Submitted:
13 October 2024
Posted:
14 October 2024
You are already at the latest version
Abstract
Keywords:
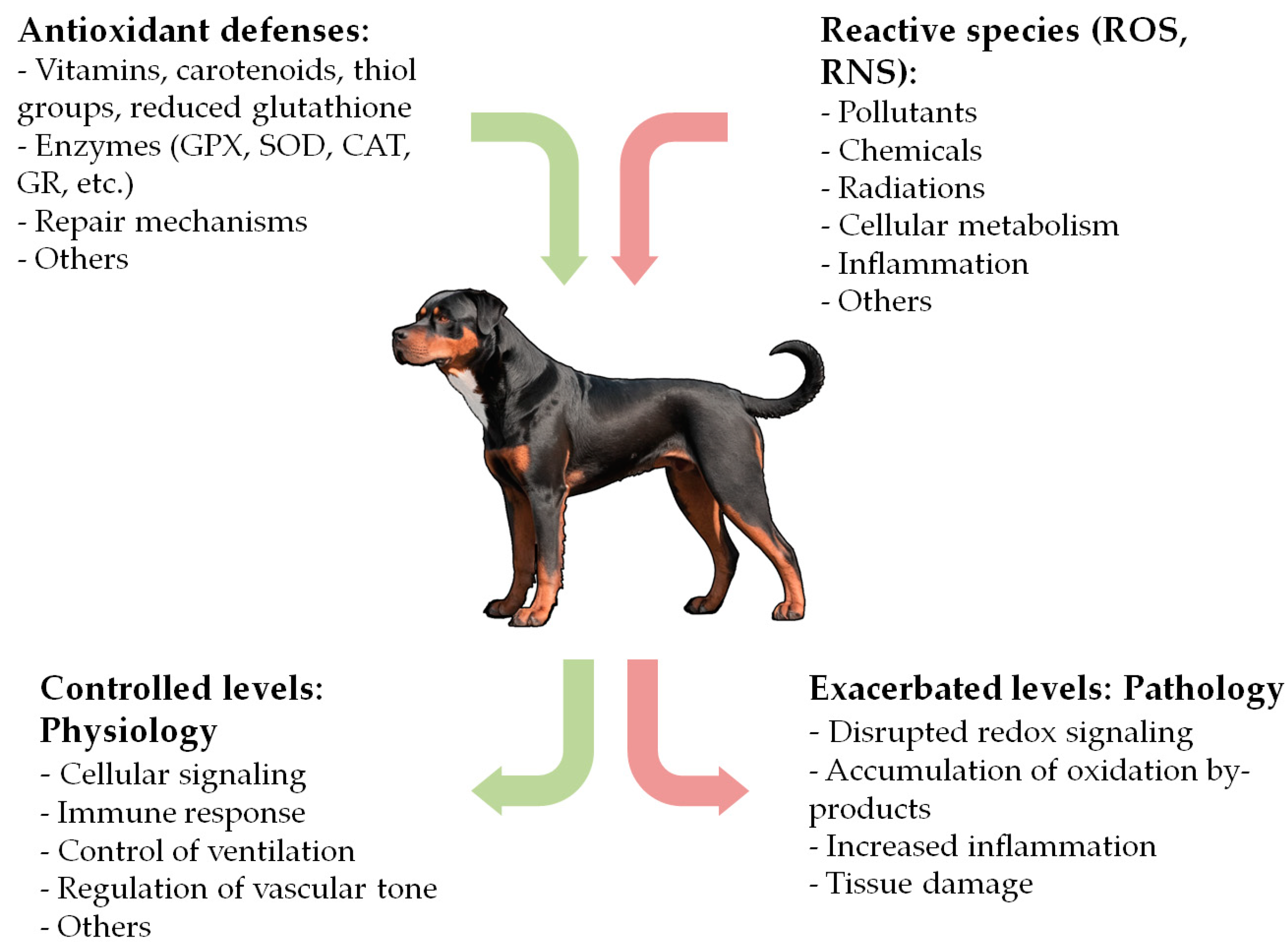
1. Introduction
2. OS in Canine Diseases
2.1. Cardiovascular, Respiratory and Related Diseases
2.2. Oncologic Diseases
2.3. Gastrointestinal and Exocrine Pancreatic Diseases
2.4. Hepatobiliary Diseases
2.5. Endocrine Diseases and Obesity
2.6. Hematologic Diseases
2.7. Infectious and Parasitic Diseases
2.7.1. Vector-Borne Diseases
- - Leishmaniosis
- - Ehrlichiosis
- - Babesiosis
- - Other vector-borne diseases
2.7.2. Infectious and Parasitic Gastrointestinal Diseases
2.7.3. Ectoparasites and Dermal Fungal Diseases
2.8. Neurologic Diseases
2.9. Renal Diseases
2.10. Dermatologic Diseases
2.11. Ophthalmologic Diseases
2.12. Orthopaedic Diseases
2.13. Reproductive System Diseases
2.14. Dental Diseases
2.15. Others
3. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sies, H.; Berndt, C.; Jones, D.P. Oxidative Stress. Annu Rev Biochem 2017, 86, 715–748. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. Oxidative Stress: Introductory Remarks. In Oxidative Stress; Sies, H., Ed.; Academic Press: London, 1985; pp. 1–8. ISBN 978-0-12-642760-8. [Google Scholar]
- Forman, H.J.; Zhang, H. Targeting Oxidative Stress in Disease: Promise and Limitations of Antioxidant Therapy. Nat Rev Drug Discov 2021, 20, 689–709. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. On the History of Oxidative Stress: Concept and Some Aspects of Current Development. Curr Opin Toxicol 2018, 7, 122–126. [Google Scholar] [CrossRef]
- Sies, H. Oxidative Stress: Concept and Some Practical Aspects. Antioxidants (Basel) 2020, 9, 852. [Google Scholar] [CrossRef]
- Halliwell, B. Reactive Species and Antioxidants. Redox Biology Is a Fundamental Theme of Aerobic Life. Plant Physiol 2006, 141, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Birben, E.; Sahiner, U.M.; Sackesen, C.; Erzurum, S.; Kalayci, O. Oxidative Stress and Antioxidant Defense. World Allergy Organ J 2012, 5, 9–19. [Google Scholar] [CrossRef]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxid Med Cell Longev 2017, 2017, 8416763. [Google Scholar] [CrossRef]
- Dröge, W. Free Radicals in the Physiological Control of Cell Function. Physiol Rev 2002, 82, 47–95. [Google Scholar] [CrossRef]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.D.; Mazur, M.; Telser, J. Free Radicals and Antioxidants in Normal Physiological Functions and Human Disease. Int J Biochem Cell Biol 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Dalle-Donne, I.; Rossi, R.; Colombo, R.; Giustarini, D.; Milzani, A. Biomarkers of Oxidative Damage in Human Disease. Clin Chem 2006, 52, 601–623. [Google Scholar] [CrossRef]
- Halliwell, B.; Whiteman, M. Measuring Reactive Species and Oxidative Damage in Vivo and in Cell Culture: How Should You Do It and What Do the Results Mean? Br J Pharmacol 2004, 142, 231–255. [Google Scholar] [CrossRef] [PubMed]
- Tejchman, K.; Kotfis, K.; Sieńko, J. Biomarkers and Mechanisms of Oxidative Stress—Last 20 Years of Research with an Emphasis on Kidney Damage and Renal Transplantation. Int J Mol Sci 2021, 22, 8010. [Google Scholar] [CrossRef] [PubMed]
- Tsikas, D. Assessment of Lipid Peroxidation by Measuring Malondialdehyde (MDA) and Relatives in Biological Samples: Analytical and Biological Challenges. Anal Biochem 2017, 524, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Chao, M.-R.; Evans, M.D.; Hu, C.-W.; Ji, Y.; Møller, P.; Rossner, P.; Cooke, M.S. Biomarkers of Nucleic Acid Oxidation – A Summary State-of-the-Art. Redox Biol 2021, 42, 101872. [Google Scholar] [CrossRef] [PubMed]
- Jelic, M.D.; Mandic, A.D.; Maricic, S.M.; Srdjenovic, B.U. Oxidative Stress and Its Role in Cancer. J Cancer Res Ther 2021, 17, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Rodríguez, M.A.; Mendoza-Núñez, V.M. Oxidative Stress Indexes for Diagnosis of Health or Disease in Humans. Oxid Med Cell Longev 2019, 2019, 4128152. [Google Scholar] [CrossRef]
- Frijhoff, J.; Winyard, P.G.; Zarkovic, N.; Davies, S.S.; Stocker, R.; Cheng, D.; Knight, A.R.; Taylor, E.L.; Oettrich, J.; Ruskovska, T.; et al. Clinical Relevance of Biomarkers of Oxidative Stress. Antioxid Redox Signal 2015, 23, 1144–1170. [Google Scholar] [CrossRef]
- Munteanu, I.G.; Apetrei, C. Analytical Methods Used in Determining Antioxidant Activity: A Review. Int J Mol Sci 2021, 22, 3380. [Google Scholar] [CrossRef]
- Pellegrini, N.; Vitaglione, P.; Granato, D.; Fogliano, V. Twenty-Five Years of Total Antioxidant Capacity Measurement of Foods and Biological Fluids: Merits and Limitations. J Sci Food Agric 2020, 100, 5064–5078. [Google Scholar] [CrossRef]
- Colitti, M.; Stefanon, B.; Gabai, G.; Gelain, M.E.; Bonsembiante, F. Oxidative Stress and Nutraceuticals in the Modulation of the Immune Function: Current Knowledge in Animals of Veterinary Interest. Antioxidants (Basel) 2019, 8, E28. [Google Scholar] [CrossRef]
- Dubois-Deruy, E.; Peugnet, V.; Turkieh, A.; Pinet, F. Oxidative Stress in Cardiovascular Diseases. Antioxidants (Basel) 2020, 9, 864. [Google Scholar] [CrossRef] [PubMed]
- Zorov, D.B.; Juhaszova, M.; Sollott, S.J. Mitochondrial Reactive Oxygen Species (ROS) and ROS-Induced ROS Release. Physiol Rev 2014, 94, 909–950. [Google Scholar] [CrossRef] [PubMed]
- D’Oria, R.; Schipani, R.; Leonardini, A.; Natalicchio, A.; Perrini, S.; Cignarelli, A.; Laviola, L.; Giorgino, F. The Role of Oxidative Stress in Cardiac Disease: From Physiological Response to Injury Factor. Oxid Med Cell Longev 2020, 2020, 5732956. [Google Scholar] [CrossRef] [PubMed]
- Chirathanaphirom, S.; Chuammitri, P.; Pongkan, W.; Manachai, N.; Chantawong, P.; Boonsri, B.; Boonyapakorn, C. Differences in Levels of Mitochondrial DNA Content at Various Stages of Canine Myxomatous Mitral Valve Disease. Animals (Basel) 2023, 13, 3850. [Google Scholar] [CrossRef]
- Freeman, L.M.; Brown, D.J.; Rush, J.E. Antioxidant Status in Dogs with Idiopathic Dilated Cardiomyopathy. J Nutr 1998, 128, 2768S–2770S. [Google Scholar] [CrossRef]
- Freeman, L.M.; Brown, D.J.; Rush, J.E. Assessment of Degree of Oxidative Stress and Antioxidant Concentrations in Dogs with Idiopathic Dilated Cardiomyopathy. J Am Vet Med Assoc 1999, 215, 644–646. [Google Scholar] [CrossRef]
- Freeman, L.M.; Rush, J.E.; Milbury, P.E.; Blumberg, J.B. Antioxidant Status and Biomarkers of Oxidative Stress in Dogs with Congestive Heart Failure. J Vet Intern Med 2005, 19, 537–541. [Google Scholar] [CrossRef]
- Michałek, M.; Tabiś, A.; Cepiel, A.; Noszczyk-Nowak, A. Antioxidative Enzyme Activity and Total Antioxidant Capacity in Serum of Dogs with Degenerative Mitral Valve Disease. Can J Vet Res 2020, 84, 67–73. [Google Scholar]
- Michałek, M.; Tabiś, A.; Noszczyk-Nowak, A. Serum Total Antioxidant Capacity and Enzymatic Defence of Dogs with Chronic Heart Failure and Atrial Fibrillation: A Preliminary Study. J Vet Res 2020, 64, 439–444. [Google Scholar] [CrossRef]
- Nemec Svete, A.; Verk, B.; Čebulj-Kadunc, N.; Salobir, J.; Rezar, V.; Domanjko Petrič, A. Inflammation and Its Association with Oxidative Stress in Dogs with Heart Failure. BMC Vet Res 2021, 17, 176. [Google Scholar] [CrossRef]
- Reimann, M.J.; Häggström, J.; Møller, J.E.; Lykkesfeldt, J.; Falk, T.; Olsen, L.H. Markers of Oxidative Stress in Dogs with Myxomatous Mitral Valve Disease Are Influenced by Sex, Neuter Status, and Serum Cholesterol Concentration. J Vet Intern Med 2017, 31, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Saril, A.; Kocaturk, M.; Tanaka, R.; Koch, J.; Ceron, J.J.; Yilmaz, Z. Changes of Inflammatory and Oxidative Stress Biomarkers in Dogs with Different Stages of Heart Failure. BMC Vet Res 2020, 16, 433. [Google Scholar] [CrossRef] [PubMed]
- Tomsič, K.; Domanjko Petrič, A.; Nemec, A.; Pirman, T.; Rezar, V.; Seliškar, A.; Vovk, T.; Nemec Svete, A. Evaluation of Antioxidant Status and Lipid Peroxidation in Dogs with Myxomatous Mitral Valve Degeneration Stage B1. Front Vet Sci 2023, 10, 1203480. [Google Scholar] [CrossRef] [PubMed]
- Verk, B.; Nemec Svete, A.; Salobir, J.; Rezar, V.; Domanjko Petrič, A. Markers of Oxidative Stress in Dogs with Heart Failure. J Vet Diagn Invest 2017, 29, 636–644. [Google Scholar] [CrossRef]
- Laflamme, D.P. Key Nutrients Important in the Management of Canine Myxomatous Mitral Valve Disease and Heart Failure. J Am Vet Med Assoc 2022, 260, S61–S70. [Google Scholar] [CrossRef]
- Pongkan, W.; Piamsiri, C.; Dechvongya, S.; Punyapornwitthaya, V.; Boonyapakorn, C. Short-Term Melatonin Supplementation Decreases Oxidative Stress but Does Not Affect Left Ventricular Structure and Function in Myxomatous Mitral Valve Degenerative Dogs. BMC Vet Res 2022, 18, 24. [Google Scholar] [CrossRef]
- Thassakorn, P.; Patchanee, P.; Pongkan, W.; Chattipakorn, N.; Boonyapakorn, C. Effect of Atorvastatin on Oxidative Stress and Inflammation Markers in Myxomatous Mitral Valve Disease in Dogs: A Comparison of Subclinical and Clinical Stages. J Vet Pharmacol Ther 2019, 42, 258–267. [Google Scholar] [CrossRef]
- Druzhaeva, N.; Nemec Svete, A.; Tavčar-Kalcher, G.; Babič, J.; Ihan, A.; Pohar, K.; Krapež, U.; Domanjko Petrič, A. Effects of Coenzyme Q10 Supplementation on Oxidative Stress Markers, Inflammatory Markers, Lymphocyte Subpopulations, and Clinical Status in Dogs with Myxomatous Mitral Valve Disease. Antioxidants (Basel) 2022, 11, 1427. [Google Scholar] [CrossRef]
- Igarashi, T.; Niwano, S.; Niwano, H.; Yoshizawa, T.; Nakamura, H.; Fukaya, H.; Fujiishi, T.; Ishizue, N.; Satoh, A.; Kishihara, J.; et al. Linagliptin Prevents Atrial Electrical and Structural Remodeling in a Canine Model of Atrial Fibrillation. Heart Vessels 2018, 33, 1258–1265. [Google Scholar] [CrossRef]
- Kishihara, J.; Niwano, S.; Niwano, H.; Aoyama, Y.; Satoh, A.; Oikawa, J.; Kiryu, M.; Fukaya, H.; Masaki, Y.; Tamaki, H.; et al. Effect of Carvedilol on Atrial Remodeling in Canine Model of Atrial Fibrillation. Cardiovasc Diagn Ther 2014, 4, 28–35. [Google Scholar] [CrossRef]
- Nishinarita, R.; Niwano, S.; Niwano, H.; Nakamura, H.; Saito, D.; Sato, T.; Matsuura, G.; Arakawa, Y.; Kobayashi, S.; Shirakawa, Y.; et al. Canagliflozin Suppresses Atrial Remodeling in a Canine Atrial Fibrillation Model. J Am Heart Assoc 2021, 10, e017483. [Google Scholar] [CrossRef]
- Yoshizawa, T.; Niwano, S.; Niwano, H.; Tamaki, H.; Nakamura, H.; Igarashi, T.; Oikawa, J.; Satoh, A.; Kishihara, J.; Murakami, M.; et al. Antiremodeling Effect of Xanthine Oxidase Inhibition in a Canine Model of Atrial Fibrillation. Int Heart J 2018, 59, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Li, R.; Wang, X.; Li, J.; Xu, X.; Liu, T.; Liu, E.; Li, G. Suppression of Experimental Atrial Fibrillation in a Canine Model of Rapid Atrial Pacing by the Phosphodiesterase 3 Inhibitor Cilostazol. J Electrocardiol 2020, 60, 151–158. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, R.; Wang, X.; Li, J.; Yuan, M.; Liu, E.; Liu, T.; Li, G. Attenuation of Atrial Remodeling by Aliskiren via Affecting Oxidative Stress, Inflammation and PI3K/Akt Signaling Pathway. Cardiovasc Drugs Ther 2021, 35, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Fischer, U.M.; Cox, C.S.; Allen, S.J.; Stewart, R.H.; Mehlhorn, U.; Laine, G.A. The Antioxidant N-Acetylcysteine Preserves Myocardial Function and Diminishes Oxidative Stress after Cardioplegic Arrest. J Thorac Cardiovasc Surg 2003, 126, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.B.; Sun, J.; Howard, L.L.; Williams, A.G.; Mallet, R.T. Oxidative Stress Reversibly Inactivates Myocardial Enzymes during Cardiac Arrest. Am J Physiol Heart Circ Physiol 2007, 292, H198–206. [Google Scholar] [CrossRef]
- Moe, G.; Konig, A.; Liu, P.; Jugdutt, B.I. Selective Type 1 Angiotensin II Receptor Blockade Attenuates Oxidative Stress and Regulates Angiotensin II Receptors in the Canine Failing Heart. Mol Cell Biochem 2008, 317, 97–104. [Google Scholar] [CrossRef]
- Moe, G.W.; Marin-Garcia, J.; Konig, A.; Goldenthal, M.; Lu, X.; Feng, Q. In Vivo TNF-Alpha Inhibition Ameliorates Cardiac Mitochondrial Dysfunction, Oxidative Stress, and Apoptosis in Experimental Heart Failure. Am J Physiol Heart Circ Physiol 2004, 287, H1813–1820. [Google Scholar] [CrossRef]
- Chueainta, P.; Punyapornwithaya, V.; Tangjitjaroen, W.; Pongkan, W.; Boonyapakorn, C. Acupuncture Improves Heart Rate Variability, Oxidative Stress Level, Exercise Tolerance, and Quality of Life in Tracheal Collapse Dogs. Vet Sci 2022, 9, 88. [Google Scholar] [CrossRef]
- Erjavec, V.; Vovk, T.; Svete, A.N. Evaluation of Oxidative Stress Parameters in Dogs with Brachycephalic Obstructive Airway Syndrome Before and after Surgery. J Vet Res 2021, 65, 201–208. [Google Scholar] [CrossRef]
- Eze, U.U.; Eke, I.G.; Anakwue, R.C.; Oguejiofor, C.F.; Onyejekwe, O.B.; Udeani, I.J.; Onunze, C.J.; Obed, U.J.; Eze, A.A.; Anaga, A.O.; et al. Effects of Controlled Generator Fume Emissions on the Levels of Troponin I, C-Reactive Protein and Oxidative Stress Markers in Dogs: Exploring Air Pollution-Induced Cardiovascular Disease in a Low-Resource Country. Cardiovasc Toxicol 2021, 21, 1019–1032. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Liu, K.; Qi, M.; Geng, H.; Hao, J.; Wang, R.; Zhao, X.; Liu, Y.; Liu, J. Effects of Cr(VI) Exposure on Electrocardiogram, Myocardial Enzyme Parameters, Inflammatory Factors, Oxidative Kinase, and ATPase of the Heart in Chinese Rural Dogs. Environ Sci Pollut Res Int 2019, 26, 30444–30451. [Google Scholar] [CrossRef] [PubMed]
- Mektrirat, R.; Rueangsri, T.; Keeratichandacha, W.; Soonsawat, S.; Boonyapakorn, C.; Pongkan, W. Polyunsaturated Fatty Acid EAB-277® Supplementation Improved Heart Rate Variability and Clinical Signs in Tracheal Collapse Dogs. Front Vet Sci 2022, 9, 880952. [Google Scholar] [CrossRef] [PubMed]
- Khademi, S.; Frye, M.A.; Jeckel, K.M.; Schroeder, T.; Monnet, E.; Irwin, D.C.; Cole, P.A.; Bell, C.; Miller, B.F.; Hamilton, K.L. Hypoxia Mediated Pulmonary Edema: Potential Influence of Oxidative Stress, Sympathetic Activation and Cerebral Blood Flow. BMC Physiol 2015, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Finotello, R.; Pasquini, A.; Meucci, V.; Lippi, I.; Rota, A.; Guidi, G.; Marchetti, V. Redox Status Evaluation in Dogs Affected by Mast Cell Tumour. Vet Comp Oncol 2014, 12, 120–129. [Google Scholar] [CrossRef]
- Jayasri, K.; Padmaja, K.; Saibaba, M. Altered Oxidative Stress and Carbohydrate Metabolism in Canine Mammary Tumors. Vet World 2016, 9, 1489–1492. [Google Scholar] [CrossRef]
- Silva, L.P.; Portela, R.W.; Machado, M.C.; Canuto, G.A.B.; Costa-Neto, J.M.; Carvalho, V. de M.P. de; Sá, H.C. de; Damasceno, K.A.; Souza, V.R.C. de; Coelho, C.S.; et al. Ozone Therapy in the Integrated Treatment of Female Dogs with Mammary Cancer: Oxidative Profile and Quality of Life. Antioxidants (Basel) 2024, 13, 673. [Google Scholar] [CrossRef]
- Karayannopoulou, M.; Fytianou, A.; Assaloumidis, N.; Psalla, D.; Constantinidis, T.C.; Kaldrymidou, E.; Koutinas, A.F. Markers of Lipid Peroxidation and α-Tocopherol Levels in the Blood and Neoplastic Tissue of Dogs with Malignant Mammary Gland Tumors. Vet Clin Pathol 2013, 42, 323–328. [Google Scholar] [CrossRef]
- Klaunig, J.E.; Kamendulis, L.M.; Hocevar, B.A. Oxidative Stress and Oxidative Damage in Carcinogenesis. Toxicol Pathol 2010, 38, 96–109. [Google Scholar] [CrossRef]
- Karakurt, E.; KURU, M.; Dağ, S.; Beytut, E.; ORAL, H.; Nuhoğlu, H.; Yıldız, A. Presence and Importance of Oxidative Stress Parameters in Malignant Mammary Gland Tumors in Dogs. Kafkas Univ Vet Fak Derg 2021. [Google Scholar] [CrossRef]
- Kumaraguruparan, R.; Balachandran, C.; Manohar, B.M.; Nagini, S. Altered Oxidant-Antioxidant Profile in Canine Mammary Tumours. Vet Res Commun 2005, 29, 287–296. [Google Scholar] [CrossRef]
- Machado, V.S.; Crivellenti, L.Z.; Bottari, N.B.; Tonin, A.A.; Pelinson, L.P.; Borin-Crivellenti, S.; Santana, A.E.; Torbitz, V.D.; Moresco, R.N.; Duarte, T.; et al. Oxidative Stress and Inflammatory Response Biomarkers in Dogs with Mammary Carcinoma. Pathol Res Pract 2015, 211, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Macotpet, A.; Suksawat, F.; Sukon, P.; Pimpakdee, K.; Pattarapanwichien, E.; Tangrassameeprasert, R.; Boonsiri, P. Oxidative Stress in Cancer-Bearing Dogs Assessed by Measuring Serum Malondialdehyde. BMC Vet Res 2013, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Schroers, M.; Walter, B.; Fischer, S.; Cremer, J.; Bauer, E.-M.; Zablotzki, Y.; Majzoub-Altweck, M.; Meyer-Lindenberg, A. Studies on the Association of Malondialdehyde as a Biomarker for Oxidative Stress and Degree of Malignancy in Dogs with Mammary Adenocarcinomas. Vet Med Sci 2024, 10, e1496. [Google Scholar] [CrossRef] [PubMed]
- Szczubiał, M.; Kankofer, M.; Łopuszyński, W.; Dabrowski, R.; Lipko, J. Oxidative Stress Parameters in Bitches with Mammary Gland Tumours. J Vet Med A Physiol Pathol Clin Med 2004, 51, 336–340. [Google Scholar] [CrossRef]
- Bottari, N.B.; Munhoz, T.D.; Torbitz, V.D.; Tonin, A.A.; Anai, L.A.; Semolin, L.M.S.; Jark, P.C.; Bollick, Y.S.; Moresco, R.N.; França, R.T.; et al. Oxidative Stress in Dogs with Multicentric Lymphoma: Effect of Chemotherapy on Oxidative and Antioxidant Biomarkers. Redox Rep 2015, 20, 267–274. [Google Scholar] [CrossRef]
- Henklewska, M.; Pawlak, A.; Li, R.-F.; Yi, J.; Zbyryt, I.; Obmińska-Mrukowicz, B. Benzyl Isothiocyanate, a Vegetable-Derived Compound, Induces Apoptosis via ROS Accumulation and DNA Damage in Canine Lymphoma and Leukemia Cells. Int J Mol Sci 2021, 22, 11772. [Google Scholar] [CrossRef]
- Pasquini, A.; Gavazza, A.; Biagi, G.; Lubas, G. Oxidative Stress in Lymphoma: Similarities and Differences between Dog and Human. Comp Clin Pathol 2015, 24, 69–73. [Google Scholar] [CrossRef]
- Vajdovich, P.; Kriska, T.; Mézes, M.; Szabó, P.R.; Balogh, N.; Bánfi, A.; Arany-Tóth, A.; Gaál, T.; Jakus, J. Redox Status of Dogs with Non-Hodgkin Lymphomas. An ESR Study. Cancer Lett 2005, 224, 339–346. [Google Scholar] [CrossRef]
- Winter, J.L.; Barber, L.G.; Freeman, L.; Griessmayr, P.C.; Milbury, P.E.; Blumberg, J.B. Antioxidant Status and Biomarkers of Oxidative Stress in Dogs with Lymphoma. J Vet Intern Med 2009, 23, 311–316. [Google Scholar] [CrossRef]
- Loftus, J.P.; Cavatorta, D.; Bushey, J.J.; Levine, C.B.; Sevier, C.S.; Wakshlag, J.J. The 5-Lipoxygenase Inhibitor Tepoxalin Induces Oxidative Damage and Altered PTEN Status Prior to Apoptosis in Canine Osteosarcoma Cell Lines. Vet Comp Oncol 2016, 14, e17–30. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Park, S.; Bazer, F.W.; Lim, W.; Song, G. Myricetin Treatment Induces Apoptosis in Canine Osteosarcoma Cells by Inducing DNA Fragmentation, Disrupting Redox Homeostasis, and Mediating Loss of Mitochondrial Membrane Potential. J Cell Physiol 2018, 233, 7457–7466. [Google Scholar] [CrossRef] [PubMed]
- Woolcock, A.D.; Cheney, A.; Deshuillers, P.; Knapp, D.; Moore, G.E. Assessment of Urinary 15-F2 -Isoprostanes in Dogs with Urothelial Carcinoma of the Urinary Bladder and Other Lower Urinary Tract Diseases. J Vet Intern Med 2020, 34, 2454–2459. [Google Scholar] [CrossRef] [PubMed]
- Candellone, A.; Girolami, F.; Badino, P.; Jarriyawattanachaikul, W.; Odore, R. Changes in the Oxidative Stress Status of Dogs Affected by Acute Enteropathies. Vet Sci 2022, 9, 276. [Google Scholar] [CrossRef]
- Cristóbal, J.I.; Duque, F.J.; Usón-Casaús, J.; Martínez, M.S.; Míguez, M.P.; Pérez-Merino, E.M. Oxidative Stress in Dogs with Chronic Inflammatory Enteropathy Treated with Allogeneic Mesenchymal Stem Cells. Vet Res Commun 2023. [Google Scholar] [CrossRef]
- Minamoto, Y.; Otoni, C.C.; Steelman, S.M.; Büyükleblebici, O.; Steiner, J.M.; Jergens, A.E.; Suchodolski, J.S. Alteration of the Fecal Microbiota and Serum Metabolite Profiles in Dogs with Idiopathic Inflammatory Bowel Disease. Gut Microbes 2015, 6, 33–47. [Google Scholar] [CrossRef]
- Rubio, C.P.; Martínez-Subiela, S.; Hernández-Ruiz, J.; Tvarijonaviciute, A.; Cerón, J.J.; Allenspach, K. Serum Biomarkers of Oxidative Stress in Dogs with Idiopathic Inflammatory Bowel Disease. Vet J 2017, 221, 56–61. [Google Scholar] [CrossRef]
- Rubio, C.P.; Hernández-Ruiz, J.; Martinez-Subiela, S.; Tvarijonaviciute, A.; Arnao, M.B.; Ceron, J.J. Validation of Three Automated Assays for Total Antioxidant Capacity Determination in Canine Serum Samples. J Vet Diagn Invest 2016, 28, 693–698. [Google Scholar] [CrossRef]
- Rubio, C.P.; Tvarijonaviciute, A.; Martinez-Subiela, S.; Hernández-Ruiz, J.; Cerón, J.J. Validation of an Automated Assay for the Measurement of Cupric Reducing Antioxidant Capacity in Serum of Dogs. BMC Vet Res 2016, 12, 137. [Google Scholar] [CrossRef]
- Cridge, H.; Lim, S.Y.; Algül, H.; Steiner, J.M. New Insights into the Etiology, Risk Factors, and Pathogenesis of Pancreatitis in Dogs: Potential Impacts on Clinical Practice. J Vet Intern Med 2022, 36, 847–864. [Google Scholar] [CrossRef]
- Tusa, N.V.; Abuelo, A.; Levy, N.A.; Gandy, J.C.; Langlois, D.K.; Cridge, H. Peripheral Biomarkers of Oxidative Stress in Dogs with Acute Pancreatitis. J Vet Intern Med 2022. [Google Scholar] [CrossRef] [PubMed]
- Center, S.A.; Warner, K.L.; Erb, H.N. Liver Glutathione Concentrations in Dogs and Cats with Naturally Occurring Liver Disease. Am J Vet Res 2002, 63, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Webb, C.; Twedt, D. Oxidative Stress and Liver Disease. Vet Clin North Am Small Anim Pract 2008, 38, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Spee, B.; Arends, B.; van den Ingh, T.S.G.A.M.; Penning, L.C.; Rothuizen, J. Copper Metabolism and Oxidative Stress in Chronic Inflammatory and Cholestatic Liver Diseases in Dogs. J Vet Intern Med 2006, 20, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Martello, E.; Perondi, F.; Bisanzio, D.; Lippi, I.; Meineri, G.; Gabriele, V. Antioxidant Effect of a Dietary Supplement Containing Fermentative S-Acetyl-Glutathione and Silybin in Dogs with Liver Disease. Vet Sci 2023, 10, 131. [Google Scholar] [CrossRef]
- Barry-Heffernan, C.; Ekena, J.; Dowling, S.; Pinkerton, M.E.; Viviano, K. Biomarkers of Oxidative Stress as an Assessment of the Redox Status of the Liver in Dogs. J Vet Intern Med 2019, 33, 611–617. [Google Scholar] [CrossRef]
- Dirksen, K.; Spee, B.; Penning, L.C.; van den Ingh, T.S.G.A.M.; Burgener, I.A.; Watson, A.L.; Groot Koerkamp, M.; Rothuizen, J.; van Steenbeek, F.G.; Fieten, H. Gene Expression Patterns in the Progression of Canine Copper-Associated Chronic Hepatitis. PLoS One 2017, 12, e0176826. [Google Scholar] [CrossRef]
- Giannetto, C.; Arfuso, F.; Giudice, E.; Rizzo, M.; Piccione, G.; Mhalhel, K.; Levanti, M. Antioxidant and Hepatoprotective Effect of a Nutritional Supplement with Silymarin Phytosome, Choline Chloride, l-Cystine, Artichoke, and Vitamin E in Dogs. Antioxidants (Basel) 2022, 11, 2339. [Google Scholar] [CrossRef]
- Hishiyama, N.; Kayanuma, H.; Matsui, T.; Yano, H.; Suganuma, T.; Funaba, M.; Fujise, H. Plasma Concentration of Vitamin C in Dogs with a Portosystemic Shunt. Can J Vet Res 2006, 70, 305–307. [Google Scholar]
- Huang, J.; Bai, Y.; Xie, W.; Wang, R.; Qiu, W.; Zhou, S.; Tang, Z.; Liao, J.; Su, R. Lyciumbarbarum Polysaccharides Ameliorate Canine Acute Liver Injury by Reducing Oxidative Stress, Protecting Mitochondrial Function, and Regulating Metabolic Pathways. J Zhejiang Univ Sci B 2023, 24, 157–171. [Google Scholar] [CrossRef]
- Kil, D.Y.; Vester Boler, B.M.; Apanavicius, C.J.; Schook, L.B.; Swanson, K.S. Age and Diet Affect Gene Expression Profiles in Canine Liver Tissue. PLoS One 2010, 5, e13319. [Google Scholar] [CrossRef]
- Phillips, R.K.; Steiner, J.M.; Suchodolski, J.S.; Lidbury, J.A. Urinary 15-F2t-Isoprostane Concentrations in Dogs with Liver Disease. Vet Sci 2023, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Vince, A.R.; Hayes, M.A.; Jefferson, B.J.; Stalker, M.J. Hepatic Injury Correlates with Apoptosis, Regeneration, and Nitric Oxide Synthase Expression in Canine Chronic Liver Disease. Vet Pathol 2014, 51, 932–945. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.M.; Sordillo, L.M.; Smedley, R.C.; Gandy, J.C.; Brown, J.L.; Langlois, D.K. Peripheral Markers of Oxidative Stress in Labrador Retrievers with Copper-Associated Hepatitis. J Small Anim Pract 2021, 62, 866–873. [Google Scholar] [CrossRef] [PubMed]
- Yamkate, P.; Lidbury, J.A.; Steiner, J.M.; Suchodolski, J.S.; Giaretta, P.R. Immunohistochemical Expression of Oxidative Stress and Apoptosis Markers in Archived Liver Specimens from Dogs with Chronic Hepatitis. J Comp Pathol 2022, 193, 25–36. [Google Scholar] [CrossRef]
- Yi, J.; Li, Y.; Mai, Q.; Li, Y.; Lin, Y.; Weng, X.; Ai, Z.; Li, M.; Shang, P.; Iqbal, M.; et al. Hepatotoxicity and the Role of the Gut-Liver Axis in Dogs after Oral Administration of Zinc Oxide Nanoparticles. Metallomics 2022, 14, mfac066. [Google Scholar] [CrossRef]
- Arostegui, L.G.G.; Prieto, A.M.; Marín, L.P.; López, G.G.; Tvarijonaviciute, A.; Madrigal, J.J.C.; Rubio, C.P. Changes in Biomarkers of Redox Status in Serum and Saliva of Dogs with Hypothyroidism. BMC Vet Res 2023, 19, 33. [Google Scholar] [CrossRef]
- González-Arostegui, L.G.; Muñoz-Prieto, A.; García-López, G.; Cerón, J.J.; Tvarijonaviciute, A.; Rubio, C.P. Changes in Biomarkers of the Redox Status in Whole Blood and Red Blood Cell Lysates in Canine Hypothyroidism. Vet Res Commun 2024. [Google Scholar] [CrossRef]
- Ryad, N.M.; Ramadan, E.S.; Salem, N.Y.; Saleh, I.A.E.-S. Oxidative Biomarkers and Lipid Alterations in Euthyroid and Hypothyroid Dogs. Comp Clin Pathol 2021, 30, 571–576. [Google Scholar] [CrossRef]
- Kim, H.; Yonezawa, T.; Maeda, S.; Tamahara, S.; Matsuki, N. Increases in Serum Carbonylated Protein Levels of Dogs with Hypercortisolism. Endocr J 2022, 69, 1387–1394. [Google Scholar] [CrossRef]
- Soares, F. a. C.; Filho, N.A.K.; Beretta, B.F.S.; Linden, T.S.; Pöppl, A.G.; González, F.H.D. Thiobarbituric Acid Reactive Substances in Dogs with Spontaneous Hypercortisolism. Domest Anim Endocrinol 2021, 77, 106634. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Suzuki, S.; Soeta, S.; Kaneda, T.; Hara, A.Y. Mechanism of Long-Term High-Dose Prednisolone Administration Producing Myocardial Fibrosis in Beagle Dogs. Open Vet J 2023, 13, 1708–1717. [Google Scholar] [CrossRef] [PubMed]
- Chansaisakorn, W.; Sriphavatsarakorn, P.; Sopakdittapong, P.; Trisiriroj, M.; Pondeenana, S.; Buranakarl, C. Oxidative Stress and Intraerythrocytic Concentrations of Sodium and Potassium in Diabetic Dogs. Vet Res Commun 2009, 33, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Liu, S.; Wang, Y.; Zhang, R.; Opoku, Y.K.; Xie, Y.; Li, D.; Ren, G. Fibroblast Growth Factor 21: A Novel Long-Acting Hypoglycemic Drug for Canine Diabetes. Naunyn Schmiedebergs Arch Pharmacol 2021, 394, 1031–1043. [Google Scholar] [CrossRef]
- Li, X.; Wu, H.; Huo, H.; Ma, F.; Zhao, M.; Han, Q.; Hu, L.; Li, Y.; Zhang, H.; Pan, J.; et al. N-Acetylcysteine Combined with Insulin Alleviates the Oxidative Damage of Cerebrum via Regulating Redox Homeostasis in Type 1 Diabetic Mellitus Canine. Life Sci 2022, 308, 120958. [Google Scholar] [CrossRef]
- Suemanotham, N.; Phochantachinda, S.; Chatchaisak, D.; Sakcamduang, W.; Chansawhang, A.; Pitchakarn, P.; Chantong, B. Antidiabetic Effects of Andrographis Paniculata Supplementation on Biochemical Parameters, Inflammatory Responses, and Oxidative Stress in Canine Diabetes. Front Pharmacol 2023, 14, 1077228. [Google Scholar] [CrossRef]
- Cavalcante, C.Z.; Michelotto, P.V.; Capriglione, L.G.A.; Roncoski, A.T.; Nishiyama, A. Weight Loss Modifies Lipid Peroxidation and Symmetric Dimethylarginine Levels in Obese Dogs. Can J Vet Res 2023, 87, 29–34. [Google Scholar]
- Grant, R.W.; Vester Boler, B.M.; Ridge, T.K.; Graves, T.K.; Swanson, K.S. Adipose Tissue Transcriptome Changes during Obesity Development in Female Dogs. Physiol Genomics 2011, 43, 295–307. [Google Scholar] [CrossRef]
- Lucena, S.; Varela Coelho, A.; Anjo, S.I.; Manadas, B.; Mrljak, V.; Capela E Silva, F.; Lamy, E.; Tvarijonaviciute, A. Comparative Proteomic Analysis of Saliva from Dogs with and without Obesity-Related Metabolic Dysfuntion. J Proteomics 2019, 201, 65–72. [Google Scholar] [CrossRef]
- Van de Velde, H.; Janssens, G.P.J.; Stuyven, E.; Cox, E.; Buyse, J.; Hesta, M. Short-Term Increase of Body Weight Triggers Immunological Variables in Dogs. Vet Immunol Immunopathol 2012, 145, 431–437. [Google Scholar] [CrossRef]
- Vecchiato, C.G.; Golinelli, S.; Pinna, C.; Pilla, R.; Suchodolski, J.S.; Tvarijonaviciute, A.; Rubio, C.P.; Dorato, E.; Delsante, C.; Stefanelli, C.; et al. Fecal Microbiota and Inflammatory and Antioxidant Status of Obese and Lean Dogs, and the Effect of Caloric Restriction. Front Microbiol 2022, 13, 1050474. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Kawasumi, K.; Okada, Y.; Ishikawa, S.; Yamamoto, I.; Arai, T.; Mori, N. Comparison of Plasma Lipoprotein Profiles and Malondialdehyde between Hyperlipidemia Dogs with/without Treatment. BMC Vet Res 2014, 10, 67. [Google Scholar] [CrossRef] [PubMed]
- Mancini, A.; Di Segni, C.; Raimondo, S.; Olivieri, G.; Silvestrini, A.; Meucci, E.; Currò, D. Thyroid Hormones, Oxidative Stress, and Inflammation. Mediators Inflamm 2016, 2016, 6757154. [Google Scholar] [CrossRef] [PubMed]
- Perez-Montero, B.; Fermin-Rodriguez, M.L.; Miro, G.; de Juan, L.; Cruz-Lopez, F. Hemolysis, Icterus and Lipemia Interfere with the Determination of Two Oxidative Stress Biomarkers in Canine Serum. BMC Vet Res 2023, 19, 172. [Google Scholar] [CrossRef] [PubMed]
- Fibach, E.; Rachmilewitz, E. The Role of Oxidative Stress in Hemolytic Anemia. Curr Mol Med 2008, 8, 609–619. [Google Scholar] [CrossRef]
- Kogika, M.M.; Lustoza, M.D.; Hagiwara, M.K.; Caragelasco, D.S.; Martorelli, C.R.; Mori, C.S. Evaluation of Oxidative Stress in the Anemia of Dogs with Chronic Kidney Disease. Vet Clin Pathol 2015, 44, 70–78. [Google Scholar] [CrossRef]
- Woolcock, A.D.; Serpa, P.B.S.; Santos, A.P.; Christian, J.A.; Moore, G.E. Reactive Oxygen Species, Glutathione, and Vitamin E Concentrations in Dogs with Hemolytic or Nonhemolytic Anemia. J Vet Intern Med 2020, 34, 2357–2364. [Google Scholar] [CrossRef]
- Kendall, A.; Woolcock, A.; Brooks, A.; Moore, G. e Glutathione Peroxidase Activity, Plasma Total Antioxidant Capacity, and Urinary F2- Isoprostanes as Markers of Oxidative Stress in Anemic Dogs. J Vet Intern Med 2017, 31, 1700–1707. [Google Scholar] [CrossRef]
- Pesillo, S.A.; Freeman, L.M.; Rush, J.E. Assessment of Lipid Peroxidation and Serum Vitamin E Concentration in Dogs with Immune-Mediated Hemolytic Anemia. Am J Vet Res 2004, 65, 1621–1624. [Google Scholar] [CrossRef]
- Tan, E.; Bienzle, D.; Shewen, P.; Kruth, S.; Wood, D. Potentially Antigenic RBC Membrane Proteins in Dogs with Primary Immune-Mediated Hemolytic Anemia. Vet Clin Pathol 2012, 41, 45–55. [Google Scholar] [CrossRef]
- Bujok, J.; Wajman, E.; Trochanowska-Pauk, N.; Walski, T. Evaluation of Selected Hematological, Biochemical and Oxidative Stress Parameters in Stored Canine CPDA-1 Whole Blood. BMC Vet Res 2022, 18, 255. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Deng, J.; Gu, C.; Shen, L.; Ren, Z.; Ma, X.; Yan, Q.; Deng, J.; Zuo, Z.; Wang, Y.; et al. Protective Effect of MitoQ on Oxidative Stress-Mediated Senescence of Canine Bone Marrow Mesenchymal Stem Cells via Activation of the Nrf2/ARE Pathway. In Vitro Cell Dev Biol Anim 2021, 57, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Almeida, B.F.M.; Narciso, L.G.; Bosco, A.M.; Pereira, P.P.; Braga, E.T.; Avanço, S.V.; Marcondes, M.; Ciarlini, P.C. Neutrophil Dysfunction Varies with the Stage of Canine Visceral Leishmaniosis. Vet Parasitol 2013, 196, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Almeida, B.F.M.; Narciso, L.G.; Melo, L.M.; Preve, P.P.; Bosco, A.M.; Lima, V.M.F.; Ciarlini, P.C. Leishmaniasis Causes Oxidative Stress and Alteration of Oxidative Metabolism and Viability of Neutrophils in Dogs. Vet J 2013, 198, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Almeida, B.F.M. de; Silva, K.L.O.; Chiku, V.M.; Leal, A.A.C.; Venturin, G.L.; Narciso, L.G.; Fink, M.F.C.B.; Eugênio, F. de R.; Santos, P.S.P.D.; Ciarlini, P.C.; et al. The Effects of Increased Heme Oxygenase-1 on the Lymphoproliferative Response in Dogs with Visceral Leishmaniasis. Immunobiology 2017, 222, 693–703. [Google Scholar] [CrossRef]
- Bildik, A.; Kargin, F.; Seyrek, K.; Pasa, S.; Ozensoy, S. Oxidative Stress and Non-Enzymatic Antioxidative Status in Dogs with Visceral Leishmaniasis. Res Vet Sci 2004, 77, 63–66. [Google Scholar] [CrossRef]
- de Sousa Gonçalves, R.; de Pinho, F.A.; Dinis-Oliveira, R.J.; Mendes, M.O.; de Andrade, T.S.; da Silva Solcà, M.; Larangeira, D.F.; Silvestre, R.; Barrouin-Melo, S.M. Nutritional Adjuvants with Antioxidant Properties in the Treatment of Canine Leishmaniasis. Vet Parasitol 2021, 298, 109526. [Google Scholar] [CrossRef]
- Heidarpour, M.; Soltani, S.; Mohri, M.; Khoshnegah, J. Canine Visceral Leishmaniasis: Relationships between Oxidative Stress, Liver and Kidney Variables, Trace Elements, and Clinical Status. Parasitol Res 2012, 111, 1491–1496. [Google Scholar] [CrossRef]
- Morabito, R.; Remigante, A.; Cavallaro, M.; Taormina, A.; La Spada, G.; Marino, A. Anion Exchange through Band 3 Protein in Canine Leishmaniasis at Different Stages of Disease. Pflugers Arch 2017, 469, 713–724. [Google Scholar] [CrossRef]
- Paltrinieri, S. Oxidative Stress and Canine Leishmaniasis: More than a Simple Consequence of Host-Parasite Interaction. Vet J 2013, 198, 547–548. [Google Scholar] [CrossRef]
- Quintavalla, F.; Basini, G.; Bussolati, S.; Carrozzo, G.G.; Inglese, A.; Ramoni, R. Redox Status in Canine Leishmaniasis. Animals (Basel) 2021, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Martinez-Subiela, S.; Tvarijonaviciute, A.; Hernández-Ruiz, J.; Pardo-Marin, L.; Segarra, S.; Ceron, J.J. Changes in Serum Biomarkers of Oxidative Stress after Treatment for Canine Leishmaniosis in Sick Dogs. Comp Immunol Microbiol Infect Dis 2016, 49, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Solcà, M.S.; Andrade, B.B.; Abbehusen, M.M.C.; Teixeira, C.R.; Khouri, R.; Valenzuela, J.G.; Kamhawi, S.; Bozza, P.T.; Fraga, D.B.M.; Borges, V.M.; et al. Circulating Biomarkers of Immune Activation, Oxidative Stress and Inflammation Characterize Severe Canine Visceral Leishmaniasis. Sci Rep 2016, 6, 32619. [Google Scholar] [CrossRef] [PubMed]
- Torrecilha, R.B.P.; Utsunomiya, Y.T.; Bosco, A.M.; Almeida, B.F.; Pereira, P.P.; Narciso, L.G.; Pereira, D.C.M.; Baptistiolli, L.; Calvo-Bado, L.; Courtenay, O.; et al. Correlations between Peripheral Parasite Load and Common Clinical and Laboratory Alterations in Dogs with Visceral Leishmaniasis. Prev Vet Med 2016, 132, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Bottari, N.B.; Crivellenti, L.Z.; Borin-Crivellenti, S.; Oliveira, J.R.; Coelho, S.B.; Contin, C.M.; Tatsch, E.; Moresco, R.N.; Santana, A.E.; Tonin, A.A.; et al. Iron Metabolism and Oxidative Profile of Dogs Naturally Infected by Ehrlichia Canis: Acute and Subclinical Disease. Microb Pathog 2016, 92, 26–29. [Google Scholar] [CrossRef]
- Chethan, G.E.; Garkhal, J.; De, U.K. Disturbance of Thyroid Function in Canine Ehrlichiosis and Babesiosis Associated with Oxidative Stress. Comp Clin Pathol 2016, 25, 987–992. [Google Scholar] [CrossRef]
- Çiftci, G.; Pekmezci, D.; Güzel, M.; Çenesiz, S.; Ural, K.; Aysul, N.; Kazak, F. Determination of Serum Oxidative Stress, Antioxidant Capacity and Protein Profiles in Dogs Naturally Infected with Ehrlichia Canis. Acta Parasitol 2021, 66, 1341–1348. [Google Scholar] [CrossRef]
- Da Silva, A.S.; Munhoz, T.D.; Faria, J.L.M.; Vargas-Hérnandez, G.; Machado, R.Z.; Almeida, T.C.; Moresco, R.N.; Stefani, L.M.; Tinucci-Costa, M. Increase Nitric Oxide and Oxidative Stress in Dogs Experimentally Infected by Ehrlichia Canis: Effect on the Pathogenesis of the Disease. Vet Microbiol 2013, 164, 366–369. [Google Scholar] [CrossRef]
- Kumar, A.; Varshney, J.P.; Patra, R.C. A Comparative Study on Oxidative Stress in Dogs Infected with Ehrlichia Canis with or without Concurrent Infection with Babesia Gibsoni. Vet Res Commun 2006, 30, 917–920. [Google Scholar] [CrossRef]
- Pedreañez, A.; Mosquera-Sulbaran, J.; Muñoz, N. Increased Plasma Levels of Nitric Oxide and Malondialdehyde in Dogs Infected by Ehrlichia Canis: Effect of Doxycycline Treatment. Rev Vet Clin 2021, 56, 185–190. [Google Scholar] [CrossRef]
- Pugliese, M.; Biondi, V.; Merola, G.; Landi, A.; Passantino, A. Oxidative Stress Evaluation in Dogs Affected with Canine Monocytic Ehrlichiosis. Antioxidants (Basel) 2022, 11, 328. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Yilmaz, Z.; Martínez-Subiela, S.; Kocaturk, M.; Hernández-Ruiz, J.; Yalcin, E.; Tvarijonaviciute, A.; Escribano, D.; Ceron, J.J. Serum Antioxidant Capacity and Oxidative Damage in Clinical and Subclinical Canine Ehrlichiosis. Res Vet Sci 2017, 115, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Rudoler, N.; Harrus, S.; Martinez-Subiela, S.; Tvarijonaviciute, A.; van Straten, M.; Cerón, J.J.; Baneth, G. Comparison of the Acute Phase Protein and Antioxidant Responses in Dogs Vaccinated against Canine Monocytic Ehrlichiosis and Naive-Challenged Dogs. Parasit Vectors 2015, 8, 175. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, G.; Ural, K.; Aysul, N.; Cenesiz, S.; Guzel, M.; Pekmezci, D.; Sogut, M.Ü. Investigation of the 8-Hydroxy-2’-Deoxyguanosine, Total Antioxidant and Nitric Oxide Levels of Serum in Dogs Infected with Babesia Vogeli. Vet Parasitol 2014, 204, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Crnogaj, M.; Petlevski, R.; Mrljak, V.; Kis, I.; Torti, M.; Kucer, N.; Matijatko, V.; Sacer, I.; Stokovic, I. Malondialdehyde Levels in Serum of Dogs Infected with Babesia Canis. Vet Med 2010, 55, 163–171. [Google Scholar] [CrossRef]
- Crnogaj, M.; Cerón, J.J.; Šmit, I.; Kiš, I.; Gotić, J.; Brkljačić, M.; Matijatko, V.; Rubio, C.P.; Kučer, N.; Mrljak, V. Relation of Antioxidant Status at Admission and Disease Severity and Outcome in Dogs Naturally Infected with Babesia Canis Canis. BMC Vet Res 2017, 13, 114. [Google Scholar] [CrossRef]
- Gonmei, C.; Sarma, K.; Roychoudhury, P.; Ali, M.A.; Singh, D.; Prasad, H.; Ahmed, F.A.; Lalmuanpuii, R.; Shah, N.; Singh, N.S.; et al. Molecular Diagnosis and Clinico-Hemato-Biochemical Alterations and Oxidant-Antioxidant Biomarkers in Babesia-Infected Dogs of Mizoram, India. J Vector Borne Dis 2020, 57, 226–233. [Google Scholar] [CrossRef]
- Murase, T.; Ueda, T.; Yamato, O.; Tajima, M.; Maede, Y. Oxidative Damage and Enhanced Erythrophagocytosis in Canine Erythrocytes Infected with Babesia Gibsoni. J Vet Med Sci 1996, 58, 259–261. [Google Scholar] [CrossRef]
- Teodorowski, O.; Winiarczyk, S.; Tarhan, D.; Dokuzeylül, B.; Ercan, A.M.; Or, M.E.; Staniec, M.; Adaszek, Ł. Antioxidant Status, and Blood Zinc and Copper Concentrations in Dogs with Uncomplicated Babesiosis Due to Babesia Canis Infections. J Vet Res 2021, 65, 169–174. [Google Scholar] [CrossRef]
- Carretón, E.; Cerón, J.J.; Martínez-Subiela, S.; Tvarijonaviciute, A.; Caro-Vadillo, A.; Montoya-Alonso, J.A. Acute Phase Proteins and Markers of Oxidative Stress to Assess the Severity of the Pulmonary Hypertension in Heartworm-Infected Dogs. Parasit Vectors 2017, 10, 477. [Google Scholar] [CrossRef]
- Rajković, M.; Glavinić, U.; Bogunović, D.; Vejnović, B.; Davitkov, D.; Đelić, N.; Stanimirović, Z. “Slow Kill” Treatment Reduces DNA Damage in Leukocytes of Dogs Naturally Infected with Dirofilaria Immitis. Vet Parasitol 2023, 322, 110008. [Google Scholar] [CrossRef] [PubMed]
- Rath, P.K.; Panda, S.; Mishra, B.; Patra, R.; Nath, I. Thoracic Radiography and Oxidative Stress Indices in Heartworm Affected Dogs. Vet World 2014, 7, 689–692. [Google Scholar] [CrossRef]
- Kiral, F.; Karagenc, T.; Pasa, S.; Yenisey, C.; Seyrek, K. Dogs with Hepatozoon Canis Respond to the Oxidative Stress by Increased Production of Glutathione and Nitric Oxide. Vet Parasitol 2005, 131, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Sarma, K.; Eregowda, C.G.; Roychoudhury, P.; Borthakur, S.K.; Jawalagatti, V.; Prasad, H.; Behera, S.K.; Thakur, N.; Bora, N.; Das, D. A 5-Year Prospective Study on Incidence and Clinico-Pathological Changes Associated with Naturally Occurring Trypanosomosis in Dogs of Mizoram, India. Acta Parasitol 2022, 67, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Chethan, G.E.; De, U.K.; Singh, M.K.; Chander, V.; Raja, R.; Paul, B.R.; Choudhary, O.P.; Thakur, N.; Sarma, K.; Prasad, H. Antioxidant Supplementation during Treatment of Outpatient Dogs with Parvovirus Enteritis Ameliorates Oxidative Stress and Attenuates Intestinal Injury: A Randomized Controlled Trial. Vet Anim Sci 2023, 21, 100300. [Google Scholar] [CrossRef]
- Gaykwad, C.; Garkhal, J.; Chethan, G.E.; Nandi, S.; De, U.K. Amelioration of Oxidative Stress Using N-Acetylcysteine in Canine Parvoviral Enteritis. J Vet Pharmacol Ther 2018, 41, 68–75. [Google Scholar] [CrossRef]
- Kocaturk, M.; Tvarijonaviciute, A.; Martinez-Subiela, S.; Tecles, F.; Eralp, O.; Yilmaz, Z.; Ceron, J.J. Inflammatory and Oxidative Biomarkers of Disease Severity in Dogs with Parvoviral Enteritis. J Small Anim Pract 2015, 56, 119–124. [Google Scholar] [CrossRef]
- Panda, D.; Patra, R.C.; Nandi, S.; Swarup, D. Oxidative Stress Indices in Gastroenteritis in Dogs with Canine Parvoviral Infection. Res Vet Sci 2009, 86, 36–42. [Google Scholar] [CrossRef]
- Pugliese, M.; Napoli, E.; Monti, S.; Biondi, V.; Zema, E.; Passantino, A. Oxidative Stress and High-Mobility Group Box 1 Assay in Dogs with Gastrointestinal Parasites. Antioxidants (Basel) 2022, 11, 1679. [Google Scholar] [CrossRef]
- Schmidt, E.M.S.; Tvarijonaviciute, A.; Martinez-Subiela, S.; Cerón, J.J.; Eckersall, P.D. Changes in Biochemical Analytes in Female Dogs with Subclinical Ancylostoma Spp. Infection. BMC Vet Res 2016, 12, 203. [Google Scholar] [CrossRef]
- Beigh, S.A.; Soodan, J.S.; Singh, R.; Khan, A.M. Trace Minerals Status and Antioxidative Enzyme Activity in Dogs with Generalized Demodecosis. Vet Parasitol 2013, 198, 180–186. [Google Scholar] [CrossRef]
- Dimri, U.; Ranjan, R.; Kumar, N.; Sharma, M.C.; Swarup, D.; Sharma, B.; Kataria, M. Changes in Oxidative Stress Indices, Zinc and Copper Concentrations in Blood in Canine Demodicosis. Vet Parasitol 2008, 154, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Subiela, S.; Bernal, L.J.; Tvarijonaviciute, A.; Garcia-Martinez, J.D.; Tecles, F.; Cerón, J.J. Canine Demodicosis: The Relationship between Response to Treatment of Generalised Disease and Markers for Inflammation and Oxidative Status. Vet Dermatol 2014, 25, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Salem, N.Y.; Abdel-Saeed, H.; Farag, H.S.; Ghandour, R.A. Canine Demodicosis: Hematological and Biochemical Alterations. Vet World 2020, 13, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.K.; Dimri, U. The Immuno-Pathological Conversions of Canine Demodicosis. Vet Parasitol 2014, 203, 1–5. [Google Scholar] [CrossRef]
- Behera, S.K.; Dimri, U.; Singh, S.K.; Mohanta, R.K. The Curative and Antioxidative Efficiency of Ivermectin and Ivermectin + Vitamin E-Selenium Treatment on Canine Sarcoptes Scabiei Infestation. Vet Res Commun 2011, 35, 237–244. [Google Scholar] [CrossRef]
- Beigh, S.A.; Soodan, J.S.; Bhat, A.M. Sarcoptic Mange in Dogs: Its Effect on Liver, Oxidative Stress, Trace Minerals and Vitamins. Vet Parasitol 2016, 227, 30–34. [Google Scholar] [CrossRef]
- Camkerten, I.; Sahin, T.; Borazan, G.; Gokcen, A.; Erel, O.; Das, A. Evaluation of Blood Oxidant/Antioxidant Balance in Dogs with Sarcoptic Mange. Vet Parasitol 2009, 161, 106–109. [Google Scholar] [CrossRef]
- Singh, S.K.; Dimri, U.; Sharma, M.C.; Swarup, D.; Sharma, B. Determination of Oxidative Status and Apoptosis in Peripheral Blood of Dogs with Sarcoptic Mange. Vet Parasitol 2011, 178, 330–338. [Google Scholar] [CrossRef]
- Beigh, S.A.; Soodan, J.S.; Singh, R.; Khan, A.M.; Dar, M.A. Evaluation of Trace Elements, Oxidant/Antioxidant Status, Vitamin C and β-Carotene in Dogs with Dermatophytosis. Mycoses 2014, 57, 358–365. [Google Scholar] [CrossRef]
- Marquis, A.; Packer, R.A.; Borgens, R.B.; Duerstock, B.S. Increase in Oxidative Stress Biomarkers in Dogs with Ascending-Descending Myelomalacia Following Spinal Cord Injury. J Neurol Sci 2015, 353, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Teleanu, D.M.; Niculescu, A.-G.; Lungu, I.I.; Radu, C.I.; Vladâcenco, O.; Roza, E.; Costăchescu, B.; Grumezescu, A.M.; Teleanu, R.I. An Overview of Oxidative Stress, Neuroinflammation, and Neurodegenerative Diseases. Int J Mol Sci 2022, 23, 5938. [Google Scholar] [CrossRef] [PubMed]
- Radaković, M.; Andrić, J.F.; Spariosu, K.; Vejnović, B.; Filipović, M.K.; Andrić, N. Serum Oxidant-Antioxidant Status and Butyrylcholinesterase Activity in Dogs with Idiopathic Epilepsy - A Pilot Study. Res Vet Sci 2023, 165, 105076. [Google Scholar] [CrossRef] [PubMed]
- Peek, S.I.; Twele, F.; Meller, S.; Packer, R.M.A.; Volk, H.A. Epilepsy Is More than a Simple Seizure Disorder: Causal Relationships between Epilepsy and Its Comorbidities. Vet J 2024, 303, 106061. [Google Scholar] [CrossRef]
- Coates, J.R.; March, P.A.; Oglesbee, M.; Ruaux, C.G.; Olby, N.J.; Berghaus, R.D.; O’Brien, D.P.; Keating, J.H.; Johnson, G.S.; Williams, D.A. Clinical Characterization of a Familial Degenerative Myelopathy in Pembroke Welsh Corgi Dogs. J Vet Intern Med 2007, 21, 1323–1331. [Google Scholar] [CrossRef]
- Green, S.L.; Bouley, D.M.; Pinter, M.J.; Cork, L.C.; Vatassery, G.T. Canine Motor Neuron Disease: Clinicopathologic Features and Selected Indicators of Oxidative Stress. J Vet Intern Med 2001, 15, 112–119. [Google Scholar] [CrossRef]
- Ogawa, M.; Uchida, K.; Park, E.-S.; Kamishina, H.; Sasaki, J.; Chang, H.-S.; Yamato, O.; Nakayama, H. Immunohistochemical Observation of Canine Degenerative Myelopathy in Two Pembroke Welsh Corgi Dogs. J Vet Med Sci 2011, 73, 1275–1279. [Google Scholar] [CrossRef]
- Brown, S.A. Oxidative Stress and Chronic Kidney Disease. Vet Clin North Am Small Anim Pract 2008, 38, 157–166. [Google Scholar] [CrossRef]
- Irazabal, M.V.; Torres, V.E. Reactive Oxygen Species and Redox Signaling in Chronic Kidney Disease. Cells 2020, 9, 1342. [Google Scholar] [CrossRef]
- Halfen, D.P.; Caragelasco, D.S.; Nogueira, J.P.d.S.; Jeremias, J.T.; Pedrinelli, V.; Oba, P.M.; Ruberti, B.; Pontieri, C.F.F.; Kogika, M.M.; Brunetto, M.A. Evaluation of Electrolyte Concentration and Pro-Inflammatory and Oxidative Status in Dogs with Advanced Chronic Kidney Disease under Dietary Treatment. Toxins (Basel) 2019, 12, E3. [Google Scholar] [CrossRef]
- Martello, E.; Perondi, F.; Bruni, N.; Bisanzio, D.; Meineri, G.; Lippi, I. Chronic Kidney Disease and Dietary Supplementation: Effects on Inflammation and Oxidative Stress. Vet Sci 2021, 8, 277. [Google Scholar] [CrossRef] [PubMed]
- Bosco, A.M.; Almeida, B.F.M.; Pereira, P.P.; Dos Santos, D.B.; Neto, Á.J.S.; Ferreira, W.L.; Ciarlini, P.C. The Uremic Toxin Methylguanidine Increases the Oxidative Metabolism and Accelerates the Apoptosis of Canine Neutrophils. Vet Immunol Immunopathol 2017, 185, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Buranakarl, C.; Trisiriroj, M.; Pondeenana, S.; Tungjitpeanpong, T.; Jarutakanon, P.; Penchome, R. Relationships between Oxidative Stress Markers and Red Blood Cell Characteristics in Renal Azotemic Dogs. Res Vet Sci 2009, 86, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Deuel, J.W.; Schaer, C.A.; Boretti, F.S.; Opitz, L.; Garcia-Rubio, I.; Baek, J.H.; Spahn, D.R.; Buehler, P.W.; Schaer, D.J. Hemoglobinuria-Related Acute Kidney Injury Is Driven by Intrarenal Oxidative Reactions Triggering a Heme Toxicity Response. Cell Death Dis 2016, 7, e2064. [Google Scholar] [CrossRef]
- Liu, J.; Xie, L.; Zhai, H.; Wang, D.; Li, X.; Wang, Y.; Song, M.; Xu, C. Exploration of the Protective Mechanisms of Icariin against Cisplatin-Induced Renal Cell Damage in Canines. Front Vet Sci 2024, 11, 1331409. [Google Scholar] [CrossRef]
- Silva, A.C.R.A.; de Almeida, B.F.M.; Soeiro, C.S.; Ferreira, W.L.; de Lima, V.M.F.; Ciarlini, P.C. Oxidative Stress, Superoxide Production, and Apoptosis of Neutrophils in Dogs with Chronic Kidney Disease. Can J Vet Res 2013, 77, 136–141. [Google Scholar]
- Briganti, S.; Picardo, M. Antioxidant Activity, Lipid Peroxidation and Skin Diseases. What’s New. J Eur Acad Dermatol Venereol 2003, 17, 663–669. [Google Scholar] [CrossRef]
- Plevnik Kapun, A.; Salobir, J.; Levart, A.; Tavčar Kalcher, G.; Nemec Svete, A.; Kotnik, T. Vitamin E Supplementation in Canine Atopic Dermatitis: Improvement of Clinical Signs and Effects on Oxidative Stress Markers. Vet Rec 2014, 175, 560. [Google Scholar] [CrossRef]
- Almela, R.M.; Rubio, C.P.; Cerón, J.J.; Ansón, A.; Tichy, A.; Mayer, U. Selected Serum Oxidative Stress Biomarkers in Dogs with Non-Food-Induced and Food-Induced Atopic Dermatitis. Vet Dermatol 2018, 29, 229–e82. [Google Scholar] [CrossRef]
- Plevnik Kapun, A.; Salobir, J.; Levart, A.; Kotnik, T.; Svete, A.N. Oxidative Stress Markers in Canine Atopic Dermatitis. Res Vet Sci 2012, 92, 469–470. [Google Scholar] [CrossRef]
- Plevnik Kapun, A.; Salobir, J.; Levart, A.; Tavčar Kalcher, G.; Nemec Svete, A.; Kotnik, T. Plasma and Skin Vitamin E Concentrations in Canine Atopic Dermatitis. Vet Q 2013, 33, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Witzel-Rollins, A.; Murphy, M.; Becvarova, I.; Werre, S.R.; Cadiergues, M.-C.; Meyer, H. Non-Controlled, Open-Label Clinical Trial to Assess the Effectiveness of a Dietetic Food on Pruritus and Dermatologic Scoring in Atopic Dogs. BMC Vet Res 2019, 15, 220. [Google Scholar] [CrossRef] [PubMed]
- Romanucci, M.; Bongiovanni, L.; Russo, A.; Capuccini, S.; Mechelli, L.; Ordeix, L.; Della Salda, L. Oxidative Stress in the Pathogenesis of Canine Zinc-Responsive Dermatosis. Vet Dermatol 2011, 22, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Zapata, G.L.; Guajardo, M.H.; Terrasa, A.M. The in Vitro Protective Effect of Alpha-Tocopherol on Oxidative Injury in the Dog Retina. Vet J 2008, 177, 266–272. [Google Scholar] [CrossRef]
- Barden, C.A.; Chandler, H.L.; Lu, P.; Bomser, J.A.; Colitz, C.M.H. Effect of Grape Polyphenols on Oxidative Stress in Canine Lens Epithelial Cells. Am J Vet Res 2008, 69, 94–100. [Google Scholar] [CrossRef]
- Barros, P.S.M.; Padovani, C.F.; Silva, V.V.; Queiroz, L.; Barros, S.B.M. Antioxidant Status of Dog Aqueous Humor after Extracapsular Lens Extraction. Braz J Med Biol Res 2003, 36, 1491–1494. [Google Scholar] [CrossRef]
- Barros, P.S.M.; Safatle, A.M.V.; Queiroz, L.; Silva, V.V.; Barros, S.B.M. Blood and Aqueous Humour Antioxidants in Cataractous Poodles. Can J Ophthalmol 2004, 39, 19–24. [Google Scholar] [CrossRef]
- De Biaggi, C.P.; Barros, P.S.M.; Silva, V.V.; Brooks, D.E.; Barros, S.B.M. Ascorbic Acid Levels of Aqueous Humor of Dogs after Experimental Phacoemulsification. Vet Ophthalmol 2006, 9, 299–302. [Google Scholar] [CrossRef]
- Madany, J. Serum Malondialdehyde Level and Activity of Total Antioxidant Status of Dogs with Age-Related Cataract. Pol J Vet Sci 2016, 19, 429–431. [Google Scholar] [CrossRef]
- Park, S.; Kang, S.; Yoo, S.; Park, Y.; Seo, K. Effect of Oral Antioxidants on the Progression of Canine Senile Cataracts: A Retrospective Study. J Vet Sci 2022, 23, e43. [Google Scholar] [CrossRef]
- Williams, D.L. Oxidation, Antioxidants and Cataract Formation: A Literature Review. Vet Ophthalmol 2006, 9, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Boillot, T.; Rosolen, S.G.; Dulaurent, T.; Goulle, F.; Thomas, P.; Isard, P.-F.; Azoulay, T.; Lafarge-Beurlet, S.; Woods, M.; Lavillegrand, S.; et al. Determination of Morphological, Biometric and Biochemical Susceptibilities in Healthy Eurasier Dogs with Suspected Inherited Glaucoma. PLoS One 2014, 9, e111873. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Gionfriddo, J.R.; Tai, P.-Y.; Novakowski, A.N.; Alyahya, K.; Madl, J.E. Oxidative Stress Increases in Retinas of Dogs in Acute Glaucoma but Not in Chronic Glaucoma. Vet Ophthalmol 2015, 18, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Graham, K.L.; McCowan, C.; White, A. Genetic and Biochemical Biomarkers in Canine Glaucoma. Vet Pathol 2017, 54, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Pizzirani, S. Definition, Classification, and Pathophysiology of Canine Glaucoma. Vet Clin North Am Small Anim Pract 2015, 45, 1127–1157. [Google Scholar] [CrossRef]
- Ajadi, A.; Sanni, J.; Sobayo, E.; Ijaopo, O. Evaluation of Plasma Trace Elements and Oxidant/Antioxidant Status in Boerboel Dogs with Hip Dysplasia. Bulg J Vet Med 2020, 23, 237–247. [Google Scholar] [CrossRef]
- Barrouin-Melo, S.M.; Anturaniemi, J.; Sankari, S.; Griinari, M.; Atroshi, F.; Ounjaijean, S.; Hielm-Björkman, A.K. Evaluating Oxidative Stress, Serological- and Haematological Status of Dogs Suffering from Osteoarthritis, after Supplementing Their Diet with Fish or Corn Oil. Lipids Health Dis 2016, 15, 139. [Google Scholar] [CrossRef]
- Dycus, D.L.; Au, A.Y.; Grzanna, M.W.; Wardlaw, J.L.; Frondoza, C.G. Modulation of Inflammation and Oxidative Stress in Canine Chondrocytes. Am J Vet Res 2013, 74, 983–989. [Google Scholar] [CrossRef]
- Goranov, N.V. Serum Markers of Lipid Peroxidation, Antioxidant Enzymatic Defense, and Collagen Degradation in an Experimental (Pond-Nuki) Canine Model of Osteoarthritis. Vet Clin Pathol 2007, 36, 192–195. [Google Scholar] [CrossRef]
- Musco, N.; Vassalotti, G.; Mastellone, V.; Cortese, L.; Della Rocca, G.; Molinari, M.L.; Calabrò, S.; Tudisco, R.; Cutrignelli, M.I.; Lombardi, P. Effects of a Nutritional Supplement in Dogs Affected by Osteoarthritis. Vet Med Sci 2019, 5, 325–335. [Google Scholar] [CrossRef]
- Gabriele, V.; Bisanzio, D.; Riva, A.; Meineri, G.; Adami, R.; Martello, E. Long-Term Effects of a Diet Supplement Containing Cannabis Sativa Oil and Boswellia Serrata in Dogs with Osteoarthritis Following Physiotherapy Treatments: A Randomised, Placebo-Controlled and Double-Blind Clinical Trial. Nat Prod Res 2023, 37, 1782–1786. [Google Scholar] [CrossRef] [PubMed]
- Polat, E.; Han, M.C.; Kaya, E.; Yilmaz, S.; Kayapinar, S.D.; Coskun, S.; Yildirim, A.; Can, U.K. The Effect of Hip Dysplasia on Some Biochemical Parameters, Oxidative Stress Factors and Hematocrit Levels in Dogs. Pol J Vet Sci 2021, 24, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Prasad, J.K.; Verma, S.; Gattani, A.; Singh, G.D.; Singh, V.K. Evaluation of Uterine Antioxidants in Bitches Suffering from Cystic Endometrial Hyperplasia-Pyometra Complex. Pol J Vet Sci 2024, 27, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Kurt, S.; Eski, F.; Mis, L. Investigation of the Usability of Kisspeptin and Oxidative Stress Parameters in the Early Diagnosis of Asymptomatic Cystic Endometrial Hyperplasia in Dogs. Reprod Domest Anim 2021. [Google Scholar] [CrossRef]
- Szczubiał, M.; Dąbrowski, R.; Bochniarz, M.; Brodzki, P. Uterine Non-Enzymatic Antioxidant Defence Mechanisms (Glutathione, Vitamin C, Copper and Zinc) in Diagnosis of Canine Pyometra. Pol J Vet Sci 2019, 22, 549–555. [Google Scholar] [CrossRef]
- Domosławska-Wyderska, A.; Zduńczyk, S.; Rafalska, A. Potential Role of Oxidative Stress in Pathogenesis of Benign Prostatic Hyperplasia in Male Dogs. Reprod Domest Anim 2024, 59, e14580. [Google Scholar] [CrossRef]
- Peștean, C.P.; Pocquet, H.; Dumitraș, D.A.; Morohoschi, A.G.; Ștefănuț, L.C.; Andrei, S. Correlation between Oxidative Stress Markers and Periodontal Disease in Dogs. Vet Sci 2024, 11, 99. [Google Scholar] [CrossRef]
- Schroers, M.; Reiser, K.; Alexander, T.; Zablotski, Y.; Meyer-Lindenberg, A. Saliva Malondialdehyde Concentration of Dogs With and Without Periodontal Disease. J Vet Dent 2024, 8987564241248042. [Google Scholar] [CrossRef]
- Vajdovich, P. Free Radicals and Antioxidants in Inflammatory Processes and Ischemia-Reperfusion Injury. Vet Clin North Am Small Anim Pract 2008, 38, 31–123. [Google Scholar] [CrossRef]
- Hagen, D.M.; Ekena, J.L.; Geesaman, B.M.; Viviano, K.R. Antioxidant Supplementation during Illness in Dogs: Effect on Oxidative Stress and Outcome, an Exploratory Study. J Small Anim Pract 2019, 60, 543–550. [Google Scholar] [CrossRef]
- Viviano, K. r.; VanderWielen, B. Effect of N-Acetylcysteine Supplementation on Intracellular Glutathione, Urine Isoprostanes, Clinical Score, and Survival in Hospitalized Ill Dogs. J Vet Intern Med 2013, 27, 250–258. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




