Submitted:
17 September 2024
Posted:
19 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Material and Methods
2.1. Review Type
2.2. Search Strategy
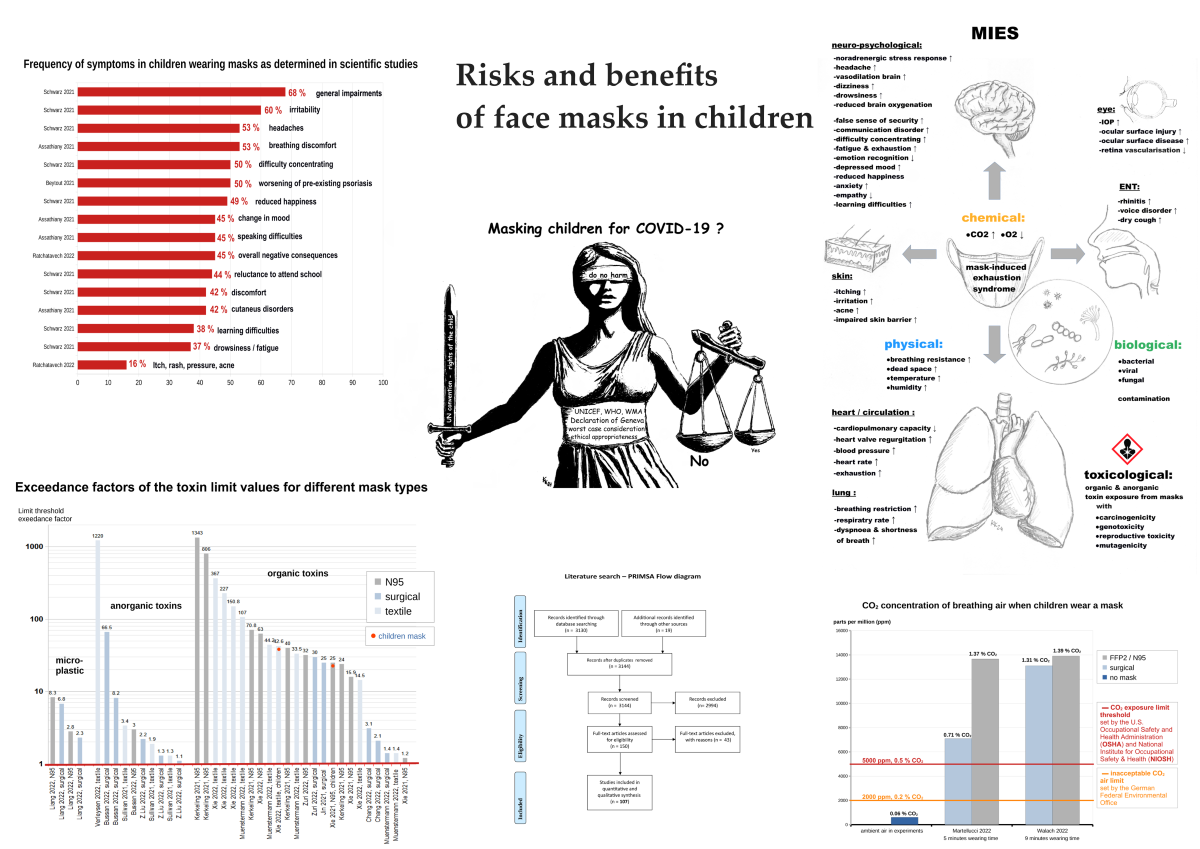
3. Results
- -
- Evidence for (non-)effectiveness (16 papers, 14.9%, supplement: Table S1),
- -
- Positive effects (13 papers, 12.2%, supplement: Table S2),
- -
- Psychological and sociological effects (41 papers, 38.3%, supplement: Table S3),
- -
- Physical symptoms, clinical conditions (8 papers, 7.5%, supplement: Table S4),
- -
- Physio-metabolic and toxicological effects (23 papers, 21.5%, supplement: Table S5),
- -
- Empirically and experimentally unproven claims – no ecological validity from a strictly empirical view (6 papers, 5.6%, supplement: Table S6).
4. Discussion
4.1. Evidence for (Non-) Effectiveness
Evidence for Effectiveness
Evidence for Non-Effectiveness
4.2. Positive Effects
4.3. Psychological and Sociological Effects
4.4. Physical Symptoms
4.5. Physio-Metabolic and Toxicological Effects
4.6. Empirically/Experimentally Unproven Claims
4.7. Bacterial, Fungal and Viral Contamination
4.8. Risk Benefit Analysis and Risk-Assessment
4.8.1. Unproven Effectiveness of Masks in Children against Viruses
4.8.2. Lack of Mask Standardisation (Virus Filtration)
4.8.3. Negligible Infectivity and COVID-19 Course in Children
4.8.4. Scientifically Proven Adverse Mask Effects and MIES
Clinical Symptoms
Restriction of Normal Breathing
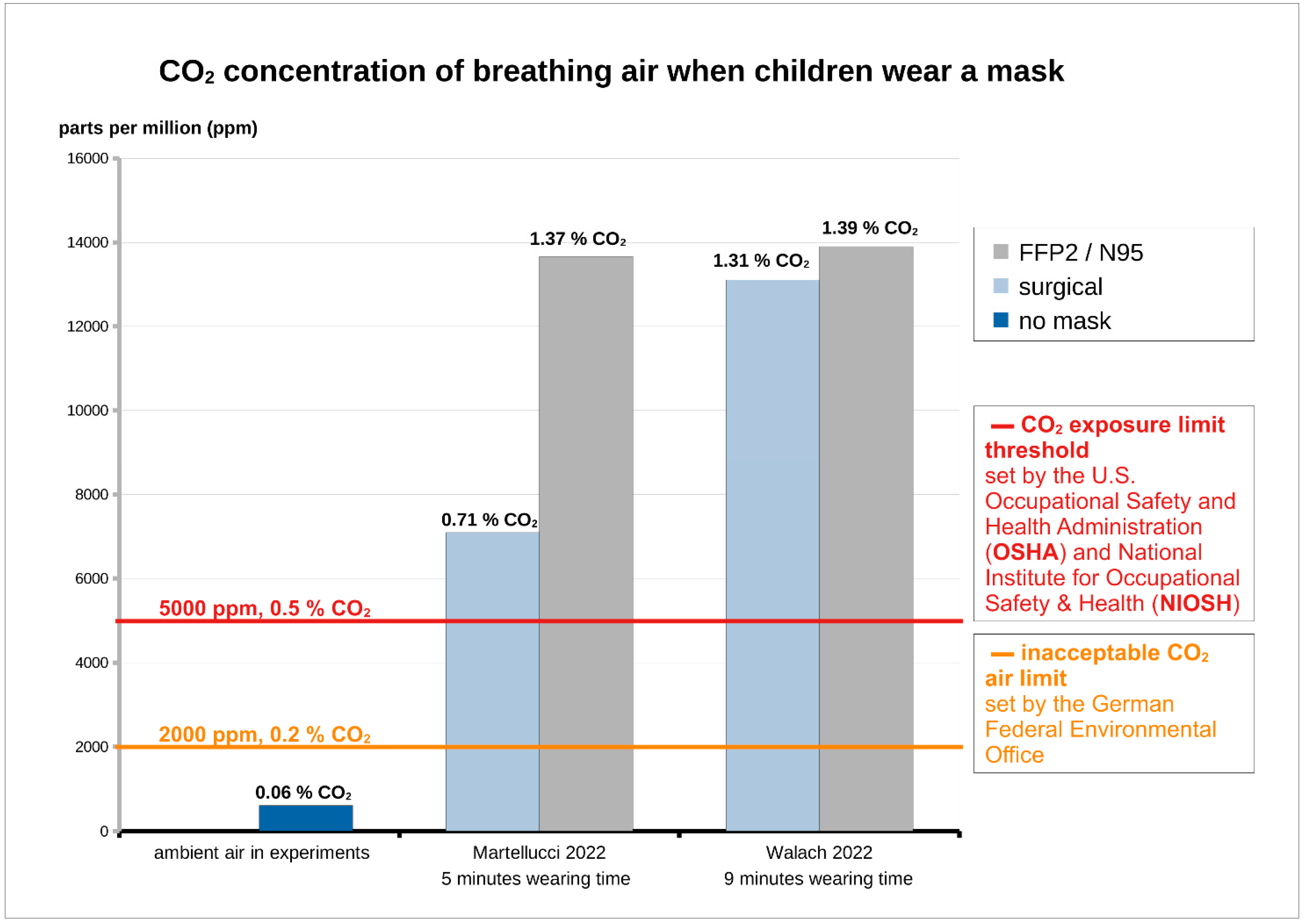
Carbon Dioxide Rise
Oxygen Drop
Microbial Contamination
Toxicity and Carcinogenicity
Psychological and Sociological Symptoms
MIES -Mask Induced Exhaustion Syndrome
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- -
- Toxicological risks, including harmful and carcinogenic substances that are inhaled at almost zero distance from the respiratory tract [23].
- -
- Biological hazards due to bacterial, fungal and viral contamination and possible spread [170]
- -
- Risk to young life, including unborn and children, with potential nerve damage, testicular damage and stillbirths [22].
4.8.5. Risk Assessment of Masks and Children
4.8.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- OECD Environment, Health and Safety Publications. Assessing the Risk of Chemicals to Children’s Health: OECD-Wide Survey 2021 Survey Report. Series on Testing and Assessment, No 376, 27. April 2023, ENV/CBC/MONO(2023)8, 1–66. [Google Scholar]
- Face Covering Policies during the COVID-19 Pandemic. Available online: https://ourworldindata.org/grapher/face-covering-policies-covid (accessed on 29 December 2022).
- Coronavirus Disease (COVID-19): Children and Masks. Available online: https://www.who.int/news-room/questions-and-answers/item/q-a-children-and-masks-related-to-covid-19 (accessed on 28 December 2022).
- Hahn, L.M.; Manny, E.; Dhaliwal, G.; Chikuma, J.; Robinson, J.; Lou, W.; Subbarao, P.; Turvey, S.E.; Simons, E.; Bell, R.C.; et al. Association of COVID-19 Government-Instituted Mask Mandates With Incidence of Mask Use Among Children in Alberta, Canada. JAMA Netw Open 2023, 6, e2317358. [Google Scholar] [CrossRef] [PubMed]
- Corpuz, J.C.G. Adapting to the Culture of “New Normal”: An Emerging Response to COVID-19. J Public Health (Oxf) 2021, 43, e344–e345. [Google Scholar] [CrossRef]
- Rowland, L.C.; Klinkhammer, M.D.; Ramirez, D.W.E. Dynamic Masking: A Proposal of Burden-Based Metrics for Masking in K-12 Schools During the COVID-19 Pandemic. Journal of School Health 2022, 92, 11–19. [Google Scholar] [CrossRef]
- Esposito, S.; Principi, N. To Mask or Not to Mask Children to Overcome COVID-19. Eur J Pediatr 2020, 179, 1267–1270. [Google Scholar] [CrossRef]
- World Health Organization (WHO) Mask Use in the Context of COVID-19: Interim Guidance, 1 December 2020. WHO/2019-nCoV/IPC_Masks/2020.5. 2020.
- Examining Our COVID-19 Response: An Update from Federal Officials | The U.S. Senate Committee on Health, Education, Labor & Pensions. Available online: https://www.help.senate.gov/hearings/examining-our-covid-19-response-an-update-from-federal-officials (accessed on 26 August 2024).
- Ladhani, S.N. Face Masking for Children - Time to Reconsider. Journal of Infection 2022, 85, 623–624. [Google Scholar] [CrossRef] [PubMed]
- Thomson, S. Mask Mandates for Children during the COVID-19 Pandemic: An International Human Rights Perspective. Scand J Public Health 2022, 50, 683–685. [Google Scholar] [CrossRef] [PubMed]
- Gimma, A.; Lal, S. Considerations for Mitigating COVID-19 Related Risks in Schools. The Lancet Regional Health – Americas 2021, 2. [Google Scholar] [CrossRef]
- Qiu, H.; Wu, J.; Hong, L.; Luo, Y.; Song, Q.; Chen, D. Clinical and Epidemiological Features of 36 Children with Coronavirus Disease 2019 (COVID-19) in Zhejiang, China: An Observational Cohort Study. The Lancet Infectious Diseases 2020, 20, 689–696. [Google Scholar] [CrossRef]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 Among Children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef]
- Høeg, T.B.; González-Dambrauskas, S.; Prasad, V. The United States’ Decision to Mask Children as Young as Two for COVID-19 Has Been Extended into 2023 and beyond: The Implications of This Policy. Paediatric Respiratory Reviews 2023, 47, 30–32. [Google Scholar] [CrossRef] [PubMed]
- McBride, D.L. New Guidelines for Children Returning to Sports after Covid-19. Journal of Pediatric Nursing: Nursing Care of Children and Families 2021, 59, 196–197. [Google Scholar] [CrossRef] [PubMed]
- Junger, N.; Hirsch, O.; Junger, N.; Hirsch, O. Ethics of Nudging in the COVID-19 Crisis and the Necessary Return to the Principles of Shared Decision Making: A Critical Review. Cureus 2024, 16. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; MacIntyre, C.R.; Baker, M.G.; Bhattacharjee, S.; Chughtai, A.A.; Fisman, D.; Kunasekaran, M.; Kvalsvig, A.; Lupton, D.; Oliver, M.; et al. Masks and Respirators for Prevention of Respiratory Infections: A State of the Science Review. Clin Microbiol Rev 2024, e0012423. [Google Scholar] [CrossRef] [PubMed]
- Sandlund, J.; Duriseti, R.; Ladhani, S.N.; Stuart, K.; Noble, J.; Høeg, T.B. Child Mask Mandates for COVID-19: A Systematic Review. Archives of Disease in Childhood 2023. [Google Scholar] [CrossRef]
- Chandra, A.; Høeg, T.B. Lack of Correlation between School Mask Mandates and Paediatric COVID-19 Cases in a Large Cohort. Journal of Infection 2022, 85, 671–675. [Google Scholar] [CrossRef]
- Jefferson, T.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Driel, M.L. van; Bawazeer, G.A.; Jones, M.A.; Hoffmann, T.C.; Clark, J.; Beller, E.M.; et al. Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses. Cochrane Database of Systematic Reviews 2023. [Google Scholar] [CrossRef]
- Kisielinski, K.; Wagner, S.; Hirsch, O.; Klosterhalfen, B.; Prescher, A. Possible Toxicity of Chronic Carbon Dioxide Exposure Associated with Face Mask Use, Particularly in Pregnant Women, Children and Adolescents – A Scoping Review. Heliyon 2023, 9. [Google Scholar] [CrossRef]
- Kisielinski, K.; Hockertz, S.; Hirsch, O.; Korupp, S.; Klosterhalfen, B.; Schnepf, A.; Dyker, G. Wearing Face Masks as a Potential Source for Inhalation and Oral Uptake of Inanimate Toxins – A Scoping Review. Ecotoxicology and Environmental Safety 2024, 275, 115858. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health 2021, 18, 4344. [Google Scholar] [CrossRef]
- Acuti Martellucci, C.; Flacco, M.E.; Martellucci, M.; Violante, F.S.; Manzoli, L. Inhaled CO2 Concentration While Wearing Face Masks: A Pilot Study Using Capnography. Environ Health Insights 2022, 16, 11786302221123573. [Google Scholar] [CrossRef] [PubMed]
- Walach, H.; Traindl, H.; Prentice, J.; Weikl, R.; Diemer, A.; Kappes, A.; Hockertz, S. Carbon Dioxide Rises beyond Acceptable Safety Levels in Children under Nose and Mouth Covering: Results of an Experimental Measurement Study in Healthy Children. Environmental Research 2022, 212, 113564. [Google Scholar] [CrossRef] [PubMed]
- Le, H.H.T.C.; Vien, N.T.; Dang, T.N.; Ware, R.S.; Phung, D.; Thai, P.K.; Ranganathan, S.; Vinh, N.N.; Dung, P.H.T.; Thanh, H.N.; et al. Wearing Masks as a Protective Measure for Children against Traffic-Related Air Pollution: A Comparison of Perceptions between School Children and Their Caregivers in Ho Chi Minh City, Vietnam. Tropical Medicine & International Health 2023, 28, 753–762. [Google Scholar] [CrossRef]
- Beauchamp, J.D.; Mayhew, C.A. Revisiting the Rationale of Mandatory Masking. J. Breath Res. 2023, 17, 042001. [Google Scholar] [CrossRef]
- Sukul, P.; Bartels, J.; Fuchs, P.; Trefz, P.; Remy, R.; Rührmund, L.; Kamysek, S.; Schubert, J.K.; Miekisch, W. Effects of COVID-19 Protective Face Masks and Wearing Durations on Respiratory Haemodynamic Physiology and Exhaled Breath Constituents. European Respiratory Journal 2022, 60. [Google Scholar] [CrossRef]
- Høeg, T.B.; González-Dambrauskas, S.; Prasad, V. Does Equipoise Exist for Masking Children for COVID-19? Public Health in Practice 2023, 6, 100428. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. How Many Children Are There in the World? Available online: https://data.unicef.org/how-many/how-many-children-under-18-are-in-the-world/ (accessed on 26 August 2024).
- World Population Clock: 8.2 Billion People (LIVE, 2024) - Worldometer. Available online: https://www.worldometers.info/world-population/ (accessed on 26 August 2024).
- Faustman, E.M.; Silbernagel, S.M.; Fenske, R.A.; Burbacher, T.M.; Ponce, R.A. Mechanisms Underlying Children’s Susceptibility to Environmental Toxicants. Environ Health Perspect 2000, 108 Suppl 1, 13–21. [Google Scholar] [CrossRef]
- Scheuplein, R.; Charnley, G.; Dourson, M. Differential Sensitivity of Children and Adults to Chemical Toxicity: I. Biological Basis. Regulatory Toxicology and Pharmacology 2002, 35, 429–447. [Google Scholar] [CrossRef]
- Roberge, R. Facemask Use by Children during Infectious Disease Outbreaks. Biosecur Bioterror 2011, 9, 225–231. [Google Scholar] [CrossRef]
- Eberhart, M.; Orthaber, S.; Kerbl, R. The Impact of Face Masks on Children-A Mini Review. Acta Paediatr 2021, 110, 1778–1783. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions, Julian P. T. Higgins, J.P.T., James Thomas, Jacqueline Chandler, Miranda Cumpston, Tianjing Li, Matthew J. Page, Vivian A. Welch, Ed.; Wiley Cochrane Series; 2nd ed.; WILEY Blackwell, 2019; ISBN 978-1-119-53662-8. [Google Scholar]
- Loke, Y.K.; Price, D.; Herxheimer, A. Cochrane Adverse Effects Methods Group Systematic Reviews of Adverse Effects: Framework for a Structured Approach. BMC Med Res Methodol 2007, 7, 32. [Google Scholar] [CrossRef] [PubMed]
- Zorzela, L.; Loke, Y.K.; Ioannidis, J.P.; Golder, S.; Santaguida, P.; Altman, D.G.; Moher, D.; Vohra, S.; Group, P. harms PRISMA Harms Checklist: Improving Harms Reporting in Systematic Reviews. BMJ 2016, 352, i157. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, J.; Theuring, S.; van Loon, W.; Mall, M.A.; Seybold, J.; Kurth, T.; Rubio-Acero, R.; Wieser, A.; Mockenhaupt, F.P. SARS-CoV-2 Seroprevalence in a Berlin Kindergarten Environment: A Cross-Sectional Study, September 2021. Children 2024, 11, 405. [Google Scholar] [CrossRef] [PubMed]
- Jarnig, G.; Kerbl, R.; van Poppel, M.N.M. Effects of Wearing FFP2 Masks on SARS-CoV-2 Infection Rates in Classrooms. International Journal of Environmental Research and Public Health 2022, 19, 13511. [Google Scholar] [CrossRef]
- Orey, F.A.H.; Sodal, A.M.; Mohamoud, J.H.; Garba, B.; Mohamed, I.H.; Adam, M.H.; Dahie, H.A.; Nur, M.A.S.; Dirie, N.I. Investigation of Severe Acute Respiratory Syndrome Coronavirus 2 Antibodies among the Paediatric Population in Mogadishu, Somalia. Trans R Soc Trop Med Hyg 2023, 117, 139–146. [Google Scholar] [CrossRef]
- Svetina, L.; Košec, A. Wearing Masks to Prevent One Epidemic May Mask Another. Journal of Infection Prevention 2023, 24, 228–231. [Google Scholar] [CrossRef]
- Littlecott, H.; Krishnaratne, S.; Burns, J.; Rehfuess, E.; Sell, K.; Klinger, C.; Strahwald, B.; Movsisyan, A.; Metzendorf, M.-I.; Schoenweger, P.; et al. Measures Implemented in the School Setting to Contain the COVID-19 Pandemic. Cochrane Database Syst Rev 2024, 5, CD015029. [Google Scholar] [CrossRef]
- Viera, L. Effect of Face Mask on Lowering COVID-19 Incidence in School Settings: A Systematic Review. Journal of School Health 2024, 94, 878–888. [Google Scholar] [CrossRef]
- Jarnig, G.; Kerbl, R.; van Poppel, M.N.M. How Middle and High School Students Wear Their Face Masks in Classrooms and School Buildings. Healthcare 2022, 10, 1641. [Google Scholar] [CrossRef]
- Satapathy, D.; Babu, T.A.; Bommidi, S.; Marimuthu, Y.; Bhavana, A.M. Prevalence and Predictors of Effective Face Mask Usage Among Children During the COVID-19 Pandemic. Indian Pediatr 2024, 61, 66–68. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Little Evidence for Facemask Use in Children against COVID-19. Acta Paediatr 2021, 110, 742–743. [Google Scholar] [CrossRef] [PubMed]
- Coma, E.; Català, M.; Méndez-Boo, L.; Alonso, S.; Hermosilla, E.; Alvarez-Lacalle, E.; Pino, D.; Medina, M.; Asso, L.; Gatell, A.; et al. Unravelling the Role of the Mandatory Use of Face Covering Masks for the Control of SARS-CoV-2 in Schools: A Quasi-Experimental Study Nested in a Population-Based Cohort in Catalonia (Spain). Archives of Disease in Childhood 2022. [Google Scholar] [CrossRef]
- Juutinen, A.; Sarvikivi, E.; Laukkanen-Nevala, P.; Helve, O. Face Mask Recommendations in Schools Did Not Impact COVID-19 Incidence among 10–12-Year-Olds in Finland – Joinpoint Regression Analysis. BMC Public Health 2023, 23, 730. [Google Scholar] [CrossRef] [PubMed]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Health Effects of Wildfire Smoke in Children and Public Health Tools: A Narrative Review. J Expo Sci Environ Epidemiol 2021, 31, 1–20. [Google Scholar] [CrossRef]
- Janapatla, R.P.; Chen, C.-L.; Dudek, A.; Li, H.-C.; Yang, H.-P.; Su, L.-H.; Chiu, C.-H. Serotype Transmission Dynamics and Reduced Incidence of Invasive Pneumococcal Disease Caused by Different Serotypes after Implementation of Non-Pharmaceutical Interventions during COVID-19 Pandemic. Eur Respir J 2021, 58, 2100978. [Google Scholar] [CrossRef]
- Xiao, J.; Dai, J.; Hu, J.; Liu, T.; Gong, D.; Li, X.; Kang, M.; Zhou, Y.; Li, Y.; Quan, Y.; et al. Co-Benefits of Nonpharmaceutical Intervention against COVID-19 on Infectious Diseases in China: A Large Population-Based Observational Study. The Lancet Regional Health - Western Pacific 2021, 17, 100282. [Google Scholar] [CrossRef]
- Suess, T.; Remschmidt, C.; Schink, S.B.; Schweiger, B.; Nitsche, A.; Schroeder, K.; Doellinger, J.; Milde, J.; Haas, W.; Koehler, I.; et al. The Role of Facemasks and Hand Hygiene in the Prevention of Influenza Transmission in Households: Results from a Cluster Randomised Trial; Berlin, Germany, 2009-2011. BMC Infect Dis 2012, 12, 26. [Google Scholar] [CrossRef] [PubMed]
- Suess, T.; Remschmidt, C.; Schink, S.; Luchtenberg, M.; Haas, W.; Krause, G.; Buchholz, U. Facemasks and Intensified Hand Hygiene in a German Household Trial during the 2009/2010 Influenza A(H1N1) Pandemic: Adherence and Tolerability in Children and Adults. Epidemiol Infect 2011, 139, 1895–1901. [Google Scholar] [CrossRef]
- Science, M.; Caldeira-Kulbakas, M.; Parekh, R.S.; Maguire, B.R.; Carroll, S.; Anthony, S.J.; Bitnun, A.; Bourns, L.E.; Campbell, D.M.; Cohen, E.; et al. Effect of Wearing a Face Mask on Hand-to-Face Contact by Children in a Simulated School Environment: The Back-to-School COVID-19 Simulation Randomized Clinical Trial. JAMA Pediatr 2022, 176, 1169–1175. [Google Scholar] [CrossRef]
- Villers, J.; Henriques, A.; Calarco, S.; Rognlien, M.; Mounet, N.; Devine, J.; Azzopardi, G.; Elson, P.; Andreini, M.; Tarocco, N.; et al. SARS-CoV-2 Aerosol Transmission in Schools: The Effectiveness of Different Interventions. Swiss Med Wkly 2022, 152, w30178. [Google Scholar] [CrossRef]
- Armero, G.; Guitart, C.; Soler-Garcia, A.; Melé, M.; Esteva, C.; Brotons, P.; Muñoz-Almagro, C.; Jordan, I.; Launes, C. Non-Pharmacological Interventions During SARS-CoV-2 Pandemic: Effects on Pediatric Viral Respiratory Infections. Arch Bronconeumol 2024, S0300-2896(24)00183-2. [Google Scholar] [CrossRef] [PubMed]
- Banholzer, N.; Zürcher, K.; Jent, P.; Bittel, P.; Furrer, L.; Egger, M.; Hascher, T.; Fenner, L. SARS-CoV-2 Transmission with and without Mask Wearing or Air Cleaners in Schools in Switzerland: A Modeling Study of Epidemiological, Environmental, and Molecular Data. PLOS Medicine 2023, 20, e1004226. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, A.; Asayama, K.; Obara, T.; Yagi, N.; Ohkubo, T. Behavioral Changes of Preventive Activities of Influenza among Children in Satellite Cities of a Metropolitan Area of Tokyo, Japan, by the COVID-19 Pandemic. BMC Public Health 2023, 23, 727. [Google Scholar] [CrossRef]
- Sombetzki, M.; Lücker, P.; Ehmke, M.; Bock, S.; Littmann, M.; Reisinger, E.C.; Hoffmann, W.; Kästner, A. Impact of Changes in Infection Control Measures on the Dynamics of COVID-19 Infections in Schools and Pre-Schools. Front. Public Health 2021, 9. [Google Scholar] [CrossRef]
- Theuring, S.; Thielecke, M.; Loon, W. van; Hommes, F.; Hülso, C.; Haar, A. von der; Körner, J.; Schmidt, M.; Böhringer, F.; Mall, M.A.; et al. SARS-CoV-2 Infection and Transmission in School Settings during the Second COVID-19 Wave: A Cross-Sectional Study, Berlin, Germany, November 2020. Eurosurveillance 2021, 26, 2100184. [Google Scholar] [CrossRef]
- Qin, Z.; Shi, L.; Xue, Y.; Lin, H.; Zhang, J.; Liang, P.; Lu, Z.; Wu, M.; Chen, Y.; Zheng, X.; et al. Prevalence and Risk Factors Associated With Self-Reported Psychological Distress Among Children and Adolescents During the COVID-19 Pandemic in China. JAMA Network Open 2021, 4, e2035487. [Google Scholar] [CrossRef] [PubMed]
- Fox, G.J.; Redwood, L.; Chang, V.; Ho, J. The Effectiveness of Individual and Environmental Infection Control Measures in Reducing the Transmission of Mycobacterium Tuberculosis: A Systematic Review. Clinical Infectious Diseases 2021, 72, 15–26. [Google Scholar] [CrossRef]
- Sarkar, M. Tuberculosis Infection Prevention and Control. Indian Journal of Tuberculosis 2024. [Google Scholar] [CrossRef]
- Kwon, M.; Jang, E.-M.; Yang, W. Mask-Wearing Perception of Preschool Children in Korea during the COVID-19 Pandemic: A Cross-Sectional Study. International Journal of Environmental Research and Public Health 2022, 19, 11443. [Google Scholar] [CrossRef]
- Halbur, M.; Kodak, T.; McKee, M.; Carroll, R.; Preas, E.; Reidy, J.; Cordeiro, M.C. Tolerance of Face Coverings for Children with Autism Spectrum Disorder. J Appl Behav Anal 2021, 54, 600–617. [Google Scholar] [CrossRef]
- Sivaraman, M.; Virues-Ortega, J.; Roeyers, H. Telehealth Mask Wearing Training for Children with Autism during the COVID-19 Pandemic. J Appl Behav Anal 2021, 54, 70–86. [Google Scholar] [CrossRef] [PubMed]
- Tamon, H.; Itahashi, T.; Yamaguchi, S.; Tachibana, Y.; Fujino, J.; Igarashi, M.; Kawashima, M.; Takahashi, R.; Shinohara, N.A.; Noda, Y.; et al. Autistic Children and Adolescents with Frequent Restricted Interest and Repetitive Behavior Showed More Difficulty in Social Cognition during Mask-Wearing during the COVID-19 Pandemic: A Multisite Survey. BMC Psychiatry 2022, 22, 608. [Google Scholar] [CrossRef] [PubMed]
- Ammann, P.; Ulyte, A.; Haile, S.R.; Puhan, M.A.; Kriemler, S.; Radtke, T. Perceptions towards Mask Use in School Children during the SARS-CoV-2 Pandemic: Descriptive Results from the Longitudinal Ciao Corona Cohort Study. Swiss Med Wkly 2022, 152, w30165. [Google Scholar] [CrossRef] [PubMed]
- Omaleki, V.; Gonzalez, A.F.; Hassani, A.; Flores, M.; Streuli, S.; Guerra, A.W.; Fielding-Miller, R. “They Protect Us as If They Were Our Mom” Masking Attitudes from Freelist Survey Data and Qualitative Interviews in San Diego School Communities. J Community Health 2024, 49, 17–25. [Google Scholar] [CrossRef]
- Aronu, A.E.; Chinawa, J.M.; Nduagubam, O.C.; Ossai, E.N.; Chinawa, A.T.; Igwe, W.C. Maternal Perception of Masking in Children as a Preventive Strategy for COVID-19 in Nigeria: A Multicentre Study. PLOS ONE 2020, 15, e0242650. [Google Scholar] [CrossRef]
- Assathiany, R.; Salinier, C.; Béchet, S.; Dolard, C.; Kochert, F.; Bocquet, A.; Levy, C. Face Masks in Young Children During the COVID-19 Pandemic: Parents’ and Pediatricians’ Point of View. Front. Pediatr. 2021, 9. [Google Scholar] [CrossRef]
- Education Recovery in Early Years Providers: Spring 2022. Available online: https://www.gov.uk/government/publications/education-recovery-in-early-years-providers-spring-2022/education-recovery-in-early-years-providers-spring-2022 (accessed on 1 February 2023).
- Charney, S.A.; Camarata, S.M.; Chern, A. Potential Impact of the COVID-19 Pandemic on Communication and Language Skills in Children. Otolaryngol Head Neck Surg 2021, 165, 1–2. [Google Scholar] [CrossRef]
- Goldin, A.; Weinstein, B.; Shiman, N. How Do Medical Masks Degrade Speech Reception? The Hearing Review 2020, 27, 8–9. [Google Scholar]
- Kwon, M.; Yang, W. Effects of Face Masks and Acoustical Environments on Speech Recognition by Preschool Children in an Auralised Classroom. Appl Acoust 2023, 202, 109149. [Google Scholar] [CrossRef]
- Lalonde, K.; Buss, E.; Miller, M.K.; Leibold, L.J. Face Masks Impact Auditory and Audiovisual Consonant Recognition in Children With and Without Hearing Loss. Front. Psychol. 2022, 13. [Google Scholar] [CrossRef]
- Taxacher, T.; Rupp, M.; Pauli, C.; Profanter, C.; Dejakum, K.; Steindl, R.; Ostertag, P. [Impact of face masks on speech intelligibility of normal hearing children]. Laryngorhinootologie 2023, 102, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Carnevali, L.; Gui, A.; Jones, E.J.H.; Farroni, T. Face Processing in Early Development: A Systematic Review of Behavioral Studies and Considerations in Times of COVID-19 Pandemic. Front. Psychol. 2022, 13. [Google Scholar] [CrossRef] [PubMed]
- Stajduhar, A.; Ganel, T.; Avidan, G.; Rosenbaum, R.S.; Freud, E. Face Masks Disrupt Holistic Processing and Face Perception in School-Age Children. Cognitive Research: Principles and Implications 2022, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Drössler, S.; Horvath, K.; Freiberg, A.; Kämpf, D.; Spura, A.; Buhs, B.; Seidler, A. [Effects of Wearing Face Masks to Prevent Infectious Diseases On Children’s and Adolescents’ Well-Being and Behavior: An Interview Study]. Gesundheitswesen 2023, 85, 688–696. [Google Scholar] [CrossRef]
- Gori, M.; Schiatti, L.; Amadeo, M.B. Masking Emotions: Face Masks Impair How We Read Emotions. Front Psychol 2021, 12, 669432. [Google Scholar] [CrossRef]
- Bourke, L.; Lingwood, J.; Gallagher-Mitchell, T.; López-Pérez, B. The Effect of Face Mask Wearing on Language Processing and Emotion Recognition in Young Children. J Exp Child Psychol 2023, 226, 105580. [Google Scholar] [CrossRef] [PubMed]
- Surrain, S.; Mesa, M.P.; Assel, M.A.; Zucker, T.A. Does Assessor Masking Affect Kindergartners’ Performance on Oral Language Measures? A COVID-19 Era Experiment With Children From Diverse Home Language Backgrounds. Lang Speech Hear Serv Sch 2023, 54, 1323–1332. [Google Scholar] [CrossRef]
- Singh, L.; Quinn, P.C. Effects of Face Masks on Language Comprehension in Bilingual Children. Infancy 2023, 28, 738–753. [Google Scholar] [CrossRef]
- Chester, M.; Plate, R.C.; Powell, T.; Rodriguez, Y.; Wagner, N.J.; Waller, R. The COVID-19 Pandemic, Mask-Wearing, and Emotion Recognition during Late-Childhood. Social Development 2023, 32, 315–328. [Google Scholar] [CrossRef]
- Ger, E.; Manfredi, M.; Osório, A.A.C.; Ribeiro, C.F.; Almeida, A.; Güdel, A.; Calbi, M.; Daum, M.M. Duration of Face Mask Exposure Matters: Evidence from Swiss and Brazilian Kindergartners’ Ability to Recognise Emotions. Cognition and Emotion 2024, 38, 857–871. [Google Scholar] [CrossRef]
- Miyazaki, Y.; Kamatani, M.; Tsurumi, S.; Suda, T.; Wakasugi, K.; Matsunaga, K.; Kawahara, J.I. Effects of Wearing an Opaque or Transparent Face Mask on the Perception of Facial Expressions: A Comparative Study between Japanese School-Aged Children and Adults. Perception 2023, 52, 782–798. [Google Scholar] [CrossRef] [PubMed]
- Gil, S.; Le Bigot, L. Emotional Face Recognition When a Colored Mask Is Worn: A Cross-Sectional Study. Sci Rep 2023, 13, 174. [Google Scholar] [CrossRef] [PubMed]
- Boucher, J.D.; Ekman, P. Facial Areas and Emotional Information. Journal of Communication 1975, 25, 21–29. [Google Scholar] [CrossRef]
- Eisenbarth, H.; Alpers, G.W. Happy Mouth and Sad Eyes: Scanning Emotional Facial Expressions. Emotion 2011, 11, 860–865. [Google Scholar] [CrossRef]
- Guarnera, M.; Hichy, Z.; Cascio, M.I.; Carrubba, S. Facial Expressions and Ability to Recognize Emotions From Eyes or Mouth in Children. Europe’s Journal of Psychology 2015, 11, 183–196. [Google Scholar] [CrossRef]
- Wegrzyn, M.; Vogt, M.; Kireclioglu, B.; Schneider, J.; Kissler, J. Mapping the Emotional Face. How Individual Face Parts Contribute to Successful Emotion Recognition. PLOS ONE 2017, 12, e0177239. [Google Scholar] [CrossRef]
- Gagnon, M.; Gosselin, P.; Maassarani, R. Children’s Ability to Recognize Emotions From Partial and Complete Facial Expressions. The Journal of Genetic Psychology 2014, 175, 416–430. [Google Scholar] [CrossRef]
- Kestenbaum, R. Feeling Happy versus Feeling Good: The Processing of Discrete and Global Categories of Emotional Expressions by Children and Adults. Developmental Psychology 1992, 28, 1132–1142. [Google Scholar] [CrossRef]
- Proverbio, A.M.; Cerri, A. The Recognition of Facial Expressions Under Surgical Masks: The Primacy of Anger. Frontiers in Neuroscience 2022, 16. [Google Scholar] [CrossRef]
- Rinck, M.; Primbs, M.A.; Verpaalen, I.A.M.; Bijlstra, G. Face Masks Impair Facial Emotion Recognition and Induce Specific Emotion Confusions. Cognitive Research: Principles and Implications 2022, 7, 83. [Google Scholar] [CrossRef]
- Tsantani, M.; Podgajecka, V.; Gray, K.L.H.; Cook, R. How Does the Presence of a Surgical Face Mask Impair the Perceived Intensity of Facial Emotions? PLOS ONE 2022, 17, e0262344. [Google Scholar] [CrossRef] [PubMed]
- Giordano, K.; Palmieri, C.S.; LaTourette, R.; Godoy, K.M.; Denicola, G.; Paulino, H.; Kosecki, O. Face Masks and Emotion Literacy in Preschool Children: Implications During the COVID-19 Pandemic. Early Child Educ J 2022, 1–9. [Google Scholar] [CrossRef]
- Freiberg, A.; Horvath, K.; Hahne, T.M.; Drössler, S.; Kämpf, D.; Spura, A.; Buhs, B.; Reibling, N.; De Bock, F.; Apfelbacher, C.; et al. [Impact of wearing face masks in public to prevent infectious diseases on the psychosocial development in children and adolescents: a systematic review]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 64, 1592–1602. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, X.; Sun, R. The Effect of Masks on Infants’ Ability to Fast-Map and Generalize New Words. J Child Lang 2024, 51, 637–655. [Google Scholar] [CrossRef] [PubMed]
- Coelho, S.G.; Segovia, A.; Anthony, S.J.; Lin, J.; Pol, S.; Crosbie, J.; Science, M.; Matava, C.T.; Parekh, R.S.; Caldeira-Kulbakas, M.; et al. Return to School and Mask-Wearing in Class during the COVID-19 Pandemic: Student Perspectives from a School Simulation Study. Paediatrics & Child Health 2022, 27, S15–S21. [Google Scholar] [CrossRef]
- Nobrega, M.; Opice, R.; Lauletta, M.M.; Nobrega, C.A. How Face Masks Can Affect School Performance. Int J Pediatr Otorhinolaryngol 2020, 138, 110328. [Google Scholar] [CrossRef]
- Shaw, C.A.; Lee, K.R.; Williams, A.; Shaw, N.A.; Weeks, D.; Jackson, L.; Williams, K.N. Best Practices for Communication While Wearing Facemasks: A Scoping Review. J Nurs Scholarsh 2024, 56, 227–238. [Google Scholar] [CrossRef]
- Schwarz, J.; Li, K.K.; Sim, J.H.; Zhang, Y.; Buchanan-Worster, E.; Post, B.; Gibson, J.L.; McDougall, K. Semantic Cues Modulate Children’s and Adults’ Processing of Audio-Visual Face Mask Speech. Front. Psychol. 2022, 13. [Google Scholar] [CrossRef]
- Mitsven, S.G.; Perry, L.K.; Jerry, C.M.; Messinger, D.S. Classroom Language during COVID-19: Associations between Mask-Wearing and Objectively Measured Teacher and Preschooler Vocalizations. Front. Psychol. 2022, 13. [Google Scholar] [CrossRef]
- Schlegtendal, A.; Eitner, L.; Falkenstein, M.; Hoffmann, A.; Lücke, T.; Sinningen, K.; Brinkmann, F. To Mask or Not to Mask—Evaluation of Cognitive Performance in Children Wearing Face Masks during School Lessons (MasKids). Children 2022, 9, 95. [Google Scholar] [CrossRef]
- Rodeheffer, C.D.; Chabal, S.; Clarke, J.M.; Fothergill, D.M. Acute Exposure to Low-to-Moderate Carbon Dioxide Levels and Submariner Decision Making. Aerospace Medicine and Human Performance 2018, 89, 520–525. [Google Scholar] [CrossRef] [PubMed]
- Hurley, R.F.; Belyamani, M.A.; Djamasbi, S.; Somasse, G.B.; Strauss, S.; Zhang, H.; Zhang, J.; Liu, S. High CO2 Exposure Due to Facemask Wear Is Unlikely to Impair Cognition Even in a Warm Environment after a Long-Term Adaptation. Energy and Built Environment 2024. [Google Scholar] [CrossRef]
- Smerdon, D. The Effect of Masks on Cognitive Performance. Proceedings of the National Academy of Sciences 2022, 119, e2206528119. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Q.; Song, J.; Shi, D.; Dung, C.-H. Protective Facemask-Induced Facial Thermal Stress and Breathing Burden during Exercise in Gyms. Building and Environment 2023, 244, 110840. [Google Scholar] [CrossRef]
- Azuma, K.; Kagi, N.; Yanagi, U.; Osawa, H. Effects of Low-Level Inhalation Exposure to Carbon Dioxide in Indoor Environments: A Short Review on Human Health and Psychomotor Performance. Environment International 2018, 121, 51–56. [Google Scholar] [CrossRef]
- Allen, J.G.; MacNaughton, P.; Cedeno-Laurent, J.G.; Cao, X.; Flanigan, S.; Vallarino, J.; Rueda, F.; Donnelly-McLay, D.; Spengler, J.D. Airplane Pilot Flight Performance on 21 Maneuvers in a Flight Simulator under Varying Carbon Dioxide Concentrations. J Expo Sci Environ Epidemiol 2019, 29, 457–468. [Google Scholar] [CrossRef]
- Pang, L.; Zhang, J.; Cao, X.; Wang, X.; Liang, J.; Zhang, L.; Guo, L. The Effects of Carbon Dioxide Exposure Concentrations on Human Vigilance and Sentiment in an Enclosed Workplace Environment. Indoor Air 2021, 31, 467–479. [Google Scholar] [CrossRef]
- Du, B.; Tandoc, M.C.; Mack, M.L.; Siegel, J.A. Indoor CO2 Concentrations and Cognitive Function: A Critical Review. Indoor Air 2020, 30, 1067–1082. [Google Scholar] [CrossRef]
- Zhang, X.; Wargocki, P.; Lian, Z.; Thyregod, C. Effects of Exposure to Carbon Dioxide and Bioeffluents on Perceived Air Quality, Self-Assessed Acute Health Symptoms, and Cognitive Performance. Indoor Air 2017, 27, 47–64. [Google Scholar] [CrossRef]
- Jagim, A.R.; Dominy, T.A.; Camic, C.L.; Wright, G.; Doberstein, S.; Jones, M.T.; Oliver, J.M. Acute Effects of the Elevation Training Mask on Strength Performance in Recreational Weight Lifters. J Strength Cond Res 2018, 32, 482–489. [Google Scholar] [CrossRef]
- Johnson, A.T. Respirator Masks Protect Health but Impact Performance: A Review. J Biol Eng 2016, 10. [Google Scholar] [CrossRef] [PubMed]
- Kyung, S.Y.; Kim, Y.; Hwang, H.; Park, J.-W.; Jeong, S.H. Risks of N95 Face Mask Use in Subjects With COPD. Respir Care 2020, 65, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Li, G.; He, Y.; Zhang, Z.; Ding, Y. Effects of Wearing Masks on Human Health and Comfort during the COVID-19 Pandemic. IOP Conf. Ser.: Earth Environ. Sci. 2020, 531, 012034. [Google Scholar] [CrossRef]
- Lang, X.; Vasquez, N.G.; Liu, W.; Wyon, D.P.; Wargocki, P. Effects of Wearing Masks Indoors on the Cognitive Performance and Physiological and Subjective Responses of Healthy Young Adults. Building and Environment 2024, 252, 111248. [Google Scholar] [CrossRef]
- Rebmann, T.; Carrico, R.; Wang, J. Physiologic and Other Effects and Compliance with Long-Term Respirator Use among Medical Intensive Care Unit Nurses. Am J Infect Control 2013, 41, 1218–1223. [Google Scholar] [CrossRef]
- Rosner, E. Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. Journal of Infectious Diseases and Epidemiology 2020, 6, 130. [Google Scholar] [CrossRef]
- Tornero-Aguilera, J.F.; Clemente-Suárez, V.J. Cognitive and Psychophysiological Impact of Surgical Mask Use during University Lessons. Physiol Behav 2021, 113342–113342. [Google Scholar] [CrossRef]
- Vakharia, R.J.; Jani, I.; Yadav, S.; Kurian, T. To Study Acute Changes in Brain Oxygenation on MRI in Healthcare Workers Using N95 Mask and PPE Kits for Six Hours a Day. Indian J Radiol Imaging 2021, 31, 893–900. [Google Scholar] [CrossRef]
- Preest, E.; Greenhalgh, T.; Farrier, C.; van der Westhuizen, H.-M. Children’s Experiences of Mask-Wearing: A Systemic Review and Narrative Synthesis. Journal of Evaluation in Clinical Practice 2024, 30, 585–621. [Google Scholar] [CrossRef]
- Smart, N.R.; Horwell, C.J.; Smart, T.S.; Galea, K.S. Assessment of the Wearability of Facemasks against Air Pollution in Primary School-Aged Children in London. International Journal of Environmental Research and Public Health 2020, 17, 3935. [Google Scholar] [CrossRef]
- Chhabra, K.; Sood, S.; Bhatia, H.P.; Sharma, N.; Singh, A. Comparative Evaluation of Psychophysiological Response of Children with Special Health Care Needs to Use of Facemask-Eyeshield and Visor in a Dental Setting-A Cross-Sectional Study. Spec Care Dentist 2020, 40, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Wild, B.M.; Kornfeld, B. Facial Recognition: More Than Just a Phone Problem. Pediatr Ann 2021, 50, e52–e54. [Google Scholar] [CrossRef] [PubMed]
- Ratchatavech, K.; Techasatian, L.; Panombualert, S.; Uppala, R. The Adverse and Advantage Effects of Wearing a Facemask in Thai Children: A Survey During the COVID-19 Pandemic. J Prim Care Community Health 2022, 13, 21501319221131704. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, S.; Jenetzky, E.; Krafft, H.; Maurer, T.; Martin, D. Corona child studies “Co-Ki”: first results of a Germany-wide register on mouth and nose covering (mask) in children. Monatsschr Kinderheilkd 2021, 169, 353–365. [Google Scholar] [CrossRef]
- Beytout, Q.; Pepiot, J.; Maruani, A.; Devulder, D.; Aubert, R.; Beylot-Barry, M.; Amici, J.-M.; Jullien, D.; Mahé, E.; Association France Psoriasis; et al. Impact of the COVID-19 Pandemic on Children with Psoriasis. Ann Dermatol Venereol 2021, 148, 106–111. [Google Scholar] [CrossRef]
- Kaliyadan, F.; Ashique, K.T.; Jayasree, P. Increased Incidence of Facial Pityriasis Versicolor in Children during the COVID-19 Pandemic-A Consequence of Mask Usage? Pediatr Dermatol 2022, 39, 834–835. [Google Scholar] [CrossRef]
- Shoaib, M.; Chomayil, Y.; Zafar, M. Corneal Abrasion Due to Face Mask in Children: A Novel and Potential Mechanism of Injury Related to COVID 19 Pandemic. Vis J Emerg Med 2022, 27, 101290. [Google Scholar] [CrossRef]
- Zanotti, B.; Parodi, P.C.; Riccio, M.; De Francesco, F.; Zingaretti, N. Can the Elastic of Surgical Face Masks Stimulate Ear Protrusion in Children? Aesth Plast Surg 2020, 44, 1947–1950. [Google Scholar] [CrossRef]
- Ali, F.M.; Wasli, A.S.; Hobani, A.H.; Faraj, S.H.A.; Mashiakhy, E.H.; Alkhayrat, A.M.; Khawaji, R.A. Prevention of Ear-looped Face Mask-induced Pressure Injury on Ears: A Technical Report with Review of Literature. Advancements in Life Sciences 2024, 11, 539–543. [Google Scholar] [CrossRef]
- WHO Conference, I.H. WHO - Constitution of the World Health Organization. 1946. Bulletin of the World Health Organization 2002, 80, 983–984. [Google Scholar]
- Amirav, I.; Lavie, M. Spurious Asthma Presentation during COVID-19. Children 2022, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Tse, G.; Li, G. Running with Face Masks or Respirators Can Be Detrimental to the Respiratory and Cardiovascular Systems. Cardiovascular Innovations and Applications 2021, 6, 63. [Google Scholar] [CrossRef]
- Reychler, G.; Standaert, M.; Audag, N.; Caty, G.; Robert, A.; Poncin, W. Effects of Surgical Facemasks on Perceived Exertion during Submaximal Exercise Test in Healthy Children. Eur J Pediatr 2022, 181, 2311–2317. [Google Scholar] [CrossRef] [PubMed]
- Mallet, M.C.; Hitzler, M.; Lurà, M.; Kuehni, C.E.; Regamey, N. Facemasks Do Not Lead to Abnormal Gas Exchange during Treadmill Exercise Testing in Children. ERJ Open Res 2022, 8, 00613–02021. [Google Scholar] [CrossRef]
- Hodges, M.; Freigeh, G.E.; Troost, J.; Baptist, A.P.; Gupta, M. Assessment of Mask Use on Oxygen Saturation in Adults and Children with Asthma. Allergy Asthma Proc 2024, 45, 24–32. [Google Scholar] [CrossRef]
- Schulte-Körne, B.; Hollmann, W.; Vassiliadis, A.; Predel, H.-G. [Effects of surgical face masks on exercise performance and perceived exertion of exercise in well-trained healthy boys]. Wien Med Wochenschr 2022, 172, 59–62. [Google Scholar] [CrossRef]
- Weigelt, A.; Schöffl, I.; Rottermann, K.; Wällisch, W.; Müller, S.K.; Dittrich, S.; Hübner, M.J. Sports despite Masks: No Negative Effects of FFP2 Face Masks on Cardiopulmonary Exercise Capacity in Children. Eur J Pediatr 2024, 183, 639–648. [Google Scholar] [CrossRef]
- Sukul, P.; Richter, A.; Junghanss, C.; Schubert, J.K.; Miekisch, W. Origin of Breath Isoprene in Humans Is Revealed via Multi-Omic Investigations. Commun Biol 2023, 6, 1–12. [Google Scholar] [CrossRef]
- Ahmadi, A.; Sabri, M.R.; Navabi, Z.S. Effect of Face Mask on Pulmonary Artery Pressure during Echocardiography in Children and Adolescents. Clin Exp Pediatr 2024, 67, 161–167. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Testa, A.; Marcellino, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; Sanseviero, M.; Del Giudice, E.; et al. Assessment of Respiratory Function in Infants and Young Children Wearing Face Masks During the COVID-19 Pandemic. JAMA Netw Open 2021, 4, e210414. [Google Scholar] [CrossRef]
- Lubrano, R.; Bloise, S.; Marcellino, A.; Ciolli, C.P.; Testa, A.; De Luca, E.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; et al. Effects of N95 Mask Use on Pulmonary Function in Children. J Pediatr 2021, 237, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, R.; Bloise, S.; Marcellino, A.; Proietti Ciolli, C.; Testa, A.; De Luca, E.; Dilillo, A.; Mallardo, S.; Isoldi, S.; Martucci, V.; et al. Assessment of Respiratory Function in Children Wearing a N95 Mask with or without an Exhalation Valve: Data Compared. Data Brief 2021, 39, 107550. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, R.; Bloise, S.; Sanseviero, M.; Marcellino, A.; Proietti Ciolli, C.; De Luca, E.; Testa, A.; Dilillo, A.; Mallardo, S.; Isoldi, S.; et al. Assessment of Cardio-Respiratory Function in Overweight and Obese Children Wearing Face Masks during the COVID-19 Pandemic. Children (Basel) 2022, 9, 1053. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.P.; Layman, J.; Willis, J. Physiologic Effects of Surgical Masking in Children versus Adults. PeerJ 2023, 11, e15474. [Google Scholar] [CrossRef]
- Goh, D.Y.T.; Mun, M.W.; Lee, W.L.J.; Teoh, O.H.; Rajgor, D.D. A Randomised Clinical Trial to Evaluate the Safety, Fit, Comfort of a Novel N95 Mask in Children. Scientific Reports 2019, 9, 18952. [Google Scholar] [CrossRef]
- Happernegg, R.; Kerbl, R. The Influence of Wearing Surgical and FFP2 Face Masks on Physiological Parameters in Children and Adolescents - a Pilot Study. Klin Padiatr 2023, 235, 101–102. [Google Scholar] [CrossRef]
- Castro, P.A.S.V. de; Freire, B.R.; Petroianu, A. Effects of Face Mask on Pulse Rate and Blood Oxygenation. Einstein (Sao Paulo) 2023, 21, eAO0349. [Google Scholar] [CrossRef]
- Canellas, E.; Vera, P.; Nerin, C.; Goshawk, J.; Dreolin, N. Migration of Contaminants from Printed Masks for Children to Saliva Simulant Using Liquid Chromatography Coupled to Ion Mobility-Time of Flight-Mass Spectrometry and Gas Chromatography-Mass Spectrometry. Ecotoxicol Environ Saf 2023, 267, 115644. [Google Scholar] [CrossRef]
- Ryu, H.; Kim, Y.-H. Measuring the Quantity of Harmful Volatile Organic Compounds Inhaled through Masks. Ecotoxicology and Environmental Safety 2023, 256, 114915. [Google Scholar] [CrossRef]
- Jefferson, T.; Mar, C.B.D.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Bawazeer, G.A.; Driel, M.L. van; Jones, M.A.; Thorning, S.; Beller, E.M.; et al. Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses. Cochrane Database of Systematic Reviews 2020. [Google Scholar] [CrossRef]
- World Health Organization Non-Pharmaceutical Public Health Measures for Mitigating the Risk and Impact of Epidemic and Pandemic Influenza: Annex: Report of Systematic Literature Reviews. 2019.
- Villani, A.; Bozzola, E.; Staiano, A.; Agostiniani, R.; Del Vecchio, A.; Zamperini, N.; Marino, F.; Vecchio, D.; Corsello, G. Facial Masks in Children: The Position Statement of the Italian Pediatric Society. Italian Journal of Pediatrics 2020, 46, 132. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; Chu, D.K.; Akl, E.A.; El-harakeh, A.; Bognanni, A.; et al. Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis. The Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Leung, N.H.L.; Chu, D.K.W.; Shiu, E.Y.C.; Chan, K.-H.; McDevitt, J.J.; Hau, B.J.P.; Yen, H.-L.; Li, Y.; Ip, D.K.M.; Peiris, J.S.M.; et al. Respiratory Virus Shedding in Exhaled Breath and Efficacy of Face Masks. Nat Med 2020, 26, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, M. Protection of Our Future Generation: Use of Face Masks in Children amidst COVID-19 Era. JNMA J Nepal Med Assoc 2021, 59, 818–820. [Google Scholar] [CrossRef] [PubMed]
- Huppertz, H.-I.; Berner, R.; Schepker, R.; Kopp, M.; Oberle, A.; Fischbach, T.; Rodeck, B.; Knuf, M.; Keller, M.; Simon, A.; et al. [Use of masks by children to prevent infection with SARS-CoV-2]. Monatsschr Kinderheilkd 2021, 169, 52–56. [Google Scholar] [CrossRef]
- Lopes, H.; Middleton, J.; De Guchtenaere, A.; Hadjipanayis, A. COVID-19 and the Use of Masks by Children. Statement From the Association of Schools of Public Health in the European Region and the European Academy of Paediatrics. Front. Pediatr. 2021, 9. [Google Scholar] [CrossRef]
- Moschovis, P.P.; Yonker, L.M.; Shah, J.; Singh, D.; Demokritou, P.; Kinane, T.B. Aerosol Transmission of SARS-CoV-2 by Children and Adults during the COVID-19 Pandemic. Pediatr Pulmonol 2021, 56, 1389–1394. [Google Scholar] [CrossRef]
- Bagus, P.; Peña-Ramos, J.A.; Sánchez-Bayón, A. COVID-19 and the Political Economy of Mass Hysteria. International Journal of Environmental Research and Public Health 2021, 18, 1376. [Google Scholar] [CrossRef]
- Cabrera, J. Dangerous Pathogens Found on Local Residents’ Face Masks. Alachua Chronicle 2021.
- Kisielinski, K.; Wojtasik, B. Suitability of Rose Bengal Sodium Salt Staining for Visualisation of Face Mask Contamination by Living Organisms. AIMSES 2022, 9, 218–231. [Google Scholar] [CrossRef]
- Kisielinski, K.; Wojtasik, B.; Zalewska, A.; Livermore, D.M.; Jurczak-Kurek, A. The Bacterial Burden of Worn Face Masks – Observational Research and Literature Review 2023.
- Amara, H.; Tadj, A.; Mahdad, Y.M.; Seddiki, S.M.L. Risques Infectieux de l’utilisation Répétée et Prolongée Des Masques Chirurgicaux Pendant La Covid-19: Surgical Masks and Covid-19. Utility. Genetics & Biodiversity Journal 2024, 8, 85–97. [Google Scholar]
- Checchi, V.; Montevecchi, M.; Valeriani, L.; Checchi, L. Bioburden Variation of Filtering Face Piece Respirators over Time: A Preliminary Study. Materials 2022, 15, 8790. [Google Scholar] [CrossRef] [PubMed]
- Chhakchhuak, Z.; Chhabra, M.C.; Panesar, S.; Duggal, N. Microbial Detection from Used Face Masks and Hygiene Practices. Journal of Communicable Diseases (E-ISSN: 2581-351X & P-ISSN: 0019-5138) 2023, 55, 111–118. [Google Scholar]
- Delanghe, L.; Cauwenberghs, E.; Spacova, I.; De Boeck, I.; Van Beeck, W.; Pepermans, K.; Claes, I.; Vandenheuvel, D.; Verhoeven, V.; Lebeer, S. Cotton and Surgical Face Masks in Community Settings: Bacterial Contamination and Face Mask Hygiene. Front Med (Lausanne) 2021, 8, 732047. [Google Scholar] [CrossRef] [PubMed]
- Gund, M.P.; Naim, J.; Hannig, M.; Halfmann, A.; Gärtner, B.; Boros, G.; Rupf, S. CHX and a Face Shield Cannot Prevent Contamination of Surgical Masks. Front Med (Lausanne) 2022, 9, 896308. [Google Scholar] [CrossRef]
- Keri, V.C.; Kumar, A.; Singh, G.; Mandal, A.; Ali, H.; Ranjan, P.; Wig, N. Pilot Study on Burden of Fungal Contamination in Face Masks: Need for Better Mask Hygiene in the COVID-19 Era. Infez Med 2021, 29, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Chang, Y.; Chu, W.; Yan, M.; Mao, Y.; Zhu, Z.; Wu, H.; Jie, Z.; Dai, K.; Li, H.; et al. Surgical Masks as Source of Bacterial Contamination during Operative Procedures. Journal of Orthopaedic Translation 2018, 14, 57–62. [Google Scholar] [CrossRef]
- Luksamijarulkul, P.; Aiempradit, N.; Vatanasomboon, P. Microbial Contamination on Used Surgical Masks among Hospital Personnel and Microbial Air Quality in Their Working Wards: A Hospital in Bangkok. Oman Med J 2014, 29, 346–350. [Google Scholar] [CrossRef]
- Merad, Y.; Belmokhtar, Z.; Hadjazi, O.; Belkacemi, M.; Matmour, D.; Merad, Z.; Bassaid, A.; Megherbi, O. Fungal Contamination of Medical Masks among Forensic Healthcare Workers in the COVID19 Era. New Microbes and New Infections 2023, 53, 101134. [Google Scholar] [CrossRef]
- Monalisa, D. Microbial Contamination of the Mouth Masks Used By Post- Graduate Students in a Private Dental Institution: An In-Vitro Study. 2017, 7.
- Nightingale, M.; Mody, M.; Rickard, A.H.; Cassone, M. Bacterial Contamination on Used Face Masks among Nursing Home Healthcare Personnel. Antimicrob Steward Healthc Epidemiol 2023, 3, e54. [Google Scholar] [CrossRef]
- Park, A.-M.; Khadka, S.; Sato, F.; Omura, S.; Fujita, M.; Hashiwaki, K.; Tsunoda, I. Bacterial and Fungal Isolation from Face Masks under the COVID-19 Pandemic. Sci Rep 2022, 12, 11361. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, R.; Garg, K.; Singh, G.; Mehrotra, V. Is Safeguard Compromised? Surgical Mouth Mask Harboring Hazardous Microorganisms in Dental Practice. J Family Med Prim Care 2020, 9, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Li, H.; Shen, S.; Zhang, G.; Huang, R.; Feng, Y.; Yang, J.; Ma, S. Study of the Micro-Climate and Bacterial Distribution in the Deadspace of N95 Filtering Face Respirators. Sci Rep 2018, 8, 17382. [Google Scholar] [CrossRef] [PubMed]
- Yousefimashouf, M.; Yousefimashouf, R.; Alikhani, M.S.; Hashemi, H.; Karami, P.; Rahimi, Z.; Hosseini, S.M. Evaluation of the Bacterial Contamination of Face Masks Worn by Personnel in a Center of COVID 19 Hospitalized Patients: A Cross-Sectional Study. New Microbes New Infect 2023, 52, 101090. [Google Scholar] [CrossRef]
- VDI 6022. Available online: https://www.vdi.de/richtlinien/unsere-richtlinien-highlights/vdi-6022 (accessed on 14 October 2023).
- Gund, M.P.; Boros, G.; Hannig, M.; Thieme-Ruffing, S.; Gärtner, B.; Rohrer, T.R.; Simon, A.; Rupf, S. Bacterial Contamination of Forehead Skin and Surgical Mask in Aerosol-Producing Dental Treatment. J Oral Microbiol 2021, 13, 1978731. [Google Scholar] [CrossRef]
- Lee, Y.-H.; Kim, H.; Heo, D.W.; Ahn, I.-S.; Park, H.-K. Oral Microbiome of the Inner Surface of Face Masks and Whole Saliva during the COVID-19 Pandemic. Frontiers in Oral Health 2023, 4. [Google Scholar] [CrossRef]
- Szostak-Kotowa, J. Biodeterioration of Textiles. International Biodeterioration & Biodegradation 2004, 53, 165–170. [Google Scholar] [CrossRef]
- Szunerits, S.; Dӧrfler, H.; Pagneux, Q.; Daniel, J.; Wadekar, S.; Woitrain, E.; Ladage, D.; Montaigne, D.; Boukherroub, R. Exhaled Breath Condensate as Bioanalyte: From Collection Considerations to Biomarker Sensing. Anal Bioanal Chem 2023, 415, 27–34. [Google Scholar] [CrossRef]
- Xiang, G.; Xu, K.; Jian, Y.; He, L.; Shen, Z.; Li, M.; Liu, Q. Prolonged Mask Wearing Changed Nasal Microbial Characterization of Young Adults during the COVID-19 Pandemic in Shanghai, China. Frontiers in Immunology 2023, 14. [Google Scholar] [CrossRef]
- Ahmad, E.F.E.M.; Mohammed, M.; Al Rayes, A.A.; Al Qahtani, A.; Elzubier, A.G.; Suliman, F.A.E. The Effect of Wearing the Veil by Saudi Ladies on the Occurrence of Respiratory Diseases. Journal of Asthma 2001, 38, 423–426. [Google Scholar] [CrossRef]
- Fögen, Z. The Foegen Effect: A Mechanism by Which Facemasks Contribute to the COVID-19 Case Fatality Rate. Medicine (Baltimore) 2022, 101, e28924. [Google Scholar] [CrossRef] [PubMed]
- Burgos-Blasco, B.; Arriola-Villalobos, P.; Fernandez-Vigo, J.I.; Oribio-Quinto, C.; Ariño-Gutierrez, M.; Diaz-Valle, D.; Benitez-del-Castillo, J.M. Face Mask Use and Effects on the Ocular Surface Health: A Comprehensive Review. The Ocular Surface 2023, 27, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Drewnick, F.; Pikmann, J.; Fachinger, F.; Moormann, L.; Sprang, F.; Borrmann, S. Aerosol Filtration Efficiency of Household Materials for Homemade Face Masks: Influence of Material Properties, Particle Size, Particle Electrical Charge, Face Velocity, and Leaks. Aerosol Science and Technology 2021, 55, 63–79. [Google Scholar] [CrossRef]
- D’Souza, S.; Vaidya, T.; Nair, A.P.; Shetty, R.; Kumar, N.R.; Bisht, A.; Panigrahi, T.; J, T.S.; Khamar, P.; Dickman, M.M.; et al. Altered Ocular Surface Health Status and Tear Film Immune Profile Due to Prolonged Daily Mask Wear in Health Care Workers. Biomedicines 2022, 10, 1160. [Google Scholar] [CrossRef]
- Huber, C. Masks, False Safety and Real Dangers, Part 4: Proposed Mechanisms by Which Masks Increase Risk of COVID-19. Primary Doctor Medical Journal 2020, 1–9. [Google Scholar]
- Mastropasqua, L.; Lanzini, M.; Brescia, L.; D’Aloisio, R.; Nubile, M.; Ciancaglini, M.; D’Amario, C.; Agnifili, L.; Mastropasqua, R. Face Mask-Related Ocular Surface Modifications During COVID-19 Pandemic: A Clinical, In Vivo Confocal Microscopy, and Immune-Cytology Study. Translational Vision Science & Technology 2021, 10, 22. [Google Scholar] [CrossRef]
- Schultheis, W.G.; Sharpe, J.E.; Zhang, Q.; Patel, S.N.; Kuriyan, A.E.; Chiang, A.; Garg, S.J.; Hsu, J. Effect of Taping Face Masks on Quantitative Particle Counts Near the Eye: Implications for Intravitreal Injections in the COVID-19 Era. American Journal of Ophthalmology 2021, 225, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Shah, Y.; Kurelek, J.W.; Peterson, S.D.; Yarusevych, S. Experimental Investigation of Indoor Aerosol Dispersion and Accumulation in the Context of COVID-19: Effects of Masks and Ventilation. Physics of Fluids 2021, 33, 073315. [Google Scholar] [CrossRef]
- Viola, I.M.; Peterson, B.; Pisetta, G.; Pavar, G.; Akhtar, H.; Menoloascina, F.; Mangano, E.; Dunn, K.E.; Gabl, R.; Nila, A.; et al. Face Coverings, Aerosol Dispersion and Mitigation of Virus Transmission Risk. IEEE Open J Eng Med Biol 2021, 2, 26–35. [Google Scholar] [CrossRef]
- Akioud, W.; Sebbata, S.; Mozarie, Y.; Oubaaz, A. Chalazion and Face Mask Wear during COVID-19 Pandemic: Is There A Link? European Journal of Medical and Health Sciences 2023, 5, 17–19. [Google Scholar] [CrossRef]
- Hadayer, A.; Zahavi, A.; Livny, E.; Gal-Or, O.; Gershoni, A.; Mimouni, K.; Ehrlich, R. PATIENTS WEARING FACE MASKS DURING INTRAVITREAL INJECTIONS MAY BE AT A HIGHER RISK OF ENDOPHTHALMITIS. Retina 2020, 40, 1651–1656. [Google Scholar] [CrossRef] [PubMed]
- Molero-Senosiain, M.; Tiew, S.; Patel, A.; Houben, I.; Dhillon, N. Impact of Face Mask Wear on Bacterial Keratitis. Journal Français d’Ophtalmologie 2023, 46, e37–e39. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, T.; Terasaki, H.; Yamashita, T.; Shiihara, H.; Funatsu, R.; Uemura, A. Increased Incidence of Endophthalmitis after Vitrectomy Relative to Face Mask Wearing during COVID-19 Pandemic. British Journal of Ophthalmology 2023, 107, 1472–1477. [Google Scholar] [CrossRef] [PubMed]
- Silkiss, R.Z.; Paap, M.K.; Ugradar, S. Increased Incidence of Chalazion Associated with Face Mask Wear during the COVID-19 Pandemic. Am J Ophthalmol Case Rep 2021, 22, 101032. [Google Scholar] [CrossRef]
- Brooks, J.K.; Sultan, A.S.; Jabra-Rizk, M.A. Prolonged Facial Mask Wear Is a Concern for the Development of Dysbiotic Microbiome. Respiratory Medicine and Research 2022, 81, 100877. [Google Scholar] [CrossRef]
- Sakr, A.; Brégeon, F.; Mège, J.-L.; Rolain, J.-M.; Blin, O. Staphylococcus Aureus Nasal Colonization: An Update on Mechanisms, Epidemiology, Risk Factors, and Subsequent Infections. Frontiers in Microbiology 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Asadi, S.; Cappa, C.D.; Barreda, S.; Wexler, A.S.; Bouvier, N.M.; Ristenpart, W.D. Efficacy of Masks and Face Coverings in Controlling Outward Aerosol Particle Emission from Expiratory Activities. Scientific Reports 2020, 10, 15665. [Google Scholar] [CrossRef]
- Bagchi, S.; Basu, S.; Chaudhuri, S.; Saha, A. Penetration and Secondary Atomization of Droplets Impacted on Wet Facemasks. Phys. Rev. Fluids 2021, 6, 110510. [Google Scholar] [CrossRef]
- Kasloff, S.B.; Leung, A.; Strong, J.E.; Funk, D.; Cutts, T. Stability of SARS-CoV-2 on Critical Personal Protective Equipment. Sci Rep 2021, 11, 984. [Google Scholar] [CrossRef]
- Córdoba-Lanús, E.; García-Pérez, O.; Cazorla-Rivero, S.; Rodríguez-Esparragón, F.; Piñero, J.-E.; Clavo, B.; Lorenzo-Morales, J. Persistence of SARS-CoV-2 Infection on Personal Protective Equipment (PPE). BMC Infect Dis 2021, 21, 1169. [Google Scholar] [CrossRef]
- Directorate-General for Health and Consumers (European Commission) Now known as Making Risk Assessment More Relevant for Risk Management; Publications Office of the European Union: LU, 2013; ISBN 978-92-79-31205-2.
- World Health Organization; Fund (UNICEF), U. N.C. WHO - Advice on the Use of Masks for Children in the Community in the Context of COVID-19: Annex to the Advice on the Use of Masks in the Context of COVID-19, 21 August 2020.
- WMA - The World Medical Association-WMA Declaration of Geneva 2018.
- Goldsmith, D.J.A.; Orlowski, E.J.W. Don’t Forget About the Children - A Narrative Review of How COVID-19 Pandemic Policy in the UK and Sweden Impacted Children’s Wellbeing. Medical Research Archives 2023, 11. [Google Scholar] [CrossRef]
- Shobako, N. Lessons from the Health Policies for Children during the Pandemic in Japan. Frontiers in Public Health 2022, 10. [Google Scholar] [CrossRef] [PubMed]
- Sezer, H.; Çınar, D.; Kılıç Akça, N. The Effect of Prolonged Use of Surgical Masks during Face-to-Face Teaching on Cognitive and Physiological Parameters of Nursing Students: A Cross-Sectional and Descriptive Study. Nurse Education in Practice 2023, 72, 103779. [Google Scholar] [CrossRef] [PubMed]
- Krishnaratne, S.; Pfadenhauer, L.M.; Coenen, M.; Geffert, K.; Jung-Sievers, C.; Klinger, C.; Kratzer, S.; Littlecott, H.; Movsisyan, A.; Rabe, J.E.; et al. Measures Implemented in the School Setting to Contain the COVID-19 Pandemic: A Rapid Scoping Review - Krishnaratne, S - 2020 | Cochrane Library.
- Cao, S.; Gan, Y.; Wang, C.; Bachmann, M.; Wei, S.; Gong, J.; Huang, Y.; Wang, T.; Li, L.; Lu, K.; et al. Post-Lockdown SARS-CoV-2 Nucleic Acid Screening in Nearly Ten Million Residents of Wuhan, China. Nat Commun 2020, 11, 5917. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.E.; Li, Z.; Chiew, C.J.; Yong, S.E.; Toh, M.P.; Lee, V.J. Presymptomatic Transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. MMWR Morb Mortal Wkly Rep 2020, 69, 411–415. [Google Scholar] [CrossRef]
- Elgersma, I.H.; Fretheim, A.; Elstrøm, P.; Aavitsland, P. Association between Face Mask Use and Risk of SARS-CoV-2 Infection: Cross-Sectional Study. Epidemiol Infect 2023, 151, e194. [Google Scholar] [CrossRef]
- Spira, B. Correlation Between Mask Compliance and COVID-19 Outcomes in Europe. Cureus 2022, 14, e24268. [Google Scholar] [CrossRef]
- Cheng, Y.; Ma, N.; Witt, C.; Rapp, S.; Wild, P.S.; Andreae, M.O.; Pöschl, U.; Su, H. Face Masks Effectively Limit the Probability of SARS-CoV-2 Transmission. Science 2021, 372, 1439–1443. [Google Scholar] [CrossRef]
- Leech, G.; Rogers-Smith, C.; Monrad, J.T.; Sandbrink, J.B.; Snodin, B.; Zinkov, R.; Rader, B.; Brownstein, J.S.; Gal, Y.; Bhatt, S.; et al. Mask Wearing in Community Settings Reduces SARS-CoV-2 Transmission. Proc Natl Acad Sci U S A 2022, 119, e2119266119. [Google Scholar] [CrossRef]
- Ueki, H.; Furusawa, Y.; Iwatsuki-Horimoto, K.; Imai, M.; Kabata, H.; Nishimura, H.; Kawaoka, Y. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere 2020, 5. [Google Scholar] [CrossRef]
- Knobloch, J.K.; Franke, G.; Knobloch, M.J.; Knobling, B.; Kampf, G. Overview of Tight Fit and Infection Prevention Benefits of Respirators (Filtering Face Pieces). Journal of Hospital Infection 2023, 134, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Gralton, J.; McLaws, M.-L. Protecting Healthcare Workers from Pandemic Influenza: N95 or Surgical Masks? Crit Care Med 2010, 38, 657–667. [Google Scholar] [CrossRef]
- Kappstein, I. Mund-Nasen-Schutz in der Öffentlichkeit: Keine Hinweise für eine Wirksamkeit. Krankenhaushygiene up2date 2020, 15, 279–295. [Google Scholar] [CrossRef]
- Mickells, G.E.; Figueroa, J.; West, K.W.; Wood, A.; McElhanon, B.O. Adherence to Masking Requirement During the COVID-19 Pandemic by Early Elementary School Children. J Sch Health 2021, 91, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Xiang Ong, S.W.; Tang, Y.W.; Linn, K.Z.; Huan, X.W.; Lim, A.; Poon, C.Y.; Ru Tan, D.H.; Binte Hamed, N.H.; Syed Husen, S.F.B.; Hui Ong, C.C.; et al. Compliance with Face Mask Use during the COVID-19 Pandemic: A Community Observational Study in Singapore. Singapore Med J 2023. [Google Scholar] [CrossRef]
- Luckman, A.; Zeitoun, H.; Isoni, A.; Loomes, G.; Vlaev, I.; Powdthavee, N.; Read, D. Risk Compensation during COVID-19: The Impact of Face Mask Usage on Social Distancing; OSF Preprints, 2020. [Google Scholar]
- Szczesniak, D.; Ciulkowicz, M.; Maciaszek, J.; Misiak, B.; Luc, D.; Wieczorek, T.; Witecka, K.-F.; Rymaszewska, J. Psychopathological Responses and Face Mask Restrictions during the COVID-19 Outbreak: Results from a Nationwide Survey. Brain Behav Immun 2020, 87, 161–162. [Google Scholar] [CrossRef] [PubMed]
- Sharma, I.; Vashnav, M.; Sharma, R. COVID-19 Pandemic Hype: Losers and Gainers. Indian Journal of Psychiatry 2020, 62, 420. [Google Scholar] [CrossRef]
- Lee, S.-A.; Grinshpun, S.A.; Reponen, T. Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation with NaCl Aerosol Representing Bacterial and Viral Particle Size Range. Ann Occup Hyg 2008, 52, 177–185. [Google Scholar] [CrossRef]
- Barari, K.; Si, X.; Xi, J. Impacts of Mask Wearing and Leakages on Cyclic Respiratory Flows and Facial Thermoregulation. Fluids 2024, 9, 9. [Google Scholar] [CrossRef]
- Jia, Z.; Ai, Z.; Cao, S.; Bekö, G. Effectiveness of Respiratory Protective Equipment on Source Control of Exhaled Pollutants. Journal of Building Engineering 2024, 86, 108742. [Google Scholar] [CrossRef]
- Zhu, Y.; Xia, Y.; Pickering, J.; Bowen, A.C.; Short, K.R. The Role of Children in Transmission of SARS-CoV-2 Variants of Concern within Households: An Updated Systematic Review and Meta-Analysis, as at 30 June 2022. Euro Surveill 2023, 28, 2200624. [Google Scholar] [CrossRef] [PubMed]
- Felsenstein, S.; Hedrich, C.M. SARS-CoV-2 Infections in Children and Young People. Clin Immunol 2020, 220, 108588. [Google Scholar] [CrossRef]
- Pezzullo, A.M.; Axfors, C.; Contopoulos-Ioannidis, D.G.; Apostolatos, A.; Ioannidis, J.P.A. Age-Stratified Infection Fatality Rate of COVID-19 in the Non-Elderly Population. Environ Res 2023, 216, 114655. [Google Scholar] [CrossRef] [PubMed]
- Fikenzer, S.; Uhe, T.; Lavall, D.; Rudolph, U.; Falz, R.; Busse, M.; Hepp, P.; Laufs, U. Effects of Surgical and FFP2/N95 Face Masks on Cardiopulmonary Exercise Capacity. Clin Res Cardiol 2020, 1–9. [Google Scholar] [CrossRef]
- Lee, H.P.; Wang, D.Y. Objective Assessment of Increase in Breathing Resistance of N95 Respirators on Human Subjects. Ann Occup Hyg 2011, 55, 917–921. [Google Scholar] [CrossRef]
- Li, Y.; Tokura, H.; Guo, Y.P.; Wong, A.S.W.; Wong, T.; Chung, J.; Newton, E. Effects of Wearing N95 and Surgical Facemasks on Heart Rate, Thermal Stress and Subjective Sensations. Int Arch Occup Environ Health 2005, 78, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Mapelli, M.; Salvioni, E.; Martino, F.D.; Mattavelli, I.; Gugliandolo, P.; Vignati, C.; Farina, S.; Palermo, P.; Campodonico, J.; Maragna, R.; et al. “You Can Leave Your Mask on”: Effects on Cardiopulmonary Parameters of Different Airway Protection Masks at Rest and during Maximal Exercise. European Respiratory Journal 2021. [Google Scholar] [CrossRef]
- Roberge, R.J.; Bayer, E.; Powell, J.B.; Coca, A.; Roberge, M.R.; Benson, S.M. Effect of Exhaled Moisture on Breathing Resistance of N95 Filtering Facepiece Respirators. Ann Occup Hyg 2010, 54, 671–677. [Google Scholar] [CrossRef]
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological Impact of the N95 Filtering Facepiece Respirator on Healthcare Workers. Respir Care 2010, 55, 569–577. [Google Scholar]
- Roberge, R.; Benson, S.; Kim, J.-H. Thermal Burden of N95 Filtering Facepiece Respirators. Ann Occup Hyg 2012, 56, 808–814. [Google Scholar] [CrossRef]
- Roberge, R.J.; Kim, J.-H.; Benson, S.M. Absence of Consequential Changes in Physiological, Thermal and Subjective Responses from Wearing a Surgical Mask. Respiratory Physiology & Neurobiology 2012, 181, 29–35. [Google Scholar] [CrossRef]
- de Yzaguirre i Maura, I.; Zabala, D.D.; Brotons i Cuixart, D.; Gutierrez Rincon, J.A.; Vives i Turcó, J.; Grazioli, G. Physiological Impact of Different Types of Mask at Rest. Apunts Sports Medicine 2022, 57, 100389. [Google Scholar] [CrossRef]
- Elbl, C.; Brunner, J.X.; Schier, D.; Junge, A.; Junge, H. Protective Face Masks Add Significant Dead Space. European Respiratory Journal 2021, 58. [Google Scholar] [CrossRef] [PubMed]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to Training in the COVID-19 Era: The Physiological Effects of Face Masks during Exercise. Scandinavian Journal of Medicine & Science in Sports 2020, n/a. [Google Scholar] [CrossRef]
- Johnson, A.T.; Scott, W.H.; Lausted, C.G.; Coyne, K.M.; Sahota, M.S.; Johnson, M.M. Effect of External Dead Volume on Performance While Wearing a Respirator. AIHAJ - American Industrial Hygiene Association 2000, 61, 678–684. [Google Scholar] [CrossRef]
- Ngo, H.; Spaeth, J.; Schumann, S. Effective Volume of Rebreathed Air during Breathing with Facepieces Increases with Protection Class and Decreases with Ambient Airflow. PLOS ONE 2024, 19, e0299919. [Google Scholar] [CrossRef]
- Roberge, R.J.; Kim, J.-H.; Powell, J.B. N95 Respirator Use during Advanced Pregnancy. Am J Infect Control 2014, 42, 1097–1100. [Google Scholar] [CrossRef]
- Shui, L.; Yang, B.; Tang, H.; Luo, Y.; Hu, S.; Zhong, X.; Duan, J. Physiological Effects of Surgical and N95 Masks During Exercise in the COVID-19 Era. The American Journal of the Medical Sciences 2022, 363, 411–419. [Google Scholar] [CrossRef]
- Xu, M.; Lei, Z.; Yang, J. Estimating the Dead Space Volume Between a Headform and N95 Filtering Facepiece Respirator Using Microsoft Kinect. Journal of Occupational and Environmental Hygiene 2015, 12, 538–546. [Google Scholar] [CrossRef]
- Butz, U. Rückatmung von Kohlendioxid bei Verwendung von Operationsmasken als hygienischer Mundschutz an medizinischem Fachpersonal, Universitätsbibliothek der Technischen Universität München, 2005.
- Laferty, E.A.; McKay, R.T. Physiologic Effects and Measurement of Carbon Dioxide and Oxygen Levels during Qualitative Respirator Fit Testing. J. Chem. Health Saf. 2006, 13, 22–28. [Google Scholar] [CrossRef]
- Pifarré, F.; Zabala, D.D.; Grazioli, G.; de Yzaguirre i Maura, I. COVID 19 and Mask in Sports. Apunts Sports Medicine 2020. [Google Scholar] [CrossRef]
- Rhee, M.S.M.; Lindquist, C.D.; Silvestrini, M.T.; Chan, A.C.; Ong, J.J.Y.; Sharma, V.K. Carbon Dioxide Increases with Face Masks but Remains below Short-Term NIOSH Limits. BMC Infect Dis 2021, 21, 354. [Google Scholar] [CrossRef] [PubMed]
- Salati, H.; Khamooshi, M.; Vahaji, S.; Christo, F.C.; Fletcher, D.F.; Inthavong, K. N95 Respirator Mask Breathing Leads to Excessive Carbon Dioxide Inhalation and Reduced Heat Transfer in a Human Nasal Cavity. Phys Fluids (1994) 2021, 33, 081913. [Google Scholar] [CrossRef] [PubMed]
- Sinkule, E.J.; Powell, J.B.; Goss, F.L. Evaluation of N95 Respirator Use with a Surgical Mask Cover: Effects on Breathing Resistance and Inhaled Carbon Dioxide. Ann Occup Hyg 2013, 57, 384–398. [Google Scholar] [CrossRef]
- Zhang, X.; Li, H.; Shen, S.; Cai, M. Investigation of the Flow-Field in the Upper Respiratory System When Wearing N95 Filtering Facepiece Respirator. J Occup Environ Hyg 2016, 13, 372–382. [Google Scholar] [CrossRef]
- Zhang, G.; Li, M.; Zheng, M.; Cai, X.; Yang, J.; Zhang, S.; Yilifate, A.; Zheng, Y.; Lin, Q.; Liang, J.; et al. Effect of Surgical Masks on Cardiopulmonary Function in Healthy Young Subjects: A Crossover Study. Front Physiol 2021, 12, 710573. [Google Scholar] [CrossRef]
- Akhondi, H.; Kaveh, S.; Kaufman, K.; Danai, T.; Ayutyanont, N. CO2 Levels Behind and in Front of Different Protective Mask Types. HCA Healthcare Journal of Medicine 2022, 3. [Google Scholar] [CrossRef]
- Balkir, B.; Lankar, V.; Hangun, Y. Comparison of Face Masks by Arduino Sensors. Cornell Undergraduate Research Journal 2023, 2, 63–73. [Google Scholar] [CrossRef]
- Bar-On, O.; Goldberg, O.; Stafler, P.; Levine, H.; Jacobi, E.; Shmueli, E.; Rothschild, B.; Prais, D.; Mei-Zahav, M. Wearing Face Masks While Climbing Stairs Influences Respiratory Physiology. J. Breath Res. 2024. [Google Scholar] [CrossRef]
- Bharatendu, C.; Ong, J.J.Y.; Goh, Y.; Tan, B.Y.Q.; Chan, A.C.Y.; Tang, J.Z.Y.; Leow, A.S.; Chin, A.; Sooi, K.W.X.; Tan, Y.L.; et al. Powered Air Purifying Respirator (PAPR) Restores the N95 Face Mask Induced Cerebral Hemodynamic Alterations among Healthcare Workers during COVID-19 Outbreak. J Neurol Sci 2020, 417, 117078. [Google Scholar] [CrossRef]
- Decha, C.; Sonthaya, S. A Long-Term Effects of Wearing a Reusable Mask While Running Exercises on Blood Gas Levels in Adults. Journal of Physical Education and Sport 2023, 255–263. [Google Scholar]
- Dirol, H.; Alkan, E.; Sindel, M.; Ozdemir, T.; Erbas, D. The Physiological and Disturbing Effects of Surgical Face Masks in the COVID-19 Era. BLL 2021, 122, 821–825. [Google Scholar] [CrossRef]
- Engeroff, T.; Heinsel, K.; Niederer, D.; Nienhaus, A.; Groneberg, D.A.; Vogt, L. Investigating Effects of FFP2 Wearing during Physical Activity on Gas Exchange, Metabolism and Affective State Using a Randomized Controlled Trial. Sci Rep 2024, 14, 6278. [Google Scholar] [CrossRef] [PubMed]
- Fantin, R. The Effect of Wearing an FFP3 Mask (3M TM Aura TM ) with an Exhalation Valve on Gas Exchange in Medical Staff. Int J Occup Med Environ Health 2021. [Google Scholar] [CrossRef] [PubMed]
- Georgi, C.; Haase-Fielitz, A.; Meretz, D.; Gäsert, L.; Butter, C. The Impact of Commonly-Worn Face Masks on Physiological Parameters and on Discomfort During Standard Work-Related Physical Effort. Dtsch Arztebl Int 2020, 117, 674–675. [Google Scholar] [CrossRef]
- Kim, J.-H.; Benson, S.M.; Roberge, R.J. Pulmonary and Heart Rate Responses to Wearing N95 Filtering Facepiece Respirators. Am J Infect Control 2013, 41, 24–27. [Google Scholar] [CrossRef]
- Kim, J.-H.; Roberge, R.J.; Powell, J.B. Effect of External Airflow Resistive Load on Postural and Exercise-Associated Cardiovascular and Pulmonary Responses in Pregnancy: A Case Control Study. BMC Pregnancy and Childbirth 2015, 15, 45. [Google Scholar] [CrossRef]
- Marek, E.-M.; van Kampen, V.; Jettkant, B.; Kendzia, B.; Strauß, B.; Sucker, K.; Ulbrich, M.; Deckert, A.; Berresheim, H.; Eisenhawer, C.; et al. Effects of Wearing Different Face Masks on Cardiopulmonary Performance at Rest and Exercise in a Partially Double-Blinded Randomized Cross-over Study. Sci Rep 2023, 13, 6950. [Google Scholar] [CrossRef]
- Mo, Y. Risk and Impact of Using Mask on COPD Patients with Acute Exacerbation during the COVID-19 Outbreak: A Retrospective Study. 2020. [CrossRef]
- Patel, S.; Mohapatra, E.; Suganthy, A.K.; Shah, S.; Abraham, J.; Nanda, R.; Behera, A.K.; Gupta, A. A Pilot Study to Evaluate the Changes in Venous Blood Gas Parameters and Hypoxia Biomarkers in Health Care Workers Using Different Kinds of Masks. Lung India 2023, 40, 134–142. [Google Scholar] [CrossRef]
- Shechtman, L.; Ben-Haim, G.; Ben-Zvi, I.; Steel, L.; Ironi, A.; Huszti, E.; Chatterji, S.; Levy, L. Physiological Effects of Wearing N95 Respirator on Medical Staff During Prolong Work Hours in Covid-19 Departments. J Occup Environ Med 2022, 64, e378–e380. [Google Scholar] [CrossRef]
- Sofonova, D.; Angelova, R. Sofronov Measuring the Carbon Dioxide Concentration under Protective Face Masks with a Sensor System. Applied Ecology and environmental research 2023, 21(4), 2775–2792. [Google Scholar] [CrossRef]
- Tong, P.S.Y.; Kale, A.S.; Ng, K.; Loke, A.P.; Choolani, M.A.; Lim, C.L.; Chan, Y.H.; Chong, Y.S.; Tambyah, P.A.; Yong, E.-L. Respiratory Consequences of N95-Type Mask Usage in Pregnant Healthcare Workers—a Controlled Clinical Study. Antimicrobial Resistance & Infection Control 2015, 4, 48. [Google Scholar] [CrossRef]
- Vogt, G.; Radtke, K.; Jagim, A.; Peckumn, D.; Lee, T.; Mikat, R.; Foster, C. Effect of Face Masks on Physiological and Perceptual Responses during 30 Minutes of Self-Paced Exercise in Older Community Dwelling Adults. International Journal of Environmental Research and Public Health 2022, 19, 12877. [Google Scholar] [CrossRef] [PubMed]
- Wangsan, K.; Sapbamrer, R.; Sirikul, W.; Panumasvivat, J.; Surawattanasakul, V.; Assavanopakun, P. Effect of N95 Respirator on Oxygen and Carbon Dioxide Physiologic Response: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health 2022, 19, 8646. [Google Scholar] [CrossRef] [PubMed]
- Kiray, M.; Sisman, A.R.; Camsari, U.M.; Evren, M.; Dayi, A.; Baykara, B.; Aksu, I.; Ates, M.; Uysal, N. Effects of Carbon Dioxide Exposure on Early Brain Development in Rats. Biotechnic & Histochemistry 2014, 89, 371–383. [Google Scholar] [CrossRef]
- Uysal, N.; Kiray, M.; Sisman, A.R.; Baykara, B.; Aksu, I.; Dayi, A.; Gencoglu, C.; Evren, M.; Buyuk, E.; Cetin, F.; et al. Effects of Exercise and Poor Indoor Air Quality on Learning, Memory and Blood IGF-1 in Adolescent Mice. Biotechnic & Histochemistry 2014, 89, 126–135. [Google Scholar] [CrossRef]
- Vandemark, N.L.; Schanbacher, B.D.; Gomes, W.R. Alterations in Testes of Rats Exposed to Elevated Atmospheric Carbon Dioxide. J Reprod Fertil 1972, 28, 457–459. [Google Scholar] [CrossRef]
- Evaluation of the Health Aspects of Carbon Dioxide as a Food Ingredient; Federation of American Societies for Experimental Biology, Bethesda, MD. Life Sciences Research Office.; Food and Drug Administration, Washington, DC. Bureau of Foods, 1979.
- Howard, W.R.; Wong, B.; Yeager, K.S.B.; Stump, D.G.; Edwards, T.; Arden James, R.; Goodwin, M.R.; Gargas, M.L. Submarine Exposure Guideline Recommendations for Carbon Dioxide Based on the Prenatal Developmental Effects of Exposure in Rats. Birth Defects Res 2019, 111, 26–33. [Google Scholar] [CrossRef]
- Howard, W.R.; Wong, B.; Okolica, M.; Bynum, K.S.; James, R.A. The Prenatal Development Effects of Carbon Dioxide (CO2) Exposure in Rats (Rattus Norvegicus):; Defense Technical Information Center: Fort Belvoir, VA, 2012. [Google Scholar]
- Casalino-Matsuda, S.M.; Wang, N.; Ruhoff, P.T.; Matsuda, H.; Nlend, M.C.; Nair, A.; Szleifer, I.; Beitel, G.J.; Sznajder, J.I.; Sporn, P.H.S. Hypercapnia Alters Expression of Immune Response, Nucleosome Assembly and Lipid Metabolism Genes in Differentiated Human Bronchial Epithelial Cells. Sci Rep 2018, 8, 13508. [Google Scholar] [CrossRef]
- Sikter, A.; Faludi, G.; Rihmer, Z. The Role of Carbon Dioxide (and Intracellular pH) in the Pathomechanism of Several Mental Disorders. Are the Diseases of Civilization Caused by Learnt Behaviour, Not the Stress Itself? Neuropsychopharmacol Hung 2009, 11, 161–173. [Google Scholar]
- Hoffman, W.E.; Charbel, F.T.; Edelman, G.; Ausman, J.I. Brain Tissue Acid-Base Response to Hypercapnia in Neurosurgical Patients. Neurol Res 1995, 17, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Huo, X.; Min, J.; Pan, C.; Zhao, C.; Pan, L.; Gui, F.; Jin, L.; Wang, X. Efficacy of Lovastatin on Learning and Memory Deficits Caused by Chronic Intermittent Hypoxia-Hypercapnia: Through Regulation of NR2B-Containing NMDA Receptor-ERK Pathway. PLOS ONE 2014, 9, e94278. [Google Scholar] [CrossRef] [PubMed]
- Dodge, F.A.; Rahamimoff, R. Co-Operative Action a Calcium Ions in Transmitter Release at the Neuromuscular Junction. J Physiol 1967, 193, 419–432. [Google Scholar] [CrossRef]
- Tombaugh, G.C.; Somjen, G.G. Differential Sensitivity to Intracellular pH among High- and Low-Threshold Ca2+ Currents in Isolated Rat CA1 Neurons. J Neurophysiol 1997, 77, 639–653. [Google Scholar] [CrossRef]
- Hota, K.B.; Hota, S.K.; Chaurasia, O.P.; Singh, S.B. Acetyl-L-Carnitine-Mediated Neuroprotection during Hypoxia Is Attributed to ERK1/2-Nrf2-Regulated Mitochondrial Biosynthesis. Hippocampus 2012, 22, 723–736. [Google Scholar] [CrossRef]
- Benjamin Ezraty; Maïalène Chabalier; Adrien Ducret; Etienne Maisonneuve; Sam Dukan CO2 Exacerbates Oxygen Toxicity. EMBO reports 2011, 12, 321–326. [CrossRef]
- Guais, A.; Brand, G.; Jacquot, L.; Karrer, M.; Dukan, S.; Grévillot, G.; Molina, T.J.; Bonte, J.; Regnier, M.; Schwartz, L. Toxicity of Carbon Dioxide: A Review. Chem. Res. Toxicol. 2011, 24, 2061–2070. [Google Scholar] [CrossRef]
- Jacobson, T.A.; Kler, J.S.; Hernke, M.T.; Braun, R.K.; Meyer, K.C.; Funk, W.E. Direct Human Health Risks of Increased Atmospheric Carbon Dioxide. Nat Sustain 2019, 2, 691–701. [Google Scholar] [CrossRef]
- Thom, S.R.; Bhopale, V.M.; Hu, J.; Yang, M. Inflammatory Responses to Acute Elevations of Carbon Dioxide in Mice. Journal of Applied Physiology 2017, 123, 297–302. [Google Scholar] [CrossRef]
- Beheshti, A.; Cekanaviciute, E.; Smith, D.J.; Costes, S.V. Global Transcriptomic Analysis Suggests Carbon Dioxide as an Environmental Stressor in Spaceflight: A Systems Biology GeneLab Case Study. Sci Rep 2018, 8, 4191. [Google Scholar] [CrossRef]
- Zappulla, D. Environmental Stress, Erythrocyte Dysfunctions, Inflammation, and the Metabolic Syndrome: Adaptations to CO2 Increases? Journal of the CardioMetabolic Syndrome 2008, 3, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Bushinsky, D.A.; Krieger, N.S. Effects of Acid on Bone. Kidney Int 2022, 101, 1160–1170. [Google Scholar] [CrossRef]
- Adeva-Andany, M.M.; Carneiro-Freire, N.; Donapetry-García, C.; Rañal-Muíño, E.; López-Pereiro, Y. The Importance of the Ionic Product for Water to Understand the Physiology of the Acid-Base Balance in Humans. BioMed Research International 2014, 2014, e695281. [Google Scholar] [CrossRef]
- Adeva-Andany, M.M.; Fernández-Fernández, C.; Sánchez-Bello, R.; Donapetry-García, C.; Martínez-Rodríguez, J. The Role of Carbonic Anhydrase in the Pathogenesis of Vascular Calcification in Humans. Atherosclerosis 2015, 241, 183–191. [Google Scholar] [CrossRef]
- Tan, S.-I.; Han, Y.-L.; Yu, Y.-J.; Chiu, C.-Y.; Chang, Y.-K.; Ouyang, S.; Fan, K.-C.; Lo, K.-H.; Ng, I.-S. Efficient Carbon Dioxide Sequestration by Using Recombinant Carbonic Anhydrase. Process Biochemistry 2018, 73, 38–46. [Google Scholar] [CrossRef]
- Kim, I.G.; Jo, B.H.; Kang, D.G.; Kim, C.S.; Choi, Y.S.; Cha, H.J. Biomineralization-Based Conversion of Carbon Dioxide to Calcium Carbonate Using Recombinant Carbonic Anhydrase. Chemosphere 2012, 87, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, K.E.; Douglas, W.H.; Messier, A.A.; Shea, M.L.; Gohman, P.A. Effect of Prolonged Exposure to 0.5% CO2 on Kidney Calcification and Ultrastructure of Lungs. Undersea Biomed Res 1979, 6 Suppl, S155–S161. [Google Scholar]
- Abdel Mowla Ahmed Abdel Mowla, H.; Hashem, E.S. Physiological Burdens of Prolonged Use of Surgical Face Masks among Healthcare Workers During the COVID-19 Pandemic Era. Egyptian Journal of Nursing and Health Sciences 2022, 3, 236–257. [Google Scholar] [CrossRef]
- Alroudhan, I.E.; Ganji, K.K.; Hamza, M.O.; Munisekhar, M.S.; Sghaireen, M.G.; Alam, M.K. Effect of N95 Filtering Facepiece Respirators on Dental Health Professionals with an Emphasis on Pulmonary Function and Heart Rate: An Intrasubject Comparison. Br J Oral Maxillofac Surg 2021, 59, 1302–1307. [Google Scholar] [CrossRef]
- Bayoumi, A.; Shawki, M.; Abdulaziz, A.; Allam, M.; Mosleh, M. Blood Oxygen Level with Long-Term Use of N95 Face Mask in Dental Practice during the Coronavirus Pandemic “Covid-19. ” Advances in Medical, Pharmaceutical and Dental Research 2022, 2, 015–021. [Google Scholar] [CrossRef]
- Beder, A.; Büyükkoçak, U.; Sabuncuoğlu, H.; Keskil, Z.A.; Keskil, S. Preliminary Report on Surgical Mask Induced Deoxygenation during Major Surgery. Neurocirugia (Astur) 2008, 19, 121–126. [Google Scholar] [CrossRef]
- Cabanillas-Barea, S.; Rodríguez-Sanz, J.; Carrasco-Uribarren, A.; López-de-Celis, C.; González-Rueda, V.; Zegarra-Chávez, D.; Cedeño-Bermúdez, S.; Pérez-Bellmunt, A. Effects of Using the Surgical Mask and FFP2 during the 6-Min Walking Test. A Randomized Controlled Trial. Int J Environ Res Public Health 2021, 18, 12420. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.R.; Peña, S.; Misztal, C.; Iglesias, T.; Alejandro, M.; Dinh, C.T.; Holt, G.; Thomas, G.R. N95 vs Half-Face Respirator Wear in Surgical Trainees: Physiologic and Psychological Effects of Prolonged Use. OTO Open 2021, 5, 2473974X211065437. [Google Scholar] [CrossRef]
- Demirag, M.E.; Akyil, M.; Karasal, M.; Bayram, S.; Metin, S.K.; Tokgoz, F.A.; Baysungur, V.; Evman, S. Prospective Analysis of the Physiological Changes Caused by Prolonged Use of N95-Type Masks. Ann Thorac Med 2023, 18, 86–89. [Google Scholar] [CrossRef]
- Gaikwad, R.P.; Banodkar, A.B.; Nandgaonkar, V.P. Respiratory Consequences of N95 Mask during Covid-19 Pandemic- An Observational Study. International Journal of Health Sciences and Research 2021, 11, 55. [Google Scholar] [CrossRef]
- Hussain, S.A.; Mahmood, N.M.A.; Mahmood, T.M.A.; Salih, N.A.M.; Abdulrahman, Z.S. Adverse Effects Associated with the Use of N95 Mask among Health-Care Workers at the COVID-19 Care Units: A Cross-Sectional Study in Sulaimani City, Iraq. J Educ Health Promot 2022, 11, 198. [Google Scholar] [CrossRef] [PubMed]
- Kao, T.-W.; Huang, K.-C.; Huang, Y.-L.; Tsai, T.-J.; Hsieh, B.-S.; Wu, M.-S. The Physiological Impact of Wearing an N95 Mask during Hemodialysis as a Precaution against SARS in Patients with End-Stage Renal Disease. J Formos Med Assoc 2004, 103, 624–628. [Google Scholar]
- Kim, J.-H.; Wu, T.; Powell, J.B.; Roberge, R.J. Physiologic and Fit Factor Profiles of N95 and P100 Filtering Facepiece Respirators for Use in Hot, Humid Environments. Am J Infect Control 2016, 44, 194–198. [Google Scholar] [CrossRef]
- Kumar, P.; Nath, K.; Prasad, A.; Tiwari, L.K.; Chowdhry, B.K.; Sinha, A.K.; Chaudhary, N. Effects of the Use of N95 Masks on the Vital Signs of Healthy Healthcare Workers During the COVID-19 Pandemic: A Hospital-Based Cross-Sectional Study. Cureus 2023, 15, e40622. [Google Scholar] [CrossRef]
- Kurt, A.; Altındal, E.U. Choroidal Thickness Changes in Healthcare Professionals Wearing Surgical Masks or FFP2 Masks: Pilot Study. Photodiagnosis Photodyn Ther 2022, 37, 102608. [Google Scholar] [CrossRef]
- Manerkar, H.U.; Nagarsekar, A.; Gaunkar, R.B.; Dhupar, V.; Khorate, M. Assessment of Hypoxia and Physiological Stress Evinced by Usage of N95 Masks among Frontline Dental Healthcare Workers in a Humid Western Coastal Region of India-A Repeated Measure Observational Study. Indian J Occup Environ Med 2021, 25, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Porcari, J.P.; Probst, L.; Forrester, K.; Doberstein, S.; Foster, C.; Cress, M.L.; Schmidt, K. Effect of Wearing the Elevation Training Mask on Aerobic Capacity, Lung Function, and Hematological Variables. J Sports Sci Med 2016, 15, 379–386. [Google Scholar] [PubMed]
- Saccomanno, S.; Manenti, R.J.; Giancaspro, S.; Paskay, L.C.; Katzenmaier, C.S.; Mastrapasqua, R.F.; Quinzi, V. Evaluation of the Effects on SpO2 of N95 Mask (FFP2) on Dental Health Care Providers: A Cross-Sectional Observational Study. BMC Health Services Research 2022, 22, 248. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Inchingolo, F.; Rapone, B.; Festa, F.; Rexhep Tari, S.; Lorusso, F. Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. International Journal of Environmental Research and Public Health 2021, 18, 2363. [Google Scholar] [CrossRef] [PubMed]
- Sinha, D.; Bhandary, S.K.; Aroor, R.; Reddy, R.; Alva, S. Effect of N-95 Mask on Oxygen Saturation Level in Health Care Workers and Their Experience While Using N-95 Mask. Journal of Health and Allied Sciences NU 2022, 12, 274–276. [Google Scholar] [CrossRef]
- Toprak, E.; Bulut, A.N. The Effect of Mask Use on Maternal Oxygen Saturation in Term Pregnancies during the COVID-19 Process. Journal of Perinatal Medicine 2021, 49, 148–152. [Google Scholar] [CrossRef]
- Wojtasz, I.; Jaracz, K.; Sobczyński, P.; Drużdż, A.; Dyk, D.; Kaźmierski, R. The Impact of FFP3 Respirators on the Blood Saturation. Sci Rep 2022, 12, 1335. [Google Scholar] [CrossRef]
- Wulandari, S.M.; Rahmawati, A.; Rohmah, U.N.; Pertiwi, H.; Zakiyah The Dilemma of Using N95 Masks for Health Workers.; Atlantis Press, June 14 2023; pp. 119–127.
- Yang, S.; Fang, C.; Liu, X.; Liu, Y.; Huang, S.; Wang, R.; Qi, F. Surgical Masks Affect the Peripheral Oxygen Saturation and Respiratory Rate of Anesthesiologists. Frontiers in Medicine 2022, 9. [Google Scholar] [CrossRef]
- Bao, R.; Ning, G.; Sun, Y.; Pan, S.; Wang, W. Evaluation of Mask-Induced Cardiopulmonary Stress. JAMA Netw Open 2023, 6, e2317023. [Google Scholar] [CrossRef]
- Morgan, B.J.; Crabtree, D.C.; Palta, M.; Skatrud, J.B. Combined Hypoxia and Hypercapnia Evokes Long-Lasting Sympathetic Activation in Humans. Journal of Applied Physiology 1995, 79, 205–213. [Google Scholar] [CrossRef]
- Choudhury, A.; Singh, M.; Khurana, D.K.; Mustafi, S.M.; Ganapathy, U.; Kumar, A.; Sharma, S. Physiological Effects of N95 FFP and PPE in Healthcare Workers in COVID Intensive Care Unit: A Prospective Cohort Study. Indian J Crit Care Med 2020, 24, 1169–1173. [Google Scholar] [CrossRef] [PubMed]
- Pongvaramitchai, R.; Nakornchai, S.; Apipan, B. Effect of an N95 Respirator and a Surgical Mask-Covered N95 on the Cardiovascular Responses of Dentists Treating Paediatric Patients: A Crossover Clinical Trial. Int J Paediatr Dent 2023, 33, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Shehade, H.; Acolty, V.; Moser, M.; Oldenhove, G. Cutting Edge: Hypoxia-Inducible Factor 1 Negatively Regulates Th1 Function. The Journal of Immunology 2015. [Google Scholar] [CrossRef] [PubMed]
- Westendorf, A.M.; Skibbe, K.; Adamczyk, A.; Buer, J.; Geffers, R.; Hansen, W.; Pastille, E.; Jendrossek, V. Hypoxia Enhances Immunosuppression by Inhibiting CD4+ Effector T Cell Function and Promoting Treg Activity. CPB 2017, 41, 1271–1284. [Google Scholar] [CrossRef]
- G. M. Al-Allaff, R.; M. Y. Al-Taee, S.; T. D. Baker, S. Some Immunological Impacts of Face Mask Usage During the COVID-19 Pandemic. Pakistan Journal of Biological Sciences 2021, 24, 920–927. [CrossRef]
- Sceneay, J.; Parker, B.S.; Smyth, M.J.; Möller, A. Hypoxia-Driven Immunosuppression Contributes to the Pre-Metastatic Niche. OncoImmunology 2013, 2, e22355. [Google Scholar] [CrossRef]
- McKenna, V.S.; Kendall, C.L.; Patel, T.H.; Howell, R.J.; Gustin, R.L. Impact of Face Masks on Speech Acoustics and Vocal Effort in Healthcare Professionals. The Laryngoscope 2022, 132, 391–397. [Google Scholar] [CrossRef]
- Sönnichsen, R.; Llorach Tó, G.; Hochmuth, S.; Hohmann, V.; Radeloff, A. How Face Masks Interfere With Speech Understanding of Normal-Hearing Individuals: Vision Makes the Difference. Otol Neurotol 2022, 43, 282–288. [Google Scholar] [CrossRef]
- Truong, T.L.; Beck, S.D.; Weber, A. The Impact of Face Masks on the Recall of Spoken Sentences. J Acoust Soc Am 2021, 149, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Zarei, N.; Negarandeh, R.; Neshat, H. Communication Challenges Caused by Wearing Masks and Strategies Used by Pediatric Nurses during the COVID-19 Pandemic: A Qualitative Study. Journal of Pediatric Nursing: Nursing Care of Children and Families 2024, 0. [Google Scholar] [CrossRef]
- Carbon, C.-C.; Held, M.J.; Schütz, A. Reading Emotions in Faces With and Without Masks Is Relatively Independent of Extended Exposure and Individual Difference Variables. Frontiers in Psychology 2022, 13. [Google Scholar] [CrossRef] [PubMed]
- Hua, D.; Xu, Y.; Heiduschka, P.; Zhang, W.; Zhang, X.; Zeng, X.; Zhu, X.; He, T.; Zheng, H.; Xiao, X.; et al. Retina Vascular Perfusion Dynamics During Exercise With and Without Face Masks in Healthy Young Adults: An OCT Angiography Study. Translational Vision Science & Technology 2021, 10, 23. [Google Scholar] [CrossRef]
- Janicijevic, D.; Redondo, B.; Jiménez, R.; Lacorzana, J.; García-Ramos, A.; Vera, J. Intraocular Pressure Responses to Walking with Surgical and FFP2/N95 Face Masks in Primary Open-Angle Glaucoma Patients. Graefes Arch Clin Exp Ophthalmol 2021, 259, 2373–2378. [Google Scholar] [CrossRef]
- Jaya, I.P.P.; Astrawan, I.P.; Negara, N.L.G.A.M.; Empuaji, M.G.D. The Effect of Wearing A Mask on Oxygen Saturation and Pulse Rate During Climbing Stair in Public Areas. Indonesian Journal of Global Health Research 2024, 6, 631–644. [Google Scholar]
- Wong, A.Y.-Y.; Ling, S.K.-K.; Louie, L.H.-T.; Law, G.Y.-K.; So, R.C.-H.; Lee, D.C.-W.; Yau, F.C.-F.; Yung, P.S.-H. Impact of the COVID-19 Pandemic on Sports and Exercise. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology 2020, 22, 39–44. [Google Scholar] [CrossRef]
- Shenal, B.V.; Radonovich, L.J.; Cheng, J.; Hodgson, M.; Bender, B.S. Discomfort and Exertion Associated with Prolonged Wear of Respiratory Protection in a Health Care Setting. J Occup Environ Hyg 2011, 9, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Balestracci, B.; La Regina, M.; Di Sessa, D.; Mucci, N.; Angelone, F.D.; D’Ecclesia, A.; Fineschi, V.; Di Tommaso, M.; Corbetta, L.; Lachman, P.; et al. Patient Safety Implications of Wearing a Face Mask for Prevention in the Era of COVID-19 Pandemic: A Systematic Review and Consensus Recommendations. Intern Emerg Med 2023, 18, 275–296. [Google Scholar] [CrossRef] [PubMed]
- Barbeito-Caamaño, C.; Bouzas-Mosquera, A.; Peteiro, J.; López-Vázquez, D.; Quintas-Guzmán, M.; Varela-Cancelo, A.; Martínez-Ruiz, D.; Yañez-Wonenburger, J.C.; Piñeiro-Portela, M.; Vázquez-Rodríguez, J.M. Exercise Testing in COVID-19 Era: Clinical Profile, Results and Feasibility Wearing a Facemask. European Journal of Clinical Investigation 2021, 51, e13509. [Google Scholar] [CrossRef]
- Dacha, S.; Chuatrakoon, B.; Sornkaew, K.; Sutthakhun, K.; Weeranorapanich, P. Effects of Wearing Different Facial Masks on Respiratory Symptoms, Oxygen Saturation, and Functional Capacity during Six-Minute Walk Test in Healthy Subjects. Can J Respir Ther 2022, 58, 85–90. [Google Scholar] [CrossRef]
- Gelmez Taş, B.; Zerenozturk, G.; Demir, I.; Acar, I.; Basanmay, M. The Complaints of Health Workers After Mask Usage. Eurasian Journal of Family Medicine 2023, 12, 125–130. [Google Scholar] [CrossRef]
- Gyapong, F.; Debrah, E.; Oforiwaa, M.; Isawumi, A.; Mosi, L. Challenges and Adverse Effects of Wearing Face Masks in the COVID-19 Era. Challenges 2022, 13, 67. [Google Scholar] [CrossRef]
- Hua, W.; Zuo, Y.; Wan, R.; Xiong, L.; Tang, J.; Zou, L.; Shu, X.; Li, L. Short-Term Skin Reactions Following Use of N95 Respirators and Medical Masks. Contact Dermatitis 2020, 83, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Kizmaz, E.; Unver, F.; Telli Atalay, O. The Effects of Face Masks on Cardiopulmonary Capacity in Healthy Young Individuals. J Sports Med Phys Fitness 2022, 62, 1301–1305. [Google Scholar] [CrossRef]
- Lässing, J.; Falz, R.; Pökel, C.; Fikenzer, S.; Laufs, U.; Schulze, A.; Hölldobler, N.; Rüdrich, P.; Busse, M. Effects of Surgical Face Masks on Cardiopulmonary Parameters during Steady State Exercise. Sci Rep 2020, 10, 22363. [Google Scholar] [CrossRef]
- Mahmud, R.; Joy, K.M.N.I.; Rassel, M.A.; Monayem, F.B.; Datta, P.K.; Hossain, M.S.; Hoque, M.M.; Habib, S.M.H.R.; Munna, N.H.; Ahmed, M.; et al. Health Hazards Related to Using Masks and/or Personal Protective Equipment among Physicians Working in Public Hospitals in Dhaka: A Cross-Sectional Study. PLOS ONE 2022, 17, e0274169. [Google Scholar] [CrossRef]
- Matusiak, Ł.; Szepietowska, M.; Krajewski, P.; Białynicki-Birula, R.; Szepietowski, J.C. Inconveniences Due to the Use of Face Masks during the COVID-19 Pandemic: A Survey Study of 876 Young People. Dermatologic Therapy 2020, 33, e13567. [Google Scholar] [CrossRef] [PubMed]
- Micheletti Cremasco, M.; Vigoroso, L.; Solinas, C.; Caffaro, F. Discomfort in Use and Physical Disturbance of FFP2 Masks in a Group of Italian Doctors, Nurses and Nursing Aides during the COVID-19 Pandemic. Safety 2023, 9, 40. [Google Scholar] [CrossRef]
- Moumneh, A.; Kofoed, P.-E.L.; Vahlkvist, S.V. Face Mask Use during the COVID-19 Pandemic Was Associated with Breathing Difficulties in Adolescent Patients with Asthma. Acta Paediatr 2023, 112, 1740–1746. [Google Scholar] [CrossRef]
- Person, E.; Lemercier, C.; Royer, A.; Reychler, G. Effet du port d’un masque de soins lors d’un test de marche de six minutes chez des sujets sains. Revue des Maladies Respiratoires 2018, 35, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Prousa, D. Studie zu psychischen und psychovegetativen Beschwerden mit den aktuellen Mund-Nasenschutz-Verordnungen. 2020. [CrossRef]
- Purushothaman, P.K.; Priyangha, E.; Vaidhyswaran, R. Effects of Prolonged Use of Facemask on Healthcare Workers in Tertiary Care Hospital During COVID-19 Pandemic. Indian Journal of Otolaryngology and Head & Neck Surgery 2021, 73, 59. [Google Scholar] [CrossRef]
- Scarano, A.; Inchingolo, F.; Lorusso, F. Facial Skin Temperature and Discomfort When Wearing Protective Face Masks: Thermal Infrared Imaging Evaluation and Hands Moving the Mask. Int J Environ Res Public Health 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, S.K.; Prasad, N.; Verma, C.; Jaiswal, S.; Jaiswal, A. Headache Associated with PPE During COVID-19 Pandemic in Health Care Workers. Acta Neurol Taiwan 2023, 32(2), 57–64. [Google Scholar]
- Chmielewska, B.; Barratt, I.; Townsend, R.; Kalafat, E.; Meulen, J. van der; Gurol-Urganci, I.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; et al. Effects of the COVID-19 Pandemic on Maternal and Perinatal Outcomes: A Systematic Review and Meta-Analysis. The Lancet Global Health 2021, 0. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.L.; Ohde, S.; Takahashi, O.; Tokuda, Y.; Omata, F.; Fukui, T. Use of Surgical Face Masks to Reduce the Incidence of the Common Cold among Health Care Workers in Japan: A Randomized Controlled Trial. Am J Infect Control 2009, 37, 417–419. [Google Scholar] [CrossRef] [PubMed]
- Marques-Sule, E.; Espí-López, G.V.; Monzani, L.; Suso-Martí, L.; Rel, M.C.; Arnal-Gómez, A. How Does the Continued Use of the Mask Affect the Craniofacial Region? A Cross-Sectional Study. Brain and Behavior 2023, 13, e3077. [Google Scholar] [CrossRef]
- Ong, J.J.Y.; Bharatendu, C.; Goh, Y.; Tang, J.Z.Y.; Sooi, K.W.X.; Tan, Y.L.; Tan, B.Y.Q.; Teoh, H.-L.; Ong, S.T.; Allen, D.M.; et al. Headaches Associated With Personal Protective Equipment - A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache 2020, 60, 864–877. [Google Scholar] [CrossRef]
- Polivka, B.J.; Eldeirawi, K.; Huntington-Moskos, L.; Nyenhuis, S.M. Mask Use Experiences, COVID-19, and Adults with Asthma: A Mixed-Methods Approach. The Journal of Allergy and Clinical Immunology: In Practice 2022, 10, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Moreno, J.M.; Ceberino, D.; Plata, A.G.; Rebollo, B.; Sedas, P.M.; Hariramani, R.; Roa, A.M.; Constantino, A.B. Mask-Associated ‘de Novo’ Headache in Healthcare Workers during the COVID-19 Pandemic. Occup Environ Med 2021, 78, 548–554. [Google Scholar] [CrossRef]
- van Kampen, V.; Marek, E.-M.; Sucker, K.; Jettkant, B.; Kendzia, B.; Strauß, B.; Ulbrich, M.; Deckert, A.; Berresheim, H.; Eisenhawer, C.; et al. Influence of Face Masks on the Subjective Impairment at Different Physical Workloads. Sci Rep 2023, 13, 8133. [Google Scholar] [CrossRef]
- Waniganayake, Y.C.; Nadeeshani, H.K.D.K.; Buddhadasa, P.S.L.S.; Iresha, G.K.; Jayatilleke, S.K. Difficulties Encountered by Health Care Workers with the Use of N95 Disposable Masks and Elastomeric Respirators during COVID 19 Pandemic. 2021, 11, 18. [CrossRef]
- Yusof, M.Z.; Mukhtar, N.I. Workers’ Perceptions on the Tolerability of Their Respirators in Malaysia. Journal of Health Research 2023, 37. [Google Scholar] [CrossRef]
- Athar, M.H.; Zubair, U.B.; Ujala, Z. Biohazards of Prolonged N95 Use: Effects on Arterial Blood Gases, Peak Expiratory Flow Rate and General Well-Being of Healthcare Professionals during COVID-19 Pandemic. JCPSP, Journal of the College of Physicians and Surgeons Pakistan 2020, S134–S135. [Google Scholar]
- Hai, C.H.; Hua, K.K.; Wen, C.J.; Wen, C.C.; Ning, K.R.; Wah, Y.C. Comparing Effect of Donning Different Types of Face Masks on Oxygen Saturation, Pulse Rate and Comforts among Healthy Wearers. Journal of Positive School Psychology 2022, 6, 4058–4068. [Google Scholar]
- İpek, S.; Yurttutan, S.; Güllü, U.U.; Dalkıran, T.; Acıpayam, C.; Doğaner, A. Is N95 Face Mask Linked to Dizziness and Headache? Int Arch Occup Environ Health 2021, 94, 1627–1636. [Google Scholar] [CrossRef] [PubMed]
- Vidua, R.K.; Chouksey, V.K.; Bhargava, D.C.; Kumar, J. Problems Arising from PPE When Worn for Long Periods. Med Leg J 2020, 88, 47–49. [Google Scholar] [CrossRef]
- Zhou, Z.; Dong, L. Experimental Investigation of the Effect of Surgical Masks on Outdoor Thermal Comfort in Xiamen, China. Building and Environment 2023, 229, 109893. [Google Scholar] [CrossRef]
- Wong, C.K.M.; Yip, B.H.K.; Mercer, S.; Griffiths, S.; Kung, K.; Wong, M.C.; Chor, J.; Wong, S.Y. Effect of Facemasks on Empathy and Relational Continuity: A Randomised Controlled Trial in Primary Care. BMC Family Practice 2013, 14, 200. [Google Scholar] [CrossRef]
- Anczyk, S.; Stępień, M.; Raczyński, M.; Anczyk, A.; Woźniakowska, M.; Miziołek, B.; Polak, K.; Bergler-Czop, B. The Impact of Face Masks on Acne-prone Skin in Polish Young Adults during COVID-19 Pandemic. Dermatol Ther 2022, 35, e15922. [Google Scholar] [CrossRef]
- Bakhsh, R. a; Saddeeg, S.Y.; Basaqr, K.M.; Alshammrani, B.M.; Zimmo, B.S. Prevalence and Associated Factors of Mask-Induced Acne (Maskne) in the General Population of Jeddah During the COVID-19 Pandemic. Cureus 2022, 14, e26394. [Google Scholar] [CrossRef]
- Berjawi, A.; Salameh, P.; Fadel, N.; El Khoury, J.R. Mask-Acne Prevalence and Risk Factors during the COVID-19 Pandemic: A Cross-Sectional Single Institution Study. Dermatologic Therapy 2023, 2023, e9470636. [Google Scholar] [CrossRef]
- Cheng, Y.-F.; Zhao, H.; Li, J.; Lipa, K.E.; Xie, H.-F.; Wang, B.; Huang, Y.-X. Factors Aggravating Acne Vulgaris during the COVID-19 Pandemic in China: A Web-Based Cross-Sectional Survey. Eur Rev Med Pharmacol Sci 2022, 26, 7305–7312. [Google Scholar] [CrossRef]
- Dani, A.; Eseonu, A.; Bibee, K. Risk Factors for the Development of Acne in Healthcare Workers during the COVID-19 Pandemic. Arch Dermatol Res 2023, 315, 1067–1070. [Google Scholar] [CrossRef] [PubMed]
- Falodun, O.; Medugu, N.; Sabir, L.; Jibril, I.; Oyakhire, N.; Adekeye, A. An Epidemiological Study on Face Masks and Acne in a Nigerian Population. PLOS ONE 2022, 17, e0268224. [Google Scholar] [CrossRef] [PubMed]
- Foo, C.C.I.; Goon, A.T.J.; Leow, Y.; Goh, C. Adverse Skin Reactions to Personal Protective Equipment against Severe Acute Respiratory Syndrome – a Descriptive Study in Singapore. Contact Dermatitis 2006, 55, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Fourie, A.; Muvhali, M.; Carman, H.; Singh, T. Occupational Skin Disease Associated with Personal Protective Equipment: A Case Series. Current Allergy & Clinical Immunology 2022, 35, 223–231. [Google Scholar]
- Kumar Shubhanshu; Singh, A. Prolonged Use of N95 Mask a Boon or Bane to Healthcare Workers During Covid–19 Pandemic. Indian J Otolaryngol Head Neck Surg 2022, 74, 2853–2856. [Google Scholar] [CrossRef]
- Lan, J.; Song, Z.; Miao, X.; Li, H.; Li, Y.; Dong, L.; Yang, J.; An, X.; Zhang, Y.; Yang, L.; et al. Skin Damage among Health Care Workers Managing Coronavirus Disease-2019. J Am Acad Dermatol 2020, 82, 1215–1216. [Google Scholar] [CrossRef]
- McKenna, K.; Bouchoucha, S.; Redley, B.; Hutchinson, A. Australian Health Care Workers Experience of PPE Related Side-Effects. A Cross-Sectional Survey. Front. Public Health 2024, 12. [Google Scholar] [CrossRef]
- Nasir, N.A.B.M.; Sarkurunatan, A.A.; Muhammaddun, M.Z.B.Z.; Yu, L.X.; Manan, N.A. The Prevalence of Adverse Skin Reactions Associated with Face Mask Wearing among Students in Malaysia. Asian Journal of Medicine and Health Sciences 2023, 6, 122–133. [Google Scholar]
- Perera, M.H.; Joshi, M.; Govindan, A.K.; Edpuganti, S.; Korrapati, N.H.; Kiladze, N. Impact of Mask Wear on the Skin of Clinical Year Medical Students during the COVID-19 Pandemic: A Cross-Sectional Study. CSDM 2022, 2. [Google Scholar] [CrossRef]
- Sliwakowska, K.; Radwanska, J.; Czuwara, J. The Impact of Masks on the Condition of Facial Skin in the Time of the COVID-19 Pandemic. Our Dermatology Online 2022, 13(e):e55, 1–8. [Google Scholar] [CrossRef]
- Techasatian, L.; Lebsing, S.; Uppala, R.; Thaowandee, W.; Chaiyarit, J.; Supakunpinyo, C.; Panombualert, S.; Mairiang, D.; Saengnipanthkul, S.; Wichajarn, K.; et al. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J Prim Care Community Health 2020, 11, 2150132720966167. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Liu, Y.; Zou, Z.; Cheng, C.; Wang, W.; Huang, Z.; Wu, G.; Zhu, W.; Sun, H. Effects of Prolonged Face Mask Use among Patients with Hypertension or Diabetes during the COVID-19 Pandemic. J Int Med Res 2024, 52, 03000605241232946. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-R.; Han, J.; Yeon, Y.M.; Kang, N.Y.; Kim, E. Effect of Face Mask on Skin Characteristics Changes during the COVID-19 Pandemic. Skin Res Technol 2021, 27, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Naylor, G.; Burke, L.A.; Holman, J.A. Covid-19 Lockdown Affects Hearing Disability and Handicap in Diverse Ways: A Rapid Online Survey Study. Ear Hear 2020, 41, 1442–1449. [Google Scholar] [CrossRef] [PubMed]
- Thomas, F.; Allen, C.; Butts, W.; Rhoades, C.; Brandon, C.; Handrahan, D.L. Does Wearing a Surgical Facemask or N95-Respirator Impair Radio Communication? Air Med J 2011, 30, 97–102. [Google Scholar] [CrossRef]
- Heider, C.A.; Álvarez, M.L.; Fuentes-López, E.; González, C.A.; León, N.I.; Verástegui, D.C.; Badía, P.I.; Napolitano, C.A. Prevalence of Voice Disorders in Healthcare Workers in the Universal Masking COVID-19 Era. The Laryngoscope 2020, n/a. [Google Scholar] [CrossRef]
- Forgie, S.E.; Reitsma, J.; Spady, D.; Wright, B.; Stobart, K. The “Fear Factor” for Surgical Masks and Face Shields, as Perceived by Children and Their Parents. Pediatrics 2009, 124, e777–781. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, Q.; Ma, Q.; Wu, Y.; Wang, Y.; Chen, C.; Yao, Y.; Feng, Z.; Yuan, X.; Shi, S.; et al. Effect of Surgical Masks and N95 Respirators on Anxiety. NDT 2024, 20, 551–559. [Google Scholar] [CrossRef]
- Hatanaka, N.; Xu, B.; Yasugi, M.; Morino, H.; Tagishi, H.; Miura, T.; Shibata, T.; Yamasaki, S. Chlorine Dioxide Is a More Potent Antiviral Agent against SARS-CoV-2 than Sodium Hypochlorite. J Hosp Infect 2021, 118, 20–26. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency (US EPA). Integrated Risk Information System (IRIS): Toxicological Review of Chlorine Dioxide and Chlorite (CAS Nos. 10049-04-4 Last Revised — 10/12/2000. National Service Center for Environmental Publications, Chemical Assessment Summary, Human health assessment information.
- Dourson, M.; Charnley, G.; Scheuplein, R. Differential Sensitivity of Children and Adults to Chemical Toxicity: II. Risk and Regulation. Regulatory Toxicology and Pharmacology 2002, 35, 448–467. [Google Scholar] [CrossRef]
- OECD PISA Results: Maths and Reading Skills in “Unprecedented Drop”. Here’s Why That Matters. Available online: https://www.weforum.org/agenda/2023/12/oecd-pisa-results-maths-reading-skills-education/ (accessed on 29 August 2024).
- Kampf, G. Effect of Face Masking on Transmission of SARS-CoV-2. In The COVID-19 Aftermath: Volume II: Lessons Learned; Rezaei, N., Ed.; Springer Nature Switzerland: Cham, 2024; ISBN 978-3-031-61943-4. [Google Scholar]
- Tenenbaum, T.; Doenhardt, M.; Diffloth, N.; Berner, R.; Armann, J.P. High Burden of RSV Hospitalizations in Germany 2021–2022. Infection 2022, 50, 1587–1590. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.C. Increase in Acute Respiratory Illnesses Among Children and Adolescents Associated with Rhinoviruses and Enteroviruses, Including Enterovirus D68 — United States, July–September 2022. MMWR Morb Mortal Wkly Rep 2022, 71. [Google Scholar] [CrossRef] [PubMed]
- Gier, B. de; Marchal, N.; Beer-Schuurman, I. de; Wierik, M. te; Hooiveld, M.; Group, I.-A.S.; Group, G.S.; Melker, H.E. de; Sorge, N.M. van Increase in Invasive Group A Streptococcal (Streptococcus Pyogenes) Infections (iGAS) in Young Children in the Netherlands, 2022. Eurosurveillance 2023, 28, 2200941. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, S.N.; Guy, R.; Bhopal, S.S.; Brown, C.S.; Lamagni, T.; Sharp, A. Paediatric Group A Streptococcal Disease in England from October to December, 2022. The Lancet Child & Adolescent Health 2023, 7, e2–e4. [Google Scholar] [CrossRef]
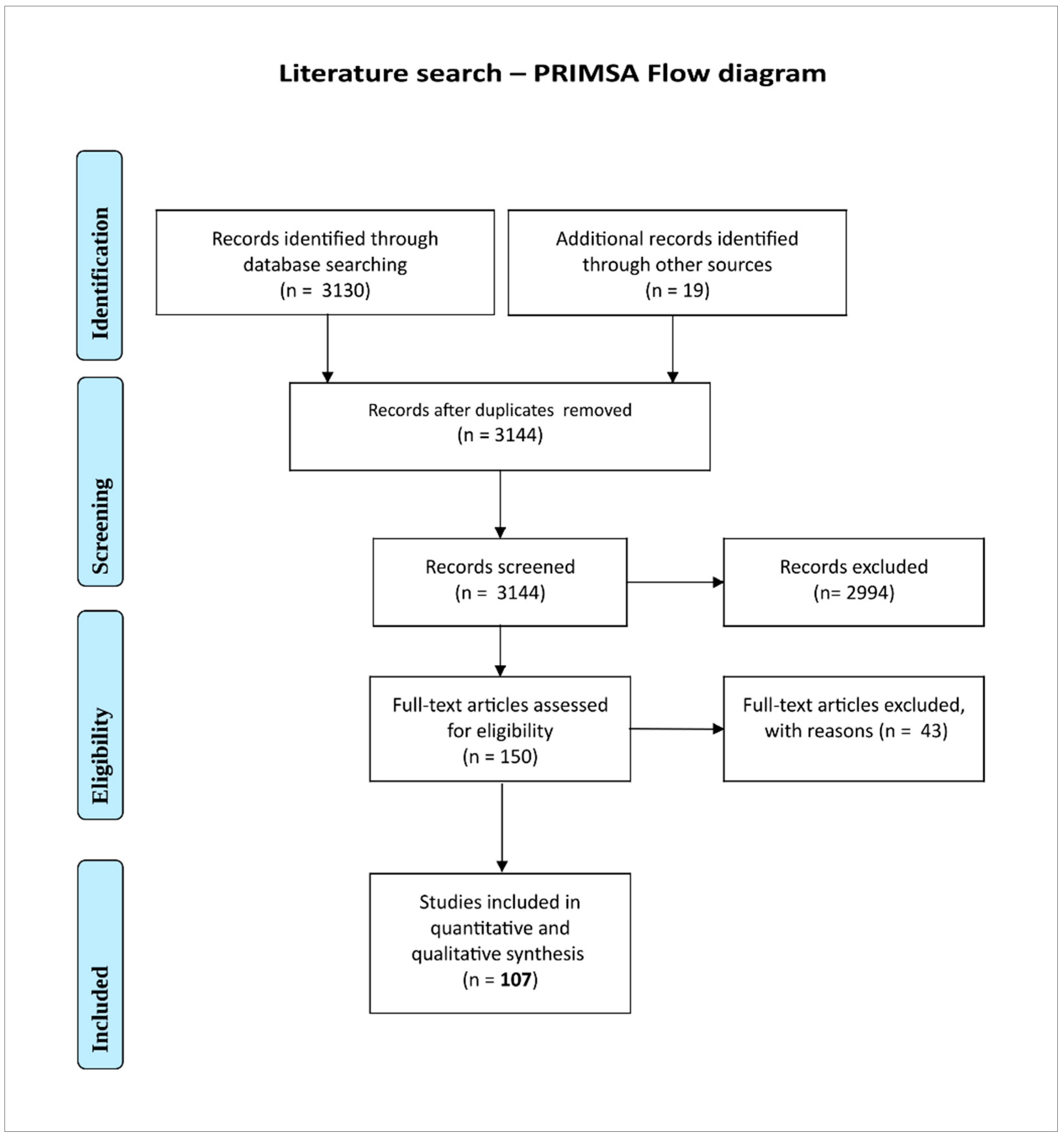
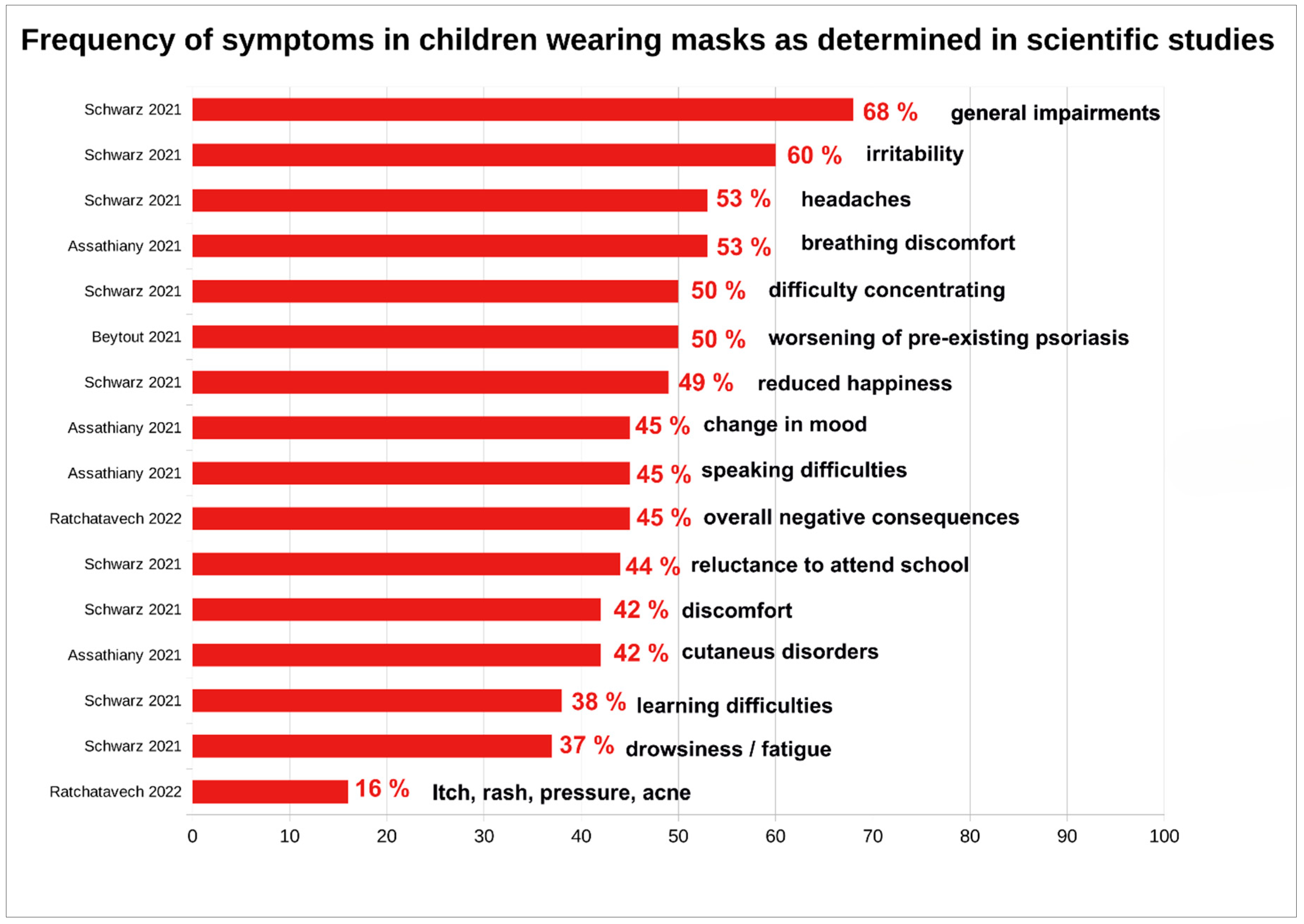
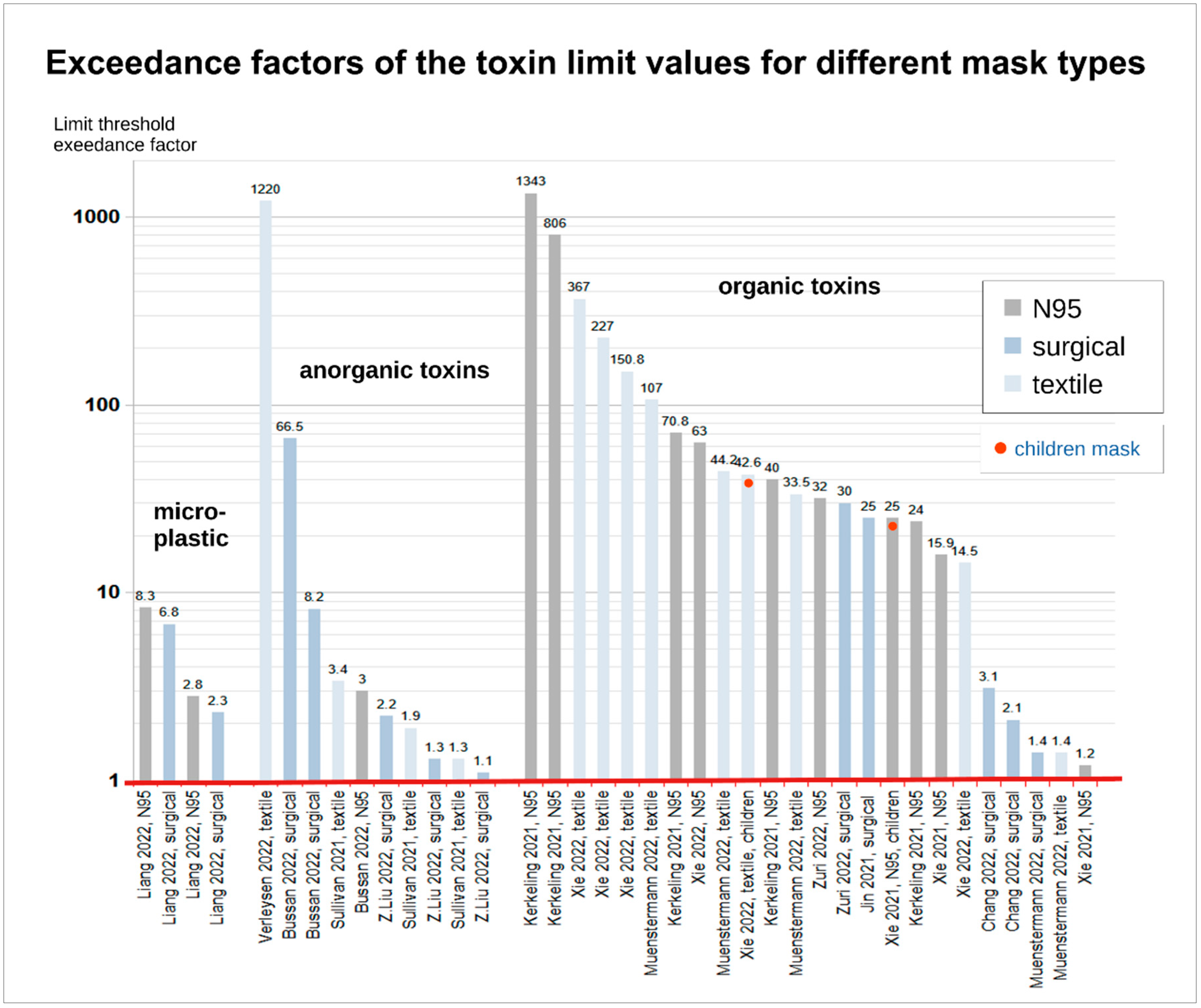
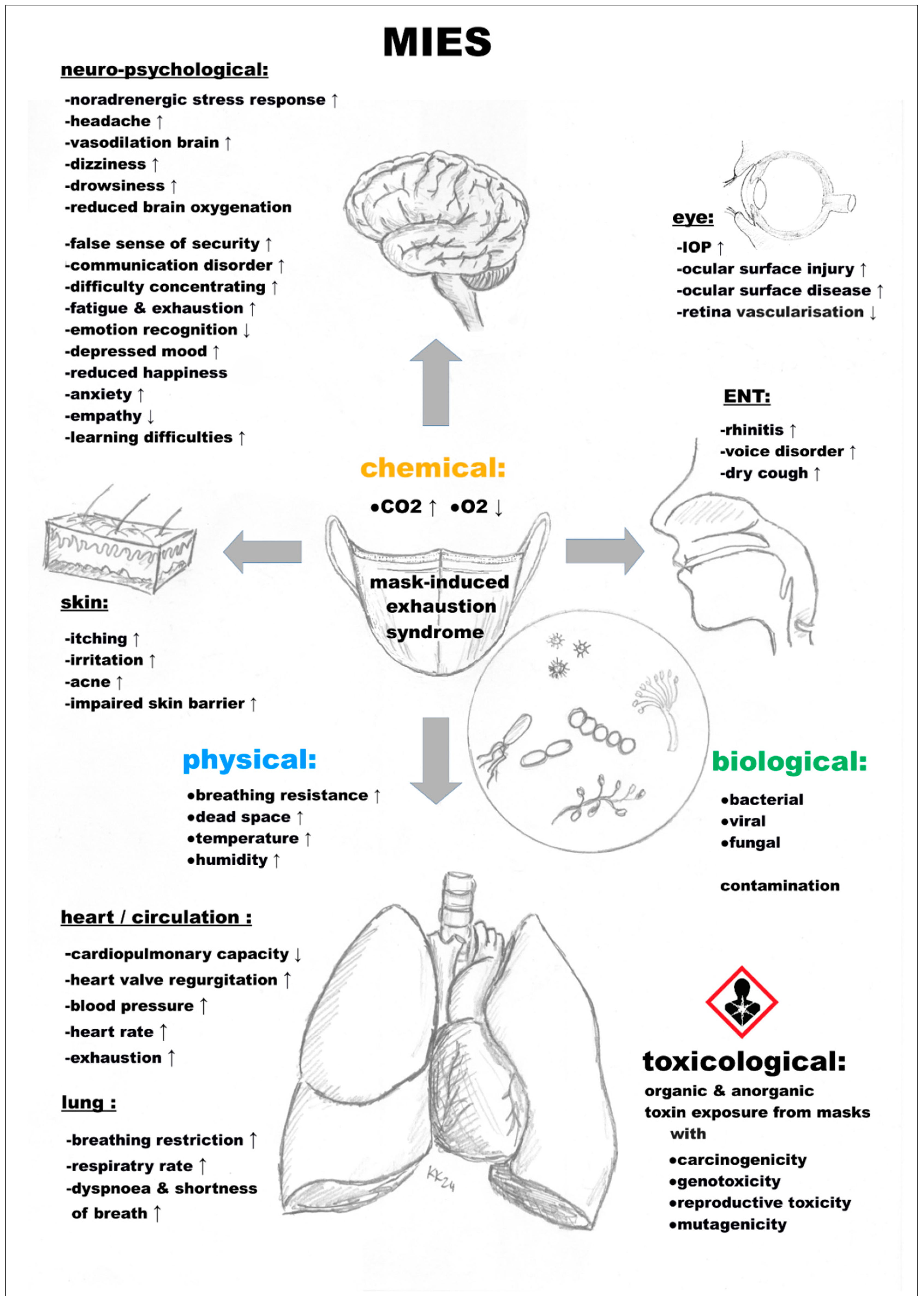
| masks and children risk assessment – adverse effects | scientific evidence | ||
| toxicological risk (carcinogenic, mutagenic, physio-metabolic) | yes | ||
| bacterial, fungal and viral burden (contamination) | unclear | ||
| physical symptoms | yes | ||
| exacerbation of existing diseases | yes | ||
| triggering of new diseases | yes | ||
| psychological symptoms | yes | ||
| sociological/developmental disruptive effect | unclear | ||
| large absence of undesirable effects | no | ||
| masks and children risk assessment – contextual factors | evidence/basics | ||
| mask standardisation (bacterial filtration) | yes | ||
| mask standardisation (particle filtration) | yes | ||
| mask standardisation (virus filtration) | no | ||
| effectiveness of masks against viruses in children | unproven | ||
| ensuring appropriate use of masks in children | unproven | ||
| high SARS-CoV-2 infectivity in children | no | ||
| frequent devastating COVID-19 course in children | no | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





