Submitted:
08 October 2024
Posted:
09 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Survey Respondents and Data Collection
2.2. Measurement Methods (Baseline Survey)
2.3. Follow-Up Survey
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Parental Attributes and Intention Regarding Vaccinating Their Children Against COVID-19
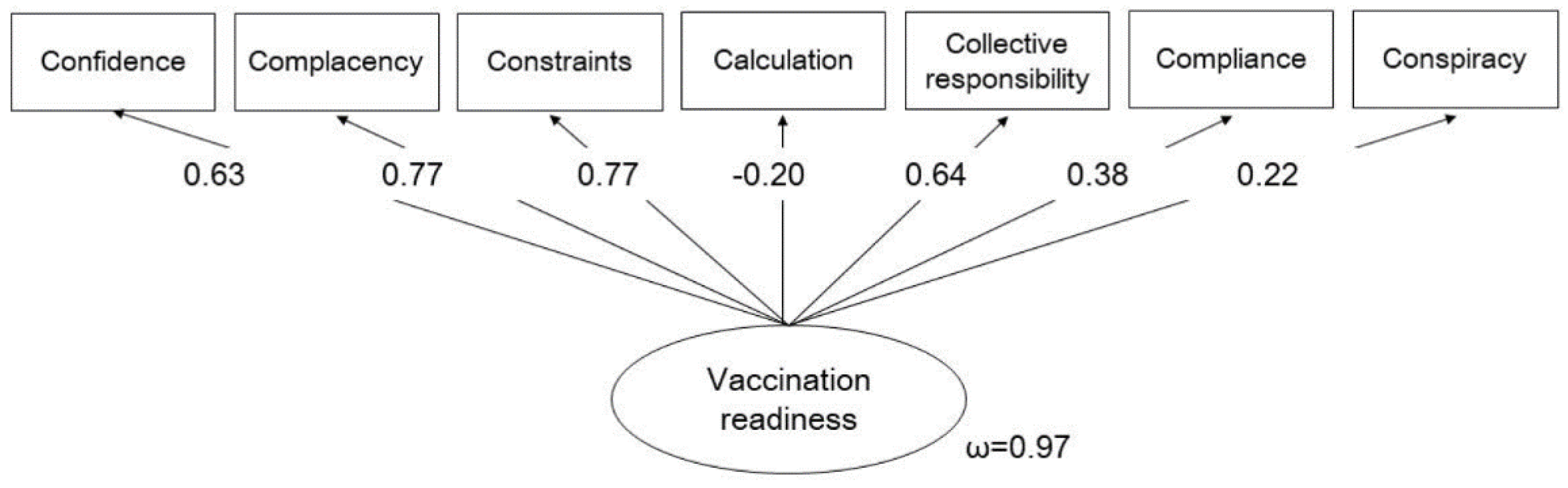
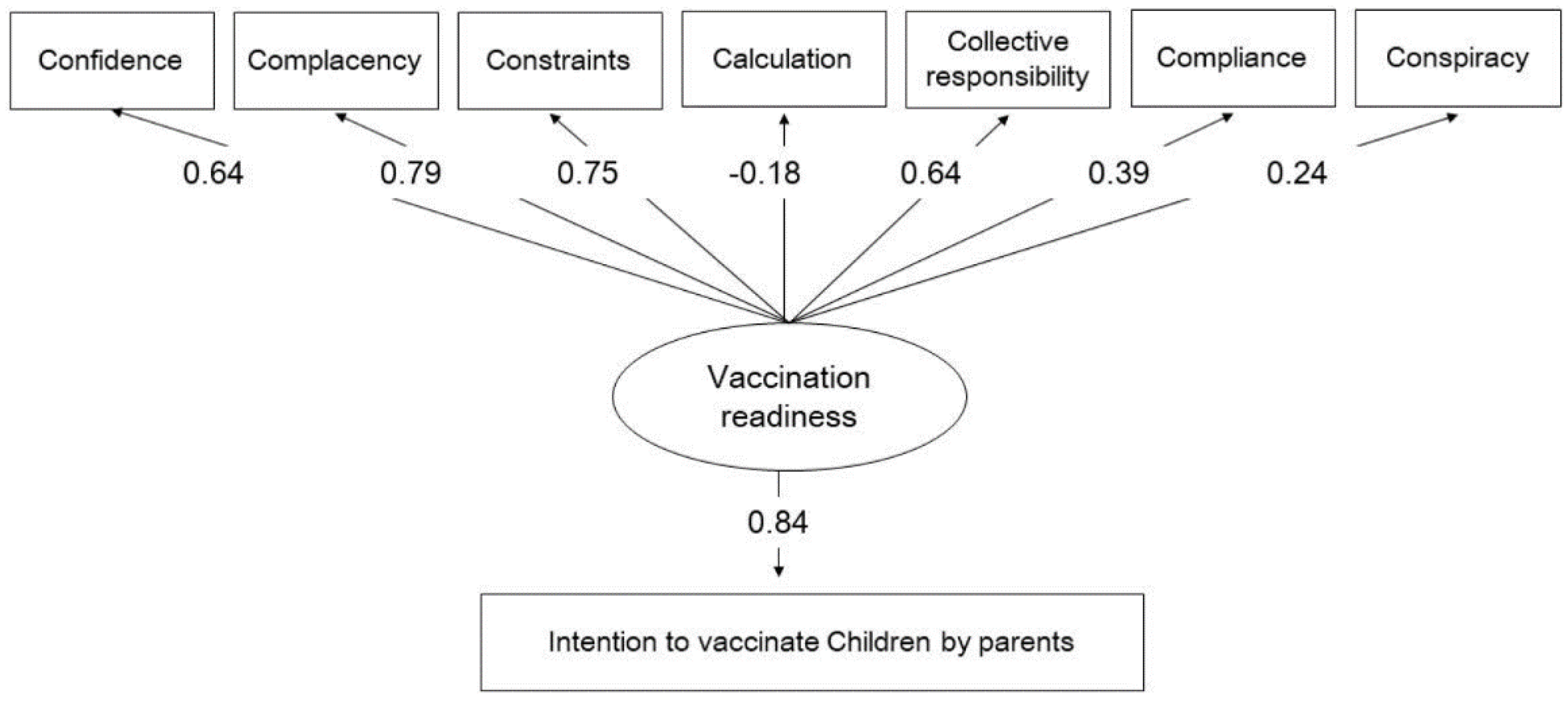
3.2. Measurement Model and Criterion Validity for Parental Readiness to Vaccinate Their Children Against COVID-19
3.3. Predictors of Parental Intention to Vaccinate Their Children Against COVID-19
3.4. Relationship between Components of the Modified Scale and Parental Intention to Vaccinate Their Children against COVID-19
3.5. Predicted and Observed Vaccination Behavior
| Vaccinated against COVID-19 | ||
|---|---|---|
| No N = 406 |
Yes N = 130 |
|
| 7C score before vaccine approval, n (%) | ||
| Strongly disagree | 30 (85.7) | 5 (14.3) |
| Disagree | 62 (89.9) | 7 (10.1) |
| Neither agree nor disagree | 184 (78.6) | 50 (21.4) |
| Agree | 114 (66.3) | 58 (33.7) |
| Strongly agree | 16 (61.5) | 10 (38.5) |
| Complacency, n (%) | ||
| Strongly disagree | 20 (80.0) | 5 (20.0) |
| Disagree | 47 (88.7) | 6 (11.3) |
| Neither agree nor disagree | 196 (83.4) | 39 (16.6) |
| Agree | 123 (66.8) | 61 (33.2) |
| Strongly agree | 20 (51.3) | 19 (48.7) |
| Constraints, n (%) | ||
| Strongly disagree | 27 (90.0) | 3 (10.0) |
| Disagree | 71 (91.0) | 7 (9.0) |
| Neither agree nor disagree | 182 (77.4) | 53 (22.6) |
| Agree | 114 (69.5) | 50 (30.5) |
| Strongly agree | 12 (41.4) | 17 (58.6) |
| Calculation, n (%) | 11 (73.3) | |
| Strongly disagree | 4 (26.7) | |
| Disagree | 38 (70.4) | 16 (29.6) |
| Neither agree nor disagree | 159 (79.5) | 41 (20.5) |
| Agree | 151 (72.2) | 58 (27.8) |
| Strongly agree | 47 (81.0) | 11 (19.0) |
| Collective responsibility, n (%) | ||
| Strongly disagree | 18 (85.7) | 3 (14.3) |
| Disagree | 17 (77.3) | 5 (22.7) |
| Neither agree nor disagree | 131 (85.1) | 23 (14.9) |
| Agree | 192 (71.6) | 76 (28.4) |
| Strongly agree | 48 (67.6) | 23 (32.4) |
| Compliance, n (%) | ||
| Strongly disagree | 123 (89.8) | 14 (10.2) |
| Disagree | 113 (76.4) | 35 (23.6) |
| Neither agree nor disagree | 120 (70.2) | 51 (29.8) |
| Agree | 41 (66.1) | 21 (33.9) |
| Strongly agree | 9 (50.0) | 9 (50.0) |
| Conspiracy, n (%) | ||
| Strongly disagree | 14 (70.0) | 6 (30.0) |
| Disagree | 65 (66.3) | 33 (33.7) |
| Neither agree nor disagree | 222 (79.6) | 57 (20.4) |
| Agree | 89 (74.8) | 30 (25.2) |
| Strongly agree | 16 (80.0) | 4 (20.0) |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lehmann, B.A.; de Melker, H.E.; Timmermans, D.R.M.; Mollema, L. Informed decision making in the context of childhood immunization. Patient Educ Couns 2017, 100, 2339–2345. [CrossRef]
- Duclos, P.; Okwo-Bele, J. M.; Gacic-Dobo, M.; Cherian T. Global immunization: Status, progress, challenges and future. BMC Int Health Hum Rights 2009, 9 Suppl 1, S2. [CrossRef]
- World Bank. World development report 1993. Oxford University Press, New York: 1993.
- Chen, F.; He, Y.; Shi, Y. Parents' and guardians' willingness to vaccinate their children against COVID-19: A systematic review and meta-analysis. Vaccines (Basel) 2022, 10, 179. [CrossRef]
- Yang, W. Transmission dynamics of and insights from the 2018-2019 measles outbreak in New York City: A modeling study. Sci Adv 2020, 6, eaaz4037. [CrossRef]
- Geiger, M.; Rees, F.; Lilleholt, L.; Santana, A.P.; Zettler, I.; Wilhelm, O.; Betsch, C.; Böhm, R. Measuring the 7Cs of vaccination readiness. Eur J Psych Assess 2021, 38, 261–269. [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [CrossRef]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond confidence: Development of a measure assessing the 5c psychological antecedents of vaccination. PLoS One 2018, 13, e0208601.
- Abdou, M.S.; Kheirallah, K.A.; Aly, M.O.; Ramadan, A.; Elhadi, Y.A.M.; Elbarazi, I.; Deghidy, E.A.; El Saeh, H.M.; Salem, K.M.; Ghazy, R.M. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5C validated tool: An online survey in 13 Arab countries. PLoS One 2021, 16, e0260321. [CrossRef]
- Al-Sanafi, M.; Sallam, M. Psychological determinants of COVID-19 vaccine acceptance among healthcare workers in Kuwait: A cross-sectional study using the 5C and vaccine conspiracy beliefs scales. Vaccines 2021, 9, 701. [CrossRef]
- Gallant, A.J.; Nicholls, L.A.; Rasmussen, B.S.; Cogan, N.; Young, D.; Williams, L. Changes in attitudes to vaccination as a result of the COVID-19 pandemic: A longitudinal study of older adults in the UK. PLoS One 2021, 16, e0261844. [CrossRef]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A; Wong, S.Y.S.; Lee, S.S. Editor's choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud 2021, 114, 103854. [CrossRef]
- Machida, M., Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; et al. Trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and their associations with the 5C psychological antecedents of vaccination by sex and age in Japan. Hum Vaccin Immunother 2021, 17, 3954–3962. [CrossRef]
- Mercadante, A.R.; Law, A.V. Will they, or won't they? Examining patients' vaccine intention for flu and COVID-19 using the health belief model. Res Social Adm Pharm 2021, 17, 1596–1605. [CrossRef]
- Obohwemu, K.; Christie-de Jong, F.; Ling, J. Parental childhood vaccine hesitancy and predicting uptake of vaccinations: A systematic review. Prim Health Care Res Dev 2022, 23, e68. [CrossRef]
- Wagner, A.; Liberatore, F.; Schmelzer, S.; Dratva, J. Confident and altruistic - parents' motives to vaccinate their children against COVID-19: A cross-sectional online survey in a Swiss vaccination centre." Swiss Med Wkly 2022, 152, w30156. [CrossRef]
- Wismans, A.; Thurik, R.; Baptista, R.; Dejardin, M.; Janssen, F.; Franken, I. Psychological characteristics and the mediating role of the 5C model in explaining students' COVID-19 vaccination intention. PLoS One 2021, 16, e0255382. [CrossRef]
- Cogordan, C.; Fressard, L.; Ramalli, S.; Rebaudet, P.; Malfait, A.; Dutrey-Kaiser, Y.; Attalah, D.; Roy, P.; Berthiaume, A.; Gagneur, A.; Verger, P. Motivational interview-based health mediator interventions increase intent to vaccinate among disadvantaged individuals. Hum Vaccin Immunother 2023, 19, 2261687. [CrossRef]
- Teng, Y.; Hanibuchi, T.; Machida, M.; Nakaya, T. Psychological determinants of COVID-19 vaccine acceptance: A comparison between immigrants and the host population in Japan. Vaccine 2023, 41, 1426–1430. [CrossRef]
- Williams, L.; Gallant, A.; Brown, L.; Corrigan, K.; Crowe, K.; Hendry, E. Barriers and facilitators to the future uptake of regular COVID-19 booster vaccinations among young adults in the UK. Hum Vaccin Immunother 2022, 18, 2129238. [CrossRef]
- Szilagyi, P. G.; Shah, M. D.; Delgado, J. R.; Thomas, K.; Vizueta, N.; Cui, Y.; Vangala, S.; Shetgiri, R.; Kapteyn, A. Parents' intentions and perceptions about COVID-19 vaccination for their children: Results from a national survey. Pediatrics 2021, 148, e2021052335. [CrossRef]
- Kezhong, A.; Lu, X.; Wang, J.; Hu, L.; Li, B; Lu, Y. Association between adult vaccine hesitancy and parental acceptance of childhood COVID-19 vaccines: A web-based survey in a northwestern region in China. Vaccines (Basel) 2021, 9, 1088. [CrossRef]
- Almalki, O.S., Alfayez, O.M.; Al Yami, M.S.; Asiri, Y. A.; Almohammed, O.A. Parents' hesitancy to vaccinate their 5-11-year-old children against COVID-19 in Saudi Arabia: Predictors from the health belief model. Front Public Health 2022, 10, 842862. [CrossRef]
- Rane, M.S.; Robertson, M.M.; Westmoreland, D.A.; Teasdale, C.A.; Grov, C.; Nash, D. Intention to vaccinate children against Covid-19 among vaccinated and unvaccinated US parents. JAMA Pediatrics 2022, 176, 201–203. [CrossRef]
- Eberhardt, C.S.; Siegrist, C.A. Is there a role for childhood vaccination against COVID-19? Pediatr Allergy Immunol 2021, 32, 9–16. [CrossRef]
- Rees, F., Geiger, M.; Lilleholt, L.; Zettler, I.; Betsch, C.; Böhm, R.; Wilhelm, O. Measuring parents' readiness to vaccinate themselves and their children against COVID-19. Vaccine 2022, 40, 3825–3834. [CrossRef]
- Swann, O.V.; Holden, K.A.; Turtle, L.; Pollock, L.; Fairfield, C.J.; Drake, T.M.; Seth, S.; Egan, C.; Hardwick, H.E.; Halpin, S.; et al. Clinical characteristics of children and young people admitted to hospital with COVID-19 in United Kingdom: Prospective multicentre observational cohort study. BMJ 2020, 370, m3249. [CrossRef]
- Horiuchi, S.; Sakamoto, H.; Abe, S.K.; Shinohara, R.; Kushima, M.; Otawa, S.; Yui, H.; Akiyama, Y.; Ooka, T.; Kojima, R.; et al. Factors of parental COVID-19 vaccine hesitancy: A cross-sectional study in Japan. PLoS One 2021, 16, e0261121. [CrossRef]
- Machida, M.; Kojima, T.; Popiel, H. A.; Geiger, M.; Odagiri, Y.; Inoue, S. Development, validity, and reliability of the Japanese version of the 7C of vaccination readiness scale. Am J Infect Control 2023, 51, 426–433. [CrossRef]
- Tokiya, M.; Hara, M.; Matsumoto, A.; Ashenagar, M.S.; Nakano; T.; Hirota, Y. Acceptance of booster COVID-19 vaccine and its association with components of vaccination readiness in the general population: A cross-sectional survey for starting booster dose in Japan. Vaccines (Basel) 2022, 10, 1102. [CrossRef]
- Ministry of Health, Labour, and Welfare. About Covid-19 vaccine (shingata korona wakutin ni tuite). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/vaccine_00184.html. (accessed on 1 October 2024).
- Machida, M.; Kojima, T. H.; Popiel, A.; Geiger, M.; Odagiri, Y.; Inoue. Japanese version of the 7Cs of vaccination readiness. 2021. http://www.tmu-ph.ac/news/data/vaccination-readiness-01.pdf. (accessed on 1 October 2024).
- Goretzko, D.; Siemund, K.; Sterner, P. Evaluating model fit of measurement models in confirmatory factor analysis. Edu Psych Manag 2023, 00131644231163813. [CrossRef]
- Ministry of Health, Labour, and Welfare. Number of doses of the COVID-19 vaccine. 2024. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/kekkaku-kansenshou/yobou-sesshu/syukeihou_00002.html. (accessed on 1 October 2024).
- Nguyen, T., Henningsen, K.H.; Brehaut, J. C.; Hoe, E.; Wilson, K. Acceptance of a pandemic influenza vaccine: A systematic review of surveys of the general public. Infect Drug Resist 2011, 4, 197–207. [CrossRef]
- Götzinger, F.; Santiago-García, B.; Noguera-Julián, A.; Lanaspa, M.; Lancella, L.; Calò Carducci, F. I.; Gabrovska, N.; Velizarova, S.; Prunk, P.; Osterman, V. et al. Covid-19 in children and adolescents in Europe: A multinational, multicentre cohort study." Lancet Child Adolesc Health 2020, 4, 653–661. [CrossRef]
- Rajapakse, N.; Dixit, D. Human and novel coronavirus infections in children: A review. Paediatr Int Child Health 2021, 41, 36–55. [CrossRef]
- Bozkurt, B.; Kamat, I.; Hotez, P.J. Myocarditis with COVID-19 mRNA vaccines. Circulation 2021, 144, 471–484. [CrossRef]
- Zimmermann, P.; Pittet, L.F.; Finn, A.; Pollard, A.J.; Curtis, N. Should children be vaccinated against COVID-19? Arch Dis Child 2022, 107, e1. [CrossRef]
- McMurray, J.; McNeil, H.; Gordon, A.; Elliott, J.; Stolee, P. Psychometric testing of a rehabilitative care patient experience instrument. Arch Phys Med Rehabil 2018, 99, 1840–1847. [CrossRef]
| 7C scale original version Short version |
Modified 7C scale original version |
Modified 7C scale Japanese version | |
|---|---|---|---|
| Confidence | I am convinced the appropriate authorities do only allow effective and safe vaccines. | I am convinced the appropriate authorities do only allow effective and safe vaccines for children. | 政府関係機関が小児に対して効果的で安全なワクチンのみを許可すると確信している. |
| Complacency | I get vaccinated because it is too risky to get infected. | I get my child vaccinated because it is too risky for children to get infected. | 小児が感染すると非常に危険なので,子どもに予防接種を受けさせる. |
| Constraints | Vaccinations are so important to me that I prioritize getting vaccinated over other things. | Vaccinations are so important for my child that I prioritize getting them vaccinated over other things. | 予防接種は子どもにとってとても大切なので,他のことよりも優先する. |
| Calculation | I only get vaccinated when the benefits clearly outweigh the risks. (R) | I only get my child vaccinated when the benefits clearly outweigh the risks. (R) | 利益が危険性より明らかに上回る場合にのみ,予防接種を受けさせる.(R) |
| Collective responsibility | I see vaccination as a collective task against the spread of diseases. | I see vaccinations as a collective task against the spread of disease in schools. | 予防接種は学校での病気の蔓延を防ぐための集団行動だと思う. |
| Compliance | It should be possible to sanction people who do not follow the vaccination recommendations by health authorities. | It should be possible to sanction parents who do not follow the vaccination recommendations by health authorities. | 保健機関による予防接種の推奨に従わない人には,制裁を加えることができるようにすべきだ. |
| Conspiracy | Vaccinations cause diseases and allergies that are more serious than the diseases they ought to protect from. (R) | Vaccinations cause diseases and allergies that are more serious than the diseases they ought to protect from. (R) | ワクチンの接種は,それが本来防ぐ病気よりも,もっと深刻な病気やアレルギーを引き起こす.(R) |
| When a pediatric vaccine for COVID-19 becomes available, I will vaccinate my children | P-valuea | |||||
|---|---|---|---|---|---|---|
| Characteristic | Strongly disagree (N = 88) n (%) |
Disagree (N = 154) n (%) |
Undecided (N = 430) n (%) |
Agree (N = 405) n (%) |
Strongly agree (N = 113) n (%) |
|
| Percent of responses | (7.4%) | (12.9%) | (36.1%) | (34.0%) | (9.5%) | |
| Sex | 0.009 | |||||
| Male | 36 (40.9) | 58 (37.7) | 171 (39.8) | 178 (44.0) | 65 (57.5) | |
| Female | 52 (59.1) | 96 (62.3) | 259 (60.2) | 227 (56.1) | 48 (42.5) | |
| Age (years), mean ± SD | 37.5 ± 6.5 | 36.5 ± 6.6 | 37.6 ± 7.8 | 40.3 ± 9.0 | 39.8 ± 9.0 | <0.001b |
| Residential region | 0.544 | |||||
| Hokkaido | 4 (4.6) | 7 (4.6) | 22 (5.1) | 19 (4.7) | 6 (5.3) | |
| Tohoku | 6 (6.8) | 5 (3.3) | 19 (4.4) | 22(5.4) | 7 (6.2) | |
| Kanto | 22 (25.0) | 37 (24.0) | 136 (31.6) | 131 (32.4) | 43 (38.1) | |
| Chubu | 14 (15.9) | 36 (23.4) | 83 (19.3) | 80 (19.8) | 17 (15.0) | |
| Kinki | 22 (25.0) | 30 (19.5) | 82 (19.1) | 74 (18.3) | 24 (21.2) | |
| Chugoku | 6 (6.8) | 7 (4.6) | 26 (6.1) | 27 (6.7) | 5 (4.4) | |
| Shikoku | 3 (3.4) | 2 (1.3) | 12 (2.8) | 12 (2.9) | 2 (1.8) | |
| Kyusyu | 11 (12.5) | 30 (19.5) | 50 (11.6) | 40 (9.9) | 9 (8.0) | |
| Marital status | 0.017 | |||||
| Unmarried | 7 (8.0) | 9 (5.8) | 36 (8.4) | 13 (3.2) | 4 (3.5) | |
| Married | 81 (92.1) | 145 (94.2) | 394 (91.6) | 392 (96.8) | 109 (96.5) | |
| Household income | 0.365 | |||||
| <4 million yen | 16 (18.2) | 15 (9.7) | 65 (15.1) | 61 (15.1) | 12 (10.6) | |
| ≥4 million yen | 54 (61.4) | 107 (69.5) | 278 (64.7) | 268 (66.2) | 85 (75.2) | |
| Unknown | 18 (20.5) | 32 (20.8) | 87 (20.2) | 76 (18.8) | 16 (14.2) | |
| Level of education | 0.140 | |||||
| ≤ High school | 15 (17.1) | 35 (22.7) | 109 (25.4) | 84 (20.7) | 18 (15.9) | |
| > High school | 73 (83.0) | 119 (77.3) | 321 (74.7) | 321 (79.3) | 95(84.1) | |
| Concerns about adverse events | ||||||
| Strongly disagree | 6 (6.8) | 5 (3.3) | 5 (1.2) | 1 (0.3) | 2 (1.8) | <0.001 |
| Disagree | 4 (4.6) | 15 (9.7) | 25 (5.8) | 14 (3.5) | 12 (10.6) | |
| Not sure | 2 (2.3) | 18 (11.7) | 91 (21.2) | 58 (14.3) | 24 (21.2) | |
| Agree | 10 (11.4) | 47 (30.5) | 148 (34.4) | 209 (51.6) | 35 (31.0) | |
| Strongly agree | 66 (75.0) | 69 (44.8) | 161 (37.4) | 123 (30.4) | 40 (35.4) | |
| Parental vaccination for COVID-19 | ||||||
| None | 40 (45.5) | 32 (20.8) | 49 (11.4) | 13 (3.2) | 4 (3.5) | <0.001 |
| Once | 1 (1.1) | 2 (1.3) | 9 (2.1) | 7 (1.7) | 1 (0.9) | |
| Twice | 47 (53.4) | 116 (75.3) | 364 (84.7) | 375 (92.6) | 106 (93.8) | |
| Three times | 0 (0.0) | 4 (2.6) | 8 (1.9) | 10 (2.5) | 2 (1.8) | |
| Number of valid responses | N = 48 | N = 122 | N = 381 | N = 392 | N = 109 | |
| Experienced any adverse eventsc | ||||||
| Fever | 26 (54.2) | 66 (54.1) | 234 (61.4) | 210 (53.6) | 62 (56.9) | 0.238d |
| Fatigue | 27 (56.3) | 70(57.4) | 240 (63.0) | 226 (57.7) | 60(55.1) | 0.429d |
| Headache | 17 (35.4) | 41 (33.6) | 140 (36.8) | 119 (30.4) | 35 (32.1) | 0.443d |
| Chill | 13 (27.1) | 20 (16.4) | 78 (20.5) | 69 (17.6) | 23 (21.1) | 0.421d |
| Vomiting | 0 (0.0) | 0 (0.0) | 11 (2.9) | 5 (1.3) | 3 (2.8) | 0.159d |
| Diarrhea | 1 (2.1) | 2 (1.6) | 7 (1.8) | 14 (3.6) | 4 (3.7) | 0.508d |
| Muscular pain | 15 (31.3) | 36 (29.5) | 102 (26.8) | 104 (26.5) | 32 (29.4) | 0.882d |
| Arthralgia | 5 (10.4) | 25 (20.5) | 58 (15.2) | 64 (16.3) | 21 (19.3) | 0.444d |
| Anaphylactic shock | 0 (0.0) | 1 (0.8) | 1 (0.3) | 1 (0.3) | 0 (0.0) | 0.702d |
| Component | When a pediatric vaccine for COVID-19 becomes available, I will vaccinate my children | ρ | P-value | ||||
|---|---|---|---|---|---|---|---|
| Strongly disagree (Mean ± SD) |
Disagree (Mean ± SD) |
Neither agree nor disagree (Mean ± SD) |
Agree (Mean ± SD) |
Strongly Agree (Mean ± SD) |
|||
| Confidence | 1.91 ± 1.06 | 2.58 ± 0.88 | 3.03 ± 0.74 | 3.49 ± 0.78 | 3.91 ± 0.87 | 0.513 | <0.001 |
| Complacency | 1.82 ± 1.07 | 2.56 ± 0.75 | 3.06 ± 0.56 | 3.74 ± 0.67 | 4.27 ± 0.90 | 0.667 | <0.001 |
| Constraints | 1.98 ±1.10 | 2.40 ± 0.79 | 2.97 ± 0.69 | 3.58 ± 0.69 | 4.14 ± 0.85 | 0.610 | <0.001 |
| Calculation | 3.16 ± 1.42 | 2.69 ± 0.96 | 2.58 ± 0.78 | 2.50 ± 0.85 | 2.50 ± 1.13 | −0.127 | <0.001 |
| Collective responsibility | 2.44 ± 1.26 | 3.09 ± 0.86 | 3.43 ± 0.76 | 3.99 ± 0.61 | 4.43 ± 0.79 | 0.549 | <0.001 |
| Compliance | 1.56 ± 0.96 | 1.93 ± 0.92 | 2.39 ± 0.94 | 2.55 ± 1.05 | 2.88 ± 1.27 | 0.278 | <0.001 |
| Conspiracy | 2.33 ± 1.15 | 2.90 ± 0.88 | 2.98 ± 0.69 | 3.03 ± 0.76 | 3.20 ± 1.15 | 0.170 | <0.001 |
| Total vaccination readiness | 15.19 ± 4.50 | 18.16 ± 2.62 | 20.45 ± 2.35 | 22.87 ± 2.36 | 25.35 ± 3.14 | 0.678 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





