Introduction
The metabolic activity, diversity and composition of the gut microbiota vary significantly between healthy individuals and insomniacs [
1,
2], and also between hypersomniacs and healthy people [
3,
4]. While Clostridiales and Bacteroides are regarded to be the two most important biomarkers for differentiating between healthy people and insomniacs [
5], a recent study demonstrated that an enhanced relative abundance of five genera including Lachnospiraceae UCG010, Hungatella, Collinsella, Gordonibacter and Blautia may be correlated with a diminished risk of some types of hypersomnia (narcolepsy type one). Contrarily, an enhanced relative abundance of class Betaproteobacteria, genus Ruminiclostridium and genus Alloprevotella may potentially increase the risk of narcolepsy type one [
6].
Here, it worth mentioning a study conducted by Valles-Colomer and colleagues [
7]. They detected substantial bacterial strain sharing across people with distinct intra-population, mother-to-infant and intra-household transmission patterns. There was considerable strain sharing among cohabiting people, with 32% and 12% median strain-sharing rates for the time since cohabitation and gut and oral microbiomes affected strain sharing more than genetics or age did.
Based on these premises, we propose a hypothesis:
Person-to-person bacterial transmission can change the sleep pattern in couples
Patients and Methods Participants
Data were drawn from a private sleep clinic, Tehran, Iran. Respondents who had been officially married during the past six months and were in a cohabiting relationship were invited to participate in this study together with their official spouses. One hundred and eighty four heterosexual couples participated in the gut microbiota composition and sleep study. Six couples were excluded because the women were taking medicines known to affect gut/oral microbiota composition or were pregnant. One hundred and seventy eight participants provided stool samples, of which twenty-one were excluded due to either low readings (n = 10) or missing data (n = 11). The remaining 157 couples were all living with their spouses in a same house. At baseline interview, respondents and their spouses were telephoned on two consecutive days and interviewed separately about their daily experiences, including time use, physical symptoms, mood, and stressful events.
Sample Collection
Fecal samples were voluntarily collected from participants using the DNA/RNA Shield Fecal Collection Tubes (Zymo Research, Freiburg, Germany). Samples were then transferred to the laboratory and frozen within 15–30 min after collection. All samples were stored at − 80 ◦C until further processing. On Day 1 and Day 2, all couples participated in a gut microbiota composition study. Three months later gut microbiota composition was analyzed again with the same protocol. All the respondents participated in the study except one couple who were divorced from each other and had spent significant time living apart. Thirty-two couples were also excluded due to their baseline microbiota resemblance (either insomniac or hypersomniac phenotype) to avoid overlap bias. Data drawn form 152 couples were analyzed.
Sleep Study
The participants voluntarily completed the validated Persian versions of Pittsburgh Sleep Quality Inventory (PSQI), Epworth Sleepiness Scale (ESS), Insomnia Severity Index (ISI), and global sleep assessment questionnaire (GSAQ) [
8]. Insomnia was defined as coexistence of both daytime dysfunction and difficulty resuming sleep [
9]. Hypersomnia was defined by a bed-rest total sleep time ≥19 hour during the 32-hour recording [
10]. SPSS ver.16 was used to analyze the data.
Results
This is an interim result and the detailed results will be published in full in a peer-reviewed journal and will be disseminated. Men had an average age of 37.20 years, with a standard deviation (SD) of 8.01, and 84.3% had attained a college degree. Women had an average age of 31.02 years (SD = 9.30), and 87.2% had attained a college degree. All participants were Iranian (ethnicities including: 83 Persian, 69 Azeri, and 5 Arab). The couples had been married and living together for an average of 5.91 months (SD = 2.03).
Briefly, gut microbiota composition in participants with normal sleep pattern were significantly changed and becomes similar to that of participant’s spouse, i.e., if the spouse was insomniac or hypersomniac, then gut composition becomes similar to his/her insomniac or hypersomniac spouse, respectively. Interestingly, in support of our hypothesis, similar and parallel changes were observed in sleep pattern of subjects with normal sleep pattern. Women/men with a normal sleep pattern, who had married with a hypersomniac or insomniac spouse, reported a disturbance in their normal sleep pattern.
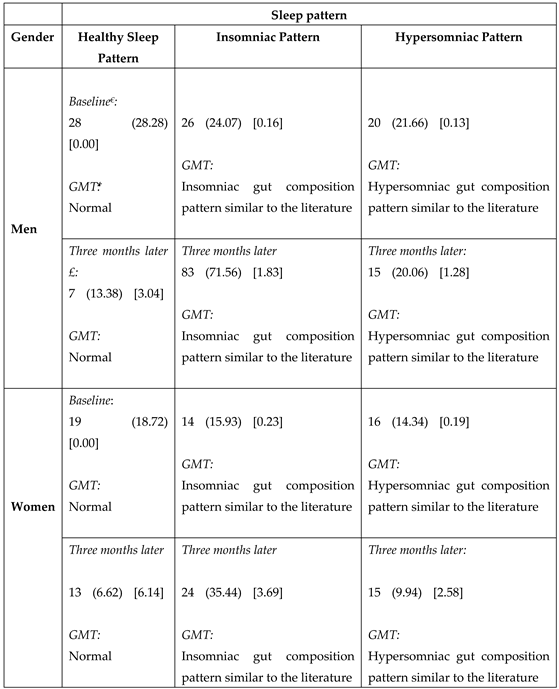
Table 1 demonstrates results of the chi square test. Statistical analyses with an array of sleep questionnaires including the PSQI, ESS, ISI and GSAQ confirmed the report. Results remained significant after controlling for confounders. The formal mediation analysis confirmed the results (data not shown due to editorial limits of the paper).
Three months after the marriage, spouses with healthy sleep pattern were significantly more likely to resemble their insomniac or hypersomniac couples.
Conclusion
We found that sleep disturbances in couples can be partially explained by changes in gut microbiota.
To the best of our knowledge this is the first paper that addresses association between microbiota and sleep disturbances in newly married couples.
Many types of physiologic synchrony have been reported between couples before, for instance, synchrony of diurnal cortisol pattern [
11], cardiac synchrony [
12] and also sleep concordance [
13], just to mention a few among many. To the best of author’s knowledge, this is the first study showing that sleep disturbances can be mediated via spouse’s gut microbiota transamination, particularly in such a short term, i.e., about almost 6 months after marriage. Previous studies have highlighted the substantial role of affective experience in regulation of sleep through behaviors such as touching, and “sleep-touch” among couples [
14]. Most definitely, socioeconomic status [
15], couples’ sleep and psychological distress [
16] can also significantly change the sleep pattern in couples. It is also known that anxiety can partially predict dyadic sleep characteristics in couples experiencing insomnia but not in couples without sleep disorders [
17]. There are obviously many other confounding factors at play in the pathophysiology of sleep disturbances. Note that this study is ongoing and further analysis will reveal the mechanism behind this novel and exciting finding. The research will have important implications in terms of diagnosis and treatment of sleep disturbances.
Ethical Consideration
All the participants were assured of confidentiality of their personal details and that the information obtained will be only used for research purposes and their profile will be kept confidential during the research and thereafter. We did this study in a private sleep clinic and all the participants expressed their informed consent to participate in the voluntarily research. Written informed consent was obtained from all study participants. Ethical approval was obtained from the Human Research Ethics Committee (IT. 24001670). We adhered to the tenets of the Declaration of Helsinki. As per the guidelines of the International Committee of Medical Journal Editors, registration is not necessary for studies whose sole purpose is to assess an intervention’s effect on providers. Furthermore, we did not have any intervention for our volunteer participants.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
- Wang, Z.; Wang, Z.; Lu, T.; Chen, W.; Yan, W.; Yuan, K.; Shi, L.; Liu, X.; Zhou, X.; Shi, J.; Vitiello, M. V.; Han, Y.; Lu, L. , The microbiota-gut-brain axis in sleep disorders. Sleep Med Rev 2022, 65, 101691. [Google Scholar] [CrossRef]
- Han, M.; Yuan, S.; Zhang, J. , The interplay between sleep and gut microbiota. Brain Res Bull 2022, 180, 131–146. [Google Scholar] [CrossRef]
- Jezkova, J.; Sonka, K.; Kreisinger, J.; Prochazkova, P.; Tlaskalova-Hogenova, H.; Nevsimalova, S.; Buskova, J.; Merkova, R.; Dvorakova, T.; Prihodova, I.; Dostalova, S.; Roubalova, R. , Guardians of Rest? Investigating the gut microbiota in central hypersomnolence disorders. Sleep Med 2024, 113, 95–102. [Google Scholar] [CrossRef]
- Busch, A.; Roy, S.; Helbing, D. L.; Colic, L.; Opel, N.; Besteher, B.; Walter, M.; Bauer, M.; Refisch, A. , Gut microbiome in atypical depression. J Affect Disord 2024, 349, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Rakoff-Nahoum, S.; Foster, K. R.; Comstock, L. E. , The evolution of cooperation within the gut microbiota. Nature 2016, 533(7602), 255–9. [Google Scholar] [CrossRef] [PubMed]
- Sheng, D.; Li, P.; Xiao, Z.; Li, X.; Liu, J.; Xiao, B.; Liu, W.; Zhou, L. , Identification of bidirectional causal links between gut microbiota and narcolepsy type 1 using Mendelian randomization. Sleep 2024, 47(3). [Google Scholar] [CrossRef] [PubMed]
- Valles-Colomer, M.; Blanco-Miguez, A.; Manghi, P.; Asnicar, F.; Dubois, L.; Golzato, D.; Armanini, F.; Cumbo, F.; Huang, K. D.; Manara, S.; Masetti, G.; Pinto, F.; Piperni, E.; Puncochar, M.; Ricci, L.; Zolfo, M.; Farrant, O.; Goncalves, A.; Selma-Royo, M.; Binetti, A. G.; Becerra, J. E.; Han, B.; Lusingu, J.; Amuasi, J.; Amoroso, L.; Visconti, A.; Steves, C. M.; Falchi, M.; Filosi, M.; Tett, A.; Last, A.; Xu, Q.; Qin, N.; Qin, H.; May, J.; Eibach, D.; Corrias, M. V.; Ponzoni, M.; Pasolli, E.; Spector, T. D.; Domenici, E.; Collado, M. C.; Segata, N. , The person-to-person transmission landscape of the gut and oral microbiomes. Nature 2023, 614(7946), 125–135. [Google Scholar] [CrossRef] [PubMed]
- Chehri, A.; Goldaste, N.; Ahmadi, S.; Khazaie, H.; Jalali, A. , Psychometric properties of insomnia severity index in Iranian adolescents. Sleep Sci 2021, 14(2), 101–106. [Google Scholar] [PubMed]
- Itani, O.; Kaneita, Y.; Munezawa, T.; Mishima, K.; Jike, M.; Nakagome, S.; Tokiya, M.; Ohida, T. , Nationwide epidemiological study of insomnia in Japan. Sleep Medicine 2016, 25, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, E.; Lopez, R.; Barateau, L.; Chenini, S.; Bosco, A.; Jaussent, I.; Dauvilliers, Y. , Alternative diagnostic criteria for idiopathic hypersomnia: a 32-hour protocol. Annals of neurology 2018, 83(2), 235–247. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Rovine, M. J.; Cousino Klein, L.; Almeida, D. M. , Synchrony of diurnal cortisol pattern in couples. Journal of Family Psychology 2013, 27(4), 579. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, J.; Pereira, A.; Oliveira-Silva, P.; Meier, D.; Lourenço, V.; Tschacher, W. , When our hearts beat together: Cardiac synchrony as an entry point to understand dyadic co-regulation in couples. Psychophysiology 2021, 58(3), e13739. [Google Scholar] [CrossRef] [PubMed]
- Gunn, H. E.; Buysse, D. J.; Hasler, B. P.; Begley, A.; Troxel, W. M. , Sleep concordance in couples is associated with relationship characteristics. Sleep 2015, 38(6), 933–939. [Google Scholar] [CrossRef] [PubMed]
- Roberts, N. A.; Burleson, M. H.; Pituch, K.; Flores, M.; Woodward, C.; Shahid, S.; Todd, M.; Davis, M. C. , Affective Experience and Regulation via Sleep, Touch, and “Sleep-Touch” Among Couples. Affect Sci 2022, 3(2), 353–369. [Google Scholar] [CrossRef] [PubMed]
- Saini, E. K.; Keiley, M. K.; Fuller-Rowell, T. E.; Duke, A. M.; El-Sheikh, M. , Socioeconomic Status and Sleep among Couples. Behav Sleep Med 2021, 19(2), 159–177. [Google Scholar] [CrossRef] [PubMed]
- Chen, J. H. , Couples’ Sleep and Psychological Distress: A Dyadic Perspective. J Gerontol B Psychol Sci Soc Sci 2017, 73(1), 30–39. [Google Scholar] [CrossRef] [PubMed]
- Walters, E. M.; Phillips, A. J.; Hamill, K.; Norton, P. J.; Drummond, S. P. , Anxiety predicts dyadic sleep characteristics in couples experiencing insomnia but not in couples without sleep disorders. Journal of Affective Disorders 2020, 273, 122–130. [Google Scholar] [CrossRef] [PubMed]
Table 1.
Distribution of study participants according to gender, gut microbiota composition and sleep pattern.
Table 1.
Distribution of study participants according to gender, gut microbiota composition and sleep pattern.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).