Submitted:
11 October 2024
Posted:
12 October 2024
You are already at the latest version
Abstract
Keywords:
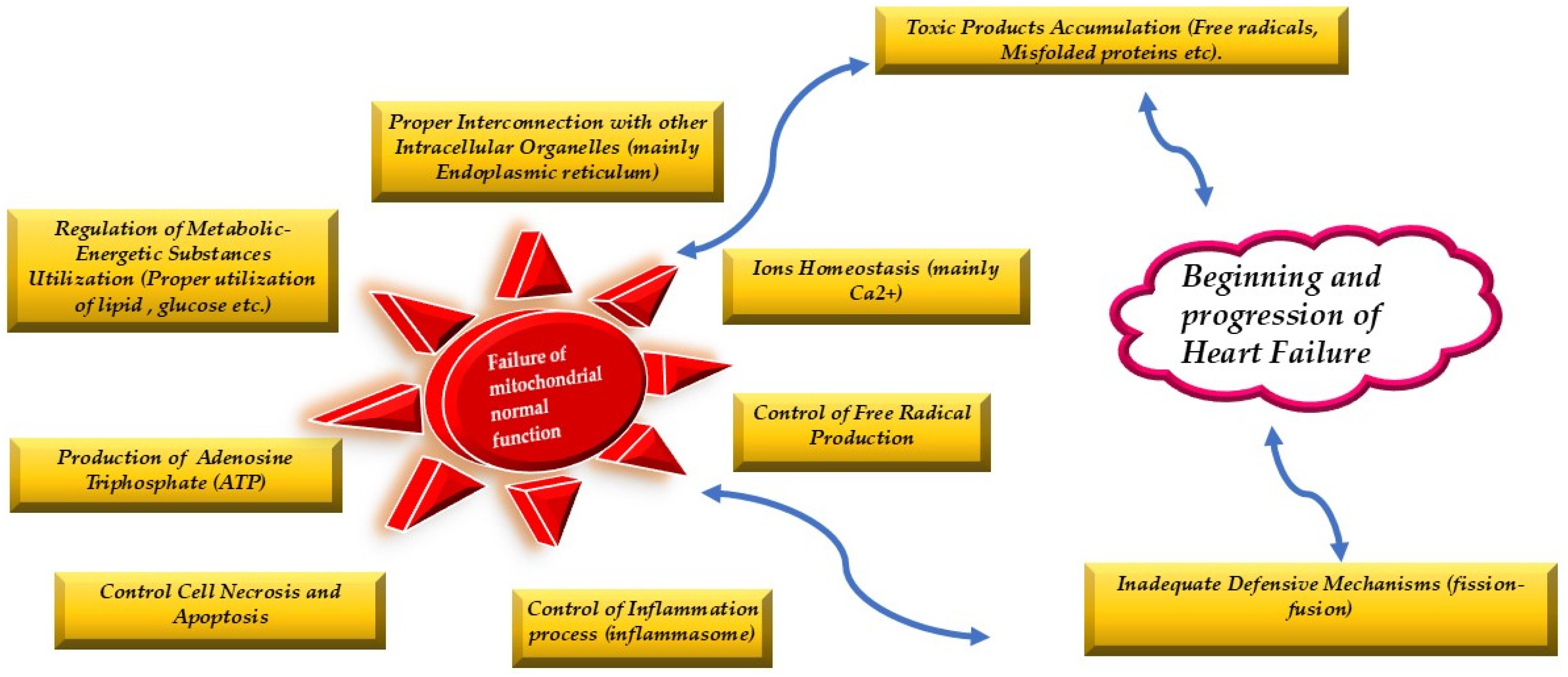
1. Introduction
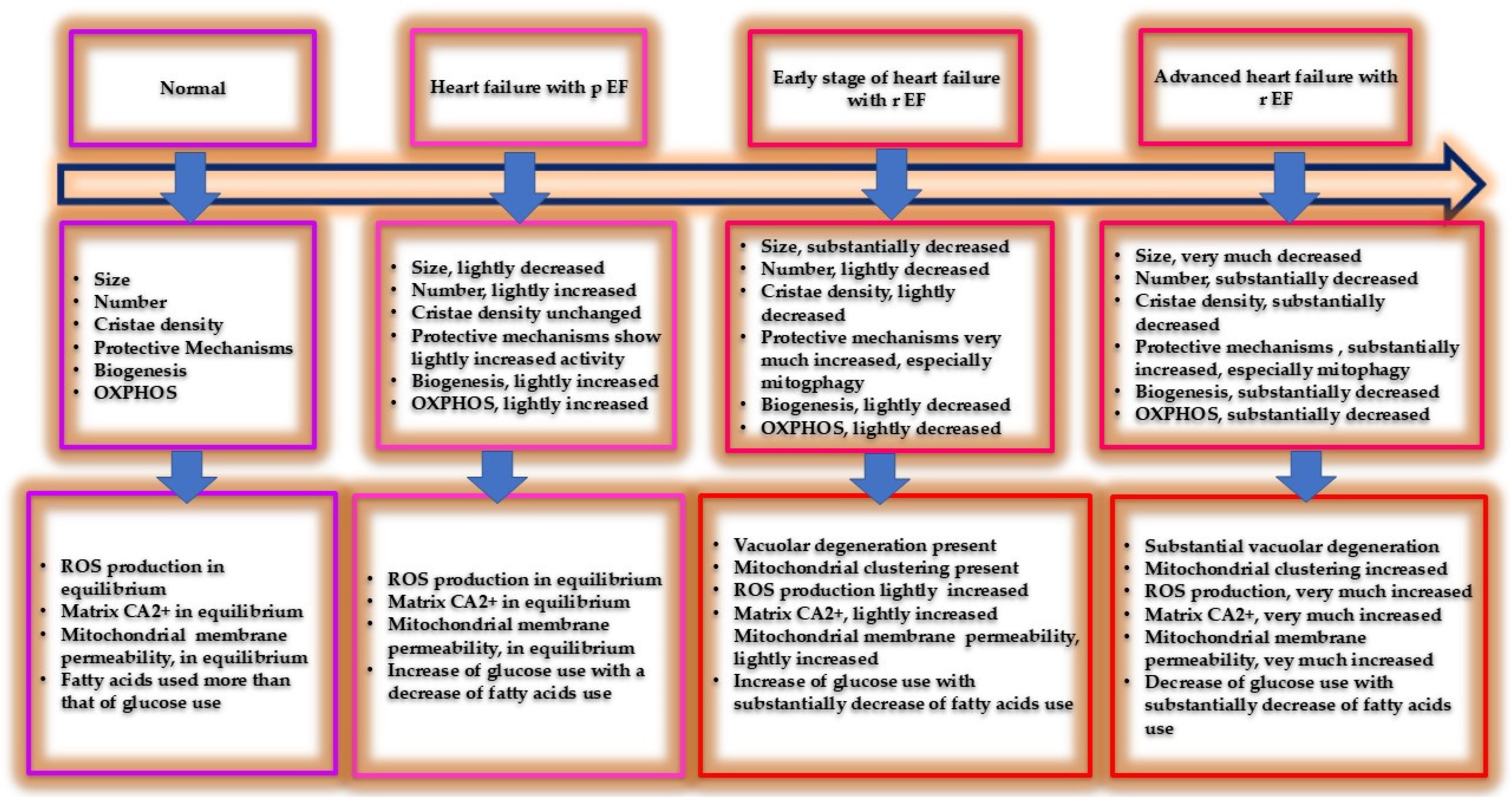
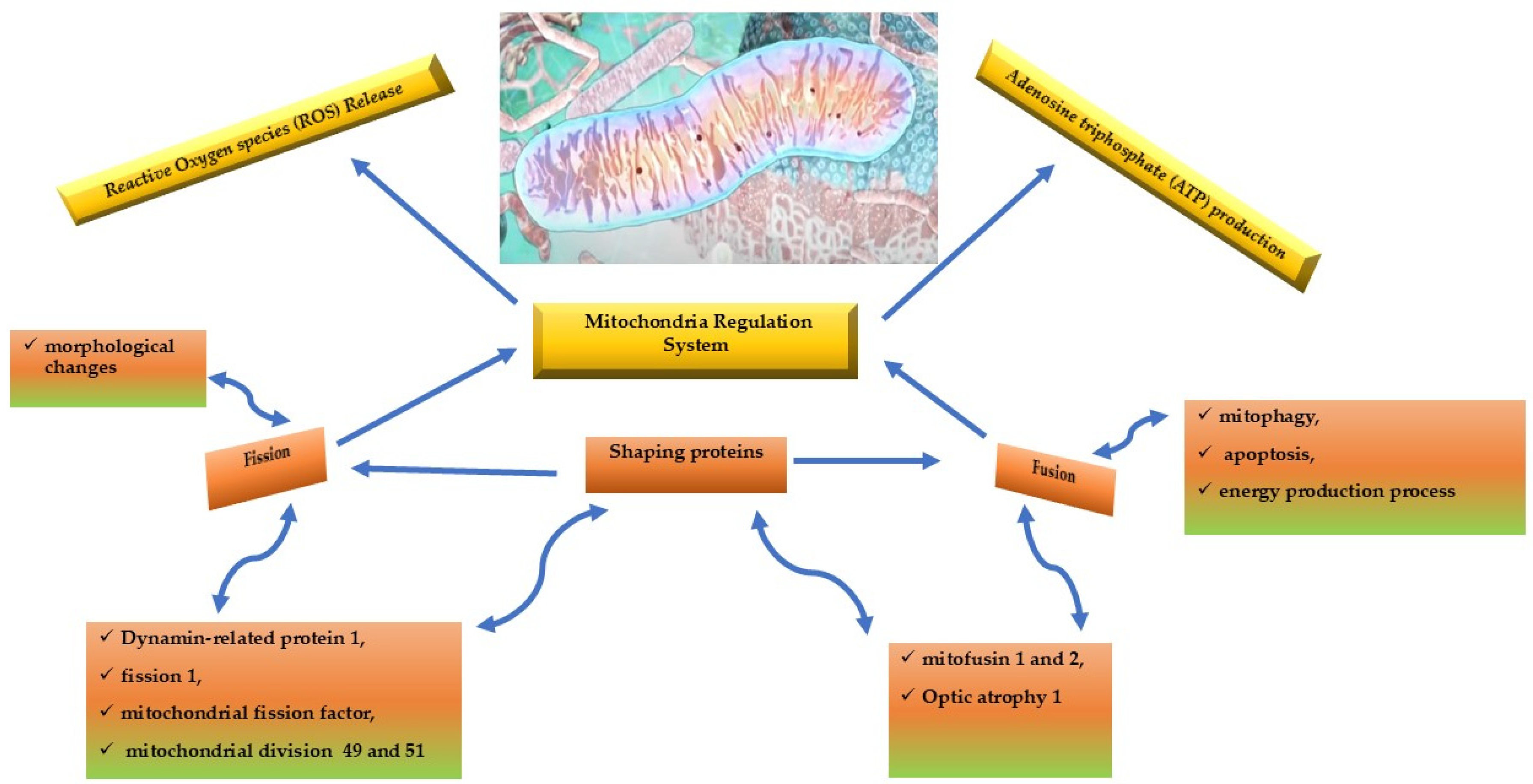
2. Mitochondrial Dynamics
3. Mitochondria, a ‘Socialized’ Organelle
3.1. Mitochondria—Endoplasmic Reticulum Connection
3.1.1. Mitochondria and Quadruple Therapy in Heart Failure Patients
3.2. Unusual Location of Mitochondria
4. Identify Mitochondria Dysfunction: Imaging Techniques and Biomarkers
5. Strategies to Keep Mitochondrial Structural and Functional Integrity
6. Future Directions
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Brown, DA.; Perry, JB.; Allen, ME.; Sabbah, HN.; Stauffer, BL; Shaikh, SR.; Cleland, JGF.; Colucci, WS.; Butler, J.; Voors, AA.; et al. Mitochondrial function as a therapeutic target in heart failure. Nat Rev Cardiol 2017;14:238-250.
- Balaban, R. S. Cardiac energy metabolism homeostasis: role of cytosolic calcium. J. Mol. Cell. Cardiol.2022; 34: 1259–1271.
- Neubauer, S. The Failing Heart — an Engine Out of Fuel. N Engl J Med 2007;356:1140-51.
- Beer, M.; Seyfarth, T.; Sandstede, J.; Landschutz, W.; Lipke, C.; Kostler, H.; von Kienlin, M.; Harre, K.; Hahn, D.; Neubauer, S. Absolute concentrations of high-energy phosphate metabolites in normal, hypertrophied, and failing human myocardium measured noninvasively with 31P SLOOP magnetic resonance spectroscopy. J. Am. Coll. Cardiol.2002; 40, 1267–1274.
- Phan, T. T.; Abozguia, K.; Shivu, GN.; Mahadevan, G.; Ahmed, I.; Williams, L.; Dwivedi ,G.; Patel, K.; Steendijk, P.; Ashrafian, H.; et al. Heart failure with preserved ejection fraction is characterized by dynamic impairment of active relaxation and contraction of the left ventricle on exercise and associated with myocardial energy deficiency. J. Am. Coll. Cardiol.2009; 54, 402–409.
- Torrent-Guasp, F.; Kocica, MJ. , Corno, A., Komeda, M., Cox, J., Flotats, A., Ballester-Rodes, M., Carreras-Costa, F. Systolic ventricular filling. European Journal of Cardio-thoracic Surgery. 2004; 25:376–386.
- Lopez-Crisosto, C. , Pennanen, Ch.; Vasquez-Trincado, C.; Morales, PE.; Bravo-Sagua, R.; Quest, AFG.; Chiong, M.; Lavandero, S. Sarcoplasmic reticulum–mitochondria communication in cardiovascular pathophysiology Nat Rev Cardiol. 2017;14: 342-360.
- Dorn, GW. Mitochondrial dynamism and heart disease: changing shape and shaping change. EMBO Mol Med 2015; 7: 865–877.
- Schon E., A.; Di Mauro, S.; Hirano, M. Human mitochondrial DNA: roles of inherited and somatic mutations. Nat. Rev. Genet. 2012; 13, 878–890.
- Dorn II, GW. Mitochondrial dynamism and heart disease: changing shape and shaping change. EMBO Mol Med 2015; 7: 865–877.
- Gallo, G.; Rubattu, S.; Volpe, M. Mitochondrial Dysfunction in Heart Failure: From Pathophysiological Mechanisms to Therapeutic Opportunities. Int. J. Mol. Sci. 2024; 25:2667.
- Zhou, B.; Tian, R. Mitochondrial dysfunction in pathophysiology of heart failure. J. Clin. Investig. 2018; 128:3716–3726.
- Chaanine, AH.; LeJemte, ThH.; Delafontaine, P. Mitochondrial Pathobiology and Metabolic Remodeling in Progression to Overt Systolic Heart Failure J. Clin. Med. 2020; 9: 3582.
- Chaanine, A.H.; Joyce, L.D.; Stulak, J.M.; Maltais, S.; Joyce, D.L.; Dearani, J.A.; Klaus, K.; Nair, K.S.; Hajjar, R.J.; Redfield, M.M. Mitochondrial morphology, dynamics, and function in human pressure overload or ischemic heart disease with preserved or reduced ejection fraction. Circ. Heart Fail. 2019; 12: e005131.
- Brustovetsky, N.; Brustovetsky, T.; Jemmerson, R.; Dubinsky, J.M. Calcium-induced cytochrome c release from CNS mitochondria is associated with the permeability transition and rupture of the outer membrane. J. Neurochem. 2002; 80: 207–218.
- Chaanine, A.H.; Kohlbrenner, E.; Gamb, S.I.; Guenzel, A.J.; Klaus, K.; Fayyaz, A.U.; Nair, K.S.; Hajjar, R.J.; Redfield, M.M. FOXO3a regulates BNIP3 and modulates mitochondrial calcium, dynamics, and function in cardiac stress. Am. J. Physiol. Circ. Physiol. 2016; 311: H1540–H1559.
- Chaanine, A.H. Morphological stages of mitochondrial vacuolar degeneration in phenylephrine-stressed cardiac myocytes and in animal models and human heart failure. Medicina 2019; 55: 239.
- Sun, M.G.; Williams, J.; Munoz-Pinedo, C.; Perkins, G.A.; Brown, J.M.; Ellisman, M.H.; Green, D.R.; Frey, T.G. Correlated three-dimensional light and electron microscopy reveals transformation of mitochondria during apoptosis. Nat. Cell Biol. 2007; 9: 1057–1065.
- Morciano, G.; Patergnani, S.; Bonora, M.; Pedriali, G.; Tarocco, A.; Bouhamida, E.; Marchi, S.; Ancora, G.; Anania, G.; Wieckowski, M.R.; et al. Mitophagy in cardiovascular diseases. J. Clin. Med. 2020; 9: 892.
- Chaanine, A.H. Autophagy and myocardial remodeling. J. Am. Coll. Cardiol. 2018; 71: 2011–2014.
- Kurz, T.; Terman, A.; Gustafsson, B.; Brunk, U.T. Lysosomes and oxidative stress in aging and apoptosis. Biochim. Biophys. Acta (BBA) Gen. Subj. 2008; 1780: 1291–1303.
- Terman, A.; Kurz, T.; Gustafsson, B.; Brunk, U.T. The involvement of lysosomes in myocardial aging and disease. Curr. Cardiol. Rev. 2008; 4: 107–115.
- Hernandez-Resendiz, S.; Prakash, A.; Loo, SL; Semenzato, M.; Chinda, K.; Crespo-Avilan, GE.; Dam, LC.; Lu, S.; Scorrano, L.; Hausenloy DH. Targeting mitochondrial shape: at the heart of cardioprotection. Basic Research in Cardiology 2023; 118:49.
- Jenkins, BC.; Neikirk, K.; Katti, P.; Claypoo, SM.; Kirabo, A.; McReynolds, MR.; Hinton, A., Jr. Mitochondria in disease: changes in shapes and dynamics. Trends Biochem Sci. 2024; 49: 346–360.
- Lobo-Jarne, T.; Ugalde, C. Respiratory chain supercomplexes: Structures, function and biogenesis. Semin. Cell Dev. Biol. 2017; 76: 179–190.
- Nesci S.; Trombetti F.; Pagliarani A.; Ventrella V;Algieri C.; Tioli G.; et al. Molecular and supramolecular structure of the mitochondrial oxidative phosphorylation system: Implications for pathology. Life 2021; 15:242.
- Valenti, D.; Vacca, R.A.; Moro, L.; Atlante, A. Mitochondria Can Cross Cell Boundaries: An Overview of the Biological Relevance, Pathophysiological Implications and Therapeutic Perspectives of Intercellular Mitochondrial Transfer. Int. J. Mol. Sci. 2021; 22: 8312.
- Ong, SB.; Hausenloy DJ. Mitochondrial morphology and cardiovascular disease. Cardiovasc. Res 2010; 88: 16–29.
- Shanmughapriya, S.; Langford, D.; Natarajaseenivasan, K. Inter and Intracellular mitochondrial trafficking in health and disease. Ageing Res. Rev. 2020; 62: 101128.
- Ahmad, T.; Mukherjee, S.; Pattnaik, B.; Kumar, M.; Singh, S.; Rehman, R.; Tiwari, B.K.; Jha, K.A.; Barhanpurkar, A.P.; Wani, M.R.; et al. Miro1 regulates intercellular mitochondrial transport & enhances mesenchymal stem cell rescue efficacy. EMBO J. 2014; 33: 994–1010.
- Sansone, P.; Savini, C.; Kurelac, I.; Chang, Q.; Amato, L.B.; Strillacci, A.; Stepanova, A.; Iommarini, L.; Mastroleo, C.; Daly, L.; et al. Packaging and transfer of mitochondrial DNA via exosomes regulate escape from dormancy in hormonal therapy-resistant breast cancer. Proc. Natl. Acad. Sci. USA 2017; 114: E9066–E9075.
- Phinney, D.; Di Giuseppe, M.; Njah, J.; Sala-Llinas, E.; Shiva, S.; Croix, C.M.S.; Stolz, D.B.; Watkins, S.; Di, Y.P.; Leikauf, G.; et al. Mesenchymal stem cells use extracellular vesicles to outsource mitophagy and shuttle microRNAs. Nat. Commun. 2015; 6: 8472.
- Pitt, J.M.; Kroemer, G.; Zitvogel, L. Extracellular vesicles: Masters of intercellular communication and potential clinical interventions. J. Clin. Investig. 2016; 126: 1139–1143.
- Paolicelli, R.C.; Bergamini, G.; Rajendran, L. Cell-to-cell Communication by Extracellular Vesicles: Focus on Microglia. Neuroscience 2019; 405: 148–157.
- Yao, Y.; Fan, X.-L.; Jiang, D.; Zhang, Y.; Li, X.; Xu, Z.-B.; Fang, S.-B.; Chiu, S.; Tse, H.-F.; Lian, Q.; et al. Connexin 43-mediated mitochondrial transfer of iPSC-MSCs alleviates asthma inflammation. Stem Cell Rep. 2018; 11: 1120–1135.
- Lyamzaev, K.G.; Nepryakhina, O.K.; Saprunova, V.B.; Bakeeva, L.E.; Pletjushkina, O.Y.; Chernyak, B.; Skulachev, V.P. Novel mechanism of elimination of malfunctioning mitochondria (mitoptosis): Formation of mitoptotic bodies and extrusion of mitochondrial material from the cell. Biochim. Biophys. Acta (BBA) Bioenerg. 2008; 1777:, 817–825.
- Shami, GJ.; Cheng, D.; Verhaegh, Koek G. Three-dimensional ultrastructure of giant mitochondria in human nonalcoholic fatty liver disease. Sci. Rep 2021;11:3319.
- Vincent, AE.; White, K.; Daney, T.; Philips, J.; Ogden, RT.; Lawless, C.; Warren, C.; Hall, MG.; Ng, YS.; Falkous, G.; et al. (2019) Quantitative 3D mapping of the human skeletal muscle mitochondrial network. Cell Rep. 2019; 26: 996–1009.e4.
- Glancy, B.; Kim, Y.; Katti, P.; Willingham, TB. The functional impact of mitochondrial structure across subcellular scales. Front. Physiol 2020;11, 541040.
- Lewis, SC.; Uchiyama, SC.; Nunnari, J. ER-mitochondria contacts couple mtDNA synthesis with mitochondrial division in human cells. Science 2016; 353: aaf5549.
- Bravo-Sagua, R.; Torrealba, N.; Paredes, F.; Morales, PE.; Pennanen, C.; López-Crisosto, C.; Troncoso, R.; Criollo, A.; Chiong, M.; Hill, JA.; et al. Organelle communication: Signaling crossroads between homeostasis and disease. The International Journal of Biochemistry & Cell Biology2014; 50:55-59v.
- Szymanski, J.; Janikiewicz, J.; Michalska, B.; Patalas-Krawczyk, P.; Perrone, M,; Ziółkowski, W.; Duszynski, J.; Pinton, P.; Dobrzyn, A.; Wieckowski, MR. Interaction of Mitochondria with the Endoplasmic Reticulum and Plasma Membrane in Calcium Homeostasis, Lipid Trafficking and Mitochondrial Structure. Int. J. Mol. Sci. 2017; 18: 1576.
- Murley, A.; Nunnari, J. The emerging network of mitochondria-organelle contacts. Mol Cell. 2016; 61: 648–653.
- Picca, A.; Guerra, F.; Calvani, R.; Romano, R.; Coelho-Junior, H.J.; Damiano, F.P.; Bucci, C.; Marzetti, E. Circulating Mitochondrial DNA and Inter-Organelle Contact Sites in Aging and Associated Conditions. Cells 2022; 11: 675.
- Wong, Y.C.; Ysselstein, D.; Krainc, D. Mitochondria-lysosome contacts regulate mitochondrial fission via RAB7 GTP hydrolysis. Nature 2018; 554: 382–386.
- Mattiazzi Ušaj, M.; Brložnik, M.; Kaferle, P.; Žitnik, M.; Wolinski, H.; Leitner, F.; Kohlwein, S.D.; Zupan, B.; Petrovič, U. Genome-wide localization study of yeast Pex11 identifies peroxisome-mitochondria interactions through the ERMES complex. J. Mol. Biol.2015; 427: 2072–2087.
- Benador, I.Y.; Veliova, M.; Liesa, M.; Shirihai, O.S. Mitochondria bound to lipid droplets: Where mitochondrial dynamics regulate lipid storage and utilization. Cell Metab. 2019; 29: 827–835.
- Ren, J.; B,i Y.; Sowers, J.;, Hetz,.; Zhang, Y. Endoplasmic reticulum stress and unfolded protein response in cardiovascular diseases. Nat Rev Cardiol. 2021; 18: 499-521.
- Zhou, H.; Wang, S.; Hu, S.; Chen, Y.; Ren, J. ER mitochondria microdomains in cardiac ischemia-reperfusion injury: a fresh perspective. Front. Physiol. 2018a; 9:755.
- Gao, P.; Yan, Z.; Zhu, Z. Mitochondria-associated endoplasmic reticulum membranes in cardiovascular diseases. Front. Cell Dev. Biol. 2020; 8: 604240.
- Bayeva, M.; Sawicki, K. T.; Butler, J.; Gheorghiade, M.; Ardehali, H. Molecular and cellular basis of viable dysfunctional myocardium. Circ. Heart Fail. 2014; 7: 680–691.
- Chen, Q.; Thompson, J.; Hu, Y.; Lesnefsky, E. J. Chronic metformin treatment decreases cardiac injury during ischemia-reperfusion by attenuating endoplasmic reticulum stress with improved mitochondrial function. Aging 2021;13:7828–7845.
- Grings, M.; Seminotti, B.; Karunanidhi, A.; Ghaloul-Gonzalez, L; Mohsen, A.; Wipf, P.; Palmfeldt, J.; Vockley, J.; Leipnitz, G. ETHE1 and MOCS1 deficiencies: disruption of mitochondrial bioenergetics, dynamics, redox homeostasis and endoplasmic reticulum-mitochondria crosstalk in patient fibroblasts. Sci. Rep. 2019; 9:12651.
- Bagur, R.; Hajnóczky, G. Intracellular Ca sensing: its role in calcium homeostasis and signaling. Mol. Cell 217;66: 780–788.
- Biczo, G.; Vegh, E.; Shalbueva, N.; Mareninova, O.; Elperin, J.; Lotshaw, E. ; Gretler, S,; Lugea, A.; Malla, SR.; Dawsonet, D.; et al. Mitochondrial dysfunction, through impaired autophagy, leads to endoplasmic reticulum stress, deregulated lipid metabolism, and pancreatitis in animal models. Gastroenterology 2018; 154: 689–703.
- Chaanine, A.H.; Gordon, R.E.; Kohlbrenner, E.; Benard, L.; Jeong, D.; Hajjar, R.J. Potential role of BNIP3 in cardiac remodeling, myocardial stiffness, and endoplasmic reticulum: Mitochondrial calcium homeostasis in diastolic and systolic heart failure. Circ.Heart Fail. 2013, 6, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.; Chen, W.; Hua, Y.; Jia, H.; Song, Y.; Wang, Y. Aerobic exercise ameliorates cardiac hypertrophy by regulatingmitochondrial quality control and endoplasmic reticulum stress through M2AChR. J. Cell. Physiol. 2021, 236, 6581–6596. [Google Scholar] [CrossRef] [PubMed]
- Paraskevaidis, I.; Farmakis, D.; Papingiotis, G.; Tsougos, E. Inflammation and Heart Failure: Searching for the Enemy—Reaching the Entelechy. J. Cardiovasc. Dev. Dis. 2023, 10, 19. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, X.; Wen, Y.; Li, S.; Lu, X.; Xu, R.; Li, C. Endoplasmic Reticulum-Mitochondria Contacts: A Potential Therapy Target for Cardiovascular, Remodeling-Associated Diseases. Front. Cell Dev. Biol. 2021;9:774989.
- Shi, Y.; Liu, L.; Deng, C.; Zhao, T.; Shi, Z.; Yan, J.; Gong, YZ.; Liao, DF.; Qin, L. Celastrol ameliorates vascular neointimal hyperplasia through Wnt5a-involved autophagy. Int. J. Biol. Sci. 2021;17, 2561–2575.
- Sciarretta, S.; Forte, M.; Frati, G.; Sadoshima, J. New insights into the role of mTOR signaling in the cardiovascular system. Circ. Res. 2018a, 122, 489–505. [Google Scholar] [CrossRef]
- Sciarretta, S.; Maejima, Y.; Zablocki, D.; Sadoshima, J. The role of autophagy in the heart. Annu. Rev. Physiol. 2018b; 80, 1–26.
- Kimball, T.; Vondriska, T. Metabolism, epigenetics, and causal inference in heart failure. Trends Endocrinol. Metab. 2020;31, 181–191.
- Lebeau, J.; Saunders, J.; Moraes, V.; Madhavan, A.; Madrazo, N.; Anthony, M.; Wiseman, RL. The PERK arm of the unfolded protein response regulates mitochondrial morphology during acute endoplasmic reticulum stress. Cell Rep. 2018;22: 2827–2836.
- Akhmedov, A.; Rybin, V.; Marín-García, J. Mitochondrial oxidative metabolism and uncoupling proteins in the failing heart. Heart Fail. Rev. 2015;20: 227–249.
- Nunnari, J.; Suomalainen, A. Mitochondria: in sickness and in health. Cell 2012;148: 1145–1159.
- Reddish, F. N.; Miller, C. L.; Gorkhali, R.; Yang, J. J. Calcium dynamics mediated by the endoplasmic/sarcoplasmic reticulum and related diseases. Int.J. Mol. Sci. 2017;18:1024.
- Lee, S.; Min, K. The interface between ER and mitochondria: molecular compositions and functions. Mol. Cells 2018;41:1000–1007.
- Ruan, L.; Wang, Y.; Zhang, X.; Tomaszewski, A.; McNamara, J.; Li, R. Mitochondria-associated proteostasis. Annu. Rev. Biophys. 2020; 49, 41–67.
- De Stefani, D.; Rizzuto, R.; Pozzan, T. Enjoy the trip: calcium in mitochondria back and forth. Annu. Rev. Biochem. 2016;85, 161–192.
- Raffaello, A; Mammucari, C.; Gherardi, G.; Rizzuto, R. Calcium at the center of cell signaling: interplay between endoplasmic reticulum, mitochondria, and lysosomes. Trends Biochem. Sci. 2016;41:1035–1049.
- Yousuf, M.S.; Maguire, A.D.; Simmen, T.; Kerr, B.J. Endoplasmic reticulum-mitochondria interplay in chronic pain: the calcium connection. Mol. Pain 2020; 16:1744806920946889.
- Tuncay, E.; Bitirim, C. V.; Olgar, Y.; Durak, A.; Rutter, G. A.; Turan, B. Zn(2+)-transporters ZIP7 and ZnT7 play important role in progression of cardiac dysfunction via affecting sarco(endo)plasmic reticulum-mitochondria coupling in yperglycemic cardiomyocytes. Mitochondrion 2019;44, 41–52.
- Liu, X.; Kwak, D.; Lu, Z.; Xu, X.; Fassett, J.; Wang, H.; et al. Endoplasmic reticulum stress sensor protein kinase R-like endoplasmic reticulum kinase (PERK) protects against pressure overload-induced heart failure and lung remodeling. Hypertension 2014; 64, 738–744.
- Li, Y.; Wang, X.; Lou, C. Gastrodin pretreatment impact on sarcoplasmic reticulum calcium transport ATPase (SERCA) and calcium phosphate (PLB) expression in rats with myocardial ischemia reperfusion. Med. Sci. Monit. 2016;22, 3309–3315.
- Silva-Palacios, A.; Zazueta, C.; Pedraza-Chaverri, J. ER membranes associated with mitochondria: possible therapeutic targets in heartassociated diseases. Pharmacol. Res. 202;156:104758.
- Brown, DA.; Perry, JB.; Allen, ME.; Sabbah, HN.; Stauffer, BL.; Shaikh, SR.; Cleland, JGF.; Colucci, WS.; Butler, J.; Voors, AA.; et al. Mitochondrial function as a therapeutic target in heart failure. Nat Rev Cardiol. 2017;14(4):238-250.
- Safari, F.; Bayat, G.; Shekarforoush, S.; Hekmatimoghaddam, S.; Anvari, Z.; Moghadam, M.F.; Hajizadeh, S. Expressional profile of cardiac uncoupling protein-2 following myocardial ischemia reperfusion in losartan- and ramiprilat-treated rats. J. Renin-Angiotensin-Aldosterone Syst. JRAAS 2014, 15, 209–217. [Google Scholar] [CrossRef]
- Kojic, Z.; Gopcevic, K.; Marinkovic, D.; Tasic, G. Effect of captopril on serum lipid levels and cardiac mitochondrial oxygen consumption in experimentally-induced hypercholesterolemia in rabbits. Physiol. Res. 2011;60 (Suppl. 1): S177–S184.
- Djanani, A.; Kaneider, N.C.; Meierhofer, C.; Sturn, D.; Dunzendorfer, S.; Allmeier, H.; Wiedermann, C.J. Inhibition of neutrophil migration and oxygen free radical release by metipranolol and timolol. Pharmacology 2003, 68, 198–203. [Google Scholar] [CrossRef]
- Betiu, A.M.; Noveanu, L.; Hâncu, I.M.; Lascu, A.; Petrescu, L.; Maack, C.; Elmér, E.; Muntean, D.M. Mitochondrial Effects of Common Cardiovascular Medications: The Good, the Bad and the Mixed. Int. J. Mol. Sci. 2022; 23:13653.
- Igarashi, N.; Fujii, N.; Suzuki, T.; Matsuki, A.; Nakadase, T.; Igawa, A.; Inoue, H. Influence of β-adrenoceptor blockade on the myocardial accumulation of fatty acid tracer and its intracellular metabolism in the heart after ischemia− reperfusion injury. Circ. J. 2006;70, 1509–1514.
- Feldman, D. S.; Carnes, C. A.; Abraham, W. T.; Bristow, M. R. Mechanism s of disease: β-adrenergic receptors — alterations in signal transduction and pharmacogenomics in heart failure. Nat. Clin. Pract. Cardiovasc. Med. 2005; 2, 475–483.
- Kourek, C.; Briasoulis, A.; Papamichail, A.; Xanthopoulos, A.; Tsougos, E.; Farmakis, D.; Paraskevaidis, I. Beyond Quadruple Therapy and Current Therapeutic Strategies in Heart Failure with Reduced Ejection Fraction: Medical Therapies with Potential to Become Part of the Therapeutic Armamentarium. Int. J. Mol. Sci. 2024, 25, 3113. [Google Scholar] [CrossRef]
- Voorrips, S.N.; Saucedo-Orozco, H.; Sánchez-Aguilera, P.I.; De Boer, R.A.; Van der Meer, P.; Westenbrink, B.D. Could SGLT2 Inhibitors Improve Exercise Intolerance in Chronic Heart Failure? Int. J. Mol. Sci. 2022; 23: 8631.
- Choi, J; Matoba, N.; Setoyama, D.; Watanabe, D.; Ohnishi, Y.; Yasui, R.; Kitai, Y.; Oomachi, A.; Kotobuki, Y.; Nishiya, Y.; et al. The SGLT2 inhibitor empagliflozin improves cardiac energy status via mitochondrial ATP production in diabetic mice. Commun. Biol 2023; 17;6(1):278.
- Cai, W.; Chong, K.; Huang, Y; Huang, C.; Yin, L. Empagliflozin improves mitochondrial dysfunction in diabetic cardiomyopathy by modulating ketone body metabolism and oxidative stress. Redox Biology 2024;69: 103010.
- Martens, P.; Mathieu, C.; Verbrugge, F.H. Promise of SGLT2 Inhibitors in Heart Failure: Diabetes and Beyond. Curr. Treat. Options Cardiovasc. Med. 2017; 19: 23.
- Miliotis, S.; Nicolalde, B.; Ortega, M.; Yepez, J.; Caicedo, A. Forms of extracellular mitochondria and their impact in health. Mitochondrion 2019, 48, 16–30. [Google Scholar] [CrossRef]
- Stier, A. Human blood contains circulating cell-free mitochondria, but are they really functional? Am. J. Physiol. Metab. 2021, 320, E859–E863. [Google Scholar] [CrossRef]
- Lindqvist, D.; Wolkowitz, O.M.; Picard, M.; Ohlsson, L.; Bersani, F.S.; Fernström, J.; Westrin, Å.; Hough, C.M.; Lin, J.; Reus, V.I.; et al. Circulating cell-free mitochondrial DNA, but not leukocyte mitochondrial DNA copy number, is elevated in major depressive disorder. Neuropsychopharmacology 2018, 43, 1557–1564. [Google Scholar] [CrossRef]
- McClintock, CR.; Mulholland, N.; Krasnodembskaya, AD. Biomarkers of mitochondrial dysfunction in acute respiratory distress syndrome: a systematic review and meta-analysis. Front Med (Lausanne) 2022;9:1.
- Rahat, B.; Ali, T.; Sapehia, D.; Mahajan, A.; Kaur, J. Circulating cell-free nucleic acids as epigenetic biomarkers in precision medicine. Front Genet 2020;11:844.
- Shayota, BJ. Biomarkers of mitochondrial disorders Neurotherapeutics 2024; 21: e00325.
- Knaapen, P.; Germans, T.; Knuuti, J.; Paulus, WJ.; Dijkmans, PA.; Allaart, CP.; Lammertsma, AA.; Visser, FC. Myocardial Energetics and Efficiency Current Status of the Noninvasive Approach. Circulation. 2007;115:918-927.
- Gabr, R. ;, El-Sharkawy, AMM.; Schär, M.; Panjrath, GS.; Gerstenblith, G.; Weiss, RG.; Bottomley PA. Cardiac work is related to creatine kinase energy supply in human heart failure: a cardiovascular magnetic resonance spectroscopy study. J Cardiovascular Magnetic Resonance 2018; 10;20(1):81.
- Cheng, ML.; Wang, CH.; Shiao, MS.; Liu, MH.; Huang, YY.; Huang, CY.; Mao, CT.; Lin, JF.; Ho, HY.; Yang, NI. Metabolic Disturbances Identified in Plasma Are Associated With Outcomes in Patients With Heart Failure. Diagnostic and Prognostic Value of Metabolomics. J Am Coll Cardiol 2015;65:1509–2084.
- Weiss, RG,; Gerstenblith, G.; Bottomley PA. ATP flux through creatine kinase in the normal, stressed, and failing human heart. Proc Natl Acad Sci U S A. 2005;102:808–13.
- Tsampasian, V.; Cameron, D.; Sobhan, R.; Bazoukis, G.; Vassiliou, V.S. Phosphorus Magnetic Resonance Spectroscopy (31P MRS) and Cardiovascular Disease: The Importance of Energy. Medicina 2023, 59, 174. [Google Scholar] [CrossRef] [PubMed]
- Bottomley, PA.; Wu, KC.; Gerstenblith.; G, Schulman, SP.; Steinberg, A.; Weiss RG. Reduced myocardial creatine kinase flux in human myocardial infarction: an in vivo phosphorus magnetic resonance spectroscopy study. Circulation. 2009;119:1918–24.
- Lamb, HJ.; Beyerbacht, HP.; van der Laarse, A.; Stoel, BC.; Doornbos, J.; van der Wall, EE.; de Roos, A. Diastolic dysfunction in hypertensive heart disease is associated with altered myocardial metabolism. Circulation 1999;99:2261–7.
- Samuel, TJ.; Lai, S.; Schär, M.; Wu, KC.; Steinberg, AM. ; Wei, A-C.; Anderson ME.; Tomaselli, GF.; Gerstenblith, G.; et al. Myocardial ATP depletion detected noninvasively predicts sudden cardiac death risk in patients with heart failure. JCI Insight 2022;7:e157557.
- Burrage, M.K.; Hundertmark, M.; Valkovic, L.; Watson, W.D.; Rayner, J.; Sabharwal, N.; Ferreira, V.M.; Neubauer, S.; Miller, J.J.; Rider, O.J.; et al. Energetic Basis for Exercise-Induced Pulmonary Congestion in Heart Failure With Preserved Ejection Fraction. Circulation 2021; 144: 1664–1678.
- Rame, JE. Chronic heart failure: a reversible metabolic syndrome? Circulation 2012;125:2809–11.
- Maekawa, K.; Hirayama, A.; Iwata, Y.; Tajima, Y.; Nishimaki-Mogami, Y.; Sugawara, S.; Ueno, N.; Abe, H.; Ishikawa, M.; Murayama, M.; et al. Global metabolomic analysis of heart tissue in a hamster model for dilated cardiomyopathy. J Mol Cell Cardiol 2013;59:76–85.
- Bakermans, AJ.; Bazil, JN.; Nederveen, AJ.; Strijkers, G.; Boekholdt, SM.; Beard, DA.; Jeneson, JAL. Human cardiac 31P-MR spectroscopy at 3 Tesla cannot detect failing myocardial energy homeostasis during exercise. Front Physiol 2017;8:93.
- Powers SK, Smuder AJ, Kavazis AN, Quindry JC. Mechanisms of exercise-induced cardioprotection. Physiology (Bethesda) 2014;29:27–38.
- Kavazis, AN. Exercise preconditioning of the myocardium. Sports Med 2009;39:923–935.
- Ding, H.; Jiang, N.; Liu, H.; Liu, X.; Liu, D.; Zhao, F.; Wen, L.; Liu, S.; Ji, LL.; Zhang, Y. Response of mitochondrial fusion and fssion protein gene expression to exercise in rat skeletal muscle. Biochim Biophys Acta 2100; 1800:250–256.
- Fulghum, K.; Hill, BG. Metabolic mechanisms of exercise induced cardiac remodeling. Front Cardiovasc Med 2018;5:127.
- Huertas, JR.; Casuso, RA.; Agustin, PH.; Cogliati, S. Stay fit, stay young: mitochondria in movement: the role of exercise in the new mitochondrial paradigm. Oxid Med Cell Longev 2019:7058350.
- Lee, Y.; Min, K.; Talbert, E.E.; Kavazis, A.N.; Smuder, A.J.; Willis, W.T.; Powers, S.K. Exercise protects cardiac mitochondria against ischemia-reperfusion injury. Med Sci Sports Exerc 2012;44:397-405.
- Niemann, B.; Chen, Y.; Issa, H.; Silber, RE.; Rohrbach, S. Caloric restriction delays cardiac ageing in rats: role of mitochondria. Cardiovasc Res 2010;88:267–276.
- Niemann, B.; Li, L.; Simm, A.; Molenda, N.; Kockskamper, J.; Boening, A.; Rohrbach, S. Caloric restriction reduces sympathetic activity similar to beta-blockers but conveys additional mitochondrio-protective efects in aged myocardium. Sci Rep 2021;11:1931].
- Wu, C.; Zhang, Z.; Zhang, W.; Liu, X. Mitochondrial dysfunction and mitochondrial therapies in heart failure. Pharmacol. Res. 2022; 175, 106038.
- Gallo, G.; Rubattu, S.; Volpe, M. Mitochondrial Dysfunction in Heart Failure: From Pathophysiological Mechanisms to Therapeutic Opportunities. Int. J. Mol. Sci. 2024; 25, 2667.
- Ogata, T.; Miyauchi, T.; Sakai, S.; Takanashi, M.; Irukayama-Tomobe, Y.; Yamaguchi, I. Myocardial fibrosis and diastolic dysfunction in deoxycorticosterone acetate-salt hypertensive rats is ameliorated by the peroxisome proliferator-activated receptoralpha activator fenofibrate, partly by suppressing inflammatory responses associated with the nuclear factor-kappa-B pathway. J. Am. Coll. Cardiol. 2004, 43, 1481–1488. [Google Scholar] [PubMed]
- Zhao, G.; Zhang, H.; Wang, Y.; Gao, X.; Liu, H.; Liu, W. Effects of levocarnitine on cardiac function, urinary albumin, hs-CRP, BNP, and troponin in patients with coronary heart disease and heart failure. Hellenic J. Cardiol. 2020, 61, 99–102. [Google Scholar] [CrossRef]
- Lopaschuk, G.D.; Verma, S. Mechanisms of Cardiovascular Benefits of Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitors: A State-of-the-Art Review. JACC Basic. Transl. Sci. 2020, 5, 632–644. [Google Scholar] [CrossRef]
- Kumar, A.A.; Kelly, D.P.; Chirinos, J.A. Mitochondrial Dysfunction in Heart Failure With Preserved Ejection Fraction. Circulation 2019; 139, 1435–1450.
- Raffa, S.; Forte, M.; Gallo, G.; Ranieri, D.; Marchitti, S.; Magrì, D.; Testa, M.; Stanzione, R.; Bianchi, F.; Cotugno, M.; et al. Atrial natriuretic peptide stimulates autophagy/mitophagy and improves mitochondrial function in chronic heart failure. Cell Mol. Life Sci. 2023, 80, 134]. [Google Scholar] [CrossRef]
- Fotino, A.D.; Thompson-Paul, A.M.; Bazzano, L.A. Effect of coenzyme Q10 supplementation on heart failure: A meta-analysis. Am. J. Clin. Nutr. 2013; 97, 268–275.
- Madmani, M.E.; Yusuf Solaiman, A.; Tamr Agha, K.; Madmani, Y.; Shahrour, Y.; Essali, A.; Kadro, W. Coenzyme Q10 for heart failure. Cochrane Database Syst. Rev. 2014; 6, CD008684.
- Hodges, W.T.; Jarasvaraparn, C.; Ferguson, D.; Griffett, K.; Gill, L.E.; Chen, Y.; Ilagan, M.X.G.; Hegazy, L.; Elgendy, B.; Cho, K.; et al. Mitochondrial pyruvate carrier inhibitors improve metabolic parameters in diet-induced obese mice. J. Biol. Chem. 2022, 298, 101554. [Google Scholar] [CrossRef]
- Dai, W.; Shi, J.; Gupta, R.C.; Sabbah, H.N.; Hale, S.L.; Kloner, R.A. Bendavia, a mitochondria-targeting peptide, improves postinfarction cardiac function, prevents adverse left ventricular remodeling, and restores mitochondria-related gene expression in rats. J. Cardiovasc. Pharmacol. 2014, 64, 543–553. [Google Scholar] [CrossRef]
- Koene, S.; Spaans, E.; Van Bortel, L.; Van Lancker, G.; Delafontaine, B.; Badilini, F.; Beyrath, J.; Smeitink, J. KH176 under development for rare mitochondrial disease: A first in man randomized controlled clinical trial in healthy male volunteers. Orphanet J. Rare Dis. 2017, 12, 163. [Google Scholar] [CrossRef]
- Detaille, D.; Pasdois, P.; Sémont, A.; Dos Santos, P.; Diolez, P. An old medicine as a new drug to prevent mitochondrial complex I from producing oxygen radicals. PLoS ONE 2019, 14, e0216385. [Google Scholar] [CrossRef]
- Ordog, K.; Horvath, O.; Eros, K.; Bruszt, K.; Toth, S.; Kovacs, D.; Kalman, N.; Radnai, B.; Deres, L.; Gallyas, F., Jr.; et al. Mitochondrial protective effects of PARP-inhibition in hypertension-induced myocardial remodeling and in stressed cardiomyocytes. Life Sci. 2021, 268, 118936. [Google Scholar] [CrossRef]
- Abudureyimu, M.; Yu, W.; Cao, R.Y.; Zhang, Y.; Liu, H.; Zheng, H. Berberine Promotes Cardiac Function by Upregulating PINK1/Parkin-Mediated Mitophagy in Heart Failure. Front. Physiol. 2020, 11, 565751. [Google Scholar] [CrossRef]
- Hallakou-Bozec, S.; Vial, G.; Kergoat, M.; Fouqueray, P.; Bolze, S.; Borel, A.L.; Fontaine, E.; Moller, D.E. Mechanism of action of Imeglimin: A novel therapeutic agent for type 2 diabetes. Diabetes Obes. Metab. 2021, 23, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.; Kitsis, RN.; Fleischer, JA.; Gavathiotis, E.; Kornfeld, OS.; Gong, G.; Biris, N.; Benz, A.; Qvit, N.; Donnelly, SK.; et al. Correcting mitochondrial fusion by manipulating mitofusin conformations. Nature 2016;540:74–79,.
- Hernandez-Resendiz, S.; Prunier, F.; Girao, H.; Dorn, G.; Hausenloy, DJ.; Action E-CC. Targeting mitochondrial fusion and fssion proteins for cardioprotection. J Cell Mol Med 2020;24:6571– 6585.
- Maneechote, C.; Palee, S.; Kerdphoo, S.; Jaiwongkam, T.; Chattipakorn, SC.; Chattipakorn, N. Pharmacological inhibition of mitochondrial fssion attenuates cardiac ischemia-reperfusion injury in pre-diabetic rats. Biochem Pharmacol 202;182:114295.
- Ong, SB.; Kalkhoran, SB.; Cabrera-Fuentes, HA.; Hausenloy, DJ. Mitochondrial fusion and fission proteins as novel therapeutic targets for treating cardiovascular disease. Eur J Pharmacol 2015;763:104–114.
- Ong, SB.; Kalkhoran, SB.; Hernandez-Resendiz, S.; Samangouei, P.; Ong, SG.; Hausenloy, DJ. Mitochondrial-shaping proteins in cardiac health and disease—the long and the short of it! Cardiovasc Drugs Ther 2017;31:87–107.
- Rocha, AG.; Franco, A.; Krezel, AM.; Rumsey, JM.; Alberti, JM.; Knight, WC.; Biris, N.; Zacharioudakis, E.; Janetka, JW.; Baloh, RH.; et al. MFN2 agonists reverse mitochondrial defects in preclinical models of Charcot-Marie-Tooth disease type 2A. Science 2018;360:336–341.
- Cao, YL.; Meng, S.; Chen. Y.; Feng, JX.; Gu, DD.; Yu, B.; Li, YJ.; Yang, JY.; Liao, S.; Chan, DC.; Gao, S. MFN1 structures reveal nucleotide-triggered dimerization critical for mitochondrial fusion. Nature 2017;542:372–376.
- Giacomello, M. ; Scorrano L The INs and OUTs of mitofusins. J Cell Biol 2018;217:439–440.
- Maneechote, C.; Palee, S.; Kerdphoo, S.; Jaiwongkam, T.; Chattipakorn, SC.; Chattipakorn, N. Diferential temporal inhibition of mitochondrial fssion by Mdivi-1 exerts efective cardioprotection in cardiac ischemia/reperfusion injury. Clin Sci (Lond) 2018;132:1669–1683.
- Bordt, EA.; Clerc, P,.;Roelofs, BA.; Saladino, AJ.; Tretter, L.; AdamVizi, V.; Cherok, E,.;Khalil, A.; Yadava, N.; Ge, SX.; et al. The putative Drp1 inhibitor mdivi-1 Is a reversible mitochondrial complex I inhibitor that modulates reactive oxygen species. Dev Cell 2017; 40(583–594):e586.
- Bordt, EA.; Zhang, N.; Waddell, J.; Polster, BM. The non-specifc Drp1 inhibitor Mdivi-1 has modest biochemical antioxidant activity. Antioxidants (Basel) 2022;24,11:450.
- Zhang, H.; Wang, P.; Bisetto, S.; Yoon, Y.; Chen, Q.; Sheu, SS.; Wang, W. A novel fssion-independent role of dynamin-related protein 1 in cardiac mitochondrial respiration. Cardiovasc Res 2017;113:160–170.
- Dalmasso, G.; Zapata, PAM.; Brady, NR.;Hamacher-Brady, A. Agent-based modeling of mitochondria links sub-cellular dynamics to cellular homeostasis and heterogeneity. PLoS One 2017;12, e0168198.
- Glancy, B.; Kim, Y.; Katti, P.; Willingham, TB. The Functional Impact of Mitochondrial Structure Across Subcellular Scales. Front. Physiol. 2020;11:541040.
- Srinivasan, S.; Guha, M.; Kashina, A.; Avadhani, NG. Mitochondrial dysfunction and mitochondrial dynamics - the cancer connection. Biochim. Biophys. Acta 2017;1858, 602–614.
- Kleele, T.; Rey, T.; Winter, J. ; Zaganelli, S,.;Mahecic, D.; Perreten Lambert, H.; Ruberto, FP.; Nemir, M,.;Wai, T.; Pedrazzini, T.; et al. Distinct fission signatures predict mitochondrial degradation or biogenesis. Nature 2021;593, 435–439.
- Ding, Y.; Liu, N.; Zhang, D.; Guo, L.; Shang, Q.; Liu, Y.; Ren, G.; Ma, X. Mitochondria-associated endoplasmic reticulum membranes as a therapeutic target for cardiovascular diseases. Front. Pharmacol. 2024;15:1398381.
- Neikirk, K.; Lopez, EG.; Marshall, AG.; Alghanem, A.; Krystofiak, E.; Kula, B.; Smith, N.; Shao, J.; Katti, P.; Hinton, A., Jr. Call to action to properly utilize electron microscopy to measure organelles to monitor disease. Eur. J. Cell Biol 12023;02, 151365.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




