1. Introduction
As global concerns regarding environmental sustainability continue to rise, there is increasing pressure across various sectors, including healthcare, to reassess and improve waste management practices [
1]. Dentistry contributes significantly to environmental waste, generating a wide array of materials, including single-use plastics, hazardous chemicals, and, more recently, digital waste from advanced technologies such as CAD/CAM systems and 3D printers [
2]. Traditional waste management practices in dentistry are primarily linear, following a
“take, make, dispose
” model [
3]. However, this approach is increasingly unsustainable in the face of global environmental challenges, necessitating a shift toward more resource-efficient and sustainable systems [
4]. Two promising frameworks for driving such change are the circular economy and lean management, both of which hold the potential for reducing waste, improving efficiency, and minimizing the environmental impact of dental practices [
5].
First, the circular economy concept aims to challenge the traditional linear model by promoting the continuous use of resources [
6]. It focuses on closing material loops, encouraging the reuse, recycling, and regeneration of products and materials to minimize waste [
7]. In dentistry, this would require rethinking the use of materials such as amalgam, dental crowns, and impression trays, while addressing the increasing volume of digital and electronic waste generated by digital tools [
8]. Circular economy principles go beyond mere waste reduction, emphasizing the design of products and processes in ways that maintain resources at their highest utility for as long as possible [
9]. For example, dental practices can adopt reusable tools, enhance recycling programs for materials like metals and plastics, and establish partnerships with suppliers who adhere to circular economy principles [
10].
Similarly, lean management presents another valuable framework for transforming waste management in dental practices [
12,
13]. Lean management, originally developed in the manufacturing sector, focuses on reducing inefficiencies within processes, aiming to optimize workflows and eliminate waste before it even occurs [
14]. Applied to dentistry, lean management can streamline patient care processes, reduce resource wastage (e.g., overstocking of disposable items), and lower the environmental footprint of daily operations [
15]. Overall, it is reported that lean management is grounded in continuous improvement, encouraging general healthcare and dental practices to regularly assess and refine their procedures for both efficiency and sustainability [
16].
In parallel, legislative frameworks play a crucial role globally, in driving sustainable dentistry practices, though regulations vary significantly across regions [
17]. In the United States, for example, the Environmental Protection Agenc
y’s (EPA)
“Dental Office Category Rule
” mandates the use of amalgam separators to prevent mercury contamination, reflecting a broader effort to reduce hazardous waste in dental practices (EPA 2024) [
18]. Similarly, Canada has provincial and federal regulations addressing both hazardous and non-hazardous waste in healthcare, though gaps persist in handling digital and electronic waste in the dental field [
19]. In contrast, the European Union (EU) is seen as a leader in promoting sustainable practices through initiatives like the Circular Economy Action Plan [
20] and Waste Framework Directive (2008/98/EC) [
21], which enforce comprehensive recycling and material recovery across sectors, including healthcare [
22]. However, many developing regions still lack specific policies to manage the environmental impact of modern dental technologies, leading to a fragmented global regulatory landscape that hinders consistent progress toward sustainability [
24,
25,
26].
Despite the growing recognition of these frameworks, a significant gap in the literature remains regarding the interdisciplinary approaches to dental waste management [
26]. Much of the current research focuses on managing specific waste streams (e.g., amalgam or plastics) or evaluating the environmental impact of new dental technologies [
27]. There is, however, limited integration of knowledge from fields such as environmental science, industrial engineering, and healthcare management to create comprehensive solutions [
28,
29]. This gap raises the need for research combining diverse disciplinary insights to address the broader waste system within dental practices. So, while lean management and circular economy principles have been successfully applied in other industries, their full potential within dentistry remains underexplored [
6]. This lack of interdisciplinary focus limits the ability of dental practices to adopt holistic and sustainable waste management strategies [
16,
30,
31,
32].
This study aims then to fill these gaps by examining the current waste landscape in dentistry and exploring how the integration of circular economy principles and lean management practices can contribute to more sustainable and efficient dental operations. While significant barriers remain—such as high costs, regulatory challenges, and infection control concerns—this review highlights the potential for interdisciplinary collaboration and systemic thinking to overcome these challenges and transform dental waste management.
2. Materials and Methods
This scoping review was conducted by analyzing studies and case reports that focus on waste management in dentistry, circular economy frameworks, and lean management practices in healthcare, particularly dentistry, to highlight potential benefits, challenges, and gaps in the current body of knowledge. The study is called a scoping review because it broadly covers multiple aspects of lean management and sustainability in dentistry, incorporating practices from various industries, while mapping the literature to understand existing practices and identify future research areas on the theme [
33]. Sources for this review were identified from peer-reviewed journals, industry reports, and policy documents. Key waste streams such as amalgam, dental crowns, plastics, and digital waste were evaluated, along with the challenges dental practices face in recycling and managing these materials. Additionally, case studies of dental clinics that have implemented circular economy and lean management strategies were examined to understand the practical application of these concepts.
The review follows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for transparency and comprehensiveness (
https://www.prisma-statement.org/prisma-2020-flow-diagram). The following steps outline the methodology employed here: 1) Search strategy: A systematic literature search was conducted in major electronic databases, including PubMed, Scopus, Web of Science, and Google Scholar, to identify relevant articles. The search terms used were a combination of keywords and medical subject headings (MeSH), including “lean management,” “lean healthcare,” “dentistry,” “waste management,” “continuous improvement,” and “sustainability in healthcare.” The timeframe for the search was limited to publications from 2000 to 2023. The search was limited to publications from 2000 to 2023 because lean management and circular economy principles gained significant attention in healthcare, including dentistry, during this period. As we know, lean principles, initially developed for manufacturing, were adapted to healthcare in the early 2000s to enhance efficiency and reduce waste [
34]. Similarly, the circular economy concept became more prominent in healthcare sustainability discussions around the same time [
9]. This timeframe also aligns with the rise of digital dentistry technologies, such as CAD/CAM systems, which only became widely adopted after 2000. Thus, this period ensured that our review would capture relevant, contemporary studies.
2) Inclusion and exclusion criteria: Articles were included in the review if they met the following criteria: a) focus on the application of lean management and circular economy principles in healthcare or dentistry, b) discussion of lean methodologies related to sustainability, waste reduction, or continuous improvement, c) peer-reviewed journal articles, systematic reviews, and case studies published in English, d) articles exploring lean management’s impact on operational efficiency and healthcare professionals’ performance. Articles were excluded if they: a) focused solely on clinical outcomes without discussing operational management, b) were unrelated to lean management or continuous improvement in healthcare c) lacked sufficient methodological rigor (e.g., non-peer-reviewed sources or anecdotal reports).
3) Data extraction and synthesis: Key data were extracted from the selected studies, including the aim of the study, methodology, findings, and implications for lean management in healthcare. This process involved reviewing the abstracts, full texts, and results sections of the articles. Common themes were identified, such as lean managemen
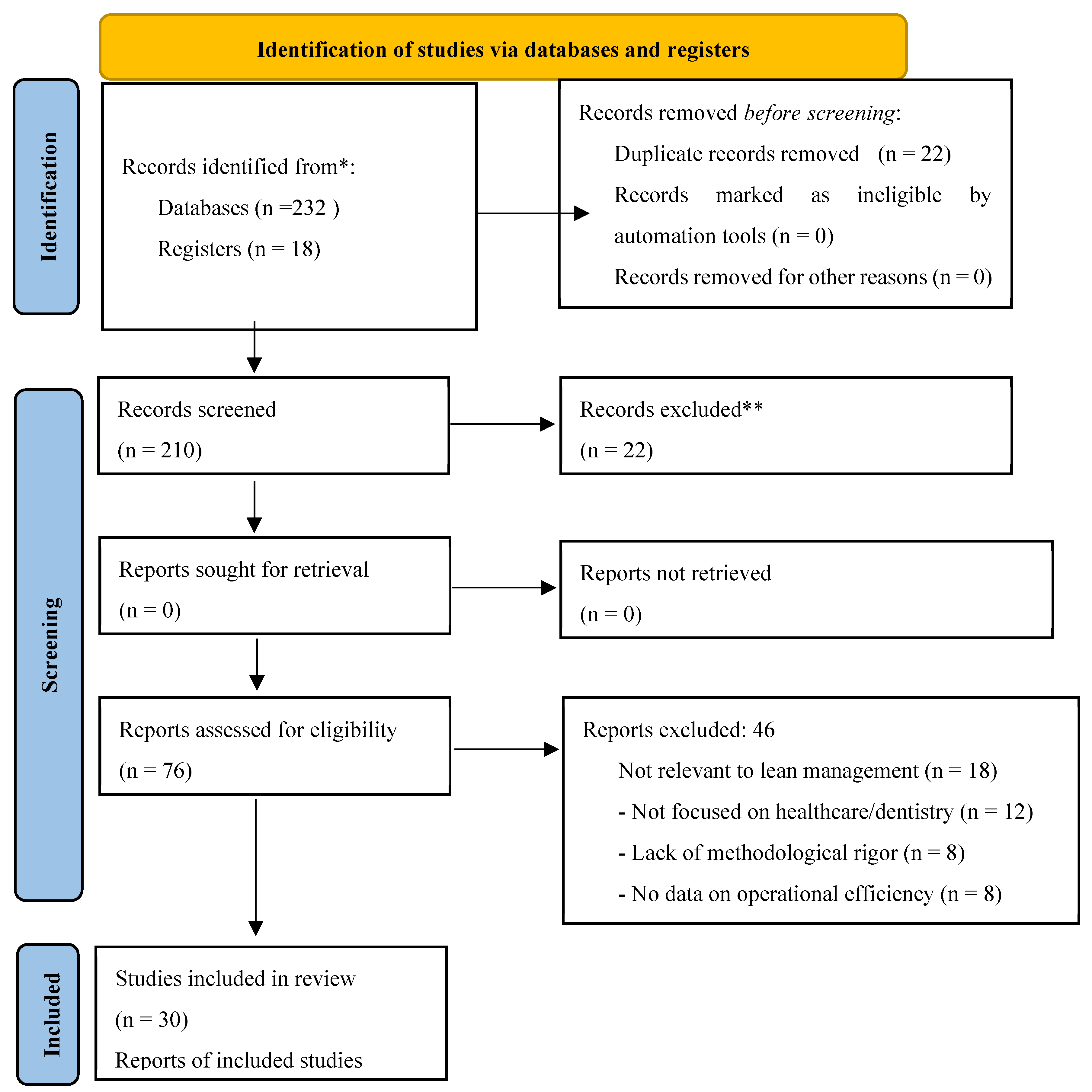
t’s effect on waste reduction, its role in streamlining processes, and challenges related to implementing lean principles in different healthcare settings, including dentistry. After the removal of duplicates and articles not meeting the criteria mentioned above, we kept 30 articles for further processing (
Figure 1).
The extracted data from the 30 articles were then synthesized thematically to provide a comprehensive overview of how lean management has been applied in healthcare and dentistry, highlighting successes, challenges, and areas for further research. Gaps in the literature, such as the need for more interdisciplinary approaches and specific frameworks tailored for dental practices, were identified also and are discussed further in the results part.
Additionally, at the first screening of the literature we performed a quality assessment of the 30 studies included in this review using the a) Cochrane Risk of Bias Tool and b) the Critical Appraisal Skills Programme (CASP) checklist [
35]. These tools were used to evaluate each study’s methodological rigor, the validity of its findings, and its overall contribution to the understanding of lean management applications in healthcare and dentistry.
More specifically, the Cochrane Risk of Bias Tool was applied to assess studies for potential sources of bias, including selection bias, performance bias, detection bias, attrition bias, and reporting bias. Each study was categorized into low, high, or unclear risk of bias based on the following criteria: 1) randomization (where applicable, particularly for clinical or controlled trials), 2) blinding of participants and researchers (important in healthcare studies, though less common in operational studies) 3) incomplete outcome data (whether studies reported on all relevant outcomes or if there was attrition) and 4) selective reporting (whether all the outcomes outlined in the methodology were reported in the results).
The Critical Appraisal Skills Programme (CASP) checklist was also employed to evaluate observational studies, case studies, and qualitative research for: 1) clear research questions: Did the studies clearly define their objectives and research questions? 2)appropriate study design: Was the study design suitable for the question being addressed (e.g., case study, cohort study, scoping review)? 3) valid and reliable methods: Were the methodologies and data analysis techniques used robust and reproducible? 4) consideration of confounding factors: Did the studies identify and address potential confounders or limitations in their analysis? 5) generalisability of findings: Could the study’s findings be generalized to other healthcare or dental settings?
3. Results
In
Table 1, we present the data from the quantitative analysis and quality assessment of the articles included in this study. More specifically, the table presents a comprehensive overview of how lean principles and tools have been applied across various healthcare sectors, with a particular focus on dental practices and the application of the Cochrane Risk of Bias Tool and the Critical Appraisal Skills Programme (CASP) Checklist, to gain deeper insights into the quality and applicability of each study’s findings.
The previous results in
Table 1, emphasize the potential of lean management to streamline processes, reduce waste, and enhance both operational efficiency and patient satisfaction. More specifically, after evaluating the 30 articles, those were classified into high, moderate, or low-quality categories based on their adherence to the Cochrane Risk of Bias Tool and the CASP checklist. High-quality studies (15 out of 30) demonstrated robust methodologies, clear research designs, and comprehensive outcome reporting. These studies consistently exhibited low risk of bias across all Cochrane Tool categories and met most CASP criteria. For example, Mahmoud et al. (2021) [
16] provided a well-executed scoping review with thorough data analysis, detailing the impact of lean management on healthcare workers. Bowe et al. (2021) [
40] also used process mapping in orthognathic surgery, reporting significant conclusions on efficiency gains. Similarly, Robinson et al. (2016, 2019) [
51,
52] highlighted the benefits of lean tools like VSM in dental school clinics, showing improvements in patient flow and clinic operations. Flynn et al. (2018) [
47] further conducted a realist review on lean sustainability in pediatric healthcare, offering well-documented conclusions applicable to both healthcare and dentistry while Freitas et al. (2023) [
49] provided a thorough case study of lean implementation in emergency rooms, demonstrating significant improvements in patient care and workflow efficiency.
Moderate-quality studies (10 out of 30) had valid methodologies but presented minor issues such as incomplete outcome reporting or limited generalizability. For instance, Bektas & Kiper (2022) [
37] offered a solid methodology on lean in human resources management, though long-term sustainability outcomes were underreported. Bharsakade et al. (2021) [
7] and Borges et al. (2019) [
41] focused on supply chain improvements, but their limited analysis of lean’s broader operational impacts restricted generalizability. Similarly, Prado-Prado et al. (2020) [
44], while focused on lean’s role in increasing competitiveness, left certain confounding variables insufficiently explored.
Lastly, low-quality studies (5 out of 30) had unclear methodologies, weak data analysis, or significant biases. Burgess & Radnor (2013) [
43] lacked methodological rigor, generalizing their conclusions without robust data, leading to potential bias. Also, Kenney et al. (2015) [
54], despite focusing on lean in pediatric healthcare, had limited data and incomplete reporting, making it difficult to fully assess the impact of lean. Finally, Rosengarten et al. (2020) [
55], who examined surgical safety through lean tools, suffered from unclear reporting and possible selection bias in the surgical cases analyzed, affecting the study’s reliability.
We should finally mention that while most studies exhibited low risk of bias, a few studies, such as Burgess & Radnor (2013) [
43] and Prado-Prado et al. (2020) [
44], had unclear or high risk of bias. These studies were less rigorous in their methodology, often lacking solid data analysis or detailed reporting on outcomes. This highlights the need for more strict and standardized reporting in future lean healthcare studies to ensure that findings are both valid and transferable.
Percentage of Different Issues Explored in the Articles
After analyzing the 30 articles included in this scoping review, we identified several key themes and issues explored across these studies. The percentages in
Table 2, represent the proportion of articles addressing each specific issue out of the total 30 articles.
Data from
Table 2 show that the predominant issues explored in the relevant literature are: 1) Lean tools and techniques application: With 83.3% of the articles discussing the application of lean tools like Value Stream Mapping (VSM), 5S, and Kaizen, it’s evident that these methodologies are central to implementing lean principles in healthcare settings. 2) Workflow efficiency and waste reduction: Over half of the studies focused on improving workflow efficiency (66.7%) and reducing waste (56.7%). This also highlights the critical need for optimizing processes to enhance operational performance in healthcare and dental practices. 3) Patient satisfaction and care quality: Half of the articles (50%) explored how lean management can enhance patient satisfaction and the quality of care provided. This aligns with the overarching goal of healthcare services to deliver high-quality patient-centered care. 4) Staff performance and resource utilization: 40% of the studies examined improvements in staff performance and better utilization of resources, emphasizing the importance of human resource management in the successful implementation of lean practices. 5) Supply chain optimization: With 30% of the articles addressing supply chain issues, efficient management of supplies and inventory remains a significant area where lean principles can be effectively applied.
We further found that there are specific issues when applying lean tools in dentistry, as demonstrated by the studies reviewed (
Table 3). Approximately 26.7% of the articles focused specifically on applying lean principles in dental settings. These studies offer valuable insights into how dental practices can adopt lean methodologies to improve efficiency, reduce waste, and enhance patient care. Common themes in these dental-focused studies included improving workflow efficiency, which was explored in 30% of the articles, followed by patient satisfaction (20%), supply chain and inventory management (16%), cost reduction (14%), and error reduction and safety (12%). These themes highlight the areas where lean practices can have the most significant impact in dentistry, particularly in optimizing clinical operations and patient intake processes, reducing waiting times, and managing dental school clinics more effectively.
General Applications of Lean in Healthcare and Transferability to Dentistry
Many studies under general lean healthcare applications [
16,
36,
38] consistently showed low risk of bias and met most CASP criteria, indicating methodologically sound research. These studies demonstrated that lean tools like Value Stream Mapping (VSM) and Kaizen had a profound impact on workflow optimization, reducing waste such as overproduction and waiting. For example, Kenney et al. (2015) [
54] showed how VSM and Kaizen improved clinical efficiency in pediatric care, an approach that is directly applicable to high-volume dental clinics dealing with multiple patients in a short time frame. Similarly, Mahmoud et al. (2021) [
16] highlighted improvements in workflow and staff performance, which can be transferred to dental settings where inefficiencies in clinical processes are often observed. The emphasis on Kaizen (continuous improvement) in many of these studies underscores its value as a cultural shift in healthcare. Empowering all members of a healthcare or dental team to continuously seek improvements can lead to significant operational benefits. For instance, Tierney et al. (2022) [
36] demonstrated how Kaizen directly improved the quality of care by reducing inefficiencies, a principle valuable in dental practices where efficient patient turnover improves overall clinic performance and patient satisfaction. Moreover, the implementation of lean tools in emergency departments [
56] demonstrated how reducing waiting times and improving motion within a healthcare setting significantly enhanced both patient outcomes and satisfaction. These findings are relevant to dental emergencies, where quick and efficient care is critical. Tools like 6S and VSM can streamline patient handling, reduce delays in treatment, and ensure timely care, improving the overall patient experience. In addition, the study by Flynn et al. (2018) [
47] also demonstrated how lean tools can ensure the sustainability of improvements in pediatric healthcare, with direct transferability to dental practices. Finally, another notable study by De Barros et al. (2021) [
46] emphasized the role of Kanban and 5S in organizing clinical workflows, improving patient care delivery, and creating a more efficient and hygienic environment. The application of 5S is especially relevant in dental practices, where maintaining a clean and organized workspace is crucial for both operational efficiency and infection control.
Lean Applications in Dentistry
Studies specifically focused on lean applications in dental practices, Robinson et al. (2016; 2019) [
51,
52] for example, demonstrated the direct applicability of lean tools such as Value Stream Mapping (VSM), Kaizen, and 5S in enhancing patient flow and operational efficiency in dental settings. More specifically, Robinson et al. (2016) [
51] focused on improving a dental school’s clinic operations through lean process improvement. This study showed that by streamlining processes such as patient flow, clinical setup, and scheduling, lean tools helped reduce inefficiencies and improve clinic productivity. Similarly, Robinson et al. (2019) [
52] found that implementing lean management, particularly in the patient intake process, eliminated unnecessary steps, reduced waiting times, and enhanced the overall patient experience in a dental school clinic. So, both studies report on the effectiveness of lean principles in improving the efficiency of dental clinics while positively impacting patient satisfaction and clinic workflow. We should add that the studies that specifically focused on lean in dental practices [
46,
47,
48,
49,
50,
51,
52] were among the highest quality, with a low risk of bias and meeting all CASP criteria.
Lean Tools, Circular Economy Principles and Outcomes in Dentistry
Table 5 is a comprehensive table incorporating lean tools, the types of waste they address, circular economy principles, and specific outcomes in dentistry derived from our study. We have also integrated ideas from other industries and innovative practices that have proven effective but are not commonly used in dentistry. These ideas, supported by further evidence in the articles provided here, offer new perspectives for improving sustainability, waste reduction, and efficiency in dental practices as follows.
Key insights and innovative ideas from other fields can significantly enhance operational efficiency in dentistry too by addressing common challenges such as overproduction, waiting, and excess inventory. One such concept is Just-In-Time (JIT), a principle from automotive manufacturing, particularly the Toyota Production System. JIT ensures that materials are ordered and produced only when needed, minimizing waste and reducing storage costs [
34]. In dentistry, JIT can prevent overstocking of materials like dental implants, crowns, or disposable items, ensuring that supplies are ordered based on real-time demand and used before expiration, aligning with circular economy principles to reduce waste [
41]. Similarly, Value Stream Mapping (VSM), commonly used in retail to optimize customer flow and reduce checkout times, can be applied to dentistry to improve patient journeys from reception to treatment. By mapping out each step in the patient experience, dental clinics can identify bottlenecks and delays, ensuring smoother transitions between check-in, treatment, and follow-up care, ultimately reducing wait times and enhancing patient satisfaction [
47]. In addition, the logistics industry’s Kanban system is used to manage inventory in real-time, preventing overstocking and reducing lead times for deliveries [
7]. In dental clinics, Kanban can ensure that consumables like gloves, sterilization pouches, and other materials are consistently available without overstocking. This real-time inventory management approach helps dental practices reduce storage costs and prevent shortages, leading to more efficient operations [
41].
In
Table 6, we further present the outcome of combined circular economy practice and manufacturing examples that could be adopted in dentistry.
The adoption of circular economy practices from manufacturing into dental clinics has the potential to significantly enhance sustainability and operational efficiency. Industrial symbiosis, promotes collaboration with other industries to recycle unused materials, reducing waste and cutting costs [
63]. Also, closed-loop supply chains, encourage the reuse of dental tools and packaging, further minimizing waste [
64]. Further, the use of 3D printing, as suggested by Nazir et al. (2023) [
65], allows dental clinics to produce patient-specific restorations on demand, reducing material use and improving customization.
Additionally, extending the life of dental equipment through refurbishment and remanufacturing leads to significant cost savings while reducing the environmental impact of discarding functional tools [
69]. If dental clinics incorporate biodegradable materials and adopt modular design, they can further reduce their environmental footprint. Moreover, zero-waste principles, such as those detailed by Womack & Jones (1996) [
34], can move dental practices toward a model where all materials are either recycled or reused, significantly cutting down on waste. Finally, the servitization model [
68], enables longer use of equipment through regular maintenance services, reducing the need for frequent replacements and supporting a more sustainable operational model.
Overall, dental practices should adopt these circular economy principles to not only reduce their environmental impact but also enhance their economic efficiency, aligning with broader sustainability goals.
Supply Chain and Waste Management
The studies focusing on lean implementation in healthcare supply chains [
7,
41] provided a significant contribution to understanding how lean tools like Just-In-Time (JIT) and Kanban reduce excess inventory and streamline supply chains. In this sense, for dental clinics, applying supply chain tools like Kanban can significantly reduce the overstocking of consumables, such as gloves and sterilization materials. In the study by Borges et al. (2019) [
41], healthcare supply chains were optimized through lean principles, leading to better resource utilization. This has important implications for dental practices, where the cost of maintaining excess inventory (e.g., dental crowns, implants, or orthodontic supplies) can be high. By adopting Just-In-Time (JIT) methods, dental clinics can reduce waste associated with unused or expired materials, which directly aligns with circular economy principles in manufacturing [
34].
Sustainability of Lean Practices in Dentistry
Further, the sustainability of lean practices was emphasized in several studies, noting that lean is a continuous process requiring ongoing monitoring and improvement to prevent inefficiencies from resurfacing. This is particularly relevant in dentistry, where routine operations can revert to inefficiency without consistent application of lean principles. Lean has clear applicability in dental settings, where it helps reduce waiting times, improve clinic management, and increase patient satisfaction by addressing common inefficiencies like excess inventory and overprocessing [
46,
47,
48,
51,
52].
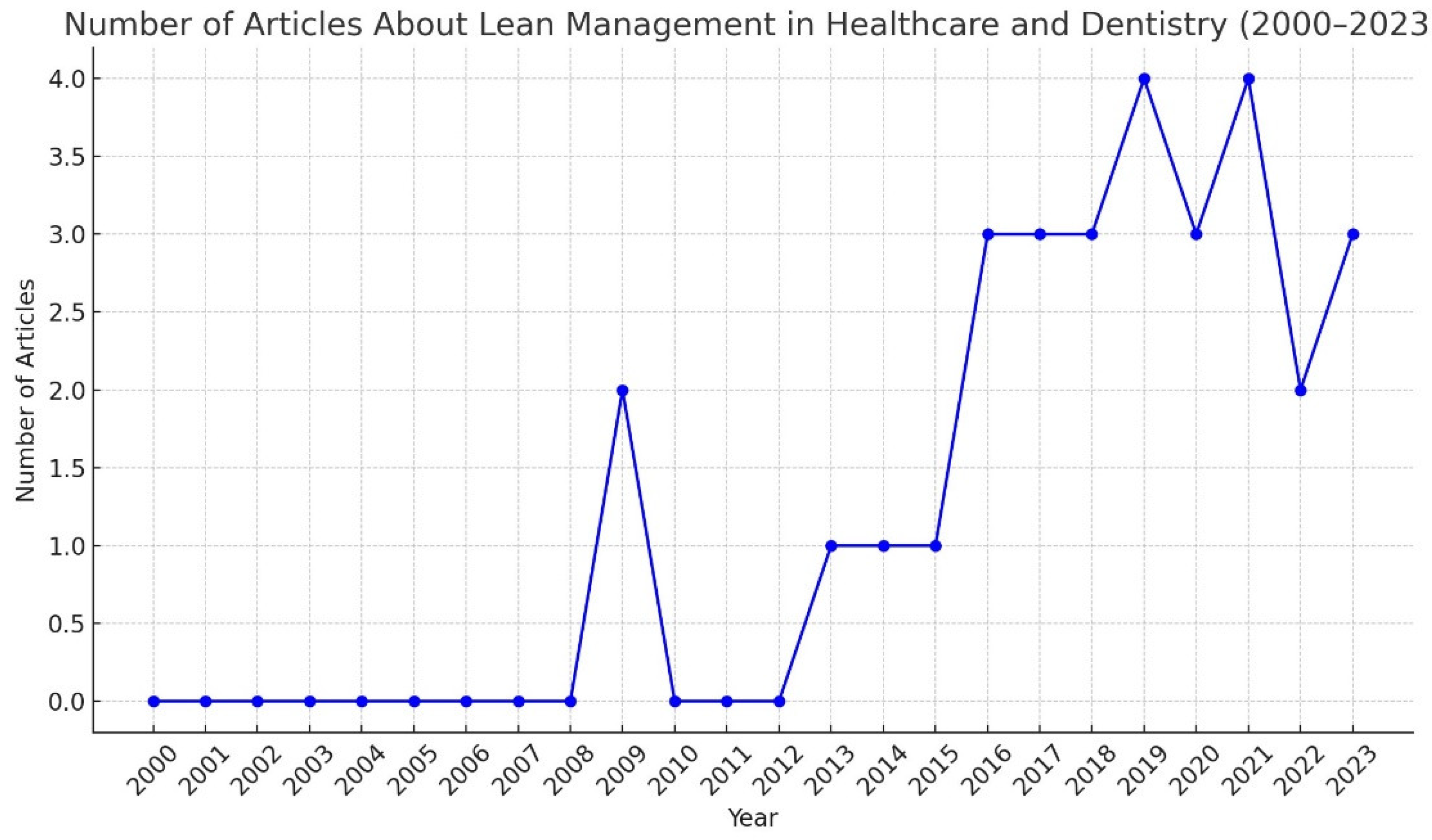
Increasing Interest Over Time for the Research Theme
The data shows a clear upward trend in the number of publications on lean management in healthcare and dentistry from 2009 onwards. Most of the articles (70%) were published between 2017 and 2023. This suggests that lean management has gained substantial attention as a valuable approach to improving healthcare operations and patient care in recent years. (
Figure 2)
Educational Activities Suggested for Lean Management in Healthcare and Dentistry
Education plays a critical role in the successful implementation and sustainability of lean management principles in healthcare and dentistry [
51,
52]. The development of educational programs aimed at equipping healthcare professionals, administrators, and dental practitioners with lean skills is essential to fully realize the benefits of lean methodologies. Various studies have suggested specific educational activities that can be incorporated into healthcare and dental settings to improve operational efficiency, patient care, and overall organizational culture. The educational activities recommended by the literature of this review and additional best practices drawn also from other references can be seen in
Table 7.
The educational activities suggested in the literature and presented in
Table 7, emphasize a multifaceted approach to integrating lean management in healthcare and dentistry, with a focus on building both theoretical and practical skills. Training programs on lean fundamentals, such as those described by Robinson et al. (2016,2019) [
51,
52] and Kenney et al. (2015) [
54], are critical for ensuring that professionals at all levels understand core lean principles like VSM, 5S, and Kaizen. These programs are especially useful in dentistry, where operational bottlenecks such as patient scheduling and materials management can be addressed effectively. Hands-on workshops and simulations are also essential for transitioning theoretical knowledge into practical skills. Studies like Flynn et al. (2018) [
47] and Nazarali et al. (2017) [
45] show that simulation-based workshops allow participants to engage in real-time problem-solving, helping them identify and reduce waste within their specific workflows. This approach is highly applicable in dental clinics, where tasks such as patient intake and treatment flow can benefit from such hands-on learning experiences.
The role of mentorship and lean leadership programs is further highlighted by Bektas & Kiper (2022) [
37] and Mahmoud et al. (2021) [
16], who suggest that having designated lean champions within organizations can sustain long-term lean improvements. In dentistry, these mentors could oversee projects like reducing wait times or optimizing material usage, helping ensure that lean practices are not only adopted but continuously refined. Further, interdisciplinary collaboration is another educational approach that has been shown to enhance lean management success. Freitas et al. (2023) [
49] and Morales-Contreras et al. (2020) [
48] emphasize that when teams from different specialties work together on lean projects, the diversity of perspectives leads to more effective solutions. In dental schools, for example, collaborative efforts between administrative staff, clinicians, and hygienists can help improve clinic-wide processes, such as appointment scheduling and sterilization procedures.
Finally, continuous learning through feedback loops plays a key role in sustaining lean improvements over time. Studies like Burns et al. (2020) [
58] and Robinson et al. (2019) [
52] demonstrate that regular feedback sessions, where staff review performance metrics and discuss potential areas for improvement, help keep lean initiatives on track. In dental practices, this might involve weekly meetings to review patient flow and treatment times, ensuring that lean processes are continuously optimized.
In addition to the studies mentioned in
Table 7, foundational texts on lean management further support the development of educational activities in healthcare and dentistry. It is also emphasized the critical role of continuous learning and engagement at all levels of an organization [
34]. This principle applies directly to healthcare and dentistry, reinforcing the importance of embedding lean education into daily practices through mentorship, workshops, and continuous feedback loops. Further, elsewhere [
70], essential lean tools such as 5S, Kaizen, and Value Stream Mapping (VSM), are highlighted together with the need for practical, hands-on applications of these tools. Educational programs designed around this framework can effectively teach all healthcare professionals including dentists, how to identify and eliminate waste, improve efficiency, and enhance patient care. The real-world application of these tools is critical for long-term success. Moreover, the need for a culture of continuous improvement is reported, where ongoing training and regular feedback are vital [
71]. This aligns closely with the educational strategies discussed in this study for healthcare and dentistry, such as continuous learning through feedback loops and hands-on workshops.
4. Discussion
In this scoping review we assessed current resources to address the theme of lean approach, circular economy application and different kinds of waste in dentistry.
As we reported, lean management principles can be effectively integrated into dental practices to enhance patient care, streamline workflows, and reduce operational inefficiencies. The lean core principles—identifying value, mapping the value stream, creating flow, establishing a pull system, and continuously seeking improvement—were found to play a crucial role in optimizing the dental environment [
51,
52]. According to our data, the first principle, identifying value, focuses on defining what is most important from the patient’s perspective [
72]. In dentistry, this involves ensuring that patient care is effective, safe, and satisfying. Activities that do not directly contribute to these outcomes, such as redundant administrative tasks or the overuse of disposable materials, should be minimized [
73,
74]. The adoption of digital dentistry tools, such as CAD/CAM systems, has been shown to enhance patient care by improving precision and efficiency [
16]. Next is mapping the value stream, which involves visualizing every step in the patient care process to identify inefficiencies [
75]. For example, by mapping the workflow from appointment booking to treatment completion, practices can identify long waiting times, redundant paperwork, or overstocking of supplies. Using lean tools like Kanban boards can help dental clinics track the progress of each task and ensure that work moves smoothly without unnecessary delays [
7,
76]. The third principle, creating flow, ensures that tasks progress without interruptions [
77]. In a dental setting, this could involve addressing common bottlenecks such as delays in check-ins or inefficiencies in handling dental instruments. Practices then can maintain a steady and efficient workflow if staff reduces waiting times through improved appointment scheduling and ensuring instruments are readily available when needed, [
78,
79]. Also, establishing a pull system ensures that resources are utilized only when there is demand, reducing excess inventory and wait times [
80]. In dentistry, this could involve implementing a “just-in-time” system for ordering supplies, ensuring that materials are replenished based on actual usage. This helps avoid overproduction and waste, while patient care is “pulled” based on individual needs rather than a rigid schedule [
36,
81]. Lastly, continuous improvement, or Kaizen, emphasizes ongoing evaluation and refinement of processes [
82]. In this sense, dental teams can hold regular meetings to discuss challenges and propose improvements, cultivating a culture where all staff is responsible for enhancing both patient care and operational efficiency [
83,
84]. This continuous feedback loop is essential for sustaining improvements over time [
85].
It is further suggested that lean principles can be scaled from small clinics to larger healthcare institutions with careful planning and phased implementation [
86]. Smaller clinics might start by adopting one or two lean tools, such as 5S for workplace organization and Kanban for inventory control, before progressing to more complex lean systems like Just-In-Time (JIT) and Root Cause Analysis [
36]. Larger institutions, with more complex workflows and greater patient volumes, can benefit from integrating lean across multiple departments simultaneously, using tools such as VSM to coordinate efforts across various units [
87]. Importantly, scalability requires ensuring that staff at all levels are engaged in the lean process, with continuous training and feedback loops to minimize disruptions to daily operations [
16]. Implementing lean incrementally and involving staff in problem-solving can ensure that changes are sustained over time and that lean principles are embedded in the organizational culture [
88].
In addition, our study highlights the value of interdisciplinary learning. Successes in implementing lean tools in various healthcare specialties, such as 6S in emergency rooms, can be adapted to dental clinics or outpatient services to improve workflow and patient throughput [
89,
90]. Lea
n’s versatility enables its application across different healthcare sectors, enhancing shared learning and improvement [
48,
51,
52,
91,
92]. In this sense, with the increasing use of digital tools like CAD/CAM systems, digital radiography, and 3D printing in dentistry, lean management plays a crucial role in optimizing these workflows
[72]. Digital technologies can create inefficiencies if not managed properly, leading to delays and waste [
93]. Lean principles help streamline these processes, reduce redundancies, and ensure the maximum use of resources (Smith et al
. 2020) [
94]. For instance, applying lean to digital dental restoration production can cut down the cycle time from digital impression to product delivery, enhancing patient satisfaction while minimizing resource use [
95].
Despite its potential, implementing lean management in dentistry is not without challenges. Some of the key barriers include resistance to change among staff, the upfront cost of lean training and technology implementation, and the difficulty in shifting from traditional workflows to lean-based processes [
96]. Healthcare and dental clinics face significant challenges in implementing lean practices, particularly due to the high initial investment required for advanced technology such as 3D printing and digital systems, which can be prohibitive for smaller practices [
97]. Additionally, a lack of trained personnel to manage and operate these tools further hampers lean adoption, as specialized training is often needed to integrate new systems effectively [
98]. Finally, existing infrastructure limitations, such as inadequate recycling facilities or supply chain inefficiencies, prevent clinics from fully embracing lean principles and sustainable practices [
6]. Additionally, infection control protocols in dentistry often necessitate the use of single-use materials, which can conflict with lean’s goal of reducing waste [
2,
32]. However, with proper planning, leadership commitment, and staff engagement, these challenges can be overcome as our data show. Success stories from other healthcare sectors demonstrate that lean principles can significantly improve efficiency and patient outcomes when applied systematically [
36,
99,
100]. Also, cultural and organizational resistance is a significant barrier too, when shifting to lean management practices, as clinics accustomed to traditional workflows may resist changes that challenge established routines [
101]. This resistance often derives from a fear of increased complexity or disruption to familiar processes, making it difficult to grow a culture of continuous improvement [
102]. Additionally, regulatory and compliance challenges are critical in limiting the adoption of circular economy practices, especially in dental settings where stringent hygiene and safety regulations prioritize single-use materials, making it harder to implement reusable or sustainable alternatives without compromising patient safety [
103].
Moreover, sustaining lean improvements requires ongoing commitment, as lean management is not a one-time fix but a continuous process that necessitates regular monitoring and adjustments [
104,
105]. Without sustained efforts, the initial gains made through lean practices may gradually diminish, leading to a return to inefficiencies [
106]. Flynn et al. (2018) [
47] specifically stress the importance of maintaining a long-term focus on lean methodologies, underlining that healthcare and dental clinics must embed lean principles into their organizational culture to ensure lasting impact. Regular feedback loops, staff engagement, and continuous process evaluations are key strategies for sustaining lean improvements [
107].
In addition to operational efficiency, we have proven in this study that lean management can also support circular economy practices, helping healthcare and dental clinics reduce waste and improve their environmental sustainability. When minimizing overproduction, optimizing resource usage, and implementing waste-reduction strategies such as Just-In-Time (JIT) inventory management, clinics can reduce their environmental footprint [
108]. Integrating lean with circular economy principles not only promotes sustainability but can also yields economic benefits, such as cost savings from reduced material waste and more efficient resource utilization [
41]. This dual focus on operational efficiency and environmental sustainability offers long-term gains that benefit both the clinic’s bottom line and the planet [
109].
In this point, we need to discuss the fact that despite the broad application of lean principles in healthcare, there is a notable gap in their specific use in dentistry. While lean management is well-studied in areas like hospital workflows and surgical settings, fewer studies, such as Robinson et al. (2019) [
52], provide detailed insights into dental practices, highlighting the need for more research on patient flow, inventory management, and multi-step procedures. Additionally, most studies as we report here, focus on short-term improvements, lacking longitudinal data to assess the long-term sustainability of lean practices [
47]. There is also a need for standardized metrics to evaluate lean outcomes consistently across healthcare settings, which would enable more comprehensive comparisons and implementation strategies [
16,
110].
We should further consider that the integration of emerging technologies such as artificial intelligence (AI), digital supply chain management, and predictive analytics presents exciting new frontiers for lean management in healthcare and dentistry [
111]. AI, for example, can be used to optimize scheduling, predict patient needs, and reduce overprocessing by tailoring treatments to specific patients [
112]. Research in this area could focus on how AI and other technologies can enhance the effectiveness of lean tools, such as Kanban for real-time inventory tracking or Just-In-Time (JIT) systems for ensuring that materials are available exactly when needed [
113]. Investigating how these technologies can streamline workflows and reduce waste would be a valuable contribution to the dental field.
As healthcare increasingly focuses on sustainability, future research should explore how lean management can support circular economy principles, particularly in waste reduction and resource efficiency in dentistry. Studies could investigate how lean tools can be applied to minimize the use of disposable materials in dental and medical practices or to create closed-loop supply chains where materials are recycled or reused. This research would provide a pathway for aligning lean practices with environmental sustainability goals, offering economic benefits through cost savings while also reducing the environmental footprint of healthcare operations. Such research would be crucial in advancing both lean management and sustainability efforts within healthcare sectors.
Conclusion
The application of lean management in healthcare and dentistry has shown clear benefits in reducing waste, improving efficiency, and enhancing patient care. However, challenges such as high initial costs, cultural resistance, and regulatory barriers must be addressed for broader adoption. Research into emerging technologies and under-researched areas like mental health, wellbeing and smaller dental clinics could provide valuable insights in the future. Also, interdisciplinary collaboration between healthcare providers, dental practitioners, and engineers will be key to developing innovative solutions that integrate lean management with technology and sustainability practices in the dental field. Despite these challenges, lean principles offer significant potential for improving clinic efficiency, resource management, and patient satisfaction, making it a valuable tool for future transformations in dentistry.