Submitted:
22 September 2024
Posted:
24 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Data Collection Methods
2.4. Data Analysis Methods
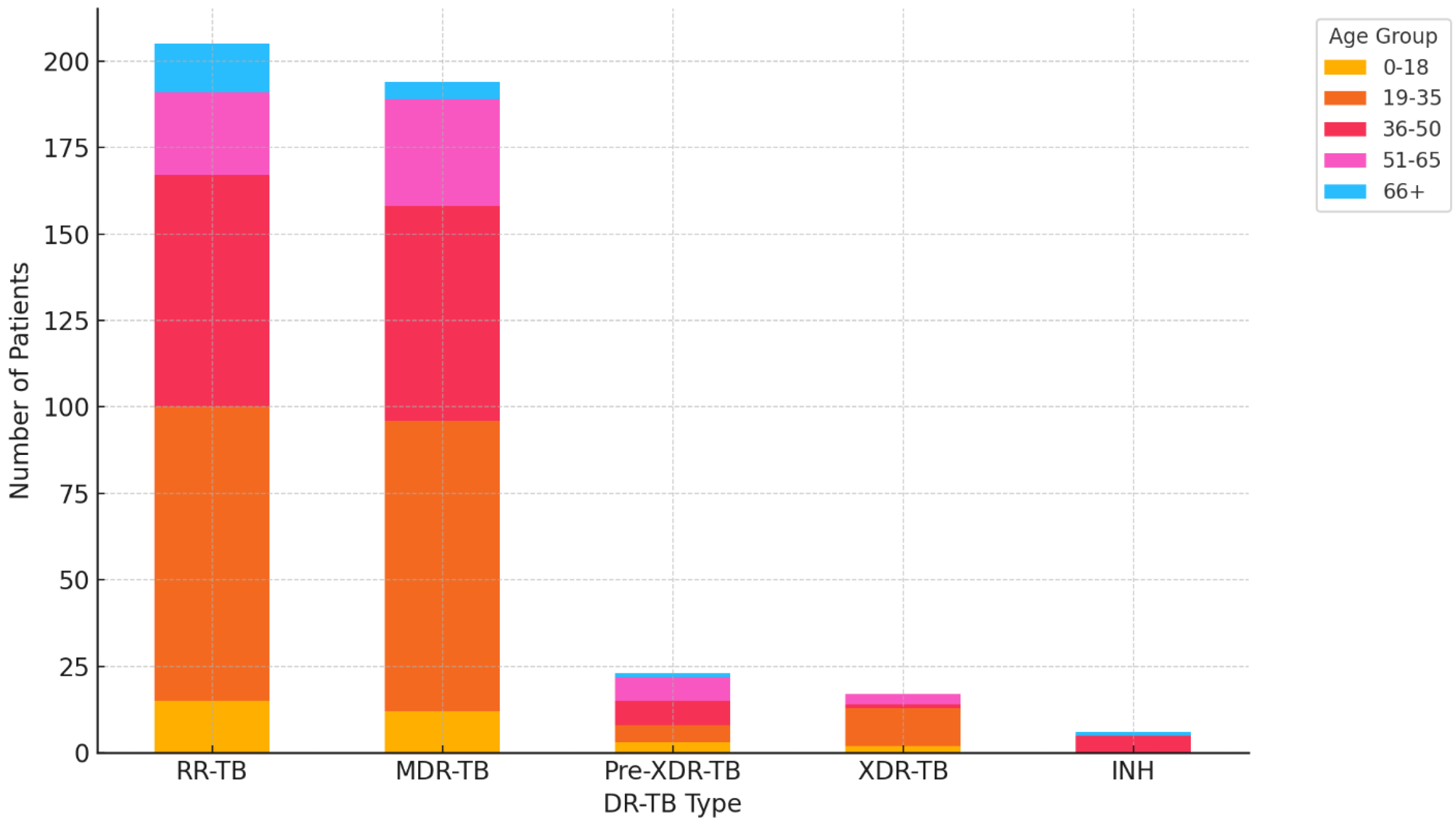
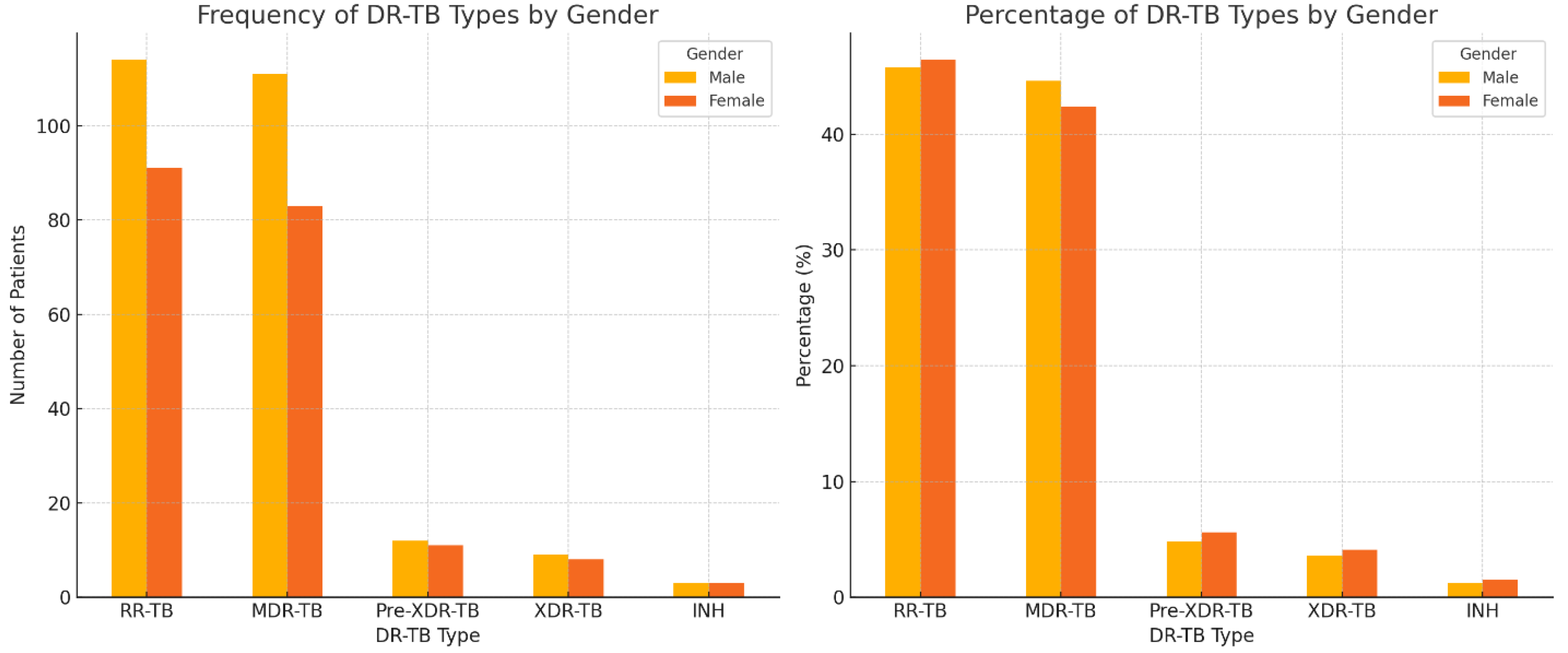
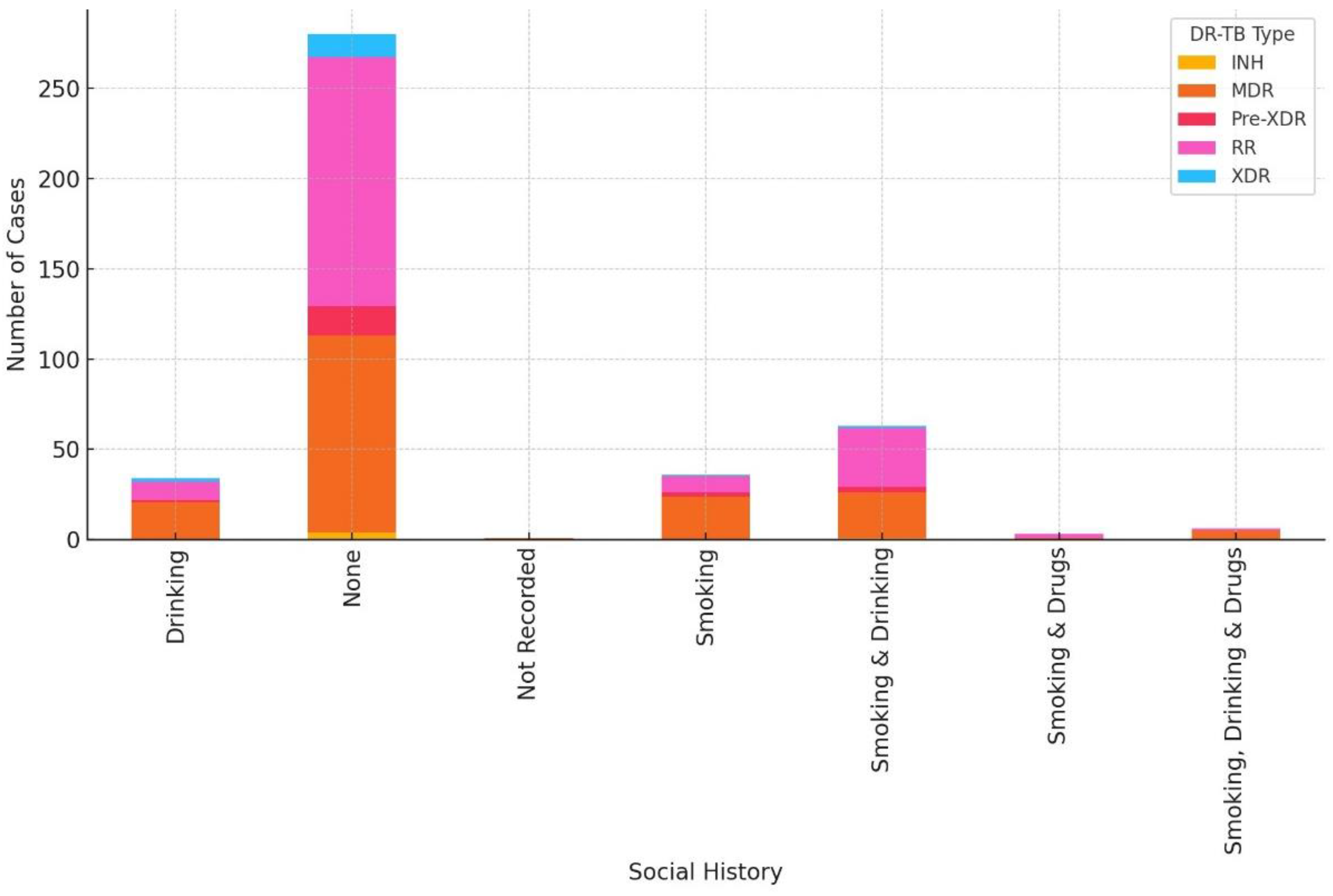
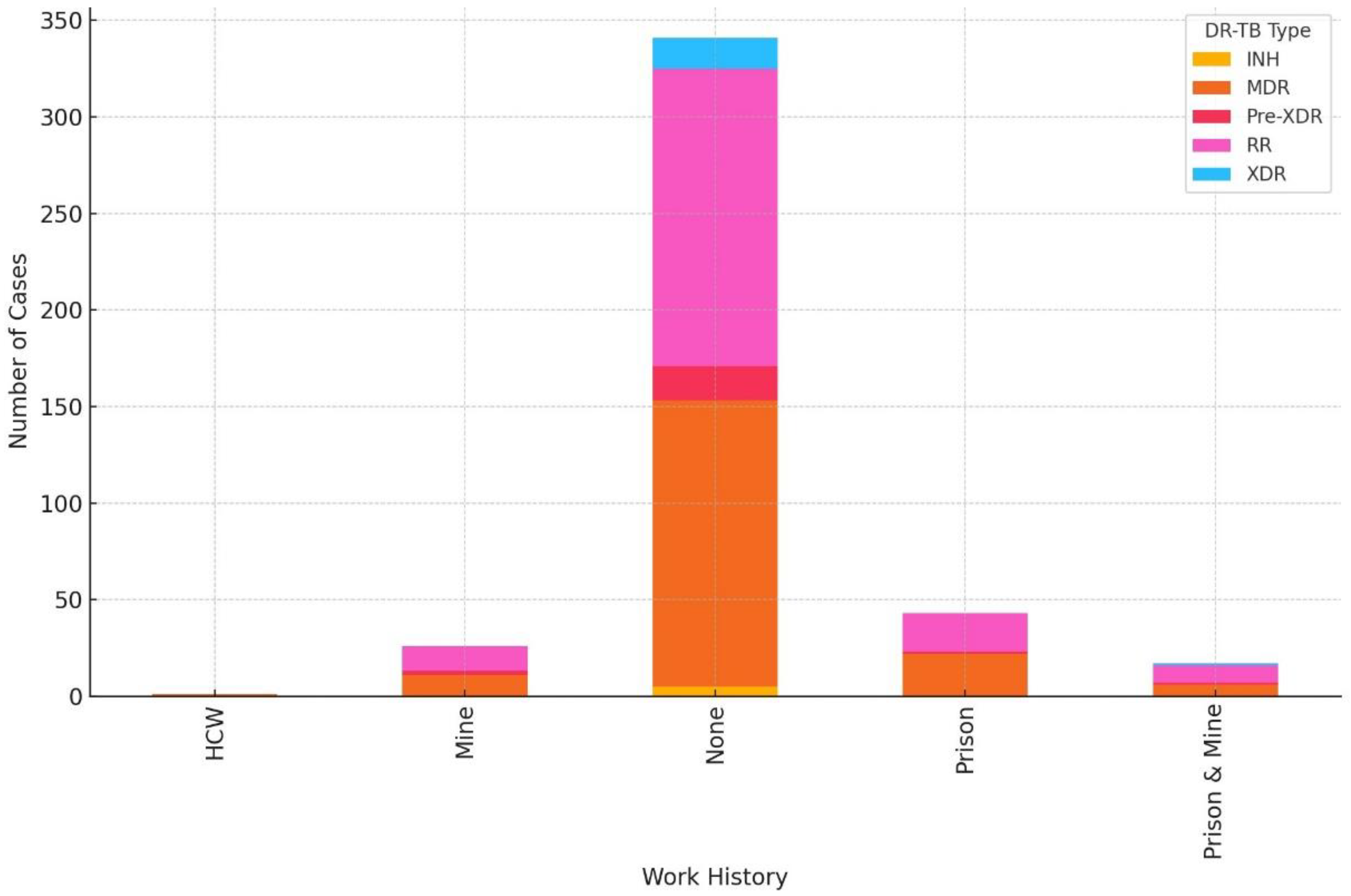
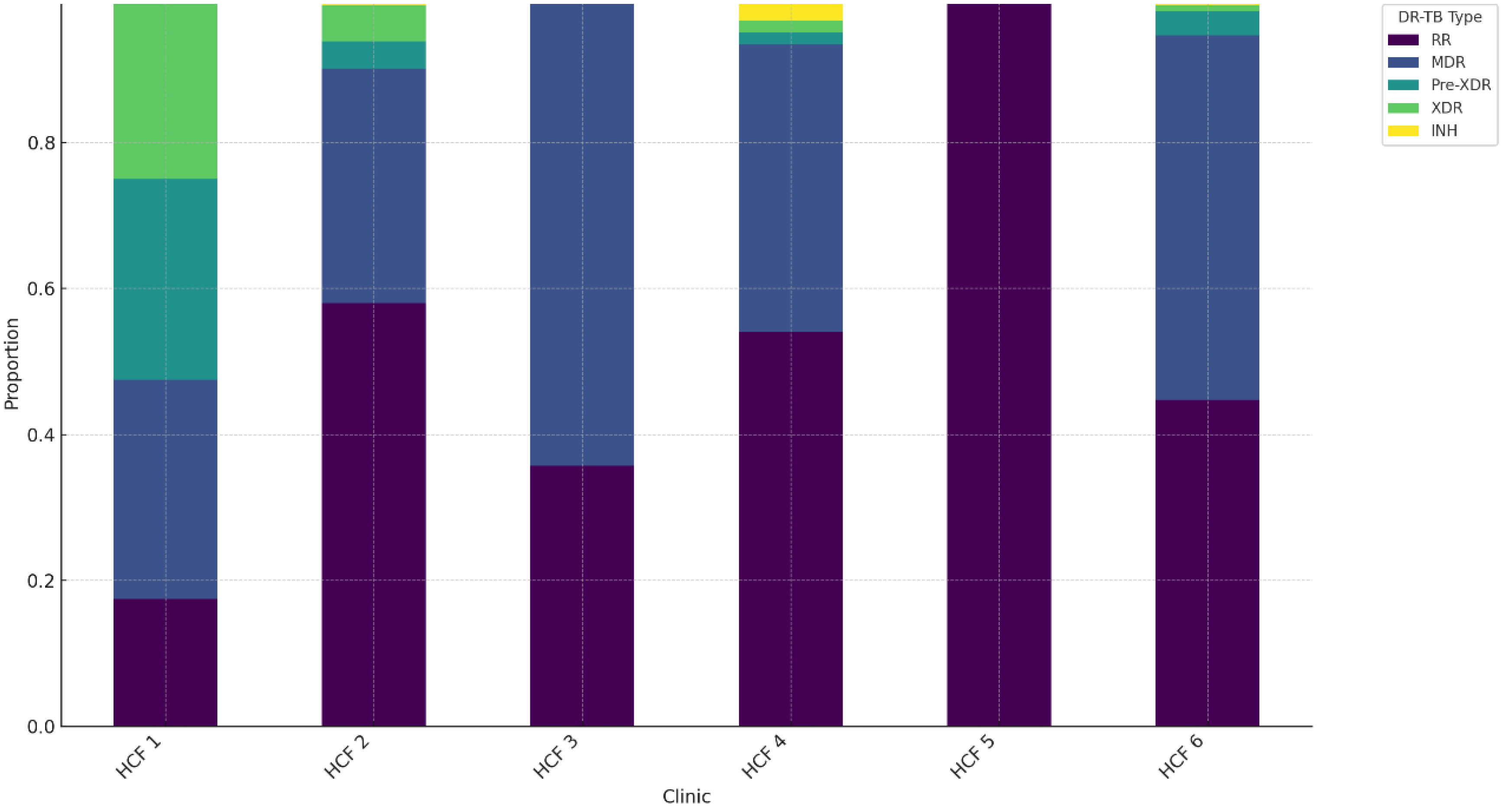
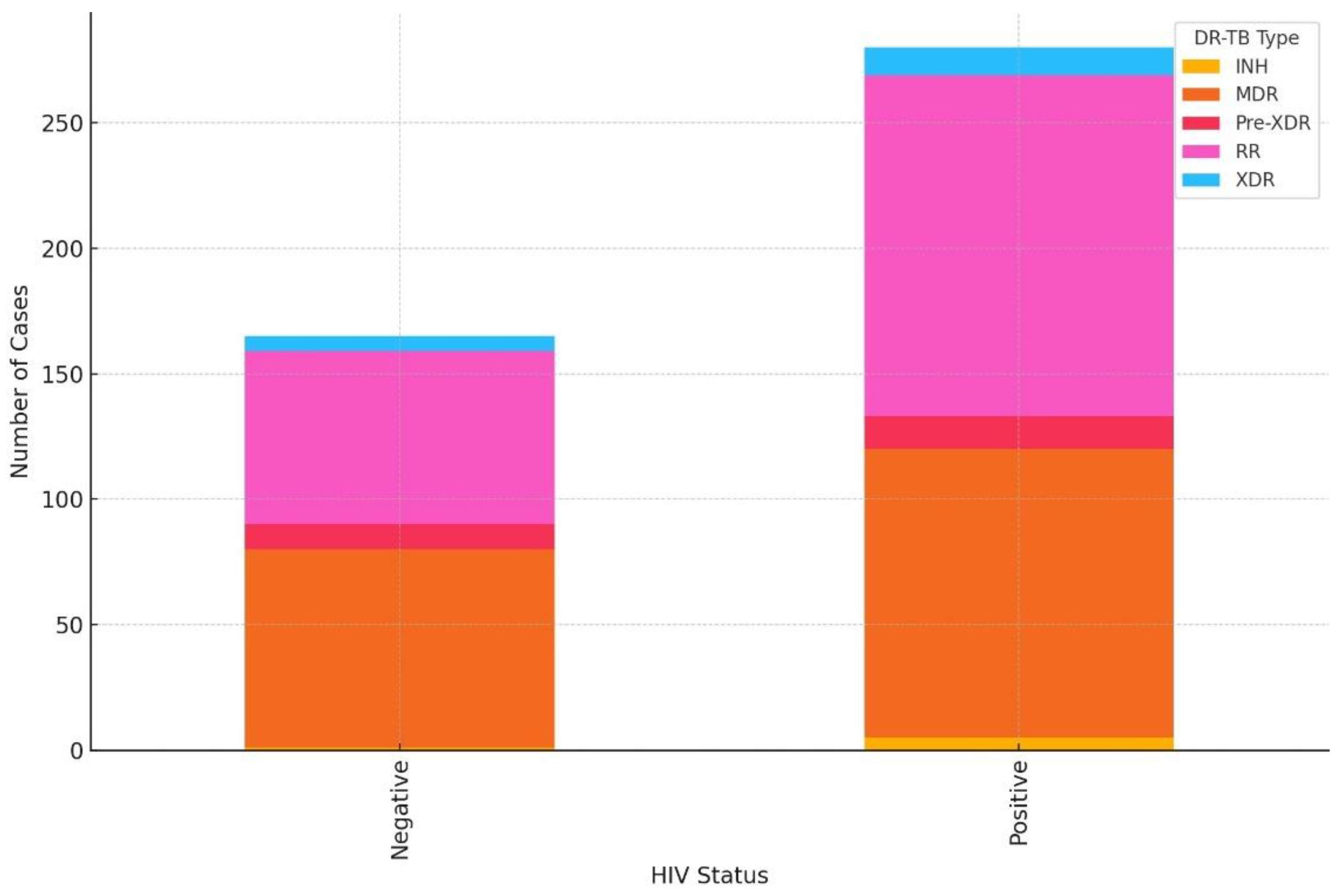
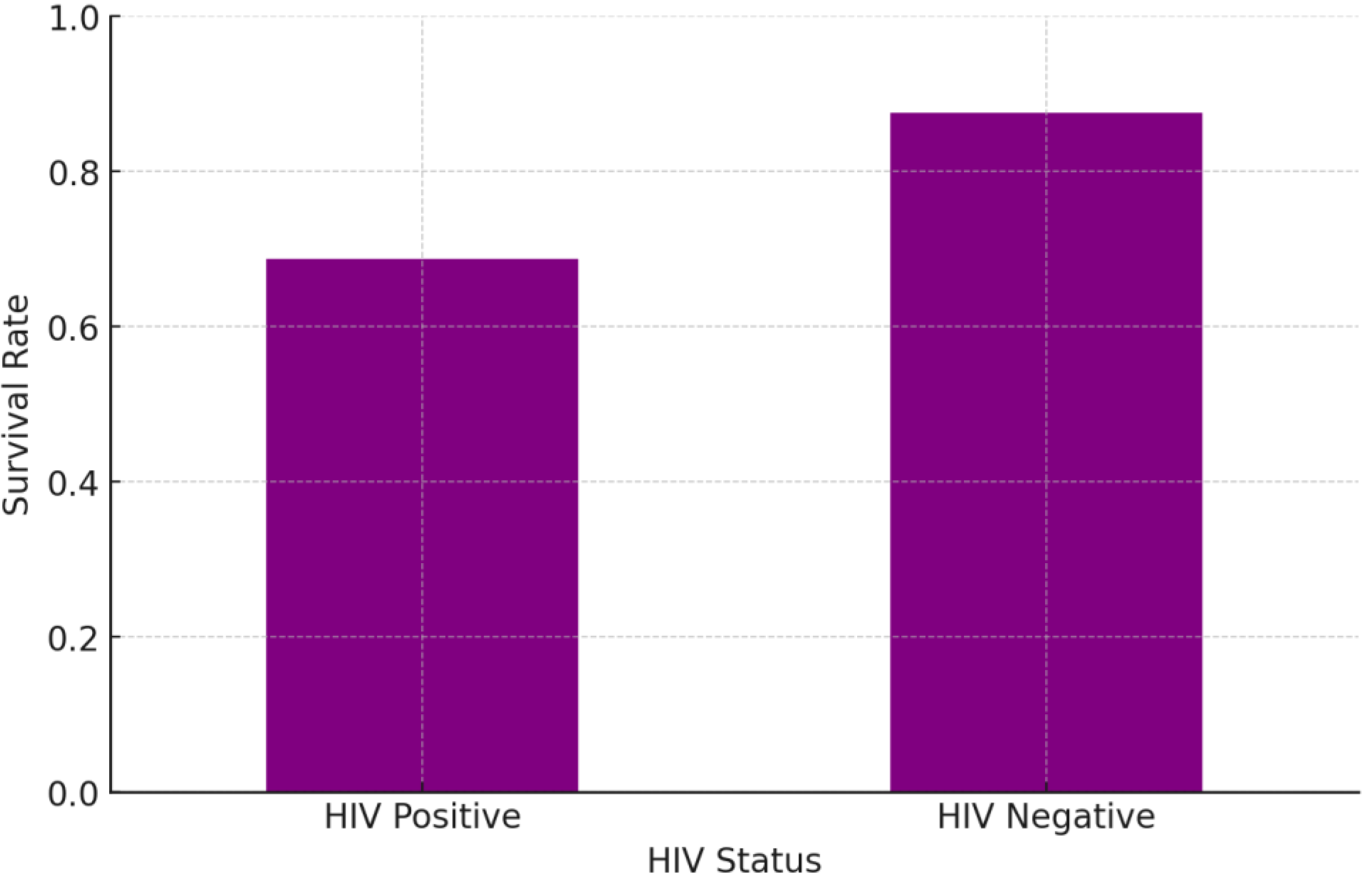
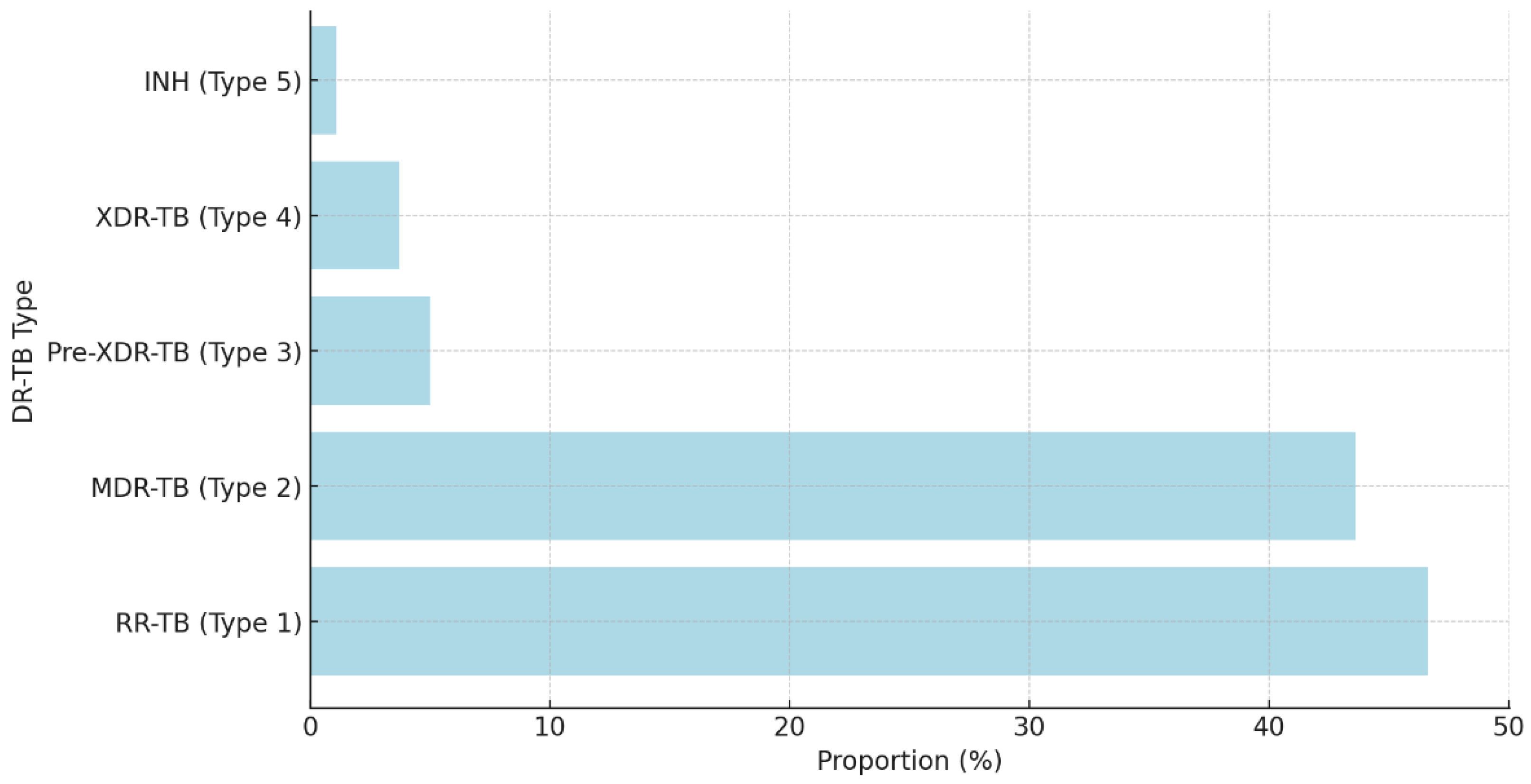
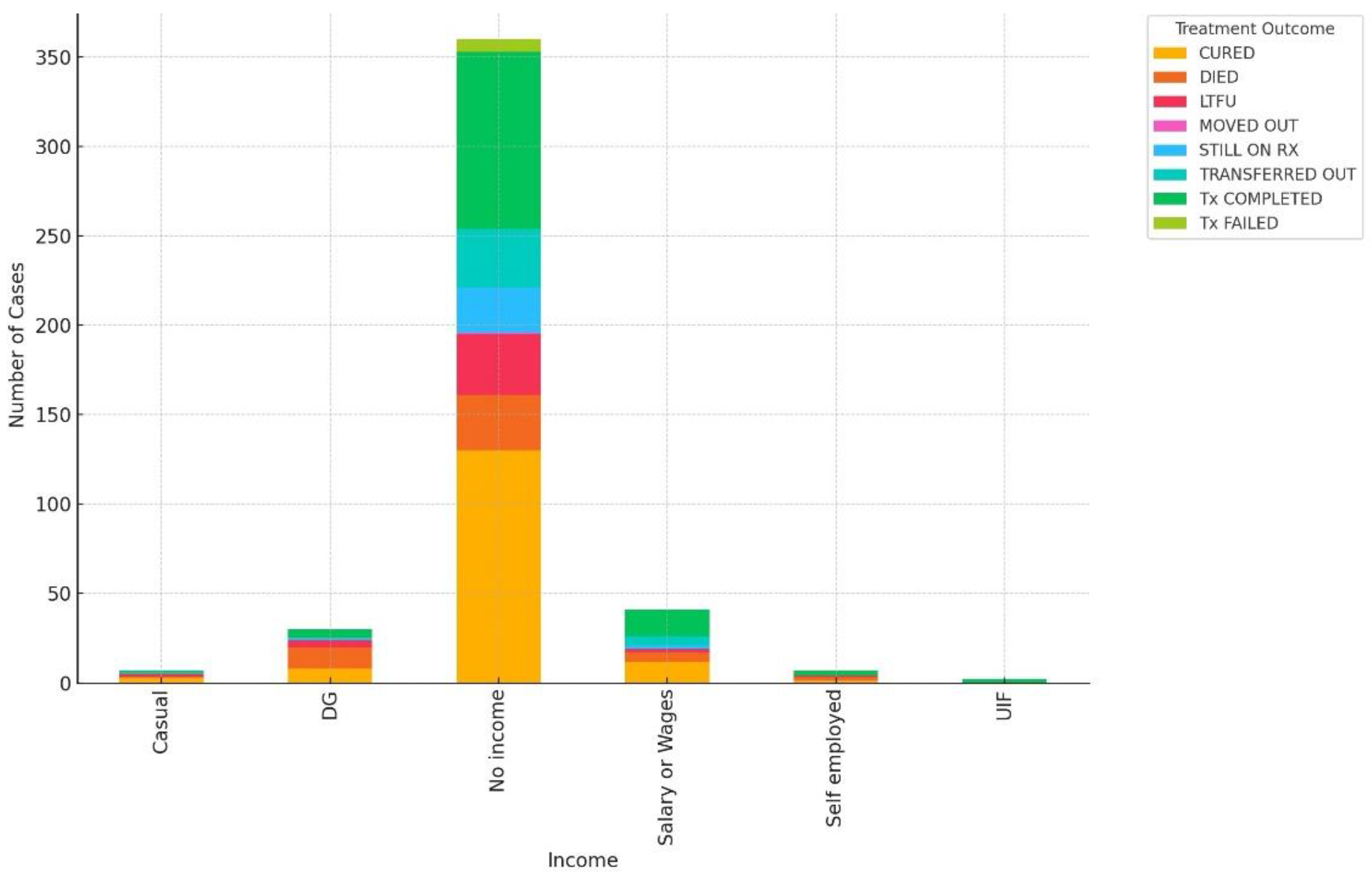
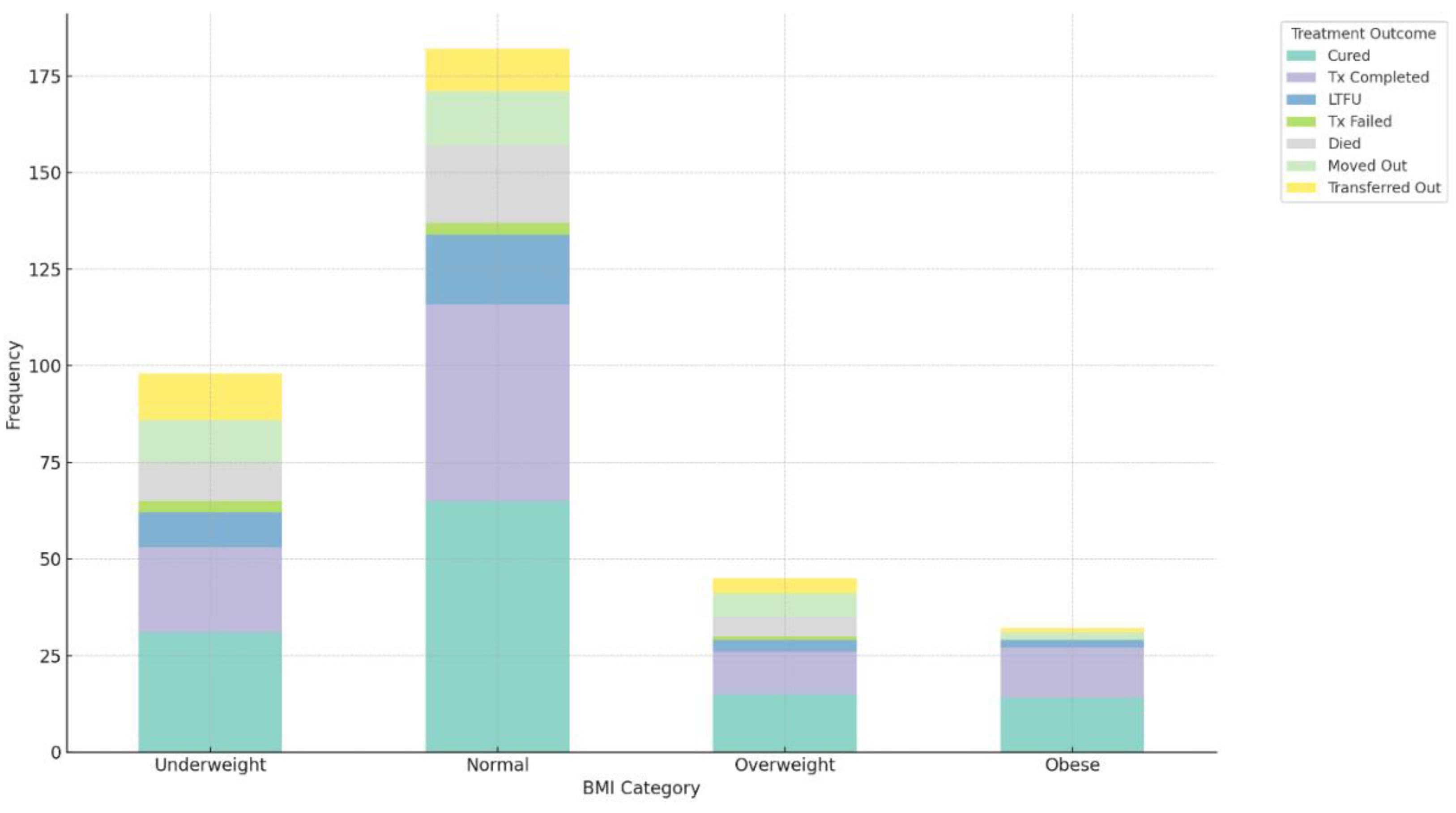
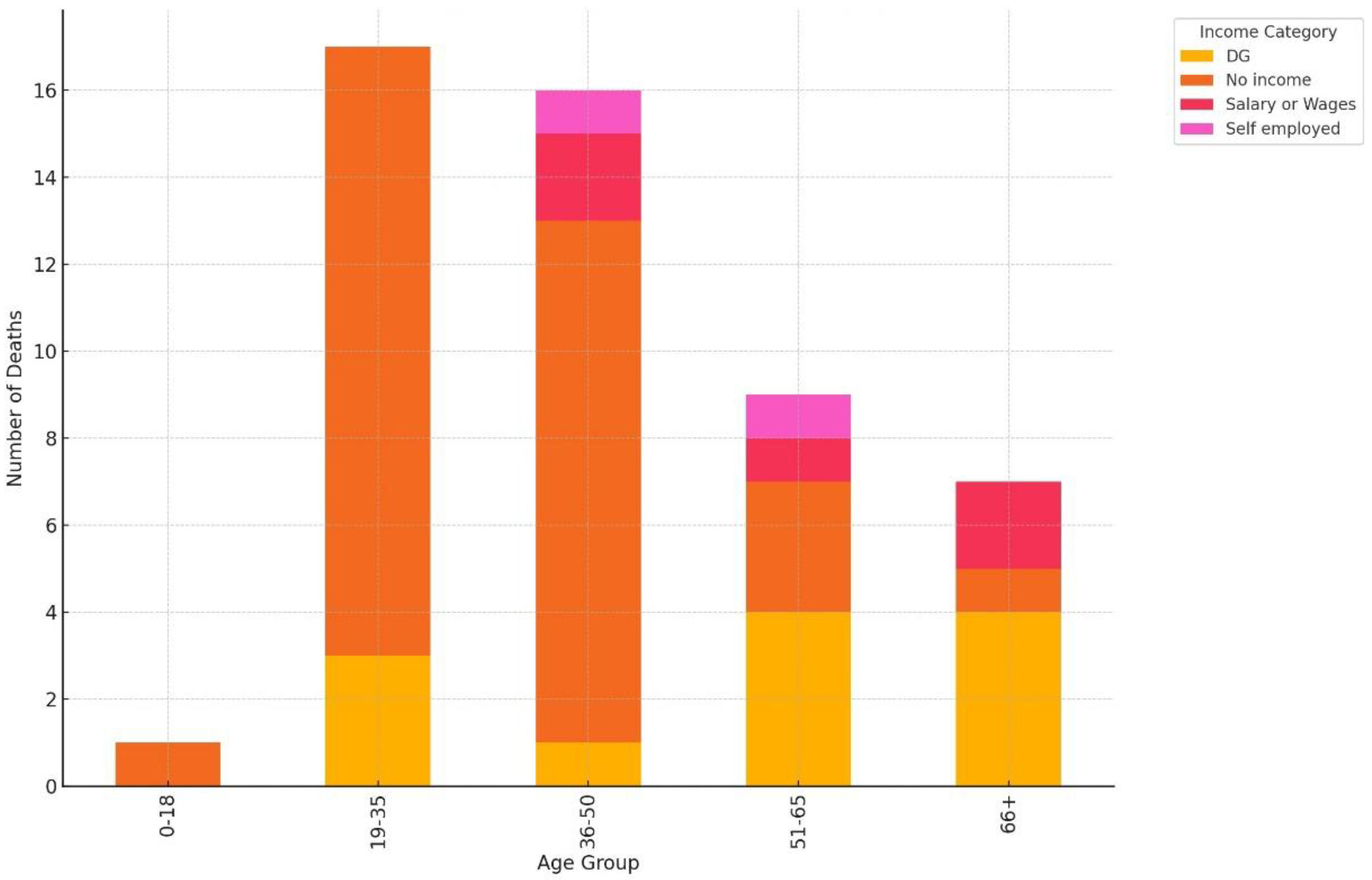
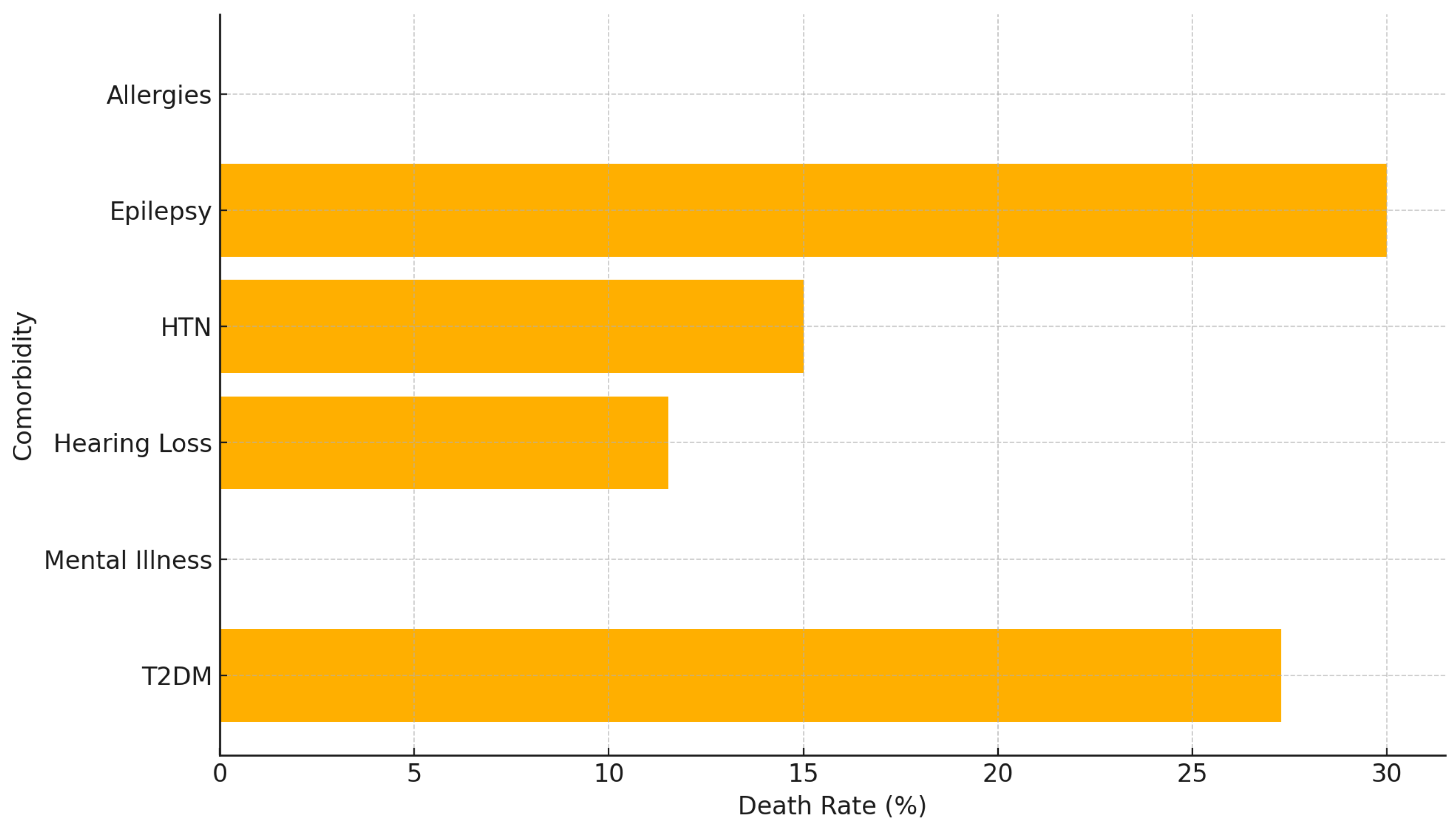
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2023. Available online: https://www.who.int/publications/i/item/9789240061729 (accessed on 13 Sep 2024).
- Seloma NM, Makgatho ME, Maimela E. Evaluation of drug-resistant tuberculosis treatment outcome in Limpopo province, South Africa. Afr J Prim Health Care Fam Med. 2023;15(1). [CrossRef]
- The National Department of Health. The National Strategic Plan for HIV, TB, and STIs 2023-2028. https://knowledgehub.health.gov.za/system/files/elibdownloads/2023-04/NSP-HIV-TB-STIs-2023-2028-MARCH20_23-PRINT2.pdf. (accessed 15 August 2024).
- Gopalaswamy R, Shanmugam S, Mondal R, Subbian S. Of tuberculosis and non-tuberculous mycobacterial infections: A comparative analysis of epidemiology, diagnosis and treatment. J Biomed Sci. 2020;27:1-17. [CrossRef]
- Mancuso G, Midiri A, De Gaetano S, Ponzo E, Biondo C. Tackling drug-resistant tuberculosis: new challenges from the old pathogen Mycobacterium tuberculosis. Microorganisms. 2023;11(9):2277. [CrossRef]
- Natarajan M, et al. Extra-pulmonary tuberculosis: A review of clinical features and management. J Clin Tuberc Other Mycobact Dis. 2020;20:100-110. [CrossRef]
- Suárez I, Fünger SM, Kröger S, Rademacher J, Fätkenheuer G, Rybniker J. The diagnosis and treatment of tuberculosis. Dtsch Arztebl Int. 2019;116(43). [CrossRef]
- Swalehe HM, Obeagu EI. Tuberculosis: Current diagnosis and management. Elite J Public Health. 2024;2(1):23-33.
- Daftary A, Mondal S, Zelnick J, Friedland G, Seepamore B, Boodhram R, et al. Dynamic needs and challenges of people with drug-resistant tuberculosis and HIV in South Africa: a qualitative study. Lancet Glob Health. 2021 Apr;9(4). [CrossRef]
- Ismail NA, Mvusi L, Nanoo A, Dreyer A, Omar SV, Babatunde S, et al. Prevalence of drug-resistant tuberculosis and imputed burden in South Africa: a national and sub-national cross-sectional survey. Lancet Infect Dis. 2018 Jul;18(7):779-87. [CrossRef]
- National Institute of Communicable Diseases (NICD). Introduction of new drugs and drug regimens for the management of drug-resistant tuberculosis in South Africa: Policy framework. 2015.https://www.nicd.ac.za/assets/files/Introduction%20of%20new%20drugs%20and%20drug%20regimens%20for%20the%20management%20of%20drug%20resistant%20TB%20in%20SA%20-%202015.pdf (accessed 15 Aug 2024).
- Oga-Omenka C, Tseja-Akinrin A, Sen P, Mac-Seing M, Agbaje A, Menzies D, et al. Factors influencing diagnosis and treatment initiation for multidrug-resistant/rifampicin-resistant tuberculosis in six sub-Saharan African countries: A mixed-methods systematic review. BMJ Glob Health. 2020;5(7). [CrossRef]
- Chanda E. The clinical profile and outcomes of drug-resistant tuberculosis in Central Province of Zambia. BMC Infect Dis. 2024 Apr 1;24(1):364. [CrossRef] [PubMed] [PubMed Central]
- Dickson L, Le Roux SR, Mitrani L, Hill J, Jassat W, Cox H, et al. Organisation of care for people receiving drug-resistant tuberculosis treatment in South Africa: a mixed methods study. BMJ Open. 2023 Nov 17;13(11). [CrossRef] [PubMed] [PubMed Central]
- World Health Organisation. Global Tuberculosis Report 2021. Available online: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2021 (accessed on 13 September 2024).
- Cox V, McKenna L, Acquah R, Reuter A, Wasserman S, Vambe D, et al. Clinical perspectives on treatment of rifampicin-resistant/multidrug-resistant TB. Int J Tuberc Lung Dis. 2020 Nov 1;24(11):1134-44. [CrossRef]
- Kielmann K, Vidal N, Riekstiņa V, Krutikov M, van der Werf MJ, Biraua E, et al. "Treatment is of primary importance, and social assistance is secondary": a qualitative study on the organisation of tuberculosis (TB) care and patients' experience of starting and staying on TB treatment in Riga, Latvia. PLoS One. 2018;13(10). [CrossRef]
- Long Q, Qu Y, Lucas HC. Drug-resistant tuberculosis control in China: progress and challenges. Infect Dis Poverty. 2016;5(1). [CrossRef]
- Mutembo S, Mutanga JN, Musokotwane K, Kanene C, Dobbin KK, Yao X, et al. Urban-rural disparities in treatment outcomes among recurrent TB cases in Southern Province, Zambia. BMC Infect Dis. 2019;19(1). [CrossRef]
- Getahun G. Patient delay and associated factors among pulmonary tuberculosis patients at Hadiya zone public health facilities in south Ethiopia, 2017. Eur J Clin Biomed Sci. 2018;4(4):55. [CrossRef]
- Ejeh FE, Undiandeye A, Okon KO, Kazeem HM, Kudi AC. Isolation and immunological detection of Mycobacterium tuberculosis from HIV and non-HIV patients in Benue State, Nigeria. Ethiop J Health Sci. 2020;30(1). [CrossRef]
- Dodd PJ, et al. The impact of health system strengthening on tuberculosis control: A systematic review. BMC Health Serv Res. 2016;16:1-10. [CrossRef]
- Siza JE, et al. Knowledge and perceptions of tuberculosis among rural communities in Mozambique. Int J Infect Dis. 2020;95:1-7. [CrossRef]
- Assefa A, Girma A, Kloos H. Factors associated with unsuccessful treatment of tuberculosis in Arsi-Robe Hospital, Arsi Zone, Ethiopia: a retrospective study. 2021. [CrossRef]
- Dhande A, et al. Clinico-epidemiological profile and adherence to antitubercular treatment of tuberculosis patients in a city of Maharashtra. Int J Community Med Public Health. 2020. [CrossRef]
- Alemu, A., et al. Predictors of mortality in patients with drug-resistant tuberculosis: A systematic review and meta-analysis. PLOS ONE. 2021. [CrossRef]
- Stuckler D, Basu S, McKee M, Lurie M. Mining and risk of tuberculosis in sub-Saharan Africa. Am J Public Health. 2011 Mar;101(3):524-30. [CrossRef] [PubMed] [PubMed Central]
- Basu S, Stuckler D, McKee M. The Health Impacts of the Economic Crisis in the European Union. Eur J Public Health. 2019;29(4):1-6. [CrossRef]
- Appiah MA, Arthur JA, Asampong E, et al. Health service providers’ perspective on barriers and strategies to tuberculosis treatment adherence in Obuasi Municipal and Obuasi East District in the Ashanti region, Ghana: a qualitative study. Discov Health Systems. 2024;3:19. [CrossRef]
- Nidoi J, Muttamba W, Walusimbi S, Imoko JF, Lochoro P, Ictho J, et al. Impact of socio-economic factors on tuberculosis treatment outcomes in north-eastern Uganda: A mixed methods study. BMC Public Health. 2021 Nov 26;21(1):2167. [CrossRef] [PubMed] [PubMed Central]
- Nyasulu PS, Ngasama E, Tamuzi JL, Sigwadhi LN, Ozougwu LU, et al. Effect of HIV status and antiretroviral treatment on treatment outcomes of tuberculosis patients in a rural primary healthcare clinic in South Africa. PLoS One. 2022;17(10). [CrossRef]
- UNAIDS. UNAIDS Fact Sheet. Tuberculosis and HIV. https://www.unaids.org/sites/default/files/media_asset/tb-and-hiv_en.pdf (accessed 16 Jun 2024).
- Parsons LM, Somoskövi A, Gutierrez C, Lee E, Paramasivan CN, Abimiku A, et al. Laboratory diagnosis of tuberculosis in resource-poor countries: challenges and opportunities. Clin Microbiol Rev. 2011 Apr;24(2):314-50. [CrossRef] [PubMed] [PubMed Central]
- Dlatu N, Longo-Mbenza B, Apalata T. Predictors of tuberculosis incidence and the effects of multiple deprivation indices on tuberculosis management in OR Tambo district over a 5-year period. PLoS One. 2022 Mar 10;17(3). [CrossRef] [PubMed] [PubMed Central]
- Colebunders R, Apers L, Dieltiens G, Worodria W. Tuberculosis in resource poor countries. BMJ. 2007 Jan 20;334(7585):105-6. [CrossRef] [PubMed] [PubMed Central]
- Marme G, Rutherford S, Harris N. What tuberculosis infection control measures are effective in resource-constrained primary healthcare facilities? A systematic review of the literature. Rural Remote Health. 2023;23:7175. [CrossRef]
- Faye LM, Hosu MC, Iruedo J, Vasaikar S, Nokoyo KA, Tsuro U, et al. Treatment outcomes and associated factors among tuberculosis patients from selected rural Eastern Cape hospitals: An ambidirectional study. Trop Med Infect Dis. 2023 Jun 9;8(6):315. [CrossRef] [PubMed] [PubMed Central]
- Paleckyte A, Dissanayake O, Mpagama S, et al. Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrob Resist Infect Control. 2021;10:106. [CrossRef]
- Atkins S, Heimo L, Carter D, et al. The socioeconomic impact of tuberculosis on children and adolescents: a scoping review and conceptual framework. BMC Public Health. 2022;22:2153. [CrossRef]
- 83. Wen Y, Zhang Z, Li X, et al. Treatment outcomes and factors affecting unsuccessful outcome among new pulmonary smear positive and negative tuberculosis patients in Anqing, China: a retrospective study. BMC Infect Dis. 2018;18:104. [CrossRef]
- Agazhu HW, Assefa ZM, Beshir MT, Tadesse H, Mengstie AS. Treatment outcomes and associated factors among tuberculosis patients attending Gurage Zone Public Hospital, Southern Nations, Nationalities, and People’s Region, Ethiopia: an institution-based cross-sectional study. Front Med. 2023;10:1105911. [CrossRef]
- Oyageshio OP, Myrick JW, Saayman J, van der Westhuizen L, Al-Hindi D, Reynolds AW, et al. Strong effect of demographic changes on tuberculosis susceptibility in South Africa. medRxiv [Preprint]. 2023 Nov 3:2023.11.02.23297990. doi: 10.1101/2023.11.02.23297990. Update in: PLOS Glob Public Health. 2024 Jul 23;4(7). [CrossRef] [PubMed] [PubMed Central]
- Guo J, Liu ZD, Feng YP, Luo SR, Jiang QM. Assessment of effective anti-TB regimens and adverse outcomes related risk factors in the elderly and senile-aged TB patients. Infect Drug Resist. 2023 Jun 19;16:3903-3915. [CrossRef] [PubMed] [PubMed Central]
- Shibabaw A, Gelaw B, Gebreyes W, Robinson R, Wang SH, Tessema B. The burden of pre-extensively and extensively drug-resistant tuberculosis among MDR-TB patients in the Amhara region, Ethiopia. PLoS One. 2020 Feb 13;15(2). [CrossRef] [PubMed] [PubMed Central]
- Utpat KV, Rajpurohit R, Desai U. Prevalence of pre-extensively drug-resistant tuberculosis (Pre XDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) among extra pulmonary (EP) multidrug resistant tuberculosis (MDR-TB) at a tertiary care center in Mumbai in pre Bedaquiline (BDQ) era. Lung India. 2023 Jan-Feb;40(1):19-23. [CrossRef] [PubMed] [PubMed Central]
- Adisa R, Ayandokun TT, Ige OM. Knowledge about tuberculosis, treatment adherence and outcome among ambulatory patients with drug-sensitive tuberculosis in two directly-observed treatment centres in Southwest Nigeria. BMC Public Health. 2021;21:677. [CrossRef]
- Cannon LL, Oladimeji KE, Goon DT. Socio-economic drivers of drug-resistant tuberculosis in Africa: a scoping review. BMC Public Health. 2021 Mar 11;21(1):488. [CrossRef] [PubMed] [PubMed Central]
- Kootbodien T, Monyane M, Mothibe N. The impact of socio-economic factors on tuberculosis treatment outcomes in South Africa: A retrospective cohort study. BMC Public Health. 2018;18(1):1234. [CrossRef]
- Lv H, Zhang X, Zhang X, et al. Global prevalence and burden of multidrug-resistant tuberculosis from 1990 to 2019. BMC Infect Dis. 2024;24:243. [CrossRef]
- Said H, Kachingwe E, Gardee Y, et al. Determining the risk-factors for molecular clustering of drug-resistant tuberculosis in South Africa. BMC Public Health. 2023;23:2329. [CrossRef]
- Ataguba JE, Akazili J, McIntyre D. Socioeconomic-related health inequality in South Africa: evidence from General Household Surveys. Int J Equity Health. 2011;10:48. [CrossRef]
- de Siqueira Filha NT, Li J, Phillips-Howard PA, et al. The economics of healthcare access: a scoping review on the economic impact of healthcare access for vulnerable urban populations in low- and middle-income countries. Int J Equity Health. 2022;21:191. [CrossRef]
- Ndaguba EA, Hlotywa A. Public health expenditure and economic development: The case of South Africa between 1996 and 2016. Cogent Econ Financ. 2021 Jan 1;9(1):1905932. [CrossRef]
- Harling G, Lima Neto AS, Sousa GS, Machado MMT, Castro MC. Determinants of tuberculosis transmission and treatment abandonment in Fortaleza, Brazil. BMC Public Health. 2017;17:508. [CrossRef]
- Wingfield T, Tovar MA, Huff D, et al. Beyond pills and tests: addressing the social determinants of tuberculosis. Clin Med (Lond). 2016;16(suppl 6):s79-91. [CrossRef]
- Roy SC, Khanam PA, Ahmed BN, Islam MA, Huq AF, Saha MR. Assessment of treatment outcomes of multidrug-resistant tuberculosis in Bangladeshi population: a retrospective cohort study. J Armed Forces Med Coll Bangladesh. 2022;18(1):57-60. [CrossRef]
- O'Donnell M, et al. The impact of socio-economic factors on tuberculosis treatment adherence: A systematic review. Int J Tuberc Lung Dis. 2016;20(1):1-10. [CrossRef]
- Adamu AL, Aliyu MH, Galadanci NA, Musa BM, Lawan UM, Bashir U, et al. The impact of rural residence and HIV infection on poor tuberculosis treatment outcomes in a large urban hospital: a retrospective cohort analysis. Int J Equity Health. 2018;17(1). [CrossRef]
- McIntyre D, Thiede M, Birch S. Universal Health Coverage: A Global Perspective. Health Econ Policy Law. 2019;14(4):1-15. [CrossRef]
- Schneider M, Hlophe H. The impact of social grants on health outcomes in South Africa. S Afr J Public Health. 2016;1(1):12-20. [CrossRef]
- Khan M, Ali S, Rahman A. Socio-economic determinants of tuberculosis treatment adherence: A cross-sectional study in urban settings. Int J Tuberc Lung Dis. 2021;25(6):567-74. [CrossRef]
- Biset S, Teferi M, Alamirew H, et al. Trends of Mycobacterium tuberculosis and Rifampicin resistance in Northwest Ethiopia: Xpert® MTB/RIF assay results from 2015 to 2021. BMC Infect Dis. 2024;24:238. [CrossRef]
- Bykov I, Dyachenko O, Ratmanov P, Liu H, Liang L, Wu Q. Factors contributing to the high prevalence of multidrug-resistance/Rifampicin-resistance in patients with tuberculosis: an epidemiological cross sectional and qualitative study from Khabarovsk krai region of Russia. BMC Infect Dis. 2022 Jul 13;22(1):612. [CrossRef] [PubMed] [PubMed Central]
- Bea S, Lee H, Kim JH, Jang SH, Son H, Kwon JW, et al. Adherence and associated factors of treatment regimen in drug-susceptible tuberculosis patients. Front Pharmacol. 2021 Mar 15;12:625078. doi: 10.3389/fphar.2021.625078. [CrossRef] [PubMed] [PubMed Central]
- Adejumo OA, Olusola-Faleye B, Adepoju V, Bowale A, Adesola S, Falana A, et al. Prevalence of rifampicin-resistant tuberculosis and associated factors among presumptive tuberculosis patients in a secondary referral hospital in Lagos Nigeria. Afr Health Sci. 2018 Sep;18(3):472-8. [CrossRef] [PubMed] [PubMed Central]
- Wekesa C, Sekaggya-Wiltshire C, Muyanja SZ, et al. Comparing adherence to MDR-TB treatment among patients on self-administered therapy and those on directly observed therapy: non-inferiority randomized controlled trial. Trials. 2023;24:326. [CrossRef]
- Djibuti M, Mirvelashvili E, Makharashvili N, Magee MJ. Household income and poor treatment outcome among patients with tuberculosis in Georgia: a cohort study. BMC Public Health. 2014 Jan 29;14:88. [CrossRef] [PubMed] [PubMed Central]
- Ngah VD, Rangoanana M, Fwemba I, Maama L, Maphalale S, Molete M, et al. Evaluating determinants of treatment outcomes among tuberculosis patients in the mining district of Butha Buthe, Lesotho. IJID Reg. 2023 Mar;6:62-67. [CrossRef] [PubMed] [PubMed Central]
- Tadokera R, Bekker LG, Kreiswirth BN, Mathema B, Middelkoop K. TB transmission is associated with prolonged stay in a low socio-economic, high burdened TB and HIV community in Cape Town, South Africa. BMC Infect Dis. 2020 Feb 10;20(1):120. [CrossRef] [PubMed] [PubMed Central]
- Cramm JM, Koolman X, Møller V, Nieboer AP. Socio-economic status and self-reported tuberculosis: a multilevel analysis in a low-income township in the Eastern Cape, South Africa. J Public Health Afr. 2011 Sep 5;2(2). [CrossRef] [PubMed] [PubMed Central]
- Carwile ME, Hochberg NS, Sinha P. Undernutrition is feeding the tuberculosis pandemic: A perspective. J Clin Tuberc Other Mycobact Dis. 2022 Mar 17;27:100311. [CrossRef] [PubMed] [PubMed Central]
- Van de Water BJ, Fulcher I, Cilliers S, Meyer N, Wilson M, Young C, et al. Association of HIV infection and antiretroviral therapy with the occurrence of an unfavorable TB treatment outcome in a rural district hospital in Eastern Cape, South Africa: A retrospective cohort study. PLoS One. 2022;17. [CrossRef]
- Lelisho ME, Wotale TW, Tareke SA, et al. Survival rate and predictors of mortality among TB/HIV co-infected adult patients: retrospective cohort study. Sci Rep. 2022;12:18360. [CrossRef]
- Murphy RA, Marconi VC, Gandhi RT, Kuritzkes DR, Sunpath H. Coadministration of lopinavir/ritonavir and rifampicin in HIV and tuberculosis co-infected adults in South Africa. PLoS One. 2012;7(9). doi: 10.1371/journal.pone.0044793. Epub 2012 Sep 28. Erratum in: PLoS One. 2013 Dec 9;8(12). [CrossRef] [PubMed] [PubMed Central]
- Kumar A, et al. Therapeutic drug monitoring in HIV-TB co-infected patients. Int J Infect Dis. 2020;95:123-30.
- Wouters E, van Rensburg AJ, Engelbrecht M, et al. How the HIV/TB co-epidemic, HIV stigma, and TB stigma syndemic impacts on the use of occupational health services for TB in South African hospitals: a structural equation modelling analysis of the baseline data from the HaTSaH Study (cluster RCT). BMJ Open. 2022;12. [CrossRef]
- Osman M, van Schalkwyk C, Naidoo P, Seddon JA, Dunbar R, Dlamini SS, et al. Mortality during tuberculosis treatment in South Africa using an 8-year analysis of the national tuberculosis treatment register. Sci Rep. 2021 Aug 5;11(1):15894. [CrossRef] [PubMed] [PubMed Central]
- Min J, Kim JS, Kim HW, Ko Y, Oh JY, Jeong YJ, et al. Effects of underweight and overweight on mortality in patients with pulmonary tuberculosis. Front Public Health. 2023 Sep 19;11:1236099. [CrossRef] [PubMed] [PubMed Central]
- Peinado J, Lecca L, Jiménez J, Espinoza RC, Yataco R, Becerra M, et al. Association between overweight/obesity and multidrug-resistant tuberculosis. Rev Peru Med Exp Salud Publica. 2023;40(1):59-66. [CrossRef]
- Diallo A, Diallo BD, Camara LM, et al. Different profiles of body mass index variation among patients with multidrug-resistant tuberculosis: a retrospective cohort study. BMC Infect Dis. 2020;20:315. [CrossRef]
- Limenh LW, Kasahun AE, Sendekie AK, et al. Tuberculosis treatment outcomes and associated factors among tuberculosis patients treated at healthcare facilities of Motta Town, Northwest Ethiopia: a five-year retrospective study. Sci Rep. 2024;14:7695. [CrossRef]
- Cáceres G, Calderon R, Ugarte-Gil C. Tuberculosis and comorbidities: treatment challenges in patients with comorbid diabetes mellitus and depression. Ther Adv Infect Dis. 2022 May 20;9:20499361221095831. [CrossRef] [PubMed] [PubMed Central]
- Starshinova A, Nazarenko M, Belyaeva E, Chuzhov A, Osipov N, Kudlay D. Assessment of comorbidity in patients with drug-resistant tuberculosis. Pathogens. 2023;12:1394. [CrossRef]
- Seegert AB, Patsche CB, Sifna A, Gomes VF, Wejse C, Storgaard M, et al. Hypertension is associated with increased mortality in patients with tuberculosis in Guinea-Bissau. Int J Infect Dis. 2021 Aug 1;109:123-8. 10.1016/j.ijid.2021.06.062.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




