1. Introduction
Attention Deficit Hyperactivity Disorder (ADHD) stands as one of the most prevalent neurodevelopmental disorders globally, with a prevalence ranging from 5.29% to 7.2% [
1] whereas it is considered the most common social, emotional, and behavioral disability, accounting for approximately 11% of all social, emotional, and behavioral disabilities [
2]. Specifically in children, the estimated worldwide prevalence of ADHD is around 5.9% [
3] and can be as high as 7.6% [
4]. Its diagnosis can be safely achieved at the age of 8-10 years; however, ADHD has been emerged more and more frequently among preschool aged children [
5,
6], with percentages of prevalence ranging from 2% [
7] to 12.8%, predominantly in boys [
8,
9,
10], highlighting the importance of early identification and intervention to provide effective support. ADHD is characterized by inattention, and/or hyperactivity, and impulsivity [
11], with negative consequences in health [
12], socio-emotional functioning [
13,
14,
15,
16], cognitive skills, and motor competence [
17] that affect several domains of life, including academic achievement [
18], and work [
19].
When considering preschool-aged children, difficulties associated with ADHD are crucial, as they may have lasting effects on academic and social functioning in later years [
20]. Fostering social-emotional competence during the preschool years holds significance, as children who exhibit such competence at this age are more likely to excel in the academic and social domains later in life [
21,
22].
Given the well-documented importance of both the socioemotional- and motor domains of human behaviour for school readiness [
23,
24], early interventions targeting these domains appear valuable. This is particularly true for children with ADHD, as such interventions have the potential to enhance their development and behaviour [
25]. However, ADHD is a lifelong disorder that requires longitudinal and individualized programmes that range from a few months to many years [
26]. The main therapeutic interventions for ADHD so far encompass medication [
27,
28], behavioural/psychological therapy [
29], or a combination of both approaches [
30]. Although the American Academy of Pediatrics advocates parent training in behaviour management as the first intervention option for young children with ADHD before the use of medication, which is only recommended in severe cases [
31], medication appears to be an increasingly common option and even predominant treatment [
32]. While it has shown positive effects on ADHD symptoms in children [
33], its efficacy in addressing the full spectrum of attention and behavioural problems of children with ADHD has been questioned [
34]. Notably, medication seems ineffective in addressing the social interaction difficulties these children experience [
35] and any benefits observed from medication-based treatments often do not appear to be long-lasting [
36].
In response to concerns about the unknown long-term effects of pharmacological treatments in children, there has been a shift towards exploring non-pharmacological interventions [
31,
37]. For instance, the US Food and Drug Administration discourages the use of psychostimulants and other psychiatric medications in children under six years old [
25]. Psychosocial therapy, coupled with parent education, often emerges as an alternative to medication and has shown promising outcomes in preschool children [
38,
39,
40].
In recent years, a growing body of research has highlighted the positive effects of physical activity programs on various neuro-psychological parameters [
41], cognitive function [
42,
43], executive functions [
44], socio-emotional parameters [
45,
46], and ADHD symptomatology [
47]. Psychomotor Therapy, a holistic therapeutic approach based on physical activity, constitutes an integral component of psychiatric care and mental health systems in several European countries [
48]. One form of Psychomotor Therapy is Group Psychomotor Therapy (GPT), which focuses on group dynamics [
49]. GPT is “experience-oriented” [
50], incorporating body, social, and material experiences within each therapy session [
51]. Drawing on the theoretical foundations of Play Therapy [
52], Cognitive Behavioral Play Therapy [
53], and Group Psychotherapy [
54], GPT offers a holistic approach to therapy. While limited studies focus on GPT, some suggest its significant impact on the motor skills of typically developing young children [
55,
56,
57]. Evidence also suggests the benefits of GPT for children with various neurodevelopmental disorders, such as autism spectrum disorder [
58]; while initial indications point to a positive effect of GPT on children with ADHD; nevertheless, supporting research evidence is currently lacking [
50]. It seems that the impact of both typical physical activity-based programs and GPT on enhancing socioemotional and motor outcomes in children aged 4-6 years with ADHD remains underexplored. Notably, there is a gap in the literature regarding the effectiveness of inclusive physical activity interventions, where children with and without ADHD participate together. On this basis, this study represents a first effort to investigate the effects of GPT on the socio-emotional and motor competence of children aged 5-6 years, both with and without ADHD, in a group setting. This research aims to provide valuable insights into the potential benefits of GPT for children in this age group, shedding light on its impact on diverse developmental aspects in a mixed-ability group context.
2. Materials and Methods
2.1. Participants
In total, 54 children (31 boys; 23 girls) between the ages of 61 and 69 months (M= 61.80±5.40 months) participated in the study. Of these, 35 (11 boys; 14 girls) were typically developing (NON-ADHD; Mage= 51.7±3.09) and 19 (12 boys; 7 girls) had been diagnosed with ADHD (Mage= 50.62±3.52). Children with ADHD receiving medication were excluded from the sample, as in studies using a combination of interventions, it is extremely difficult to clarify the extent of the effect of each intervention [
26].
Children’s participation in GPT groups was voluntary, with written consent obtained from parents or legal guardians. Participants belonged to 5 different groups that participated in GPT sessions led by the same therapists and within the same therapeutic context across different time periods. Specifically, children of groups 1 (n=10) and 2 (n=11) partook in GPT session during 2017-2018, with 8 children diagnosed with ADHD in these groups. Groups 3 (n=12), 4 (n=10) and 5 (n=11) engaged in GPT sessions during 2018-2019, with 11 ADHD-diagnosed children among them.
2.2. Measures
2.2.1. Motor Competence
The Democritos Movement Screening Test for preschool children (DEMOST-PRE©) [
59] was employed to assess children’s motor competence. The DEMOST-PRE© is a valid and reliable assessment tool [
60,
61,
62] specifically designed to assess motor competence in preschool-aged children. It consists of nine items: tapping; jumping repeatedly sideways; running, carrying, and placing a ball in a box; toe-to-heel walking in a backward direction; overhead toss to a specific target; picking up coins and placing them in a box; stepping though three vertical hoops; catching a bean bag; standing jump over a stick. Before the administration of the above items, a hand preference test is performed. Short fairytales, which are part of a story, are used for the presentation of the above items to the examinee so as he/she to be motivated to participate. The administration of the test typically takes around 15 minutes, depending on the child's pace.
Following a standard procedure common to movement assessment batteries, the child's performance on each task is recorded in raw scores (e.g., time taken, number of coins transferred), which are then converted into point scores based on the DEMOST-PRE© manual guidelines. The total DEMOST-PRE© score is derived by summing up the nine-point scores. Scores below 3 are categorized as "below average," while scores exceeding 4 are considered "average" [
59].
2.2.2. Socio-Emotional Competence
Social-emotional competence was assessed using the Psychosocial Adjustment Test [
63]. The test, whose psychometrics are sufficiently supported [
64], is tailored for children aged 4-12 years. In the case of children aged 4-6 years, the assessment is conducted by their teacher(s), focusing on the child's social adjustment within the school environment. The Psychosocial Adjustment Test comprises four subscales (social competence, school competence, emotional competence, and behavioural problems), with each of them including several dimensions. In this study, the subscales of social and emotional competence were used. The social competence (SC) subscale comprises 23 items classified into three dimensions: leadership (L; 5 items), interpersonal relationships (R; 13 items), and cooperation with peers (C; 5 items). The emotional competence (EC) subscale consists of 26 items classified into four dimensions: self-control (SC; 8 items), stress management (SM; 5 items), emotion management (EM; 5 items), and empathy (E; 6 items).
Each behaviour is rated on a 5-point Likert scale (ranging from 1= “not at all” to 5= “very much”), indicating to what extent this particular behaviour applies to the child. High scores on both subscales indicate positive adjustment. Scoring is conducted at both at the dimension level and at the overall subscale level. Point scores for each dimension and subscale are converted into standard scores (T-scores), with a mean of 50 and a standard deviation of 10. Scores exceeding 60 are considered high, scores above 50 are typical; scores between 30 and 40 are labeled as "poor"; scores below 30 are classified as "very poor" [
64].
2.2.3. Group Psychomotor Therapy Programme (GPT)
GPT is a comprehensive therapeutic approach that can be implemented independently or in conjunction with other interventions for young children. It is designed to address a wide range of motor, behavioral, and socio-emotional difficulties as well as various neuro-developmental disorders. By incorporating a diverse array of physical activities, GPT focuses on enhancing children’s cognitive processes, through movement within interactive play sessions. Each GPT session is structured around the principles outlined by [
51], who categorizes experiences into three key areas: body, social, and material. These sessions typically consist of three main components: (a) the awakening phase, aiming to foster group cohesion and establish a supportive environment, (b) the therapeutic core that comprises activities targeting the development of children's motor skills while also addressing cognitive and socio-emotional aspects of their behavior, and (c) the relaxation rituals that involves calming and relaxing activities to conclude the session.
The aims of GPT for its participants are developing independence and responsibility; enhancing social skills and self-awareness; expanding motor skills and self-esteem; promoting empathy and trust; fostering self-respect and acceptance. Within this context, the therapist takes on a more subtle and "invisible" role, allowing the children to feel more at ease and included in the group activities. This approach provides the therapist with better access to observe and understand each child's unique needs and behaviors within the group dynamic. The group setting of GPT serves as a natural socialization environment, where children interact with their peers, face challenges, and learn to respect common rules. These rules are co-decided with the children, allowing the group to develop its own dynamics. This group dynamic often serves as a solution for those children who have the most difficulties, as they can benefit from the supportive and inclusive nature of the group [
50].
In this study, the GPT program lasted six months (27 weeks), including three 50-minute sessions per week. During the first sessions of the program, individualized treatment was mainly provided within the group, depending on the symptoms and the needs of the participants to ensure that each participant could master their personal objectives, even if they were not at the same starting level as their peers. After an initial observation period to assess the children's motor, emotional, and social competencies, the program transitioned to group-based and interactive activities.
2.3. Data Analysis
The IBM SPSS 29 software was used for statistical processing of data. Descriptive statistics were generated for the key study variables (MC, SC, and EC) and potential differences between the two groups (ADHD; NON-ADHD) at the pre-test measurement in MC, SC, and EC were examined via t-tests for independent samples. Then, differences between the 1st and 2nd measurements for each dependent variable were computed and t-tests for independent samples with the abovementioned calculated differences as dependent variables were conducted to address the question of which group (ADHD; NON-ADHD) presented the higher change in MC, SC, and EC from the first to the second measurement. Moreover, paired t-tests were performed for each pair of MC, SC, and EC scores (1st vs 2nd measurement) within the ADHD and NON-ADHD groups separately to examine whether the change in each group was statistically significant. Throughout these analyses, besides examining the p-values, Cohen's d effect size was also taken into account to provide a comprehensive understanding of the results.
3. Results
Descriptive statistics (means, standard deviations) of participants’ scores on the DEMOST-PRE© (total score) and the Psychosocial Adjustment Test (social and emotional competence subscales scores; key variables are presented in
Table 1.
The comparison of children’s performance at the pre-test revealed statistically significant higher scores of NON-ADHD in all variables (MC: t=2.98, p<.005, d=1.78; SC: t=5.53, p<.001, d=4.39; L: t=3.64, p<.001, d=3.70; R: t=5.11, p<.001, d=4.61 ; C: t=6.17, p<.001, d=5.42; EC: t=6.18, p<.001, d=1.59; C: t=2.36, p<.001, d=3.17; SM: t=2.90, p<.001, d=3.95; EM :t=2.74; p<.001, d=2.39 ; E: t=4.85, p<.001, d=2.85).
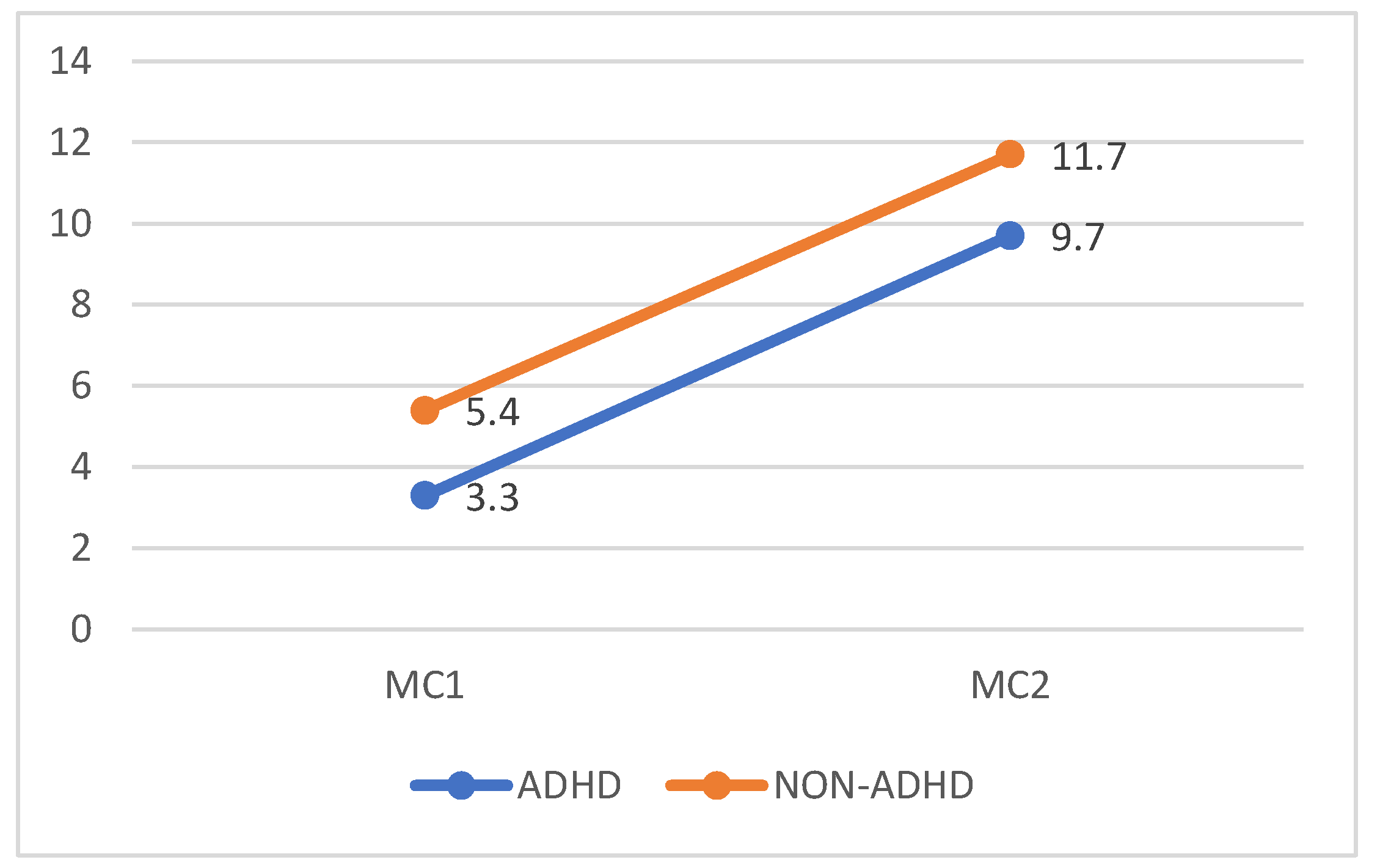
As far as the impact of GPT, the two groups had similar changes in MC (t=.121, p=.904, d=.049), with both presenting significant improvements (ADHD: t=6.39, p<.001, d=2.01, NON-ADHD: t=8.33, p<.001, d=2.08) (
Figure 1).
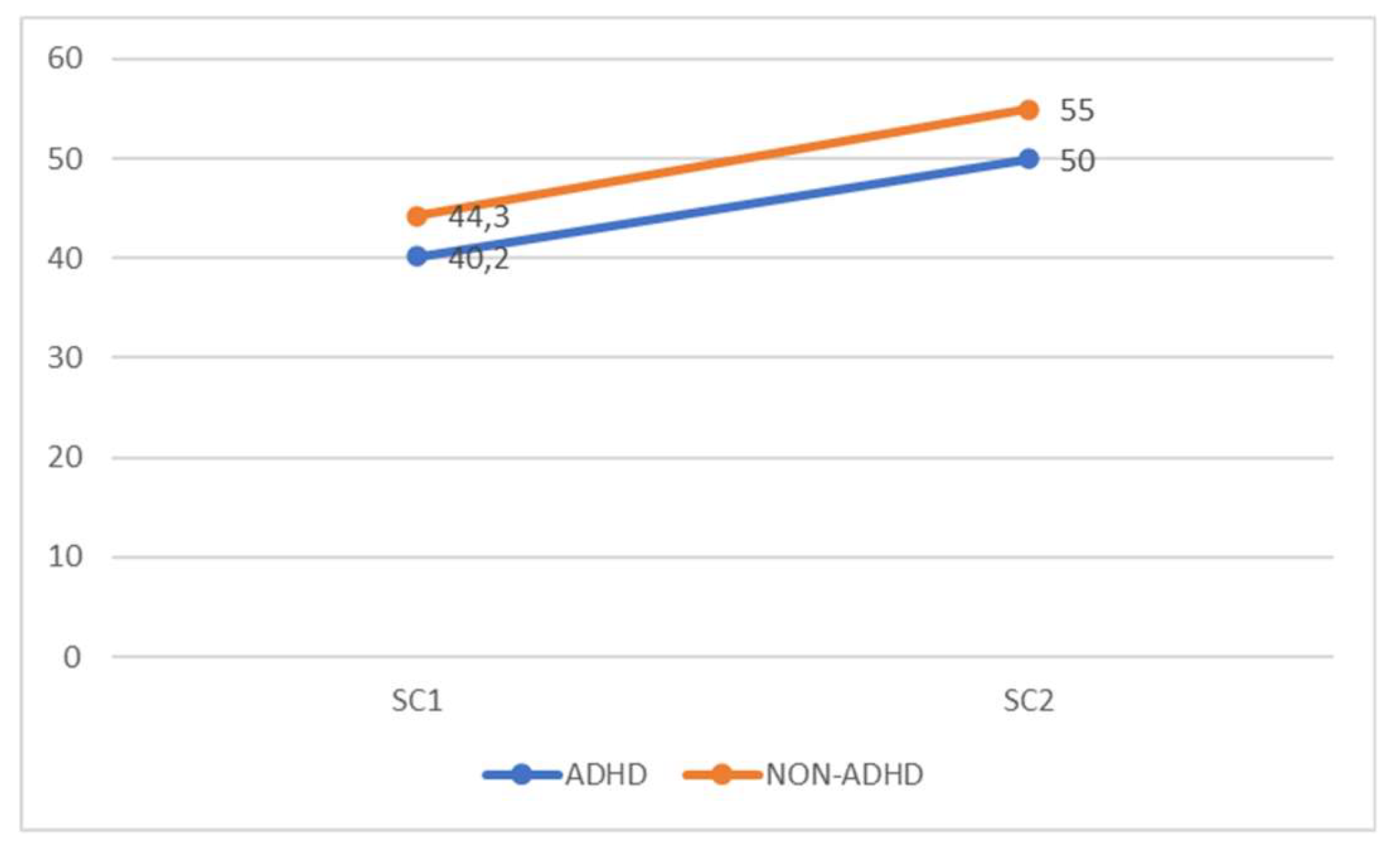
The two groups had equal change in time (t=.338, p=.738, d=.136) that was positive and significant for both groups (ADHD: t=5.68, p<.001, d=1.8, NON-ADHD: t=2.45, p<.05, d=.61), with NON-ADHD presenting a lower improvement, though (
Figure 2).
The analyses on children’s scores in SC dimensions revealed only one significant difference between the groups in leadership (t=2. 92, p<.01, d=1.17). There were no significant differences in interpersonal relationships (t=.191, p=.850, d=.077) or cooperation with peers (t=.276, p=.785, d=.111). As far as the progress of each group, separately, in ADHD group significant improvement were identified in all three SC dimensions (L: t=6.39, p<.001, d=2.02; R: t=3.0, p<.05, d=.949; C: t=2.88, p<.05, d=. 910). In the NON-ADHD group, no statistically significant improvements were found in any dimension (L: t=1.51, p=.153, d=.377; R: t=.99, p=.340, d=.246; C: t=1.82, p=.089, d=.454).
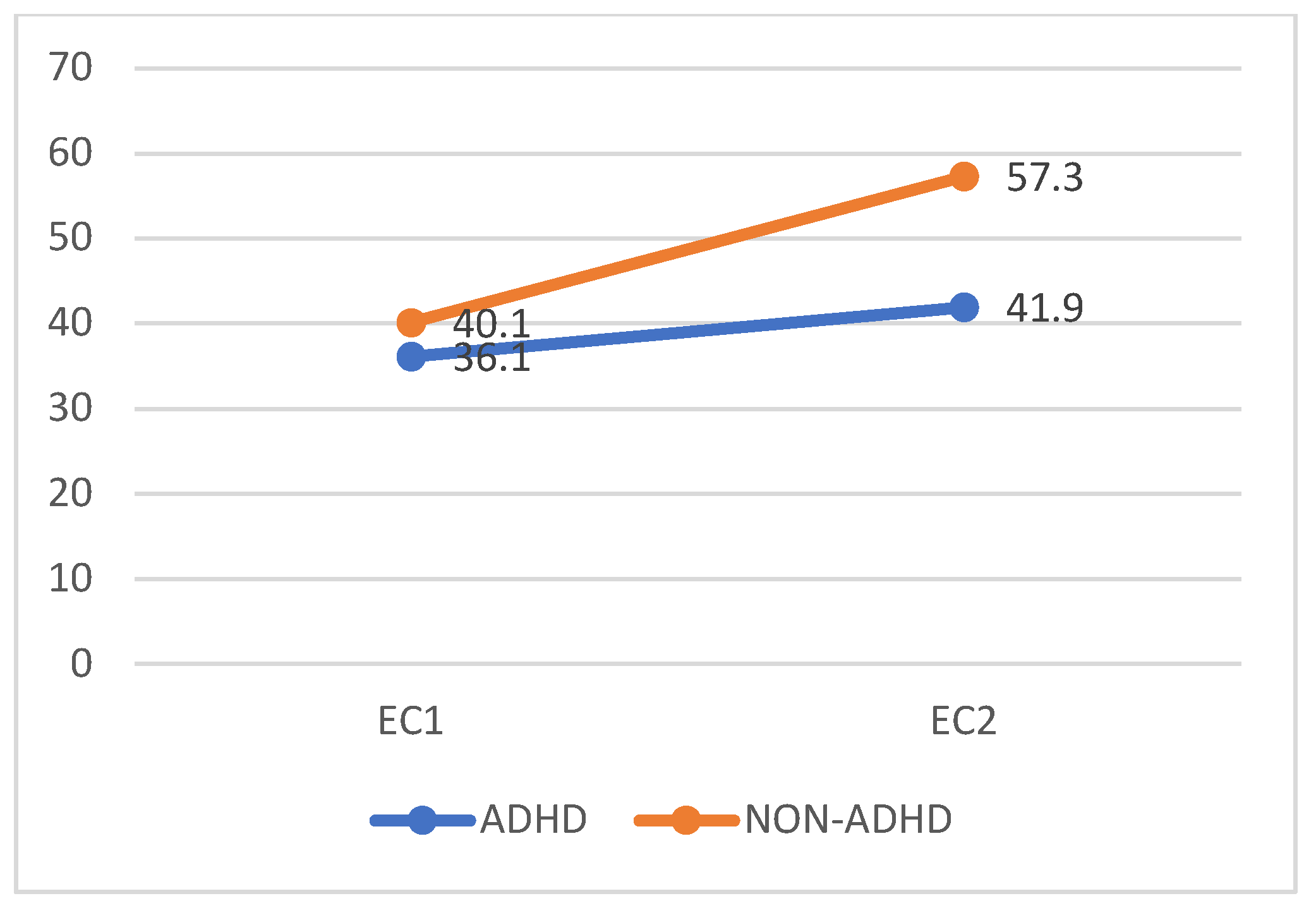
The analyses conducted for the EC subscale total scores showed that the ADHD presented a significantly lower improvement than their NON-ADHD peers (t=8.76, p<.001, d=3.53). Nevertheless, the EC scores of both groups after the GPT were significantly higher than their baseline measurement (ADHD: t=15.76, p<.001, d=3.94, NON-ADHD: t=11.11, p<.001, d=3.52) (
Figure 3).
Focusing on the four EC dimensions, statistically significant differences in favor of the changes presented by the NON-ADHD group (C: t=4.77, p<.001, d=1.92; SM: t=4.36, p<.001, d=1.76; EM: t=3.73, p<.005, d=1.50E; E: t=8.09, p<.001, d=3.26) were revealed. However, both groups improved statistically significantly on all EC subscales: ADHD (C: t=7.71, p<.001, d=1.93; SM: t=11.20, p<.001, d=2.80; EM t=6.83, p<.001, d=1.71; E: t=10.31, p<.001, d=2.58) and NON-ADHD (C: t=6.19, p<.001, d=1.96; SM: t=5.76, p<.001, d=1.82; EM t=13.20, p<.001, d=4.17; E: t=8.65, p<.001, d=2.74).
4. Discussion
Although medication is a common treatment option for children with ADHD, its effectiveness in addressing the full range of symptoms is questionable [
34,
35], whereas non-pharmacological interventions are recommended, particularly for young children [
25,
31,
65] with the physical activity programmes having accumulated supportive research evidence regarding their positive effects of ADHD symptomatology [
47]. This study is the first to investigate the impact of an inclusive GPT programme on the social, emotional, and motor competence of children with and without ADHD. Our results indicate that the GPT programme significantly improved all the measure parameters (i.e., MC, SC, and EC) in both groups. This finding is particularly noteworthy as it supports the empirical findings of psychomotor therapists that the inclusive GPT context benefits both children with disorders and their typically developing peers.
Starting with MC, the positive effect of the GPT is in aligned with previous studies in which GPT programmes were implemented in young children and led to significant improvements in their MC [
56,
57]. Baseline measurements revealed an expected disparity in MC between children with ADHD and their NON-ADHD peers, consistent with existing literature [
66,
67,
68]. In fact, according to the manuals of the DEMOST-PRE©, participants with ADHD seemed to be at risk for motor difficulties. Thus, one could argue that such a programme might not adequately challenge NON-ADHD children with proficient motor skills. Nevertheless, NON-ADHD children showed remarkable improvement. This outcome can be attributed to GPT's approach of accommodating participants with varying levels of MC. GPT employs a strategy of adjusting activity difficulty levels to ensure suitability for each participant, contributing to the notable progress observed in the NON-ADHD children.
Another fundamental principle in GPT is the principle of self-action, which empowers each child to choose their own ways to perform the task without restrictions. Thus, GPT does not rely on the “average performance” of the group, but rather allows for individual improvement in MC tailored to each child’s initial level [
50].
As far as social competence is concerned, NON-ADHD children outperformed their ADHD counterparts in pre-test measurement, a finding that is in alignment with previous studies [
69,
70]. Interestingly, ADHD children's baseline total SC scores were marginally categorised as "middle" on the psychodiagnostic chart, contradicting with Nixon’s [
71] assertion of significant social difficulties.
The study results showed similar SC scores changes for both groups, indicating that the GPT programme positively affected SC in both NON-ADHD and ADHD children. Remarkably, the post-test SC scores of the ADHD group were characterised as typical, signifying substantial achieved within the intervention’s 27-week duration. This finding is particularly encouraging, given Storebø et al.'s [
35] report of low to extremely low effectiveness for social skills training interventions targeting ADHD children aged 5-18 years, regardless of duration. The study's results and the intervention's effectiveness in a relatively short period are consistent with the findings of Wilkes-Gillan et al.'s study [
72], which employed a play-based intervention with parent- and peer-mediated components for children with ADHD aged 5-11 years. Both GPT and Wilkes-Gillan et al.'s [
72] intervention share the idea that "free child-led play is the primary occupation of children and the context which facilitates children's social development" [
73]. However, an important point of difference between the two approaches is that in GPT no video is used and feedback is given during the sessions, while recall of information concerning social situations handled by the group members is done at the awakening, i.e. at the beginning of each new session and relates to the previous sessions [
50].
In terms of children's performance on SC subscales, it appears that ADHD children particularly benefited in assertive skills, surpassing the improvements observed in NON-ADHD children. Notably, ADHD children demonstrated a baseline assertive skills score of 41, which falls marginally within the "average" range according to the psychodiagnostic chart, but lower compared to the score of 49 recorded by NON-ADHD children. Therefore, it stands to reason that they would experience a more pronounced improvement, especially given the direct targeting of parameters such as assertiveness by the physical activities utilized in the GPT program. The observed benefits extend to other subscales as well. The improvements in "interpersonal relationships" and "cooperation" for children with ADHD are significant considering their post-test score of above 40, a value that represents the lower limit of the middle category on the psychodiagnostic scale.
The observed improvement in SC among children with ADHD in the present study is a noteworthy, especially considering that these children often struggle with rule-breaking behaviour in competitive play, which can lead to rejection by their peers. The absence of competitive games in the Group Psychomotor Therapy (GPT) program design appears to have played a significant role in enhancing the SC of children with ADHD, while concurrently preserving the benefits observed in typically developing (NON-ADHD) children. Although the study was conducted in an out-of-school context, many of the principles underlying GPT can be integrated into physical education lessons, ensuring that children with ADHD are not excluded.
Regarding EC, ADHD children had lower scores than NON-ADHD children at baseline, a finding that was expected based on previous research [
74,
75]. Nevertheless, the noteworthy finding here was that both groups presented scores below 43 that indicates significant emotional difficulties and a need for referral for support. However, in the second measurement, both groups showed statistically significant improvement, with ADHD-children improving comparatively less than NON-ADHD children. Specifically, the NON-ADHD group increased their EC score to above 57, classifying them in the typical values range, while the ADHD group remained in the below 43 zone, that indicates the need for further treatment. Nevertheless, the significant benefits of both groups should not be overlooked. Positive effects in ADHD children’s EC have been reported also in studies where psychosocial interventions were applied, indicating that such interventions can have positive effects, such as reducing emotional problems, improving the regulation of negative emotions, and decreasing emotional symptoms [
76,
77].
Literature on the impact of GPT on ADHD is scarce. It is important more studies to be conducted with different group settings, in combination with other therapeutic interventions, and in comparison with other experimental groups applying different protocols. One such combination that is of particular interest and is mentioned by several therapists, although there is no research data available, is a protocol known as "inclusive exercise". That includes GPT, individual training in a sport of the participant's choice, and behavioral/psychological treatment. Future research in this area with a larger sample and a wider age range would provide a clearer picture of the impact of this protocol and would also contribute to a better understanding of how each therapeutic approach affects outcomes.
In terms of EC subscales, the low scores of the two groups in the EM both at baseline and post-test measurements should be mentioned. NON-ADHD children exhibited a baseline score below 43, with an improvement to 46.5 at the re-measurement, failing to reach the standard scores of 50 considered as average. The ADHD group demonstrated a notably low baseline score of 31.5, with an improvement to 36.8, remaining within the "low" category on the psychodiagnostic chart. This finding suggests that EM in five-year-old children may not be sufficiently developed. However, it's noteworthy that participation in GPT yielded significant benefits for both groups of children, indicating the potential of such interventions to enhance emotional regulation skills in young children.
This study presents data on therapy in children with ADHD in an inclusive environment, marking a significant contribution to the existing literature. Previous therapeutic programs mentioned in the literature so far included exclusively children with ADHD, highlighting the unique approach of this study. Furthermore, the proposed therapy cumulatively targets three areas of development that children with ADHD have difficulties with (i.e., motor, social, and emotional) providing promising outcomes. Nevertheless, this study has some limitations that should be considered when interpreting its results. A significant weakness that could not have been addressed is that in an inclusive environment, children start from different performance levels, making it difficult to interpret the effectiveness of the therapeutic program. Moreover, the absence of comparative groups undergoing different types of therapies hinders the ability to evaluate the relative effectiveness of the interventions. These limitations underscore the need for further research and consideration when drawing conclusions from this study.
The literature on the impact of GPT on ADHD is limited. There is a need for further studies across diverse group settings, incorporating various therapeutic interventions, and comparing results with other experimental groups using different protocols. A notable approach mentioned by several therapists, though lacking empirical research, is the "inclusive exercise" protocol. This protocol consists of GPT, individualized sports training tailored to the participant's preferences, as well as behavioral/ psychological treatment. Future research with larger sample sizes and a wider age range could offer a more comprehensive understanding of the impact of this protocol and contribute to the understanding of the outcomes of each therapeutic approach.
5. Conclusions
GPT yields significant benefits on the motor, social and emotional competence of both children with and without ADHD. The findings of this study underscore the efficacy of the GPT as a valuable practice, which can complement other therapeutic approaches. Furthermore, they challenge the misconception that integrating children with and without ADHD in a group setting is impractical, and importantly, dispel the notion that only children with ADHD derive benefits from such interventions.
Author Contributions
Conceptualization, A.K.; methodology, A.K. and F.V.; formal analysis, F.V.; investigation, A.K., F.V., D.K. and M.K.; data curation, F.V., D.K. and M.K.; writing—original draft preparation, A.K. and F.V.; project administration, A.K., F.V.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study because no ethics committee had been established at our university at that time. However, the research was approved by the general assembly of the department.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are only available on request from the corresponding author due to ethical reasons.
Acknowledgments
The authors express their gratitude to the families who took part in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Posner, J.; Polanczyk, G.V.; Sonug-Barke, E. Attention-deficit hyperactivity disorder. Lancet 2020, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Tayla, A.; Bowling, A.; Davison, K.; Garcia, J. Physical Activity Interventions for Children with Social, Emotional, and Behavioral Disabilities—A Systematic Review. J. Dev. Behav. Pediatr. 2017, 431–445. [Google Scholar] [CrossRef]
- Willcutt, E.G. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics 2012, 490–499. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Ghasemi, H.; Abdoli, N.; Rahmani, A.; Shiri, M.; Hashemian, A.H.; Akbari, H.; Mohammadi, M. The global prevalence of ADHD in children and adolescents: A systematic review and meta-analysis. Ital. J. Pediatr. 2023, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Atladottir, H.O.; Gyllenberg, D.; Langridge, A.; Sandin, S.; Hansen, S.N.; Leonard, H.; Gissler, M.; Reichenberg, A.; Bourke, J. The increasing prevalence of reported diagnoses of childhood neurodevelopmental disorders: A Nordic comparison. Eur. Child Adolesc. Psychiatry 2015, 173–183. [Google Scholar] [CrossRef]
- Zito, J.M.; Safer, D.J.; dosReis, S.; Gardner, J.F.; Boles, M.; Lynch, F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000, 1025–1030. [Google Scholar] [CrossRef]
- Schmidt, S.; Petermann, F. Developmental Psychopathology: Attention Deficit Hyperactivity Disorder (ADHD). BMC Psychiatry 2009, 58. [Google Scholar] [CrossRef]
- Bauermeister, J.J.; Barkley, R.A.; Smallish, L.; Martinez, J.V. ADHD and gender: Are risks and sequela of ADHD the same for boys and girls? Child Psychol. Psychiatry 2007, 831–839. [Google Scholar] [CrossRef]
- Egger, H.L.; Angold, A. Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. J. Child Psychol. Psychiatry 2006, 313–337. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Lebailly, S.A.; Hopkins, J.; Gouze, K.R.; Binns, H.J. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J. Clin. Child Adolesc. Psychol. 2009, 315–328. [Google Scholar] [CrossRef]
- Do, J.A. ADHD and behavioral disorders: Assessment, management, and an update from DSM-5. Cleve. Cleve. J. Med. 2015. [CrossRef]
- Brevik, E.J.; Lundervold, A.J.; Halmøy, A.; Posserud, M.B.; Øie, M.; Andresen, B.; Haavik, J.; Lundervold, A. Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatr. Scand. 2017, 220–227. [Google Scholar] [CrossRef]
- Beheshti, A.; Chavanon, M.-L.; Christiansen, H. ; Emotion dysregulation in adults with attention deficit hyperactivity disorder: A meta-analysis. BMC Psychiatry 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Das, D.; Cherbuin, N.; Butterworth, P.; Anstey, K.J.; Easteal, S. A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PLoS One 2012. [CrossRef] [PubMed]
- Graziano, P.A.; Garcia, A. Attention-deficit hyperactivity disorder and children's emotion dysregulation: A meta-analysis. Clin. Psychol. Rev. 2016, 106–123. [Google Scholar] [CrossRef] [PubMed]
- Ros, R.; Graziano, P.A. Social functioning in children with or at risk for attention deficit/hyperactivity disorder: A meta-analytic review. J. Clin. Child Adolesc. Psychol. 2017, 213–235. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders, 4th edn. Washington, DC: American Psychiatric Association, 2000.
- Kuriyan, A.B.; Pelham, W.E.; Molina, B.S.G.; Waschbusch, D.A.; Gnagy, E.M.; Sibley, M.H.; Biswas, A.; Babinski, D.E.; Coles, E.K. Young adult educational and vocational outcomes of children diagnosed with ADHD. J. Abnorm. Child Psychol. 2013, 27–41. [Google Scholar] [CrossRef]
- Kirino, E.; Imagawa, H.; Goto, T.; Montgomery, W. Sociodemographics, comorbidities, healthcare utilization and work productivity in Japanese patients with adult ADHD. PLoS One 2015. [CrossRef]
- Campbell, S.B.; Spieker, S.; Burchinal, M.; Poe, M.D. Trajectories of aggression from toddlerhood to age 9 predict academic and social functioning through age 12. J. Child Psychol. Psychiatry 2006, 791–800. [Google Scholar] [CrossRef]
- Landry, S.H.; Smith, K.E. Early social and cognitive precursors and parental support for self-regulation and executive function: Relations from early childhood into adolescence. In Sokol, B.W.; Müller, U.; Carpendale, J.I.M.; Young, A.R.; Iarocci, G. (Eds.), Self and Social Regulation: Social Interaction and the Development of Social Understanding and Executive Functions; Oxford University Press, 2010, 386-417. [CrossRef]
- Rose-Krasnor, L.; Denham, S. Social-emotional competence in early childhood. In Handbook of Peer Interactions, Relationships, and Groups; Bukowski, W.M.; Laursen, B.; Rubin, K.H., Eds.; The Guilford Press, 2009, 162-179.
- Pagani, L.S.; Fitzpatrick, C.; Archambault, I.; Janosz, M. School readiness and later achievement: A French Canadian replication and extension. Dev. Psychol. 2010, 984–994. [Google Scholar] [CrossRef]
- Pritchard, V.E.; Bora, S.; Austin, N.C.; Levin, K.J.; Woodward, L.J. Identifying very preterm children at educational risk using a school readiness framework. Pediatrics 2014, e825–e832. [Google Scholar] [CrossRef] [PubMed]
- Charach, A.; Carson, P.; Fox, S.; Ali, M.U.; Becket, J.; Li, C.G. Interventions for preschool children at high risk for ADHD: A comparative effectiveness review. Pediatrics 2013, e1584–e1604. [Google Scholar] [CrossRef] [PubMed]
- Cardoso-Moreno, M.J.; Tomás-Aragonés, L.; Rodríguez-Ledo, C. Socio-emotional intervention in attention deficit hyperactivity disorder. Eur. J. Educ. Psychol. 2015, 53–59. [Google Scholar] [CrossRef]
- Chirdkiatgumchai, V.; Xiao, H.; Fredstrom, B.K.; Adams, R.E.; Epstein, J.N.; Shah, S.S.; Brinkman, W.B.; Kahn, R.S.; Froehlich, T.E. National trends in psychotropic medication use in young children: 1994–2009. Pediatrics 2013, 515–623. [Google Scholar] [CrossRef]
- Ng, Q.X. A systematic review of the use of bupropion for attention-deficit/hyperactivity disorder in children and adolescents. J. Child Adolesc. Psychopharmacol. 2017, 112–116. [Google Scholar] [CrossRef]
- Pliszka, S. Practice Parameter for the Assessment and Treatment of Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. J. Am. Acad. Child Adolesc. Psychiatry, 1097. [Google Scholar]
- Centers for Disease Control and Prevention. Attention-Deficit/Hyperactivity Disorder: Data & statistics. 2016.
- Wolraich, M.; Brown, L.; Brown, R.T.; DuPaul, G.; Earls, M.; Feldman, H.M.; Ganiats, T.G.; Kaplanek, B.; Meyer, B.; Perrin, J.; Pierce, K.; Reiff, M.; Stein, M.T.; Visser, S. ADHD: Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics 2011, 1007–1022. [Google Scholar] [CrossRef]
- Bachmann, C.J.; Wijlaars, L.P.; Kalverdijk, L.J.; Burcu, M.; Glaeske, G.; Schuiling-Veninga, C.C.; Hoffmann, F.; Aagaard, L.; Zito, J.M. Trends in ADHD medication use in children and adolescents in five western countries, 2005–2012. Eur. Neuropsychopharmacol. 2017, 27, 484–493. [Google Scholar] [CrossRef]
- Mohammadi, M.R.; Akhondzadeh, S. Pharmacotherapy of attention-deficit/hyperactivity disorder: Nonstimulant medication approaches. Expert Rev. Neurother. 2007, 195–201. [Google Scholar] [CrossRef]
- Hoza, B.; Gerdes, A.C.; Mrug, S.; Hinshaw, S.P.; Bukowski, W.M.; Gold, J.A.; Arnold, L.E.; Abikoff, H.B.; Conners, C.K.; Elliott, G.R.; Greenhill, L.L.; Hechtman, L.; Jensen, P.S.; Kraemer, H.C.; March, J.S.; Newcorn, J.H.; Severe, J.B.; Swanson, J.M.; Vitiello, B.; Wells, K.C.; Wigal, T. Peer-Assessed Outcomes in the Multimodal Treatment Study of Children With Attention Deficit Hyperactivity Disorder. J. Clin. Child Adolesc. Psychol. 2005, 74–86. [Google Scholar] [CrossRef]
- Storebø, O.J.; Andersen, M.E.; Skoog, M.; Hansen, S.J.; Simonsen, E.; Pedersen, N.; Tendal, B.; Callesen, H.E.; Faltinsen, E.; Gluud, C. Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database Syst. Rev. 2019. [CrossRef]
- Jensen, P.S.; Arnold, L.E.; Swanson, J.M.; Wigal, T.; Gibbons, R.D.; Hur, K. 3-Year Follow-up of the NIMH MTA Study. J. Am. Acad. Child Adolesc. Psychiatry 2007, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Visser, S.N.; Bitsko, R.H.; Danielson, M.L.; Ghandour, R.M.; Blumberg, S.J.; Schieve, L.A.; Holbrook, J.R.; Wolraich, M.L.; Cuffe, S.P. Treatment of Attention Deficit/Hyperactivity Disorder among Children with Special Health Care Needs. J. Pediatr. 2015, 1423–1430. [Google Scholar] [CrossRef] [PubMed]
- Chronis, A.M.; Jones, H.A.; Raggi, V.L. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clin. Psychol. Rev. 2006, 486–502. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Daley, D.; Hutchings, J.; Bywater, T.; Eames, C. Efficacy of the Incredible Years Basic parent training programme as an early intervention for children with conduct problems and ADHD. Child Care Health Dev. 2007, 749–756. [Google Scholar] [CrossRef]
- Jones, K.; Daley, D.; Hutchings, J.; Bywater, T.; Eames, C. Efficacy of the Incredible Years Programme as an Early Intervention for Children with Conduct Problems and ADHD: Long-Term Follow-Up. Child Care Health Dev. 2008, 3, 380–390. [Google Scholar] [CrossRef]
- Kamp, C.F.; Sperlich, B. ; Holmberg, H-C. Exercise reduces the symptoms of attention-deficit/hyperactivity disorder and improves social behaviour, motor skills, strength and neuropsychological parameters. Acta Paediatr. 2014, 709–714. [Google Scholar] [CrossRef]
- Piepermeier, A.T.; Etnier, J.L.; Zebas, C.J.; Saliba, S.A. The effect of acute exercise on cognitive performance in children with and without ADHD. J. Sport Health Sci. 2015, 97–104. [Google Scholar] [CrossRef]
- Verret, C.; Guay, M.-C.; Berthiaume, C.; Gardiner, P.; Beliveau, L. A physical activity program improves behavior and cognitive functions in children with ADHD: An exploratory study. J. Atten. Disord. 2012, 71–80. [Google Scholar] [CrossRef]
- Chang, Y-K. ; Liu, S.; Yu, H-H.; Lee, Y-H. Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Arch. Clin. Neuropsychol. 2012, 225–237. [Google Scholar] [CrossRef]
- Piek, J.P.; McLaren, S.; Kane, R.; Jensen, L.; Dender, A.; Roberts, C.; Rooney, R.; Packer, T.; Straker, L. Does the Animal Fun program improve motor performance in children aged 4–6 years? Mov. Sci. 2013, 1086–1096. [Google Scholar] [CrossRef]
- Zang, Y. Impact of physical exercise on children with attention deficit hyperactivity disorders. Medicine 2019, e17980. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Gao, X.; Song, Y.; Zhu, X.; Chen, M.; Yang, L.; Ren, Y. Effectiveness of physical activity intervention on ADHD symptoms: A systematic review and meta-analysis. Syst. Rev. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Probst, M.; Knapen, J.; Poot, G.; Vancampfort, D. Psychomotor therapy and psychiatry: What’s in a name? Med. J. 2010, 2. [Google Scholar] [CrossRef]
- Foulds, M.L.; Hannigan, P.S. Effects of psychomotor group therapy on ratings of self and others. Psychother. Theory Res. Pract. 1974, 11, 351–353. [Google Scholar] [CrossRef]
- Kambas, A.; Venetsanou, F. Group Psychomotor Therapy in children. Eur. Psychomotricity J. 2022, 1–4. [Google Scholar]
- Zimmer, R. Handbuch der Psychomotorik: Theorie und Praxis der psychomotorischen Förderung von Kindern. Freiburg: Herber, 2006.
- Axline, V.M. Play Therapy. New York, NY: Ballantine Books, 1974.
- Knell, S.M. Cognitive-behavioral play therapy. J. Clin. Child Psychol. 1998, 27, 28–33. [Google Scholar] [CrossRef]
- Yalom, I.D.; Leszcz, M. The Theory and Practice of Group Psychotherapy, 5th ed. Basic Books/Hachette Book Group, 2005.
- Marouli, A.; Papavasileiou, G.E.; Dania, A.; Venetsanou, F. Effect of a psychomotor program on the motor proficiency and self-perceptions of preschool children. J. Phys. Educ. Sport 2016, 16, 1365. [Google Scholar] [CrossRef]
- Kouli, O.; Avloniti, A.; Venetsanou, F.; Giannakidou, D.; Gazi, D.; Kambas, A. The effect of a psychomotor training program on the motor proficiency of preschool children in a multicultural environment. Eur. Psychomotricity J. 2010, 31–36. [Google Scholar]
- Zimmer, R.; Christoforidis, Ch.; Xanthi, P.; Aggeloussis, P.; Kambas, A. The effects of a psychomotor training program on motor proficiency of Greek preschoolers. Eur. Psychomotricity J. 2008, 3–9. [Google Scholar]
- ElGarhy, S.; Liu, T. Effects of psychomotor intervention program on students with autism spectrum disorder. Sch. Psychol. Q. 2016, 491–506. [Google Scholar] [CrossRef]
- Kambas, A.; Venetsanou, F.; Gavriilidou, Z. Fisiki Drasthriotita & Psixokinhtikh sthn prosxolikh hlikia. Athens: Gutenberg, 2019.
- Gkotzia, E.; Venetsanou, F.; Kambas, A.; Pollatou, E. Construct validity of the Democritos Movement Screening Tool for preschool children: An examination of the known groups’ criterion. Eur. Psychomotricity J. 2016, 8, 17–28. [Google Scholar]
- Kambas, A.; Venetsanou, F. The Democritos Movement Screening Tool for preschool children (DEMOST-PRE©): Development and factorial validity. Res. Dev. Disabil. 2014, 35, 1528–1533. [Google Scholar] [CrossRef] [PubMed]
- Kambas, A.; Venetsanou, F. Construct and concurrent validity of the Democritos Movement Screening Tool for preschoolers. Pediatr. Phys. Ther. 2016, 28, 94–99 101097/PEP0000000000000206. [Google Scholar] [CrossRef] [PubMed]
- Chatzichristou, C.; Polychronis, F.; Bezevegis, H.; Mylonas, K. Psychosocial Test Adjustment for preschool and school-age children. 2008.
- Hatzichristou, C.; Polychroni, F.; Besevegis, E.; Mylonas, K. Examination of developmental characteristics of school and psychosocial adjustment of preschool and school aged children according to the standardized test of Psychosocial Adjustment. Psychol. J. Hellenic Psychol. Soc. 2011.
- Wolraich, M.L.; Hagan, J.F. Jr.; Allan, C.; Chan, E.; Davison, D.; Earls, M.; Evans, S.W.; Flinn, S.K.; Froehlich, T.; Frost, J.; Holbrook, J.R.; Lehmann, C.U.; Lessin, H.R.; Okechukwu, K.; Pierce, K.L.; Winner, J.D.; Zurhellen, W. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics 2019, 144. [Google Scholar] [CrossRef]
- Hyde, C.; Fuelscher, I.; Sciberras, E.; Efron, D.; Anderson, V.A.; Silk, T. Understanding motor difficulties in children with ADHD: A fixel-based analysis of the corticospinal tract. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021. [CrossRef]
- Fliers, E.A.; de Hoog, M.L.; Franke, B.; Faraone, S.V.; Rommelse, N.N.; Buitelaar, J.K.; Nijhuis-van der Sanden, M.W. Actual motor performance and self-perceived motor competence in children with ADHD compared to healthy siblings and peers. J. Dev. Behav. Pediatr. 2010, 35–40. [Google Scholar] [CrossRef]
- Kaiser, M.-L.; Schoemaker, M.M.; Albaret, J.-M.; Geuze, R.H. What is the evidence of impaired motor skills and motor control among children with attention deficit hyperactivity disorder (ADHD)? Systematic review of the literature. Res. Dev. Disabil. 2015, 338–357. [Google Scholar] [CrossRef]
- De Boo, G.M.; Prins, P.J.M. Social incompetence in children with ADHD: Possible moderators and mediators in social-skills training. Clin. Psychol. Rev. 2007, 78–97. [Google Scholar] [CrossRef]
- Mrug, S.; Hoza, B.; Gerdes, A.C. Children with Attention-Deficit/Hyperactivity Disorder: Peer relationships and peer-oriented interventions. New Dir. Child Adolesc. Dev. 2001, 51–77. [Google Scholar] [CrossRef]
- Nixon, E. The social competence of children with Attention Deficit Hyperactivity Disorder: A review of the literature. Child Psychol. Psychiatry Rev. 2001, 6, 172–180. [Google Scholar] [CrossRef]
- Wilkes-Gillan, S.; Bundy, A.; Cordier, R.; Lincoln, M.; Chen, Y.-W. A randomized controlled trial of a play-based intervention to improve the social play skills of children with Attention Deficit Hyperactivity Disorder (ADHD). PLoS One 2016, 1–22. [Google Scholar] [CrossRef]
- Parham, L.D.; Cohn, E.S.; Spitzer, S.; Koomar, J.A.; Miller, L.J.; Burke, J.P.; Brett-Green, B.; Mailloux, Z.; May-Benson, T.A.; Roley, S.S.; Schaaf, R.C.; Schoen, S.A.; Summers, C.A. Fidelity in sensory integration intervention research. Am. J. Occup. Ther. 2007, 61, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Kats-Gold, B.; Priel, I. Emotion, understanding, and social skills among boys at risk of Attention Deficit Hyperactivity Disorder. Psychol. Sch. 2009, 658–678. [Google Scholar] [CrossRef]
- Jogsan, Y.A. Emotional maturity and adjustment in ADHD children. J. Psychol. Psychother. 2013, 1–4. [Google Scholar] [CrossRef]
- Hannesdottir, D.K.; Ingvarsdottir, E.; Bjornsson, A. The OutSMARTers program for children with ADHD: A pilot study on the effects of social skills, self-regulation, and executive function training. J. Atten. Disord. 2017, 21, 353–364. [Google Scholar] [CrossRef]
- Sánchez, M.; Lavigne, R.; Romero, J.F.; Elósegui, E. Emotion regulation in participants diagnosed with Attention Deficit Hyperactivity Disorder, before and after an emotion regulation intervention. Front. Psychol. 2019, 10, 1092. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).