1. Introduction
Brain (B-type) natriuretic peptide (BNP) is a peptide hormone released primarily from the cardiac ventricles in response to myocyte stretch. It is synthesized as an inactive prohormone that is split into the active hormone BNP and the inactive N-terminal fragment (NT-pro-BNP). BNP has several systemic effects, including vasodilation, increases in urinary volume and sodium output, and inhibition of the sympathetic nervous system and the renin–angiotensin–aldosterone system. (Levin, ER, Gardner ; 1998)
The prognostic importance of BNP and NT-pro-BNP has been extensively studied in patients with heart failure as well as in patients with acute coronary syndromes, and both markers have been shown to be strong predictors of morbidity and mortality. (Tsutamoto, T, Wada ; 1997)
However, BNP and NT- pro – BNP as a prognostic indicator among elderly population has not been evaluated extensively. Significant number of heart failure cases accounts to be of elderly population and evaluating BNP as a prognostic indicator would enable the care providers to plan their treatment and follow up effectively. This study is to evaluate the prognostic value of BNP as a predictor of overall outcome in elderly patients with heart failure.
2. Methods
Study Population
We conducted a retrospective observational cohort study of 98 elderly patients who were admitted with decompensated heart failure between September 2023 to April 2024 in Lagan valley hospital – Lisburn and Ulster Hospital – Dundonald, Northern Ireland. These two major tertiary care and secondary care hospitals covers entire south eastern trust of Norther Ireland which represent most of the elderly population in the country. Both hospitals have focused protocols on elderly care with onsite availability of cardiac services. We assessed 120 suspected heart failure patients throughout 8 months. The cases were randomly selected as snapshots covering each month. Among these 120 patients, confirmed 88 heart failure cases based on clinical symptoms, echocardiography findings and NT – Pro BNP findings on admission.
Verbal informed consent for Echocardiography, bloods and clinical history and follow up was obtained and consent was taken for anonymized patient information sharing.
Baseline Measurements
In all patients, a thorough medical history was recorded, including details of any previous myocardial infarction, previous revascularization, angina pectoris, arterial hypertension, suspected congestive heart failure (defined by symptoms of shortness of breath or leg edema), previous stroke or transient ischemic attacks, diabetes, atrial fibrillation, and any malignancy. Information came from medical records, directly from patients, or both. Clinical frailty was evaluated as per Rockwood frailty scale for all the patients.
Echocardiography findings were evaluated for all the identified cases. Ejection fraction, presence of any regional wall motion abnormalities, any valve pathologies and presence of any LV thrombus was documented. Majority of the patients received NT- pro BNP during the admission.
The inclusion criteria were being more than 65 years old or Rockwood clinical frailty score of more than 4, Established acute hospital admission with heart failure and NT-pro-BNP value of more than 400 ng/L
Follow Up
The heart failure medications upon the discharge were documented under categories of beta blockers, diuretics, dapagliflozin, digoxin, antiplatelet or anticoagulation.
All 98 patients were followed up for 12 weeks after initial hospital discharge. The follow up pathways were traced through the electronic data records. Follow up with cardiologist, heart failure nurse or community base heart failure care provider was included. Any medication changes or additions during the follow up were recorded. Patients who received repeat NT-pro-BNP was also recorded with values. The follow up was monitored for two major end points. One is heart failure related deaths and the second point is any heart failure re-admissions
Data Analysis
All the patients were categorized to two main cohorts. Heart failure with reduced Ejection fraction (HFrEF/ EF more than 60%) cohort and Heart failure with preserved Ejection fraction ( HFpEF / EF more than 40%) cohort.
Each cohort was again categorized to 3 main sub cohorts according to NT- Pro BNP values on admission. BNP less than 400, BNP between 400 -2000 and BNP more than 2000.
Altogether 6 sub cohorts were formed and data was analyzed under each sub-cohort. Average age, gender distribution, clinical frailty score, presenting symptoms and past medical history was listed under demographic distribution cohort.
Follow up details, heart failure admissions and deaths were listed under morbidity and mortality section.
Demographic Characteristics
HFpEF Cohort were categorized to three sub cohorts according to BNP values. Majority of the sub cohorts were male patients and most of the population had Rockwood clinical frailty score of 6. Majority of the patients presented with Shortness of breath and minority of the population had evidence of fluid overload. The sub cohorts who had moderately and highly elevated BNP had other associated vascular risk factors including coronary artery disease, Hypertension, CKD, CVA and AF. (Further details are at
Table 1)
HFrEF Cohort
Similarly, HFrEF cohort was categorized to sub cohorts according to BNP values. Again, majority of the population were male patients. Average Rockwood clinical frailty score was 5. Again, majority of the patients presented with shortness of breath and was diagnosed as heart failure. Minority of the cohorts presented with evidence of fluid overload. Similarly, the sub-cohorts with moderately and highly elevated BNP values had other cardiovascular risk factors. Further details and specifications are at
Table 2
NT – Pro BNP Values and End Points
The same cohorts were further followed up for 12 -15 weeks for specific end points. On this study, the specific end points that were considered was Readmissions with heart failure admissions and Deaths. Furthermore, the cohorts were assessed whether they received outpatient heart failure follow up or not. All types of follow ups including heart failure nurses, cardiac hub and cardiology specialist follow up were considered in to the follow up data base. Repeat BNP values the patients had during follow ups were compared with the initial BNP value and documented as a ‘reduction’ or ‘increase’. These parameters were again correlated with the end points that was initially mentioned.
The Basic Data Analysis for the End Points
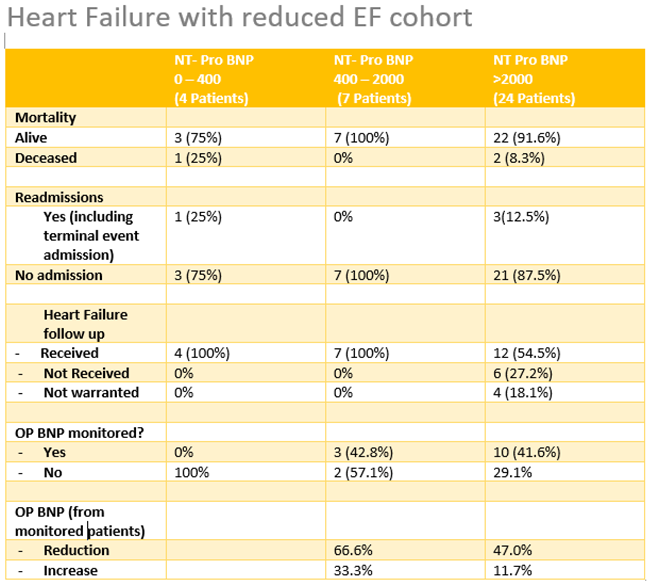
Table 3.
Heart failure with reduced EF cohort.
Table 3.
Heart failure with reduced EF cohort.
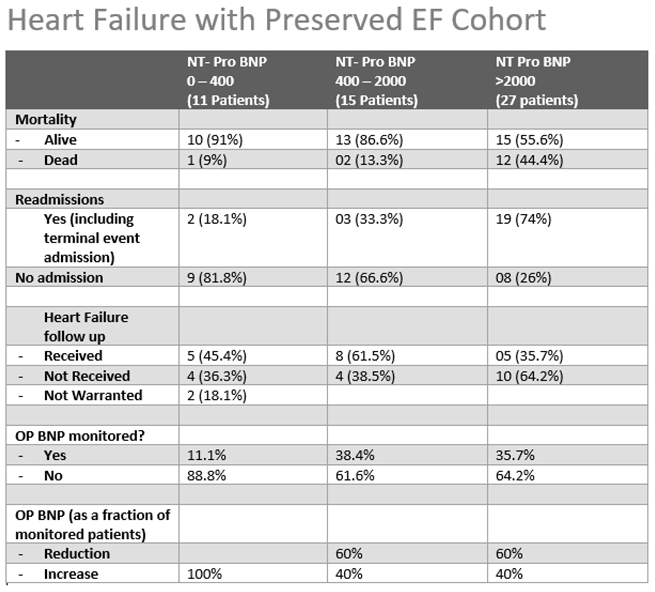
Table 4.
Heart failure with preserved EF cohort.
Table 4.
Heart failure with preserved EF cohort.
3. Results
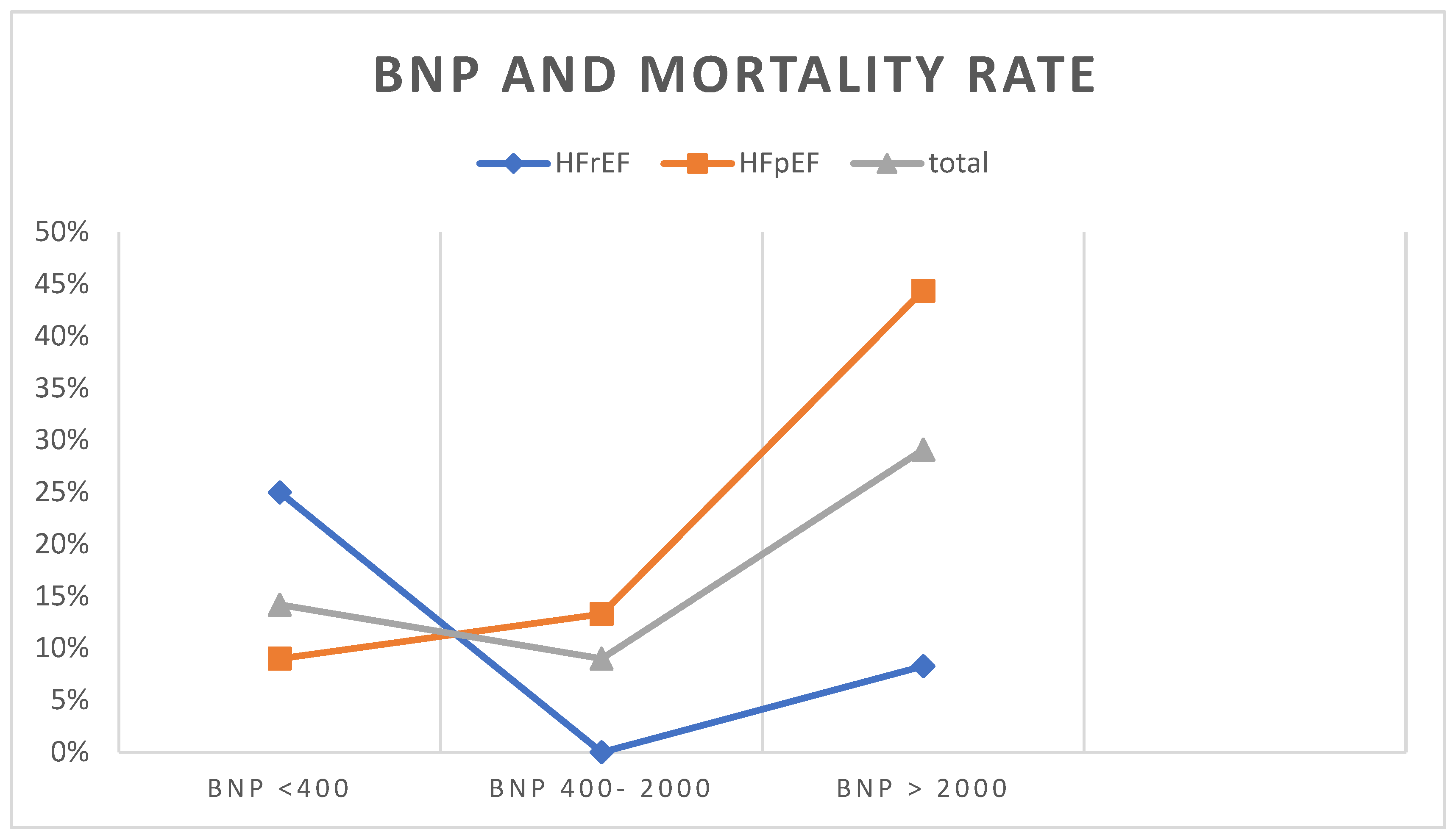
NT Pro BNP and Mortality
The association between NT- pro BNP value and the mortality were evaluated among both HFrEF cohort and HFpEF cohort. In HFpEF group, Sub cohort who had initial BNP value of more than 2000 on admission demonstrated high mortality rate of 44% during the admission and the course of follow up. This observation was slightly differed in HFrEF cohort as the mortality rate that was demonstrated was 8.3%
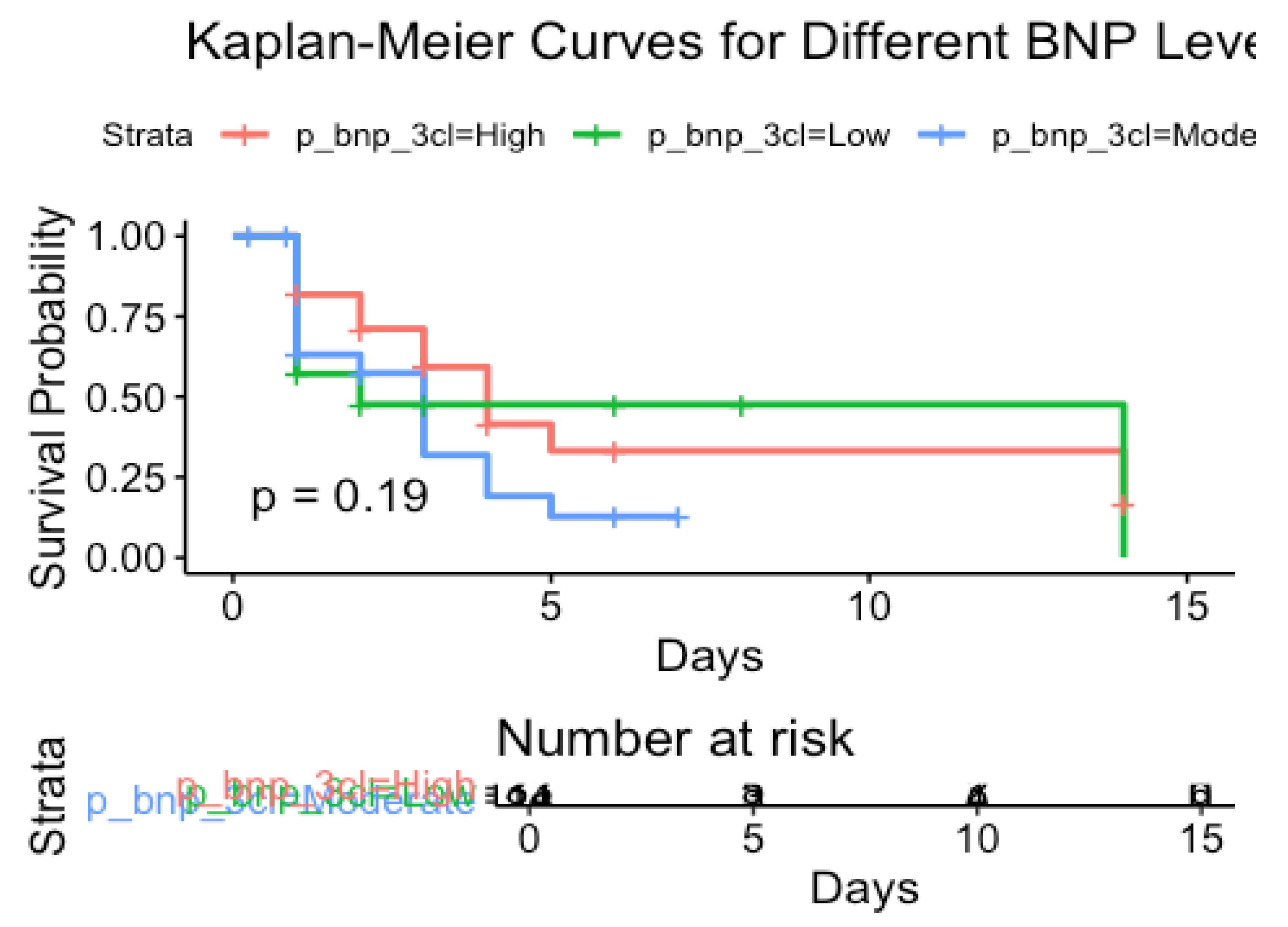
All the mortality rates of sub cohorts were standardized and plotted against the BNP levels. The total cohort demonstrate higher mortality the analysis demonstrated a mortality rate of 29.1% for the sub cohorts who had higher NT- pro BNP value of more than 2000. (
Figure 1)
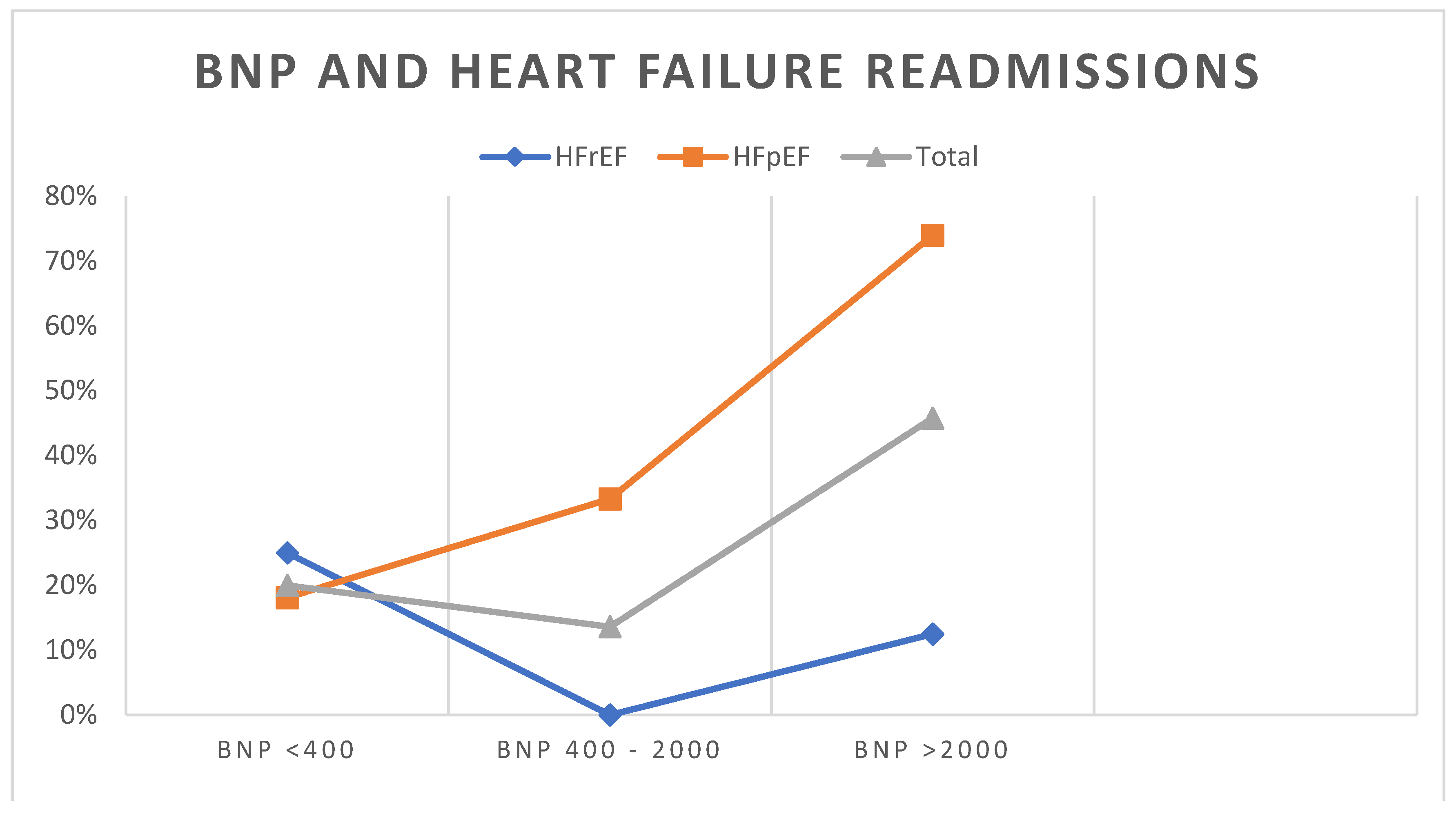
NT- Pro BNP and Heart Failure Readmissions
Similarly, all the date from six sub cohorts were analyzed on the end point for heart failure re-admissions. In HFpEF group, Sub cohort who had initial BNP value of more than 2000 on admission demonstrated high readmission rate of 74% during follow up. This observation was slightly differed in HFrEF cohort as the mortality rate for the same sub cohort with higher BNP demonstrated lower readmission rate of 12.5%. This was a similar observation to the analysis with the end point for mortality. The data was statistically standardized for the whole population and plotted against the BNP values. This showed higher incidence with readmissions. (
Figure 2)
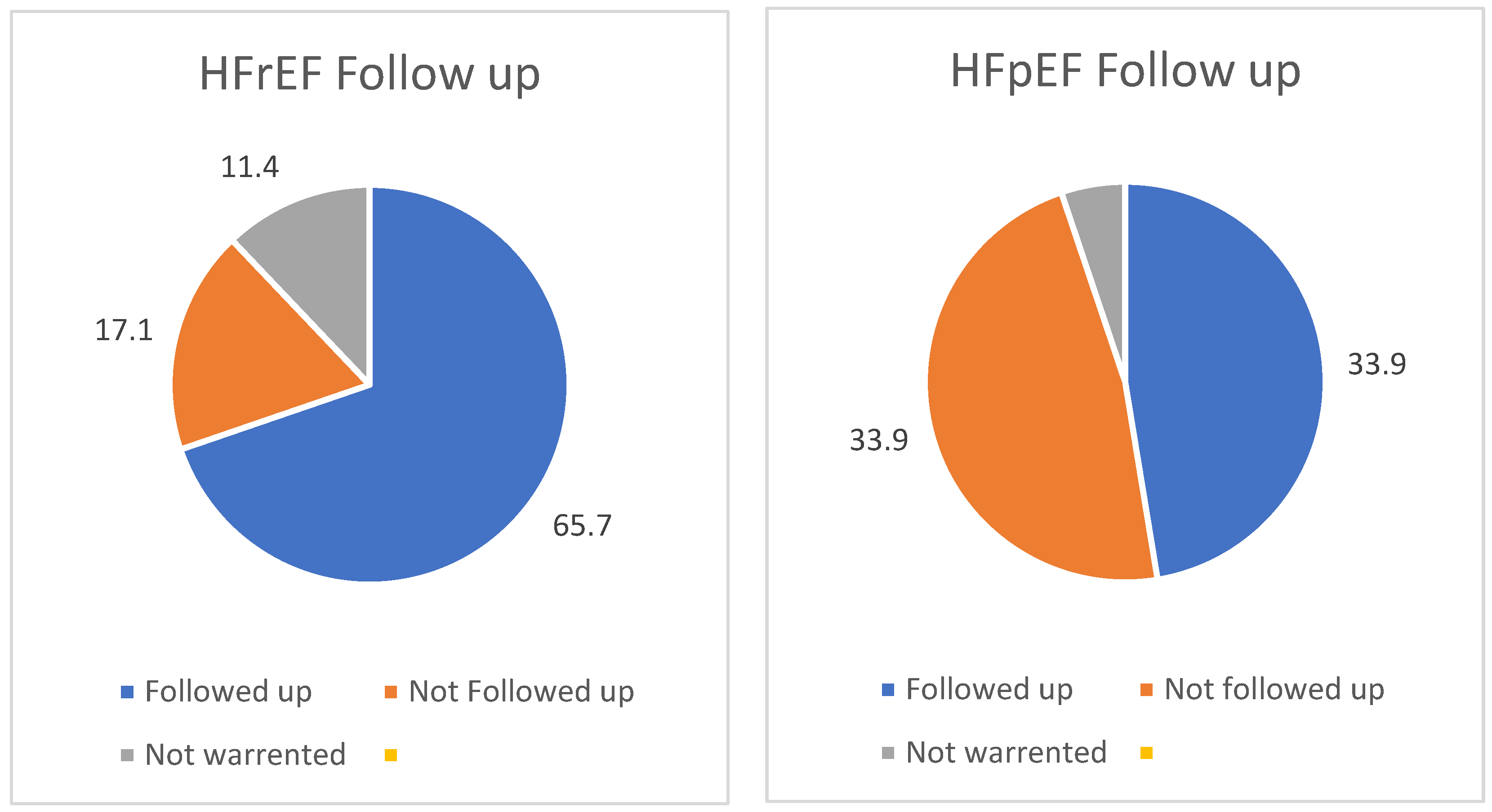
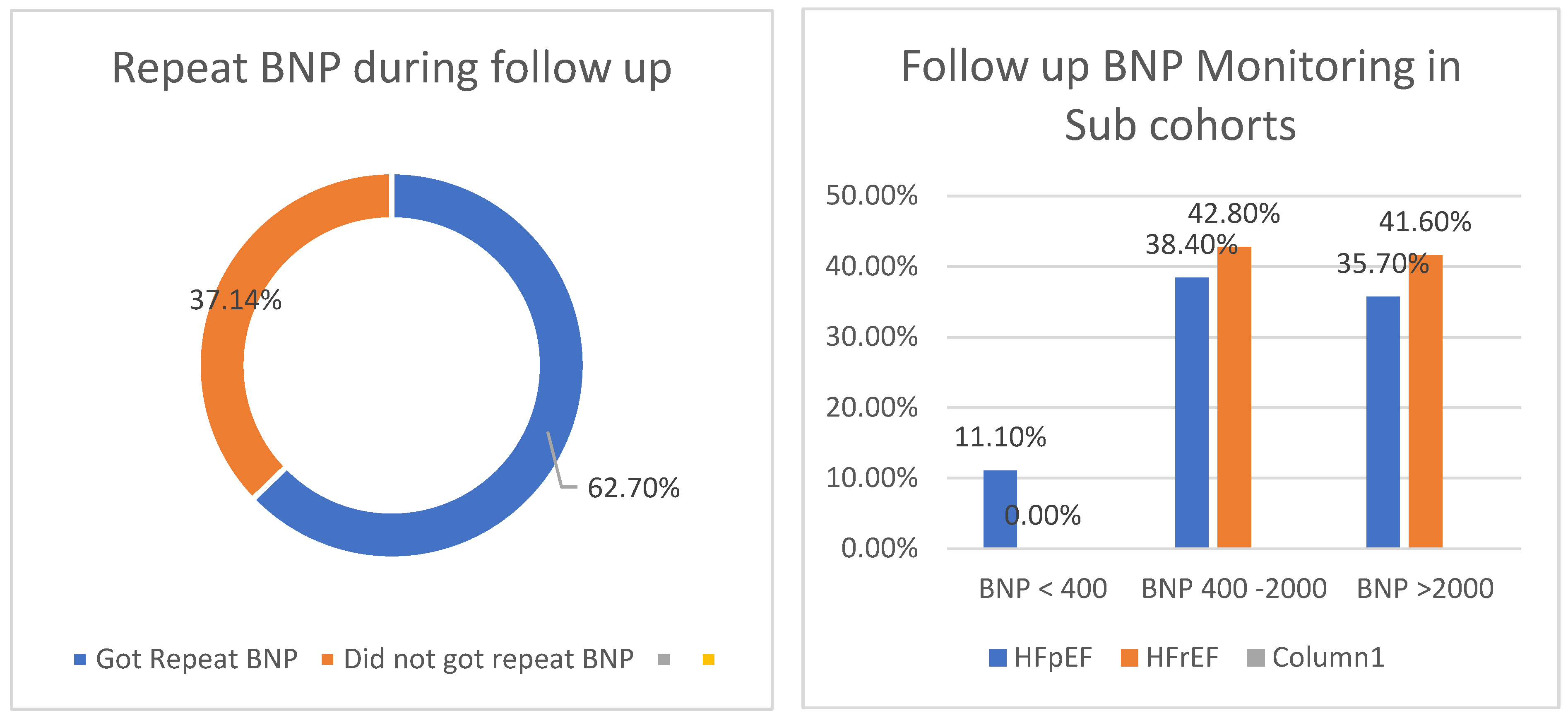
Heart Failure Follow Up
65.7% of the HFrEF cohort received the heart failure follow up under specialist or heart failure nurse lead clinic. Only 33.7% of HFpEF patients received the follow up (
Figure 3). From Followed up patients, 62.7% patients received a repeat NT- pro BNP evaluation either during the follow up or during a readmission. More than 35% of patients who represents sub cohorts with moderately high NT- Pro BNP ( 400 -2000) received repeat BNP during the follow up. This was 38.4% for HFpEF cohort and 42.8% for HFrEF.
Sub cohorts who had NT- Pro BNP values of more than 2000 demonstrated similar statistics by having repeat BNP during follow up. This was 37.5% for HFpEF cohort and 41.6% for HFrEF cohort.
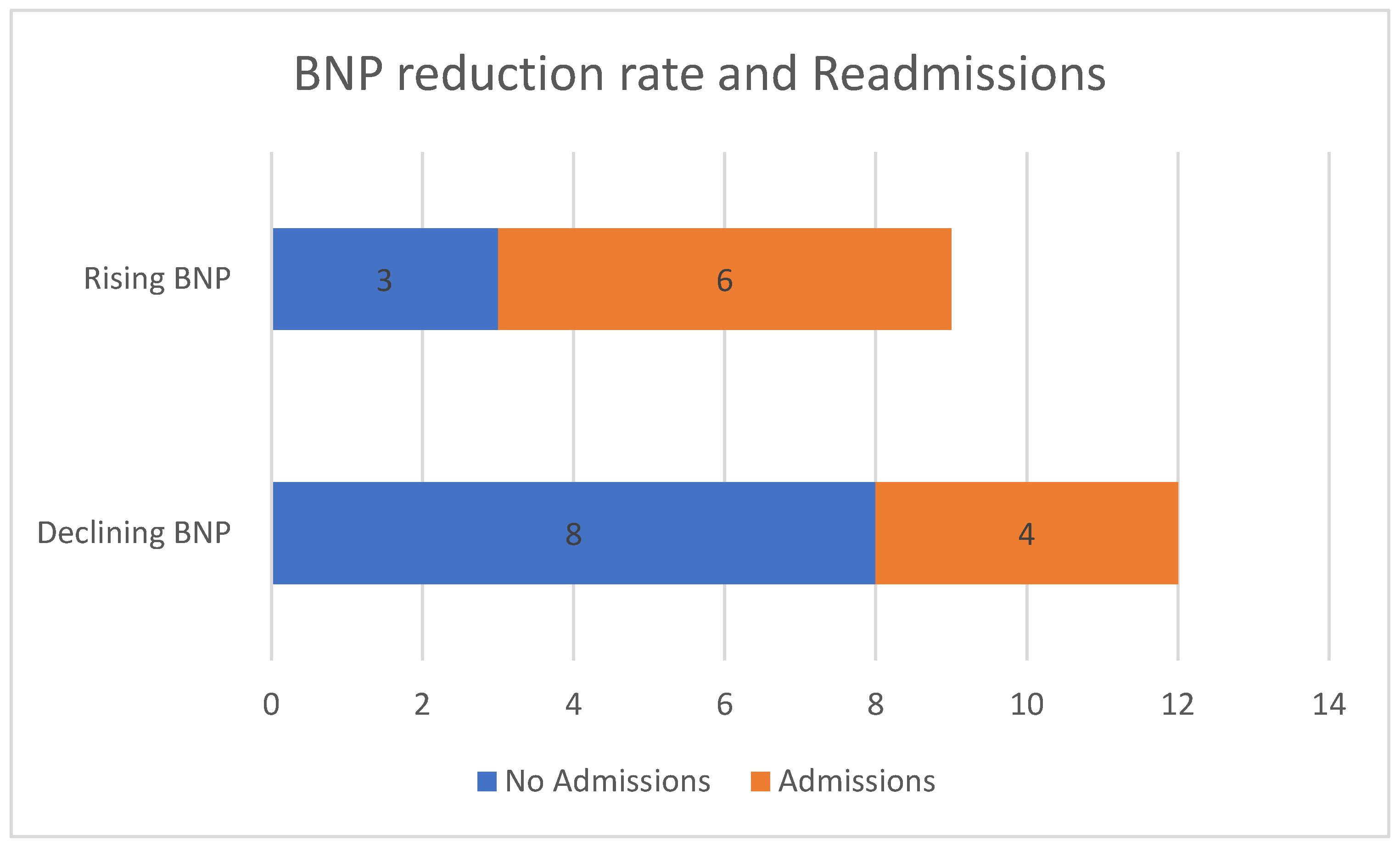
The data analysis was further extended to see whether the patients had declining BNP values or rising BNP values during heart failure follow up. And compared the BNP reduction rate with the re-admissions. During the follow up, there were Total 9 patients who had rising BNP and 6 of them re-admitted with heart failure exacerbation. This is 66.6% re-admission rate for patients with rising BNP.
There were total 12 patients who had declining BNP during the follow up, and only 4 of them got re-admitted with heart failure exacerbation. This is 33.3% re-admission rate for patients with declining BNP. See figure
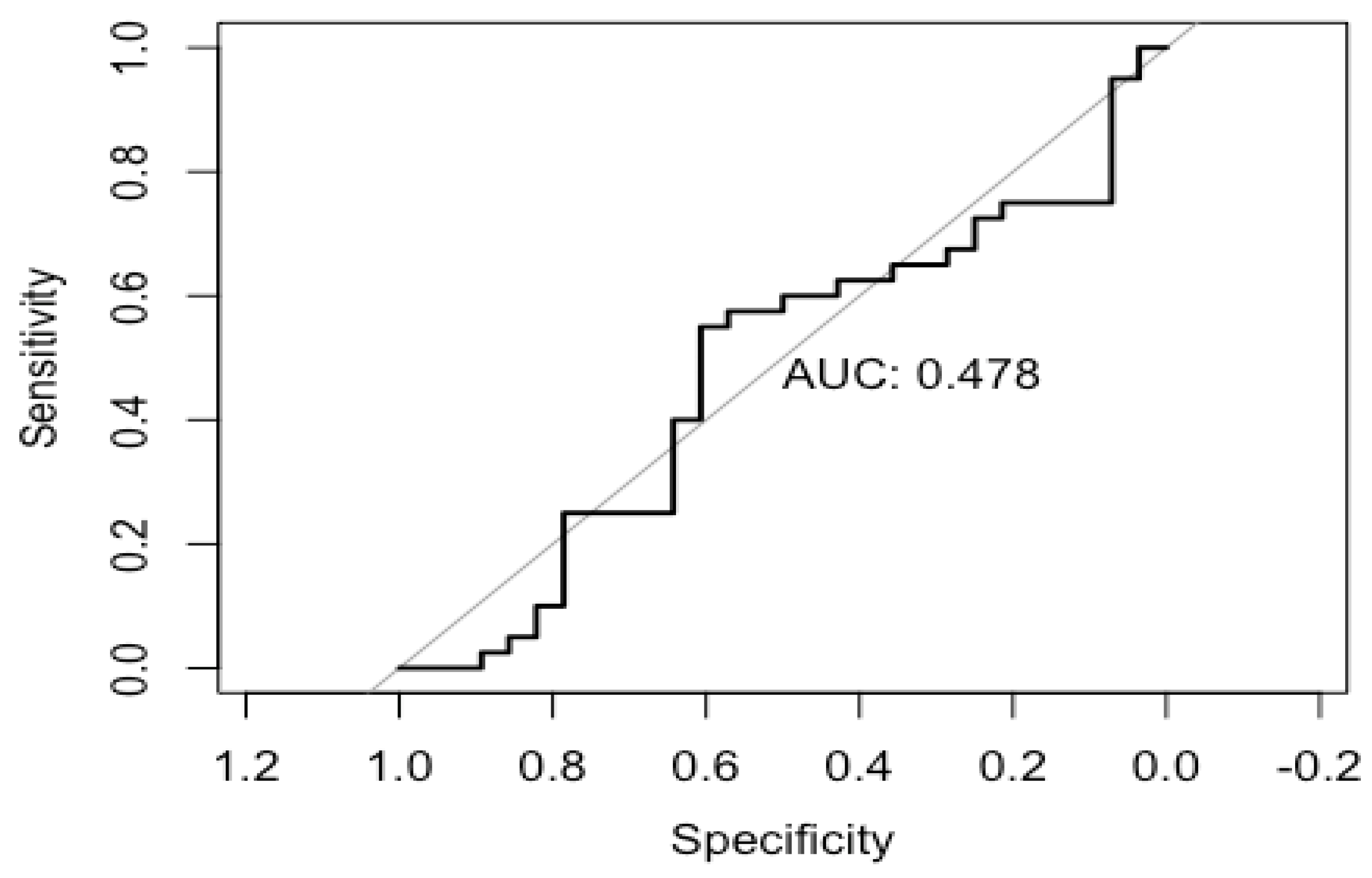
Statistical Power
Categorical variables were reported as numbers and percentages. Normally distributed continuous variables were presented as the mean±SD, while those that were nonnormally distributed were shown as the median and interquartile range. Student’s t test or the Mann–Whitney U test for continuous variables and chi-square or Fisher’s exact tests for categorical variables were used for comparison between the groups, as appropriate. When needed, the variables were transformed for further analysis.
We have re-categorized all the data according to BNP values. Area under the receiver operating curve (AUROC) was calculated for each cohort to measure the natriuretic peptide’s performance in predicting HF mortality at first admission screening. Multiple logistic regression was then performed, using all cohorts combined, to examine whether BNP was predictive of mortality in heart failure. (See
Figure 6)
The area under curve is 0.478, which statically proves that NT- Pro BNP values can be used as a prognostic biomarker for predicting mortality in heart failure patients in elderly.
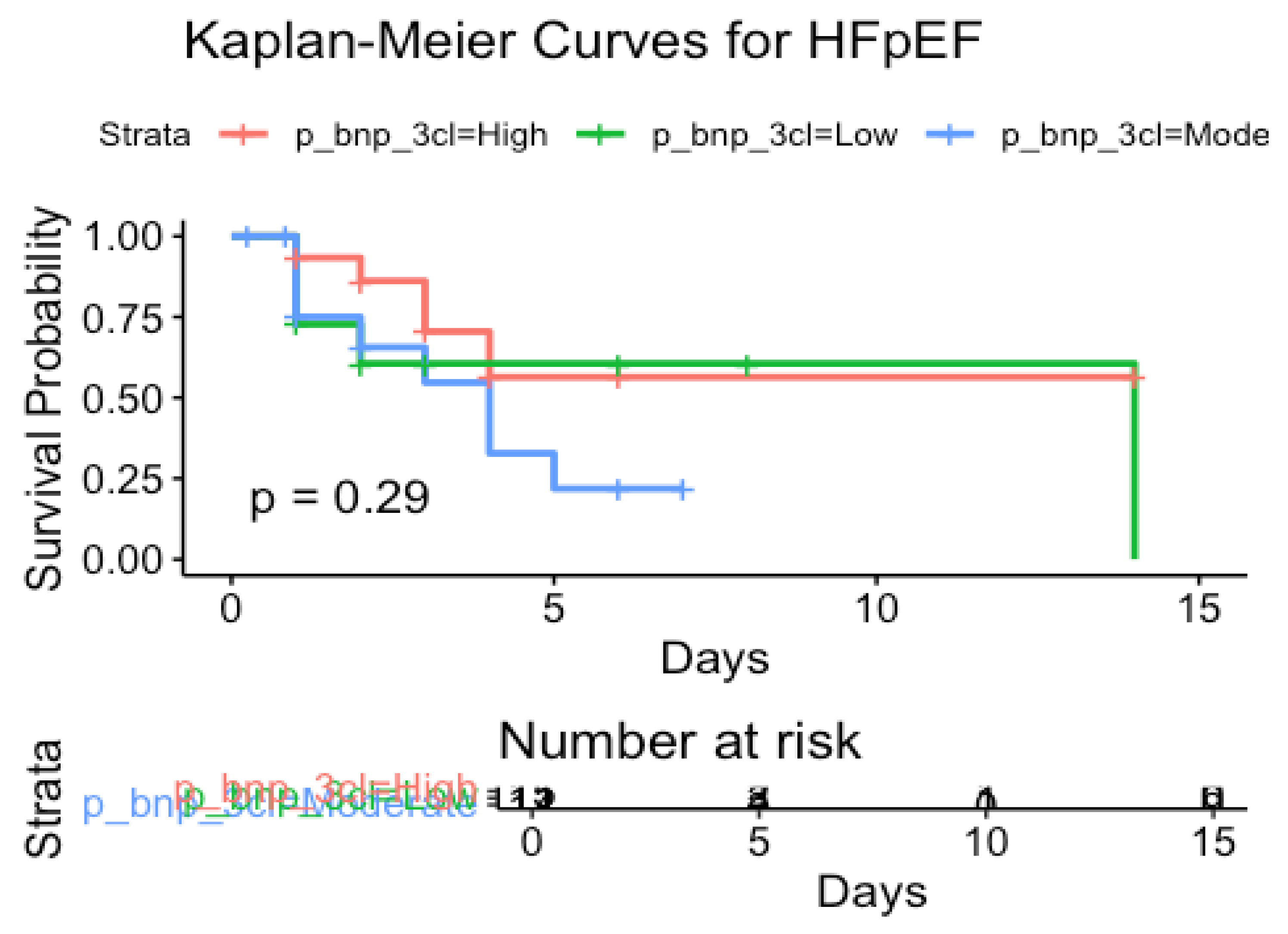
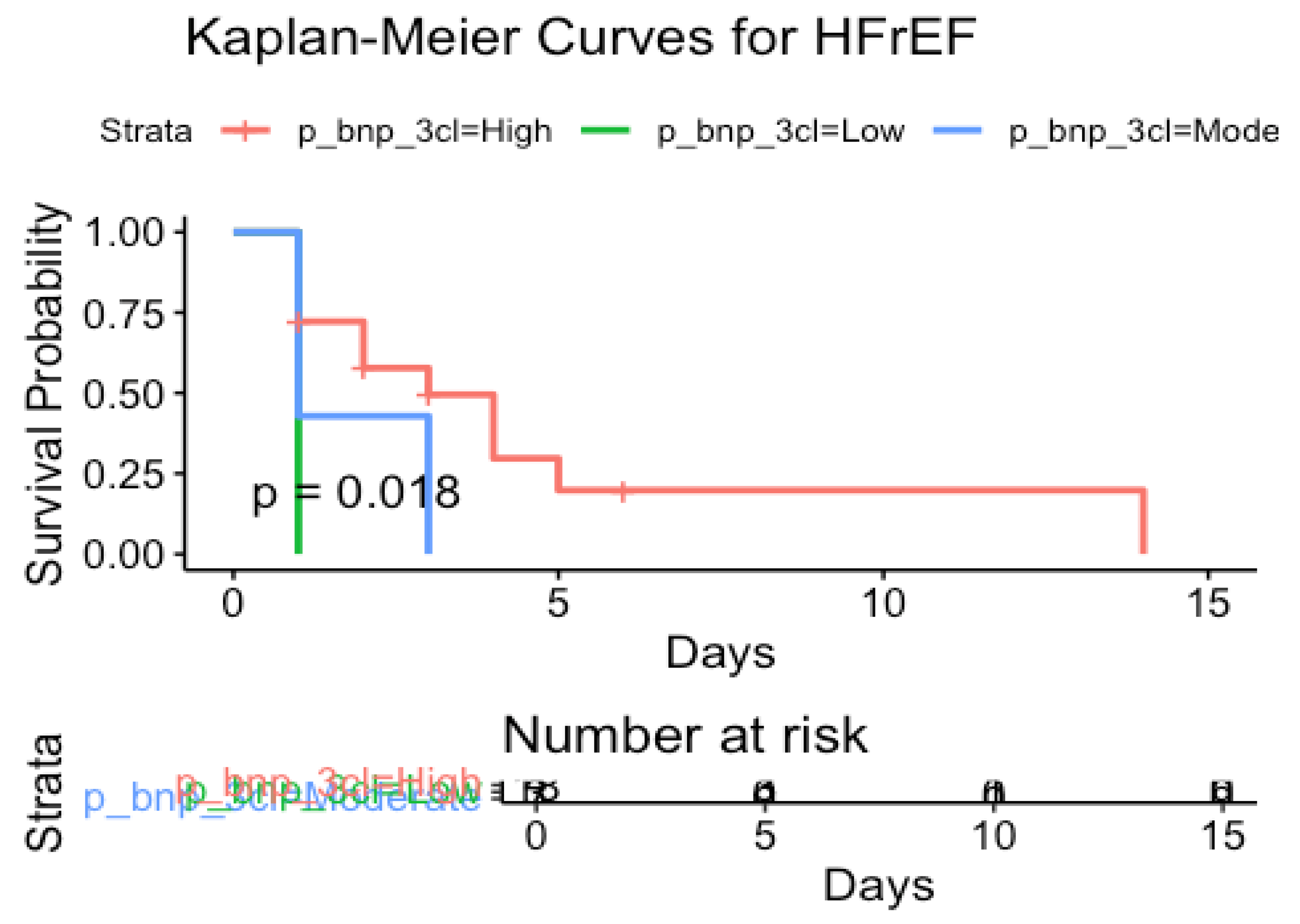
Kaplan–Meier curves with log-rank analysis were used to compare the cumulative incidence of the primary end point between the groups. (
Figure 7 and
Figure 8). Kaplan -Meier curves for both sub-cohorts demonstrated that survival probability gets low when the BNP levels are high.
P value for HFpEF cohort is 0.29 and P value for HFrEF cohort is 0.018.
The null hypothesis on this study is BNP could not be used as a prognostic indicator for elderly patients with heart failure. The significance level for this study is considered as 1. P values for both cohorts are less than significance level so that the null hypothesis is rejected.
4. Discussion and Conclusion
Summary of Main Findings
In this cohort study, two major heart failure cohorts were analyzed for specific end points under six main sub-cohorts. The data analysis shows that mortality rate is 29.1% when NT Pro BNP values is more than 2000. The heart failure readmission rate is 45.6% when NT Pro BNP value is more than 2000.
66.6% re-admission rate was demonstrated with rising NT-Pro BNP values during heart failure follow up. This was much lower with patients who had declining NT- Pro -BNP values during heart failure follow u which was 33.3%
Satisfactory statistical power of the study, which demonstrated that NT- Pro BNP can be used as prognostic marker for mortality in elderly patients with heart failure irrespective of their ejection fraction.
Limitations
The data collection was done randomly as snap shots of each month. Initial approach for data collection was tracing through patients who had inpatient echocardiography for heart failure, assuming all heart failure admissions have got an inpatient echo. During this selection process, smaller proportion of patients can be missed.
There are other factors that can cause for high NT Pro BNP values. The demographic characteristics were documented were included most of these and the results have been standardized. Inclusion of BMI, Serum creatinine levels and sepsis were not done for the data collection as it was challenging to access for these data set. We are hoping to carry out a separate study with an extensive analysis on this.
The mortality and re-admission records were analyzed to see the causes for mortality and readmissions. For some patients there were associated other causes for mortality which contributed similarly as heart failure. (Example – sepsis, AKI on CKD, Cardio renal syndrome). Most of the re-admissions were actual heart failure re-admissions. But minority of the patients were presented with respiratory conditions which exacerbated the existing heart failure (Example- Pneumonia, infective exacerbation of COPD). Associated other conditions alongside heart failure which contributes to the mortality and readmissions was an unavoidable limitation on this study.
The follow up was done up to 12 -15 weeks’ time. It would be ideal if follow up could be extended further.
Conclusion
NT Pro BNP can be used as a prognostic biomarker for elderly patients with heart failure. Satisfactory statistical evidence was shown on this study to prove that higher BNP values on admission predicts higher mortality rate. Significant evidence was demonstrated to show that there are higher re-admission rates with higher NT pro BNP levels specially in elderly population. Furthermore, the study demonstrated that, there is higher mortality and morbidity rate with rising NT Pro BNP levels during heart failure follow up. In conclusion all these three parameters shows that NT Pro- BNP levels can be used as a prognostic bio marker for elderly patients with heart failure, irrespective of their ejection fraction status. Furthermore, we would like to indicate that monitoring NT Pro BNP levels in all heart failure cases could be beneficial to prevent mortality and morbidity. Furthermore, it would be an aid to optimize heart failure medications prior to have an episode of decompensation of heart failure as well.
Institutional Review Board Statement
We confirm that ethical Committee approval was sought where necessary and is acknowledged by the team whenever needed.
Acknowledgments
We would like to acknowledge all our mentors and existing literature that aided to complete this study.
References
- Taylor CJ, Roalfe AK, Iles R, et al. The potential role of NT-proBNP in screening for and predicting prognosis in heart failure: a survival analysis. BMJ Open 2014, 4, e004675. [Google Scholar] [CrossRef]
- Salah K, Stienen S, Pinto YM, et al. Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction. Heart 2019, 105, 1182–1189. [Google Scholar]
- Charlotte Kragelund, M.D. Bjørn Grønning, M.D., Lars Køber, D.M.Sc., Per Hildebrandt, D.M.Sc., and Rolf Steffensen, M.D ;2005; N-Terminal Pro–B-Type Natriuretic Peptide and Long-Term Mortality in Stable Coronary Heart Disease. N Engl J Med 2005, 352, 666–675. [Google Scholar] [CrossRef]
- Zhang, B, Xu, H, Zhang, H. et al. Prognostic Value of N-Terminal Pro–B-Type Natriuretic Peptide in Elderly Patients With Valvular Heart Disease. JACC 2020, 75, 1659–1672. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).