1. Introduction
As global climate change intensifies, the impact of environmental factors on health has become a crucial research direction in the medical field. The increasing frequency of extreme weather events may significantly affect vulnerable groups, such as hemodialysis patients. Therefore, studying the influence of environmental factors on these patients has both immediate clinical significance and long-term public health value.
Recent studies have identified potential links between various environmental conditions and cardiovascular events, hospitalization rates, and mortality [
1,
2,
3,
4]. Environmental temperature changes, in particular, have been found to significantly affect blood pressure and alter the hemodynamics of peripheral and aortic vessels [
5,
6]. This influence extends beyond temperature, with variations in sunlight duration potentially associated with blood pressure fluctuations [
7]. These findings reveal the profound impact of environmental factors on human physiology and open new avenues for further research.
Environmental factors may influence the body through various physiological mechanisms, including activation of the sympathetic nervous system and promotion of hormone release, such as arginine vasopressin, norepinephrine, epinephrine, and angiotensin II [
3]. These complex physiological responses can lead to changes in endothelial function, affecting vasoconstriction and blood pressure regulation [
8]. Notably, these responses may vary among individuals, especially in populations with chronic diseases, such as hemodialysis patients. The effects of environmental factors may be more pronounced in these patients due to their compromised cardiovascular system and fluid balance regulation mechanisms [
9].
In the context of hemodialysis, blood pressure management is crucial. Studies show that blood pressure levels during dialysis, not just daily averages, are closely related to cardiovascular mortality and morbidity in patients [
9,
10,
11,
12]. Furthermore, blood pressure fluctuations during dialysis have been associated with increased risks of hospitalization and death [
13,
14]. These findings highlight the importance of understanding the various factors affecting blood pressure in dialysis patients and raise an important question: Can we improve patient outcomes by better understanding and managing these influencing factors?
The effects of environmental temperature on blood pressure are multifaceted. Cold weather can cause peripheral vasoconstriction, leading to increased blood pressure, while high temperatures can cause vasodilation, potentially lowering blood pressure [
15,
16]. These reactions may be more complex in hemodialysis patients, who may be more sensitive to temperature changes due to their altered cardiovascular physiology and fluid balance regulation mechanisms [
7]. However, the current research on how seasonal and specific meteorological changes affect hemodialysis patients remains limited, warranting further exploration.
In addition to temperature, other meteorological factors such as humidity, atmospheric pressure, and wind speed may also influence blood pressure [
17]. These factors may interact in complex ways, impacting patients’ physiological states. For example, high humidity can exacerbate the effects of high temperatures on blood pressure, while changes in atmospheric pressure may be associated with the incidence of cardiovascular events [
1]. Understanding these complex relationships requires more in-depth research.
Given the current state of research, this study aims to explore the potential associations between weather-related data and intradialytic blood pressure in dialysis patients. We aim to provide new scientific insights that could inform clinical practice by investigating these relationships. For example, if certain meteorological conditions are linked to blood pressure fluctuations, medical teams may adjust treatment plans in advance based on weather forecasts, potentially improving blood pressure control in hemodialysis patients.
2. Materials and Methods
Study Design and Population
This retrospective and longitudinal cohort study was conducted at a hospital in a subtropical region. Clinical data was gathered from a hemodialysis unit at a typical general hospital. The unit conducted 2,000-2,500 monthly hemodialysis sessions during the study period. Adult patients (age ≥ 18 years) with end-stage renal disease who underwent chronic hemodialysis between January 2016 and December 2020 were included. Due to the outbreak of Coronavirus disease 2019 (COVID-19) in January 2021, data collection was suspended after this date( due to outbreak of COVID19). Patients with a dialysis vintage of less than three months or over 90 years old were excluded from the study.
Data Acquirement
The data for this study was extracted from the Hospital Information System. The data were extracted and stored in the warehouse behind the firewall after being encoded for data privacy protection. These variables included demographic details, medical history, laboratory results, and medication profiles. The demographic data comprised age, gender, and medical conditions. Laboratory parameters included hemoglobin, potassium, sodium, calcium, phosphate, and albumin levels. Data from individual hemodialysis sessions encompassed metrics such as interdialysis weight gain, history of intradialytic hypotension, predetermined target body weight, and intradialytic blood pressure measurements.
The meteorological data for this study was sourced from the Central Weather Bureau’s official archives, which included hourly records of atmospheric pressure, ambient temperature, relative humidity, wind speed, and precipitation. Initially, hourly data was averaged, with precipitation summed to obtain daily values. Before linking to each dialysis session, the average weather data from the seven days preceding the dialysis day was calculated.
Outcome Variables
The primary outcome variables of this study were the average intradialytic systolic blood pressure (SBP), the difference between the maximum and minimum SBP (referred to as the SBP difference), and the average mean arterial pressure. The average SBP was calculated as the mean of multiple SBP measurements taken during dialysis. The SBP difference was subtracting the minimum SBP from the maximum SBP. The average mean arterial pressure was derived from the mean of multiple mean arterial pressure measurements.
Statistical Analysis
The analysis was conducted using STATA software. Linear regression and Generalized Estimation Equations (GEE) were used for statistical analysis. A p-value threshold of 0.05 was treated as significance.
Hypothesis
The initial hypothesis posited that meteorological variables autonomously impact intradialytic blood pressure, indicating a potential inherent correlation between these external environmental factors and patient-specific clinical outcomes.
3. Results
Demographic, Clinical, and Meteorological Characteristics
In this cohort, 224 patients met the inclusion criteria and were subsequently subjected to detailed analysis. The demographic and clinical attributes can be found in
Table 1. The cohort’s mean age was 67.84, with a standard deviation of 11.04. Most participants were male, constituting 63.3% (n=143) of the total sample. A significant proportion of the study population, 88.8% (n=199), had been diagnosed with diabetes mellitus. Hypertension was prevalent in 83.9% (n=188) of the patients. Additionally, dyslipidemia was identified in 60.2% (n=135) of the cohort.
Further examination of the cohort’s medical history revealed the presence of several comorbidities. Specifically, coronary artery disease was diagnosed in 13.8% (n=31) of the patients, hypothyroidism in 8.4% (n=19), a prior incidence of stroke in 9.8% (n=22), and peripheral obstructive artery disease was observed in a smaller fraction, 2.6% (n=6), of the participants.
Meteorological Variables
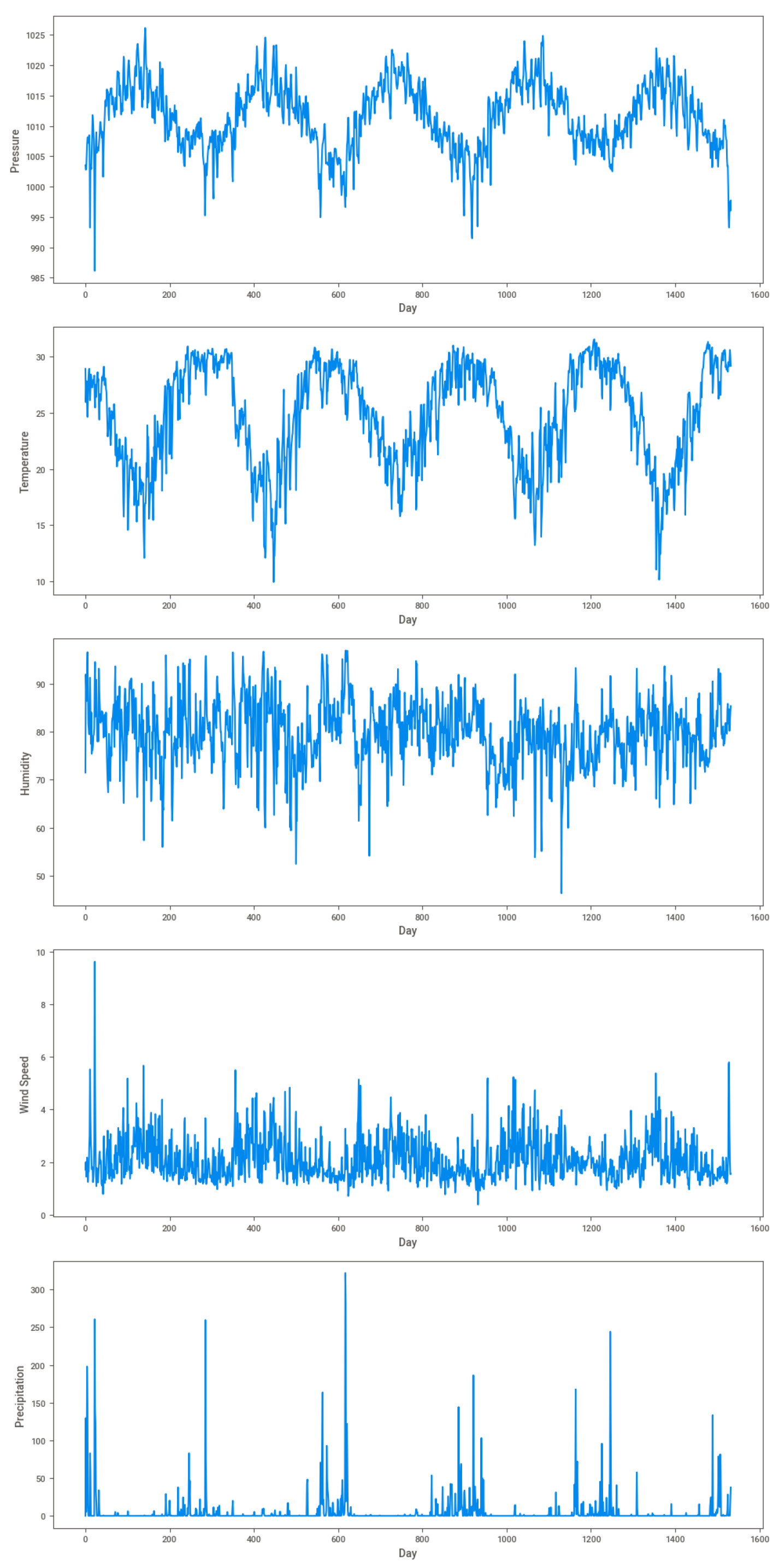
The time series plots (
Figure 1) illustrate the variations in atmospheric pressure, temperature, humidity, wind speed, and precipitation over the study period. Atmospheric pressure and temperature exhibit seasonal fluctuations, with temperature variations centered around a mean of 17.5°C. Humidity levels display considerable dispersion, with fluctuations showing less pronounced seasonal differences than pressure and temperature. Wind speeds predominantly remain below four m/s, indicating generally calm weather conditions. Precipitation demonstrates a highly skewed distribution characterized by distinct intermittent patterns. The time series graphs clearly show that the temporal distributions of wind speed and precipitation align with those of temperature and atmospheric pressure.
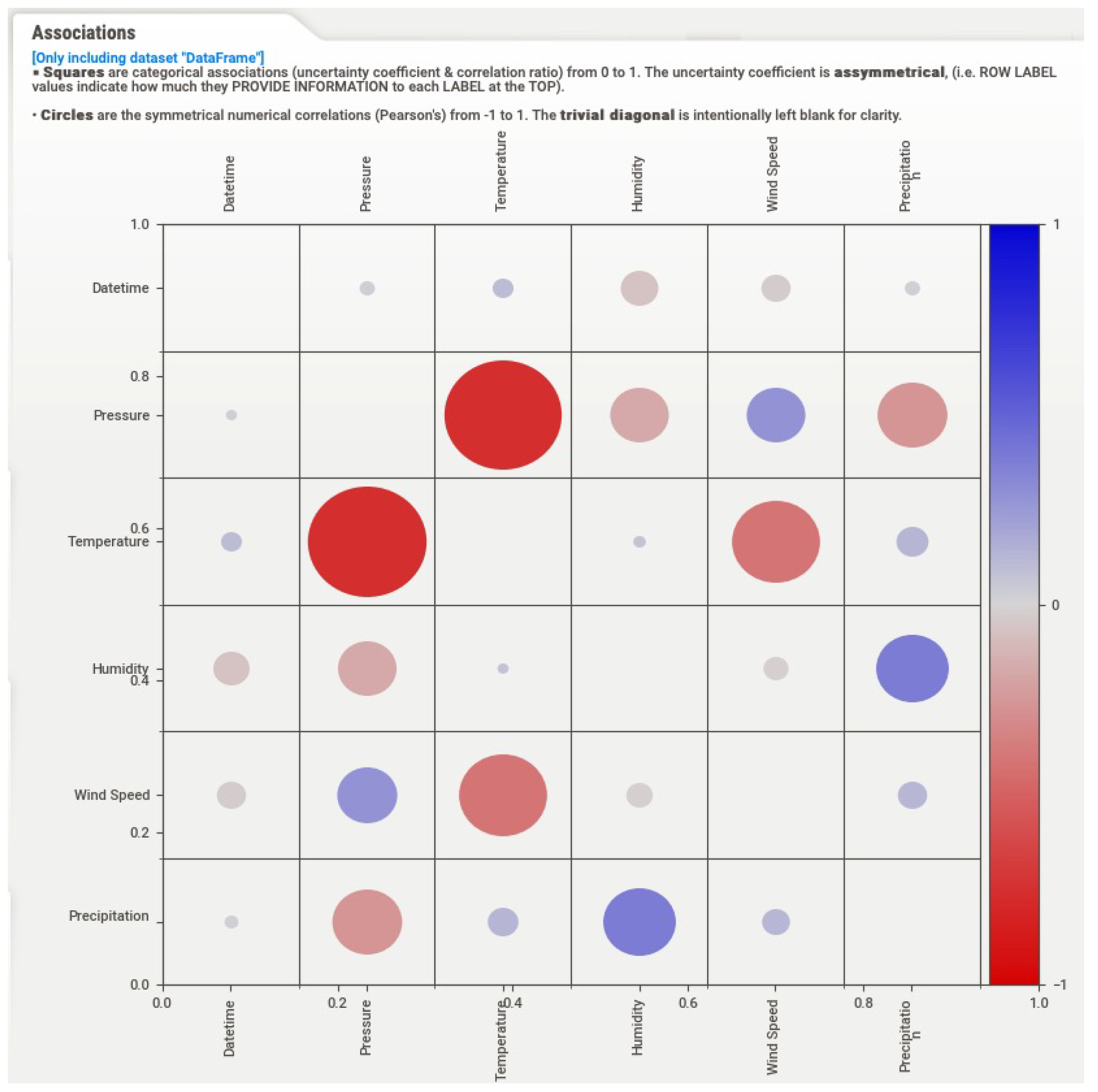
The correlation matrix (
Figure 2) reveals the relationships among the studied variables. Atmospheric pressure exhibits a weak negative correlation with temperature and humidity. Temperature demonstrates a robust inverse relationship with atmospheric pressure and wind speed, with higher temperatures typically corresponding to lower atmospheric pressure and wind speeds. Humidity shows a positive correlation with precipitation and a slight negative correlation with temperature.
Associations Between Clinical and Meteorological Factors with Mean Systolic Pressure
The Generalized Estimating Equation (GEE) analysis examining the associations between clinical and meteorological factors and average systolic blood pressure (SBP) in hemodialysis patients is summarized in
Table 2. Age, gender, and diabetes showed no significant associations with SBP (Coefficients = -0.141, 0.449, and 1.033; P-values = 0.193, 0.859, and 0.765, respectively). Hypertension exhibited a positive but non-significant association (Coefficient = 5.478, P = 0.073).
Among clinical factors, dyslipidemia showed a significant positive association with SBP (Coefficient = 4.139, P = 0.044). Erythropoiesis-stimulating agent (ESA) dosage also had a significant positive correlation (Coefficient = 5.049, P = 0.007). A history of intradialytic hypotension showed a strong negative association (Coefficient = -14.827, P < 0.001). Interdialytic weight gain was significantly negatively correlated with SBP (Coefficient = -2.526, P < 0.001). Hemoglobin levels had a significant negative association (Coefficient = -2.118, P < 0.001), as did serum potassium (Coefficient = -2.970, P = 0.006) and serum phosphate (Coefficient = -1.150, P = 0.007). In contrast, target body weight, serum albumin, serum sodium, and serum total calcium were not significantly associated with SBP.
Regarding meteorological factors, mean temperature had a significant inverse association with SBP (Coefficient = -0.206, P < 0.001). Mean wind speed also demonstrated a significant negative correlation (Coefficient = -0.363, P = 0.002). Mean humidity was negatively correlated with SBP (Coefficient = -0.044, P = 0.011). Additionally, daily precipitation was positively associated with SBP (Coefficient = 0.015, P < 0.001).
Associations Between Clinical and Meteorological Factors with Difference in Intradialytic Systolic Pressure
The Generalized Estimating Equation (GEE) analysis for associations between clinical and meteorological factors and the difference in intradialytic systolic pressure is summarized in
Table 3. Age, gender, coronary artery disease, and peripheral obstructive artery disease showed no significant correlation (Coefficients = -0.088, 0.144, -1.503, and -2.544; P-values = 0.412, 0.950, 0.469, and 0.748, respectively). Hypertension and erythropoiesis-stimulating agent (ESA) dosage had positive but non-significant associations (Coefficients = 1.821 and -3.790; P-values = 0.490 and 0.053, respectively). Diabetes showed a significant positive association (Coefficient = 7.399, P = 0.018).
A significant positive correlation was found for the history of intradialytic hypotension (Coefficient = 11.196, P < 0.001), and interdialytic weight gain showed a significant increase in SBP differences (Coefficient = 2.003, P < 0.001). In contrast, target body weight had a significant inverse relationship (Coefficient = -0.547, P < 0.001). Hemoglobin levels were positively associated (Coefficient = 1.715, P < 0.001). Serum potassium had a significant positive correlation (Coefficient = 3.426, P < 0.001). However, serum albumin, serum sodium, serum total calcium, and serum phosphate showed no significant associations (P-values = 0.353, 0.606, 0.068, and 0.112, respectively).
Regarding meteorological factors, mean temperature and mean humidity had significant inverse relationships with SBP differences (Coefficients = -0.282 and -0.050; P-values < 0.001 and 0.001, respectively). Mean wind speed now meets the significance threshold (Coefficient = -0.277, P = 0.048). Daily precipitation and atmospheric pressure showed no significant associations (P-values = 0.520 and 0.437, respectively).
Updated Table (witThe Generalized Estimating Equation (GEE) analysis for associations between clinical and meteorological factors and the difference in intradialytic systolic pressure is summarized in
Table 3. Age, gender, coronary artery disease, and peripheral obstructive artery disease showed no significant correlation (Coefficients = -0.088, 0.144, -1.503, and -2.544; P-values = 0.412, 0.950, 0.469, and 0.748, respectively). Hypertension and erythropoiesis-stimulating agent (ESA) dosage had positive but non-significant associations (Coefficients = 1.821 and -3.790; P-values = 0.490 and 0.053, respectively). Diabetes showed a significant positive association (Coefficient = 7.399, P = 0.018).
A significant positive correlation was found for the history of intradialytic hypotension (Coefficient = 11.196, P < 0.001), and interdialytic weight gain showed a significant increase in SBP differences (Coefficient = 2.003, P < 0.001). In contrast, target body weight had a significant inverse relationship (Coefficient = -0.547, P < 0.001). Hemoglobin levels were positively associated (Coefficient = 1.715, P < 0.001). Serum potassium had a significant positive correlation (Coefficient = 3.426, P < 0.001). However, serum albumin, serum sodium, serum total calcium, and serum phosphate showed no significant associations (P-values = 0.353, 0.606, 0.068, and 0.112, respectively).
Regarding meteorological factors, mean temperature and mean humidity had significant inverse relationships with SBP differences (Coefficients = -0.282 and -0.050; P-values < 0.001 and 0.001, respectively). Mean wind speed now meets the significance threshold (Coefficient = -0.277, P = 0.048). Daily precipitation and atmospheric pressure showed no significant associations (P-values = 0.520 and 0.437, respectively).
Associations Between Clinical and Meteorological Factors with Average Mean Arterial Pressure
The Generalized Estimating Equation (GEE) analysis results examining the associations between various clinical and meteorological factors and the mean arterial pressure in hemodialysis patients are presented in
Table 4.
The Generalized Estimating Equation (GEE) analysis results examining the associations between various clinical and meteorological factors and the mean arterial pressure in hemodialysis patients are presented in
Table 4.
The mean arterial pressure analysis revealed several significant associations. The erythropoiesis-stimulating agents (ESA) dosage showed a significant positive association (Coefficient = 3.448, P = 0.012). The vintage of intradialytic hypotension exhibited a strong negative association with mean arterial pressure (Coefficient = -10.395, P = 0.001), suggesting that patients with a history of intradialytic hypotension tend to have lower mean arterial pressure. Interdialytic weight gain was significantly negatively correlated with mean arterial pressure (Coefficient = -1.493, P < 0.001), as was hemoglobin level (Coefficient = -1.133, P < 0.001).
Among the serum electrolytes, serum potassium (Coefficient = -2.077, P = 0.001) and serum phosphate (Coefficient = -0.803, P = 0.002) showed significant negative associations with mean arterial pressure. Regarding meteorological factors, mean temperature (Coefficient = -0.092, P = 0.018), mean humidity (Coefficient = -0.031, P = 0.006), and wind speed (Coefficient = -0.234, P = 0.004) were all significantly inversely related to mean arterial pressure. Daily precipitation was positively associated with mean arterial pressure (Coefficient = 0.009, P < 0.001).
These results indicate that certain clinical factors, such as ESA dosage, serum electrolyte levels, and environmental conditions, such as temperature, humidity, wind speed, and precipitation, can significantly influence mean arterial pressure in hemodialysis patients.
Comparative Analysis of Significant Associations Across Blood Pressure Outcomes
To investigate the influence of weather on hemodialysis patients, our study employed a generalized estimating equation (GEE) model, adjusting for multiple clinical variables. This approach was particularly suitable for analyzing our longitudinal data, as GEE effectively accounts for correlations between repeated measurements within individual patients while providing robust parameter estimates, even without precise knowledge of the underlying correlation structure.
The analyses in our study revealed key clinical and meteorological factors significantly associated with average systolic blood pressure (SBP), intradialytic systolic pressure differences, and mean arterial pressure in hemodialysis patients.
Erythropoiesis-stimulating agent (ESA) dosage showed a significant positive association with both SBP (P = 0.012) and mean arterial pressure (P = 0.007). A history of intradialytic hypotension consistently exhibited a strong negative association across all outcomes, significantly correlated with lower SBP, intradialytic systolic pressure differences (P < 0.001), and mean arterial pressure (P = 0.001). Interdialytic weight gain was significantly negatively correlated with both SBP (P < 0.001) and mean arterial pressure (P < 0.001). In comparison, it showed a positive association with systolic pressure differences (P < 0.001), emphasizing the importance of fluid management.
Hemoglobin levels were negatively associated with both SBP (P < 0.001) and mean arterial pressure (P < 0.001) and positively correlated with systolic pressure differences (P < 0.001), suggesting its role in affecting both blood pressure levels and fluctuations. Serum potassium showed a significant negative relationship with SBP (P = 0.006) and mean arterial pressure (P = 0.001) but had a positive association with systolic pressure differences (P < 0.001), highlighting the need for optimal potassium management.
Regarding meteorological factors, the mean temperature had a significant inverse association with both SBP (P < 0.001) and systolic pressure differences (P < 0.001), and it was also significantly associated with mean arterial pressure (P = 0.018). Mean humidity was significantly inversely related to systolic pressure differences (P = 0.001) and mean arterial pressure (P = 0.006). Wind speed was negatively associated with SBP (P = 0.002), mean arterial pressure (P = 0.004), and systolic pressure differences (P = 0.048). Daily precipitation showed a positive relationship with both SBP (P < 0.001) and mean arterial pressure (P < 0.001).
In summary, ESA dosage, intradialytic hypotension history, interdialytic weight gain, hemoglobin, serum potassium, temperature, humidity, and wind speed were significant factors associated with hemodialysis patients’ blood pressure outcomes, emphasizing their multifactorial influence.
4. Discussion
This study provides novel insights into the complex interplay between clinical factors, meteorological conditions, and intradialytic blood pressure in hemodialysis patients. Our Generalized Estimating Equation (GEE) model, adjusting for crucial variables such as hypertension and diabetes, revealed significant associations between environmental factors and blood pressure outcomes.
Our results demonstrated a nuanced relationship between weather patterns and blood pressure dynamics:
Higher temperatures and stronger winds were associated with lower systolic blood pressure and mean arterial pressure.
Higher humidity correlated with lower mean arterial pressure and smaller changes in systolic pressure.
Interestingly, increased daily rainfall was linked to higher mean arterial pressure and systolic blood pressure.
These findings highlight the intricate influence of meteorological conditions on hemodialysis patients’ cardiovascular responses.
Among clinical factors, erythropoiesis-stimulating agent (ESA) dosage emerged as a significant variable, showing a positive correlation with both systolic blood pressure (SBP) and mean arterial pressure. This aligns with previous research suggesting ESA therapy’s impact on blood pressure regulation in hemodialysis patients. Additionally, a history of intradialytic hypotension and serum potassium levels significantly affected blood pressure outcomes.
The hemodialysis treatment itself plays a crucial role in blood pressure regulation. Our study found a significant negative correlation between interdialytic weight gain and mean arterial pressure, underscoring the importance of effective fluid management strategies. This finding emphasizes the need for maintaining optimal dry weight and preventing volume overload, which is key in managing hypertension among hemodialysis patients [
18].
In conclusion, our study reveals that both environmental and clinical variables critically influence blood pressure dynamics during hemodialysis. This comprehensive understanding offers new perspectives for patient management, suggesting the need for adaptive treatment strategies that consider both meteorological conditions and individual clinical factors to optimize blood pressure control in hemodialysis patients.
Weather and Intradialytic Blood Pressure
Our study significantly advances the understanding of the relationship between environmental factors and intradialytic blood pressure. We identified robust associations between meteorological conditions and blood pressure outcomes in hemodialysis patients. Specifically, our results revealed significant negative correlations between high ambient temperatures and both intradialytic systolic pressure and mean arterial pressure, aligning with previous findings [
5,
6].
The body’s response to heat involves systemic changes, primarily through peripheral vasodilation and sweating to reduce core temperature. This loss of peripheral resistance is counteracted by sympathetic activation, which helps prevent a sharp drop in blood pressure by increasing heart rate and stroke volume. Additionally, sweat-induced salt loss and reduced blood volume are particularly relevant for hemodialysis patients who already face challenges in fluid balance. Our study supports these mechanisms, highlighting the complexities of blood pressure regulation in patients exposed to varying temperature conditions [
12,
15].
Previous research has demonstrated the impact of humidity on blood pressure, with varying effects observed depending on individual and environmental factors. For instance, Guo et al. found that high relative humidity, particularly in conjunction with particulate matter exposure, can exacerbate hypertension in mice [
19]. Conversely, Sandi et al. observed that lower humidity levels (e.g., 40
Our findings revealed an interesting positive correlation between daily precipitation and mean arterial pressure, suggesting that increased rainfall might be associated with higher blood pressure levels in hemodialysis patients. To our knowledge, this is the first study to explore the relationship between precipitation and intradialytic blood pressure. While we didn’t directly measure patients’ activity levels or dietary habits, we believe that weather conditions, including rainfall, could influence these factors. Rainy weather might affect patients’ daily routines, potentially altering their physical activity and eating patterns, which in turn could impact their blood pressure. Although our study didn’t collect data on these specific behaviors, this observation opens up new avenues for future research to better understand the complex interplay between environmental factors, lifestyle choices, and blood pressure regulation in hemodialysis patients.
It’s important to note that our study didn’t account for indoor environmental conditions, such as the temperature and humidity within the dialysis facility. This limitation could influence our findings, as indoor factors like air conditioning, heating, and ventilation could modulate patients’ physiological responses to external weather. Despite this, understanding the influence of external meteorological data remains crucial as it offers insights into broader environmental factors that affect patient health and could inform preemptive care strategies.
Laboratory Data and Intradialytic Blood Pressure
Our study found a significant positive correlation between hemoglobin levels and intradialytic systolic pressure, aligning with previous findings [
20]. This correlation may be attributed to increased blood viscosity associated with higher hemoglobin levels, potentially affecting systolic and mean arterial pressure during dialysis.
Regarding serum potassium, our study found that pre-dialysis serum potassium was significantly associated with mean systolic and arterial pressure. Specifically, lower pre-dialysis potassium levels correlated with higher mean systolic and arterial pressures. This underscores the critical importance of maintaining optimal potassium levels for effective blood pressure management in hemodialysis patients.
Summary and Applications
This study is the first to analyze the association between ambient weather parameters and intradialytic blood pressure in hemodialysis patients in subtropical regions, including mean arterial pressure. Our findings reveal significant correlations between meteorological parameters and their specific effects on systolic blood pressure (SBP) and mean arterial pressure in hemodialysis patients.
Based on our findings, we propose several specific clinical applications:
Personalized treatment plans: Healthcare professionals should actively adjust dialysis treatment plans in response to seasonal and weather changes. This includes modifying medication dosages and dialysate composition to counteract fluctuations in SBP and mean arterial pressure.
Dynamic fluid management: Implement weather forecast-based fluid management strategies, especially during extreme weather conditions. By closely monitoring and adjusting interdialytic weight gain, clinicians can better maintain stable blood pressure levels and minimize the risk of fluctuations.
Patient education: Actively educate patients on how to protect themselves against the impacts of weather changes on blood pressure. Encourage wearing appropriate clothing during colder months or ensuring adequate hydration in warmer conditions to mitigate temperature-related blood pressure effects.
Environmental control: Although this study focused on external weather conditions, dialysis centers should take immediate action to optimize indoor environmental control measures. This includes adjusting room temperature and humidity levels to mitigate external weather impacts on patients’ intradialytic blood pressure.
This work lays the foundation for the future development of weather forecast-based blood pressure prediction models that include mean arterial pressure as a key parameter. Such models could allow medical teams to anticipate and prevent potential blood pressure fluctuations in advance, thereby improving patients’ long-term health outcomes.
Given the trend of global climate change, this study’s implications are even more significant. As global temperatures rise, hemodialysis patients may experience more pronounced blood pressure fluctuations. Our research provides a scientific basis for developing strategies to address these challenges, including modifying dialysis treatment plans based on seasonal and weather conditions.
5. Conclusions
This comprehensive four-year analysis underscores the complex interplay between environmental factors and clinical variables in influencing intradialytic blood pressure in hemodialysis patients. Our findings show that higher ambient temperatures, increased humidity, stronger wind speeds, and lower precipitation levels are significantly associated with lower systolic blood pressure (SBP) and mean arterial pressure. Clinical factors, particularly hemoglobin levels and serum potassium, also play a crucial role in blood pressure regulation during dialysis sessions.
These results emphasize the necessity of incorporating environmental variables into blood pressure predictive models and adapting treatment protocols to account for seasonal changes. Proactive measures, such as weather-adapted fluid management strategies, personalized treatment plans, and patient education, are essential for mitigating potential adverse effects on blood pressure and improving patient outcomes. As global temperatures continue to rise, these insights offer a foundation for developing tailored interventions that ensure effective, patient-centered care, ultimately enhancing the quality of life for hemodialysis patients.
Author Contributions
Conceptualization, Lin HM.; methodology, Lin HM.; software, Lin HM.; validation, Lin HM., Lyu JJ.; formal analysis, Lin HM.; original draft preparation, Lin HM.; Review and editing, Lyu JJ.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Institutional Review Board (IRB) of An-Nan Hospital, Tainan, Taiwan, approved the study (IRB REC number: TMANH107-REC006CR2).
Informed Consent Statement
"Patient consent was waived as this study utilized a retrospective database, making it impractical to obtain consent from individual patients
Data Availability Statement
The data used in this study is unavailable due to ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| GEE |
Generalized Estimating Equations |
| SBP |
systolic blood pressure |
| COVID-19 |
Coronavirus disease 2019 |
References
- Dilaveris, P.; Synetos, A.; Giannopoulos, G.; Gialafos, E.; Pantazis, A.; Stefanadis, C. CLimate Impacts on Myocardial Infarction Deaths in the Athens TErritory: The CLIMATE Study. Heart (British Cardiac Society) 2006, 92, 1747–1751. [Google Scholar] [CrossRef] [PubMed]
- Gerber, Y.; Jacobsen, S.J.; Killian, J.M.; Weston, S.A.; Roger, V.L. Seasonality and Daily Weather Conditions in Relation to Myocardial Infarction and Sudden Cardiac Death in Olmsted County, Minnesota, 1979 to 2002. Journal of the American College of Cardiology 2006, 48, 287–292. [Google Scholar] [CrossRef] [PubMed]
- See, C.Y.; Tseng, C.T.; Lin, W.R.; Chao, J.Y.; Kuo, T.H.; Wang, M.C. Seasonal Change in Home Blood Pressure Monitoring Is Associated With Renal Outcome and Mortality in Patients With Chronic Kidney Disease. Frontiers in Medicine 2021, 8, 672651. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Kario, K.; Chia, Y.C.; Turana, Y.; Chen, C.H.; Buranakitjaroen, P.; Nailes, J.; Hoshide, S.; Siddique, S.; Sison, J.; Soenarta, A.A.; Sogunuru, G.P.; Tay, J.C.; Teo, B.W.; Zhang, Y.Q.; Shin, J.; Van Minh, H.; Tomitani, N.; Kabutoya, T.; Sukonthasarn, A.; Verma, N.; Wang, T.D.; Wang, J.G.; HOPE Asia Network. The Influence of the Ambient Temperature on Blood Pressure and How It Will Affect the Epidemiology of Hypertension in Asia. Journal of Clinical Hypertension (Greenwich, Conn.) 2020, 22, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Adamopoulos, D.; Vyssoulis, G.; Karpanou, E.; Kyvelou, S.M.M.; Argacha, J.F.F.; Cokkinos, D.; Stefanadis, C.; van de Borne, P. Environmental Determinants of Blood Pressure, Arterial Stiffness, and Central Hemodynamics. Journal of Hypertension 2010, 28, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Wang, J.; Tian, J.; Tang, X.; Yu, C.; Marshall, R.J.; Chen, D.; Cao, W.; Zhan, S.; Lv, J.; Lee, L.; Hu, Y. Association between Ambient Temperature and Blood Pressure and Blood Pressure Regulators: 1831 Hypertensive Patients Followed up for Three Years. PLoS One 2013, 8, e84522. [Google Scholar] [CrossRef] [PubMed]
- Aubinière-Robb, L.; Jeemon, P.; Hastie, C.E.; Patel, R.K.; McCallum, L.; Morrison, D.; Walters, M.; Dawson, J.; Sloan, W.; Muir, S.; Dominiczak, A.F.; McInnes, G.T.; Padmanabhan, S. Blood Pressure Response to Patterns of Weather Fluctuations and Effect on Mortality. Hypertension 2013, 62, 190–6. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.n.; Wood, J.; Bergeron, A.L.; McBride, L.; Ball, C.; Yu, Q.; Pusiteri, A.E.; Holcomb, J.B.; Dong, J.f. Effects of Low Temperature on Shear-Induced Platelet Aggregation and Activation. Journal of Trauma and Acute Care Surgery 2004, 57, 216. [Google Scholar] [CrossRef] [PubMed]
- Flythe, J.E.; Xue, H.; Lynch, K.E.; Curhan, G.C.; Brunelli, S.M. Association of Mortality Risk with Various Definitions of Intradialytic Hypotension. J Am Soc Nephrol 2015, 26, 724–34. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Wang, W.; Wu, X.; Lv, J.; Cai, S.; Li, Y. Intra-Dialytic Blood Pressure Variability Is a Greater Predictor of Cardiovascular Events in Hemodialysis Patients. BMC Nephrology 2023, 24, 113. [Google Scholar] [CrossRef] [PubMed]
- Stefánsson, B.V.; Brunelli, S.M.; Cabrera, C.; Rosenbaum, D.; Anum, E.; Ramakrishnan, K.; Jensen, D.E.; Stålhammar, N.O. Intradialytic Hypotension and Risk of Cardiovascular Disease. Clinical Journal of the American Society of Nephrology 2014, 9, 2124–2132. [Google Scholar] [CrossRef] [PubMed]
- Shafi, T.; Sozio, S.M.; Bandeen-Roche, K.J.; Ephraim, P.L.; Luly, J.R.; St. Peter, W.L.; McDermott, A.; Scialla, J.J.; Crews, D.C.; Tangri, N.; Miskulin, D.C.; Michels, W.M.; Jaar, B.G.; Herzog, C.A.; Zager, P.G.; Meyer, K.B.; Wu, A.W.; Boulware, L.E. Predialysis Systolic BP Variability and Outcomes in Hemodialysis Patients. Journal of the American Society of Nephrology 2014, 25, 799–809. [CrossRef]
- Inrig, J.K.; Oddone, E.Z.; Hasselblad, V.; Gillespie, B.; Patel, U.D.; Reddan, D.; Toto, R.; Himmelfarb, J.; Winchester, J.F.; Stivelman, J.; Lindsay, R.M.; Szczech, L.A. Association of Intradialytic Blood Pressure Changes with Hospitalization and Mortality Rates in Prevalent ESRD Patients. Kidney International 2007, 71, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Inrig, J.K.; Patel, U.D.; Toto, R.D.; Szczech, L.A. Association of Blood Pressure Increases During Hemodialysis With 2-Year Mortality in Incident Hemodialysis Patients: A Secondary Analysis of the Dialysis Morbidity and Mortality Wave 2 Study. American journal of kidney diseases : the official journal of the National Kidney Foundation 2009, 54, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Castellani, J.W.; Young, A.J. Human Physiological Responses to Cold Exposure: Acute Responses and Acclimatization to Prolonged Exposure. Autonomic Neuroscience 2016, 196, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Jin, S.; Wang, C.; Yan, S.; Zhou, X.; Cui, X.; Tang, Z.; Luan, Q.; Guo, Y.; Bian, Z.; Li, L.; Chen, Z.; Na, L. The Association of Outdoor Temperature with Blood Pressure, and Its Influence on Future Cardio-Cerebrovascular Disease Risk in Cold Areas. Journal of Hypertension 2020, 38, 1080. [Google Scholar] [CrossRef] [PubMed]
- Danet, S.; Richard, F.; Montaye, M.; Beauchant, S.; Lemaire, B.; Graux, C.; Cottel, D.; Marécaux, N.; Amouyel, P. Unhealthy Effects of Atmospheric Temperature and Pressure on the Occurrence of Myocardial Infarction and Coronary Deaths. A 10-Year Survey: The Lille-World Health Organization MONICA Project (Monitoring Trends and Determinants in Cardiovascular Disease). Circulation 1999, 100, E1–7. [Google Scholar] [CrossRef] [PubMed]
- Van Buren, P.N.; Inrig, J.K. Mechanisms and Treatment of Intradialytic Hypertension. Blood Purification 2016, 41, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Li, B.; Peng, Q.; Yao, R.; Wu, Y.; Ma, P.; Du, C.; Liu, H.; Shu, Z.; Qin, S.; Yang, X.; Yu, W. Co-Exposure to Particulate Matter and Humidity Increases Blood Pressure in Hypertensive Mice via the TRPV4-cPLA2-COX2 Pathway. Ecotoxicology and Environmental Safety 2023, 255, 114800. [Google Scholar] [CrossRef] [PubMed]
- Hara, T.; Kasahara, Y.; Nakagawa, T. Pre-Dialysis Diastolic Blood Pressure and Intradialytic Hypotension in Patients Undergoing Maintenance Haemodialysis. J Nephrol 2022. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).