; Adebiyi, A.; Abdullahi, A.; Ejiade, OO.; Adewole, IF. Individual and Ecological Analyses of Antenatal Care: Prospects for Delivery Assistance and Use of Modern Family Planning in Nigeria. Afr J Reprod Health 2022, 26, 69–76. [Google Scholar]
- Alem, A. Z.; Yeshaw, Y.; Liyew, A. M.; Tesema, G. A.; Alamneh, T. S.; Worku, M. G.; Teshale, A. B.; Tessema, Z. T. Timely Initiation of Antenatal Care and Its Associated Factors among Pregnant Women in Sub-Saharan Africa: A Multicountry Analysis of Demographic and Health Surveys. PLoS One 2022, 17. [Google Scholar] [CrossRef] [PubMed]
- Bayati, T.; Dehghan, A.; Bonyadi, F.; Bazrafkan, L. Investigating the Effect of Education on Health Literacy and Its Relation to Health-Promoting Behaviors in Health Center. J Educ Health Promot 2018, 7, 127. [Google Scholar] [CrossRef] [PubMed]
- Vamos, S.; Okan, O.; Sentell, T.; Rootman, I. Making a Case for “Education for Health Literacy”: An International Perspective. Int J Environ Res Public Health. 2020, 17, 1436. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).