1. Introduction
Severe obesity (OB) in adults is defined by a body mass index (BMI) value ≥40 kg/m
2. It has been associated with a high risk of developing type 2 diabetes, hypertension, congestive heart failure, and poor therapeutic success. In such cases, bariatric surgery currently represents the main therapeutic option able to induce significant weight loss and mitigation of cardiometabolic comorbidities including type 2 diabetes [
1].
The definition of severe OB in children and adolescents is still a matter of debate and depends on the BMI reference values used. In Canada and several European countries, including Italy, the World Health Organization (WHO) cut-offs [
2] are used. According to this system, the definition is based either on BMI Z-score >3 standard deviations (which corresponds to 99.9th percentile) [
3] or BMI ≥99th percentile (as a rounded percentile of the 99.9th) [
3,
4]. On the contrary, the recent guideline for the treatment of obesity released by the American Academy of Pediatrics recommends using percentages of the 95th percentile of BMI-for-age and sex (BMI
95) to indicate different levels of severe OB [
5]. In fact, the extreme values of BMI Z-score released by the Centers for Disease Control (CDC) are considered less reliable due to sparse reference data and compression >97th percentile. Namely, the limit of BMI
95 ≥120% of CDC has been proposed to classify children and adolescents with severe OB [
6,
7].
The discrepancy in the categorization of severe OB may have consequences either in public health or in clinical practice. For instance, by using different definitions the classification of severe OB in children is heterogeneous, as shown by a recent systematic review with meta-analysis [
8]. Therefore, a unified cut-off would provide a better comparison at international level and understanding of the clinical implications. Of note, the indication of bariatric surgery in adolescents is based on percentages of BMI
95 (namely BMI
95 ≥140%, or BMI
95 ≥120% with a comorbidity), or on absolute values of 40 and 35 kg/m
2 (5), which does not have the equivalent in those countries using BMI Z-scores.
It is well known that cardiometabolic risk factors worsen with increasing severity of OB [
9]. As far as we know, the empirical evidence for comparing the cardiometabolic risk across different BMI derived metrics of the WHO tables, namely extended values of BMI over the 97th percentile (BMI
97) and BMI Z-scores is lacking. Therefore, we compared individual and clustered cardiometabolic risk factors among different metrics of OB and severe OB, namely 97th percentile, 99th percentile, BMI
97 ≥120% of the WHO tables in children and adolescents with OB. Furthermore, a comparison of the cardiometabolic variables between youths with BMI Z-score >3 and BMI
97 ≥120% was evaluated.
2. Materials and Methods
Study Design and Participants
We retrospectively analysed the data of children and adolescents (age range 6-17 years) retrieved from the database of the CARITALY (CARdiometabolic risk factors in overweight and obese children in ITALY) study, a multicentre cross-sectional study on the behalf of the Obesity study group of the Italian Society for Pediatric Endocrinology and Diabetology [
10]. Participants were observed between 2003-2020 in ten Italian centers for the management of paediatric obesity distributed across different regions. We selected youths with OB as defined by the 97th percentile of BMI from the WHO tables, in whom anthropometric, clinical, and biochemical variables were available. Youths with type 1 or type 2 diabetes, LDL-C ≥190 mg/dL, TG ≥400 mg/dL, secondary obesity or under pharmacological treatment were excluded.
Anthropometric Assessement
In each centre, physical examinations were performed by trained pediatricians and puberal maturation was evaluated according to Tanner staging. Anthropometric parameters were measured following standard procedures [
10]. BMI was calculated as weight (Kg)/height (m)
2, BMI Z-scores were calculated using the WHO AnthroPlus software (
https://www.who.int/tools/growth-reference-data-for-5to19-years/application-tools). Waist circumference was measured at the midpoint between the last rib and the iliac crest at minimal respiration when the participant was in a standing position. The waist to height ratio (WHtR) was calculated by dividing waist circumference (cm) by height (cm).
Clinical and Laboratory Evaluations
Blood pressure (BP) was measured three times within two minutes in the sitting position after 5-minute rest through an aneroid sphygmomanometer with an appropriately sized cuff as elsewhere described [
10].
Blood samples for glucose, insulin, triglycerides (TG), cholesterol, and high-density lipoprotein-cholesterol (HDL-C) were drawn after an overnight fast. These biochemical parameters were analysed in the centralized laboratory of each center, as elsewhere described [
10].
All laboratories belonged to the Italian National Health System and are certified according to International Standards ISO 9000 (
www.iso9000.it/) with semi-annual quality controls and inter-lab comparisons.
Definition of Severe Obesity
Obesity was defined as BMI >97th percentile (BMI97). Severe OB was defined according to the following thresholds: BMI >99th percentile (BMI99), BMI97 ≥120% or BMI Z-score > 3 of the WHO tables.
Statistical Analyses
The normal distribution of the variables was assessed by using the Kolmogorov-Smirnov test. Continuous variables with normal distribution were expressed as mean±standard deviation. Variables with skewed distribution were log transformed using natural log (Ln) for statistical analyses, but they were presented as median and interquartile range for a better understanding. The sample was stratified into three mutually exclusive groups according to the following BMI cut-offs: BMI97, BMI99 and BMI97 ≥120%. Between group comparison for continuous variables was assessed by t-test or ANOVA. Qualitative variables were presented as number and percentage (%) and compared using χ2 test.
The diagnostic accuracy of either BMI Z-score >3 or BMI97 ≥120% to discriminate the presence of clustered cardiometabolic risk factors was assessed. Receiver operating characteristic (ROC) curve analysis was used to evaluate accuracy (area under the curve), specificity, sensitivity, positive predictive value (PPV) and negative predictive value (NPV), using 2x2 tables.
A p value <0.05 was considered for statistical significance Statistical analyses were conducted using IBM SPSS Statistics software, Version 20.0 (IBM, Armonk, NY).
3. Results
The sample was represented by 3727 youths (1937 boys and 1790 girls), divided into 2225 children (age <12 years) and 1502 adolescents (age ≥12 years). Mean age was 11.2±2.4 years (range 6-17 years).
The characteristics of the three mutually exclusive categories based on different BMI derived metrics are described in
Table 1. Anthropometric, clinical, and biochemical variables progressively increased from the lowest to the highest BMI category, while HDL-C levels decreased (
p <0.0001 for all). No difference among groups was observed only for fasting glucose and total cholesterol.
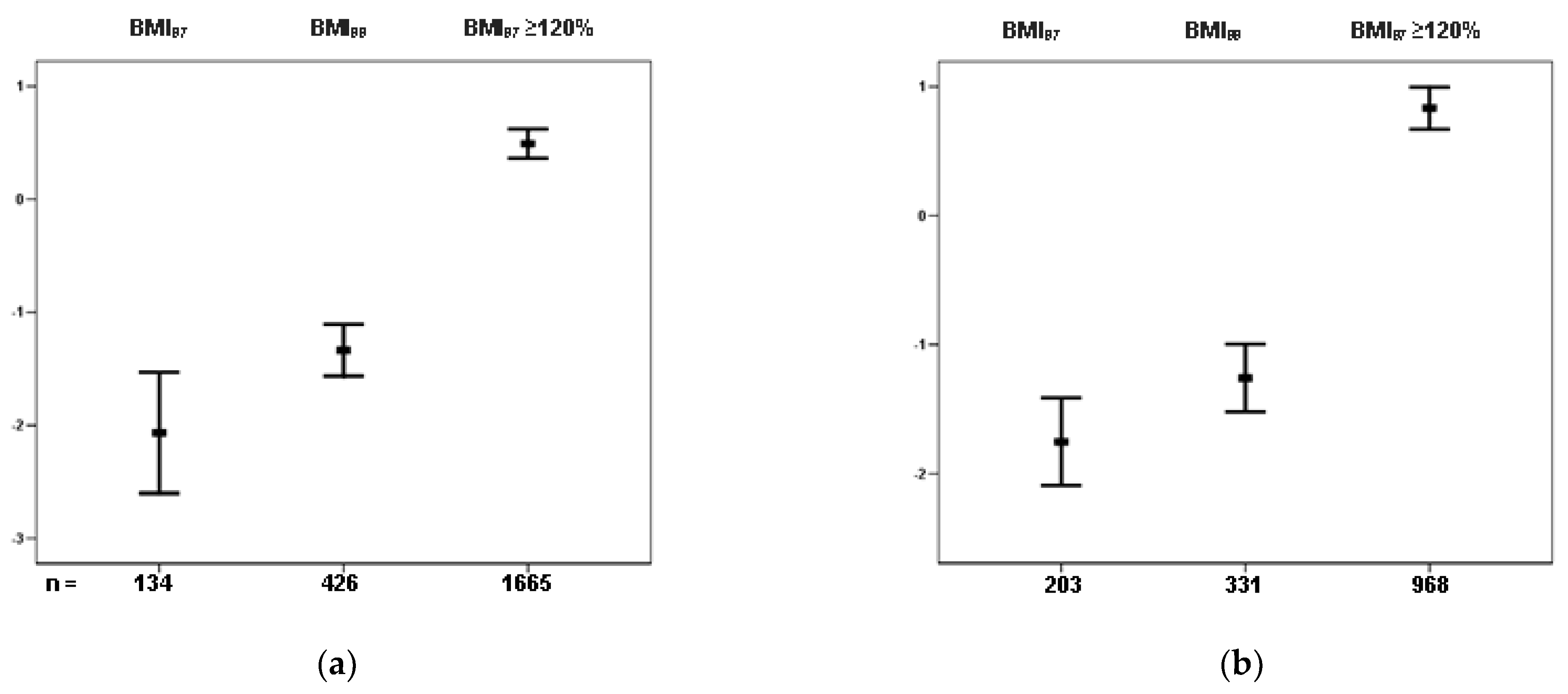
Mean values of cCMR Z-score stratified in the three BMI categories are shown in
Figure 1 separately by age group (children, panel a; adolescents, panel b). Differences between categories were significant for all groups (
p <0.0001), either in children or adolescents.
Comparisons between groups with severe OB classified by BMI Z-score >3 or BMI
97 ≥120% are shown separately by age group in
Table 2. The prevalence of severe OB as defined by the cut-off of BMI
97 ≥120%, was significantly higher than that observed by using BMI Z-score >3, both in children (74.8% vs 60.5%) and adolescents (64.4% vs 37.7%),
p <0.0001.
Children with severe OB defined by BMI Z-score >3 showed higher values of BMI, BMI Z-score, and WHtR than those defined by BMI
97 ≥120%, while they showed no difference with respect to individual cardiometabolic risk factors, except for a borderline difference for cCMRF (
p =0.08). Similar findings were found in adolescents, except for significantly higher levels of insulin and cCMR Z-score (
Table 2).
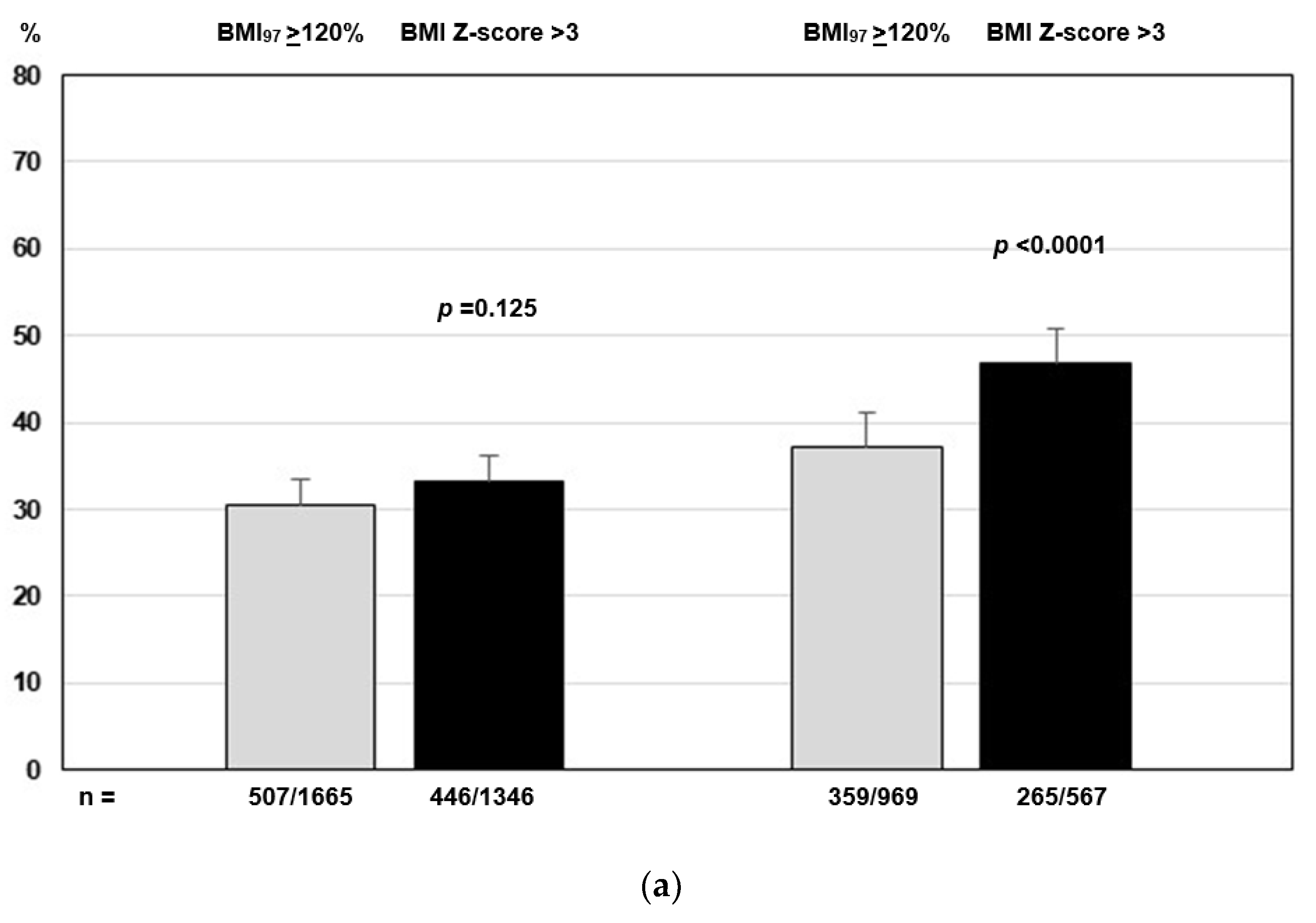
Similarly, the prevalence of clustered cardiometabolic risk factors was higher in adolescents with severe Ob classified by BMI Z-score >3 (
p <0.001), while no substantial difference was found between the two classification methods in children (
Figure 2).
AUC, sensitivity, specificity, PPV, NPV of BMI Z-score >3 or BMI
97 ≥120% defined categories of severe OB for predicting clustered cardiometabolic risk are synthetized in
Table 3. The AUC values were 0.60 for BMI
97 ≥120%, and 0.63 for BMI Z-score >3 in children, and 0.62 and 0.66 respectively in adolescents. Compared to BMI
97 ≥120%, BMI Z-score >3 had higher specificity and PPV, but lower sensitivity and PPN in identifying children and adolescents with clustered cardiometabolic risk factors.
4. Discussion
The present study provided the empirical evidence that cardiometabolic risk factors increased with rising degrees of OB, as defined by BMI-derived metrics from the WHO system; specifically, the threshold of 120% BMI97 had a stronger association with clustered risk factors compared to BMI99 in children and adolescents. Furthermore, compared to BMI97 ≥120%, BMI Z-score >3 was associated with worse adiposity measures either in children and adolescents, although neither definition was significantly associated with individual cardiometabolic risk factors. On the contrary, adolescents with severe OB defined by BMI Z-score >3 had worse cCMR score and higher prevalence of clustered cardiometabolic risk factors than those defined by BMI97 ≥120%.
Severe OB affects a large number of children in Europe [
13]. Between 2007-2013 the prevalence of severe OB in 6- to 9-year-old school children from 21 countries of the WHO European Region ranged from 1.0% to 5.5% (WHO definition), with the highest levels (above 4%) in Southern Europe, including Italy.
As it emerged by a recent systematic review on the global prevalence of severe OB in childhood, several definitions have been used in children and adolescents [
8]. In particular, BMI
95 ≥120%, as proposed by the CDC and endorsed by the American Academy of Pediatrics [
5] and BMI ≥35 kg/m
2 were the most frequently used. Other definitions relied upon the cut-off of age- and gender-specific 99th percentile from the CDC or WHO standards, or BMI >3 SDS from the WHO system.
The drawbacks of using BMI Z-score for very high BMIs from the CDC system led to adopt the BMI
95 ≥120%. On the contrary, the BMI Z-score is still in use in those countries that adhered to the WHO definition, since it does not suffer from limitation associated to CDC [
2]. In fact, despite both CDC and WHO used the same database from the US National Center for Health Statistics [
14], some manipulations were done to build the WHO standards: measurements taken after 1973 were truncated to avoid the obesity epidemic and 3% of children with ‘unhealthy’ weights for heights were excluded. In addition, the SD23 restriction of the LMS (Lambda Mu and Sigma) method (i.e., the standard deviation at each age was fixed to the distance between ±2 SD and ±3 SD) was applied for data beyond the limits of the observed values (i.e., between -3 SD and 3 SD) [
2].
Previous cross-sectional studies reported that the prevalence of several cardiometabolic risk factors, such as dyslipidemia, hypertension, type 2 diabetes and fatty liver disease was higher in individuals with severe OB compared to mild OB with any of the definition used [
9,
15,
16,
17]. In agreement with previous studies, anthropometric, clinical, and individual cardiometabolic risk factors (except for fasting glucose and total cholesterol) progressively worsened from the lowest to the highest BMI category, as represented by BMI
97 ≥120%. In particular, the cCMR score was greatly higher both in children and adolescents with severe OB defined by BMI
97 ≥120% compared to BMI
99. These results confirm a previous study conducted by our group in a different cohort of youths with OB, where the definition of severe OB slightly varied from the definition adopted in the present study (respectively, BMI
95 ≥120% instead of BMI
97 ≥120%) [
18].
To make the situation more complicated, the definition of severe OB can be alternatively based on BMI
99 or BMI
99.9 (equivalent to 3 standard deviations). Therefore, we also compared anthropometric, clinical, and individual cardiometabolic risk factors between BMI
97 ≥120% to the BMI Z-score >3. Although the prevalence of severe OB was significantly higher when the cut-off of BMI
97 ≥120% was compared to BMI Z-score >3 both in children (69.7% vs 56.4%) and adolescents (63.9% vs 37.4%), both systems appeared to be interchangeable in children, without a particular superiority one to another in stratifying individuals at cardiometabolic risk. Instead, in adolescents worse cCMR scores and higher prevalence of clustered cardiometabolic risk factors were found in individuals with severe OB defined by BMI Z-score >3 compared to BMI
97 ≥120%. The ability to discriminate the cluster of at least two cardiometabolic risk factors between the two definitions of severe OB was modest with both definitions (AUCs ranging from 0.60 for BMI
97 ≥120% in children to 0.66 for BMI Z-score in adolescents) (
Table 3). Remarkably, it was quite similar to that reported by Ball et al. in a large sample of children and adolescents enrolled in the CANadian Pediatric Weight management Registry (AUC 0.62 for BMI Z-score and 0.64 for BMI
97 ≥120%) [
19]. In our sample BMI Z-score >3 had higher specificity and PPV, but lower sensitivity and PPN in identifying individuals with clustered cardiometabolic risk factors, especially in adolescents.
Our study is not exempt of having some limitations. Youths with OB were recruited in pediatric obesity services, therefore findings cannot be extended to the general population. Moreover, BMI is not the only factor influencing the cardiometabolic risk: genetics, perinatal and early life deteminants, lifestyle habits and fat distribution can also modulate the risk in children. In addition, the investigation was limited to cardiometabolic risk factors, without considering the respiratory, musculoskeletal, or psychosocial complications associated with severe OB. Lastly, the cross sectional design of the study does not allow to assess the ability of the BMI derived metrics to predict cardiometabolic outcomes in adulthood.
5. Conclusions
Our results show that within the WHO system, the definition of severe OB based on BMI97 ≥120% is superior to BMI99 but it is inferior to BMI Z score >3 as far as the association between severe OB and cardiometabolic risk factors is concerned. The definition based on BMI Z-score >3 has a discriminatory advantage over of the BMI97 ≥120% for identifying severely obese children at increased cardiometabolic risk, particularly in adolescents. However, the higher sensitivity of the BMI97 ≥120% definition in identifying a higher number of children and adolescents with severe OB at expense of lower specificity may provide advantages in terms of early cardiovascular prevention. Pediatricians should take the into consideration the implication of the use of BMI99 or BMI Z-score >3 in those countries that recommend using the WHO growth reference.
Author Contributions
Conceptualization, G.V., P.D.B.; methodology, G.V., P.D.B., G.B.; formal analysis, P.D.B; investigation, A.D.S.,, V.C., D.C., M.F.F., F.F., M.R.L., C.M.,G.M., E.M.d.G., A.M., E.M., M.W.; data curation, G.V., P.D.B, G.B.; writing—original draft preparation, G.V., P.D.B. A.D.S.; writing—review and editing, G.V., P.D.B, A.D.S.,, G.B, V.C., D.C., M.F.F., F.F., M.R.L., C.M.,G.M., E.M.d.G., A.M., E.M., M.W.; supervision, G.V., P.D.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Campania ‘Luigi Vanvitelli’ (reference number 834/2016) for youths observed from 2003-2013 and by the Ethics Committee of the AORN Santobono-Pausilipon (reference number 22877/2020) for youths observed from 2016 to 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
We encourage all authors of articles published in MDPI journals to share their research data. In this section, please provide details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study. Where no new data were created, or where data is unavailable due to privacy or ethical restrictions, a statement is still required. Suggested Data Availability Statements are available in section “MDPI Research Data Policies” at
https://www.mdpi.com/ethics.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes. Res. 1998, 6 Suppl 2, 51S–209S. [Google Scholar]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Dietitians of Canada; Canadian Paediatric Society; College of Family Physicians of Canada; Community Health Nurses of Canada; Secker, D. Promoting Optimal Monitoring of Child Growth in Canada: Using the New WHO Growth Charts. Can. J. Diet. Pract. Res. Publ. Dietit. Can. Rev. Can. Prat. Rech. En Diet. Une Publ. Diet. Can. 2010, 71, e1–3. [Google Scholar] [CrossRef]
- Valerio, G.; Maffeis, C.; Saggese, G.; Ambruzzi, M.A.; Balsamo, A.; Bellone, S.; Bergamini, M.; Bernasconi, S.; Bona, G.; Calcaterra, V.; et al. Diagnosis, Treatment and Prevention of Pediatric Obesity: Consensus Position Statement of the Italian Society for Pediatric Endocrinology and Diabetology and the Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 88. [Google Scholar] [CrossRef] [PubMed]
- Hampl, S.E.; Hassink, S.G.; Skinner, A.C.; Armstrong, S.C.; Barlow, S.E.; Bolling, C.F.; Avila Edwards, K.C.; Eneli, I.; Hamre, R.; Joseph, M.M.; et al. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity. Pediatrics 2023, 151, e2022060640. [Google Scholar] [CrossRef]
- Flegal, K.M.; Wei, R.; Ogden, C.L.; Freedman, D.S.; Johnson, C.L.; Curtin, L.R. Characterizing Extreme Values of Body Mass Index-for-Age by Using the 2000 Centers for Disease Control and Prevention Growth Charts. Am. J. Clin. Nutr. 2009, 90, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Dietz, W.H. Time to Adopt New Measures of Severe Obesity in Children and Adolescents. Pediatrics 2017, 140, e20172148. [Google Scholar] [CrossRef] [PubMed]
- Pinhas-Hamiel, O.; Hamiel, U.; Bendor, C.D.; Bardugo, A.; Twig, G.; Cukierman-Yaffe, T. The Global Spread of Severe Obesity in Toddlers, Children, and Adolescents: A Systematic Review and Meta-Analysis. Obes. Facts 2022, 15, 118–134. [Google Scholar] [CrossRef]
- Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults. N Engl J Med. 2015 Oct;373(14):1307-17. [CrossRef]
- Di Bonito, P.; Valerio, G.; Pacifico, L.; Chiesa, C.; Invitti, C.; Morandi, A.; Licenziati, M.R.; Manco, M.; Giudice, E.M.D.; Baroni, M.G.; et al. Impact of the 2017 Blood Pressure Guidelines by the American Academy of Pediatrics in Overweight/Obese Youth. J. Hypertens. 2019, 37, 732–738. [Google Scholar] [CrossRef] [PubMed]
- de Simone, G.; Mancusi, C.; Hanssen, H.; Genovesi, S.; Lurbe, E.; Parati, G.; Sendzikaite, S.; Valerio, G.; Di Bonito, P.; Di Salvo, G.; et al. Hypertension in Children and Adolescents. Eur. Heart J. 2022, 43, 3290–3301. [Google Scholar] [CrossRef] [PubMed]
- Saydah, S.; Bullard, K.M.; Imperatore, G.; Geiss, L.; Gregg, E.W. Cardiometabolic Risk Factors among US Adolescents and Young Adults and Risk of Early Mortality. Pediatrics 2013, 131, e679–686. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Starc, G.; Pérez, N.; Rito, A.I.; Kunešová, M.; et al. Prevalence of Severe Obesity among Primary School Children in 21 European Countries. Obes. Facts 2019, 12, 244–258. [Google Scholar] [CrossRef] [PubMed]
- Turck, D.; Michaelsen, K.F.; Shamir, R.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Kolacek, S.; et al. World Health Organization 2006 Child Growth Standards and 2007 Growth Reference Charts: A Discussion Paper by the Committee on Nutrition of the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Nur Zati Iwani, A.K.; Jalaludin, M.Y.; Roslan, F.A.; Mansor, F.; Md Zain, F.; Hong, J.Y.H.; Zin, R.M.W.M.; Yahya, A.; Ishak, Z.; Selamat, R.; et al. Cardiometabolic Risk Factors among Children Who Are Affected by Overweight, Obesity and Severe Obesity. Front. Public Health 2023, 11, 1097675. [Google Scholar] [CrossRef] [PubMed]
- Bendor, C.D.; Bardugo, A.; Pinhas-Hamiel, O.; Afek, A.; Twig, G. Cardiovascular Morbidity, Diabetes and Cancer Risk among Children and Adolescents with Severe Obesity. Cardiovasc. Diabetol. 2020, 19, 79. [Google Scholar] [CrossRef] [PubMed]
- Zabarsky, G.; Beek, C.; Hagman, E.; Pierpont, B.; Caprio, S.; Weiss, R. Impact of Severe Obesity on Cardiovascular Risk Factors in Youth. J. Pediatr. 2018, 192, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Valerio, G.; Maffeis, C.; Balsamo, A.; Del Giudice, E.M.; Brufani, C.; Grugni, G.; Licenziati, M.R.; Brambilla, P.; Manco, M. ; Childhood Obesity Group of the Italian Society of Pediatric Endocrinology and Diabetology Severe Obesity and Cardiometabolic Risk in Children: Comparison from Two International Classification Systems. PloS One 2013, 8, e83793. [Google Scholar] [CrossRef]
- Ball, G.D.C.; Sharma, A.K.; Moore, S.A.; Metzger, D.L.; Klein, D.; Morrison, K.M. ; CANadian Pediatric Weight management Registry (CANPWR) Investigators Measuring Severe Obesity in Pediatrics Using Body Mass Index-Derived Metrics from the Centers for Disease Control and Prevention and World Health Organization: A Secondary Analysis of CANadian Pediatric Weight Management Registry (CANPWR) Data. Eur. J. Pediatr. 2023, 182, 3679–3690. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).