Submitted:
24 September 2024
Posted:
24 September 2024
You are already at the latest version
Abstract
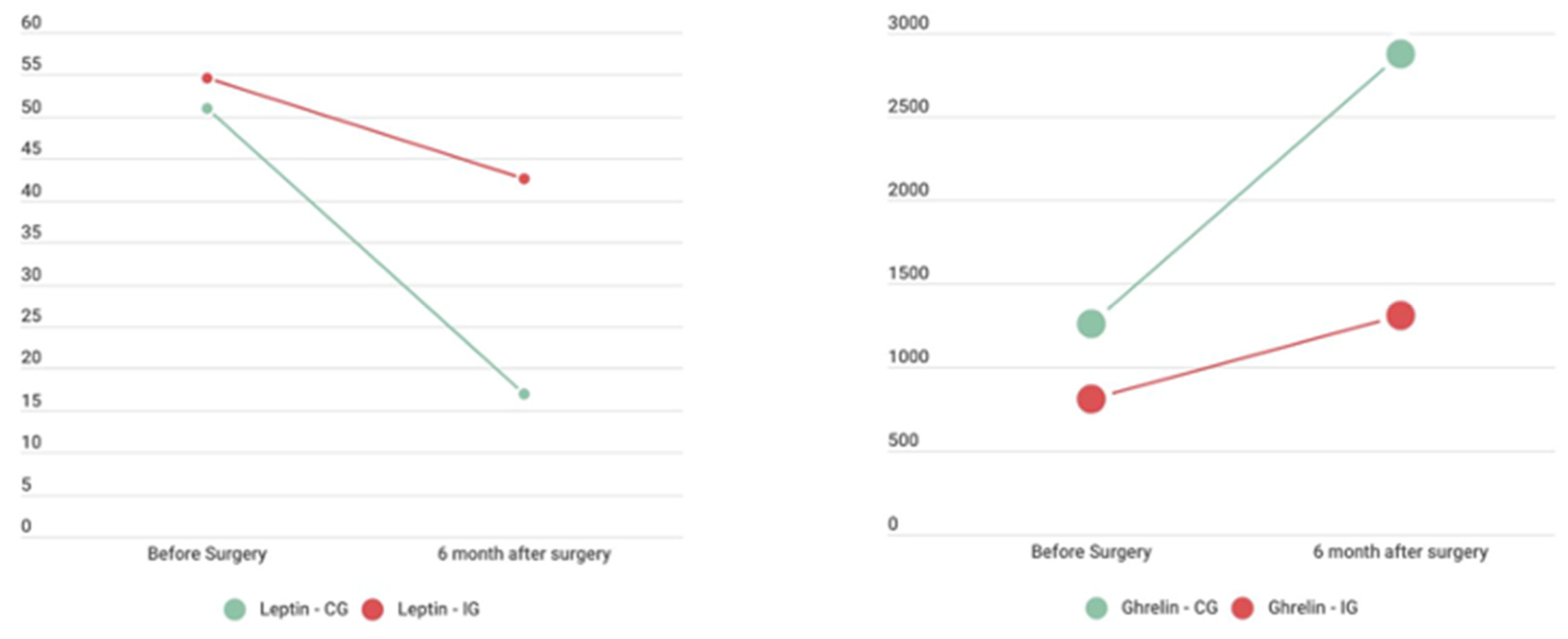
Introduction: Leptin and ghrelin are two hormones that play a role in weight homeostasis. Leptin, which is produced primarily by adipocytes and is dependent on body fat mass, suppresses appetite and increases energy expenditure. Conversely, ghrelin is the “hunger hormone”, it stimulates appetite and promotes fat storage. Bariatric surgery significantly alters the levels and activity of these hormones, contributing to weight loss and metabolic improvements. Clarifying the interplay between bariatric surgery, weight loss, physical exercise, leptin, and ghrelin is essential for developing comprehensive strategies for optimizing long-term outcomes for candidates for bariatric surgery, especially sarcopenic patients. Methods: This was a randomized controlled study with two groups (n=22). The patients in both groups have obesity and sarcopenia. A Roux-en-Ygastric bypass (RYGB) procedure was performed in all patients. The intervention group participated in a structured exercise program three times per week beginning one month after surgery and lasting 16 weeks. Patient assessment was performed before surgery (baseline) and after completion of the exercise program. The control group received the usual standard of care and was assessed similarly. Results: After surgery, weight, BMI and lean mass decreased significantly in both groups from baseline to the second assessment. Leptin was not significantly different from baseline to the second assessment in the physical exercise group but was significantly lower in the control group (p=0.05). Ghrelin increased over time in both groups, but the differences were not significant. When we associated leptin (the dependent variable) with weight (the independent variable), we found that lower weight was associated with lower leptin levels. A similar relationship was also observed between leptin and sarcopenia parameters (muscle strength and mass), as well as with bone health parameters (bone mineral density and t-score). Higher ghrelin levels were significantly associated with higher t-scores and z-score (p<0.05). Conclusion: Exercise has been shown to have a significant effect on leptin and ghrelin levels after bariatric surgery. By incorporating regular physical activity into their lifestyle, bariatric patients can optimize their weight loss outcomes and improve their overall health. After the physical exercise protocol, patients in the intervention group revealed more established leptin levels, which may indicate a protected pattern concerning decreased leptin levels. An unfavorable profile was evidenced, according to which greater weight loss, sarcopenia, and osteoporosis were associated with lower leptin levels.
Keywords:
1. Introduction
2. Methods
Study Design
Eligibility Criteria
Sample Size and Randomization
Intervention
Outcomes
Statistical Methods
3. Results
4. Discussion
5. Conclusions
References
- Bentham, J.; Di Cesare, M.; Bilano, V.; Bixby, H.; Zhou, B.; Stevens, G.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet [Internet]. 2017 Dec 16 [cited 2022 May 22];390(10113):2627–42. Available online: https://pubmed.ncbi.nlm.nih.gov/29029897/.
- Hämälaïnen, R.M.; Breda, J.; Da Silva Gomes, F.; Gongal, G.; Khan, W.; Mendes, R.; et al. New global physical activity guidelines for a more active and healthier world: the WHO Regional Offices perspective. Br J Sports Med [Internet]. 2020 Dec 1 [cited 2022 Sep 3];54(24):1449–50. Available online: https://bjsm.bmj.com/content/54/24/1449.
- Welbourn, R.; Hollyman, M.; Kinsman, R.; Dixon, J.; Liem, R.; Ottosson, J.; et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Fourth IFSO Global Registry Report 2018. Obesity Surgery 2018 29:3 [Internet]. 2018 Nov 12 [cited 2022 Sep 3];29(3):782–95. Available online: https://link.springer.com/article/10.1007/s11695-018-3593-1.
- Yuan, S.; Larsson, S.C. Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism [Internet]. 2023 Jul 1 [cited 2024 Aug 4];144:155533. Available online: http://www.metabolismjournal.com/article/S0026049523001361/fulltext.
- Ethgen, O.; Beaudart, C.; Buckinx, F.; Bruyère, O.; Reginster, J.Y. The Future Prevalence of Sarcopenia in Europe: A Claim for Public Health Action. Calcif Tissue Int [Internet]. 2017 Mar 1 [cited 2024 Aug 4];100(3):229–34. Available online: https://pubmed.ncbi.nlm.nih.gov/28012107/.
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L. , et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008 Jul;9(7):629–35.
- Ionut, V.; Burch, M.; Youdim, A.; Bergman, R.N. Gastrointestinal Hormones and Bariatric Surgery-induced Weight Loss. Obesity (Silver Spring) [Internet]. 2013 Jun [cited 2022 Jun 24];21(6):1093. Available from: /pmc/articles/PMC4423817/.
- Rios, I.N.M.S.; Lamarca, F.; Vieira, F.T.; de Melo, H.A.B.; Magalhães, K.G.; de Carvalho, K.M.B. et al. The Positive Impact of Resistance Training on Muscle Mass and Serum Leptin Levels in Patients 2-7 Years Post-Roux-en-Y Gastric Bypass: A Controlled Clinical Trial. Obes Surg [Internet]. 2021 Aug 1 [cited 2024 Jul 16];31(8):3758–67. Available online: https://pubmed.ncbi.nlm.nih.gov/34041699/.
- Dorling, J.L.; Clayton, D.J.; Jones, J.; Carter, W.G.; Thackray, A.E.; King, J.A. et al. A randomized crossover trial assessing the effects of acute exercise on appetite, circulating ghrelin concentrations, and butyrylcholinesterase activity in normal-weight males with variants of the obesity-linked FTO rs9939609 polymorphism. Am J Clin Nutr [Internet]. 2019 Nov 1 [cited 2022 Jun 25];110(5):1055–66. Available online: https://pubmed.ncbi.nlm.nih.gov/31504106/.
- Matei, B.; Winters-Stone, K.M.; Raber, J. Examining the Mechanisms behind Exercise’s Multifaceted Impacts on Body Composition, Cognition, and the Gut Microbiome in Cancer Survivors: Exploring the Links to Oxidative Stress and Inflammation. Antioxidants 2023, Vol 12, Page 1423 [Internet]. 2023 Jul 14 [cited 2024 Aug 3];12(7):1423. Available online: https://www.mdpi.com/2076-3921/12/7/1423/htm.
- Serna-Gutiérrez, A.; Castro-Juarez, A.A.; Romero-Martínez, M.; Alemán-Mateo, H.; Giovanni Díaz-Zavala, R.; Quihui-Cota, L.; et al. Prevalence of overweight, obesity and central obesity and factors associated with BMI in indigenous yaqui people: a probabilistic cross-sectional survey. 2021 [cited 2022 Sep 3]; [CrossRef]
- Kubik, J.F.; Gill, R.S.; Laffin, M.; Karmali, S. The impact of bariatric surgery on psychological health. J Obes. 2013;2013.
- Coleman, K.J.; Caparosa, S.L.; Nichols, J.F.; Fujioka, K.; Koebnick, C.; McCloskey, K.N. et al. Understanding the Capacity for Exercise in Post-Bariatric Patients. Obes Surg [Internet]. 2017 Jan 1 [cited 2022 Jun 25];27(1):51–8. Available online: https://pubmed.ncbi.nlm.nih.gov/27229736/.
- Balaguera-Cortes, L.; Wallman, K.E.; Fairchild, T.J.; Guelfi, K.J. Energy intake and appetite-related hormones following acute aerobic and resistance exercise. Applied Physiology, Nutrition and Metabolism. 2011 Dec;36(6):958–66.
- Ekici, E.; Özden, F.; Özkeskin, M. The Effect of Aerobic and Resistance Exercise after Bariatric Surgery: A Systematic Review. Surgeries 2023, Vol 4, Pages 367-380 [Internet]. 2023 Jul 18 [cited 2024 Aug 6];4(3):367–80. Available online: https://www.mdpi.com/2673-4095/4/3/37/htm.
- Thackray, A.E.; Stensel, D.J. The impact of acute exercise on appetite control: Current insights and future perspectives. Appetite. 2023 Jul 1;186:106557.
- Bellicha, A.; van Baak, M.A.; Battista, F.; Beaulieu, K.; Blundell, J.E.; Busetto, L. , et al. Effect of exercise training before and after bariatric surgery: A systematic review and meta-analysis. Obesity Reviews. 2021 Jul 1;22(S4).
- Cornejo-Pareja, I.; Clemente-Postigo, M.; Tinahones, F.J. Metabolic and Endocrine Consequences of Bariatric Surgery. Front Endocrinol (Lausanne) [Internet]. 2019 Sep 19 [cited 2024 Aug 6];10:439786. Available from: www.frontiersin.
- Casimiro, I.; Sam, S.; Brady, M.J. Endocrine implications of bariatric surgery: a review on the intersection between incretins, bone, and sex hormones. Physiol Rep [Internet]. 2019 May 1 [cited 2024 Aug 6];7(10):e14111. Available online: https://onlinelibrary.wiley.com/doi/full/10.14814/phy2.14111.
- Greenway, F.L. Physiological adaptations to weight loss and factors favouring weight regain. International Journal of Obesity 2015 39:8 [Internet]. 2015 Apr 21 [cited 2024 Aug 6];39(8):1188–96. Available online: https://www.nature.com/articles/ijo201559.
- Amaro Santos, C.; Cinza, A.M.; Laranjeira, Â.; Amaro, M.; Carvalho, M.; Martins, S. et al. The impact of exercise on prevention of sarcopenia after bariatric surgery: The study protocol of the EXPOBAR randomized controlled trial. Contemp Clin Trials Commun [Internet]. 2023 Feb 1 [cited 2022 Dec 29];31:101048. Available from: /pmc/articles/PMC9768230/.
- Santos, C.A.; Cinza, A.M.; Laranjeira, Â.; Amaro, M.; Carvalho, M.; Bravo, J. et al. A dataset on skeletal muscle mass index, body composition and strength to determinate sarcopenia in bariatric patients. Data Brief [Internet]. 2023 Feb 1 [cited 2024 Jul 16];46. Available online: http://www.data-in-brief.com/article/S2352340922010848/fulltext.
- Amaro Santos udia Margarida Cinza, A.; Laranjeira, Â.; Amaro, M.; Carvalho, M.; Bravo, J. et al. Effects of physical exercise in sarcopenia on patients undergoing bariatric surgery: A protocol for a randomized clinical trial. 2023 [cited 2024 Jul 16]; [CrossRef]
- Bushman, B.A. Determining the i (Intensity) for a FITT-VP aerobic exercise prescription. ACSMs Health Fit J [Internet]. 2014 [cited 2023 Nov 5];18(3):4–7. Available online: https://journals.lww.com/acsm-healthfitness/fulltext/2014/05000/determining_the_i__intensity__for_a_fitt_vp.4.aspx.
- Burke, L.M.; Slater, G.J.; Matthews, J.J.; Langan-Evans, C.; Horswill, C.A. ACSM Expert Consensus Statement on Weight Loss in Weight-Category Sports. Curr Sports Med Rep [Internet]. 2021 Apr 1 [cited 2024 Jul 9];20(4):199–217. Available online: https://journals.lww.com/acsm-csmr/fulltext/2021/04000/acsm_expert_consensus_statement_on_weight_loss_in.7.aspx.
- ACSM’s Guidelines for Exercise Testing and Prescription [Internet]. [cited 2024 Jul 11]. Available online: https://shop.lww.com/ACSM-s-Guidelines-for-Exercise-Testing-and-Prescription/p/9781975150181.
- Castello, V.; Simões, R.P.; Bassi, D.; Catai, A.M.; Arena, R.; Borghi-Silva, A. Impact of aerobic exercise training on heart rate variability and functional capacity in obese women after gastric bypass surgery. Obes Surg [Internet]. 2011 Nov [cited 2023 Nov 5];21(11):1739–49. Available online: https://pubmed.ncbi.nlm.nih.gov/21104041/.
- Cesari, M.; Kritchevsky, S.B.; Newman, A.B.; Simonsick, E.M.; Harris, T.B.; Penninx, B.W. et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging And Body Composition Study. J Am Geriatr Soc [Internet]. 2009 Feb [cited 2024 Apr 5];57(2):251–9. Available online: https://pubmed.ncbi.nlm.nih.gov/19207142/.
- Tsigos, C.; Hainer, V.; Basdevant, A.; Finer, N.; Mathus-Vliegen, E.; Micic, D. et al. Criteria for EASO-Collaborating Centres for Obesity Management. Obes Facts [Internet]. 2011 Aug [cited 2022 Jun 25];4(4):329. Available from: /pmc/articles/PMC6444795/.
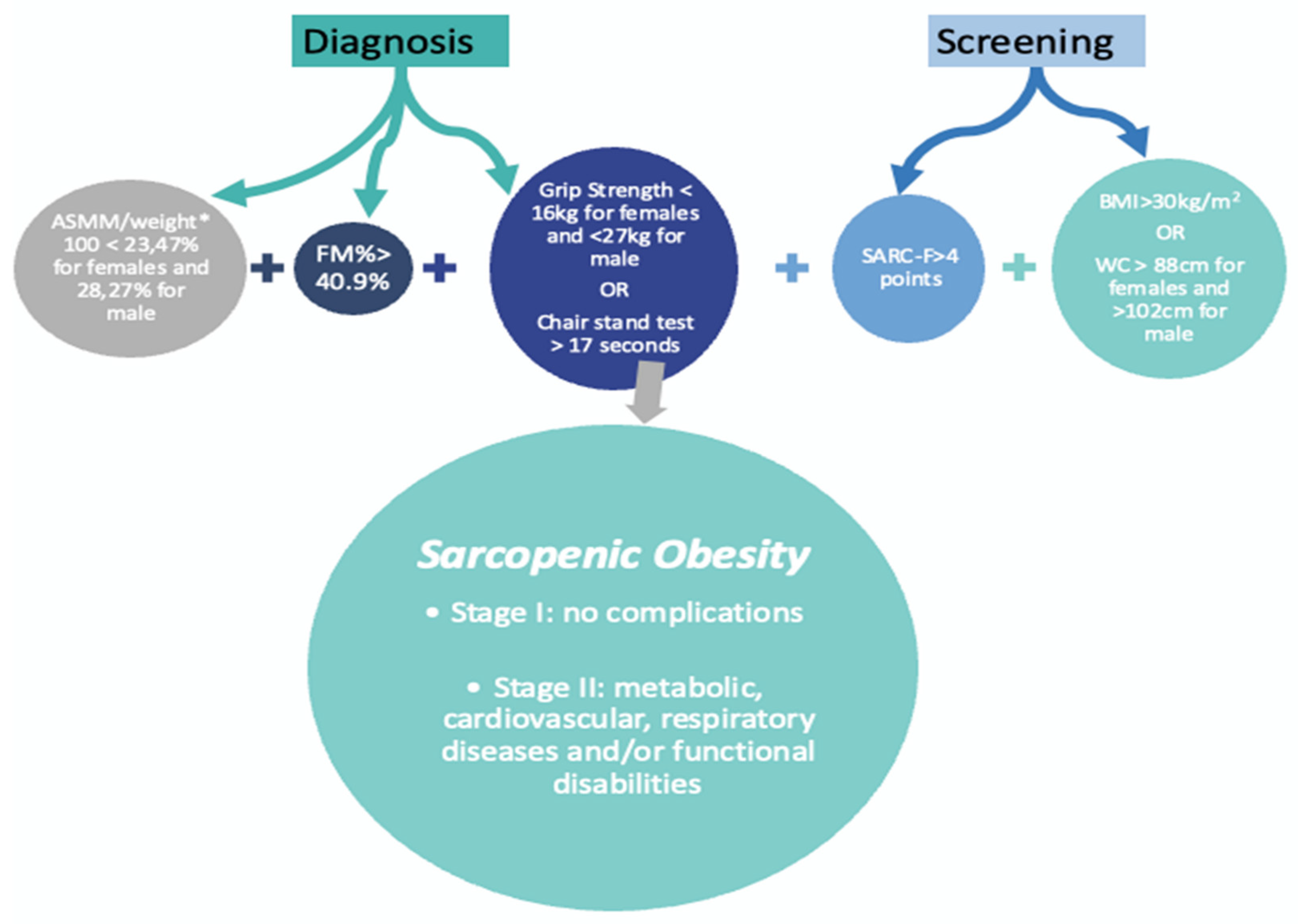
- Donini, L.M.; Busetto, L.; Bischoff, S.C.; Cederholm, T.; Ballesteros-Pomar, M.D.; Batsis, J.A. et al. Consensus Statement Definition and Diagnostic Criteria for Sarcopenic Obesity: ESPEN and EASO Consensus Statement. 2022 [cited 2022 Sep 13]; Available online: www.karger.com/ofa.
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences. Statistical Power Analysis for the Behavioral Sciences [Internet]. 2013 May 13 [cited 2024 Aug 28]; Available online: https://www.taylorfrancis.com/books/mono/10.4324/9780203771587/statistical-power-analysis-behavioral-sciences-jacob-cohen.
- van de Laar, A.W.; van Rijswijk, A.S.; Kakar, H.; Bruin, S.C. Sensitivity and Specificity of 50% Excess Weight Loss (50%EWL) and Twelve Other Bariatric Criteria for Weight Loss Success. Obes Surg [Internet]. 2018 Aug 1 [cited 2022 Nov 22];28(8):2297–304. Available online: https://pubmed.ncbi.nlm.nih.gov/29484610/.
- Mohammadi, S.M.; Saniee, N.; Borzoo, T.; Radmanesh, E. Osteoporosis and Leptin: A Systematic Review. Iran J Public Health [Internet]. 2024 [cited 2024 Jul 23];53(1):93–103. Available online: https://creativecommons.org/licenses/by-nc/4.0/.
- Mendes, C. Effects of exercise for the prevention of sarcopenia after bariatric surgery: A Systematic Review. 2023 Nov 8 [cited 2024 Aug 5]; Available online: https://www.researchsquare.com.
- Mendes, C.; Carvalho, M.; Bravo, J.; Martins, S.; Raimundo, A. Impact of Bariatric Surgery on Sarcopenia Related Parameters and Diagnosis—The Preliminary Results of EXPOBAR Study. 2024 Jul 12 [cited 2024 Aug 5]; Available online: https://www.preprints.org/manuscript/202407.1018/v1.
- Min, T.; Prior, S.L.; Dunseath, G.; Churm, R.; Barry, J.D.; Stephens, J.W. Temporal Effects of Bariatric Surgery on Adipokines, Inflammation and Oxidative Stress in Subjects with Impaired Glucose Homeostasis at 4 Years of Follow-up. Obes Surg [Internet]. 2020 May 1 [cited 2024 Aug 7];30(5):1712–8. Available online: https://link.springer.com/article/10.1007/s11695-019-04377-3.
- de Assis, G.G.; Murawska-Ciałowicz, E. Exercise and Weight Management: The Role of Leptin—A Systematic Review and Update of Clinical Data from 2000–2022. J Clin Med [Internet]. 2023 Jul 1 [cited 2024 Aug 7];12(13):4490. Available from: /pmc/articles/PMC10342435/.
- Kojima, M.; Hosoda, H.; Date, Y.; Nakazato, M.; Matsuo, H.; Kangawa, K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999 402:6762 [Internet]. 1999 Dec 9 [cited 2024 Aug 7];402(6762):656–60. Available online: https://www.nature.com/articles/45230.
- Frühbeck, G.; Diez-Caballero, A.; Gil, M.J.; Montero, I.; Gómez-Ambrosi, J.; Salvador, J. et al. The decrease in plasma ghrelin concentrations following bariatric surgery depends on the functional integrity of the fundus. Obes Surg [Internet]. 2004 May [cited 2024 Aug 7];14(5):606–12. Available online: https://pubmed.ncbi.nlm.nih.gov/15186626/.
- Frühbeck, G.; Rotellar, F.; Hernández-Lizoain, J.L.; Gil, M.J.; Gómez-Ambrosi, J.; Salvador, J. et al. Fasting plasma ghrelin concentrations 6 months after gastric bypass are not determined by weight loss or changes in insulinemia. Obes Surg [Internet]. 2004 Oct [cited 2024 Aug 7];14(9):1208–15. Available online: https://pubmed.ncbi.nlm.nih.gov/15527636/.
- Kruljac, I.; Mirošević, G.; Kirigin, L.S.; Nikolić, M.; Ljubičić, N.; Budimir, I. et al. Changes in metabolic hormones after bariatric surgery and their predictive impact on weight loss. Clin Endocrinol (Oxf) [Internet]. 2016 Dec 1 85(6):852–60. Available online: https://pubmed.ncbi.nlm.nih.gov/27439154/ (accessed on 7 August 2024).
- Karamanakos, S.N.; Vagenas, K.; Kalfarentzos, F.; Alexandrides, T.K. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg [Internet]. 2008 Mar [cited 2024 Aug 7];247(3):401–7. Available online: https://pubmed.ncbi.nlm.nih.gov/18376181/.
- Ghrelin and Adipose Tissue Regulatory Peptides: Effect of Gastric Bypass Surgery in Obese Humans | Oxford Academic [Internet]. [cited 2024 Aug 7]. Available online: https://oxfordjournals.org/view-large/53351672.
- Alamuddin, N.; Vetter, M.L.; Ahima, R.S.; Hesson, L.; Ritter, S.; Minnick, A. et al. Changes in Fasting and Prandial Gut and Adiposity Hormones Following Vertical Sleeve Gastrectomy or Roux-en-Y-Gastric Bypass: an 18-Month Prospective Study. Obes Surg [Internet]. 2017 Jun 1 [cited 2024 Aug 7];27(6):1563–72. Available online: https://pubmed.ncbi.nlm.nih.gov/28004304/.
- Tsouristakis, A.I.; Febres, G.; McMahon, D.J.; Tchang, B.; Conwell, I.M.; Tsang, A.J. et al. Long-Term Modulation of Appetitive Hormones and Sweet Cravings After Adjustable Gastric Banding and Roux-en-Y Gastric Bypass. Obes Surg [Internet]. 2019 Nov 1 [cited 2024 Aug 7];29(11):3698–705. Available online: https://pubmed.ncbi.nlm.nih.gov/31376135/.
- Ouerghi, N.; Feki, M.; Bragazzi, N.L.; Knechtle, B.; Hill, L.; Nikolaidis, P.T. et al. Ghrelin Response to Acute and Chronic Exercise: Insights and Implications from a Systematic Review of the Literature. Sports Med [Internet]. 2021 Nov 1 [cited 2024 Aug 7];51(11):2389. Available from: /pmc/articles/PMC8514378/.
- Malin, S.K.; Heiston, E.M.; Gilbertson, N.M.; Eichner, N.Z.M. Short-term interval exercise suppresses acylated ghrelin and hunger during caloric restriction in women with obesity. Physiol Behav. 2020 Sep 1;223:112978.
- Gunton, J.E.; Girgis, C.M. Vitamin D and muscle. Bone Rep [Internet]. 2018 Jun 1 [cited 2024 Aug 7];8:163. Available from: /pmc/articles/PMC6021354/.
- Zhang, J.; Jiang, J.; Qin, Y.; Zhang, Y.; Wu, Y.; Xu, H. Systemic immune-inflammation index is associated with decreased bone mass density and osteoporosis in postmenopausal women but not in premenopausal women. Endocr Connect [Internet]. 2023 Feb 1 [cited 2024 Aug 5];12(2). Available online: https://ec.bioscientifica.com/view/journals/ec/12/2/EC-22-0461.xml.
- Matos, O.; Ruthes, E.M.P.; Malinowski, A.K.C.; Lima, A.L.; Veiga, M.S.; Krause, M.P. et al. Changes in bone mass and body composition after bariatric surgery. Gynecol Endocrinol [Internet]. 2020 Jul 2 [cited 2022 May 22];36(7):578–81. Available online: https://pubmed.ncbi.nlm.nih.gov/32406280/.
- Mohammadi, S.M.; Saniee, N.; Borzoo, T.; Radmanesh, E. Osteoporosis and Leptin: A Systematic Review. Iran J Public Health [Internet]. 2024 [cited 2024 Aug 7];53(1):93. Available from: /pmc/articles/PMC11058394/.
| Parameter (Mean ± SD) | Intervention Group n=12 |
Control Group n=10 |
p value |
|---|---|---|---|
| Sex (% female) | 75% | 90% | 0.388 |
| Age (years) | 44.08 ± 13.2 | 50.4 ± 11.1 | 0.240 |
| Weight (kg) | 117.1 ± 15.8 | 103.6 ± 16.9 | 0.067 |
| BMI (kg/m2) | 43.1 ± 5.17 | 41.8 ± 3.40 | 0.388 |
| Leptin (ng/mL) | 54.6 ± 29.75 | 50.9 ± 28.47 | 0.355 |
| Ghrelin (pg/mL) | 811 ± 762.72 | 1261 ± 1424 | 0.773 |
| Baseline | 6 months | Sig. | d | |||
|---|---|---|---|---|---|---|
| CG | IG | CG | IG | |||
| Weight (kg) | 103.55 ± 16.86 | 117.08 ± 15.79 | 73.5 ± 13.2a | 83.0±12.4a | p= 0.099 | 0.425 |
| BMI (kg/m2) | 41.8 ± 3.40 | 43.10 ± 5.17 | 29.4 ± 2.62 a | 30.6 ± 4.37 a | p= 0.821 | 0.067 |
| Leptin (ng/mL) | 50.9 ± 28.47 | 54.6 ± 29.75 | 17.0 ± 18.0 a | 42.5 ± 44.1 | p= 0.050 | 0.013 |
| Ghrelin (pg/mL) | 1261 ± 1424 | 811 ± 762.72 | 2870 ± 2230 | 1311 ± 968 | p= 0.175 | 0.067 |
| Body fat (%) | 46.60 ± 3.23 | 46.7 ± 6.47 | 39.5 ± 5.91 a | 37.2 ± 8.02a | p= 0.107 | 0.417 |
| Handgrip (kg) | 20.60 ± 7.18 | 25.5 ± 6.87 | 16.4 ± 5.79 a | 22.2 ± 7.09 | p= 0.050 | 0.500 |
| Lean mass (kg) | 53.45 ± 12.48 | 58.19 ± 8.02 | 45.23 ± 11.47 a | 43.38 ± 9.07a | p= 0.456 | 0.200 |
| BMC (kg) | 2.33 ± 0.44 | 2.50 ± 0.37 | 1.96 ± 0.17 a | 2.42 ± 0.37 | p= 0.004 | 0.733 |
| BMD (g/cm2) | 1.14 ± 0.13 | 1.21 ± 0.17 | 1.10 ± 0.08 | 1.16 ± 0.12 | p= 0.276 | 0.283 |
| Total Body T score | 0.43 ± 1.51 | 0.54 ± 1.51 | -0.07 ± 0.68 | 0.76 ± 1.23 | p= 0.306 | 0.267 |
| Total Body Z score | 0.55 ± 1.14 | 0.49 ± 1.22 | 0.15 ± 0.46 | 0.49 ± 1.23 | p= 0.842 | 0.058 |
| Leptin (ng/mL) | Ghrelin (pg/mL) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| CG | IG | CG | IG | ||||||
| r | p value | r | p value | r | p value | r | p value | ||
| Age (years) | -0.384 | 0.921 | -0.369 | 0.903 | -0.088 | 0.622 | -0.059 | 0.579 | |
| %TWL (%) | -0.518 | 0.937 | 0.194 | 0.273 | 0.353 | 0.159 | 0.314 | 0.160 | |
| Weight (kg) | 0.475 | 0.009 | 0.102 | 0.376 | 0.356 | 0.156 | -0.145 | 0.673 | |
| BMI (kg/m2) | 0.625 | 0.022 | 0.051 | 0.431 | 0.137 | 0.353 | -0.167 | 0.716 | |
| Body fat (%) | 0.359 | 0.154 | 0.225 | 0.241 | 0.230 | 0.205 | 0.040 | 0.245 | |
| Handgrip (kg) | 0.689 | 0.014 | -0.068 | 0.658 | 0.027 | 0.470 | -0.097 | 0.618 | |
| Lean mass (kg) | 0.718 | 0.010 | -0.316 | 0.841 | 0.502 | 0.028 | -0.151 | 0.680 | |
| BMC (g) | 0.144 | 0.304 | -0.094 | 0.561 | 0.348 | 0.162 | -0.084 | 0.612 | |
| BMD (g/cm2) | 0.709 | 0.011 | -0.008 | 0.510 | 0.341 | 0.167 | 0.208 | 0.258 | |
| Total Body T score | 0.171 | 0.319 | 0.510 | 0.045 | 0.578 | 0.040 | 0.640 | 0.012 | |
| Total Body Z score | 0.197 | 0.293 | 0.283 | 0.186 | 0.673 | 0.016 | 0.628 | 0.014 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





