1. Introduction
The atrophic maxilla is considered a challenge in oral rehabilitation and consequently in the patient's quality of life. The significant disproportion in the lateral, anteroposterior and vertical dimensions of the maxillary arches, resulting in the failure of osseointegrated implants due to insufficient bone quality and quantity. [
1,
2,
3,
4,
5]
Therefore, in relation to phonetics, mastication and aesthetics, the treatment and rehabilitation of patients with severely atrophic maxilla is of utmost importance, however, many challenges still arise.[
4,
5] Different types of treatment are available, including placement of short implants, elevation of the maxillary sinus floor, distraction osteogenesis, guided bone regeneration, and the use of zygomatic implants. [
6,
7]
Branemark introduziu os ZIs como uma nova alternativa de tratamento para ancoragem posterior em próteses implantossuportadas em pacientes maxilectomizados. Com a evolução da técnica a mesma foi inserida na reabilitação em maxilas severamente atróficas. [
8]
ZIs are a safe and effective option, with high success rates in clinical studies in the literature on the rehabilitation of atrophic maxilla. In some cases with extreme resorption, the use of zygomatic implants is indicated, associated or not with bone grafting. Another alternative would be the use of 04 zygomatic implants.[
9]
Total rehabilitation of atrophic maxillas with zygomatic implants (ZI) has become a more common practice encouraged by the growing number of relevant scientific publications evidencing high success and survival rates. However, the need for training and expertise of surgeons to correctly perform the technique is described in order to minimize possible complications such as: sinusitis, orbital perforation, zygomatic body fracture, and invasion of the infratemporal fossa. [
10,
11,
12]
The installation of zygomatic implants requires expertise and knowledge from the dental surgeon, as it is a complex procedure due to the delicate anatomical structures such as the orbit, maxillary sinus and zygomaticofacial nerve. Therefore, several surgical techniques have been described in order to facilitate the installation of zygomatic implants and to reduce the risks during and after surgery. However, there are still atypical complications that are rarely described in the literature and that are important to report in order to prepare surgeons for certain complications [
1,
10,
14].
This article describes an atypical case of tearing for 24 hours after the installation of a zygomatic implant.
2. Case Report
A 58-year-old male patient with black skin, no systemic alterations, who had been using a complete upper denture for 6 years, sought private care to undergo rehabilitation with dental implants. For planning the zygomatic fixations, the following were requested: surgical risk, panoramic radiography, computed tomography (efficient and accurate examination), preoperative laboratory tests (coagulogram, electrocardiogram, glycated hemoglobin, urine type I, creatinine, blood glucose, complete blood count), in addition to anamnesis and clinical examination intra and extra orally. During the physical examination, total edentulism in the maxilla was observed, with no mucosal pathologies, loss of upper lip projection and excessive lip sealing. The tomographic examination showed severe resorption of the maxilla (class VI – CAWHOOD & HOWELL) with extensive pneumatization of the maxillary sinuses [
13] (
Figure 1).
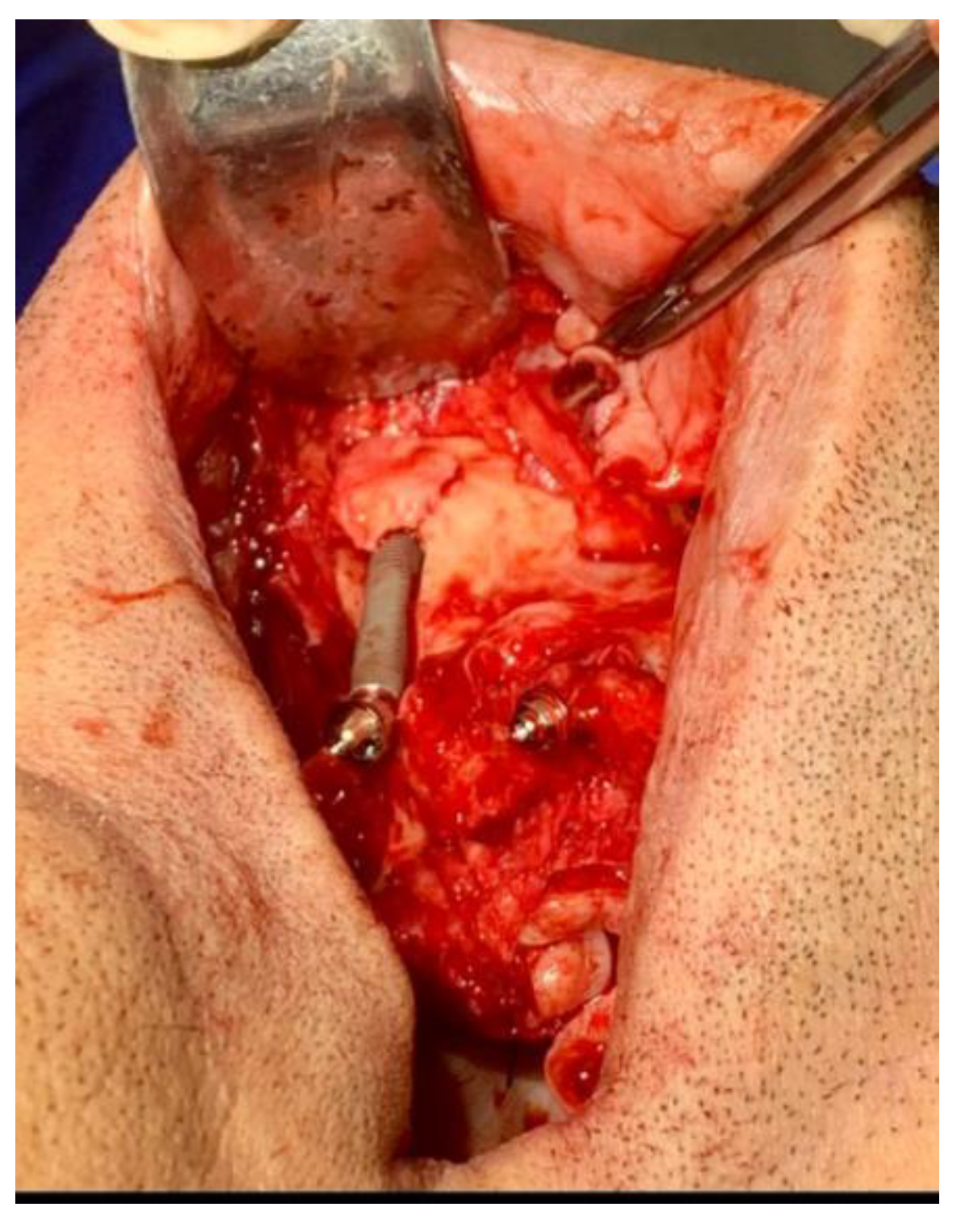
Extreme anteroposterior bone loss was observed and bilateral ZIs without the need for bone grafting were chosen as the best rehabilitation treatment for the patient. The patient underwent surgery on an outpatient basis under intravenous sedation intravenous performed by an anesthetist, which provides greater comfort to the patient during the intraoperative period and local anesthesia (Articaine 4% DFL – Rio de Janeiro-RJ Brasil). An incision was made in the region of the remaining alveolar process, extending from the second molar region to the contralateral second molar, and two more vertical posterior incisions and one anterior incision in the midline to facilitate detachment and exposure of the zygomatic body. After detachment, two conventional implants measuring 3.75 x 13.0 mm were installed in the anterior region of the maxilla, and one ZI on each side in the posterior region of the maxilla, measuring 4.0 x 35 mm on the right side and 4.0 x 37.5 mm on the left side. During the installation of the implant on the right side, a greenstick fracture of the zygomatic body occurred, so a second, deeper milling was performed in the zygomatic body (
Figure 2).
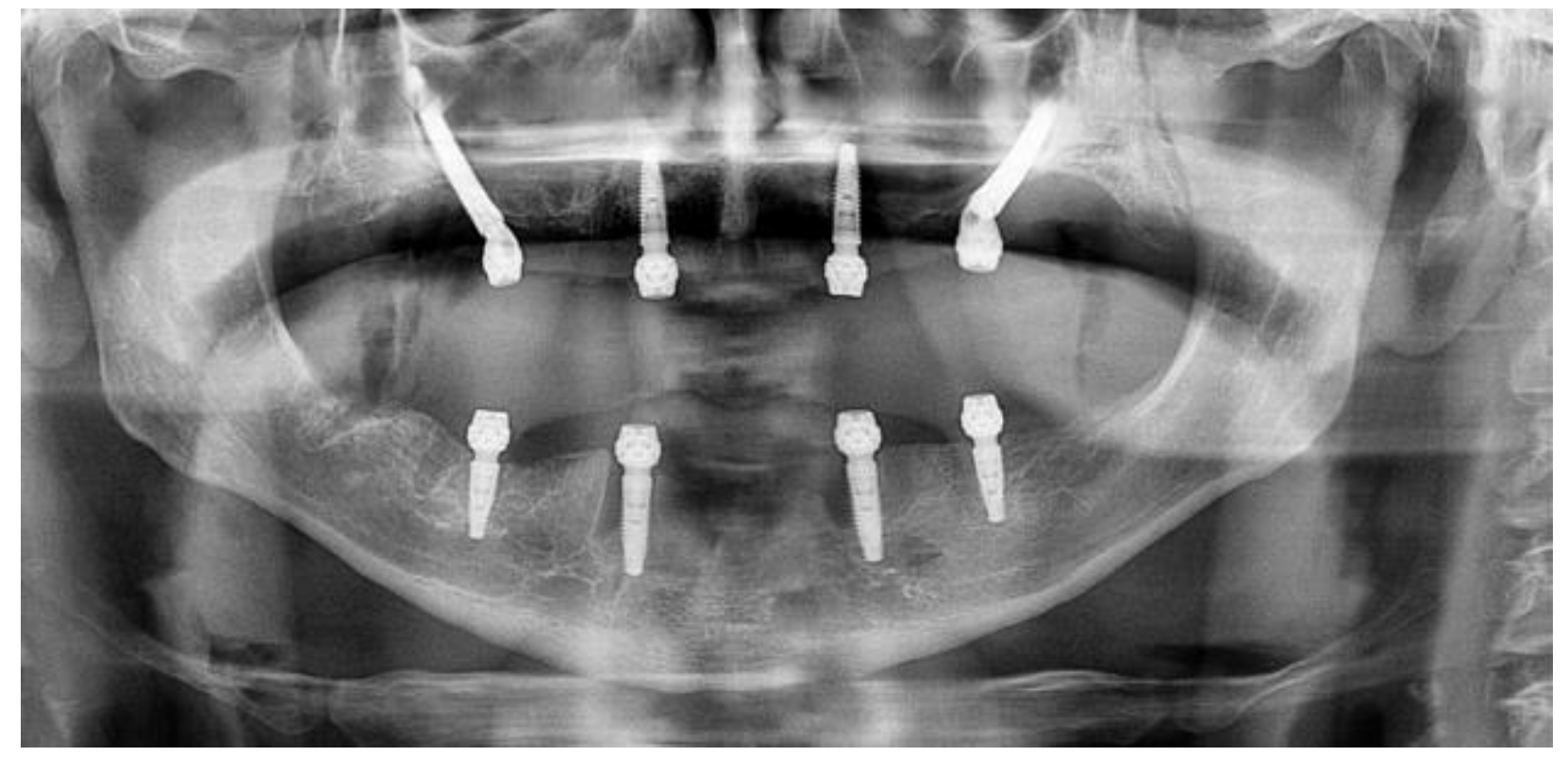
The anterior implants had a locking of 60N and the ZI had a locking of 90N. After installation of the implants and prosthetic components, suturing was performed with resorbable thread and a postoperative control panoramic radiograph was performed (
Figure 3).
The maxilla was immediately molded for the fabrication of a prosthesis with immediate loading. During the molding, the patient reported excessive tearing in his right eye, which subsided 24 hours after surgery. The implant-supported prosthesis was installed one week after surgery, and the patient is undergoing rehabilitation without any functional or aesthetic complaints.
The patient underwent active monitoring by the dental team responsible for the procedure in order to verify possible long-term changes, however, no changes occurred again and the patient continued with the ZIs in function.
It is important to understand that rehabilitation with zygomatic implants is not a technique that has come to replace rehabilitation with grafts, but rather as an adjuvant to the technical repertoire in extreme cases in which the technique with grafts has a doubtful prognosis.
3. Dicussion
Zygomatic implants (ZIs) are considered an alternative treatment for severe maxillary atrophy, and are recognized for their safety and high success rates.[
2,
5]These devices are composed of self-threading titanium with a regular surface, with varying lengths from 30 mm to 52.5 mm and a 45° inclination to adjust to the angle between the zygoma and the maxilla.[
1,
4,
8]
The surgical approach to zygomatic implants is characterized by limited intraoperative visibility due to the anatomical complexities of the region. This limitation, together with a technique that depends on the surgeon's expertise, can contribute to an increase in postoperative complication rates. Among the most common complications are penetration of the orbital cavity, which can result in extraocular injury, intracranial placement, injury to the infraorbital nerve and paresthesia of the zygomaticofacial nerve, in addition to penetration of the eyeball. [
12]
Postoperative tearing was a cause for concern for the surgical team, as there were no cases described in the literature with this type of complication. However, the clinical picture regressed 24 hours after surgery, leaving doubt as to the cause of this complication.
Studies in the scientific literature focused on anatomy show us possible explanations for this atypical case, such as the presence of a synapse between the zygomaticofacial nerve (branch of V2) and the lacrimal nerve (branch of V1). In other words, since they are part of the trigeminal nerve, stimulation during milling and installation of the implant near the foramen of the zygomaticofacial nerve stimulated excessive tear production for the lacrimal nerve. [
10,
11]
Another possibility is that the presence of a greenstick fracture near the zygomaticofacial foramen may have caused pinching of the nerve and consequently stimulation of the zygomaticofacial nerve to the lacrimal nerve. However, we believe that if this were the cause, the tearing would continue until the cause was removed.
In this context, we believe that since the milling and installation of the ZI are always close to the zygomaticofacial nerve foramen, this type of complication may become more frequent due to the increase in indications for rehabilitation through ZI.
One way to reduce tissue manipulation and milling close to the zygomaticofacial foramen is to use an initial drilling guide planned virtually in specific software. In this way, during virtual planning it would be possible to divert the milling along the nerve path and reduce detachment of the zygomatic body.[
14,
15,
16]
The literature on the use of zygomatic implants is extensive; however, randomized clinical trials with a long follow-up period, in addition to clinical case reports describing atypical complications such as the one in this article, are necessary. This would increase predictability and ways to avoid complications for dental surgeons.[
17,
18,
19,
20]
Greatest advantage of the surgical technique with ZIs is that the density of the zygomatic bone allows excellent initial stability of the implants, which enables correct osseointegration and allows them to be subjected to immediate load. Furthermore, other studies have shown that the success rate is higher in implants fixed in mature residual bone than in areas of grafted bone. [
21,
22,
23]
In cases where the installationand sucess of two zygomatic implants is necessary, both the need for detachment of the zygomatic body and the more restricted milling area increase the chances of manipulation of the zygomaticofacial foramen region, which allows us to suggest the presence of the possibility of this complication in the preoperative guidelines and in the service provision contract.
4. Conclusions
Therefore, it is concluded that the installation of ZI has proven to be a reliable technique for the rehabilitation of severely atrophic maxillar. However, further studies are necessary regarding atypical transoperative and postoperative complications regarding the complex anatomy involved, providing the surgeon with greater predictability.
Author Contributions
All authors attest that they meet the current ICMJE criteria for authorship. V.N.L collected, analyzed, and interpreted the clinical data and wrote the manuscript. L, K.T., G.A., L.F.O and O.M.F. made substantial contributions to the acquisition of the clinical data. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Consent to publish the case report was obtained. This report does not contain any personal information that could lead to the identification of the patient.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- BHALERAO, A. et al. Dynamic navigation for zygomatic implant placement: A randomized clinical study comparing the flapless versus the conventional approach. Journal of dentistry, v. 130, n. 104436, p. 104436, 2023a. [CrossRef]
- ERKUT, S.; UCKAN, S. Alveolar distraction osteogenesis and implant placement in a severely resorbed maxilla: A clinical report. The journal of prosthetic dentistry, v. 95, n. 5, p. 340– 343, 2006. Disponível em: . [CrossRef]
- PÉREZ, A. S. et al. Success rates of zygomatic implants for the rehabilitation of severely atrophic maxilla: A systematic review. Dentistry journal, v. 10, n. 8, p. 151, 2022. Disponível em: . [CrossRef]
- Brånemark P. et al., Zygoma Fixture in the Management of Advanced Atrophy of the Maxilla: Technique and Long-Term Results. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004;38:70–85. [CrossRef]
- Davis D.M. et al., The Emotional Effects of Tooth Loss: A Preliminary Quantitative Study. Br. Dent. J. 2000;188:503–506. [CrossRef]
- Aparicio C. et al., Zygomatic implants: indications, techniques and outcomes, and the zygomatic success code. Periodontol 2000. 2014 Oct;66(1):41-58.
- Kawade R. et al., Zygomatic Implant-Supported Prosthetic Rehabilitation of a Patient with Post-COVID-19 Mucormycosis and Maxillectomy. Case Rep Dent. 2024 May 10;2024:8193822. PMID: 38764612; PMCID: PMC11101258. [CrossRef]
- Chan MFW-Y. Howell RA, Cawood JI. Prosthetic rehabilitation of the atrophic maxilla using pre-implant surgery and endosseous implants. Britsh Dental Journal 1996;181: 51-58.
- BEDROSSIAN, E. et al. Zygoma implant under function: biomechanical principles clarified. International journal of implant dentistry, v. 9, n. 1, p. 15, 2023. [CrossRef]
- Chrcanovic BR, Abreu MH. Survival and complications of zygomatic implants: a systematic review. Oral Maxillofac Surg. 2013 Jun;17(2):81-9. Epub 2012 May 6. PMID: 22562293. [CrossRef]
- Kämmerer PW. Et al.,Evaluation of surgical techniques in survival rate and complications of zygomatic implants for the rehabilitation of the atrophic edentulous maxilla: a systematic review. Int J Implant Dent. 2023 May 17;9(1):11. PMID: 37198345; PMCID: PMC10192488. [CrossRef]
- Gabriele G. et al.,Technique-Related Survival Rate and Complications of Zygomatic Implant Placement: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2023 Oct 17;38(5):855-875. [CrossRef]
- Cawood JI, Howell RA. A Classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988; 17:232-236.
- Rinaldi M, Ganz SD. Computer-Guided Approach for Placement of Zygomatic Implants: Novel Protocol and Surgical Guide. Compend Contin Educ Dent. 2019 Mar;40(3):e1-e4. PMID: 30829495.
- Goiato MC, Pellizzer EP, Moreno A, Gennari-Filho H, dos Santos DM, Santiago JF Jr, et al. Implants in the zygomatic bone for maxillary prosthetic rehabilitation: a systematic review. Int J Oral Maxillofac Surg. 2014;43(6):748-57. [CrossRef]
- Fernández H, Gómez-Delgado A, Trujillo-Saldarriaga S, VarónCardona D, Castro-Núñez J. Zygomatic implants for the management of the severely atrophied maxilla: a retrospective analysis of 244 implants. J Oral Maxillofac Surg. 2014;72(5):887-91. [CrossRef]
- Gonçalves LM, Gonçalves TM, Rodrigues AH, Lanza MD, do Nascimento PR, Girundi FM. Intra-and extraoral prostheses retained by zygoma implants following resection of the upper lip and nose. J Prosthodont. 2015;24(2):172-7. [CrossRef]
- Albrektsson T, Zarb GA, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986,1(1):11-25.
- Bedrossian E. Rehabilitation of the edentulous maxilla with the zygoma concept: a 7-year prospective study. Int J Oral Maxillofac Implants 2010;25(6):1213-21.
- Nkenke E, Hahn M, Lell M, Wiltfang J, Schultze MS, Stech B, et al. Anatomic site evaluation of the zygomatic bone for dental implant placement. Clin Oral Implants Res. 2003; 14(1):72-9. [CrossRef]
- Pena N, Campos PC, De Almeida SM, Boscolo FN. Determination of the length of zygomatic implants through computed tomography: establishing a protocol. Dentomaxillofac Radiol 2008;37(8):453-7. http://dx.doi.org/10.1259/dmfr/16676031.
- Rosenstein JD, Dym H. Zygomatic Implants: A Solution for the Atrophic Maxilla: 2021 Update. Dent Clin North Am. 2021;65(1):229-239.
- Davó R, Pons O, Rojas J, Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur J Oral Implantology. 2010;3(4):323-34. PMid:21180685.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).