1. Introduction
Prostate cancer ranks first among cancers affecting males 1.
The age of affected patients is becoming younger, thus problems related to surgery such as sexual function, fertility, or urinary incontinence are increasingly of interest and concern for this younger and sexually active population 2.
The surgical treatment of choice is radical prostatectomy (RP), involving the complete removal of the prostate gland 3.
Potential complications of radical prostatectomy include erectile dysfunction (ED) and urinary incontinence (UI)4,5.
Following radical prostatectomy, damage to the internal sphincter can be partially or totally compensated by the activity of the external sphincter, including the complex formed by the rhabdomyosfincter and the levator ani 6.
Greater preoperative strength of the pelvic floor muscles is associated with a lower postoperative incidence of urinary incontinence. Centemero et al. found that patients who began performing pelvic floor muscle strengthening exercises before radical prostatectomy had better rates of urinary incontinence 3 months after the operation (59.3% vs. 37.3%). Therefore, nursing interventions aimed at strengthening the pelvic floor muscles can reduce the incidence of urinary incontinence 7,8.
Additionally, many patients have difficulty differentiating between abdominal or rectal muscles and the perineal muscles, therefore, we consider prior training by a specialized professional necessary to help them identify the muscles they will subsequently work on.
We believe that the impact of pelvic floor training assisted by biofeedback can be an important tool in improving urinary incontinence after prostatectomy 9,10. In this regard, the conclusions of a meta-analysis conducted in 2016 by Lan-Fang Hsu 10 state that biofeedback can be a complementary treatment to pelvic floor muscle training.
2. Materials and Methods
This is a two-arm Clinical Trial, comprising an experimental group and a control group. Both groups included patients who were to undergo robotic radical prostatectomy.
For sample size calculation, we used the GRAMNO v7.12 program, which is related to the preceding population of patients undergoing surgery, robotic radical prostatectomy, in the years 2018 and 2019. Considering the two study groups, the sample size was calculated accepting an alpha risk of 0.05 and a beta risk of 0.2 in a bilateral test. It was determined that 29 subjects were needed in the first group and 29 in the second to detect a statistically significant difference between two proportions. We could also calculate the sample size based on the work of Parra et al. 11 and Appoloni et al. 12, related to the incidence of patients developing urinary incontinence or erectile dysfunction after radical prostatectomy. Thus, accepting an alpha risk of 0.05 and a beta risk of 0.2 in a bilateral test, 34 subjects were required in the first group and 34 in the second to detect a statistically significant difference. A follow-up loss rate of 10% was estimated.
Given that the difference in sample sizes is not very large between the two calculation methods, we opted for the larger of the two. Therefore, we will recruit 34 patients in the study group and 34 in the control group.
Study Group: Two pelvic floor training sessions assisted by biofeedback were conducted prior to surgery, where a nurse trained in the technique taught the identification of the muscles to work on, the correct performance of perineal contraction without the involvement of auxiliary muscles, and the two types of exercises for strengthening phasic and tonic fibers. After this, once admitted to the Urology unit, they received standard treatment.
Control Group: Upon admission to the Urology unit, they received standard treatment, consisting of explanation by the attending nurse on how to perform pelvic floor muscle strengthening exercises.
Upon admission to the Urology service for robotic radical prostatectomy, both groups completed the following questionnaires:
- -
-International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF) 13
- -
-International Index of Erectile Function-5(IIEF-5) 14.
- -
-Quality of Life Questionnaire (EPIC-CP) 15.
These are validated questionnaires in the Spanish language that allow determining the impact of urinary incontinence and erectile dysfunction prior to surgery.
After surgery, both groups were instructed to perform exercises, consisting of strengthening exercises for type I or tonic fibers, through prolonged contractions of ten seconds with a twenty-second rest, and strengthening exercises for type II or phasic fibers, through ten rapid contractions of one-second duration.
At 4 months post-hospital discharge, a second telephone call was made to complete the following questionnaires:
- -
-International Consultation on Incontinence Questionnaire - Short Form (ICIQ-SF) 13.
- -
-International Index of Erectile Function - 5 (IIEF-5) 14.
- -
-Medication Adherence Report Scale - 8 (MMAS-8) 16.
- -
-Client Satisfaction Questionnaire (CSQ-8) 17.
- -
-Quality of Life Questionnaire (EPIC-CP) 15.
At 12 months, a call was made to complete the same questionnaires and thus conclude the study with results 12 months after the intervention.
3. Results
The obtained results were as follows: out of the total participants (68), 34 were randomly assigned to the study group, and 34 to the control group. Finally, 4 patients were excluded from the study,(reoperation after surgery 2), (impossibility of follow-up 2). We did not find any adverse effects or complications associated with biofeedback in the patients belonging to the study group. Demographic Variables.
Study Group: 33 Patients (1 loss)
Mean age: 62.85
Smokers: 2
Diabetics: 3
Previous medication for erectile dysfunction (ED): 1
Previous medication for urinary incontinence (UI): 0
Control Group: 31 Patients (3 losses)
Mean age: 62.00
Smokers: 3
Diabetics: 5
Previous medication for ED: 3
Previous medication for UI: 1
Primary Variables.
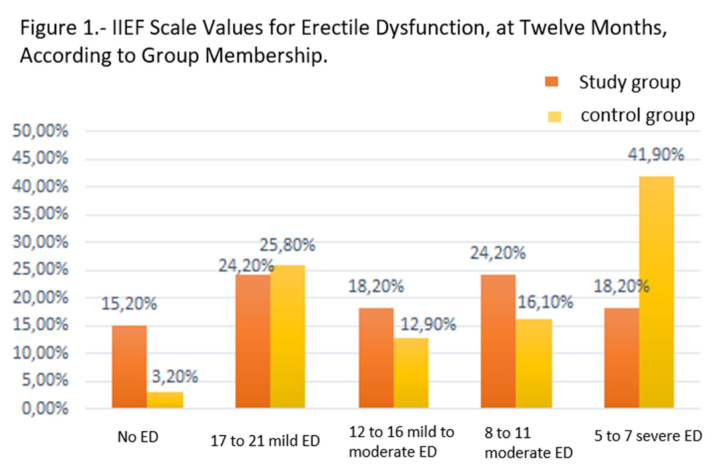
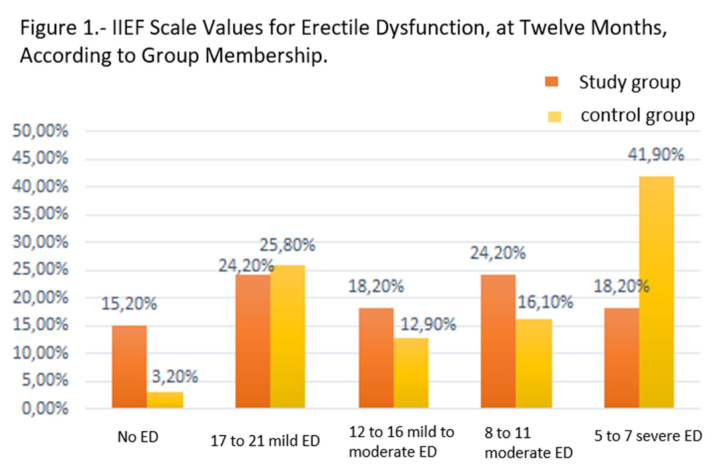
Erectile Dysfunction Questionnaire (IIEF): After applying statistics such as Chi-Square (p=0.159), we can observe a difference of almost 5 times more patients without ED in the study group compared to the control group. Furthermore, we observe a significant difference in the severity of ED between both groups, noting that the control group has almost double the number of patients with severe ED compared to the study group. (Figure 1).
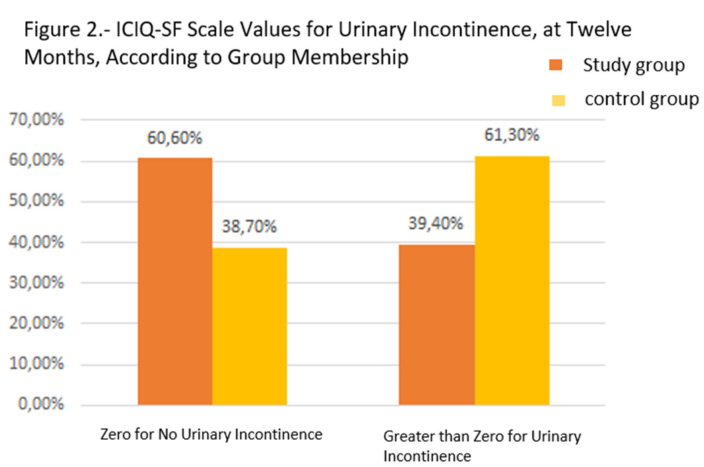
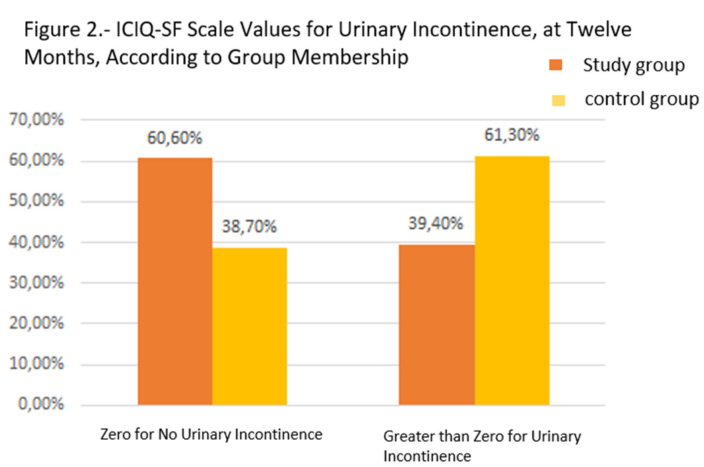
Urinary Incontinence Questionnaire (ICIQ-SF): Applying again, as these are two descriptive variables, the Chi-Square test, we obtained a result with a significance level of 0.080, concluding that there is a relationship between the two variables. We observed clearly that almost double the number of patients in the study group do not have UI compared to the control group. Despite these data, there is a decrease in the number of UI cases between 4 and 12 months in both groups; from 66.7% of incontinent patients at 4 months to 39.4% at 12 months in the study group, and from 74.2% to 61.3% in the control group (Figure 2).
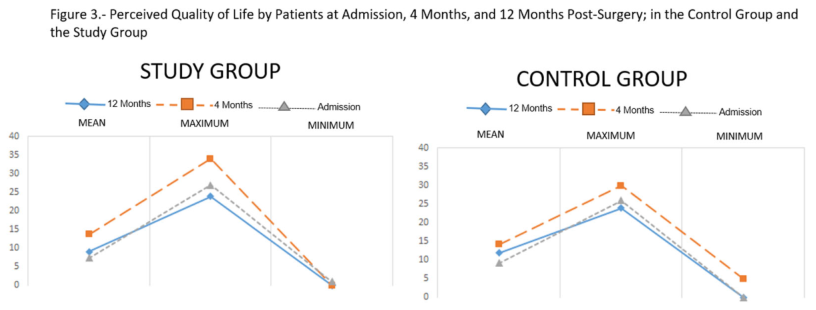
Quality of Life Questionnaire (EPIC-CP): This questionnaire contains 16 items divided into 4 domains; each domain contains 3 questions with Likert scale response options ranging from 0 to 4 points. Scores range from 48 points to 0 points, with lower scores indicating better perceived quality of life. Comparing the scores of both groups, we see a slight difference in the perceived quality of life at 12 months for patients in the study group (average score of 9.09) compared to the control group (average score of 11.97). Although their minimum and maximum values are the same (0-24), we can conclude that the perception of quality of life in patients in the study group is slightly higher than that perceived by the control group (Figure 3).
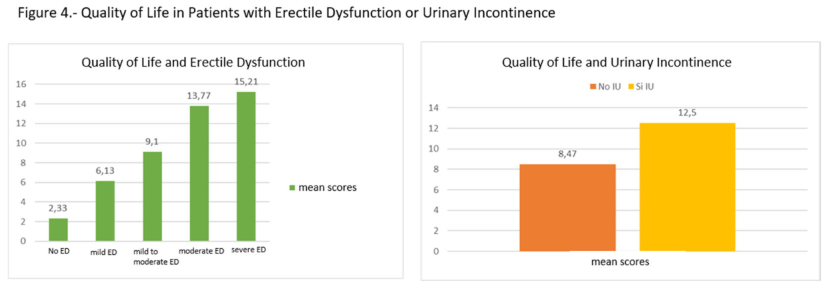
Similarly, comparing these results with those obtained in the two main questionnaires, we can draw certain conclusions.
Quality of Life and Erectile Dysfunction:
Patients without ED have an average score of 2.33.
With ED, the difference from patients without ED also varies, and among the ED subgroups, the average score increases as the severity of ED increases. Thus, the correlation between the perception of quality of life and erectile dysfunction is clearly observed.
Quality of Life and Urinary Incontinence:
Patients without urinary incontinence have a lower average score (8.47) than those with urinary incontinence (12.50). Therefore, the perceived quality of life by patients without urinary incontinence is higher than that perceived by patients with incontinence. (Figure 4)
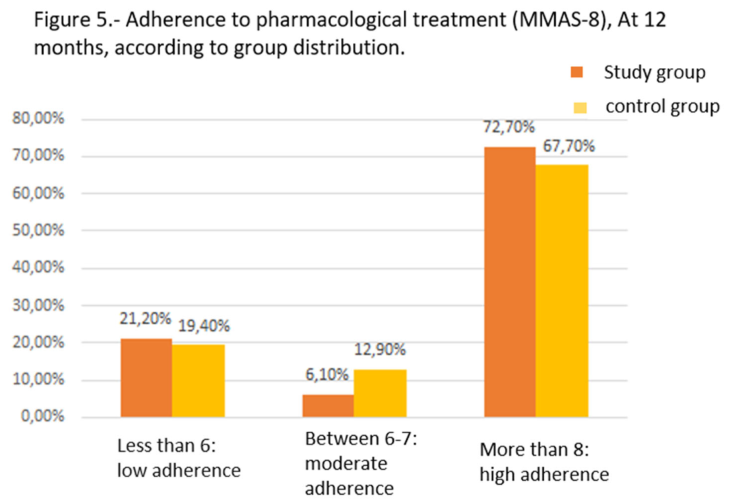
Medication Adherence Questionnaire (MMAS-8): This questionnaire, validated by Morisky (2008) (18), consists of several questions with YES/NO responses (scored as YES=0 points/NO=1 point), and one question scored on a Likert scale (0-4). Scores thus range across various ranges:
Low Adherence <6
Moderate Adherence 6 or 7
High Adherence 8
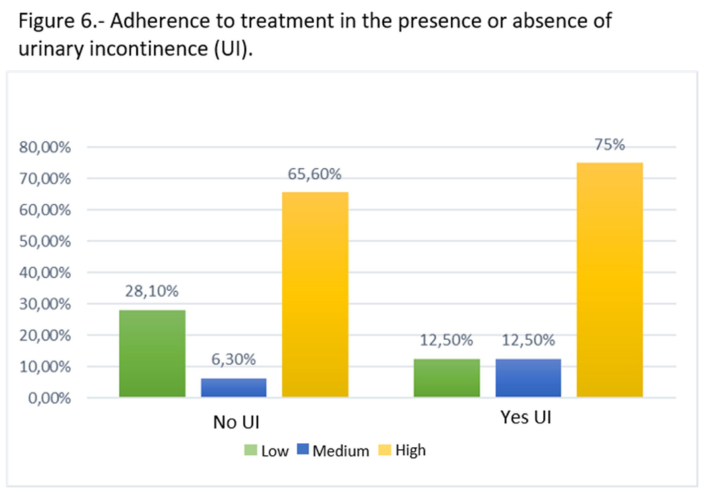
The results obtained in our study show an overall high adherence (70.3%). By cross-referencing the data obtained in the MMAS-8 test with those of the urinary incontinence questionnaire, we obtain the following results, where there is a high adherence to treatment in both patient groups. There are almost 10% more patients with UI who adhere strictly to treatment, (Figure 5), (Figure 6)
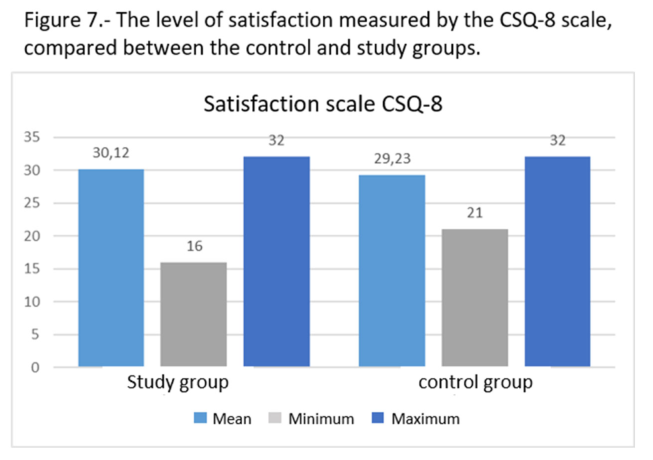
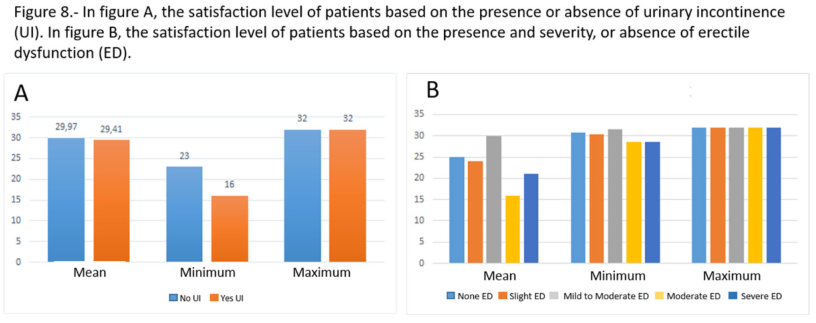
Level of Satisfaction with the Service (CSQ-8): This questionnaire is based on 8 questions with evaluations ranging from 1 to 4 points, and satisfaction is directly related to the number of points. Differentiating by groups, the results obtained are as follows (Figure 7):
Study Group: 30.12 points; (Figure 8)
Control Group: 29.23 points; . The significance level after performing Mann-Whitney T-tests is 0.199, concluding that there are no differences between both groups. Analyzing the results together with the results obtained in the UI and ED questionnaires, we obtain the following results: Based on this data, we can conclude that both groups present a high level of satisfaction regardless of the group they belonged to and regardless of whether they currently have UI and/or ED
1. Discussion
After surgery and immediate postoperative period, other problems arise that have not been previously described in most cases, and once the fear of tumor consequences is overcome, it jeopardizes their new daily life. Erectile dysfunction and urinary incontinence are aspects that determine the quality of life of the patient.
Hence the importance of preoperative health education, not only to recover the perineal musculature as soon as possible or for the patient to perform the exercises correctly, but also for the patient to know from the very beginning the real possibility of experiencing incontinence and/or erectile dysfunction.
We cannot attribute the lack of statistical significance in the study of variables to the diversity of personnel in the performance of the biofeedback technique, as the same professional was responsible for carrying out the training with this technique.
The degree of adherence obtained in our series is relevant, if we take as a reference the work of Morris et al. 18, where they estimate between 30% to 50% the lack of adherence to a treatment regardless of the disease, prognosis, or treatment, in our series we achieved an adherence of 70% in performing perineal rehabilitation at one year.
As Girotti et al. 20, in a prospective cohort study of 60 patients performing intermittent catheterization where the adherence rate at 6 months (61.7%) was similar to that at one year (58%), in our series, there are also no significant differences in adherence at 4 months and at one year.
The erectile dysfunction rates vary for robotic surgery between 3-51% in the literature. Other authors speak of erectile dysfunction rates of 30%, while others speak of recovery to pre-surgery states in only 33%.
In our series, we observed moderate/severe dysfunction rates of 42% for the study group compared to 58% for the control group, indicating an improvement in rates in the study group. This improvement is observed in all subdivisions, including patients who do not have erectile dysfunction, who are up to 5 times more numerous in the study group. Severe dysfunction is present in double the number of patients in the control group compared to the study group.
Regarding urinary incontinence, the literature speaks of rates of up to 80%. In our work, we observed rates of incontinence that double in the case of the control group, maintaining a rate of incontinence in the study group of 39%.
Our work coincides with other studies such as LF Hsu et al. 10, where time is crucial for continence recovery. In our series, for the study group, we went from incontinence rates of 66% at 4 months to incontinence rates of 39% one year after surgery. This improvement is not reflected in the control group to the same extent.
These long-term incontinence results are similar to those obtained by Dijkstra-Eshuis et al. 21, who, after randomizing 122 patients into two groups, one with prior biofeedback technique and the control group, obtained an incontinence rate at one year of 32.8% (in our work 38.7% in the study group; 61.3% in the control group), without a clear improvement in the study group. However, Grabbert et al. (26), who, on a sample of more than 4000 patients and a median follow-up of 42 months, obtained incontinence rates of 77% (ICIQ = 0), in our work the study group ICIQ = 0 is obtained by 60.6% of the patients and in the control group only 38.7%.
Johansson E et al. 22, in a sample of 182 patients undergoing radical prostatectomy with a median follow-up of 12.2 years, obtained urinary incontinence rates of 41%, similar to the control group in our series.
Erectile dysfunction results also improve in the long term, coinciding with the work of Grabbert, M et al. 23, who obtained erectile dysfunction rates of 39% with an IIEF-5 score greater than 20 points. In our study, this score is only obtained by the study group (39.4% IIEF-5 >17 points) and not by the control group (29.0% IIEF-5 >17 points). This author identifies time as a risk factor in quality of life.
Johansson E et al. 22 obtained erectile dysfunction rates of 84%, very similar to the rates obtained in the study group (84.8%) of the present work and differing from the control group, which obtained much higher rates (96.8%).
2. Conclusions
The use of biofeedback as a supportive element in preventing urinary incontinence and erectile dysfunction in patients undergoing robotic radical prostatectomy is a safe technique that can provide advantages in helping patients learn pelvic floor muscle strengthening exercises more easily and rigorously.
With the use of biofeedback, we have improved the incidence of urinary incontinence and erectile dysfunction in patients undergoing robotic prostatectomy at the Hospital Clínico San Carlos in Madrid, with a 50% improvement in the rates of urinary incontinence and severe erectile dysfunction.
Although the sample distribution is very homogeneous between the two groups, and there is an evident improvement in the incidence of urinary incontinence and erectile dysfunction in patients who have undergone biofeedback sessions, a significant proportion between its use and the improvement of the study variables is not achieved. We can attribute this to an insufficient sample size as a possible cause, despite observing a favorable trend, we do not obtain a statistically significant relationship.
In conclusion, we would like to emphasize the importance of continuing studies related to the role of nursing in radical prostatectomy, where it can be seen that helps to improve UI and ED, as well as the quality of life of patients undergoing these types of interventions.
This clinical trial highlights the need for more studies in this area, where nursing can develop an important and decisive role in the perioperative care of these patients, directly influencing an improvement in their quality of life.
Author Contributions
Carlos Lorenzo García: Conceptualization, methodology, software, Validation, Formal analysis, Research, Resources, Data curation, Original draft writing, Review and editing writing, Visualization, Supervision, Project administration, Financing acquisition Paloma Coronel Rosado: Conceptualization, methodology, software, Validation, Formal analysis, Research, Resources, Data curation, Original draft writing, Review and editing writing, Visualization, Supervision, Project administration, Financing acquisition Ana Lucía Guzmán Bellodas: Conceptualization, methodology, software, Validation, Formal analysis, Research, Resources, Data curation, Original draft writing, Review and editing writing, Visualization, Supervision, Project administration, Financing acquisition. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of NAME OF CEim Hospital Clínico San Carlos Código 21/493-E 29/07/2021
Informed Consent Statement
“Informed consent was obtained from all subjects involved in study.” “Written informed consent has been obtained from the patient(s) to publish this paper”
Data Availability Statement
The data sets presented in this article are not available because they are part of an ongoing study. Requests to access the data sets should be directed to carlos.lorenzo@salud.madrid.org
Acknowledgments
Our thanks to Dr. Santos;Dr. Gallant; Dr. Senovilla; Dr. Moreno; Mr. Enrique Pacheco for his invaluable help
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| (ICIQ-SF) |
International Consultation on Incontinence SF |
| (IIEF-5) |
International Index of Erectile Function -5 |
| (MMAS-8) |
Medication Adherence Report Scale - 8 |
| (CSQ-8) |
Client Satisfaction Questionnaire |
| (EPIC-CP) |
Quality of Life Questionnaire |
| ED |
Erectile dysfunction |
| UI |
Urinary Incontinence |
| RP |
Radical prostatectomy |
References
- SEER [Internet]. [citado 9 de mayo de 2024]. SEER Cancer Statistics Review, 1975-2016. Disponible en: https://seer.cancer.
- Teloken P, Valenzuela R, Parker M, Mulhall J. The Correlation Between Erectile Function and Patient Satisfaction. J Sex Med. 1 de marzo de 2007;4(2):472-6. https://www.sciencedirect.com/science/article/abs/pii/S1743609515315101.
- Bianco FJ, Scardino PT, Eastham JA. Radical prostatectomy: Long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology. 1 de noviembre de 2005;66(5, Supplement):83-94https://pubmed.ncbi.nlm.nih.gov/16194712/.
- Kundu SD, Roehl KA, Eggener SE, Antenor JAV, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urol. diciembre de 2004;172(6 Pt 1):2227-31. https://www.auajournals.org/doi/10.1097/01.ju.0000145222.94455.73.
- Documento de consenso sobre disfunción eréctil. SEMERGEN - Med Fam. 1 de enero de 2003;29(5):255-63https://www.sciencedirect.com/science/article/abs/pii/S1138359303741884.
- Valero, R. , Ko, Y. H., Chauhan, S., Schatloff, O., Sivaraman, A., Coelho, R. F.,... & Patel, V. R. (2011). Cirugía robótica: Historia e impacto en la enseñanza. Actas urológicas españolas, 35(9), 540-545. [CrossRef]
- Santos DRF dos, Silva FBL e, Saldanha E de A, Lira ALB de C, Vitor AF. Cuidados de enfermagem ao paciente em pós-operatório de prostatectomia: revisão integrativa. Nursing care of postoperative prostatectomy patients: an integrative review [Internet]. 2012 [citado 9 de mayo de 2024]; Disponible en: https://repositorio.ufrn.br/handle/1/11716.
- do Nascimento Oliveira, D. M. , Lima da Nóbrega, M. M., Lima de Andrade, L., da Silva, A. F., Lopes Costa, M. M., & Abrantes de Carvalho, M. W. (2017). DIAGNOSES, RESULTS AND NURSING INTERVENTIONS FOR THE PROSTATECTOMIZED PATIENT. Journal of Nursing UFPE/Revista de Enfermagem UFPE, 11(11).
- Un programa guiado por biorretroalimentación o estimulación eléctrica de los músculos del suelo pélvico puede mejorar la recuperación temprana de la continencia urinaria después de una prostatectomía radical: un metanálisis y una revisión sistemática - Sciarra - 2021 - International Journal of Clinical Practice - Wiley Online Library [Internet]. [citado 9 de mayo de 2024]. Disponible en: https://onlinelibrary.wiley.com/doi/full/10.1111/ijcp.14208.
- Hsu LF, Liao YM, Lai FC, Tsai PS. Beneficial effects of biofeedback-assisted pelvic floor muscle training in patients with urinary incontinence after radical prostatectomy: A systematic review and metaanalysis. Int J Nurs Stud. 1 de agosto de 2016;60:99-111. https://pubmed.ncbi.nlm.nih.gov/27297372/.
- Parra López ML, Lozano Blasco JM, Osman García I, Congregado Ruiz B, Conde Sánchez JM, Medina López RA. Climacturia after robot-assisted laparoscopic radical prostatectomy. Rev Int Andrología. 1 de enero de 2021;19(1):49-52https://pubmed.ncbi.nlm.nih.gov/32147377/.
- Appoloni Eduardo Aline Helena, Napoleão Anamaria Alves, Carvalho Emilia Campos de. Intervenciones de enfermería en pacientes con disfunción eréctil después de prostatectomía radical: una revisión integral. Enferm. glob. [Internet]. 2016 Abr [citado 2024 Mayo 09] ; 15( 42 ): 424-439. Disponible en: https://scielo.isciii.es/scielo.php?pid=S1695-61412016 000200015&script=sci_arttext.
- Espuña Pons M, Rebollo Álvarez P, Puig Clota M. Validación de la versión española del International Consultation on Incontinence Questionnaire-Short Form. Un cuestionario para evaluar la incontinencia urinaria. Med Clínica. 1 de enero de 2004;122(8):288-92. https://www.sciencedirect.com/science/article/abs/pii/S0025775304742128.
- Pacenza NA, Ponzo O, Pierini A, Sinay IR. Utilidad de la versión abreviada del Indice Internacional de Función Eréctil (IIEF-5) pra la evaluación de la severidad de la disfunción eréctil y de la respuesta al tratamiento con sildenafil. Prensa Méd Argent. 2005;501-6.
- Chang P, Szymanski KM, Dunn RL, Chipman JJ, Litwin MS, Nguyen PL, et al. Expanded Prostate Cancer Index Composite for Clinical Practice: Development and Validation of a Practical Health Related Quality of Life Instrument for Use in the Routine Clinical Care of Patients With Prostate Cancer. J Urol. septiembre de 2011;186(3):865- 72. https://www.auajournals.org/doi/10.1016/j.juro.2011.04.085.
- Definición del cambio mínimo detectable en las puntuaciones en la escala de adherencia a la medicación de Morisky de ocho ítems - Paul Muntner, Cara Joyce, Elizabeth Holt, Jiang He, Donald Morisky, Larry S Webber, Marie Krousel-Wood, 2011 [Internet]. [citado 9 de mayo de 2024]. Disponible en: https://journals.sagepub.com/doi/10.1345/aph.1P677.
- De la Higueras J, Anguita F, Bueno A, Castellanos P, De la Montaña C, Fernández M, et al. Cuestionario de Satisfacción Client Satisfaction Questionnaire (CSQ-8) Personas Usuarias y Familiares [Internet]. Vol. 6, De-sarrollo de Programas de Tratamiento Asertivo Comunitario en Andalucía. 2010 [cited 2021 Jul 22]. Available from: http://www.sspa.juntadeandalucia.es/servicioandaluzdesalud/contenidos/publicaciones/ Datos/42 6/pdf/ Anexo_3-3_CSQ.pdf.
- Retracted: Predictive Validity of a Medication Adherence Measure in an Outpatient Setting - Morisky - 2008 - The Journal of Clinical Hypertension - Wiley Online Library [Internet]. [citado 9 de mayo de 2024]. Disponible en: https://onlinelibrary.wiley.com/doi/10.1111/j.1751-7176.2008.07572.x.
- Cumplimiento del paciente: descripción general - Morris - 1992 - Journal of Clinical Pharmacy and Therapeutics - Wiley Online Library [Internet]. [citado 9 de mayo de 2024]. Disponible en: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2710.1992.tb01306.x.
- Sabaté E, World Health Organization, editores. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. 198 p.
- Girotti ME, MacCornick S, Perissé H, Batezini NS, Almeida FG. Determining the variables associated to clean intermittent self-catheterization adherence rate: one-year follow-up study. Int Braz J Urol. diciembre de 2011;37:766- 72. https://www.scielo.br/j/ibju/a/MTrFgS8hM5fVM6FQvHfDmfR/?lang=en.
- Ruiz-Aragón J, Márquez-Peláez S, Luque Romero LG. Erectile dysfunction in patients with prostate cancer who have undergone surgery: Systematic review of literature. Actas Urol Esp Engl Ed. 1 de enero de 2010;34(8):677-85. [CrossRef]
- Alper K, Ozgur Y, Akif E, Cubuk A, Murat T, Onder C, et al. Long term erectile function results of radical perineal prostatectomy. Rev Int Andrología. 1 de julio de 2022;20(3):152-7. https://pubmed.ncbi.nlm.nih.gov/35331662/.
- VIDA DESPUÉS DE LA PROSTATECTOMÍA RADICAL: UN ESTUDIO LONGITUDINAL | Revista de Urología [Internet]. [citado 9 de mayo de 2024]. Disponible en: https://www.auajournals.org/doi/10.1016/S0022-5347%2805%2965989-7.
- Dijkstra-Eshuis J, Van den Bos TWL, Splinter R, Bevers RFM, Zonneveld WCG, Putter H, et al. Effect of preoperative pelvic floor muscle therapy with biofeedback versus standard care on stress urinary incontinence and quality of life in men undergoing laparoscopic radical prostatectomy: a randomised control trial. Neurourol Urodyn. febrero de 2015;34(2):144-50. https://onlinelibrary.wiley.com/doi/abs/10.1002/nau.22523.
- Grabbert M, Buchner A, Butler-Ransohoff C, Kretschmer A, Stief CG, Bauer RM. Long-term functional outcome analysis in a large cohort of patients after radical prostatectomy. Neurourol Urodyn. septiembre de 2018;37(7):2263-70. [CrossRef]
- Johansson E, Steineck G, Holmberg L, Johansson JE, Nyberg T, Ruutu M, et al. Long-term quality-of-life outcomes after radical prostatectomy or watchful waiting: the Scandinavian Prostate Cancer Group-4 randomised trial. Lancet Oncol. septiembre de 2011;12(9):891-9. https://pubmed.ncbi.nlm.nih.gov/21821474/.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).