1. Introduction
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA®) is an innovative and increasingly utilized technique in trauma care for the management of massive hemorrhage. Over recent years, REBOA has emerged as a valuable tool in controlling non-compressible torso hemorrhage, which is a leading cause of preventable death in trauma patients [
1,
2]. The procedure involves the percutaneous insertion of a balloon catheter into the aorta to temporarily occlude distal blood flow, thereby controlling hemorrhage while maintaining perfusion to vital organs [
3,
4].
Despite its potential benefits, the application of REBOA requires careful patient selection and specialized training due to risks associated with aortic occlusion, such as ischemia and vascular injury [
5,
6]. Ongoing research focuses on refining the technique, determining optimal balloon positioning, and integrating REBOA usage with advanced imaging modalities to enhance patient outcomes [
7,
8]. Moreover, recent studies have explored the utility of REBOA in pre-hospital settings and its impact on survival rates in severe trauma cases[
9].
This report presents the case of a 45-year-old woman treated with REBOA® following a suicide attempt involving a fall from a height of approximately 5 meters, leading to massive hemorrhage and multiple traumatic injuries. The case underscores the potential life-saving role of REBOA® in severe trauma where conventional resuscitation efforts may be insufficient
2. Materials and Methods
2.1. Case Presentation
A 45-year-old woman was transported to the emergency department (ED) following a fall from an estimated height of 5 meters in a suspected suicide attempt. Initial clinical assessment revealed profound hemodynamic instability with a blood pressure of 52/30 mmHg and a heart rate of 167 beats per minute, yielding a shock index of 3.2. Capillary refill time exceeded 3 seconds, indicating severe circulatory collapse.
Given the clinical suspicion of a pelvic fracture, a T-POD® device was applied for stabilization. Airway management was promptly addressed with orotracheal intubation, and manual ventilation was initiated. End-tidal CO₂ measurement was 47 mmHg, indicating adequate ventilation post-intubation. Physical examination revealed symmetrical chest expansion without signs of facial or cranial trauma. The trachea was midline, and jugular veins were flat. Cardiac examination revealed tachycardia with normal S1 and S2 heart sounds, and no murmurs were detected. Abdominal examination was unremarkable. The left lower limb exhibited internal rotation, suggestive of a pelvic fracture. A cautious log roll revealed no abrasions, hematomas, or additional injuries.
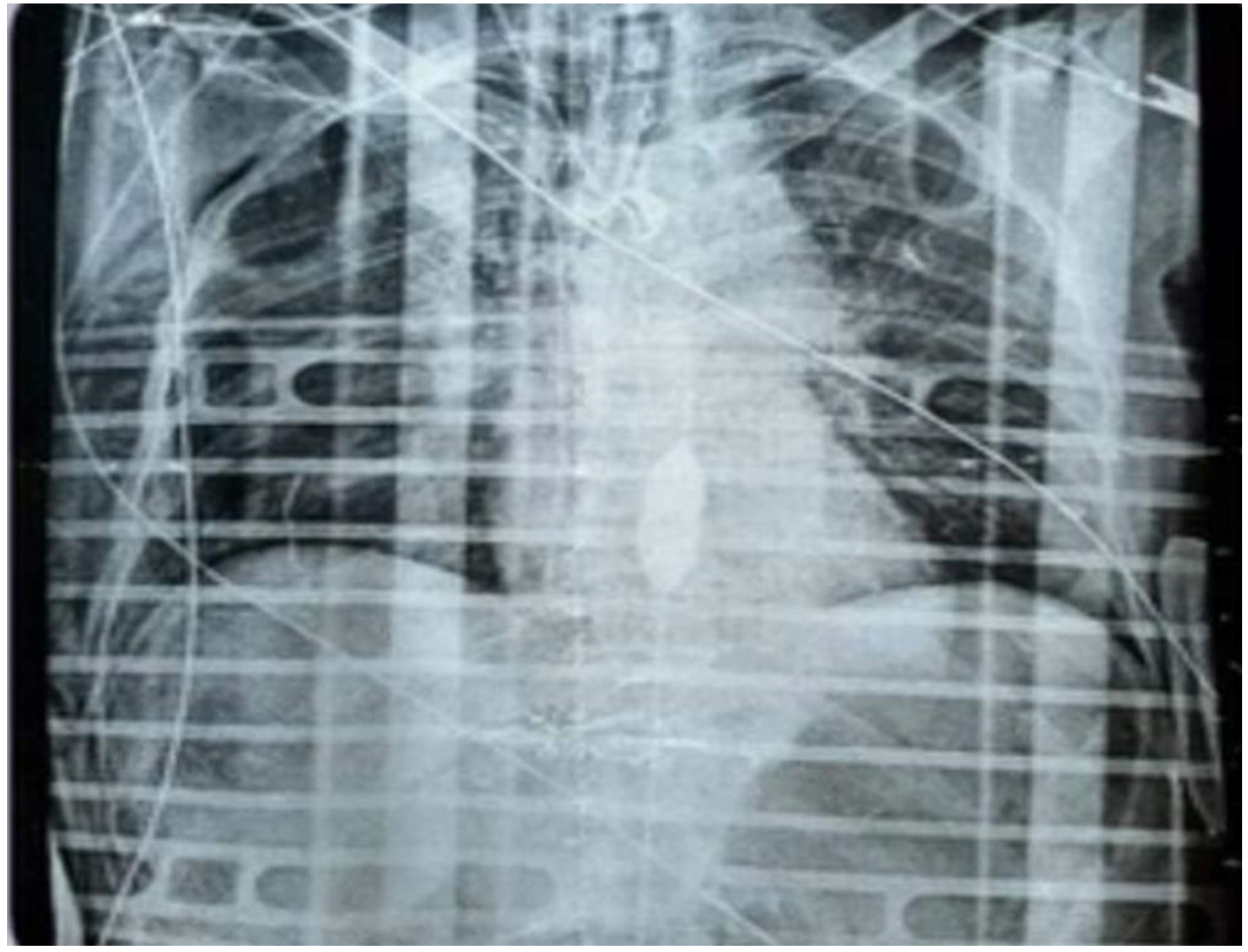
Diagnostic imaging included chest and pelvic radiographs. The chest X-ray demonstrated subcutaneous emphysema of the right chest wall, a small right apical pneumothorax, and displaced fractures of the right 6th rib with non-displaced fractures of the 7th and 8th ribs. A right subclavian central venous catheter was visualized with its tip in the right atrium. The pelvic X-ray revealed a displaced comminuted fracture of the bilateral iliopubic rami, more pronounced on the left side, and a fracture of the left acetabulum with misalignment of bone fragments.
Arterial blood gas analysis indicated severe hyperlactatemic metabolic acidosis with mild uncompensated hypercapnia and mild hypocalcemia. Laboratory results on admission showed hemoglobin at 10 g/dL, moderate leukocytosis, platelet count of 218 × 10⁹/L, elevated creatinine at 1.54 mg/dL, fibrinogen at 187 mg/dL (normal range: 200–400 mg/dL), high-sensitivity troponin at 1184.3 pg/mL (normal range: 4–11 pg/mL), alanine aminotransferase (ALT) at 714 U/L (normal range: 10–40 U/L), urea at 32.6 mg/dL, and lactate dehydrogenase (LDH) at 2497 U/L (normal range: up to 250 U/L). Coagulation tests showed an international normalized ratio (INR) of 1.4 and activated partial thromboplastin time (aPTT) of 15 seconds. Electrolytes were within normal ranges except for glucose at 256 mg/dL. Urinalysis was normal.
An Extended Focused Assessment with Sonography for Trauma (E-FAST) was performed, revealing no evidence of massive pneumothorax but slight bilateral basal fluid collections. A small amount of free fluid was detected in Morrison's pouch and the Douglas pouch, suggesting intra-abdominal bleeding. Hyperechoic areas in the spleen indicated potential splenic injury.
2.2. Resuscitation
Damage Control Resuscitation was initiated promptly. A bolus of 1000 mL of Ringer's Lactate was administered intravenously to address hypovolemia. Tranexamic acid (1 g IV) was given to promote hemostasis. Blood products were transfused, including one unit of packed red blood cells, one unit of fresh frozen plasma, and pooled platelets to manage volume depletion and coagulopathy. Calcium chloride (2 g IV) was administered to correct hypocalcemia, which can occur in massive transfusion or acidosis. Norepinephrine infusion was started at 1 μg/kg/min to maintain adequate perfusion pressure. Sodium bicarbonate (1.4% and 8.4%) was administered to correct metabolic acidosis, a common complication in trauma patients. Coagulation factors, including Factor IX (Kedcom® 2500 U), Factor II (2500 U), and Factor VII (Provertinum® 600 U), along with vitamin K, were administered to reverse coagulopathy. Rotational thromboelastometry (ROTEM®) was performed to assess the patient’s coagulation status, which is crucial in managing trauma patients at high risk of bleeding.
Neurologically, the patient was profoundly impaired with a Glasgow Coma Scale (GCS) of 3T. Pupillary response showed miosis, but there were no signs of cranial trauma such as periorbital ecchymosis or Battle's sign, and no cerebrospinal fluid rhinorrhea was observed.
2.3. Hemodynamic Instability and REBOA Deployment
Despite aggressive resuscitative efforts, the patient's hemodynamic condition deteriorated, culminating in cardiac arrest with ventricular fibrillation observed on the monitor. Defibrillation was attempted without return of spontaneous circulation, and pulseless electrical activity ensued. Given the critical situation, a REBOA® catheter was urgently inserted using the blind method and positioned in Zone 1 of the aorta during ongoing chest compressions facilitated by an automated CPR device (LUCAS®). Correct placement was assessed by verifying the device’s centimeter markings. This intervention successfully restored a palpable central pulse, temporarily stabilizing the patient's circulation with a blood pressure of 155/62 mmHg and a heart rate of 110 bpm.
Following return of spontaneous circulation, the patient was transferred to the radiology department for a full-body contrast-enhanced CT scan. Imaging revealed a significant aortic rupture extending from the aortic isthmus to the arch. It was noted that the REBOA® balloon had been inadvertently placed within a false lumen, necessitating repositioning under radiological guidance. Additional findings included burst fractures of the thoracic vertebrae at T5 and T9, a comminuted pelvic fracture, a transverse fracture of the sacrum at S3, and a blowout fracture of the left acetabulum (
Figure 1).
3. Results
The timely insertion of the REBOA® device provided critical hemodynamic support, allowing for temporary stabilization and enabling the patient's transfer to a Level 1 Trauma Center for definitive care. Upon arrival, she underwent emergency surgery, including placement of an aortic endograft, splenectomy, and pelvic stabilization with an external fixator. Postoperatively, she was admitted to the intensive care unit.
4. Discussion
This case represents the utilization of REBOA® in a Zone Trauma Center (ZTC) to arrest major bleeding from non-compressible injuries in a patient experiencing cardiac arrest. The deployment of REBOA® facilitated a 'bridge to surgery,' allowing for the patient's transfer to a higher-level trauma center located approximately 20 minutes away [
10]. The intended 30-minute occlusion time, based on the balloon's placement in Zone 1, was partially adhered to by employing partial and intermittent occlusion techniques. This approach aimed to maintain some distal perfusion, thereby limiting ischemia-reperfusion injury typically associated with prolonged aortic occlusion [
5,
6]. In the days following the procedure, the patient exhibited only mild renal, gastrointestinal, and lower limb distress, suggesting that partial occlusion may mitigate some complications associated with REBOA®.
Despite the severe nature of her injuries, the use of REBOA® was instrumental in stabilizing the patient for transport and subsequent surgical intervention. This case underscores the potential life-saving role of REBOA® in emergency settings, particularly when conventional resuscitation methods are insufficient.
Several studies have demonstrated the effectiveness of REBOA in temporarily controlling hemorrhage and stabilizing patients for definitive surgical intervention [
7]. However, the timing of REBOA deployment is critical. Early application may prevent progression to cardiac arrest, while delayed use may reduce its efficacy [
9,
11]. Complications associated with REBOA include vascular injuries, limb ischemia, and organ dysfunction due to prolonged aortic occlusion [
5,
6]. Therefore, guidelines recommend limiting occlusion time and continuous monitoring of distal perfusion [
12]. Advances in REBOA technology, such as partial or intermittent balloon occlusion, aim to mitigate these risks [
8,
13].
The integration of REBOA into trauma protocols requires multidisciplinary collaboration and training [
12]. Simulation-based education has been shown to enhance provider competence and improve patient outcomes [
14]. The authors advocate for the acquisition of operational competence in REBOA® deployment within emergency departments, especially in settings where immediate surgical intervention is not available. Mastery of this technique can enhance patient outcomes by serving as a critical bridge to definitive care, even when transfer to a specialized trauma center is required.
5. Conclusions
This case illustrates the potential utility of REBOA® in managing severe hemorrhagic shock due to traumatic injuries when conventional resuscitation is insufficient. The successful temporary stabilization achieved with REBOA® allowed for continued resuscitative efforts and transfer for definitive care. Further research is warranted to refine REBOA® techniques, optimize patient selection, and integrate its use with imaging modalities to improve outcomes in trauma care. Training in REBOA® deployment should be considered essential for emergency department personnel to improve patient outcomes in severe trauma cases.
Author Contributions
Conceptualization, I.C., A.B., and M.B.; methodology, I.C. and A.B.; software, S.M. and M.Z.; validation, I.C., A.B., and M.B.; formal analysis, I.C. and A.B.; investigation, M.B. and S.M.; resources, M.Z. and F.M.; data curation, M.B. and S.M.; writing—original draft preparation, I.C., A.B., and M.B.; writing—review and editing, I.C., A.B., M.B., and F.L.; visualization, M.Z. and F.M.; supervision, F.L. and V.P.; project administration, S.C. and A.C.; funding acquisition, F.L. and V.P.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Not Applicable.
Acknowledgments
Not Applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jansen, J.O.; Hudson, J.; Cochran, C.; MacLennan, G.; Lendrum, R.; Sadek, S.; Gillies, K.; Cotton, S.; Kennedy, C.; Boyers, D.; et al. Emergency Department Resuscitative Endovascular Balloon Occlusion of the Aorta in Trauma Patients With Exsanguinating Hemorrhage: The UK-REBOA Randomized Clinical Trial. JAMA 2023, 330, 1862–1871. [CrossRef]
- Castellini, G.; Gianola, S.; Biffi, A.; Porcu, G.; Fabbri, A.; Ruggieri, M.P.; Coniglio, C.; Napoletano, A.; Coclite, D.; D’Angelo, D.; et al. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in Patients with Major Trauma and Uncontrolled Haemorrhagic Shock: A Systematic Review with Meta-Analysis. World J. Emerg. Surg. WJES 2021, 16, 41. [CrossRef]
- Manzano Nunez, R.; Naranjo, M.P.; Foianini, E.; Ferrada, P.; Rincon, E.; García-Perdomo, H.A.; Burbano, P.; Herrera, J.P.; García, A.F.; Ordoñez, C.A. A Meta-Analysis of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) or Open Aortic Cross-Clamping by Resuscitative Thoracotomy in Non-Compressible Torso Hemorrhage Patients. World J. Emerg. Surg. WJES 2017, 12, 30. [CrossRef]
- van de Voort, J.C.; Kessel, B.; Borger van der Burg, B.L.S.; DuBose, J.J.; Hörer, T.M.; Hoencamp, R. Consensus on Resuscitative Endovascular Balloon Occlusion of the Aorta in Civilian (Prehospital) Trauma Care: A Delphi Study. J. Trauma Acute Care Surg. 2024, 96, 921–930. [CrossRef]
- Ribeiro Junior, M.A.F.; Feng, C.Y.D.; Nguyen, A.T.M.; Rodrigues, V.C.; Bechara, G.E.K.; de-Moura, R.R.; Brenner, M. The Complications Associated with Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). World J. Emerg. Surg. WJES 2018, 13, 20. [CrossRef]
- Russo, R.M.; Neff, L.P.; Lamb, C.M.; Cannon, J.W.; Galante, J.M.; Clement, N.F.; Grayson, J.K.; Williams, T.K. Partial Resuscitative Endovascular Balloon Occlusion of the Aorta in Swine Model of Hemorrhagic Shock. J. Am. Coll. Surg. 2016, 223, 359–368. [CrossRef]
- Saito, N.; Matsumoto, H.; Yagi, T.; Hara, Y.; Hayashida, K.; Motomura, T.; Mashiko, K.; Iida, H.; Yokota, H.; Wagatsuma, Y. Evaluation of the Safety and Feasibility of Resuscitative Endovascular Balloon Occlusion of the Aorta. J. Trauma Acute Care Surg. 2015, 78, 897–903; discussion 904. [CrossRef]
- Sadek, S.; Lockey, D.J.; Lendrum, R.A.; Perkins, Z.; Price, J.; Davies, G.E. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in the Pre-Hospital Setting: An Additional Resuscitation Option for Uncontrolled Catastrophic Haemorrhage. Resuscitation 2016, 107, 135–138. [CrossRef]
- Norii, T.; Miyata, S.; Terasaka, Y.; Guliani, S.; Lu, S.W.; Crandall, C. Resuscitative Endovascular Balloon Occlusion of the Aorta in Trauma Patients in Youth. J. Trauma Acute Care Surg. 2017, 82, 915–920. [CrossRef]
- Borger van der Burg, B.L.S.; Kessel, B.; DuBose, J.J.; Hörer, T.M.; Hoencamp, R. Consensus on Resuscitative Endovascular Balloon Occlusion of the Aorta: A First Consensus Paper Using a Delphi Method. Injury 2019, 50, 1186–1191. [CrossRef]
- Hoshi, H.; Endo, A.; Yamamoto, R.; Yamakawa, K.; Suzuki, K.; Akutsu, T.; Morishita, K. Use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) for Trauma and Its Performance in Japan over the Past 18 Years: A Nationwide Descriptive Study. World J. Emerg. Surg. 2024, 19, 19. [CrossRef]
- Moore, L.J.; Brenner, M.; Kozar, R.A.; Pasley, J.; Wade, C.E.; Baraniuk, M.S.; Scalea, T.; Holcomb, J.B. Implementation of Resuscitative Endovascular Balloon Occlusion of the Aorta as an Alternative to Resuscitative Thoracotomy for Noncompressible Truncal Hemorrhage. J. Trauma Acute Care Surg. 2015, 79, 523–530; discussion 530-532. [CrossRef]
- K, K.; A, S.; M, M.; A, E. Resuscitative Endovascular Balloon Occlusion of Aorta: A Systematic Review. Am. Surg. 2022, 88. [CrossRef]
- Birrenbach, T.; Wespi, R.; Hautz, W.E.; Berger, J.; Schwab, P.R.; Papagiannakis, G.; Exadaktylos, A.K.; Sauter, T.C. Development and Usability Testing of a Fully Immersive VR Simulation for REBOA Training. Int. J. Emerg. Med. 2023, 16, 67. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).