1. Introduction
It is well documented that the average age of death is increasing and there has been an increase in chronic illnesses as the primary cause of death. Globally, the largest cause of death is ischaemic heart disease, accounting for 13% of all deaths and rising from 2.7 million deaths in 2000 to 9.1 million in 2021.
1 In 2020 and 2021, COVID-19 was the second-leading cause of death, followed by stroke and chronic obstructive pulmonary disease (COPD). In Canada, the leading causes of death in 2019 were ischaemic heart disease, Alzheimer’s and dementia, trachea, bronchus, lung cancer, and stroke [
1]. In 2020 and 2021 COVID-19 was the fourth-leading cause of death in Canada.
The increased prevalence of chronic diseases and multimorbid conditions underscores the limitations of monitoring mortality using a single cause of death. There are increasing numbers of people with multiple comorbidities, and this is increasing at a rate independent of aging [
2,
3]. Despite this, most research and mortality surveillance is focussed on single risk factors or single diseases. This shortcoming leaves gaps in our knowledge about disease interactions and how these may influence occurrence, treatment, and outcomes [
4,
5].
A comparison of underlying versus multiple cause approaches in France and Italy showed that the underlying cause approach underestimates the role of certain conditions, such as hypertension, blood disorders, renal failure, and infectious diseases, which often act as contributory causes [
5,
6]. In Australia, it was shown that incorporating multiple causes of death reveals that certain conditions, such as hypertension, atrial fibrillation, and diabetes, contribute substantially more to mortality than is recognized when only the underlying cause is considered [
7].
The average number of causes reported on death certificates varies across countries and regions. In Italy, the mean was 4.3 causes per certificate [
8], while in Brazil, it ranged from 2.07 to 3.15 depending on the state, with a national average of 2.81 [
9,
10]. In Italy and France in 2003, deaths had on average 4.0 and 3.1 causes reported on the death certificate respectively [
5]. Recent research in Australia calculated an average of 3.4 causes on average, where 24.4% of deaths had 4 or more causes [
7]. While the underlying cause of death remains essential for historical trends and international comparisons, multiple-cause-of-death data can offer new insights into mortality studies.
Various methods have been developed to analyze multiple cause of death data, including descriptive measures such as the proportional measure for multiple causes and the Standardized Ratio of Multiple to Underlying causes (SRMU) [
11,
12,
13,
14,
15,
16]. Another approach involves weighting multiple causes of death, which can identify underrecognized contributors to mortality [
15]. Multiple-cause-of-death weighting methods have been proposed to improve mortality rate calculations, as they can identify underrecognized contributors to mortality; however, they have only been used in a small number of studies [
7,
15,
17,
18,
19,
20,
21,
22].
The objective of this study is to provide a comprehensive population-level analysis of cause-related mortality in Canada, with a specific aim to highlight the changes in leading causes of death before the COVID-19 pandemic and the years following the onset of the COVID-19 pandemic. There has been no prior attempt to analyze multiple cause-related mortality in Canada at the population level and this study is the first to assess national trends of multiple cause indicators over time, by age group, and by neighbourhood income quintile [
23,
24,
25].
2. Materials and Methods
Deaths from January 1, 2018, through 31 December 2021, were extracted from individual-level death records in the Canadian Vital Statistics, Deaths Database (CVSD), with access provided through the secure Statistics Canada Research Data Centre program [
26]. Individual-level data including age at death, sex, year of death, province of registration, registration number, and underlying cause of death were used.
The provincial and territorial Vital Statistics Registries report to Statistics Canada which compiles a census of all deaths occurring in Canada each year. Deaths are coded according to the International Classification of Diseases (ICD) version at the time of death. To facilitate easier comparison, we opted to follow the coding schema proposed by Bishop et al. and constructed 21 groups for level 1 leading cause of death and 138 groups for level 2 leading cause of death data using ICD-10 coding schemas [
7]. The derived list included leading causes of death in Canada and usually non-fatal conditions that contribute to morbidity. Death records with an ill-defined underlying cause of death were excluded.
A supplementary multiple cause of death file was joined to the CVSD by year of death, province of registration, and registration number. Multiple cause-of-death data is available in two forms, “entity-axis” which represents what is written on a death certificate in terms of ICD codes including what number the cause of death was labelled as on the death certificate, and “record-axis” data which represents further processing of the entity-axis data, and includes an underlying cause of death and up to 19 contributing causes of death. Record-axis data were used in calculations of mortality rates based on the underlying cause. Entity-axis entries were used for the calculation of rates using contributing cause weighting as these entries reflect the certifiers’ perspective on potential pathways of causes related to the death event.
An additional geographic file developed via Postal Code conversion is used to link each CVSD record to geographic information, including neighborhood income quintiles. Income quintiles are estimated using the household size-adjusted income per single person equivalent for small geographic areas, then ranked within a given Census Metropolitan Area into 5 quintiles from Q1 (the lowest) to Q5 (the highest) according to the calculated income per single person equivalent. The calculated area-based quintiles are linked to death records via the Postal Code of residence at the time of death.
We calculated the age- and sex-standardized mortality rates for when a specific cause is reported as the underlying cause of death, and when the same cause is listed as a multiple cause of death The 2021 Canadian population, categorized by sex and five-year age intervals, served as the standard population.
The above rates were used to calculate the SRMU, which compares age-standardized rates based on underlying and multiple causes, estimating the contribution of a cause to mortality [
5,
7]. This ratio highlights how much a condition’s contribution to overall mortality is underestimated when only the underlying cause is considered. A low SRMU indicates the condition is often identified as the underlying cause, while a high SRMU suggests it is rarely selected as such.
For each cause group, we calculated the ASMR (per 100,000) based on the single underlying cause of death for the years 2018–2021. We also calculated the ASMR for 3 different weighting strategies [
11,
15]. First, we applied a 50% weight to the underlying cause, with the remaining 50% of the weight apportioned across all contributing causes (ASMR
w1). Second, all underlying and contributing causes were weighted equally (ASMR
w2). Third, the underlying cause was weighted twice that of each contributing cause (ASMR
w3).
ASMRs were directly standardized to the 2021 Canadian Population Estimates by 5-year age groups. Analysis was undertaken using SAS Enterprise version 9.4 or R 4.2.
3. Results
The impact of the COVID-19 pandemic resulted in increases in the number of deaths and higher ASMRs for both males and females. While the number of deaths decreased between 2020 and 2021, it remains higher than in 2019. The same pattern is visible in the number of mentions, which sums up the total number of conditions listed on each death certificate.
Since 2018 there has been a small increase in the percentage of deaths coded with a single underlying cause (
Table 1). Following this, there has been a decrease in deaths coded with between 2 and 4 contributing causes, while there was an increase in the percentage of deaths coded with more than 4 contributing causes. In 2021, the second year of the COVID-19 pandemic, the percentage of deaths with 1 cause is 24.56, compared to 20.17 in 2019. The percent of deaths with more than 1 cause is lower in 2021 compared to 2019, with 25.53 percent of deaths having 4 or more causes in 2019 compared to 22.99 percent of deaths in 2021.
There are consistent differences in the average number of causes recorded by neighbourhood income quintile (
Table 1). Since 2018, the difference in the average number of causes between the highest and lowest neighbourhood income quintiles was 0.19. Deaths occurring to those residing in the lowest income quintile neighbourhoods had an average of 3.30 causes in 2021 and those in the highest neighbourhood income quintiles had an average of 3.11 causes. This difference between income quintiles was consistent across the study period, even though the average number of causes in 2021 differs from 2018 and 2019.
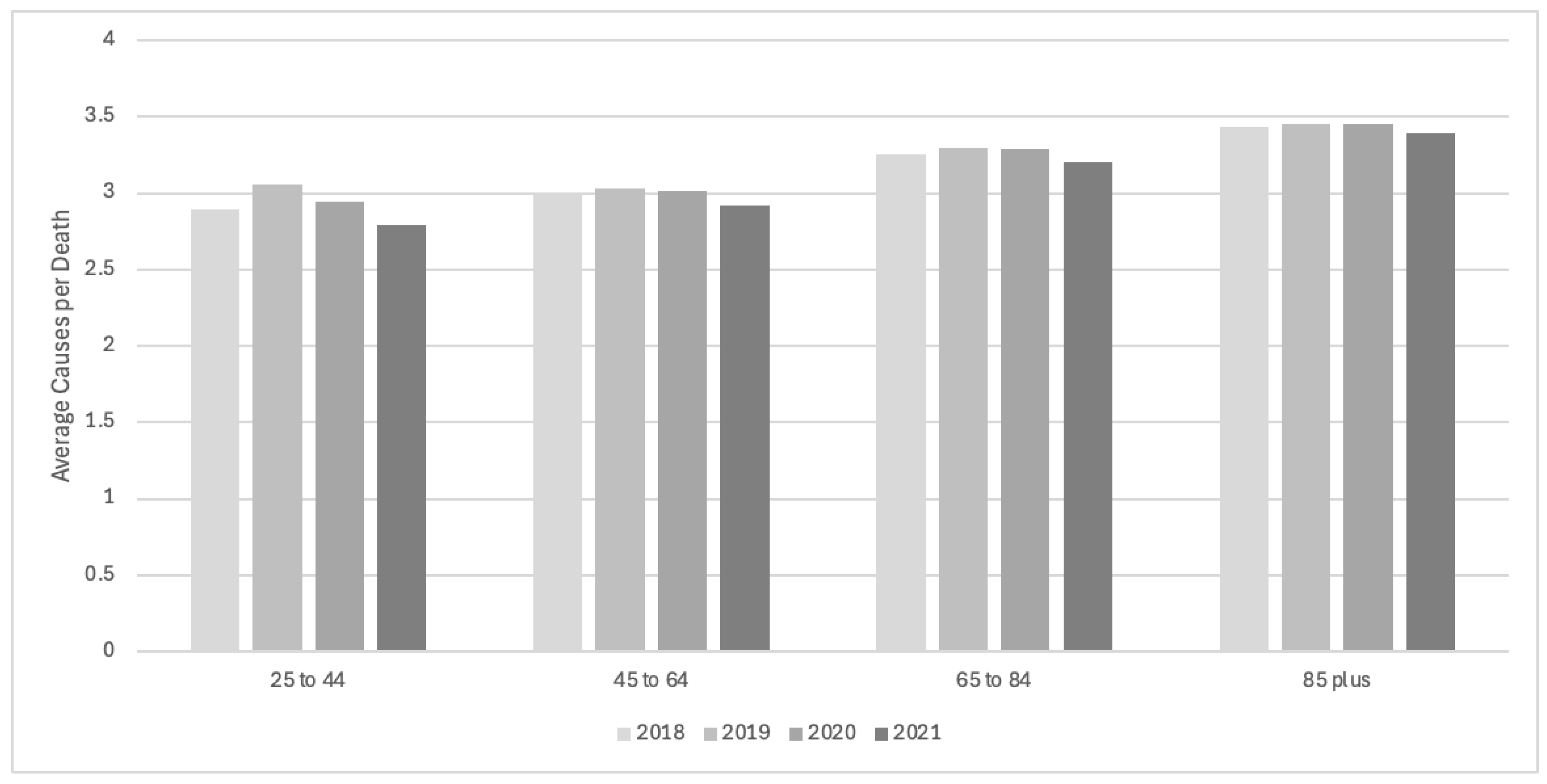
The average number of causes on death certificates by age group has changed between 2018 and 2021 (
Figure 1). As expected, the average number of causes is higher for older age groups, with an average in 2018 of 3.43 causes for deaths occurring to those 85 years and older and 2.89 for those 25 to 44. The average number of causes for those aged 25 to 44 was lower in 2021 at 2.79.
Tables 2a and 2b show the ASMR for the top 20 causes and conditions using the underlying cause approach and multiple-cause weighting approaches. From these tables, it is clear the extent to which using multiple-cause weighting approaches changes the rank order of diseases. The diseases most often coded as underlying are lowered in rankings, and the conditions or complications most often coded as contributing are increased in rankings (Tables 2a and 2b).
The highest ASMRs and top three causes of death are dementia & Alzheimer’s disease, ischaemic heart disease, and cerebrovascular diseases and remain as such for each weighting method. When weighting methods were applied, the rank order of some conditions decreased, including colorectal cancer, falls, other blood cancers, pancreatic cancer, breast cancer, and COVID-19. The largest decreases in rank are seen when using the 50% underlying weight method (ASMRw1). In general, the decreased rank for these diseases is not surprising as they are more often coded as the underlying cause and have fewer contributing causes.
The conditions that increase the most in relative contribution to mortality are renal failure, hypertension, pneumonitis, pneumonia, atrial fibrillation, septicemia, and artery diseases. These causes are most often coded as causes contributing to death rather than the underlying cause, but when weighting is applied, they exert a strong influence on weighted ASMRs.
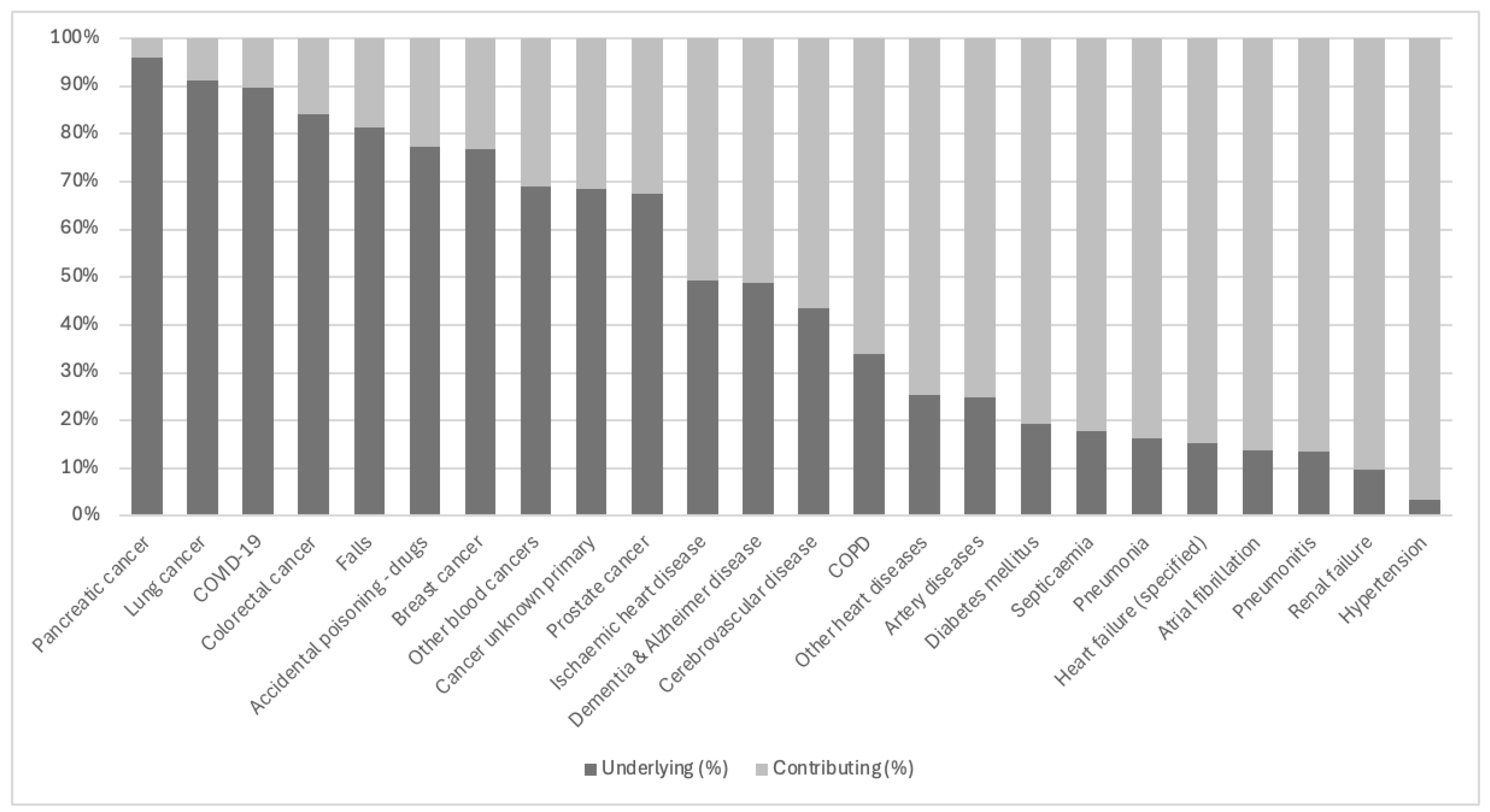
Figure 2 shows the relative percent of coding as underlying or contributing causes for the most common conditions, sorted by most to least often coded as the underlying cause. The conditions displayed here are all among the top 20 causes listed on the death certificates among all mentions. It is important to note that the ordering of this figure doesn’t show the contribution to overall mortality rates, only the percent of each cause coded as underlying or contributing.
Cancers and injuries are most often indicated as the underlying cause of death when mentioned on the death certificate, ranging from 95.87% for pancreatic cancer to 67.46% for prostate cancer. COVID-19 is an outlier for infectious diseases, where it is indicated as the underlying cause in 89.56% of mentions. This is most likely reflective of international coding practice guidelines implemented at the beginning of the COVID-19 pandemic.
Table 2a.
Age-standardized mortality rates by leading causes of death, unweighted and by weighting method, Canada.
Table 2a.
Age-standardized mortality rates by leading causes of death, unweighted and by weighting method, Canada.
| Rank |
Cause of Death |
ASMR |
Change |
Cause of Death |
ASMRw1
|
| 1 |
Dementia & Alzheimer’s disease |
104.24 |
0 |
Dementia & Alzheimer’s disease |
79.98 |
| 2 |
Ischemic heart disease |
97.29 |
0 |
Ischemic heart disease |
71.45 |
| 3 |
Lung cancer |
48.87 |
2 |
Cerebrovascular disease |
33.66 |
| 4 |
COVID-19 |
42.86 |
−1 |
Lung cancer |
32.79 |
| 5 |
Cerebrovascular disease |
40.88 |
1 |
COPD |
25.48 |
| 6 |
COPD |
29.09 |
−2 |
COVID-19 |
24.88 |
| 7 |
Colorectal cancer |
24.79 |
10 |
Renal failure |
23.86 |
| 8 |
Falls |
21.68 |
7 |
Pneumonia |
22.97 |
| 9 |
Diabetes mellitus |
20.32 |
0 |
Diabetes mellitus |
22.32 |
| 10 |
Other blood cancers |
15.43 |
n/a |
Cancer secondary site |
20.81 |
| 11 |
Pancreatic cancer |
14.70 |
5 |
Heart failure (specified) |
20.05 |
| 12 |
Breast cancer |
14.64 |
50 |
Hypertension |
18.99 |
| 13 |
Prostate cancer |
13.69 |
−6 |
Colorectal cancer |
17.00 |
| 14 |
Other heart diseases |
13.45 |
0 |
Other heart diseases |
14.90 |
| 15 |
Pneumonia |
13.3 |
5 |
Atrial fibrillation |
14.12 |
| 16 |
Heart failure (specified) |
12.99 |
36 |
Pneumonitis |
12.18 |
| 17 |
Renal failure |
12.08 |
−9 |
Falls |
11.40 |
| 18 |
Accidental poisoning—drugs |
11.17 |
−8 |
Other blood cancers |
11.16 |
| 19 |
Cancer unknown primary |
10.78 |
−8 |
Pancreatic cancer |
10.70 |
| 20 |
Atrial fibrillation |
10.67 |
−8 |
Breast cancer |
10.42 |
Table 2b.
Age-standardized mortality rates by leading causes of death, unweighted and by weighting method, Canada.
Table 2b.
Age-standardized mortality rates by leading causes of death, unweighted and by weighting method, Canada.
| Change |
Cause of Death |
ASMRw2
|
Change |
Cause of Death |
ASMRw3
|
| 0 |
Dementia & Alzheimer’s disease |
70.92 |
0 |
Dementia & Alzheimer’s disease |
78.16 |
| 0 |
Ischemic heart disease |
61.06 |
0 |
Ischemic heart disease |
68.57 |
| 2 |
Cerebrovascular disease |
31.03 |
2 |
Cerebrovascular disease |
33.16 |
| 13 |
Renal failure |
29.68 |
−1 |
Lung cancer |
32.9 |
| -2 |
Lung cancer |
27.98 |
12 |
Renal failure |
26.35 |
| 9 |
Pneumonia |
25.93 |
0 |
COPD |
24.59 |
| 55 |
Hypertension |
25.8 |
−3 |
COVID-19 |
23.03 |
| n/a |
Cancer secondary site |
25.77 |
7 |
Pneumonia |
22.98 |
| -3 |
COPD |
23.63 |
53 |
Hypertension |
21.61 |
| 6 |
Heart failure (specified) |
23.2 |
−1 |
Diabetes mellitus |
21.46 |
| -2 |
Diabetes mellitus |
22.28 |
5 |
Heart failure (specified) |
21.26 |
| -8 |
COVID-19 |
17.74 |
n/a |
Cancer secondary site |
19.32 |
| 7 |
Atrial fibrillation |
16.2 |
−6 |
Colorectal cancer |
16.93 |
| 0 |
Other heart diseases |
15.5 |
6 |
Atrial fibrillation |
15.36 |
| -8 |
Colorectal cancer |
14.53 |
−1 |
Other heart diseases |
15.04 |
| 36 |
Pneumonitis |
13.79 |
36 |
Pneumonitis |
12.01 |
| 33 |
Septicemia |
10.46 |
−7 |
Other blood cancers |
10.91 |
| 23 |
Artery diseases |
10.11 |
−7 |
Pancreatic cancer |
10.81 |
| -8 |
Pancreatic cancer |
9.84 |
−7 |
Breast cancer |
10.43 |
| -10 |
Other blood cancers |
9.59 |
21 |
Artery diseases |
10.13 |
Conditions listed on the right side of the
x-axis in
Figure 2 show causes of death that are most often indicated as contributing to mortality rather than the underlying cause. For hypertension, it is coded as a contributing cause in 96.64% of deaths where it is mentioned. Other causes such as renal failure, pneumonitis, arterial fibrillation, or heart failure are also coded much more often as a contributing factor to a death.
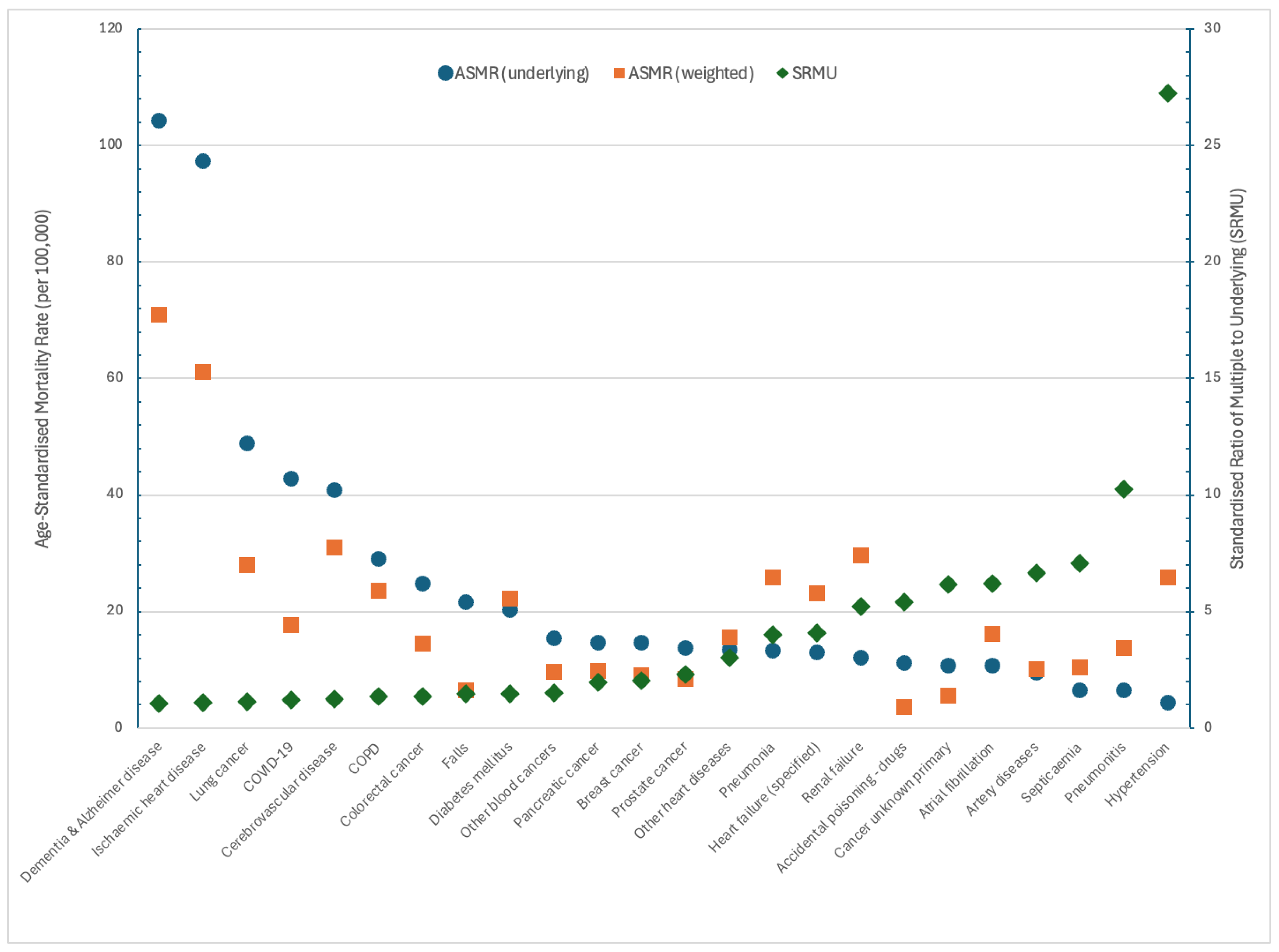
Figure 3 shows the ASMRs for selected causes (blue circles) and the ASMR
w2 where the underlying cause was weighted double each contributing cause (orange squares). The SRMU for each cause (green diamonds) is shown on the right
y-axis and causes are ordered by the lowest to highest SRMU. The results of this differ from
Figure 2, as the SRMU is based on standardized rates, not unweighted percentages.
The lowest SRMU is for dementia & Alzheimer’s, indicating that these conditions are generally coded as the underlying cause rather than the contributing cause. As such, when weighting techniques are used, the weighted ASMR is reduced. In contrast, the SRMU for hypertension is very high, showing how it is almost always coded as a contributing cause of death. Similarly, the ASMR for hypertension increases using a weighted approach.
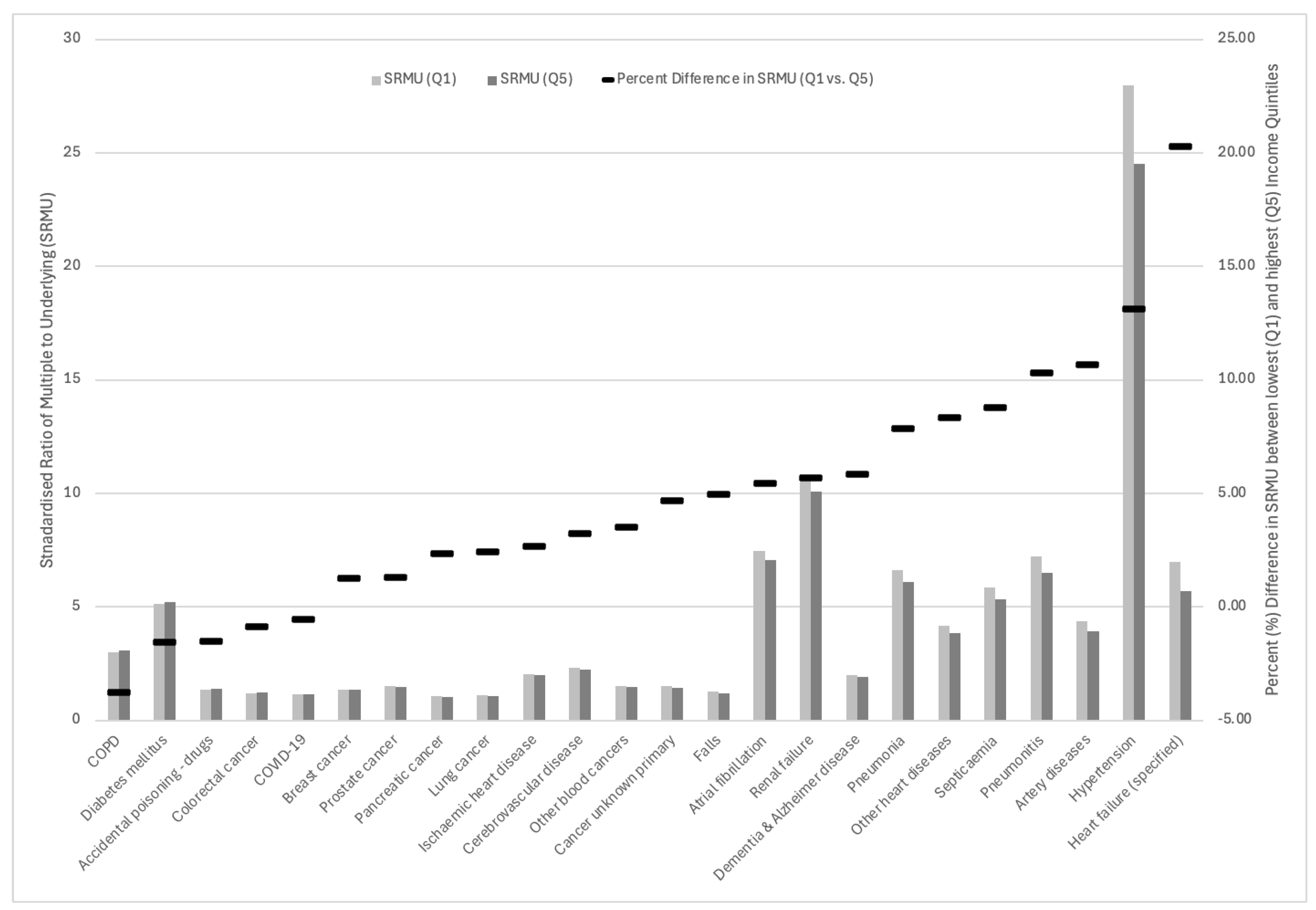
Examining the SRMU by income neighbourhood quintile highlights differences in how certain diseases are indicated as underlying or contributing causes.
Figure 4 shows the SRMU by cause of deaths in the lowest (Q1) and highest (Q5) income quintile neighbourhoods. The secondary
y-axis shows the percent (%) difference between the Q1 and Q5 SRMUs. The largest percent differences in the SRMU are for three major cardiovascular diseases: heart failure, hypertension, and artery diseases.
The smallest percent differences in the SRMU between the lowest and highest income quintiles are for COPD, diabetes mellitus, accidental poisoning—drugs, colorectal cancer, and COVID-19, where the differences are all below 5%. There are also smaller differences in other cancers including breast, prostate, pancreatic, and lung cancers. Except for diabetes mellitus, the smallest percent differences between income quintiles are for diseases with low SRMUs that are most often coded as the underlying cause.
4. Discussion
This paper provides the first comprehensive population-level estimates of multiple-cause mortality in Canada, encompassing the years preceding and during the COVID-19 pandemic. These estimates were developed to provide a comparison to recent work in Australia by Bishop et. al. and to extend this work through the analysis of socioeconomic inequalities [
7].
We have found key differences in mortality rates calculated using a single underlying cause compared to rates considering multiple contributing causes. As with underlying-cause mortality rates, there are important differences in multiple-cause mortality rates by age group and income quintile.
The proportion of deaths involving more than 4 causes of death has increased over time, reflecting an aging population and a related increasing complexity in the causes and conditions contributing to death. This may also reflect changes in coding practices rather than shifts in disease patterns and contributions to mortality. These changes are more pronounced in 2021, which could be attributed to either a lagged impact on mortality of changes to healthcare provision due to the COVID-19 pandemic, or delays in reporting for complex cases that may diminish with revisions to vital statistics records.
Large rate differences were found between ASMRs based on the underlying cause and multiple cause weighting approaches. Dementia and Alzheimer’s disease and ischaemic heart disease were the top causes across all approaches. The rank of cerebrovascular disease increased via weighting approaches, while lung cancer decreased. COVID-19 was the fourth-ranked disease in 2021, but this was reduced when weighting was applied.
Although our findings do not alter the ranking of the 3 leading causes of death, they strongly suggest that ignoring contributory causes results in a significant underestimation of the role played by certain conditions in the process leading to death. The ranks of hypertension, pneumonitis, pneumonia, septicemia, renal failure, and artery diseases show large increases in their rank order across the weighting approaches. These conditions fall into two broad categories as discussed by Desequelles [
5].
The first category includes diseases that are not directly lethal but act as background factors, increasing the risk of death when combined with other serious conditions. These conditions often exhibit “synergistic” or “additive” effects [
27]. Across all weighting approaches, pneumonitis increased significantly in the ranking of weighted ASMRs. Pneumonitis has been recognized as contributing significantly to mortality and hypersensitivity pneumonitis-related deaths have increased substantially in recent years, particularly for those in older age groups with pulmonary functional impairments related to other conditions [
28,
29]. A Danish population-based study found pneumonitis patients had higher comorbidity rates and nearly double the mortality risk compared to matched controls, with most deaths attributed to heart and lung diseases [
30]. Similarly, hypertension is frequently cited as a contributory cause of death and has been discussed elsewhere as a mortality risk when paired with other diseases [
31].
The second category includes complications arising from either the primary disease or its medical treatment, particularly conditions like blood disorders. Using the underlying cause approach also overlooks the contribution of conditions like anemia and coagulation defects to mortality [
32,
33]. These blood disorders can result from other diseases, such as liver conditions, or treatments like cancer therapy. Other examples in this category include renal failure and sepsis. Renal failure can arise as a complication of diabetes, while sepsis and other infections remain significant contributors to mortality, not as primary causes but as contributory factors.
Grouping of causes using ICD chapters may underestimate the actual role of infectious diseases in mortality as infections such as influenza, pneumonia, and acute bronchitis are classified under other chapters. Our findings show that infectious diseases, including septicemia and pneumonia, are leading factors of mortality as contributory causes, as was the case before the epidemiological transition [
34,
35]. Population aging may lead to a resurgence of infectious diseases, as chronic conditions weaken the body, leaving it vulnerable to lethal infections [
36]. Research for septicemia has shown that there is approximately a 2-fold black-white disparity in septicemia deaths, with socioeconomic status the strongest mediator of this disparity [
37]. This reinforces the need for a multiple cause-of-death approach for surveillance of infectious disease trends [
36].
Unique to this study, SRMUs have been calculated by cause and by neighbourhood income quintile. Causes and conditions with the highest percent difference between low- and high-income quintiles are also those with high SRMUs and are those that are substantial risk factors or disease complications. This suggests that there are pronounced differences between income quintiles, where these causes of death in lower-income areas are coded as an underlying cause more often than in higher-income neighbourhoods.
Our study has several limitations, the most notable being the reliance on how causes are positioned on death certificates for classifying multiple causes of death. This method depends on the accuracy and thoroughness of physicians in reporting both the chains of events leading to death and contributory causes. Other analyses on multiple-cause mortality during the COVID-19 pandemic have noted the consistent underreporting of multiple causes before the pandemic, which may have inflated excess death estimates, and the replacement coding of COVID-19 as the underlying cause instead of other conditions, potentially affecting the SRMU denominators [
17].
Analyzing multiple-cause data is more complex than focusing solely on the underlying cause of death. Key considerations include recognizing that the international death certificate format is not designed to capture all conditions or diseases the deceased may have had. Multiple-cause data from death certificates do not provide a complete list of a decedent’s conditions and may not accurately reflect disease prevalence. As such, it’s important to differentiate between dying from a condition and dying from it. For instance, not all individuals with diabetes die from it, so it may not always be listed as a contributing cause on the certificate [
24].
5. Conclusions
Mortality statistics are most often calculated and reported using a single underlying cause of death determined from the causes and conditions reported on the death certificate. This is despite a long-standing recognition that with population aging and an increasing proportion of the population with multiple, concurrent chronic conditions, analysis based on a single, underlying cause is increasingly unsatisfactory, especially for the very old [
38,
39,
40]. This research contributes to a growing body of evidence that demonstrates the significant benefit that regularized calculation and reporting of multiple-cause indicators can have for disease surveillance.
Using multiple cause of death approaches provides a clearer image of the pathological involvement of the causes contributing to death. This requires, however, high-quality cause-of-death coding. Given that the World Health Organization doesn’t require multiple-cause data from member countries, there are still many places that only record the underlying cause of death. As such, improvements in death certificate registration and data protection rules may first be necessary to enhance international surveillance of mortality statistics.
Author Contributions
Conceptualization, P.P., T.M. and M.L.-B.; methodology, P.P., M.K., T.M. and M.L.-B.; formal analysis, P.P., M.K. and M.L.-B.; writing—review and editing, P.P. and M.K.; visualization, P.P. and M.K.; supervision, P.P.; funding acquisition, P.P. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
This research was conducted at Carleton University, a part of the Canadian Research Data Centre Network (CRDCN). This service is provided through the support of the Canada Foundation for Innovation, the Canadian Institutes of Health Research, the Social Sciences and Humanities Research Council, and Statistics Canada, and through the support of Carleton University. All views expressed in this work are our own.
Funding:
This research was funded by the Social Sciences and Humanities Research Council of Canada, grant number 435-2021-1052.
Institutional Review Board Statement
Approval for data access was provided through the Statistics Canada Research Data Centre program, project 21-MAPA-CAR-7072.
Data Availability Statement
Data used in this project were provided by Statistics Canada and accessed through one or more of the RDCs (Research Data Centre) in the Canadian Research Data Centre Network (CRDCN). Because of the confidential nature of these microdata, they cannot be shared. Researchers in Canada working at one of CRDCN’s member institutions can access the data at no additional cost to the researcher. Other researchers will have to pay cost-recovery to access the data. Access to the data is subject to a background check and research approval process. The protocols for data access, including fees for researchers at non-CRDCN institutions, can be found on the CRDCN website (
www.crdcn.ca).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization Global Health Estimates: Leading Causes of Death. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (accessed on 23 September 2024).
- Gerhardt, T.; Gerhardt, L.M.S.; Ouwerkerk, W.; Roth, G.A.; Dickstein, K.; Collins, S.P.; Cleland, J.G.F.; Dahlstrom, U.; Tay, W.T.; Ertl, G.; et al. Multimorbidity in Patients with Acute Heart Failure across World Regions and Country Income Levels (REPORT-HF): A Prospective, Multicentre, Global Cohort Study. Lancet Glob. Heal. 2023, 11, e1874–e1884. [Google Scholar] [CrossRef] [PubMed]
- Tran, J.; Norton, R.; Conrad, N.; Rahimian, F.; Canoy, D.; Nazarzadeh, M.; Rahimi, K. Patterns and Temporal Trends of Comorbidity among Adult Patients with Incident Cardiovascular Disease in the UK between 2000 and 2014: A Population-Based Cohort Study. PLoS Med. 2018, 15, e1002513. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, K.; Lam, C.S.P.; Steinhubl, S. Cardiovascular Disease and Multimorbidity: A Call for Interdisciplinary Research and Personalized Cardiovascular Care. PLoS Med. 2018, 15, e1002545. [Google Scholar] [CrossRef]
- Désesquelles, A.; Salvatore, M.A.; Frova, L.; Pace, M.; Pappagallo, M.; Meslé, F.; Egidi, V. Revisiting the Mortality of France and Italy with the Multiple-Cause-of-Death Approach. Demogr. Res. 2010, 23, 771–806. [Google Scholar] [CrossRef]
- Désesquelles, A.; Demuru, E.; Pappagallo, M.; Frova, L.; Meslé, F.; Egidi, V. After the Epidemiologic Transition: A Reassessment of Mortality from Infectious Diseases among over-65s in France and Italy. Int. J. Public Heal. 2015, 60, 961–967. [Google Scholar] [CrossRef]
- Bishop, K.; Moreno-Betancur, M.; Balogun, S.; Eynstone-Hinkins, J.; Moran, L.; Rao, C.; Banks, E.; Korda, R.J.; Gourley, M.; Joshy, G. Quantifying Cause-Related Mortality in Australia, Incorporating Multiple Causes: Observed Patterns, Trends and Practical Considerations. Int. J. Epidemiology 2023, 52, 284–294. [Google Scholar] [CrossRef]
- Fedeli, U.; Schievano, E.; Avossa, F.; Pitter, G.; Amidei, C.B.; Grande, E.; Grippo, F. Different Approaches to the Analysis of Causes of Death during the COVID-19 Epidemic. Eur. Rev. Méd. Pharmacol. Sci. 2021, 25, 3610–3613. [Google Scholar] [CrossRef]
- Santo, A.H. Potencial Epidemiológico Da Utilização Das Causas Múltiplas de Morte Por Meio de Suas Menções Nas Declarações de Óbito, Brasil, 2003. Rev. Panam. Salud Pública 2007, 22, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Santo, A.H. Causas Mal Definidas de Morte e Óbitos Sem Assistência. Revista da Associação Médica Brasileira 2008, 54, 23–28. [Google Scholar] [CrossRef]
- Bishop, K.; Balogun, S.; Eynstone-Hinkins, J.; Moran, L.; Martin, M.; Banks, E.; Rao, C.; Joshy, G. Analysis of Multiple Causes of Death: A Review of Methods and Practices. Epidemiology 2023, 34, 333–344. [Google Scholar] [CrossRef]
- Désesquelles, A.F.; Salvatore, M.A.; Pappagallo, M.; Frova, L.; Pace, M.; Meslé, F.; Egidi, V. Analysing Multiple Causes of Death: Which Methods For Which Data? An Application to the Cancer-Related Mortality in France and Italy. Eur. J. Popul. Rev. Eur. Démographie 2012, 28, 467–498. [Google Scholar] [CrossRef]
- Frova, L.; Salvatore, M.A.; Pappagallo, M.; Egidi, V. The Multiple Cause of Death Approach to Analyse Mortality Patterns. Genus 2009, 1, 1–21. [Google Scholar]
- Santos, D.A.D.; Deutsch, R. The Positive Matching Index: A New Similarity Measure with Optimal Characteristics. Pattern Recognit. Lett. 2010, 31, 1570–1576. [Google Scholar] [CrossRef]
- Piffaretti, C.; Moreno-Betancur, M.; Lamarche-Vadel, A.; Rey, G. Quantifying Cause-Related Mortality by Weighting Multiple Causes of Death. Bull. World Heal. Organ. 2016, 94, 870–879. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Betancur, M.; Sadaoui, H.; Piffaretti, C.; Rey, G. Survival Analysis with Multiple Causes of Death. Epidemiology 2017, 28, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Ukolova, E.; Burcin, B. What Can Multiple Causes of Death Tell about Cardiovascular Mortality during COVID-19 Pandemic in the United States? J. Public Heal. 2024, 46, 97–106. [Google Scholar] [CrossRef]
- Grundy, E.M.; Stuchbury, R. Multimorbidity as Assessed by Reporting of Multiple Causes of Death: Variations by Period, Sociodemographic Characteristics and Place of Death among Older Decedents in England and Wales, 2001–2017. J. Epidemiology Community Heal. 2022, 76, 699–706. [Google Scholar] [CrossRef]
- Trias-Llimós, S.; Permanyer, I. Cause-of-Death Diversity From a Multiple-Cause Perspective in the United States. Demography 2023, 60, 73–98. [Google Scholar] [CrossRef]
- Breger, T.L.; Edwards, J.K.; Cole, S.R.; Saag, M.; Rebeiro, P.F.; Moore, R.D.; Eron, J.J. Estimating a Set of Mortality Risk Functions with Multiple Contributing Causes of Death. Epidemiology 2020, 31, 704–712. [Google Scholar] [CrossRef]
- Fihel, A.; Janicka, A.; Buschner, A.; Ustinavičienė, R.; Trakienė, A. Unrecognised COVID-19 Deaths in Central Europe: The Importance of Cause-of-Death Certification for the COVID-19 Burden Assessment. PLoS ONE 2024, 19, e0307194. [Google Scholar] [CrossRef]
- Fihel, A.; Muszyńska-Spielauer, M. Using Multiple Cause of Death Information to Eliminate Garbage Codes. Demogr. Res. 2021, 45, 345–360. [Google Scholar] [CrossRef]
- Wilkins, K.; Wysocki, M.; Morin, C.; Wood, P. Multiple Causes of Death. Health Reports 1997, 9, 19–29. [Google Scholar]
- Park, J.; Peters, P.A. Mortality from Diabetes Mellitus, 2004 to 2008: A Multiple-Cause-of-Death Analysis. Heal. Rep. 2014, 25, 12–16. [Google Scholar]
- Park, J. Mortality from Alzheimer’s Disease in Canada: A Multiple-Cause-of-Death Analysis Mortality from Alzheimer’s Disease in Canada: A Multiple-Cause-of-Death Analysis, 2004 to 2011; Statistics Canada; 2015; pp. 17–21.
- Statistics Canada Canadian Vital Statistics—Death Database (CVSD). Available online: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3233 (accessed on 23 September 2024).
- Speizer, F.E.; Trey, C.; Parker, P. The Uses of Multiple Causes of Death Data to Clarify Changing Patterns of Cirrhosis Mortality in Massachusetts. Am. J. Public Heal. 2011, 67, 333–336. [Google Scholar] [CrossRef]
- Creamer, A.W.; Barratt, S.L. Prognostic Factors in Chronic Hypersensitivity Pneumonitis. Eur. Respir. Rev. 2020, 29, 190167. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Bhattacharya, A.; Abhijit, R.D.; Chowdhury, S.R.; Chaudhury, K. Risk Factors Associated with Mortality in Hypersensitivity Pneumonitis: A Meta-Analysis. Expert Rev. Respir. Med. 2022, 16, 801–811. [Google Scholar] [CrossRef]
- Rittig, A.H.; Hilberg, O.; Ibsen, R.; Løkke, A. Incidence, Comorbidity and Survival Rate of Hypersensitivity Pneumonitis: A National Population-Based Study. ERJ Open Res. 2019, 5, 00259–02018. [Google Scholar] [CrossRef] [PubMed]
- Kolte, D.; Lakshmanan, S.; Jankowich, M.D.; Brittain, E.L.; Maron, B.A.; Choudhary, G. Mild Pulmonary Hypertension Is Associated with Increased Mortality: A Systematic Review and Meta-Analysis. J. Am. Hear. Assoc. 2018, 7, e009729. [Google Scholar] [CrossRef] [PubMed]
- Gardner, W.M.; Razo, C.; McHugh, T.A.; Hagins, H.; Vilchis-Tella, V.M.; Hennessy, C.; Taylor, H.J.; Perumal, N.; Fuller, K.; Cercy, K.M.; et al. Prevalence, Years Lived with Disability, and Trends in Anaemia Burden by Severity and Cause, 1990–2021: Findings from the Global Burden of Disease Study 2021. Lancet Haematol. 2023, 10, e713–e734. [Google Scholar] [CrossRef]
- Vlagopoulos, P.T.; Tighiouart, H.; Weiner, D.E.; Griffith, J.; Pettitt, D.; Salem, D.N.; Levey, A.S.; Sarnak, M.J. Anemia as a Risk Factor for Cardiovascular Disease and All-Cause Mortality in Diabetes: The Impact of Chronic Kidney Disease. J. Am. Soc. Nephrol. 2005, 16, 3403–3410. [Google Scholar] [CrossRef]
- Omran, A.R. The Epidemiologic Transition: A Theory of the Epidemiology of Population Change. Milbank Q. 2005, 83, 731–757. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, G.L.; Conn, L.A; Pinner, R.W. Trends in Infectious Disease Mortality in the United States during the 20th Century. Journal of the American Medical Association 1999, 281, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.N. International Handbook of Adult Mortality. Int. Handb. Popul. 2011, 467–489. [Google Scholar] [CrossRef]
- Kempker, J.A.; Kramer, M.R.; Waller, L.A.; Martin, G.S. Risk Factors for Septicemia Deaths and Disparities in a Longitudinal US Cohort. Open Forum Infect. Dis. 2018, 5, ofy305. [Google Scholar] [CrossRef]
- Janssen, T.A. Importance of Tabulating Multiple Causes of Death. American Journal of Public Health 1940, 5, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Dorn, H.F.; Moriyama, I.M. Uses and Significance of Multiple Cause Tabulations for Mortality Statistics. Am. J. Public Heal. Nations Heal. 1964, 54, 400–406. [Google Scholar] [CrossRef]
- Israel, R.L.; Rosenberg, H.M.; Curtin, L.R. Analytical Potential for Multiple Cause-of-Death Data. Am. J. Epidemiology 1986, 124, 161–179. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).