Introduction
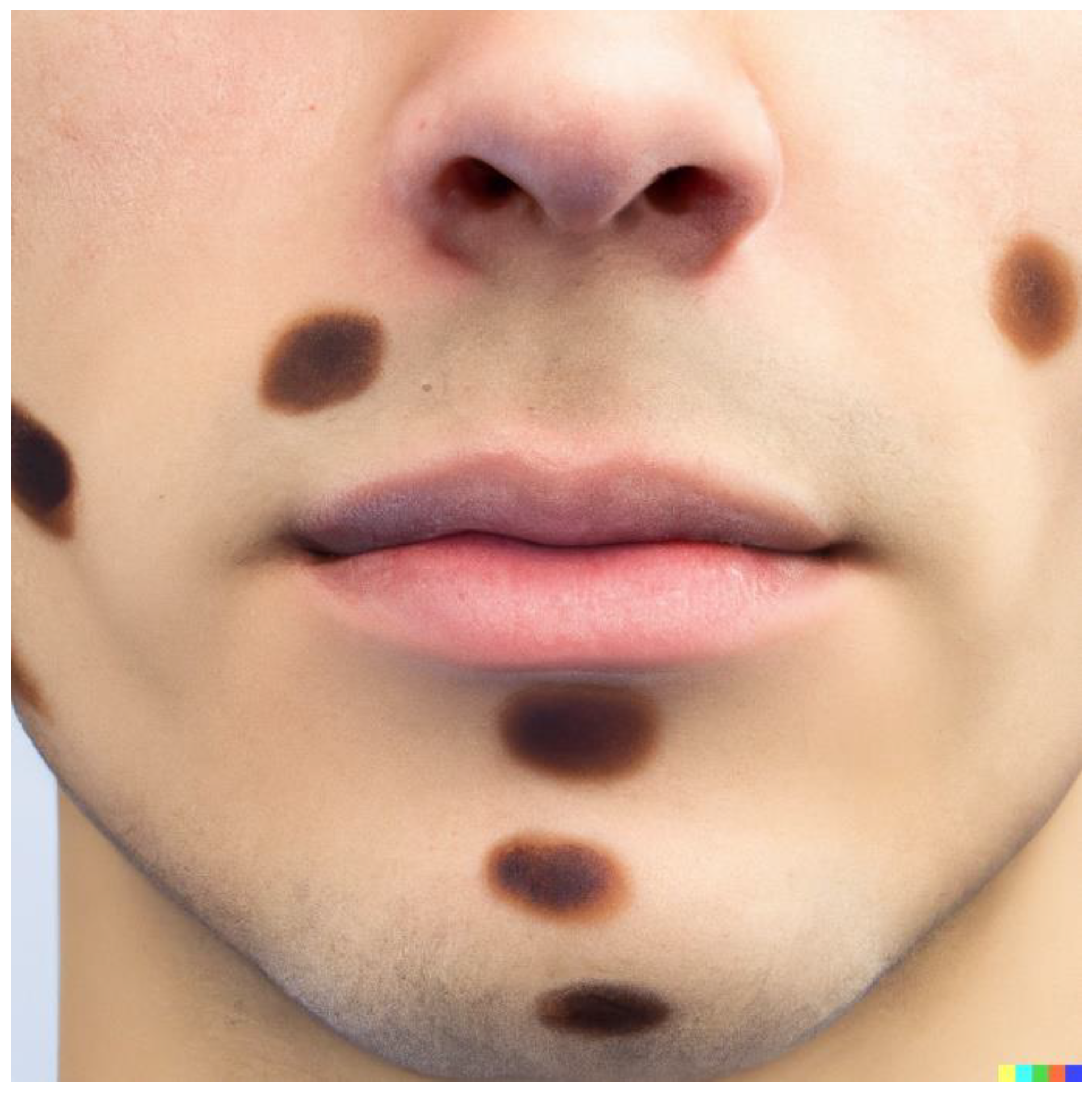
Leishmaniasis is considered one of the life-threatening diseases that come under the category of Neglected Tropical Diseases (NTDs), contributing to the third-highest fatality rate in the category. Leishmaniasis is endemic to the tropical regions, subtropical regions, and the southern parts of Europe including 98 countries and 350 million people vulnerable to the infection caused by the intracellular pathogen of the Leishmania genus (Prevention, 2019). Around 90 species of sandflies are the primary mode of transmission of the pathogens to humans(hosts) and it occurs predominantly by the bite of tainted female phlebotomine sandflies (vectors)(Cobo, 2014). According to WHO, 18 pathogenic Leishmania species were reported, and they cause clinical forms including Visceral leishmaniasis (VL), Cutaneous leishmaniasis (CL), and mucocutaneous leishmaniasis (ML). The disease is mostly found in the impoverished as it is related to a weak immune system, malnutrition, lack of cleanliness, migration, and several environmental changes. If the patient does not undergo proper treatment, the disease can cause several consequences including irreversible abnormalities or even death (WHO,2018). Prevention of leishmaniasis is a strenuous task as it involves a network of biological systems consisting of a parasite, a vector, an animal reservoir, and a host. Measures like vector control, early diagnosis, and monitoring of animal reservoirs increase the effectiveness of prevention while drugs and vaccines also have a pivotal role during action.
Among the variants of leishmaniasis, Visceral leishmaniasis (kala-azar/black fever/disease) is the life-threatening variant (Bi
et al., 2018). Circulation of amastigotes through the blood leads to infection of the reticulo-endothelial system and various internal organs like bone marrow, spleen, lymph nodes, and liver. Among the variants, VL commonly occurs internally and can be asymptomatic, resulting in a barrier to detecting and curing the disease (Lun
et al., 2015). The approximate number of novel cases reported annually may come up to < 1,00,000, but a recent estimate reflects a hike in the reported cases.
Leishmania donovani and
Leishmania infantum are the leading causative pathogen species and sometimes
Leishmania tropica (Lypaczewski and Matlashewski, 2021). The incubation period of pathogens in the host is from 2 months to decades. Due to immunosuppression, the pathogens possess the potential to reinfect the host even after years. Typical infection symptoms are weight loss, hepatosplenomegaly, chronic fever, thrombocytopenia, leukopenia, anemia, and swelling of the liver and spleen (Akuffo
et al., 2018).
Transmission of Leishmaniasis
Promastigote and amastigote are the two morphological forms of the pathogen. The promastigote will endure in the vector while the amastigote in the hosts. Promastigote is the morphological version of the pathogen having a flagellum or simply the developmental stage of the pathogen present in the foregut of the vector, and the amastigotes are the intracellular phase of the pathogen that resides within the host that doesn’t have a flagella/cilia(Freitas-Mesquita, Dos-Santos and Meyer-Fernandes, 2021). It is assumed that the transmission of the pathogens starts from a blood meal by the vector, sandfly. The promastigote was transferred to the host skin by the bite of female phlebotomine sandflies. The vector lesions will channel the entry of promastigotes into the cells, and they will be absorbed by the phagocytic cells like neutrophils and macrophages. Phagolysosomes (phagocytic cells) is the medium for the promastigotes, to transform into amastigotes and multiply. After multiplication, the cell gets lysed followed by the infection of amastigotes to the neighboring cells. When sandfly bites the infected individual, they ingest the infected macrophages. Then the amastigotes develop back into promastigotes and get multiplied in the gut of the vector. They migrate to the proboscis of the sandfly and get prepared to infect another individual, this cycle repeats (
Figure 2).
Types of Visceral Leishmaniasis
Based on the mode of transmission, visceral leishmaniasis can be categorized into two groups; Zoonotic visceral leishmaniasis (ZVL) and Anthroponotic visceral leishmaniasis (AVL).
Zoonotic Visceral Leishmaniasis
Zoonotic visceral leishmaniasis is a pervasive disease that repeatedly results in the demise of infected individuals. Comparatively, the ZVL infection rate is high in infants with severe symptoms and chachetia. In ZVL, animal reservoirs play an important role in the spreading of the disease. The main causative organism and vector of ZVL are reported as L. infantum and Phlebotomus perniciosusin (sandfly) respectively(Rodrigues et al., 2022). P. langeroni, P. longicuspis, P. syriacus, P. halepensis, P. perniciosus, P. galilaeus, P. perfiliewi, P. tobbi and P. ariasi. Mammalian reservoirs function as the reason for sustaining the disease within a community as they can be the unlimited supply of pathogens for vectors. Canis familiaris (dogs) acts as the primary non-human pathogen reservoir and other animals like marsupials, primates, edentates, lagomorphs, bats, rodents, horses, and foxes can be considered as the secondary reservoirs. Since dogs are brought up as pets and guards for animal husbandry their presence within the human population is not negligible. The presence of other reservoirs in the endemic regions along with primary reservoirs provides a combined donation in the transmission of leishmaniasis. The pathogens need to overlap between the reservoirs and vectors to facilitate the emergence of ZVL. To perform this, pathogens have their manipulating mechanisms that can change properties like the odour and pheromone emission of their reservoir hosts so that the vectors will be easily attracted. Preventive measures like vector control and culling of reservoirs have not been that successful in the spreading of disease (Chelbi et al., 2021).
Anthroponotic visceral leishmaniasis
In AVL, humans are the reservoirs for pathogens. AVL spreads from human to human through vectors. Humans are not considered natural reservoirs and are considered accidental hosts(Mollalo and Khodabandehloo, 2016). L. donovani is the main causative organism along with P. orientalis and P. alexandri as the main vectors. Asymptotic behavior of VL is a risk factor for two reasons, as the infected persons do not exhibit any symptoms they can transmit the disease to healthy individuals and they are not undergoing any treatment either, leading them to be a walking reservoir among the population. Prevention measures can be taken by providing better health facilities, regular health checkups, continuous monitoring, and also human user-friendly insect repellents and insecticides can be applied on the body and clothes respectively (Romero and Boelaert, 2010).
Treatment
Leishmaniasis is a disease that can be treated through proper medical attendance, nutrition, and cleanliness. Several factors were taken into consideration while treating leishmaniasis including infection species, disease pathway, the geography of the endemic region, immunocompetency of the patient, etc A systematic approach is an essential element in the treatment as supportive therapy like nutritional supply, and treatment for leukopenia and anemia should go hand in hand with the primary therapy (drugs).
An FDA- approved drug, Liposomal amphotericin B is a widely used drug for the treatment of VL and is given to patients as an IV infusion and the dosage will vary according to the intensity of the disease. Due to the adverse effects and toxicity of another drug - amphotericin B deoxycholate, liposomal amphotericin B is more acceptable.
Miltefosine is also an approved drug used for treatment, but only for adolescents and adults, not for children. As the ZVL is more common among children this drug cannot be used for most patients. It can only be given to patients with leishmaniasis caused by L. donovani and the exception of pregnant patients is the limitation of this drug.
For most geographic regions, Pentavalent antimonial (SbV) therapy is a better drug of choice as it covers the age barrier but a high risk of cardiotoxicity makes this drug a potential threat to life. Paromomycin sulfate and pentamidine isethionate can also be considered but the irreversible toxicity of these two on kidneys and ears has reduced the acceptance(van Griensven and Diro, 2012).
Alternative Approaches
Alternate remedies or approaches should be tried since the existing drugs have serious drawbacks like severe side effects, high cost, and unavailability. Several research studies have been conducted to find a better drug and treatment for the disease. Drug/lead molecules from natural compounds can be explored in this aspect. Among them, phytocompounds are promising agents as they possess innumerable potential characteristics. In silico studies based on plant secondary metabolites anticipate drug development against various diseases. Phytocompounds with anti-parasitic/ antiprotozoal activities can be considered and analyzed as lead molecules which may be vital in the treatment of Visceral Leishmaniasis.
Conclusions
Leishmaniasis is a vector-borne parasitic/protozoal disease caused by the Leishmania species. Visceral Leishmaniasis is a severe form of the disease which occurs internally, can be asymptomatic, and even lead to death if proper treatment is not provided. L. donovani and L. infantum are the two major species that cause the VL, and the Phlebotomus species are the major carriers of the pathogens. Based on the reservoirs, VL is again classified into ZVL and AVL. Different animals play the role of reservoirs and some of them have become an inevitable part of the human population. Therefore, preventive measures like culling the reservoirs can be done only to an extent. Other measures like vector control, medical attendance, nutrition, and cleanliness can be provided to fight against the endemic. ZVL is predominantly seen in children, pointing out that the eradication of malnutrition has to be taken seriously. Patients have to undergo proper treatment focusing on both the infection and the symptoms that accompany the disease. Half of the infected population can’t afford the drugs for treatment, while the drugs are not even available in some countries. Severe side effects of the drugs also need to be sorted out. Therapeutic agents from natural resources, especially phytocompounds may lighten the way to the treatment of the disease.
References
- Prevention, C.-C. for D. C. and. (2019, February 27). CDC - Leishmaniasis. Www.cdc.gov. https://www.cdc.gov/parasites/leishmaniasis/.
- Cobo, F. (2014). 16-Leishmaniasis. Imported infectious diseases: Woodhead Publishing, 227-42.
- World Health Organisation. (2018, March 14). Leishmaniasis. Who.int; World Health Organization: WHO. https://www.who.int/news-room/fact-sheets/detail/leishmaniasis.
- Bi, K. , Chen, Y., Zhao, S., Kuang, Y., & John Wu, C. H. (2018). Current visceral leishmaniasis research: a research review to inspire future study. BioMed research international, 2018.
- Lun, Z. R. , Wu, M. S., Chen, Y. F., Wang, J. Y., Zhou, X. N., Liao, L. F.,... & Chang, K. P. (2015). Visceral leishmaniasis in China: an endemic disease under control. Clinical microbiology reviews, 28(4), 987-1004.
- Lypaczewski, P. , & Matlashewski, G. (2021). Leishmania donovani hybridisation and introgression in nature: a comparative genomic investigation. The Lancet Microbe, 2(6), e250-e258.
- Akuffo, H. , Costa, C., van Griensven, J., Burza, S., Moreno, J., & Herrero, M. (2018). New insights into leishmaniasis in the immunosuppressed. PLOS Neglected Tropical Diseases, 12(5), e0006375. [CrossRef]
- Freitas-Mesquita, A. L. , Dos-Santos, A. L. A., & Meyer-Fernandes, J. R. (2021). Involvement of Leishmania Phosphatases in Parasite Biology and Pathogeny. Frontiers in Cellular and Infection Microbiology, 11. [CrossRef]
- Centers for Disease Control and Prevention. (2019). CDC - DPDx - Leishmaniasis. Centers for Disease Control and Prevention. https://www.cdc.gov/dpdx/leishmaniasis/index.html.
- Rodrigues, A. V. , Valério-Bolas, A., Alexandre-Pires, G., Aires Pereira, M., Nunes, T., Ligeiro, D., Pereira da Fonseca, I., & Santos-Gomes, G. (2022). Zoonotic Visceral Leishmaniasis: New Insights on Innate Immune Response by Blood Macrophages and Liver Kupffer Cells to Leishmania infantum Parasites. Biology, 11(1), 100. [CrossRef]
- Chelbi, I. Chelbi, I., Maghraoui, K., Zhioua, S., Cherni, S., Labidi, I., Satoskar, A., Hamilton, J. G. C., & Zhioua, E. (2021). Enhanced attraction of sand fly vectors of Leishmania infantum to dogs infected with zoonotic visceral leishmaniasis. PLOS Neglected Tropical Diseases, 15(7), e0009647. [CrossRef]
- MOLLALO, A. , & KHODABANDEHLOO, E. (2016). Zoonotic cutaneous leishmaniasis in northeastern Iran: a GIS-based spatio-temporal multi-criteria decision-making approach. Epidemiology and Infection, 144(10), 2217–2229. [CrossRef]
- Romero, G. A. S. , & Boelaert, M. (2010). Control of Visceral Leishmaniasis in Latin America—A Systematic Review. PLoS Neglected Tropical Diseases, 4(1), e584. [CrossRef]
- van Griensven, J. van Griensven, J., & Diro, E. (2019). Visceral Leishmaniasis. Infectious Disease Clinics of North America, 33(1), 79–99. [CrossRef]
- Images.
- https://www.who.int/news-room/fact-sheets/detail/leishmaniasis.
- https://www.cdc.gov/parasites/images/leishmaniasis/Leishmania_LifeCycle.gif.
- https://timesofindia.indiatimes.com/topic/amphotericin-b.
- https://emedz.net/blog/miltefosine-impavido-miltex.
- http://acronymsandslang.com/acronym_image/339/e2eb9a535d51b30f91bb833683c9491e.jpg.
- https://d2gdaxkudte5p.cloudfront.net/system/images/P11000-25.0_.jpg.
- https://emedz.net/blog/wp-content/uploads/2020/05/pentamidine-injection-pentam-300-mg-uses-dose-side-effects-scaled.jpg.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).