1. Introduction
Evidence from both animal and human studies have shown that macro-hemodynamic targeted therapeutic approaches often fail to improve organ function and survival in critical situations [
1,
2]. In recent years, with advancements in technology, particularly in the field of direct imaging, there is an increasing body of evidence that microcirculation may represent a crucial target for hemodynamic resuscitation. This represents a shift from the traditional approach of hemodynamic resuscitation which has been focused on blood pressure and cardiac output in emergency and intensive care units. This review discusses the general characteristics of microcirculation, advances in microvascular imaging techniques, and its clinical relevance in several pathological states.
2. Importance of Microcirculation
The vascular components of the cardiovascular system constitute a networked structure within all organs, facilitating the transport of substances. The movement of blood through the smallest vessels of the network (vessels with a diameter of less than 100 μm, including arterioles, post-capillary venules, and capillaries) is referred to as microcirculation. The process of microcirculation permits the transfer of oxygen from the bloodstream to parenchymal cells via passive diffusion. The regulation of blood flow in the tissue is dependent upon the contraction and relaxation of smooth muscles in arterioles and precapillary sphincters, which are controlled through local and neural interactions. It is therefore evident that microcirculation fulfils its primary role of meeting local metabolic needs and removing waste products from the tissues [
3,
4]. Oxygen is transported in the blood in two forms: bound to hemoglobin in erythrocytes (as oxyhemoglobin) and dissolved in plasma. In areas where the partial pressure of oxygen (pO2) decreases due to dissolved oxygen, the affinity of hemoglobin for oxygen reduced, thereby facilitating the passage of oxygen through the capillary wall into the interstitium and subsequently into cells. Once inside the cell, oxygen is utilized in the electron transport chain within the inner mitochondrial membrane facilitating the production of adenosine 5′-triphosphate (ATP) through oxidative phosphorylation. It is therefore evident that microcirculation plays a pivotal role in ensuring ATP production by maintaining a consistent and adequate oxygen supply, and by regulating its levels in accordance with the cellular demand [
5].
3. Cellular Processes of Hemodynamic Coherence
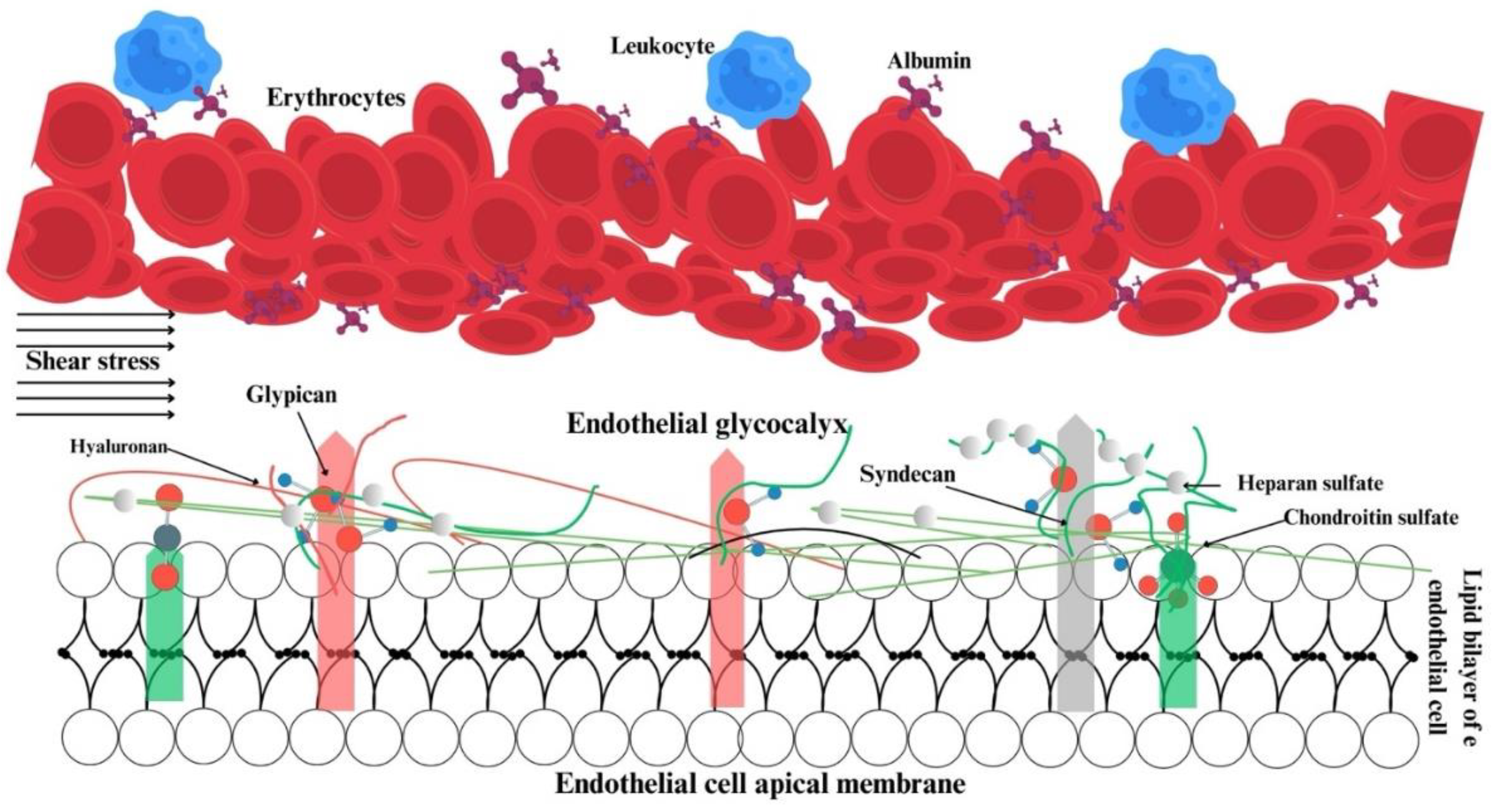
The maintenance of microcirculation and its distinction from macrohemodynamics are contingent upon physiological events occurring in and around the endothelium. Three key elements are responsible for the hemodynamic coherence: the glycocalyx, the endothelium, and erythrocytes (
Figure 1).
The glycocalyx is defined as a reticulated layer of membrane-bound proteoglycans and glycoproteins that surrounds the lumen-facing surface of the endothelium. Additionally, the glycocalyx contains a variety of substances, including antioxidants, growth factors, and anticoagulants, which are collected from plasma for use when necessary [
6,
7]. In physiological conditions, there is a state of equilibrium between the processes of glycocalyx synthesis and degradation. The degradation of the glycocalyx is facilitated by inflammatory processes, whereas optimal tissue perfusion is ensured by glycocalyx synthesis, which is promoted by shear stress [
8,
9]. The negatively charged glycocalyx structure of cell surface prevents blood and endothelial cells from contacting each other [
6]. Damage to the glycocalyx results in a reduction of a distance between erythrocytes and the endothelium, leading to disruption of microvascular perfusion [
10]. Furthermore, the glycocalyx plays a role in regulating the adhesion of leukocytes and erythrocytes to each other and to the endothelium [
6,
11] (
Figure 1).
Secondly, the endothelium itself, its junctional complexes, and the elements of the glycocalyx act as a selectively permeable barrier between the inside and outside of the vessel. This barrier permits the retention of plasma and large molecular-weight protein structures within the vessel [
12]. The regulation of capillary wall permeability is specifically provided by glycosaminoglycans, sialic acid, and proteins gathered from plasma within the glycocalyx structure [
6,
13]. While studies indicate that glycocalyx disruption may result in capillary leakage and that the extent of leakage is associated with the quantity of components shed from the glycocalyx [
14,
15,
16], recent studies suggest that the glycocalyx itself does not contribute to capillary permeability [
17,
18].
Furthermore, the glycocalyx serves to convey shear stress data generated by erythrocytes to the endothelium, thereby regulating vascular tone and endothelial function [
19]. Impairment of the glycocalyx has been demonstrated in numerous pathological conditions, including sepsis, septic shock, cardiogenic shock, and coronavirus disease 2019 COVID-19, as well as in surgical procedures such as cardiopulmonary bypass and transplantation. This is associated with a poor prognosis [
20,
21,
22,
23,
24,
25].
The endothelial layer in arterioles regulates microcirculation through the release of mediators that induce vascular contraction and relaxation, process that occur independently of the glycocalyx. This function is fulfilled through autocrine and paracrine interactions [
26,
27]. The endothelium not only processes local hemodynamic information but also plays a pivotal role in regulating hemostasis, ensuring unimpeded blood flows within the vessel. The process of hemostasis is regulated by molecules released from the endothelium, including von Willebrand factor (vWF), tissue factor (TF), and plasminogen activator inhibitor type 1 (PAI-1). During period of inflammation, the balanced between prothrombotic and antifibrinolytic processes can lead to microvascular occlusion, resulting in ischemia and subsequent multiple organ dysfunction syndrome (MODS) [
26,
28].
Proinflammatory cytokines play a pivotal role in the meditation of systemic inflammation. The endothelium responds to these cytokines in order to regulate its barrier function, vascular tone, and coagulation process. When activated by proinflammatory cytokines, the endothelial barrier is compromised, and the endothelium synthesizes specific molecules on its luminal surface, facilitating the adhesion of leukocytes and erythrocytes [
26,
29]. At this juncture, there is a notable degree of interdependence between the glycocalyx and the endothelium [
6,
7]. The weakened barrier results in tissue oedema, and the adherence of leukocytes to the endothelium causes obstructions in the microvascular beds [
28]. The presence of oedema and obstructions in the microcirculation can be readily identified using with imaging devices [
30,
31].
Lastly, erythrocytes, which have a diameter of approximately 7-8 μm in the absence of external forces, must undergo a deformation of their membranes in order to traverse capillaries during movement. This reversible deformation entails a transformation in geometric shape without any alteration in surface area, thereby enabling erythrocytes to traverse through capillaries with a diameter of 3-5 μm [
32]. A reduction of erythrocyte deformability has been demonstrated in numerous pathologies, including sepsis. A reduction of deformability results in increase in blood viscosity. The stiffening of cells impedes microvascular flow, and oxygenation is further impaired by the reduced affinity of hemoglobin for oxygen [
33]. The deformability of individual erythrocytes can be quantified using techniques such as micropipette aspiration, atomic force microscopy, and optical trapping. The deformability of groups of erythrocytes can be assessed using methods including quantitative phase imaging, filtration, microfluidic filtration, and laser diffractometry [
34]. A reduction of erythrocyte deformability has been linked to a decline in capillary density and survival in sepsis [
35,
36].
A number of processes can occur concurrently in critical illness, including a systemic inflammatory response, damage to the glycocalyx, endothelial dysfunction, endothelial activation, coagulation processes, and erythrocyte deformability problems. These processes, which occur in and around the endothelium, disrupt the relationship between the macro- and microenvironments, leading to a loss of coherence. The extent to which current therapeutic approaches can improve microcirculation through cellular processes remains a matter of debate.
4. Importance of Microcirculation in Shock
The term “shock” can be defined as the inadequate supply and utilization of oxygen in tissues, which significantly impacts microcirculation. Although hypotension is a crucial indicator of shock, the activation of the sympathetic nervous system often results in a masking of a drop in blood pressure. Furthermore, while the lower limit for systolic pressure is typically regarded as 90 mmHg, lower values may be considered normal due to inter-individual variability. Four distinct categories of shock have been identified: hypovolemic, cardiogenic, obstructive, and distributive shock. In hypovolemic, cardiogenic, and obstructive shock, cardiac output is low and the convection characteristics of microcirculation are weak. Conversely, in distributive shock, high cardiac output is typically observed in the early stages, with microcirculation redirected by inflammatory-oxidant mediators. It is possible for multiple types of shock to occur simultaneously, such as distributive-cardiogenic and hypovolemic-cardiogenic [
37].
The primary objective of resuscitation in all four types of shock is to enhance tissue perfusion and oxygenation. Macro-hemodynamic variables, such as blood pressure, are managed within a specific range with the assumption that this will improve hypoxia and hypoperfusion. Nevertheless, researches have demonstrated that pursuing macro-hemodynamic objectives does not invariably enhance oxygenation [
38], organ performance [
2], or survival [
39,
40,
41]. The damage to organs and fatalities observed during and after shock treatment are attributed to hemodynamic incoherence. In physiological conditions, improvements in microcirculation follow improvements in systemic hemodynamics, indicating a synergy between macro- and microcirculation. This is known as the haemodynamic coherence concept, and it leads to a correction of the shock [
42]. However, it has been demonstrated that microcirculatory improvement does not always follow systemic hemodynamic improvement [
43]. The loss of hemodynamic coherence has been shown to impair oxygenation by reducing tissue oxygen extraction. It has been established that hemodynamic incoherence is directly associated with four different types of microcirculatory changes, all of which can be monitored using direct imaging systems. These changes have been observed to uniformly show a decrease in capillary density and oxygen-carrying capacity.
Type 1: Sepsis is an example of a Type 1 alteration. In this type, there is a discrepancy in the flow of blood between different capillaries. Furthermore, even in vessels with a flow, there is a disparity in flow rate between them. This heterogeneous vascular flow exceeds the physiological limits, thereby affecting both the convection and diffusion characteristics of microcirculation. Consequently, the density of capillaries and the flow of microvasculature are both impaired in Type 1 alterations.
Type 2: The second type of alteration is observed in conditions such as fluid overload, which frequently occurs during bypass surgery. As a consequence of dilution, both the number of erythrocytes per unit blood volume and the space between them decrease. The diffusion characteristics of microcirculation are particularly affected.
Type 3: Vasoactive agents, such as noradrenaline, or increased venous pressure may result in a reduction or cessation of microvascular flow. In this type of change, the convection characteristics of microcirculation are affected.
Type 4: This type occurs when capillary leakage causes tissue oedema. Oedema can increase the diffusion distance between erythrocytes and cells, thereby affecting oxygen extraction (
Table 1) [
44].
5. Microcirculatory Changes in Sepsis
The term "sepsis" is used to describe organ dysfunction resulting from an uncontrolled host response to infection. If not promptly identified and treated, it can result in septic shock, multi-organ failure and mortality. Despite the administration of fluids in cases of septic shock, hypotension (defined as a mean arterial pressure of less than 65 mmHg) and perfusion disorder (defined as a lactate level exceeding 2 mmol/L) remain uncorrected [
45].
The microcirculation of patients with sepsis differs significantly from that of healthy individuals and even non-septic ICU patients, with a notable redirection of microcirculatory flow [
46]. Leukocyte and platelet-induced obstructions resulting from endothelial dysfunction lead to redirection of blood flow. The increased diffusion distance caused by shunted microcirculation reduces oxygen consumption [
47].
Decreased perfusing capillaries and increased flow heterogeneity are hallmarks of sepsis. These changes are more pronounced in non-survivors than in survivors, and improve over time in survivors. Changes in microcirculation are independent predictors of mortality in septic patients [
48].
The phenomenon of microcirculatory heterogeneity permits oxygen to gain access to the venous system prior to utilisation, which in turn affects the extraction of oxygen from tissues. In addition to microcirculatory heterogeneity, decreased functional density and slowed erythrocyte velocity are observed in sepsis [
49].
While erythrocyte velocity may be similar in survivors and non-survivors, but perfused capillary density and heterogeneity are prominent in non-survivors. Variables determining oxygen diffusion are more related to the sepsis picture than erythrocyte velocity, which directly determines convection [
50].
The inflammatory process and systemic vasodilation caused by mediators released in sepsis create a hypovolemic-like situation [
51]. Although fluid resuscitation is the initial step in improving macro-hemodynamic variables in sepsis and septic shock, there is still debate regarding the optimal type of fluid and the appropriate volume to administer. Furthermore, disturbances in microcirculation and an inadequate of response to resuscitation are directly correlated to survival outcomes. Nevertheless, fluid administration can increase blood flow by enhancing cardiac output and thus the propulsive power of the blood, thereby fulfilling the convective component of oxygen transport. Conversely, the administration of substantial quantities of fluid may result in the elevation of oxidant mediators within the vessel, leading to the disruption of endothelial integrity and damage of surface elements. In this context, oedema may ensue as intravascular fluid leaks into the interstitial space. The formation of oedema can be attributed to either the direct effect of the fluid or the disruption of cell-cell connections and surface elements, which is a consequence of the nature of sepsis itself. The presence of oedema may result in a reduction in blood flow, due to the creation of pressure within the perivascular space and an increase in the distance between capillaries and cells. This can lead to a limitation in the efficiency of gas exchange. Consequently, both convection and diffusion are impaired, but macrohemodynamics may remain within acceptable physiological limits, a condition known as hemodynamic incoherence [
52,
53].
6. Microcirculatory Changes in Cardiac Surgery
Cardiopulmonary bypass surgery has a significant impact on the body’s hemodynamic and biochemical processes. During extracorporeal circulation, systemic hemodynamics are maintained within desired ranges, although there is a decrease in oxygen delivery and hemoglobin concentration. Additionally, the density of perfused capillaries decreases. These alterations in microcirculation are accompanied by an increased in hemoglobin oxygen saturation and erythrocyte velocity at the capillary level, resulting from impaired oxygen extraction [
34]. The administration of blood transfusions following surgical procedures has been demonstrated to enhance capillary density and hemoglobin levels in the absence of increase in microvascular flow. This occurs independently of haemodynamic and volume status, thereby improving oxygen delivery [
35]. Furthermore, reducing the size of the external pump may also prevent microvascular hypoperfusion [
35]. However, the pulsatile nature of the pump [
54] and the composition of the inner lining material of the cannula circuit [
55] do not influence microvascular capillary density or perfusion impairment during surgical procedures.
Contact of blood with the foreign surface during cardiopulmonary bypass surgery induces a systemic inflammatory response, affecting all levels from systemic to subcellular [
56,
57]. The presence of elevated cytokine levels in the blood and visualization of leukocytes adhering directly to the endothelium [
58] and microaggregates in capillaries [
59] serve to illustrate the inflammatory process. The presence of microaggregates in the postoperative period may be an indicator of an increased risk of stroke [
59].
Cardiac surgery can be performed without using a cardiopulmonary bypass circuit, which has the effect of reducing cardiac output directly. A reduction in cardiac output affects microvascular flow, impacting all variables related to convection. While pump use has been shown to decrease microvascular haematocrit and blood viscosity, these variables remain unaffected in non-pump surgery [
34,
60].
Acute microcirculatory deterioration following bypass surgery is observed until the third day post-surgery, accompanied by glycocalyx damage. Targeted therapeutic approaches to the delayed glycocalyx repair process may improve postoperative outcomes [
24].
7. Microcirculatory Changes in Coronavirus Disease 2019 (COVID-19)
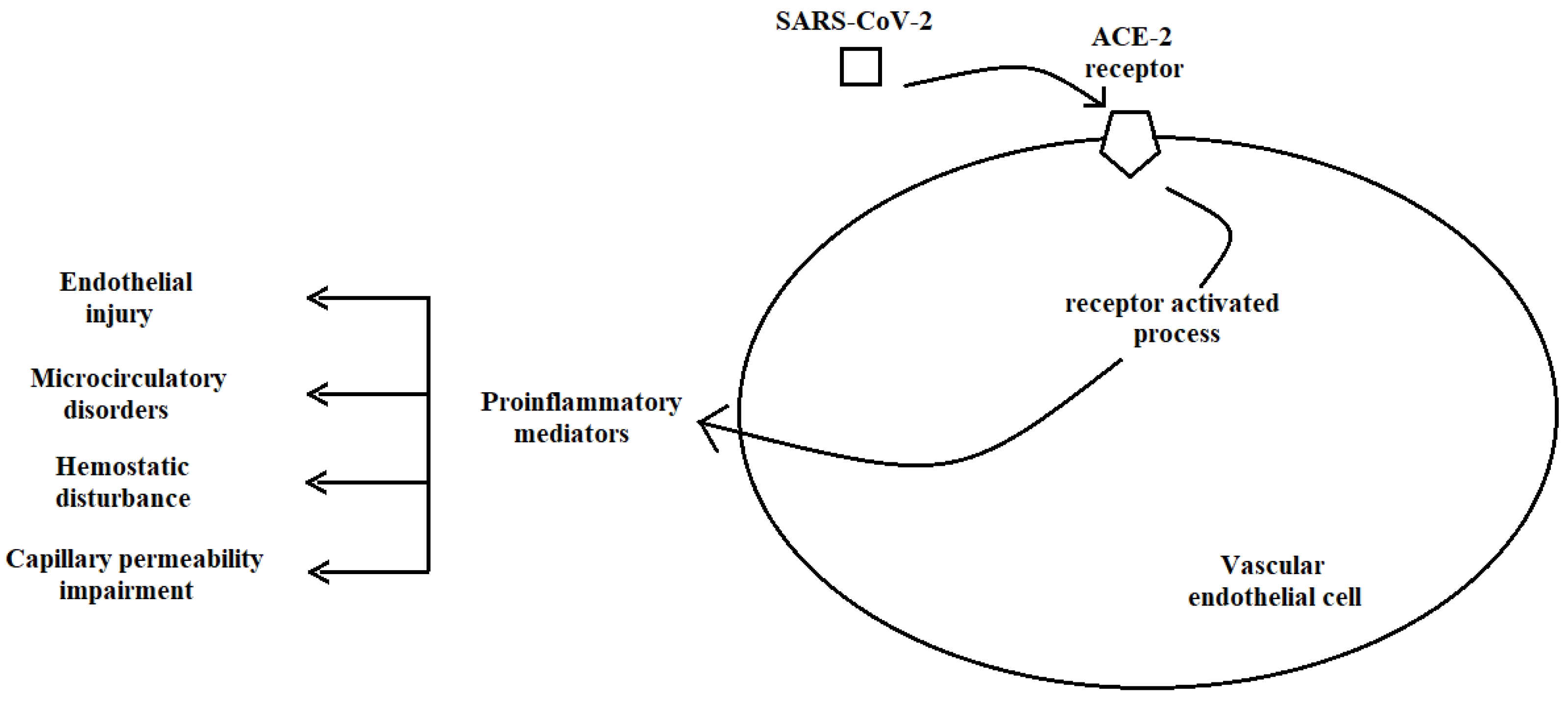
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the strain of the coronavirus responsible for the respiratory illness known as Coronavirus Disease 2019 (Covid-19), which triggered the global pandemic. The initial identification of the virus in Wuhan, China, was followed by a rapid global dissemination [
61]. Given its propensity for transmission, SARS-CoV-2 gains entry to vascular endothelial cells via the angiotensin-converting enzyme (ACE) 2 receptor [
62]. Activation of the ACE-2 receptor results in a significant release of pro-inflammatory mediators, collectively termed "cytokine storms," which contribute to endothelial damage [
63]. Endothelial dysfunction presents in a variety of ways, including impaired capillary permeability and disturbances in hemostasis [
64] (
Figure 2).
The presence of microvascular thrombosis is prominent feature observed in microcirculatory images of patients diagnosed with COVID-19 [
65]. It is possible that this thrombosis contributes to the underlying oxygen delivery deficiencies observed in patients with COVID-19. The resolution of thrombosis is a prerequisite for the management of conditions associated with SARS-CoV-2, such as acute respiratory distress syndrome (ARDS) and myocardial damage [
63,
66].
In patients with COVID-19, despite blood pressure values within the normal ranges, there may be a high heart rate, slightly elevated lactate levels, low systemic hemoglobin, and decreased hematocrit values [
67]. It is noteworthy that perfused vessel density, erythrocyte velocity, and capillary hematocrit levels are elevated in the microcirculation of these patients. The elevated capillary hematocrit results from capillary plasma leakage due to vascular barrier dysfunction caused by endothelial and glycocalyx damage, despite a reduction in systemic hematocrit [
68].
The microcirculatory characteristics observed in patients with coronavirus disease 2019 (COVID-19) differ from those observed in patients with sepsis. While microcirculation in sepsis and septic shock typically exhibits heterogeneity with reduced vascular density and impaired flow [
46,
69], patients with coronavirus disease 2019 (Covid-19) display a non-heterogeneous microcirculation [
70]. Furthermore, reductions in functional capillary density may not be observed in patients with Covid-19 [
48,
71,
72]. The pathophysiology of Covid-19 differs from that of other viral infections [
73].
The maintenance of functional capillaries in patients with COVID-19 represents a compensatory mechanism that increases oxygen extraction in response to hypoxia induced by hyperinflammation and hypercoagulation [
67]. Nevertheless, in patients with severe SARS-CoV-2 infection and high Sequential Organ Failure Assessment (SOFA) scores, characterized by increased leukocytes and microaggregates in the microcirculation, this compensatory mechanism may prove ineffective [
67]. Mechanical ventilation has been observed to increase erythrocyte velocity in patients with COVID-19 [
72]. However, the impact of mechanical ventilation on diffusion distance against increased erythrocyte velocity remains unknown. Additionally, various studies have reported high vascular densities in the sublingual microcirculation of patients with confirmed or suspected cases of SARS-CoV-2 infection, alongside decreases in perfused vessels and flow velocity [
74]. Notwithstanding the absence of a global pandemic caused by the SARS-CoV-2 virus, comprehensive and large-scale studies of microcirculatory changes in patients diagnosed with the disease will facilitate a deeper understanding of the nature of viral pandemics derived from SARS-CoV-2 and inform the development of more effective prevention and treatment strategies in the future.
8. Assessment and Visualization of Microcirculation
The intricate processes occurring in microcirculation are currently only elucidated at the research level, employing imaging techniques that are not yet integrated into routine clinical practice. Nevertheless, to some extent, the microenvironment is in fact assessed in the clinical setting. For instance, the color of the skin color can provide some indication of the state of microcirculation in the skin. In addition to color changes, the skin blood supply can be estimated by measuring temperature or capillary refill time. A reduction in skin temperature in surgical patients has been linked to low cardiac output, low central venous oxygen saturation, and elevated lactate levels [
75]. The measurement of capillary refill time is a straightforward method that has been linked to blood lactate levels, the Sequential Organ Failure Assessment (SOFA) score, and survival in patients with sepsis. However, inter-clinician variability in assessment could potentially impact the results. Despite impaired skin microcirculation in conditions such as hypertension and renal failure, the relationship between skin and systemic circulation remains poorly understood [
76,
77]
The measurement of blood lactate levels represents a widely utilised biochemical approach for the evaluation of disruptions in microcirculation. Lactate levels above 2 mM indicate the presence of shock, and even minor fluctuations in lactate levels are associated with direct correlations with survival rates [
78]. It should be noted that although lactate is a product of anaerobic metabolism, exogenous catecholamines or decreased hepatic clearance may also cause an increase in lactate levels [
79]. Moreover, lactate levels might not increase even if oxygenation is poor and blood pressure is within normal limits [
1]. Therefore, it cannot be assumed that evaluating microcirculation based solely on blood lactate levels is a reliable method.
Near-infrared spectroscopy (NIRS) devices are capable of measuring oxygenation at the microcirculatory level. However, it is important to note that the technique has significant limitations when it comes to evaluating microcirculation. A significant challenge is the inability of these devices to provide the requisite detailed spatial resolution for the accurate assessment of microvascular structures. NIRS primarily measures changes in oxygenated and deoxygenated haemoglobin within capillaries, arterioles and venules. Furthermore, NIRS signals are frequently affected by the absorption and scattering of light in diverse tissue layers, rendering it challenging to discern the precise impact of microcirculatory blood flow from the overall tissue oxygenation. This limitation is particularly problematic in heterogeneous tissues, where multiple layers of blood vessels and different tissue types may contribute to the signal, thereby complicating the interpretation of microcirculatory dynamics. Furthermore, NIRS does not provide direct information on red blood cell velocity, capillary density, or microvascular perfusion heterogeneity, which are crucial parameters for a comprehensive assessment of microcirculation [
80,
81].
Retinal vessel diameter (RVD) measurement is a technique used to evaluate the diameters of arteries and veins in the retina. While it provides valuable information about the structure and function of the retinal vasculature, RVD has also significant limitations when it comes to assessing microcirculation. Firstly, RVD measurements typically focus on larger and medium-sized vessels, which do not provide direct information about the microcirculation's smallest components, such as capillaries. Therefore, RVD measurements do not adequately reflect changes or dysfunctions in the microcirculation. Additionally, RVD measurements are designed to assess structural and geometric changes in retinal arterioles and venules, but they do not measure the functional dynamics of microcirculation, such as blood flow rates, oxygenation status, or microvascular reactivity. And, RVD measurements lack the ability to distinguish whether observed changes occur at the microcirculatory level or in the larger vascular network. For example, observed changes such as arteriolar narrowing or venular dilation may not be a direct result of pathological processes occurring in the microcirculation, potentially leading to misleading conclusions about the state of the microcirculation [
82,
83].
A variety of imaging devices can be employed to ascertain information regarding tissue perfusion. Laser Doppler, laser speckle contrast, and photoacoustic imaging systems represent non-invasive imaging techniques. The acquisition of real-time images is achieved through the alteration of the optical properties of the transmitted light subsequent to the excitation of the tissue or by the absorption of light by the tissue. While these devices may be suitable for skin imaging in terms of ergonomics, they are not practical for other parts of the body [
84,
85]. Furthermore, these devices provide information about convection properties of microcirculation, which is a significant factor influencing oxygen transport. However, these techniques are non-quantitative, provide only percentage change information, are affected by individual differences, and, more importantly, are unable to provide diffusion-related information in microcirculation. The transport of oxygen to the tissue is determined by two processes: convection and diffusion. In other words, for the tissue to receive oxygen, it must pass at a certain speed from a location in close proximity to the cell. It is therefore evident that in order to evaluate the oxygen transport capacity of the microcirculation, both microvascular flow (convection) and capillary distance (diffusion) information are required. In order to achieve this, it is necessary to conduct direct visualization of the microcirculation [
3]. The direct imaging of microcirculation without the use of any dye has been a viable technique in clinical research for the past 25 years. For the first time, microcirculation was imaged at the bedside in humans using orthogonal polarization spectral (OPS) technology. Subsequently, technological advancements led to the development of two subsequent generations of devices using dark field microscopy: initially the Sidestream Dark Field (SDF) and subsequently the Incident Dark Field (IDF) approach. All three generations of devices are based on the principle that hemoglobin becomes visible by absorbing green light. In the images, microvessels can be easily visualized, and the velocity of small vessels and their quantity in the region of interest can be determined. Consequently, the second component of oxygen transport namely diffusion information, can also be obtained [
86,
87].
The sublingual region has typically been evaluated with imaging devices. Microvessels are identified according to their flow and branching direction. Despite the sublingual region’s distance from the heart and other organs, it is a well-defined area for understanding pathophysiology and treatment efficacy [
49,
88]. In addition to the sublingual region, other areas have been imaged, including as the vagina [
89], colon [
90], skin [
91], rectum [
92], labia [
93], conjunctiva [
94], brain [
95], and peritoneum [
96].
A novel system has recently been developed for the simultaneous assessment of microvascular oxygen saturation and microcirculatory variables. This system maps oxygen saturation in the microcirculation based on the principle that oxyhemoglobin absorbs blue light. It has been demonstrated that there is a correlation between the inspired oxygen fraction (FiO2) and microvascular saturation and that local saturation changes were associated with changes in the microcirculation [
97].
9. Variables Obtained from Microcirculation Images
The rise in sublingual microcirculation studies has enabled the acquisition of a multitude of variables. A consensus was reached at meeting in 2007 and 2018 regarding the variables related to capillary density, perfusion, and erythrocyte flow behaviour [
98,
99]. While the initial approach was predominantly based on manual measurements, more recently, novel variables have been proposed that calculated using computer software [
100]. These variables in question are now out lined as follows:
Microvascular Flow Index (MFI): The MFI provides information regarding the quality of perfusion in the region of interest. The video image is hypothetically divided into four parts, with each part assigned a value between 0 and 3 according to the observed flow type. The MFI value is presented as the mean without units (with 0 indicating no flow; 1 indicating intermittent flow; 2 indicating slow flow; 3 indicating continuous flow).
Total Vessel Density (mm/mm²) (TVD): The TVD is calculated as the total length of vessels divided by the total surface area of the region of interest. This provides information about the vessel density in the region.
Perfused Vessel Density (mm/mm²) (FCD): The FCD is calculated as the total perfused vessel length divided by the total surface area. This variable provides information about functional vessel density.
Proportion of Perfused Vessels (%) (PPV): The PPV is calculated as the number of perfused vessels per hundred divided by the total number of vessels and provides information about perfusion quality.
Flow Heterogeneity Index (FHI): This provides information about perfusion heterogeneity. The calculation is performed by dividing the difference between the highest microvascular flow and the lowest microvascular flow indices by the mean microvascular flow index.
Erythrocyte Velocity (mm/s) (RBCv): This is the weighted average of the absolute erythrocyte velocity in all capillary segments within the field of view. It provides quantitative information as a determinant of the convection capacity of the microcirculation.
Density Distribution Between Capillaries (#RBCv): It is a variable that gives the density distribution of erythrocyte velocity at the level of individual capillaries. The heterogeneity of capillary perfusion provides in-depth information about the pathophysiological state of the microcirculation. It can be calculated with software.
Capillary Hematocrit (cHct): The weighted average of the ratio of whole blood volume to erythrocyte volume in all capillary segments within the field of view. It can be calculated with software. It corresponds to the distribution of erythrocytes within the boundaries of capillaries and represents the microcirculatory diffusion capacity.
Hematocrit Discharge (#dHct): The weighted average of the product of the integral over time of the linear displacement of erythrocytes and capillary hematocrit divided by the capillary segment length and the field of view. It represents the displacement of capillary hematocrit as the ratio between erythrocyte volume and blood volume per unit time.
Tissue Erythrocyte Perfusion (tRBCp): The linear displacement of erythrocytes, the weighted average of the integral over time of capillary segment whole blood volume and capillary hematocrit (capillary segment length) divided by the field of view. Tissue perfusion with red blood cells is the most representative measure of tissue perfusion in a clinical and physiologic context [
98,
99,
100].
10. Conclusion
The direct visualisation of the microcirculation without the use of dyes has been possible for approximately 25 years within the advent of handheld microcirculatory imaging devices. In recent years, there has been a notable surge in interest in microcirculation, which has become a subject of investigation across various disciplines. The capacity to directly observe and quantify microcirculatory function at the bedside with the aid of handheld vital microscopes enables the translation of findings from basic research, ultimately benefiting patients. Furthermore, given that the shortcomings of macro-hemodynamic targets remain a topic of contention, the monitoring of microcirculation is of particular importance in order to minimise fluid administration and to avoid the use of unnecessary medications.
In other words, when a microcirculation-guided therapeutic approach addresses the root causes of critical illnesses, physicians will be able to discern how endothelial and microvascular dysfunction not only contribute to organ damage but also impede treatment strategies in complex illness conditions.
However, on the other side of the coin, the situation is somewhat different in the real world. Despite the considerable interest in microcirculation, the imaging of microcirculation and the evaluation of events remain outside the scope of routine clinical practice. The primary reason for this is that the data obtained from imaging techniques exclusively pertains to the oxygen-carrying capacity of the blood at the tissue level. However, the most significant shortcoming is the lack of assessment of the actual oxygen saturation levels in the blood that reach the cells through microcirculation and the cellular energy metabolism in this region. In broader terms, the viability of cells can be evaluated by determining the proportion of oxygen delivered to the patient that is delivered to the cells and the ability of these cells to utilize the oxygen supplied. The development of microcirculation imaging technologies in this direction may enable a reassessment of traditional treatment methods in pathological conditions related to emergency medicine, intensive care, surgery, and internal medicine.
Author Contributions
Conceptualization, UA, BYA, NG; writing, UA, BYA. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
None-applicable.
Informed Consent Statement
None-applicable.
Acknowledgments
The authors are grateful to Muzaffer Utku Cakir who drew Figure 1.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Aksu, U.; Bezemer, R.; Yavuz, B.; Kandil, A.; Demirci, C.; Ince, C. Balanced vs unbalanced crystalloid resuscitation in a near-fatal model of hemorrhagic shock and the effects on renal oxygenation, oxidative stress, and inflammation. Resuscitation. 2012 Jun;83(6):767-73. [CrossRef]
- den Uil, CA.; Lagrand, WK.; van der Ent, M.; Nieman, K.; Struijs, A.; Jewbali, LS.; Constantinescu, AA.; Spronk, PE.; Simoons, ML. Conventional hemodynamic resuscitation may fail to optimize tissue perfusion: an observational study on the effects of dobutamine, enoximone, and norepinephrine in patients with acute myocardial infarction complicated by cardiogenic shock. PLoS One. 2014 Aug 1;9(8):e103978. [CrossRef]
- Guven, G.; Hilty, MP.; Ince, C. Microcirculation: Physiology, Pathophysiology, and Clinical Application. Blood Purif. 2020;49(1-2):143-150. [CrossRef]
- Klijn, E.; Den Uil, CA.; Bakker, J.; Ince, C. The heterogeneity of the microcirculation in critical illness. Clin Chest Med. 2008 Dec;29(4):643-54, viii. [CrossRef]
- Mik, EG. Special article: measuring mitochondrial oxygen tension: from basic principles to application in humans. Anesth Analg. 2013 Oct;117(4):834-46. [CrossRef]
- Villalba, N.; Baby, S.; Yuan, SY. The Endothelial glycocalyx as a double-edged sword in microvascular homeostasis and pathogenesis. Front Cell Dev Biol. 2021 Jul 14;9:711003. [CrossRef]
- Kolářová, H.; Ambrůzová, B.; Svihálková Šindlerová, L.; Klinke, A.; Kubala, L. Modulation of endothelial glycocalyx structure under inflammatory conditions. Mediators Inflamm. 2014;2014:694312. [CrossRef]
- Arisaka, T.; Mitsumata, M.; Kawasumi, M.; Tohjima, T.; Hirose, S.; Yoshida, Y. Effects of shear stress on glycosaminoglycan synthesis in vascular endothelial cells. Ann N Y Acad Sci. 1995 Jan 17;748:543-54. [CrossRef]
- Mulivor, AW.; Lipowsky, HH. Inflammation- and ischemia-induced shedding of venular glycocalyx. Am J Physiol Heart Circ Physiol. 2004 May;286(5):H1672-80. [CrossRef]
- Lee, DH.; Dane, MJ.; van den Berg, BM.; Boels, MG.; van Teeffelen, JW.; de Mutsert, R.; den Heijer, M.; Rosendaal, FR.; van der Vlag, J.; van Zonneveld, AJ.; et al. Deeper penetration of erythrocytes into the endothelial glycocalyx is associated with impaired microvascular perfusion. PLoS One. 2014 May 9;9(5):e96477. [CrossRef]
- Nishiguchi, E.; Okubo, K.; Nakamura, S. Adhesion of human red blood cells and surface charge of the membrane. Cell Struct Funct. 1998 Jun;23(3):143-52. [CrossRef]
- Myburgh, JA.; Mythen, MG. Resuscitation fluids. N Engl J Med. 2013 Sep 26;369(13):1243-51. [CrossRef]
- Cioffi, DL.; Pandey, S.; Alvarez, DF.; Cioffi, EA. Terminal sialic acids are an important determinant of pulmonary endothelial barrier integrity. Am J Physiol Lung Cell Mol Physiol. 2012 May 15;302(10):L1067-77. [CrossRef]
- Tang, TH.; Alonso, S.; Ng, LF.; Thein, TL.; Pang, VJ.; Leo, YS.; Lye, DC.; Yeo, TW. Increased serum hyaluronic acid and heparan sulfate in dengue fever: Association with plasma leakage and disease severity. Sci Rep. 2017 Apr 10;7:46191. [CrossRef]
- Suwarto, S.; Sasmono, RT.; Sinto, R.; Ibrahim, E.; Suryamin, M. Association of endothelial glycocalyx and tight and adherens junctions with severity of plasma leakage in dengue infection. J Infect Dis. 2017 Mar 15;215(6):992-999. [CrossRef]
- Lam, PK.; McBride, A.; Le, DHT.; Huynh, TT.; Vink, H.; Wills, B.; Yacoub, S. Visual and biochemical evidence of glycocalyx disruption in human dengue infection, and association with plasma leakage severity. Front Med (Lausanne). 2020 Oct 16;7:545813. [CrossRef]
- Guerci, P.; Ergin, B.; Uz, Z.; Ince, Y.; Westphal, M.; Heger, M.; Ince, C. Glycocalyx degradation is independent of vascular barrier permeability increase in nontraumatic hemorrhagic shock in rats. Anesth Analg. 2019 Aug;129(2):598-607. [CrossRef]
- Ergin, B.; Guerci, P.; Uz, Z.; Westphal, M.; Ince, Y.; Hilty, M.; Ince, C. Hemodilution causes glycocalyx shedding without affecting vascular endothelial barrier permeability in rats. J Clin Transl Res. 2020 May 12;5(5):243-252.
- Mochizuki, S.; Vink, H.; Hiramatsu, O.; Kajita, T.; Shigeto, F.; Spaan, JA.; Kajiya, F. Role of hyaluronic acid glycosaminoglycans in shear-induced endothelium-derived nitric oxide release. Am J Physiol Heart Circ Physiol. 2003 Aug;285(2):H722-6. [CrossRef]
- Saoraya, J.; Wongsamita, L.; Srisawat, N.; Musikatavorn, K. Plasma syndecan-1 is associated with fluid requirements and clinical outcomes in emergency department patients with sepsis. Am J Emerg Med. 2021 Jan 15;42:83-89. [CrossRef]
- Schmidt, EP.; Overdier, KH.; Sun, X.; Lin, L.; Liu, X.; Yang, Y.; Ammons, LA.; Hiller, TD.; Suflita, MA.; Yu, Y.; et al. Urinary glycosaminoglycans predict outcomes in septic shock and acute respiratory distress syndrome. Am J Respir Crit Care Med. 2016 Aug 15;194(4):439-49. [CrossRef]
- Jung, C.; Fuernau, G.; Muench, P.; Desch, S.; Eitel, I.; Schuler, G.; Adams, V.; Figulla, HR.; Thiele, H. Impairment of the endothelial glycocalyx in cardiogenic shock and its prognostic relevance. Shock. 2015 May;43(5):450-5. [CrossRef]
- Yamaoka-Tojo, M. Endothelial glycocalyx damage as a systemic inflammatory microvascular endotheliopathy in COVID-19. Biomed J. 2020 Oct;43(5):399-413. [CrossRef]
- Wu, Q.; Gao, W.; Zhou, J.; He, G.; Ye, J.; Fang, F.; Luo, J.; Wang, M.; Xu, H.; Wang, W. Correlation between acute degradation of the endothelial glycocalyx and microcirculation dysfunction during cardiopulmonary bypass in cardiac surgery. Microvasc Res. 2019 Jul;124:37-42. [CrossRef]
- Rancan, L.; Simón, C.; Sánchez Pedrosa, G.; Aymonnier, K.; Shahani, PM.; Casanova, J.; Muñoz, C.; Garutti, I.; Vara, E. Glycocalyx degradation after pulmonary transplantation surgery. Eur Surg Res. 2018;59(3-4):115-125. [CrossRef]
- Galley, HF.; Webster, NR. Physiology of the endothelium. Br J Anaesth. 2004 Jul;93(1):105-13. [CrossRef]
- Juffermans NP.; van den Brom CE.; Kleinveld DJB. Targeting endothelial dysfunction in acute critical illness to reduce organ failure. Anesth Analg. 2020 Dec;131(6):1708-1720. [CrossRef]
- Ten Tusscher B.; Gudden C.; van Vliet S.; Smit B.; Ince C.; Boerma EC.; de Grooth HS.; Elbers PWG. Focus on focus: lack of coherence between systemic and microvascular indices of oedema formation. Anaesthesiol Intensive Ther. 2017;49(5):350-357. [CrossRef]
- Uz, Z.; Ince, C.; Shen, L.; Ergin, B.; van Gulik, TM. Real-time observation of microcirculatory leukocytes in patients undergoing major liver resection. Sci Rep. 2021 Feb 25;11(1):4563. [CrossRef]
- Bateman, RM.; Sharpe, MD.; Singer, M.; Ellis, CG. The Effect of sepsis on the erythrocyte. Int J Mol Sci. 2017 Sep 8;18(9):1932. [CrossRef]
- Kim, J.; Lee, H.; Shin, S. Advances in the measurement of red blood cell deformability: A brief review. J Cell Biotechn. 2015; 1, 63–79. [CrossRef]
- Bateman, RM.; Jagger, JE.; Sharpe, MD.; Ellsworth, ML.; Mehta, S.; Ellis, CG. Erythrocyte deformability is a nitric oxide-mediated factor in decreased capillary density during sepsis. Am J Physiol Heart Circ Physiol. 2001 Jun;280(6):H2848-56. [CrossRef]
- Donadello, K.; Piagnerelli, M.; Reggiori, G.; Gottin, L.; Scolletta, S.; Occhipinti, G.; Zouaoui Boudjeltia, K.; Vincent, JL. Reduced red blood cell deformability over time is associated with a poor outcome in septic patients. Microvasc Res. 2015 Sep;101:8-14. [CrossRef]
- Atasever, B.; Boer, C.; Goedhart, P.; Biervliet, J.; Seyffert, J.; Speekenbrink, R.; Schwarte, L.; de Mol, B.; Ince, C. Distinct alterations in sublingual microcirculatory blood flow and hemoglobin oxygenation in on-pump and off-pump coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2011 Oct;25(5):784-90. [CrossRef]
- Atasever, B.; van der Kuil, M.; Boer, C.; Vonk, A.; Schwarte, L.; Girbes, AR.; Ince, C.; Beishuizen, A.; Groeneveld, AB. Red blood cell transfusion compared with gelatin solution and no infusion after cardiac surgery: effect on microvascular perfusion, vascular density, hemoglobin, and oxygen saturation. Transfusion. 2012 Nov;52(11):2452-8. [CrossRef]
- Yuruk, K.; Bezemer, R.; Euser, M.; Milstein, DM.; de Geus, HH.; Scholten, EW.; de Mol, BA.; Ince, C. The effects of conventional extracorporeal circulation versus miniaturized extracorporeal circulation on microcirculation during cardiopulmonary bypass-assisted coronary artery bypass graft surgery. Interact Cardiovasc Thorac Surg. 2012 Sep;15(3):364-70. [CrossRef]
- Vincent, JL.; Ince, C.; Bakker, J. Clinical review: Circulatory shock - an update: a tribute to Professor Max Harry Weil. Crit Care. 2012, 16, 239. [Google Scholar] [CrossRef] [PubMed]
- Legrand, M.; Mik, EG.; Balestra, GM.; Lutter, R.; Pirracchio, R.; Payen, D.; Ince, C. Fluid resuscitation does not improve renal oxygenation during hemorrhagic shock in rats. Anesthesiology. 2010 Jan;112(1):119-27. [CrossRef]
- Yealy, DM.; Kellum, JA.; Huang, DT.; Barnato, AE.; Weissfeld, LA.; Pike, F.; Terndrup, T.; Wang, HE.; Hou, PC.; LoVecchio, F.; et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014 May 1;370(18):1683-93. [CrossRef]
- Pearse, RM.; Harrison, DA.; MacDonald, N.; Gillies, MA.; Blunt, M.; Ackland, G.; Grocott, MP.; Ahern, A.; Griggs, K.; Scott, R.; et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA. 2014 Jun 4;311(21):2181-90. [CrossRef]
- Boyd, JH.; Forbes, J.; Nakada, TA.; Walley, KR.; Russell, JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011 Feb;39(2):259-65. [CrossRef]
- Ince, C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19 Suppl 3(Suppl 3):S8. [CrossRef] [PubMed]
- Tachon, G.; Harrois, A.; Tanaka, S.; Kato, H.; Huet, O.; Pottecher, J.; Vicaut, E.; Duranteau, J. Microcirculatory alterations in traumatic hemorrhagic shock. Crit Care Med. 2014 Jun;42(6):1433-41. [CrossRef]
- Bakker, J.; Ince, C. Monitoring coherence between the macro and microcirculation in septic shock. Curr Opin Crit Care. 2020 Jun;26(3):267-272. [CrossRef]
- Levy, MM.; Evans, LE.; Rhodes, A. The Surviving Sepsis Campaign Bundle: 2018 update. Intensive Care Med. 2018 Jun;44(6):925-928. [CrossRef]
- De Backer, D.; Creteur, J.; Preiser, JC.; Dubois, MJ.; Vincent, JL. Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med. 2002; 166: 98–104.
- Ince, C. The microcirculation is the motor of sepsis. Crit Care. 2005;9(Suppl 4). [CrossRef]
- De Backer, D.; Donadello, K.; Sakr, Y.; Ospina-Tascon, G.; Salgado, D.; Scolletta, S.; Vincent, JL. Microcirculatory alterations in patients with severe sepsis: impact of time of assessment and relationship with outcome. Crit Care Med. 2013 Mar;41(3):791-9. [CrossRef]
- Verdant, CL.; De Backer, D.; Bruhn, A.; Clausi, CM.; Su, F.; Wang, Z.; Rodriguez, H.; Pries, AR.; Vincent, JL. Evaluation of sublingual and gut mucosal microcirculation in sepsis: a quantitative analysis. Crit Care Med. 2009 Nov;37(11):2875-81. [CrossRef]
- Sakr, Y.; Dubois, MJ.; De Backer, D.; Creteur, J.; Vincent, JL. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2004 Sep;32(9):1825-31. [CrossRef]
- Seitz, KP.; Qian, ET.; Semler, MW. Intravenous fluid therapy in sepsis. Nutr Clin Pract Off Publ Am Soc Parenter Enter Nutr. 2022 Oct;37(5):990–1003.
- Kanoore Edul, VS.; Ince, C.; Dubin, A. What is microcirculatory shock? Curr Opin Crit Care. 2015 Jun;21(3):245-52. [CrossRef]
- Kuttab, HI.; Lykins, JD.; Hughes, MD.; Wroblewski, K.; Keast, EP.; Kukoyi, O.; Kopec, JA.; Hall, S.; Ward, MA. Evaluation and Predictors of Fluid Resuscitation in Patients With Severe Sepsis and Septic Shock. Crit Care Med. 2019 Nov;47(11):1582-1590. [CrossRef]
- Elbers, PW.; Wijbenga, J.; Solinger, F.; Yilmaz, A.; van Iterson, M.; van Dongen, EP.; Ince, C. Direct observation of the human microcirculation during cardiopulmonary bypass: effects of pulsatile perfusion. J Cardiothorac Vasc Anesth. 2011 Apr;25(2):250-5. [CrossRef]
- Dekker NAM.; Veerhoek D.; van Leeuwen ALI.; Vonk ABA.; van den Brom CE.; Boer C. Microvascular Alterations During Cardiac Surgery Using a Heparin or Phosphorylcholine-Coated Circuit. J Cardiothorac Vasc Anesth. 2020 Apr;34(4):912-919. [CrossRef]
- Ball, L.; Costantino, F.; Pelosi, P. Postoperative complications of patients undergoing cardiac surgery. Curr Opin Crit Care. 2016 Aug;22(4):386-92. [CrossRef]
- Cherry, AD. Mitochondrial Dysfunction in Cardiac Surgery. Anesthesiol Clin. 2019 Dec;37(4):769-785. [CrossRef]
- Uz, Z.; Aykut, G.; Massey, M.; Ince, Y.; Ergin, B.; Shen, L.; Toraman, F.; van Gulik, TM.; Ince, C. Leukocyte-Endothelium Interaction in the Sublingual Microcirculation of Coronary Artery Bypass Grafting Patients. J Vasc Res. 2020;57(1):8-15. [CrossRef]
- Uz Z.; Milstein DMJ.; Ince C.; de Mol BAJM. Circulating microaggregates during cardiac surgery precedes postoperative stroke. J Thromb Thrombolysis. 2017 Jul;44(1):14-18. [CrossRef]
- Koning, NJ.; Atasever, B.; Vonk, AB.; Boer, C. Changes in microcirculatory perfusion and oxygenation during cardiac surgery with or without cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2014 Oct;28(5):1331-40. [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 Feb 20;382(8):727-733. [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, ML.; Lely, AT.; Navis, G.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004 Jun;203(2):631-7. [CrossRef]
- McGonagle, D.; O'Donnell, JS.; Sharif, K.; Emery, P.; Bridgewood, C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020 Jul;2(7):e437-e445. [CrossRef]
- Joffre, J.; Hellman, J.; Ince, C.; Ait-Oufella, H. Endothelial Responses in Sepsis. Am J Respir Crit Care Med. 2020 Aug 1;202(3):361-370. [CrossRef]
- Do Espírito Santo DA.; Lemos ACB.; Miranda CH. In vivo demonstration of microvascular thrombosis in severe COVID-19. J Thromb Thrombolysis. 2020 Nov;50(4):790-794. [CrossRef]
- Zheng, YY.; Ma, YT.; Zhang, JY.; Xie, X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020 May;17(5):259-260. [CrossRef]
- Favaron, E.; Ince, C.; Hilty, MP.; Ergin, B.; van der Zee, P.; Uz, Z.; Wendel Garcia, PD.; Hofmaenner, DA.; Acevedo, CT.; van Boven, WJ.; et al. Capillary Leukocytes, Microaggregates, and the Response to Hypoxemia in the Microcirculation of Coronavirus Disease 2019 Patients. Crit Care Med. 2021 Apr 1;49(4):661-670. [CrossRef]
- Brouwer, F.; Ince, C.; Pols, J.; Uz, Z.; Hilty, MP.; Arbous, MS. The microcirculation in the first days of ICU admission in critically ill COVID-19 patients is influenced by severity of disease. Sci Rep. 2024 Mar 18;14(1):6454. [CrossRef]
- Farquhar, I.; Martin, CM.; Lam, C.; Potter, R.; Ellis, CG.; Sibbald, WJ. Decreased capillary density in vivo in bowel mucosa of rats with normotensive sepsis. J Surg Res. 1996; 61: 190–196. [CrossRef]
- Abou-Arab, O.; Beyls, C.; Khalipha, A.; Guilbart, M.; Huette, P.; Malaquin, S.; Lecat, B.; Macq, PY.; Roger, PA.; Haye, G.; et al. Microvascular flow alterations in critically ill COVID-19 patients: A prospective study. PLoS One. 2021 Feb 8;16(2):e0246636. [CrossRef]
- Edul, VS.; Enrico, C.; Laviolle, B.; Vazquez, AR.; Ince, C.; Dubin, A. Quantitative assessment of the microcirculation in healthy volunteers and in patients with septic shock. Crit Care Med. 2012 May;40(5):1443-8. [CrossRef]
- Massey, MJ.; Hou, PC.; Filbin, M.; Wang, H.; Ngo, L.; Huang, DT.; Aird, WC.; Novack, V.; Trzeciak, S.; Yealy, DM.; et al. Microcirculatory perfusion disturbances in septic shock: results from the ProCESS trial. Crit Care. 2018 Nov 20;22(1):308. [CrossRef]
- Salgado, DR.; Ortiz, JA.; Favory, R.; Creteur, J.; Vincent, JL.; De Backer, D. Microcirculatory abnormalities in patients with severe influenza A (H1N1) infection. Can J Anaesth. 2010 Oct;57(10):940-6. [CrossRef]
- Kanoore Edul VS.; Caminos Eguillor JF.; Ferrara G.; Estenssoro E.; Siles DSP.; Cesio CE.; Dubin A. Microcirculation alterations in severe COVID-19 pneumonia. J Crit Care. 2021 Feb;61:73-75. [CrossRef]
- Kaplan, LJ.; McPartland, K.; Santora, TA.; Trooskin, SZ. Start with a subjective assessment of skin temperature to identify hypoperfusion in intensive care unit patients. J Trauma. 2001 Apr;50(4):620-7; discussion 627-8. [CrossRef]
- Tibby, SM.; Hatherill, M.; Murdoch, IA. Capillary refill and coreperipheral temperature gap as indicators of haemodynamic status in paediatric intensive care patients. Arch Dis Child 1999 80(2):163–166. [CrossRef]
- Kruger A.; Stewart J.; Sahityani R.; O’Riordan E.; Thompson C.; Adler S.; Garrick R.; Vallance P.; Goligorsky M.; Laser Doppler flowmetry detection of endothelial dysfunction in end-stage renal disease patients: correlation with cardiovascular risk. Kidney Int. 2006; 70: 157–164. [CrossRef]
- Nichol, AD.; Egi, M.; Pettila, V.; Bellomo, R.; French, C.; Hart, G.; Davies, A.; Stachowski, E.; Reade, MC.; Bailey, M.; et al. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care. 2010;14(1):R25. [CrossRef]
- Sepsis-associated hyperlactatemia. Crit Care. 2014 Sep 9;18(5):503. [CrossRef]
- Rathbone, E.; Fu, D. Quantitative Optical Imaging of Oxygen in Brain Vasculature. J Phys Chem B. 2024 Jul 25;128(29):6975-6989. [CrossRef]
- Thomas, R.; Shin, SS.; Balu, R. Applications of near-infrared spectroscopy in neurocritical care. Neurophotonics. 2023 Apr;10(2):023522. [CrossRef]
- Hanssen, H.; Streese, L.; Vilser, W. Retinal vessel diameters and function in cardiovascular risk and disease. Prog Retin Eye Res. 2022 Nov;91:101095. [CrossRef]
- Kawasaki, R.; Cheung, N.; Wang, JJ.; Klein, R.; Klein, BE.; Cotch, MF.; Sharrett, AR.; Shea, S.; Islam, FA.; Wong, TY. Retinal vessel diameters and risk of hypertension: the Multiethnic Study of Atherosclerosis. J Hypertens. 2009 Dec;27(12):2386-93. [CrossRef]
- Toraman, F.; Aksu, U. Monitoring Tissue Oxygenation and Perfusion. Turkiye Klinikleri J Anesthesiology and Reanimation-Special Topics. 2015 8(1): 8-14.
- Chen, M.; Knox, HJ.; Tang, Y.; Liu, W.; Nie, L.; Chan, J.; Yao, J. Simultaneous photoacoustic imaging of intravascular and tissue oxygenation. Opt Lett. 2019 Aug 1;44(15):3773-3776. [CrossRef]
- Groner, W.; Winkelman, JW.; Harris, AG.; Ince, C.; Bouma, GJ.; Messmer, K.; Nadeau, RG. Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med. 1999 Oct;5(10):1209-12. [CrossRef]
- Aykut, G.; Veenstra, G.; Scorcella, C.; Ince, C.; Boerma, C. Cytocam-IDF (incident dark field illumination) imaging for bedside monitoring of the microcirculation. Intensive Care Med Exp. 2015 Dec;3(1):40. [CrossRef]
- Creteur, J.; De Backer, D.; Sakr, Y.; Koch, M.; Vincent, JL. Sublingual capnometry tracks microcirculatory changes in septic patients. Intensive Care Med. 2006 Apr;32(4):516-23. [CrossRef]
- Kastelein AW.; Diedrich CM.; de Waal L.; Ince C.; Roovers JWR. The vaginal microcirculation after prolapse surgery. Neurourol Urodyn. 2020 Jan;39(1):331-338. [CrossRef]
- De Bruin AFJ.; Tavy ALM.; van der Sloot K.; Smits A.; Ince C.; Boerma EC.; Noordzij PG.; Boerma D.; van Iterson M. Can sidestream dark field (SDF) imaging identify subtle microvascular changes of the bowel during colorectal surgery? Tech Coloproctol. 2018 Oct;22(10):793-800. [CrossRef]
- van Elteren, HA.; Ince, C.; Tibboel, D.; Reiss, IK.; de Jonge, RC. Cutaneous microcirculation in preterm neonates: comparison between sidestream dark field (SDF) and incident dark field (IDF) imaging. J Clin Monit Comput. 2015 Oct;29(5):543-8. [CrossRef]
- Boerma, EC.; Kaiferová, K.; Konijn, AJ.; De Vries, JW.; Buter, H.; Ince, C. Rectal microcirculatory alterations after elective on-pump cardiac surgery. Minerva Anestesiol. 2011 Jul;77(7):698-703.
- Gilbert-Kawai, E.; Coppel, J.; Phillip, H.; Grocott, M.; Ince, C.; Martin, D. Changes in labial capillary density on ascent to and descent from high altitude. F1000Res. 2016 Aug 30;5:2107. [CrossRef]
- van Zijderveld, R.; Ince, C.; Schlingemann, RO. Orthogonal polarization spectral imaging of conjunctival microcirculation. Graefes Arch Clin Exp Ophthalmol. 2014 May;252(5):773-9. [CrossRef]
- Pennings, FA.; Bouma, GJ.; Ince, C. Direct observation of the human cerebral microcirculation during aneurysm surgery reveals increased arteriolar contractility. Stroke. 2004 Jun;35(6):1284-8. [CrossRef]
- Kastelein AW.; Vos LMC.; van Baal JOAM.; Koning JJ.; Hira VVV.; Nieuwland R.; van Driel WJ.; Uz Z.; van Gulik TM.; van Rheenen J.; et al. Poor perfusion of the microvasculature in peritoneal metastases of ovarian cancer. Clin Exp Metastasis. 2020 Apr;37(2):293-304. [CrossRef]
- Hashimoto, R.; Kurata, T.; Sekine, M.; Nakano, K.; Ohnishi, T.; Haneishi, H. Two-wavelength oximetry of tissue microcirculation based on sidestream dark-field imaging. J Biomed Opt. 2018 Oct;24(3):1-8. [CrossRef]
- De Backer, D.; Hollenberg, S.; Boerma, C.; Goedhart, P.; Büchele, G.; Ospina-Tascon, G.; Dobbe, I.; Ince, C. How to evaluate the microcirculation: report of a round table conference. Crit Care. 2007;11(5):R101. [CrossRef]
- Ince C.; Boerma EC.; Cecconi M.; De Backer D.; Shapiro NI.; Duranteau J.; Pinsky MR.; Artigas A.; Teboul JL.; Reiss IKM.; et al. Cardiovascular Dynamics Section of the ESICM. Second consensus on the assessment of sublingual microcirculation in critically ill patients: results from a task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2018 Mar;44(3):281-299. [CrossRef]
- Hilty, MP.; Ince, C. Automated quantification of tissue red blood cell perfusion as a new resuscitation target. Curr Opin Crit Care. 2020 Jun;26(3):273-280. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).