1. Introduction
Myocarditis is the inflammatory injury of the myocardium, resulting in symptoms and electrocardiographic changes similar to acute coronary syndromes (ACS). It is a rare condition and affects approximately 4 to 14 of 100 000 people globally in a year [
1].
Electrocardiogram (ECG) in case of myocarditis may suggest the pattern of ST segment elevation myocardial infarction (STEMI) or non-ST segment elevation myocardial infarction (NSTEMI), and together with elevated blood cardiac troponins concentration and similar symptoms imitates ACS [
2]. ST segment elevation in presence of myocarditis refers to diagnostical challenges. Although, there are some factors suggesting that patient is presented with myocarditis – these patients are younger (usually less than 40 years old), had recent viral infection, ECG changes involves more than one vascular territory and diffuse or absent wall motion abnormalities on echocardiogram [
3].
NSTEMI pattern is less frequent in case of myocarditis [
4], but it remains unclear if presence of ST segment elevation in case of myocarditis is related to more severe condition and more damage in myocardium, even though ST segment elevation might suggest more aggressive course of the disease. As there are limited studies evaluating clinical differences and severity of the myocarditis due to ECG pattern, we aimed to evaluate differences between myocarditis patients in our centre.
As for future perspectives, studies like this might help to predict the course of the myocarditis based by ECG pattern and lead to more accurate treatment and monitoring options for these patients. Evaluation of differences between different ECG patterns might suggest more approachable course of management for these patients. Also, there are limited evidence for the prognostic predictors in case of the myocarditis [
5], with a longer and more standartised follow-up period, ECG pattern might become one more prognostic factor for the outcomes.
The subject of this study was to evaluate and compare epidemiology, laboratory and instrumental tests results of the patients with myocarditis and STEMI pattern to those without STEMI pattern.
2. Materials and Methods
2.1. Study Design and Population
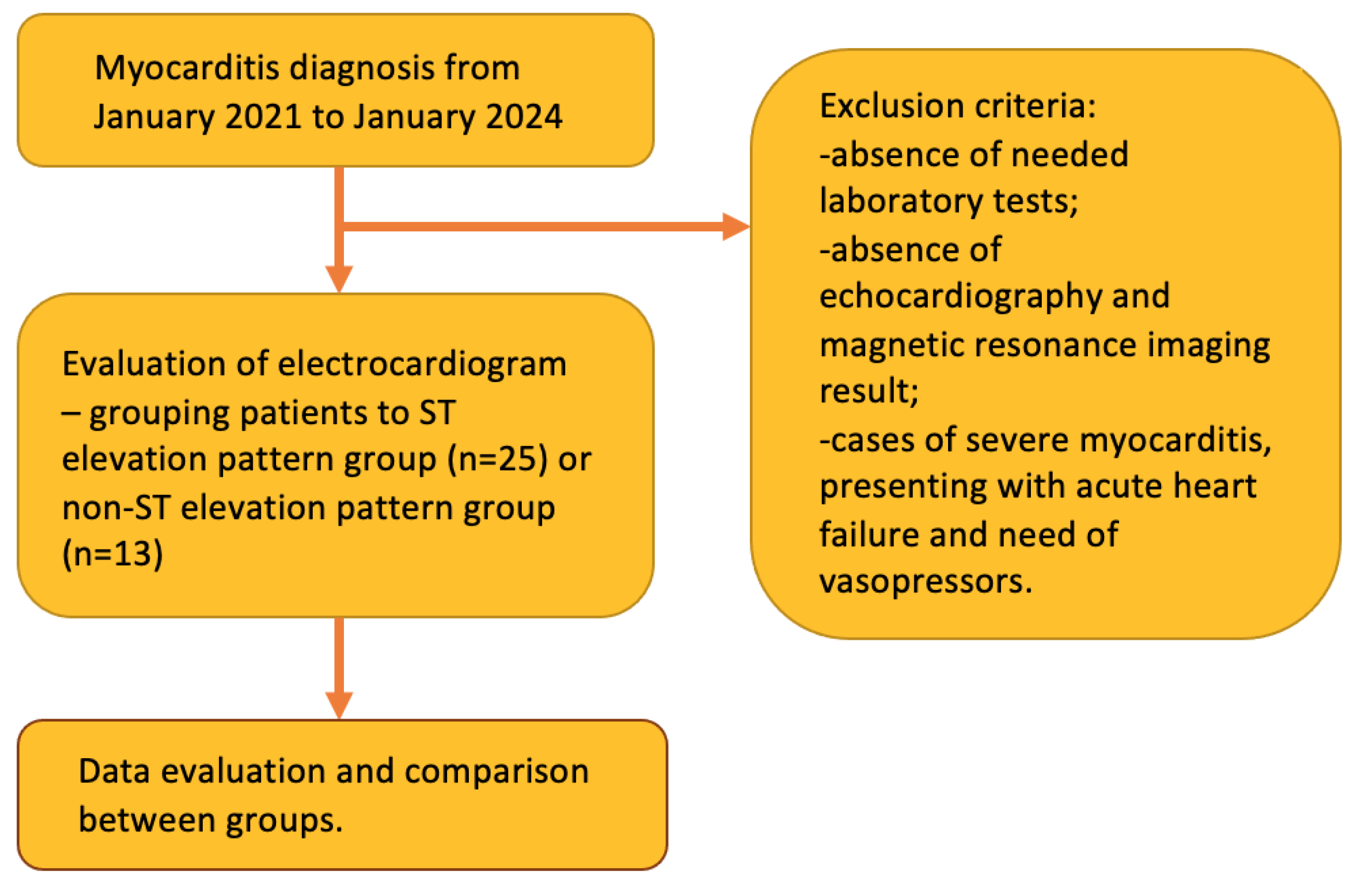
This was a retrospective study, involving 38 patients, admitted to our hospital with myocarditis between January 2021 and January 2024. Study design is shown in
Figure 1. Patients were enroled based by the ICD-10 classification codes I40.0, I40.1, I40.8, I40.9 and then evaluated based by inclusion and exclusion criteria, mentioned below. All patients included had ECG performed, laboratory tests, including troponin I (TnI) levels at the time of the admission and at the time of the discharge, C-reaactive protein (CRP) levels at the time of admission and at the time of the discharge, creatinine concentration, complete blood count (CBC), brain natriuretic peptide levels (BNP), performed. Also, all of the included patients had echocardiography and cardiac magnetic resonance imaging (MRI) performed during their hospitalisation. All cases of myocarditis were confirmed by MRI. Follow-up echocardiography during the period of six months after the discharge was evaluated too. The methods of treatment were also assessed. Patients were divided into two groups – first group were patients with ST segment elevation pattern in ECG (25) and second group were patients without ST segment elevation pattern (13).
2.2. Inclusion and Exclusion Criteria
Inclusion criteria were age over 18 years, diagnosis of myocarditis in clinical history, based by ICD-10 classification, and presence of laboratory tests (TnI, CRP, BNP, creatinine, CBC), echocardiography results and diagnosis of myocarditis confirmed by heart MRI. Exclusion criteria were absence of needed laboratory and instrumental tests, no evidence of myocarditis during cardiac MRI and cases of severe myocarditis, presenting with acute heart failure and need of vasopressors. We excluded these patients in order to evaluate mild and most usual form of myocarditis.
2.3. Data Collection
All of the data was collected retrospectively from medical history, available through hospital data systems. Data collected was epidemiological data, clinical symptoms, laboratory test results (TnI, CRP, BNP, creatinine concentration, CBC) at the time of admission and at the time of the discharge, echocardiographic and heart magnetic resonance imaging (MRI) data during admission and echocardiographic data at 6 months follow-up after the discharge.
2.4. Statistical Data Analysis
Data was analysed using IBM SPSS Statistics v26.0. Data distribution was assessed using Smirnov-Kolmogorov test – all of the data was distributed normally. Parametrical quantitative data was presented as mean with standart deviation. Parametrical comparative data was assessed using Student T-test and paired samples T-test. Numeric data was presented as numbers and percentages. Categorical variables were expressed as absolute numbers (percentages) and compared using the χ2 test. Correlations were evaluated using Pearson’s correlation coefficient. A p value <0,05 was concerned as statistically significant data.
3. Results
3.1. Epidemiological and Clinical Differences
38 patients were included – 25 of them were assigned to ST segment elevation (STE) pattern group and 13 patients were assigned to group without STE pattern (non-STE pattern group). There were significantly more men in both groups – 96.00% in STE pattern group and 69.23% in non-STE pattern group (p=0.038). Patients in non-STE pattern group were significantly more obese (body mass index (BMI) 25.78±3.95 in STE group vs 29.05±5.39, p=0.049), but this has no clinical significance. All of the admitted patients had chest pain as a symptom, presence of infection (recent or ongoing) was significantly more often in STE pattern group (84.00% vs 46.15%, p=0.024). All epidemiological and clinical differences between groups are shown in
Table 1.
3.2. Laboratory Tests Comparison
Laboratory test differences were also assessed – there were higher TnI and BNP levels in STE pattern group, but these differences were not statistically significant. There were significantly higher CRP levels in STE pattern group (103.40±82.04mg/l vs 43.54±61.93mg/l, p = 0.017). TnI levels and CRP levels at the discharge were also evaluated. There were significantly lower CRP levels at the discharge in non-STE pattern group (12.02 ± 10.82mg/l vs 7.10 ± 3.62mg/l, p = 0.002). Other laboratory tests did not differ significantly between the groups. Differences between laboratory test results are shown in
Table 2.
TnI and CRP levels were assessed at the admission – the maximal TnI level and at the time of the discharge and CRP at the admission and at the time of the discharge. There were significantly lower rates of TnI and CRP concentrations at the discharge, evaluating all of the study population regardless of ECG pattern (p = 0.010 and p<0.001, accordingly). The results are shown in
Table 3.
There was a moderate correlation between higher levels of TnI and higher levels of BNP (r = 0.566, p = 0.002). Discharge TnI moderate correlated positively with discharge CRP levels (r = 0.516, p = 0.004).
3.3. Echocardiographical Differences
All of the admitted patients underwent echocardiography. Right ventricle (RV) function was normal in all included patients. Left ventricle ejection fraction (LVEF) was significantly higher in non-STE pattern group (49.71±4.14 vs 56.58±3.99, p<0.001). Other echocardiographic data did not differ significantly between the groups. Echocardiographic differences between groups are shown in
Table 4.
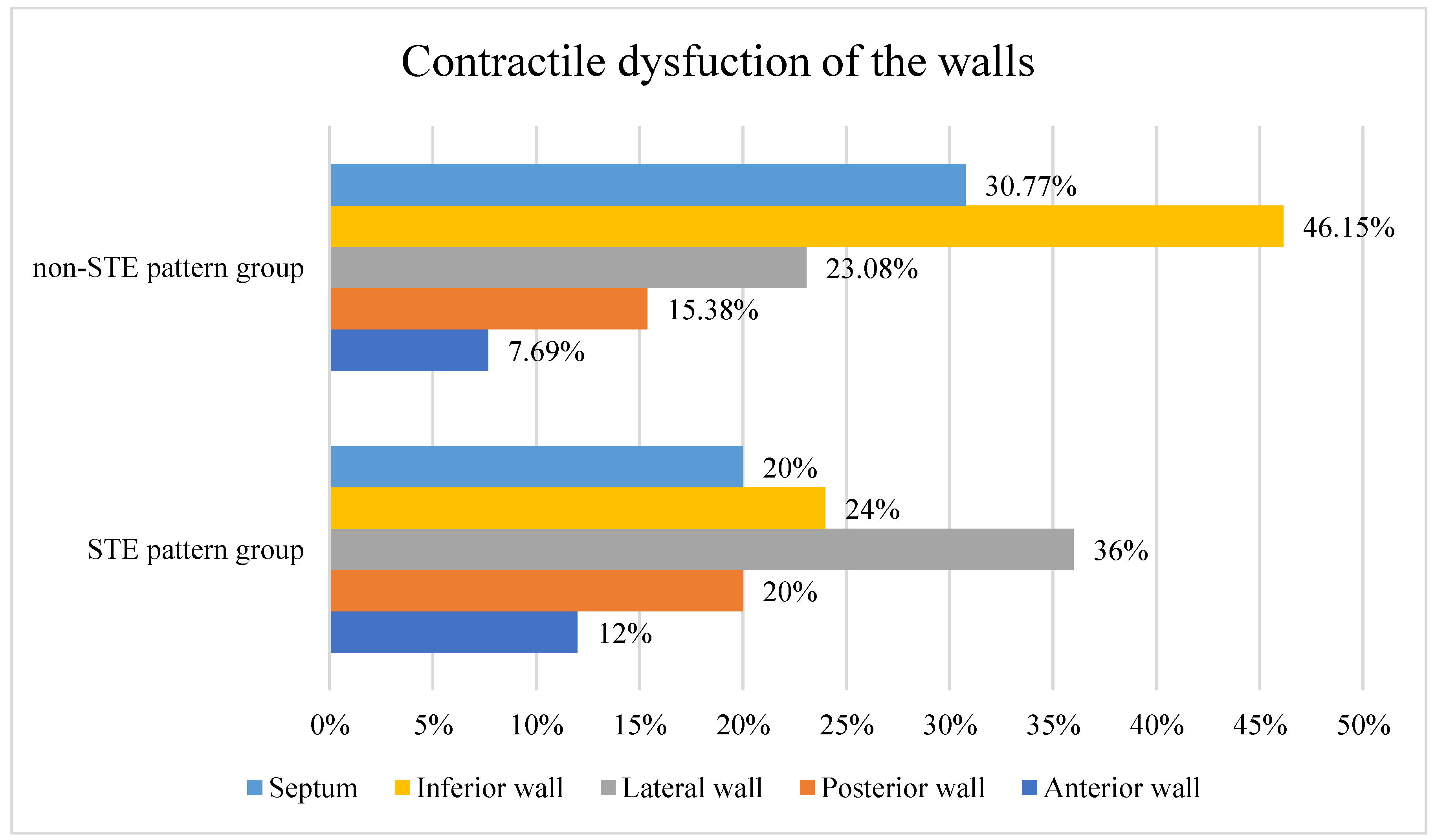
Contractile function was dispaired for 9 (69.23%) patients in non-STE pattern group and for 15 (65.21%) patients in STE pattern group (p=1.000). The results by the location of dysfunction are shown in
Figure 2.
Although there were no significant echocardiographic differences between the groups, there were correlations with other parameters. Higher left ventrical end diastolic diameter (LVEDD) weakly correlates with lower S’ (r = -0.361, p = 0.033). LVEF correlated with BMI – there was a weak correlation between lower LVEF and higher BMI (r = -0.354, p = 0.040). Lower LVEF also correlated with higher TnI levels (r= -0.353, p=0.032), but this correlation was also weak. There was moderate correlation between lower LVEF and higher CRP levels (r = -0.554, p<0.001). There was a strong correlation between lower left ventricle strain and higher levels of TnI (r = -0.641, p = 0.013).
3.4. Heart Magnetic Resonance Imaging Differences between the Groups
Heart MRI results did not differ significantly between the groups. Differences between main parameters are shown in
Table 5. In all of the included cases, myocarditis diagnosis was confirmed by heart MRI.
There was a moderate correlation between lower LVEF based by MRI and higher TnI concentration (r = -0.479, p = 0.003). Also, moderate correlation was between higher TnI value and higher left ventricle end-systolic volume (r = 0.418, p = 0.011).
3.5. Treatment Differences
Treatment was also compared between groups. Treatment strategy included a few options – no specific treatment at all, only symptomatic treatment (infusions, antipyretics); only antibiotics; optimal heart failure treatment; only beta-adrenoblockers; antibiotics and optimal heart failure treatment. Significantly more patients were prescribed antibiotics and heart failure medications in STE pattern group, however, more patients were prescribed heart failure treatment in non-STE pattern group (p=0.008). The results are shown in
Table 6.
3.6. 6 Months Echocardiographical Follow-Up
At six months follow-up echocardiography results were assessed. In study population, despite of the ECG pattern, LVEF during follow-up was improved, although this data was not statistically significant (52.27±5.59% during the admission and 55.45±2.69% at follow-up, p = 0.064).
4. Discussion
Myocarditis could present in a lot of different clinical appearances – it could have asymptomatic course, heart failure (HF) symptoms, symptoms of ACS or cardiogenic shock [
6]. Most of the patients of our study were admitted to the hospital because of the symptoms of ACS – all of them had acute chest pain, ECG and laboratory tests findings similar to ACS. We excluded patients, which were admitted with cardiogenic shock and treated in intensive care unit, because we wanted to evaluate a mild and the most usual form of myocarditis.
In patients, who are admitted to the hospital with ACS like symptoms and test results it is important to asses ECG changes – whether there is ST segment elevation in ECG or not. Our findings suggest that in case of myocarditis ST segment elevation in ECG predicts more damage in myocardium – these patients had lower LVEF, and higher CRP levels. As previous studies has shown – higher CRP levels correlates with the extent of myocardial damage [
7]. Also, patients in ST segment elevation group had insignificantly higher TnI levels – higher TnI levels correlated with lower LV strain and lower LVEF – that predicts more damage in the myocardium. Multiple clinical studies demonstrated, that elevation in TnI levels, in the absence of myocardial infarction, have an impact on long-term prognosis, are associated with cardiovascular related events and negatively impact survival [
8]. Elevated TnI levels may be considered as an important prognostic marker, and lead to more adequate treatment in every single case of myocarditis [
9].
In case of myocarditis with LVEF ≤50% and stable hemodynamics, it is recommended to prescribe usual guidelines recommended HF treatment. Betablockers should be considered for all patients with myocarditis, because of their antiarrhythmic mechanism – to prevent ventricular events [
10]. Antibiotics are only recommended if there is active infection of other cause, as myocarditis is usually caused by a viral infection [
11]. In our study group, patients in ST segment elevation group were prescribed more aggressive treatment – more usual they had signs of other infections and were prescribed antibiotics, also in this group there were more patients with lower LVEF – HF treatment was prescribed more in this group.
In our patients population there were no patients, who had endomyocardial biopsy (EMB) performed. This was due to mild forms of myocarditis – as American Heart Association/American Heart College recommend – EMB should be performed if patient is hemodynamically unstable, has high-degree atrioventricular block or symptomatic ventricular tachycardia [
12]. EMB could be considered in case of unclear diagnosis too [
12], as it helps to find the exact cause of the disease and exclude or confirm myocarditis diagnosis and its fenotype. Furthermore, all cases of myocarditis in our study group were confirmed by MRI, so there were no need to confirm diagnosis using interventional methods.
Patients, who had myocarditis should sustain sports or intense physical activities for 3 to 6 months after the diagnosis. After these months patients should undergo follow-up examinations – including echocardiography or MRI. Follow-up echocardiography in our study group had shown improved LVEF and these findings lead to good prognosis for these patients. This may be due to mild - intermediate form of myocarditis in our patients group. Patients in case of myocarditis could have a partial or full recovery and this relies on a few predictors – poor outcome predictors could be acute HF at the onset, ventricular arrhythmias, persistent abnormal levels of TnI, reduced LVEF and reduced LV strain with no improvement at follow-up [
13].
As for future perspectives, studies like this might help to predict the course of the myocarditis based by ECG pattern and lead to more accurate treatment and monitoring options for these patients from the very beginning of their hospitalisation. As ECG is a simple and approachable test method, nowadays it is usually underestimated. Future findings in differences between various ECG patterns in myocarditis patients might help to improve the care of these patient and help to establish a more accurate follow-up options. As the new abilities to evaluate ECG emerges, like artificial inteligence, there are a lot more options to evaluate even subclinical ECG changes, that leads to more accurate diagnostics and prediction based by ECG [
14].
5. Conclusions
In case of myocarditis, mimicking ST segment elevation myocardial infarction, the LVEF is lower comparing to patients, who had myocarditis without ST segment elevation in ECG. Also, ST segment elevation was associated with higher CRP levels. Higher TnI levels in case of myocarditis were associated with lower LV strain and lower LVEF, higher CRP levels also correlated with lower LVEF. Patients with ST segment elevation more usually were prescribed heart failure treatment and antibiotics. Based by 6 months echocardiographic follow-up – the prognosis of myocarditis is favorable.
6. Limitations
Limitations of this study are relatively small study population and possible variations in the echocardiography. As this was a retrospective study, echocardiography was performed based on standartised hospital algorithm and due to restropective nature of the study, there were no abbility to standartise examination protocol for the myocarditis patients.
Author Contributions
Conceptualization, V.M.; methodology, V.M., G.R., K.A.O.; validation, G.R., K.A.O., V.M.; formal analysis, G.R.; investigation, G.R.; resources, V.M., G.R.; data curation, G.R., K.A.O..; writing—original draft preparation, G.R.; writing—review and editing, G.R., V.M.; visualization, G.R.; supervision, V.M.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by Ethics Committee of Lithuanian University of Health Sciences (protocol code 2024-BEC2-697, date of approval 2024-05-20).
Informed Consent Statement
Patient consent was waived due to retrospective nature of the study – all data was gathered retrospectively and do not involve any details, by which the patients could be identified.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. Journal of the American College of Cardiology. 2020 Dec;76(25):2982–3021. doi:10.1016/j.jacc.2020.11.010.
- Ammirati E, Moslehi JJ. Diagnosis and Treatment of Acute Myocarditis. JAMA. 2023 Apr 4;329(13):1098. doi: 10.1001/jama.2023.3371.
- Caforio ALP, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal. 2013 Jul 3;34(33):2636–48. doi: https://doi.org/10.1093/eurheartj/eht210.
- Buttà C, Zappia L, Laterra G, Roberto M. Diagnostic and prognostic role of electrocardiogram in acute myocarditis: A comprehensive review. Annals of Noninvasive Electrocardiology. 2019 Nov 28;25(3). doi: https://doi.org/10.1111/anec.12726.
- Piccirillo F, Watanabe M, Di Sciascio G. Diagnosis, treatment and predictors of prognosis of myocarditis. A narrative review. Cardiovascular Pathology. 2021 Sep;54:107362. doi: 10.1016/j.carpath.2021.107362.
- Biesbroek PS, Beek AM, Germans T, Niessen HWM, van Rossum AC. Diagnosis of myocarditis: Current state and future perspectives. International Journal of Cardiology. 2015 Jul;191:211–9. doi: https://doi.org/10.1016/j.ijcard.2015.05.008.
- Goitein O, Sabag A, Koperstein R, Hamdan A, Di Segni E, Konen E, et al. Role of C reactive protein in evaluating the extent of myocardial inflammation in acute myocarditis. Journal of Cardiovascular Magnetic Resonance. 2015 Feb 3;17(S1). doi: https://doi.org/10.1186/1532-429x-17-s1-p291.
- Chapman AR, Adamson PD, Shah ASV, Anand A, Strachan FE, Ferry AV, et al. High-Sensitivity Cardiac Troponin and the Universal Definition of Myocardial Infarction. Circulation. 2020 Jan 21;141(3):161–71.
- Chaulin AM. Elevation Mechanisms and Diagnostic Consideration of Cardiac Troponins under Conditions Not Associated with Myocardial Infarction. Part 1. Life. 2021 Sep 2;11(9):914. doi: https://doi.org/10.3390/life11090914.
- Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy. Circulation: Heart Failure. 2020 Nov;13(11). doi: https://doi.org/10.1161/circheartfailure.120.007405.
- Blauwet LA, Cooper LT. Antimicrobial agents for myocarditis: target the pathway, not the pathogen. Heart. 2009 Jul 16;96(7):494–5. doi: https://doi.org/10.1136/hrt.2009.173740.
- Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, et al. Recognition and Initial Management of Fulminant Myocarditis. Circulation. 2020 Feb 11;141(6). doi: https://doi.org/10.1161/cir.0000000000000745.
- Piccirillo F, Watanabe M, Di Sciascio G. Diagnosis, treatment and predictors of prognosis of myocarditis. A narrative review. Cardiovascular Pathology. 2021 Sep;54:107362. doi: https://doi.org/10.1016/j.carpath.2021.107362.
- Attia ZI, Harmon DM, Behr ER, Friedman PA. Application of artificial intelligence to the electrocardiogram. European Heart Journal. 2021 Sep 17;42(46):4717–30. doi: https://doi.org/10.1093/eurheartj/ehab649.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).