1. Introduction
The serum level of vitamin D plays a crucial role not only in the healthy development of children and the maintenance of adult health (considering its relevance in different diseases) [
1] but also serves a protective function against acute infections in the oropharyngeal level [
2,
3]. It is vital to continue studies on the association between vitamin D and oropharyngeal diseases to effectively manage these conditions, especially considering their prevalence in early childhood [
4]. Vitamin D deficiency is a significant global concern, given the established links between these deficiencies and various acute and chronic conditions. Particularly, there is limited data on the vitamin D status among hospitalized children with non-critical illnesses, highlighting the necessity to investigate and better understand the impact of this deficiency on the health of this patient group [
5].
Despite the implementation of vitamin D fortification programs over the past two decades, the prevalence of rickets has increased significantly. Although nutritional rickets is a preventable disease by maintaining an adequate intake of vitamin D through both dietary sources and sunlight exposure, eating fast food, junk food, or simply having a unilateral and undiversified diet greatly reduces the likelihood of managing rickets [
6,
7]. Globally, preschool children face a heightened risk of micronutrient deficiency, leading to substantial morbidity and mortality [
8].
The COVID-19 pandemic has further exacerbated malnutrition with micronutrients, impacting the quality of the diet and the food security, and considerably affecting the intake of beneficial active substances for the body, which has reflected on immunity and health status. [
9,
10,
11,
12]. The consequences include a rise in vitamin D deficiency, which, in turn, contributes to clinical manifestations such as fractures, bone deformities, seizures, and stridor in young children and adults [
13,
14]. The impact extends to pregnancy, where low vitamin D status is associated with the infant's low vitamin D status at birth, and poor intake of vitamin D-rich foods or supplements in childhood heightens the risk [
15].
Vitamin D reduces inflammation and enhances the clearance of viruses in the lungs, also supplementation has been observed to significantly decrease levels of interleukin 6 (IL-6), a prognostic marker [
16].
The association between body mass index (BMI) and vitamin D in childhood has been a subject of considerable investigation in scientific literature. Numerous studies have consistently reported an inverse relationship between BMI and vitamin D levels in pediatric populations. For instance, a study found that as BMI increased, there was a corresponding decrease in serum vitamin D concentrations [
17]. Another study by Akter et al. (2022) supported these findings, indicating a negative correlation between BMI and vitamin D levels in a diverse sample of children [
18].
The inverse association between BMI and vitamin D may be attributed to various factors, including lifestyle choices and limited sun exposure. Insights from the National Health and Nutrition Examination Survey (NHANES) study [
19] suggested that decreased outdoor activities and inadequate sunlight exposure, essential for endogenous vitamin D synthesis, contribute to lower vitamin D levels in patients with higher BMI. According to WHO, the best indicator of vitamin D stores is the blood serum concentration of 25-hydroxyvitamin D (25(OH)D). Levels below 30 nmol/L indicate deficiency risk, while healthy levels for infants are 50 nmol/L or above. In infants, stores can decline rapidly without adequate vitamin D [
20].
Furthermore, the impact of adipose tissue on vitamin D bioavailability is noteworthy. Adipose tissue, prevalent in individuals with higher BMI, may sequester vitamin D, making it less available for circulation. This observation aligns with research by Drincic et al. [
21], emphasizing the role of adiposity in influencing vitamin D status.
Understanding the intricate dynamics between BMI and vitamin D in childhood is crucial for promoting optimal health. Adequate vitamin D is essential for bone health and overall well-being in patients. As childhood obesity rates rise globally, addressing the complex relationship between BMI and vitamin D becomes imperative for public health interventions. Continued research, such as that conducted by Cashman et al. [
22], is essential to further elucidate the mechanisms underlying this relationship and inform targeted strategies for improving vitamin D status in pediatric populations.
The observations revealed direct links between vitamin D deficiency and dermatological diseases involved in the regulation of the processing of long-chain glycosylceramides, which are critical for the formation of the skin barrier but also play an important role in skin aging, being directly correlated to the formation of collagen. The role of vitamin D in immunological diseases has been particularly evident in the last decade, where a direct link was found between metabolic and inflammatory autoimmune diseases, with vitamin D deficiency being directly correlated with inflammatory bowel disease and colon cancer [
23,
24,
25].
The study seeks to explore the correlation between vitamin D levels, behavioral disorders, and the recurrence of oropharyngeal infections (nasopharyngitis, otitis media, and rhinosinusitis). It aims to provide a comprehensive view of the role of vitamin D in managing these infections, particularly considering the sensitive issue of antibiotic consumption. The research will analyze how these diseases distribute across different sexes and investigate the influence of age and environment on vitamin D levels. By examining these factors, the study aims to uncover potential connections and demographic influences, providing insights into the relationship between vitamin D levels and the prevalence and recurrence of respiratory diseases.
2. Materials and Methods
Between 2022 and 2023, a prospective study was conducted at a private otolaryngology (ENT) practice, in accordance with the guidelines outlined in the World Medical Association's Declaration of Helsinki. The patient visited the private specialized medical clinic " OTORHINOMED" (Oradea, Romania) with their legal representative, reporting oto-rhino-pharyngeal issues (nasopharyngitis, otitis media, and rhinosinusitis). A clinical assessment was conducted. Each patient was followed by the ENT specialist for 6 months, with weekly visits during the acute phase or every 3 days in case of complications, and then monthly, from January 2023 to January 2024. Patients followed their general diet, except for those with severe malnutrition. Sun exposure was reduced or moderate for all patients.
Inclusion Criteria:
Patients aged between 0 and 73 years, presenting acute forms of oropharyngeal diseases, particularly nasopharyngitis, otitis media, and rhinosinusitis, were included in the study. Patients must have a confirmed diagnosis of acute oropharyngeal infections, specifically nasopharyngitis, otitis media, or rhinosinusitis. These diagnoses must adhere to the current clinical guidelines for acute infections, characterized by:
Nasopharyngitis: Acute onset of nasal congestion, rhinorrhea, sore throat, and possible fever.
Otitis Media: Sudden onset of ear pain, otorrhea, or hearing loss, with possible tympanic membrane inflammation observed during otoscopy.
Rhinosinusitis: Acute inflammation of the nasal passages and sinuses, presenting with symptoms such as facial pain, nasal discharge, and congestion.
Exclusion Criteria:
Individuals aged over 73 years, those without vitamin D (25(OH)D3) measurements, individuals with diseases other than the specified acute oropharyngeal conditions, including chronic ailments that could impact serum vitamin D levels (e.g., osteoporosis), malnutrition, and those who declined participation were excluded from the study.
The study, involving 311 patients with an average age of 15.96±15.06 years, aimed to examine the correlation between serum vitamin D levels and prevalent oropharyngeal diseases in children and adults, including rhinosinusitis, otitis media, and nasopharyngitis. The cohort was stratified into four groups based on the cumulative number of acute diseases as follows:
- a control group without any acute illness (0), with 32 persons (10,3%)
- a group with one acute disease (1), with 111 patients (35,7%)
- a group with two acute diseases (2), with 125 peoples (40,2%) and
- a group with all three cumulative acute diseases (3), with 43 persons (13,8%).
Each patient underwent testing using a rapid vitamin D test.
2.1. Clinical and Paraclinical Investigation:
The clinical assessment took place at the medical office (OTORHINOMED, Romania), while the evaluation of paraclinical parameters was conducted at authorized laboratories. Paraclinical examinations included checking the blood pressure, blood sugar levels, and behavioral disorders. Lack of concentration, anxiety, exhaustion, aggressiveness, and hyperactivity were considered behavioral disorders. The patients completed the anamnesis sheet, and if at least one of these disorders was present, they were included in the group with behavioral disorders. Furthermore, a thorough local clinical examination was performed, taking into consideration the comprehensive medical history. The clinical assessment utilized the Tanita MC780MA, a bioelectrical impedance body analyzer (BIA) sourced from Tokyo, Japan [
26]. The obtained data were analyzed through the GMON 3.4.1 medical software developed in Chemnitz, Germany. Recognized by the World Public Health Nutrition Association (WPHNA), BIA body analyzers are renowned for their high accuracy and are frequently employed in assessing body composition. Up to the age of 18, BMI percentile was employed for assessment. The margin of error for the measurements was minimal, at 0.1 kg.
2.2. Rapid Vitamin D Test:
For testing the vitamin D level, a rapid, cassette-type test can be utilized to semi-quantitatively detect 25-hydroxyvitamin D in whole blood using a fingerstick sample. The Vitamin D Rapid Test Kit employs a rapid chromatographic immunoassay to semi-quantitatively identify 25-hydroxyvitamin D (25(OH)D) in whole human blood. It provides a preliminary diagnostic test result and can be used to assess vitamin D deficiency. The JusChek (Bucharest, Romania) rapid test was employed to conduct vitamin D testing and to colorimetrically determine the baseline vitamin D (25(OH)D) level. As a result, there are four categories for interpreting the results:
Insufficient: 0-20 µg/ml
Adequate: 21-29 µg/ml
Optimal: 30-55.5 µg/ml
Excessive: 55.5-150 µg/ml
The patients in the study initially did not receive regular vitamin D supplementation, possibly only for a short period, and their exposure to the sun was average or low, according to local statistics. After testing their vitamin D levels, supplementation was recommended where appropriate, based on age, with a reevaluation of vitamin D levels scheduled after 3 months. I have completed the manuscript.
2.3. Statistical Analysis:
The data analysis utilized the Statistical Product and Service Solutions (version 20; IBM, Armonk, NY, USA) computer software program. Demographic variables, procedure frequency, and cost data obtained from the medical office were assessed for the two surveyed time points and across the two study groups to identify noteworthy trends. Calculations for means, frequency ranges, standard deviations, and tests of statistical significance were performed using Student's t-test and the chi-square test. The Bravais–Pearson correlation coefficient gauged the relationship between the two variables. A level of p<0.05 denoted statistical significance, while p<0.01 indicated a high level of statistical significance. Post-hoc analysis (Bonferroni) was implemented for additional subgroup analysis to scrutinize distinctions between groups.
3. Results
3.1. Demographic Description
The study, involving 311 patients with an average age of 15.96±15.06 years, aimed to investigate the correlation between serum vitamin D levels and prevalent oropharyngeal diseases in children (rhinosinusitis, otitis media, and nasopharyngitis). The sample was assessed for skewness and kurtosis, with values falling between -3.000 and 3.000, and analyzed using a 95% confidence interval.
Notably, boys exhibited multiple episodes of rhinosinusitis, with 53.4% of recurrent otitis media cases, having 4 more episodes in girls and 5 more episodes in boys. A high frequency of nasopharyngitis episodes in the last 6 months (83.3%) was observed, predominantly in females. Over half of the subjects (52.7%) had deficiencies or insufficient vitamin D levels, predominantly among females. A significant majority (89.7%) experienced at least one of the respective diseases, with 13.8% having all three acute forms.
In a comparative study on individuals from urban and rural environments, the following observations were made: Nasopharyngitis was more common in rural areas, with 29.3% of people experiencing an episode, compared to 24.4% in urban areas. Otitis media was reported more often in urban areas, with 25.4% having episodes compared to 21.2% in rural areas. Rhinosinusitis had a higher prevalence in urban areas, with 44.4% experiencing episodes compared to 34.7% in rural areas. Regarding cumulative diseases, the rural environment presented fewer disease-free cases (2.9%) compared to the urban environment (7.4%). Behavioral disorders were more common in urban areas (35.4%) than in rural areas (27.3%). The study revealed a statistical association between decreased vitamin D levels and a significant increase in disease frequency, particularly in nasopharyngitis, otitis media, and when considering all cumulative diseases. Boys were more commonly affected by two cumulative diseases, while three cumulative diseases were more prevalent in girls, presented in
Table 1.
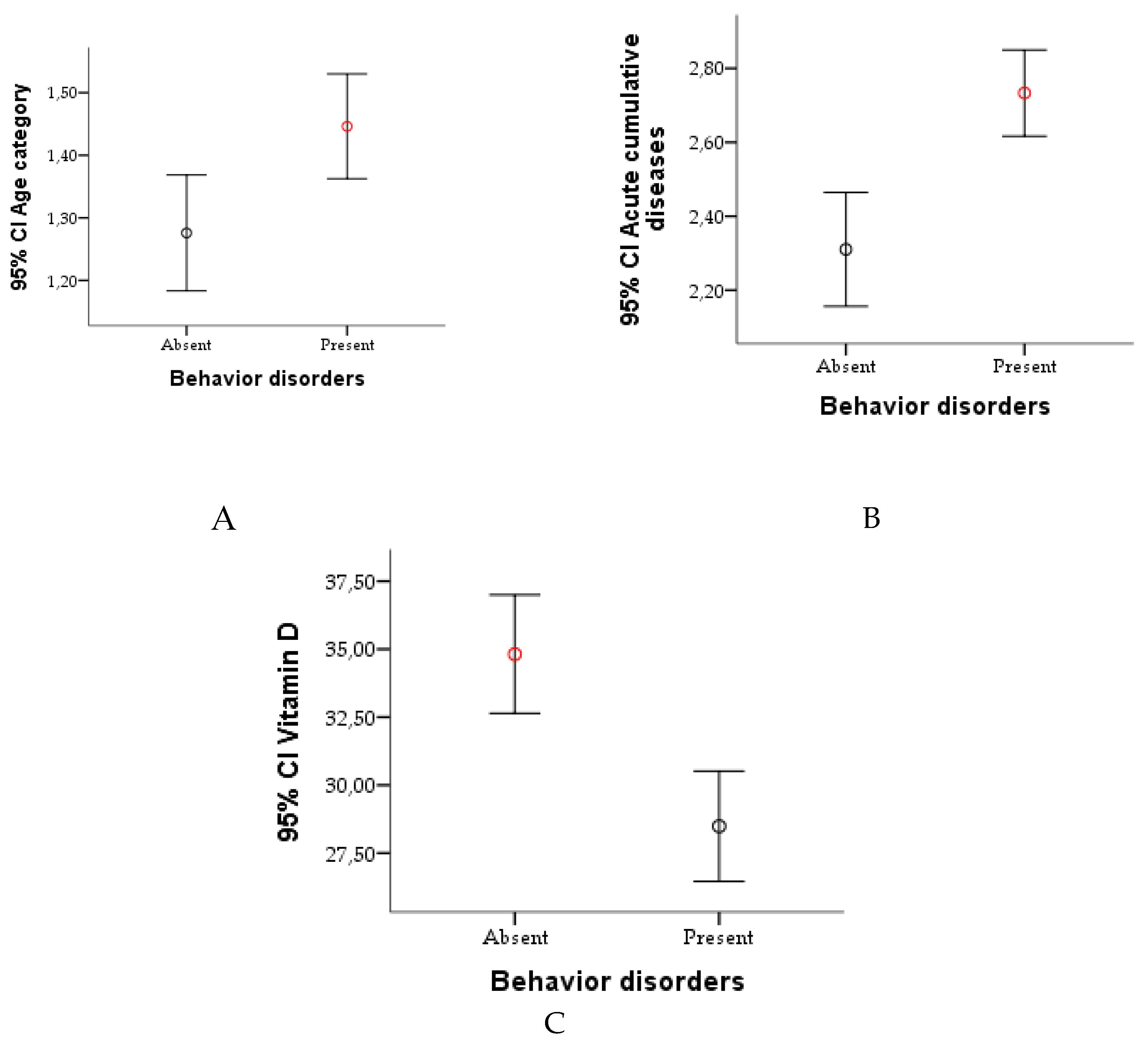
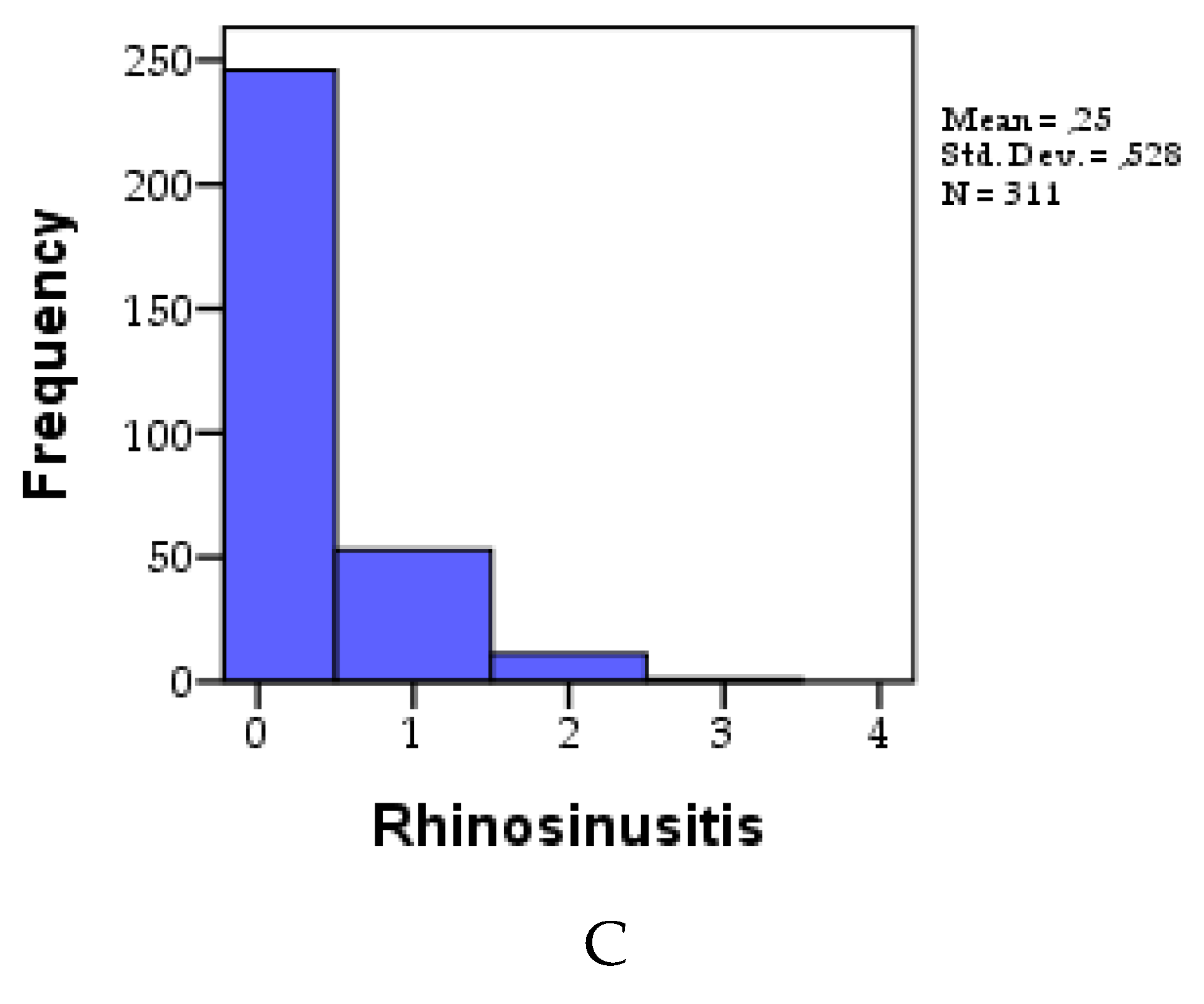
3.2. Description of Acute Diseases and Their Recurrence:
At the cohort level, the study meticulously monitored three acute diseases—namely, nasopharyngitis, otitis media, and rhinosinusitis—and tracked their recurrence over the preceding 6 months. Nasopharyngitis manifested in 259 individuals (83.27%) at least once, exhibiting a recurrence frequency of 1.30±1.01, visually represented in
Figure 1A. Otitis media, while less prevalent, was identified in 166 individuals (53.37%), displaying a recurrence frequency of 0.96±1.16, as elucidated in
Figure 1B. Rhinosinusitis occurred in 65 individuals (20.90%) at least once during the 6-month study period, with a recurrence frequency of 0.25±0.53, visually depicted in
Figure 1C.
3.3. Frequency of Diseases According to Gender
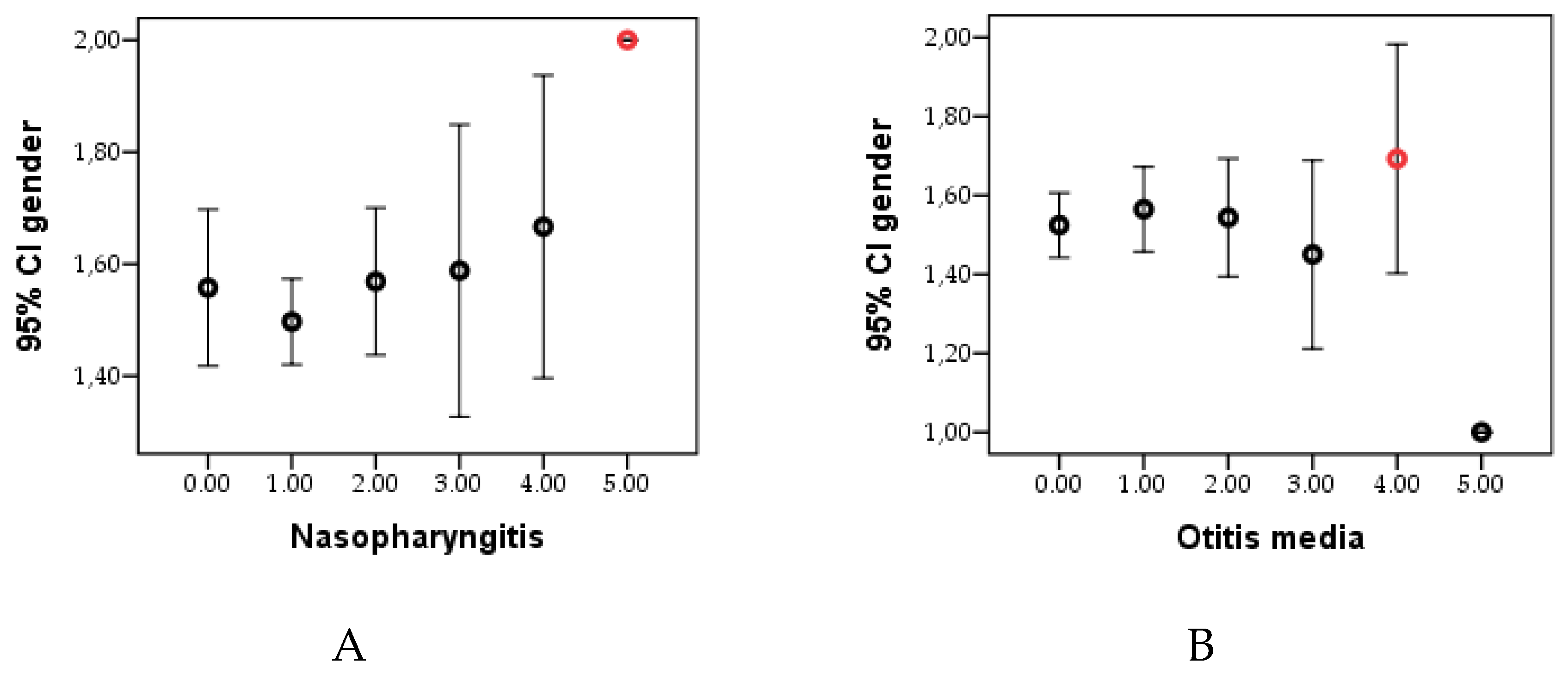
The comprehensive depiction of disease distribution according to gender is visually presented in
Figure 2. Intriguingly, the highest frequency of diseases is discerned among girls, with the exception of otitis, which exhibits greater prevalence in boys. An in-depth statistical analysis revealed that for the control group, differences between the sexes were statistically insignificant (p>0.05). However, when delving into the recurrence frequencies of 3, 4, or 5, noteworthy and statistically significant differences (p<0.05) emerged between males and females. This nuanced exploration underscores the gender-specific variations in disease occurrence and recurrence, providing valuable insights into potential predispositions or susceptibilities within the studied cohort.
For nasopharyngitis, 7.4% of males and 9.3% of females had no episodes, while 27.0% of males and 26.7% of females had one episode. A higher percentage of females experienced two episodes (10.6%) compared to males (8.0%). For otitis media, 22.2% of males and 24.4% of females had no episodes. A notable difference is that more females experienced one episode (15.4%) compared to males (11.9%). Regarding rhinosinusitis, 39.9% of males and 39.2% of females had no episodes. Females had a higher prevalence of one episode (11.9%) compared to males (5.1%).
3.4. Vitamin D Level by Cohort
Following serum vitamin D level testing, with an average value per cohort of 30.85±13.81, the results were categorized into four groups based on the obtained values: 0-20 (deficiency), 20-29 (insufficient), 30-55.5 (optimal), and 55.5-150 (high). For a more accurate assessment of vitamin D levels by age category, the 0-18 years group was divided into two subgroups: 0-15 years and 16-18 years.
Table 2 reveals a lower level of vitamin D in older individuals, with patients having the highest levels (average age of 6.80±9.83), and these differences were statistically significant (p< 0.05). Statistically insignificant differences were observed between genders based on the vitamin D level category (p>0.05), while a significant discrepancy was noted, with more individuals from rural areas facing vitamin D deficiency compared to those from urban areas (p<0.05). It was observed that in the 16-18 years age category, as well as in the under 45 years category, no patient had an optimal level of vitamin D.
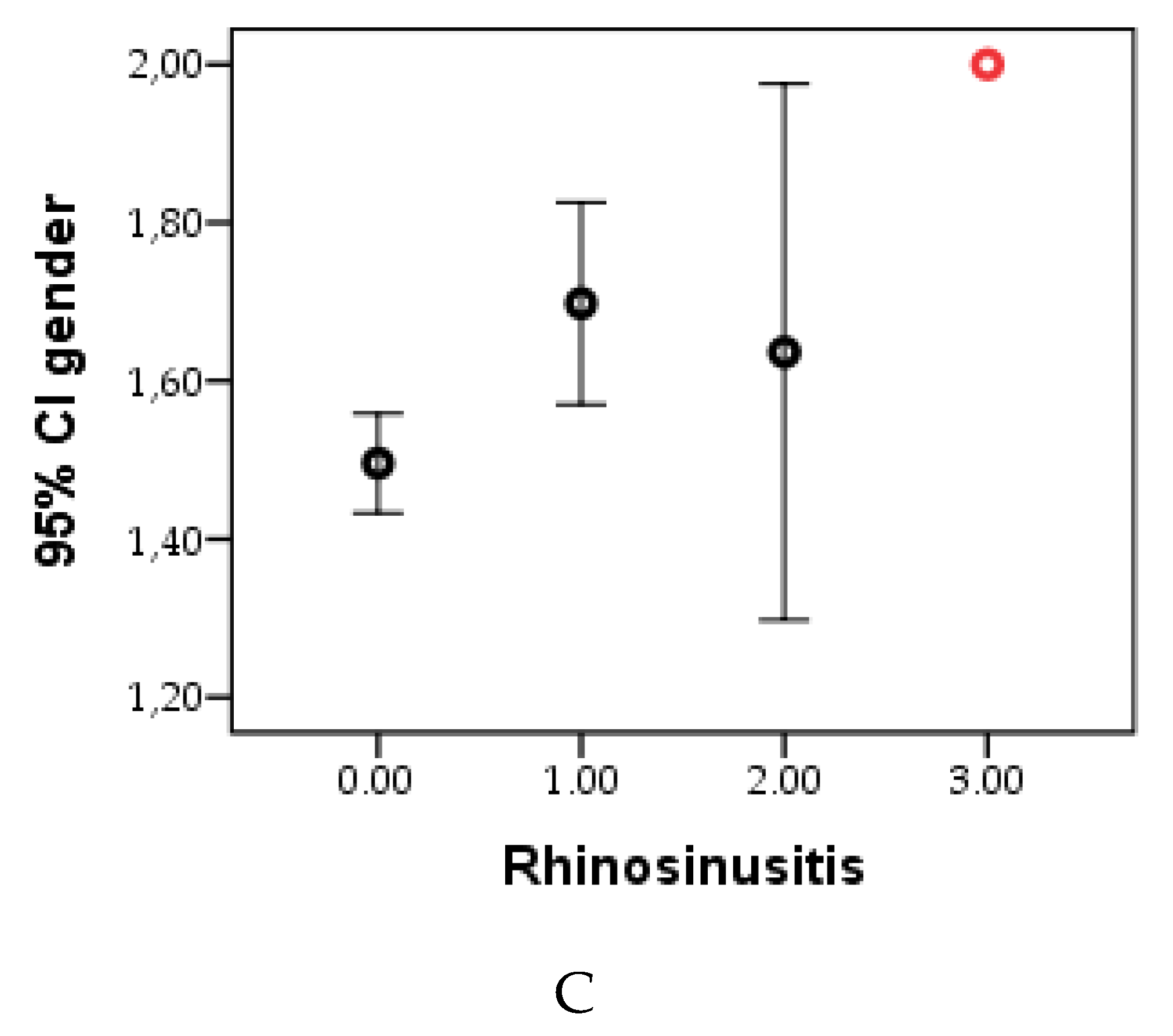
Regarding disease recurrence based on vitamin D levels,
Figure 3 illustrates a higher recurrence in nasopharyngitis for those with vitamin D deficiency (
Figure 3A), recurrent otitis in individuals with low vitamin D levels (
Figure 3B), and rhinosinusitis with recurrence 3 observed in the sole patient (Patient 1) with vitamin D deficiency (
Figure 3C). The fewest recurrences were recorded at high vitamin D levels.
Following statistical analysis, the mean recurrence in nasopharyngitis was 1.91±1.15 in individuals with vitamin D deficiency (0-20), significantly higher (p=0.001) than 0.93±0.59. The average frequency of otitis was highest at 1.38±1.40 in those with deficiency and lowest at 0.20±0.56 in individuals with high vitamin D levels (p=0.023). Rhinosinusitis exhibited an exceptional case in those with a high vitamin D level, while more frequent recurrence was noted in individuals with vitamin D deficiency.
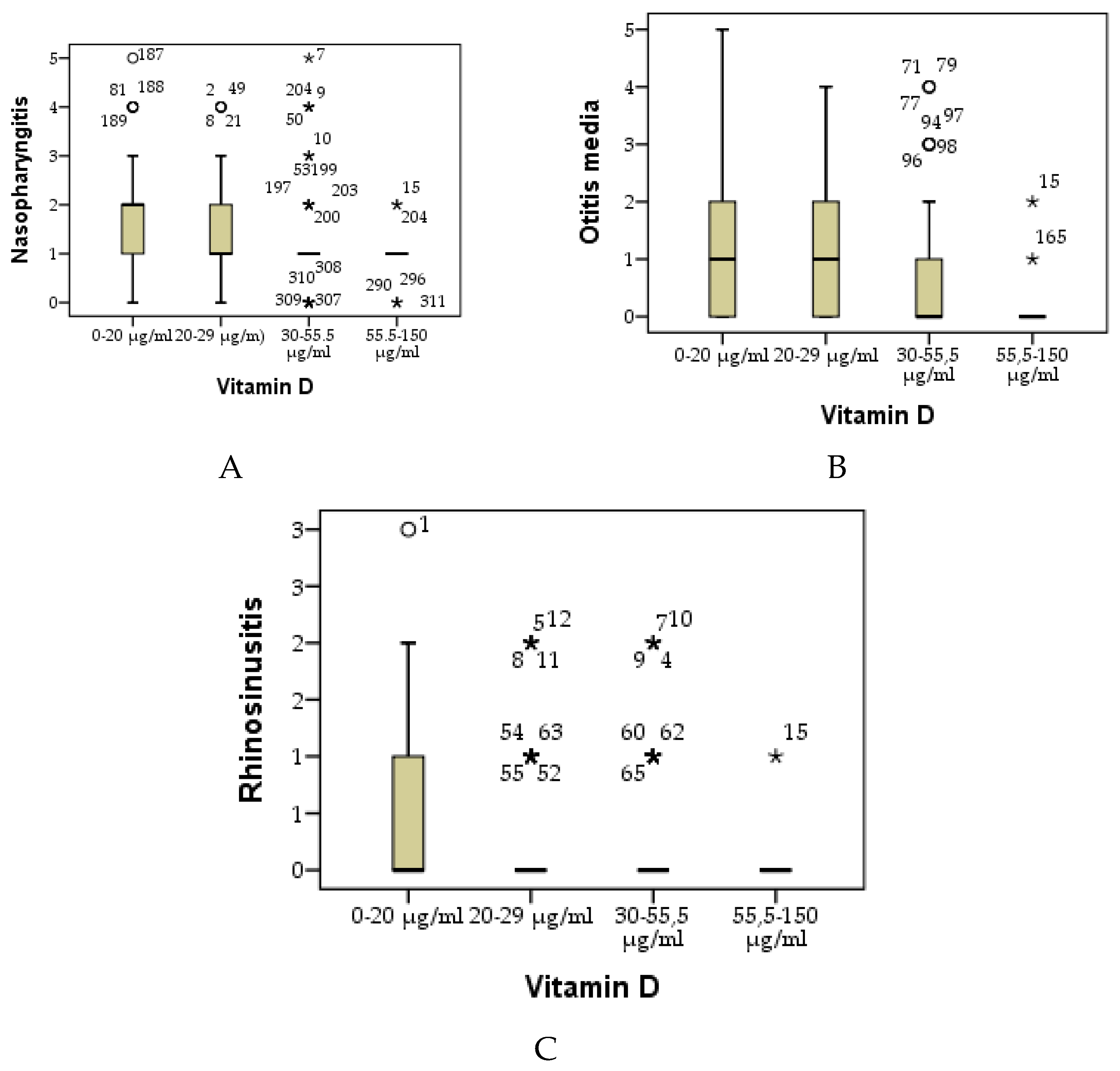
3.5. Cumulative Diseases
Patients experiencing one, two, or all three of the acute conditions were monitored and assessed based on their serum vitamin D levels, as depicted in
Figure 4. The highest value (36.66±12.88) was observed in the control group comprising individuals without any of the tracked diseases. Simultaneously, a trend of decreasing vitamin D levels was noted: 35.54±16.97 in those with only one of the tracked diseases, 26.08±9.05 in individuals with two tracked diseases, and 28.29±11.45 in those with all three conditions encountered in the last 6 months.
3.6. Description of Body Status
At the cohort level, the average BMI was recorded as 20.90 ± 7.04 kg/m². In boys, the average BMI was 19.42 ± 6.44, while in girls, it was higher at 22.17 ± 7.31. It was observed that individuals from urban environments had a higher BMI (21.50 ± 7.34) compared to those from rural environments (20.21 ± 6.64).
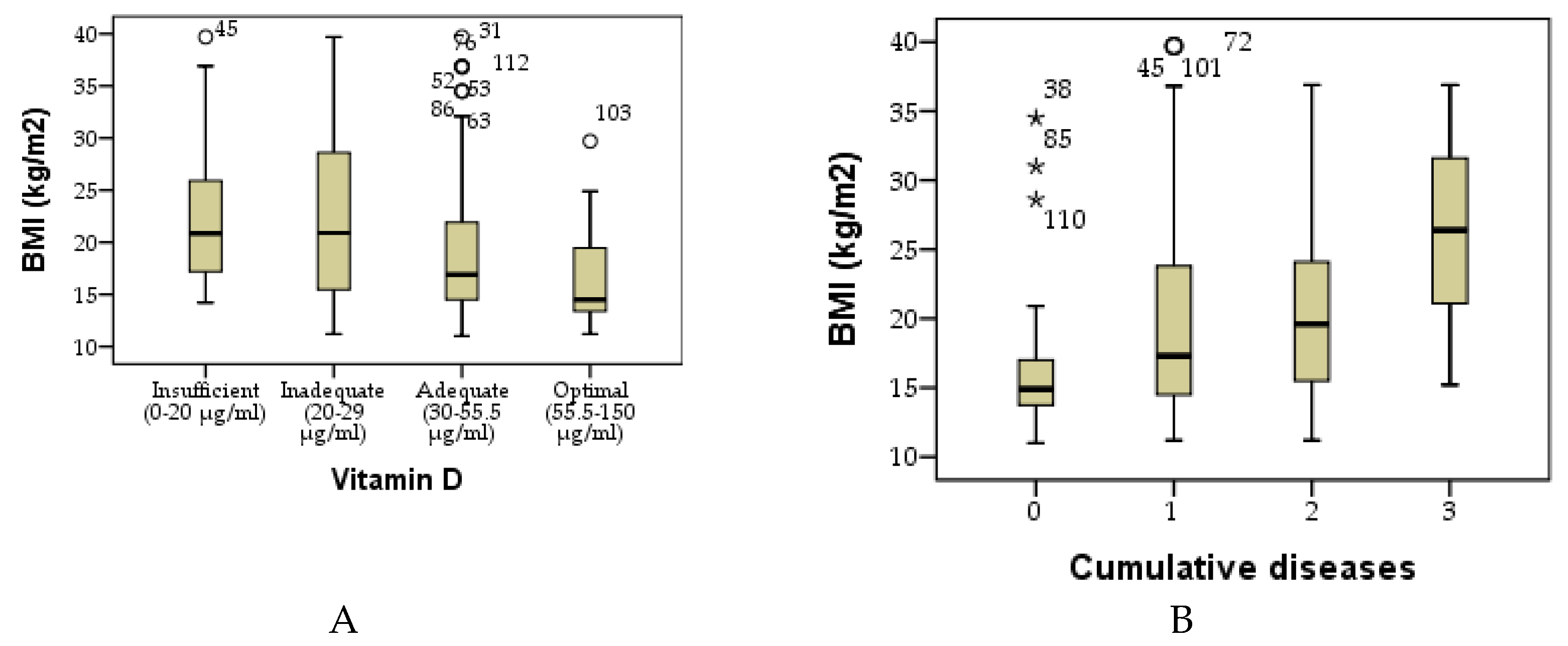
When examining the average BMI based on the category of vitamin D (
Figure 5A), a higher BMI was evident in individuals with insufficient and inadequate vitamin D levels, with no statistically significant difference between them (p > 0.05). Conversely, at adequate or optimal levels of vitamin D, a lower BMI was recorded, falling within the normal range.
In terms of the number of cumulative diseases, a statistically significant increase in BMI (p = 0.001) was observed in individuals with three cumulative diseases compared to those with no cumulative diseases (
Figure 5B).
3.7. Behavior Disorders
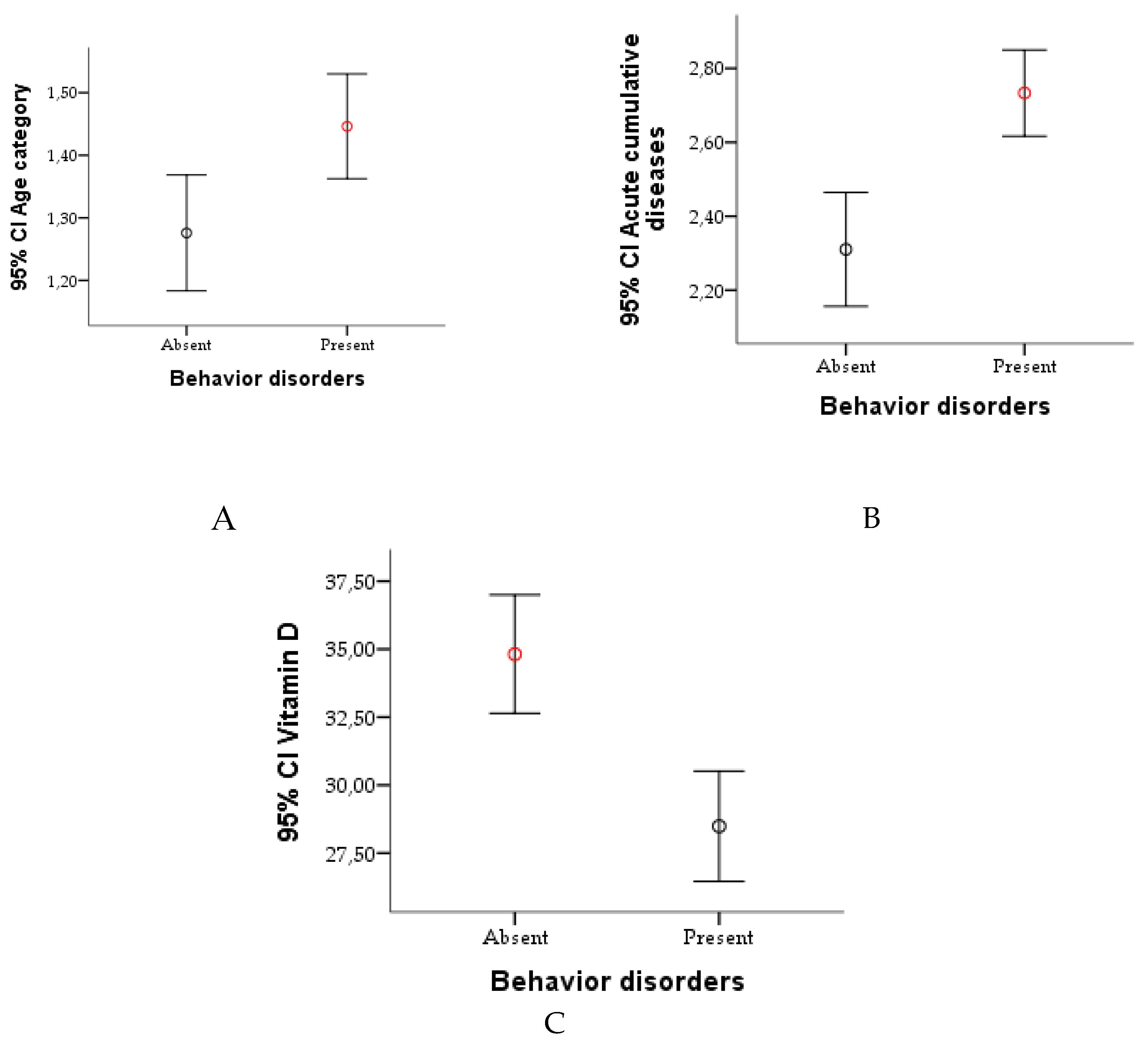
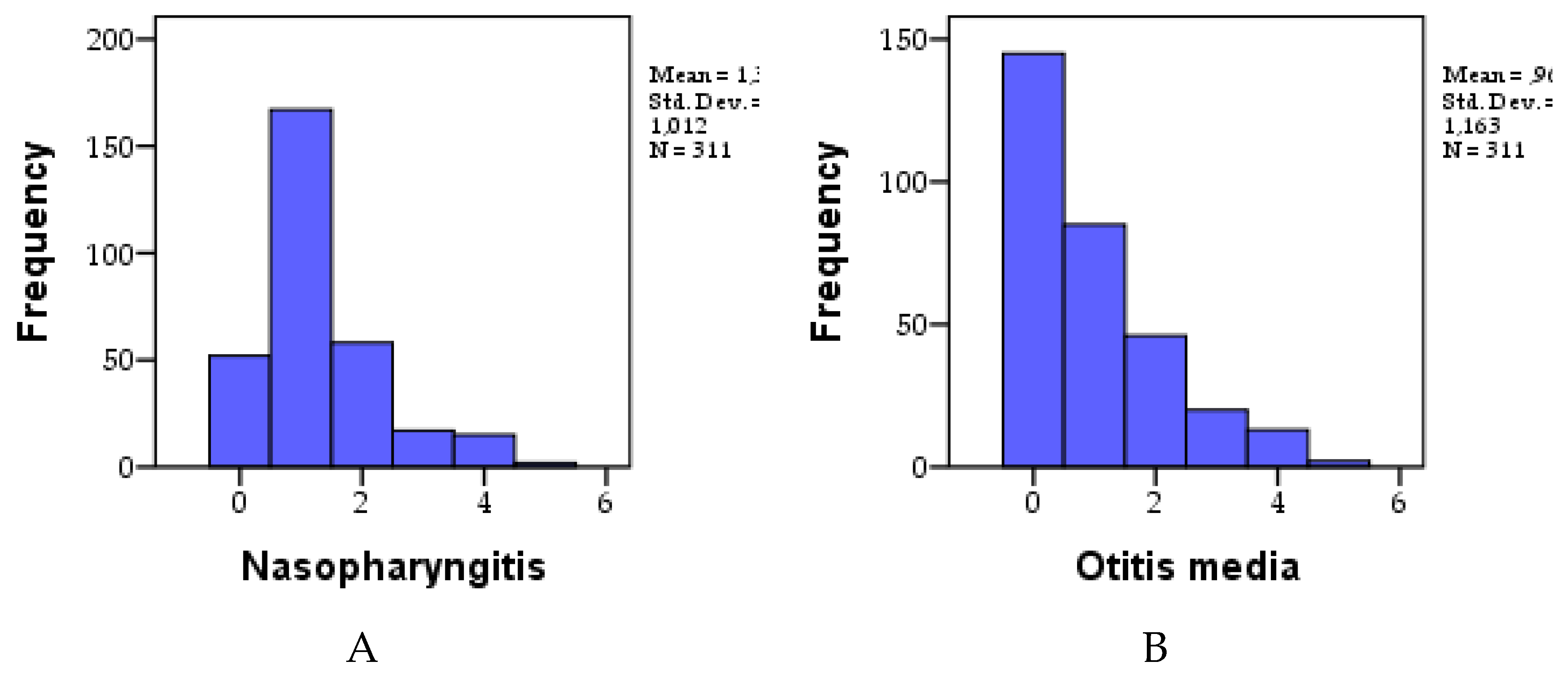
The study analyzed the presence and absence of behavioral disorders according to age groups, the number of cumulative acute illnesses, and vitamin D levels.
Regarding the age categories, for the 0-18 years group, 28.0% of the participants did not have behavioral disorders, while 37.9% had such disorders. In the 19-45 age group, 8.4% had no disorders, and 21.5% had disorders. For those over 45 years of age, 1.0% had no behavioral disorders, and 3.2% had a disorder.
Based on the number of cumulative illnesses, 5.8% of participants who did not have any illness had no behavioral disorder, while 4.5% had a disorder. In the single-disease group, 17.4% had no behavioral disorder, while 18.3% had a disorder. Among those with two diseases, 10.9% had no disorders, and 29.3% had behavioral disorders. Among those with three diseases, 3.2% had no disorders, and 10.6% had disorders.
Regarding vitamin D levels, 3.5% of participants with a deficiency (0-20 ng/mL) had no behavioral disturbances, while 14.5% had disturbances. In the insufficient group (20-29 ng/mL), 10.9% had no impairments, and 23.8% had impairments. For the optimal level (30-55.5 ng/mL), 20.3% had no behavioral disturbances, and 22.2% had disturbances. In the high-level category (55.5-150 ng/mL), 2.6% had no disorders, and 2.3% had behavioral disorders.
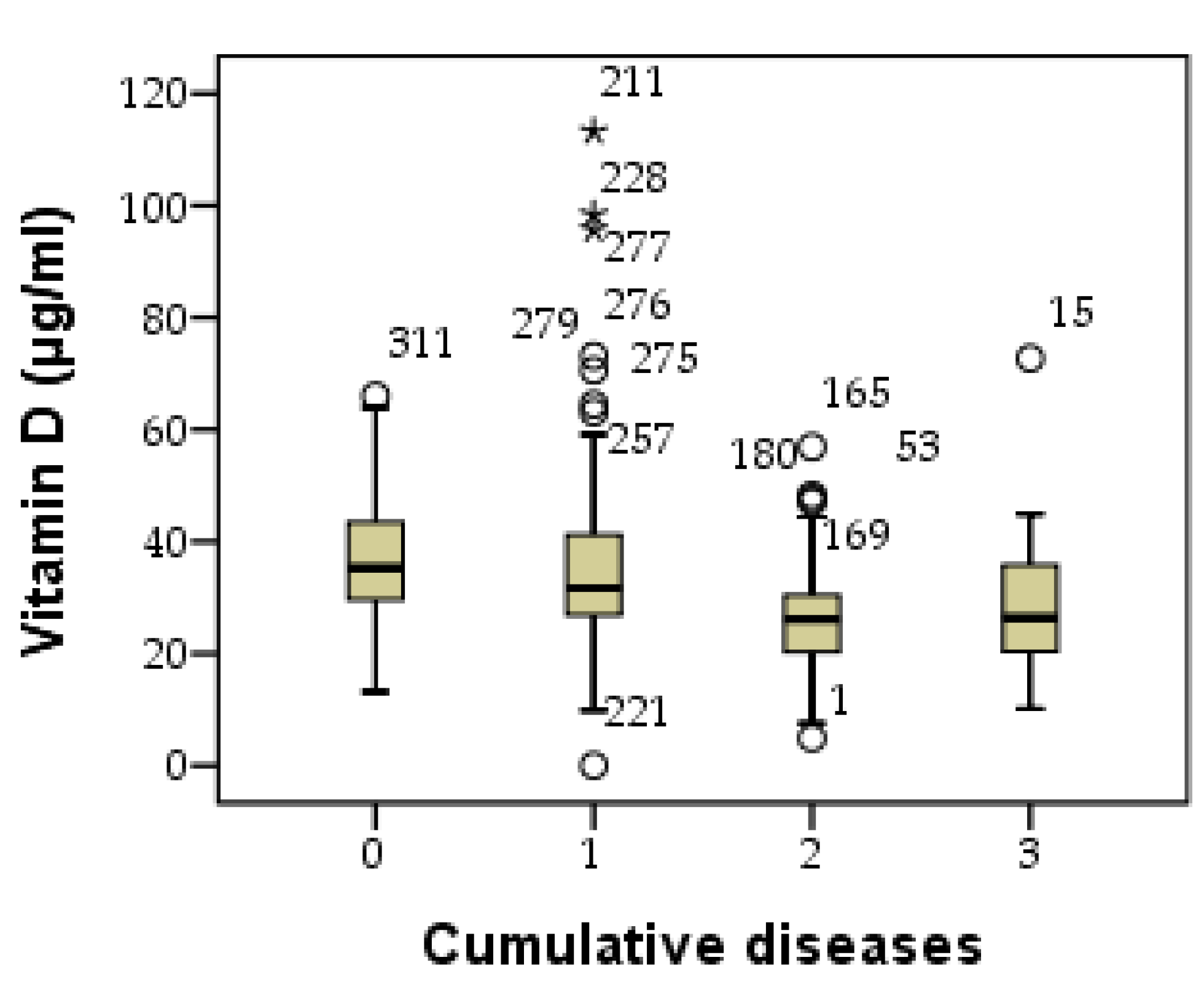
3.8. Correlations
The Pearson correlation analysis revealed a statistically significant and inversely proportional relationship between serum vitamin D levels and nasopharyngitis, indicated by a negative Pearson coefficient (r=-0.263, p=0.001). As serum vitamin D levels decrease, the recurrence frequency of nasopharyngitis significantly increases. A similar pattern was observed for the correlation between serum vitamin D levels and otitis media, with statistical significance and an inverse relationship, as indicated by the negative Pearson coefficient (r=-0.316, p=0.001). In the case of rhinosinusitis, an inversely proportional relationship was recorded, although statistically insignificant (r=-0.109, p=0.055).
Regarding the correlation between cumulative diseases and serum vitamin D levels, a significant negative relationship was identified, suggesting that a decrease in vitamin D levels leads to the accumulation of diseases (r=-0.274, p=0.001). These correlations are visually represented using the dot cloud technique in
Figure 6.
Figure 6.
Relationship between behavior disorders and age categories (A), as well as the association with the number of cumulative conditions (B) and vitamin D.
Figure 6.
Relationship between behavior disorders and age categories (A), as well as the association with the number of cumulative conditions (B) and vitamin D.
Figure 7.
Visual Representation of Correlations Regarding Vitamin D and Rhinopharyngitis (A), Otitis Media (B), and Rhinosinusitis (C).
Figure 7.
Visual Representation of Correlations Regarding Vitamin D and Rhinopharyngitis (A), Otitis Media (B), and Rhinosinusitis (C).
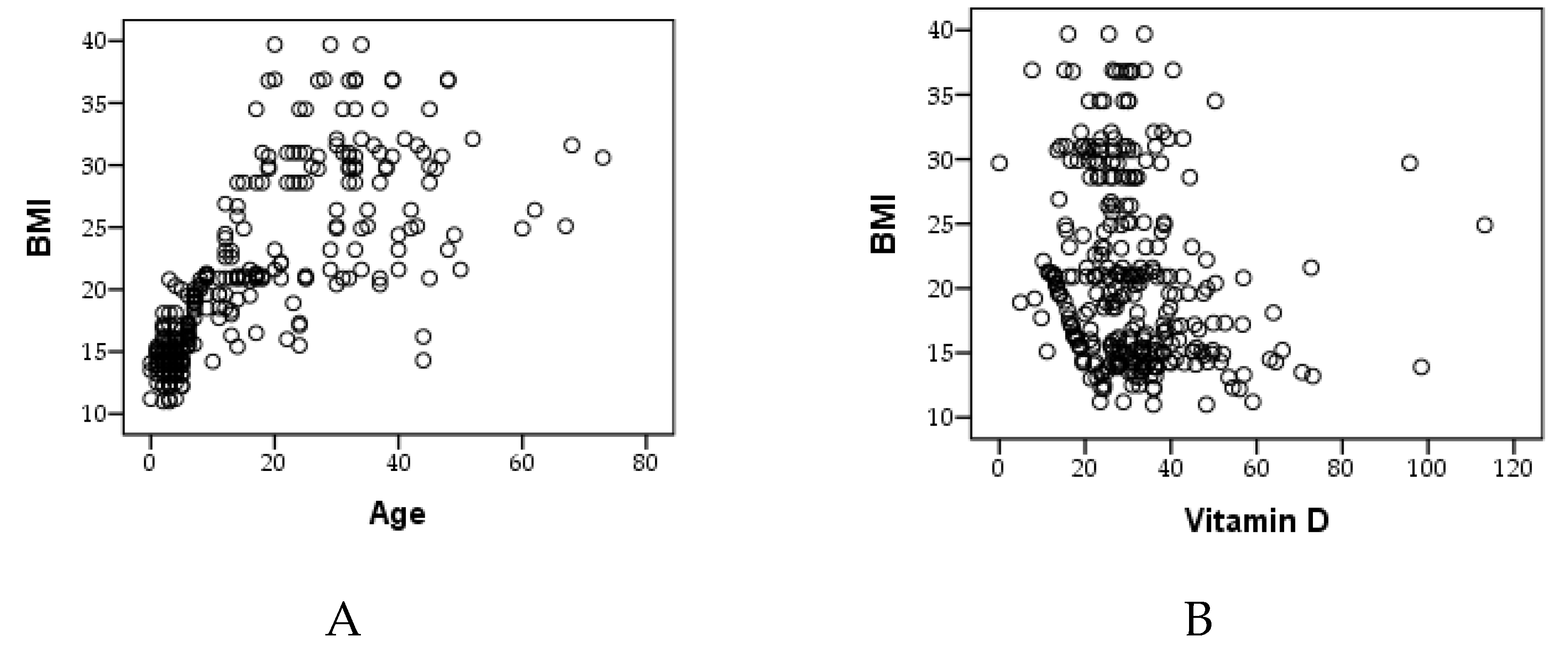
Analysis using Pearson's correlation revealed significant findings concerning the association between BMI and age. Specifically, a noteworthy and directly proportional relationship emerged (r=0.738, p=0.001). This suggests that as age increases, the incidence of obesity also increases. Thus, more cases of overweight and obesity were documented in older individuals (
Figure 8A).
Regarding BMI and vitamin D, an inverse relationship was observed with statistical significance (r=-0.205, p=0.001). This indicates a higher incidence of vitamin D deficiency in individuals with higher BMI. Consequently, it can be concluded that obesity has an impact on the serum level of vitamin D (
Figure 8B).
In
Figure 8 these correlations are visually depicted using the dot cloud technique, providing a clear representation of the observed relationships.
The study analyzed Pearson correlations between several factors and behavioral disorders (
Table 3). The results are as follows: Vitamin D has a negative and significant correlation with behavioral disorders, with a correlation coefficient of -0.222 and a level of statistical significance (p) of 0.000. Age shows a positive and significant correlation with behavioral disorders, with a correlation coefficient of 0.152 and a p-value of 0.007. Body mass index (BMI) has a positive and significant correlation with behavioral disorders, with a coefficient of 0.174 and a p-value of 0.002. Nasopharyngitis did not show a significant correlation with behavioral disorders, with a coefficient of 0.110 and a p-value of 0.053. Otitis media has a positive and significant correlation with behavioral disorders, with a coefficient of 0.238 and a p-value of 0.000. Rhinosinusitis did not show a significant correlation, with a coefficient of 0.102 and a p-value of 0.072. Cumulative factors show a positive and significant correlation with behavioral disorders, with a coefficient of 0.240 and a p-value of 0.000.
4. Discussion
Natural sources of vitamin D play a crucial role in childhood for the prevention of infections. Exposure to sunlight, consumption of vitamin D-rich foods like fatty fish, eggs, and fortified milk, and maintaining outdoor activities are key for sufficient vitamin D levels. Recent studies highlight the immunomodulatory effects of vitamin D, showing a significant reduction in the incidence of respiratory infections and other common childhood illnesses [
27]. A 2023 study published in the Journal of Pediatric Health demonstrated that children with adequate vitamin D levels had a 30% lower risk of respiratory infections compared to those with deficiencies [
28]. Another study from the American Journal of Clinical Nutrition in 2022 emphasized the importance of natural sunlight exposure, noting that young patients who spent more time outdoors had better overall immune function and fewer sick days [
29]. Ensuring patients receive adequate natural vitamin D can significantly enhance their immune response and reduce infection rates, promoting better long-term health outcomes.
The study revealed a high prevalence of nasopharyngitis, affecting approximately 83.27% of individuals, with an average recurrence of 1.30±1.01. This finding is consistent with previous research on nasopharyngeal carriage of Streptococcus pneumoniae, which indicated a high prevalence of nasopharyngeal colonization [
30,
31,
32,
33]. Additionally, the prevalence of nasopharyngeal carriage of respiratory pathogens was reported to be around 29% in another study, further supporting the high prevalence of nasopharyngitis.
In contrast, otitis media was found to have a lower incidence, affecting approximately 53.37% of individuals, with a mean recurrence of 0.96±1.16. This lower incidence aligns with the lower prevalence of nasopharyngeal colonization by pneumococci in patients, which was reported to be 17% in a control group [
34].
Rhinosinusitis was recorded at a lower percentage, diagnosed in 20.90% of the people studied, with an average recurrence of 0.25±0.53. This finding is consistent with the meta-analysis of data from young children in China, which showed a high prevalence of nasopharyngeal carriage of Streptococcus pneumoniae, indicating a lower prevalence of rhinosinusitis compared to nasopharyngitis [
33,
35].
The study also indicated a trend towards a higher frequency of conditions in girls, with the exception of otitis, which was more common in boys. This observation aligns with the prevalence of nasopharyngeal carriage of S. pneumoniae by sex, which showed a slightly higher prevalence in males [
33].
Rapid tests for vitamin D measurement, such as immunoassays and point-of-care devices, offer quick results but may lack the precision and specificity of standard methods like high-performance liquid chromatography (HPLC) or liquid chromatography-tandem mass spectrometry (LC-MS/MS). Standard methods are considered more accurate as they precisely detect various vitamin D metabolites, including the biologically active form 1,25-dihydroxyvitamin D (1,25(OH)2D).
The accuracy of rapid tests can be influenced by factors such as cross-reactivity and test calibration. This is particularly significant when measuring vitamin D3, as 1,25(OH)2D plays a crucial role in immune system modulation, influencing T cell activity and antimicrobial peptide production. Moreover, accurate assessment of vitamin D levels is vital due to emerging correlations between vitamin D deficiency and behavioral disorders. Studies suggest that low vitamin D levels may be associated with an increased risk of conditions such as depression, anxiety, and even cognitive impairments. Thus, precise measurement of vitamin D3 is essential for understanding its broader impacts on both physical and mental health.
Furthermore, the analysis of vitamin D levels suggested a significant correlation between vitamin D deficiency and the recurrence of nasopharyngitis and otitis media. This finding is consistent with previous literature reporting a higher prevalence of vitamin D deficiency among individuals with certain diseases, such as Graves' disease and wheezing [
36,
37,
38,
39,
40].
The observed direct correlation between BMI and age aligns with several studies in the specialized literature that have reported an increased prevalence of obesity among older individuals [
41]. This finding supports the notion that age is a significant factor contributing to the incidence of obesity [
42]. Additionally, our identification of an inverse relationship between BMI and vitamin D levels corroborates existing research highlighting the association between higher BMI and increased risk of vitamin D deficiency [
43,
44,
45,
46]. These consistent patterns underscore the relevance of considering age and BMI when assessing obesity trends and their potential impact on vitamin D status, providing valuable insights for public health interventions and personalized healthcare strategies.
In conclusion, the study's findings on the prevalence of nasopharyngitis, otitis media, and rhinosinusitis, as well as the association between vitamin D levels and disease recurrence, are supported by existing research on nasopharyngeal carriage of pathogens and vitamin D deficiency.
Limitations of this study include its narrow focus on three acute diseases. Additionally, the absence of consideration for potential risk factors that may influence serum vitamin D levels represents another limitation. The study's short duration can be regarded as a further constraint. An extended study, incorporating a group receiving vitamin D supplementation, would provide better control over the outcomes.
A notable strength of this study lies in emphasizing the significance of maintaining an optimal level of vitamin D in the context of acute diseases. This is underscored by the study's findings, which suggest a potential role in reducing the frequency, recurrence, and cumulative burden of acute diseases.
Lack of concentration, anxiety, exhaustion, aggressiveness, and hyperactivity are considered behavioral disorders [
47,
48]. In the ENT specialty medical office, the availability of a rapid vitamin D test is very helpful. Although the accuracy is lower than that of laboratory biochemical analyses, this rapid test can be used to check for vitamin D deficiency using only capillary sampling. While the serum level of vitamin D is not typically monitored directly in ENT specialist offices, as are behavior disorders, it appears to be a useful tool for establishing correlations. These correlations can serve as guidelines for establishing procedures in the management of acute oropharyngeal infections.
This pioneering research delves into the vitamin D status among people with non-critical illnesses, offering a comprehensive insight into potential advancements in pediatric healthcare. The objective is to develop universally applicable approaches for other healthcare systems. The review exposes current challenges in recognizing the interdependence and function of these systems in children's and adult's health, emphasizing the necessity for enhanced strategies. Further analysis may uncover additional themes, and thorough data collection would significantly contribute to a better understanding and improvement of children's and adult's healthcare.
5. Conclusions
The study shows a high prevalence of nasopharyngitis (83.27%) and otitis media (53.37%), with significant gender differences in recurrence rates, particularly higher in girls, except for otitis, which is more common in boys.
Vitamin D deficiency correlates significantly with recurrent nasopharyngitis and otitis media, and lower levels are found in older individuals, particularly in rural areas. Behavioral disorders are more common in younger individuals, those with more cumulative illnesses, and those with lower vitamin D levels.
The study also highlights that increasing age correlates with increased obesity, which is associated with lower vitamin D levels.
Natural sources of vitamin D can help maintain optimal levels and reduce oropharyngeal infections.
Author Contributions
Conceptualization, F.M., T.C.G. and A.M.; methodology, F.M.; software, A.M.; validation, F.M.; formal analysis, F.M.; investigation, F.M..; resources, F.M.; data curation, F.M.; writing—original draft preparation, F.M.; writing—review and editing, F.M. and D.F.T.; visualization, F.M.; supervision, F.M.; project administration, F.M.; funding acquisition, F.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the University of Oradea (protocol code CEFMF/1 from 31 January 2023 and date of approval).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed con-sent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
All the data processed in this article are part of the research for a doctoral thesis, being archived in the aesthetic medical office, where the interventions were performed.
Acknowledgments
No acknowledgments.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Behl, T.; Kumar, S.; Sehgal, A.; Singh, S.; Sharma, N.; Chirgurupati, S.; Aldubayan, M.; Alhowail, A.; Bhatia, S.; Bungau, S. Linking COVID-19 and Parkinson's disease: Targeting the role of Vitamin-D. Biochemical and Biophysical Research Communications 2021, 583, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Charoenngam, N.; Holick, M.F. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Trifan, D.F.; Tirla, A.G.; Mos, C.; Danciu, A.; Bodog, F.; Manole, F.; Ghitea, T.C. Involvement of Vitamin D3 in the Aging Process According to Sex. Cosmetics 2023, 10, 114. [Google Scholar] [CrossRef]
- Abudawood, M.; Tabassum, H.; Ansar, S.; Almosa, K.; Sobki, S.; Ali, M.N.; Aljohi, A. Assessment of gender-related differences in vitamin D levels and cardiovascular risk factors in Saudi patients with type 2 diabetes mellitus. Saudi Journal of Biological Sciences 2018, 25, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Ferrante, G.; Fasola, S.; Piazza, M.; Tenero, L.; Zaffanello, M.; La Grutta, S.; Piacentini, G. Vitamin D and Healthcare Service Utilization in Children: Insights from a Machine Learning Approach. Journal of Clinical Medicine 2022, 11, 7157. [Google Scholar] [CrossRef] [PubMed]
- Chanchlani, R.; Nemer, P.; Sinha, R.; Nemer, L.; Krishnappa, V.; Sochett, E.; Safadi, F.; Raina, R. An Overview of Rickets in Children. Kidney Int Rep 2020, 5, 980–990. [Google Scholar] [CrossRef]
- Creo, A.L.; Thacher, T.D.; Pettifor, J.M.; Strand, M.A.; Fischer, P.R. Nutritional rickets around the world: an update. Paediatrics and International Child Health 2017, 37, 84–98. [Google Scholar] [CrossRef]
- Stevens, G.A.; Beal, T.; Mbuya, M.N.; Luo, H.; Neufeld, L.M.; Addo, O.Y.; Adu-Afarwuah, S.; Alayón, S.; Bhutta, Z.; Brown, K.H. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: a pooled analysis of individual-level data from population-representative surveys. The Lancet Global Health 2022, 10, e1590–e1599. [Google Scholar] [CrossRef]
- Sabir, G.; Bernet, T.; Espinoza, A.; Zilly, B. Nutrition-sensitive agriculture and improved nutrition in mountain areas: Rural service providers as catalysts. Rural 21 2021, 3, 27–29. [Google Scholar]
- Kabir, M.T.; Uddin, M.S.; Hossain, M.F.; Abdulhakim, J.A.; Alam, M.A.; Ashraf, G.M.; Bungau, S.G.; Bin-Jumah, M.N.; Abdel-Daim, M.M.; Aleya, L. nCOVID-19 pandemic: from molecular pathogenesis to potential investigational therapeutics. Frontiers in cell and developmental biology 2020, 8. [Google Scholar] [CrossRef]
- Tagde, P.; Tagde, S.; Tagde, P.; Bhattacharya, T.; Monzur, S.M.; Rahman, M.H.; Otrisal, P.; Behl, T.; ul Hassan, S.S.; Abdel-Daim, M.M.; et al. Nutraceuticals and Herbs in Reducing the Risk and Improving the Treatment of COVID-19 by Targeting SARS-CoV-2. Biomedicines 2021, 9, 1266. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, A.F.; Moga, I.; Moga, T.; Ghitea, E.C.; Babes, K.; Ghitea, T.C. Assessing the Risk of Stroke in the Elderly in the Context of Long-COVID, Followed Through the Lens of Family Medicine. in vivo 2023, 37, 2284–2295. [Google Scholar] [CrossRef] [PubMed]
- Uday, S.; Högler, W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res 2020, 152, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Garfinkel, R.J.; Dilisio, M.F.; Agrawal, D.K. Vitamin D and its effects on articular cartilage and osteoarthritis. Orthopaedic journal of sports medicine 2017, 5, 2325967117711376. [Google Scholar] [CrossRef] [PubMed]
- Mannion, C.A.; Gray-Donald, K.; Koski, K.G. Association of low intake of milk and vitamin D during pregnancy with decreased birth weight. Cmaj 2006, 174, 1273–1277. [Google Scholar] [CrossRef]
- Kuang, L.; Liang, Z.; Wang, C.; Lin, T.; Zhang, Y.; Zhu, B. Serum 25-Hydroxy Vitamin D Levels in Children with Acute Respiratory Infections Caused by Respiratory Virus or Atypical Pathogen Infection. Nutrients 2023, 15, 1486. [Google Scholar] [CrossRef]
- Smotkin-Tangorra, M.; Purushothaman, R.; Gupta, A.; Nejati, G.; Anhalt, H.; Ten, S. Prevalence of vitamin D insufficiency in obese children and adolescents. Journal of Pediatric Endocrinology and Metabolism 2007, 20, 817–824. [Google Scholar] [CrossRef]
- Akter, R.; Afrose, A.; Sharmin, S.; Rezwan, R.; Rahman, M.R.; Neelotpol, S. A comprehensive look into the association of vitamin D levels and vitamin D receptor gene polymorphism with obesity in children. Biomedicine & Pharmacotherapy 2022, 153, 113285. [Google Scholar]
- Vimaleswaran, K.S.; Berry, D.J.; Lu, C.; Tikkanen, E.; Pilz, S.; Hiraki, L.T.; Cooper, J.D.; Dastani, Z.; Li, R.; Houston, D.K. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS medicine 2013, 10, e1001383. [Google Scholar] [CrossRef]
- Vitamin D Supplementation for Infants, World Health Organization. Available online: https://www.who.int/tools/elena/bbc/vitamind-infants (accessed on 3 August 2024).
- Drincic, A.T.; Armas, L.A.; Van Diest, E.E.; Heaney, R.P. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity 2012, 20, 1444–1448. [Google Scholar] [CrossRef]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C. Vitamin D deficiency in Europe: pandemic? The American journal of clinical nutrition 2016, 103, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, W.Z.; Hegazy, R.A. Vitamin D and the skin: Focus on a complex relationship: A review. J Adv Res 2015, 6, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Meeker, S.; Seamons, A.; Maggio-Price, L.; Paik, J. Protective links between vitamin D, inflammatory bowel disease and colon cancer. World J Gastroenterol 2016, 22, 933–948. [Google Scholar] [CrossRef] [PubMed]
- Trifan, D.F.; Tirla, A.G.; Moldovan, A.F.; Moș, C.; Bodog, F.; Maghiar, T.T.; Manole, F.; Ghitea, T.C. Can Vitamin D Levels Alter the Effectiveness of Short-Term Facelift Interventions? Healthcare 2023, 11, 1490. [Google Scholar] [CrossRef] [PubMed]
- Jabłonowska-Lietz, B.; Wrzosek, M.; Włodarczyk, M.; Nowicka, G. New indexes of body fat distribution, visceral adiposity index, body adiposity index, waist-to-height ratio, and metabolic disturbances in the obese. Kardiol Pol 2017, 75, 1185–1191. [Google Scholar] [CrossRef]
- Bleakley, A.S.; Licciardi, P.V.; Binks, M.J. Vitamin D modulation of the innate immune response to paediatric respiratory pathogens associated with acute lower respiratory infections. Nutrients 2021, 13, 276. [Google Scholar] [CrossRef]
- Marusca, L.M.; Reddy, G.; Blaj, M.; Prathipati, R.; Rosca, O.; Bratosin, F.; Bogdan, I.; Horhat, R.M.; Tapos, G.-F.; Marti, D.-T. The effects of vitamin D supplementation on respiratory infections in children under 6 years old: a systematic review. Diseases 2023, 11, 104. [Google Scholar] [CrossRef]
- Alexander, L.; Christensen, S.M.; Richardson, L.; Ingersoll, A.B.; Burridge, K.; Golden, A.; Karjoo, S.; Cortez, D.; Shelver, M.; Bays, H.E. Nutrition and physical activity: an obesity medicine association (OMA) clinical practice statement 2022. Obesity Pillars 2022, 1, 100005. [Google Scholar] [CrossRef]
- Husseini, Y.; Sahraei, H.; Meftahi, G.H.; Dargahian, M.; Mohammadi, A.; Hatef, B.; Zardooz, H.; Ranjbaran, M.; Hosseini, S.B.; Alibeig, H.; et al. Analgesic and anti-inflammatory activities of hydro-alcoholic extract of Lavandula officinalis in mice: possible involvement of the cyclooxygenase type 1 and 2 enzymes. Revista Brasileira de Farmacognosia 2016, 26, 102–108. [Google Scholar] [CrossRef]
- Bakhshaee, M.; Rajati Haghi, M.; Naderi, H.R.; Khomarian, M.; Ghazvini, K. Breastfeeding and Nasopharyngeal Colonization With Common Respiratory Pathogens Among Children. Shiraz E-Med J 2015, 16, e20295. [Google Scholar] [CrossRef]
- Friborg, J.; Jarrett, R.F.; Liu, M.Y.; Falk, K.I.; Koch, A.; Olsen, O.R.; Duncan, P.; Wohlfarht, J.; Chen, J.Y.; Melbye, M. Epstein-Barr virus immune response in high-risk nasopharyngeal carcinoma families in Greenland. Journal of medical virology 2007, 79, 1877–1881. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Fu, J.; Liang, Z.; Chen, J. Prevalence and serotype distribution of nasopharyngeal carriage of Streptococcus pneumoniae in China: a meta-analysis. BMC infectious diseases 2017, 17, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, P.B.B.; Farhat, C.K.; Succi, R.C.l.d.M.; Machado, A.n.M.d.O.; Braga, J.A.P. Penicillin Resistance in Nasopharyngeal <i>Streptococcus pneumoniae</i> among Children with Sickle Cell Disease Immunized with 7-Valent Pneumococcal Conjugate Vaccine. World Journal of Vaccines 2013, Vol.03No.02, 7. [Google Scholar] [CrossRef]
- Mwangi, C.N.; Revathi, G.; Muigai, A.W.; Kariuki, S. Serotypes and Antimicrobial Susceptibility Patterns of Nasopharyngeal Pneumococci Isolated from HIV-Infected Children in Selected Pediatric Clinics in Nairobi, Kenya. Open Journal of Medical Microbiology 2016, 6, 42–52. [Google Scholar] [CrossRef]
- Cho, Y.Y.; Chung, Y.J. Vitamin D supplementation does not prevent the recurrence of Graves’ disease. Scientific Reports 2020, 10, 16. [Google Scholar] [CrossRef]
- Hussain, M.; Malik, Q.; Bashir, J.; Abbas, M.; Ijaz, M. The Association between Vitamin D and Wheezing. Pakistan Armed Forces Medical Journal 2022, 72, 1593–1596. [Google Scholar] [CrossRef]
- Irungu, C.W.; Oburra, H.O.; Ochola, B. Prevalence and predictors of malnutrition in nasopharyngeal carcinoma. Clinical Medicine Insights: Ear, Nose and Throat 2015, 8, CMENT–S12119. [Google Scholar] [CrossRef]
- Chen, Z.; Lv, X.; Hu, W.; Qian, X.; Wu, T.; Zhu, Y. Vitamin D status and its influence on the health of preschool children in Hangzhou. Frontiers in Public Health 2021, 9, 675403. [Google Scholar] [CrossRef]
- Jung, S.S.; Kim, M.S.; Lee, D.Y. Serum vitamin D status in children and adolescence with diabetes according to season and age. Annals of pediatric endocrinology & metabolism 2014, 19, 13. [Google Scholar]
- Rai, M.F.; Sandell, L.J.; Cheverud, J.M.; Brophy, R.H. Relationship of age and body mass index to the expression of obesity and osteoarthritis-related genes in human meniscus. International Journal of Obesity 2013, 37, 1238–1246. [Google Scholar] [CrossRef]
- Tam, B.; Morais, J.; Santosa, S. Obesity and ageing: Two sides of the same coin. Obesity Reviews 2020, 21. [Google Scholar] [CrossRef]
- Tobias, D.K.; Luttmann-Gibson, H.; Mora, S.; Danik, J.; Bubes, V.; Copeland, T.; LeBoff, M.S.; Cook, N.R.; Lee, I.-M.; Buring, J.E. Association of body weight with response to vitamin d supplementation and metabolism. JAMA Network Open 2023, 6, e2250681–e2250681. [Google Scholar] [CrossRef]
- Güngör, N.D.; Güngör, K.; Celik, N.; Önal, M.; Madenli, A. Impact of body mass index and vitamin D on serum AMH levels and antral follicle count in PCOS. Eur Rev Med Pharmacol Sci 2023, 27, 179–187. [Google Scholar]
- Wu, Y.; Zeng, Y.; Zhang, Q.; Xiao, X. The Role of Maternal Vitamin D Deficiency in Offspring Obesity: A Narrative Review. Nutrients 2023, 15, 533. [Google Scholar] [CrossRef]
- Matiș, L.; Daina, L.G.; Maris, L.; Ghitea, T.C.; Trifan, D.F.; Moga, I.; Fodor, R. Variety of Serotonin Levels in Pediatric Gastrointestinal Disorders. Diagnostics 2023, 13, 3675. [Google Scholar] [CrossRef]
- Ogundele, M.O. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World J Clin Pediatr 2018, 7, 9–26. [Google Scholar] [CrossRef]
- Matiș, L.; Alexandru, B.A.; Ghitea, T.C. Catecholamine Variations in Pediatric Gastrointestinal Disorders and Their Neuropsychiatric Expression. Biomedicines 2023, 11, 2600. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).