1. Introduction
Radiotherapy is one of the most popular cancer treatment methods, using ionizing X-rays with high ionization energy. Ionization energy causes electrons to be ejected. As the energy increases, the ability of the rays to penetrate the skin increases, this property helps to reduce the dose. Cells undergoing division are most susceptible to radiation. Cancer cells have a higher division frequency than healthy cells, making them more susceptible to damage caused by radiotherapy [
1].
Therapies using ionizing radiation are characterized by local effects and are limited to places where cancer lesions occur. The aim of treatment is to induce specific but desired physicochemical phenomena [
2]. They cause biological effects such as: damage to cell membranes and DNA, as a result of which their ability to divide and further metabolic processes is impaired, or immediate cell apoptosis. Radiotherapy can be implemented as an independent form of treatment or as an accompanying therapy to chemotherapy [
3].
Unfortunately, the use of radiotherapy also causes side effects, both in the epidermis, dermis and subcutaneous tissue. Skin reactions after radiotherapy can be divided into early and late reactions. Early reactions usually appear within a few weeks of starting treatment. It is characterized by excessive skin dryness, pigmentation disorders, erythema and hair loss. As a result of exposure, sebaceous and sweat glands, hair follicles and pigment cells are damaged. The body produces more pro-inflammatory cytokines, including: interleukins 1 and 6, TGF-β and TNF-α [
4]. Erythema on the skin is a photochemical reaction, as a result of which the cells of the spinous layer of the epidermis are damaged and the proteins of this layer are denatured, and then histamine is released, blood vessels dilate, resulting in skin hyperemia. The duration of erythema depends on the dose and frequency of radiation to which the skin was exposed. The consequence of erythema is exfoliation of the epidermis and its thickening.
In the early stage of post-radiation reaction, we observe exfoliation of the epidermis, which occurs as a result of damage to keratinocytes in the basal layer, accompanied by itching. Dry exfoliation turns into wet exfoliation, accompanied by the exudation of serous fluid. An early reaction is also permanent dilation of blood vessels, i.e., the development of telangiectasia.
Late reaction occurs several months after the end of therapy. It is caused by the reaction of fibroblasts to radiation. Fibroblasts are cells characterized by low proliferation potential. With the degradation of collagen fibers, atrophic changes appear in the skin. Increased synthesis of collagen with an irregular arrangement of fibers contributes to the appearance of thickening and fibrosis in the skin tissue, and the skin loses its elasticity [
5].
Ionizing radiation, which is used in cancer radiotherapy, is responsible for the formation of free oxygen radicals (Reactive Oxygen Species - ROS), which interact with biomolecules. They contribute to the development of the above-mentioned radiation reactions in the skin and subcutaneous tissue [
6,
7].
More and more women, after undergoing anti-cancer treatment, are looking for solutions to specific skin problems in dermatological and cosmetic clinics. The appropriate care treatment should be selected very individually, taking into account the type of cancer, the time since the end of treatment, the general condition of the patient, as well as factors such as smoking, previous care and skin condition. All treatments that regenerate, moisturize and soothe itchy skin are applicable. Proper skin moisturizing is important primarily due to the damage to the function of the sebaceous and sweat glands during anti-cancer therapy. You should not decide on treatments that are invasive, irritating and damaging the outer protective layer of the skin [
8,
9,
10].
The aim of the study was to check skin tolerance and the effectiveness of a cosmetic preparation whose main active substance was collagen of fish origin, and to select other ingredients in such a way as to minimize the occurrence of side effects of oncological therapy after radiotherapy.
Most skin reactions associated with anticancer treatment should subside within a few weeks of its completion. However, there are so-called late skin complications that can persist for months or years after the end of therapy. They usually take the form of pigmentation disorders (darker skin, areas of lighter spots), fibrosis, skin hardening, and the appearance of telangiectasia, i.e. visible dilation of small blood vessels. Much less common are complications in the form of ulcers and increased susceptibility to skin infections. The formation of late skin reactions is associated with a decrease in the population of fibroblasts in the skin and their production of collagen molecules with an irregular fiber arrangement, which clinically causes hardening, fibrosis, and scarring. The formation of keloids promotes lymph circulation disorders and the formation of edema, and consequently trophic changes and ulcers. All of the above symptoms may take the form of recurrent symptoms, but sometimes they take the form of chronic changes. It should also be remembered that secondary cancers may develop in the area of irradiated skin years after the end of treatment [
11,
12,
13,
14].
The most important building blocks of the skin are collagen type I and type III. Collagen I is a fibrillar collagen that has long fibers and serves as a support in human skin. However, its proper functioning is closely linked to collagen type III, which in turn determines the appropriate spatial arrangement of collagen type I fibers. The state of oxidative stress occurring in the skin of a patient undergoing radiotherapy causes significant dysfunctions in the functioning and structure of collagen.
One of the few forms of collagen used in cosmetology and care that is not subject to chemical processing is collagen type III - interchangeably called native collagen or tropocollagen.
Collagen type III is most often obtained from the skin of young animals. Recently, the use of marine collagen, isolated from fish processing waste, such as skin, bones, fins, scales, etc., has been increasing. Using waste instead of throwing it away allows for the maximum use of resources and is undoubtedly an environmentally friendly approach. The source of marine collagen can be fish, invertebrates, marine mammals and algae. It is also important to note that collagen obtained from marine resources is characterized by a low probability of sensitization, biocompatibility, is soluble in water, biodegradable and easy to obtain [
14,
15,
16].
It is these features of collagen obtained from marine resources that made it the main component of the tested preparation. The product uses collagen from fish skin, which plays an analogous role to tropocollagen. In addition, it is characterized by a low molecular weight, thanks to which it effectively soothes irritations and supports the regeneration of skin subjected to radiotherapy [
17].
2. Materials and Methods
The cosmetic preparation collagen laminate obtained by ultrafiltration was tested on patients who underwent therapy at the University Hospital and who underwent radiotherapy. Patients are currently no longer undergoing treatment. The research group of 50 women suffered from breast cancer (n = 50). Before the experiment, the patients' skin was examined to diagnose its condition (zero condition). The study was conducted with the consent of the Bioethics Committee (consent number 692/23). Each participant received a commercial cosmetic preparation. People who underwent radiotherapy applied the cosmetic to the area exposed to radiation, i.e., their breasts. Patients used the preparation twice a day, in the morning and in the evening. The preparation was used to eliminate skin reactions to oncological treatment. The study lasted 6 months. The test subjects came mainly from small towns and villages in the Lubusz Voivodeship. The average age in the study group was 54 years (age range: 35–74 years). Then, digital measurements were performed monthly using a Courage + Khazaka Electronic GmbH device to measure hydration, TEWL and pH value. Patients were asked to wash their skin with water. Then wait 10 minutes before applying the preparation. The above-mentioned skin parameters (stratum corneum) were measured using probes. The experiment was conducted with the patients' informed consent. They were also interviewed to collect information about their health and skin condition. Patients used a commercial collagen laminate cream that contained the following INCI ingredients: Aqua, Pectin, Collagen (Soluble Collagen), Saccharomyces Cerevisiae (Yeast Hulls) /Hexapeptide-11 Ferment Lysate, Pyrus Malus Fruit Extract/Pectin, Lactobionic Acid, Linum Usitatissimum Seed Extract, Gluconolactone, Panthenol, Polysorbate 20, Citric Acid, Trisodium Ethylenediamine Disuccinate, Calcium Gluconate, Sodium Benzoate, Potassium Sorbate.
3. Results
The figures below 1-3 show the average variation in the levels of hydration, transepidermal water loss and skin pH value, before the application of the tested formula and throughout the entire study. Measurement checks were performed once a month. All parameters were measured in a group of 50 people in the place that was exposed to radiation, i.e., the pedestrian area.
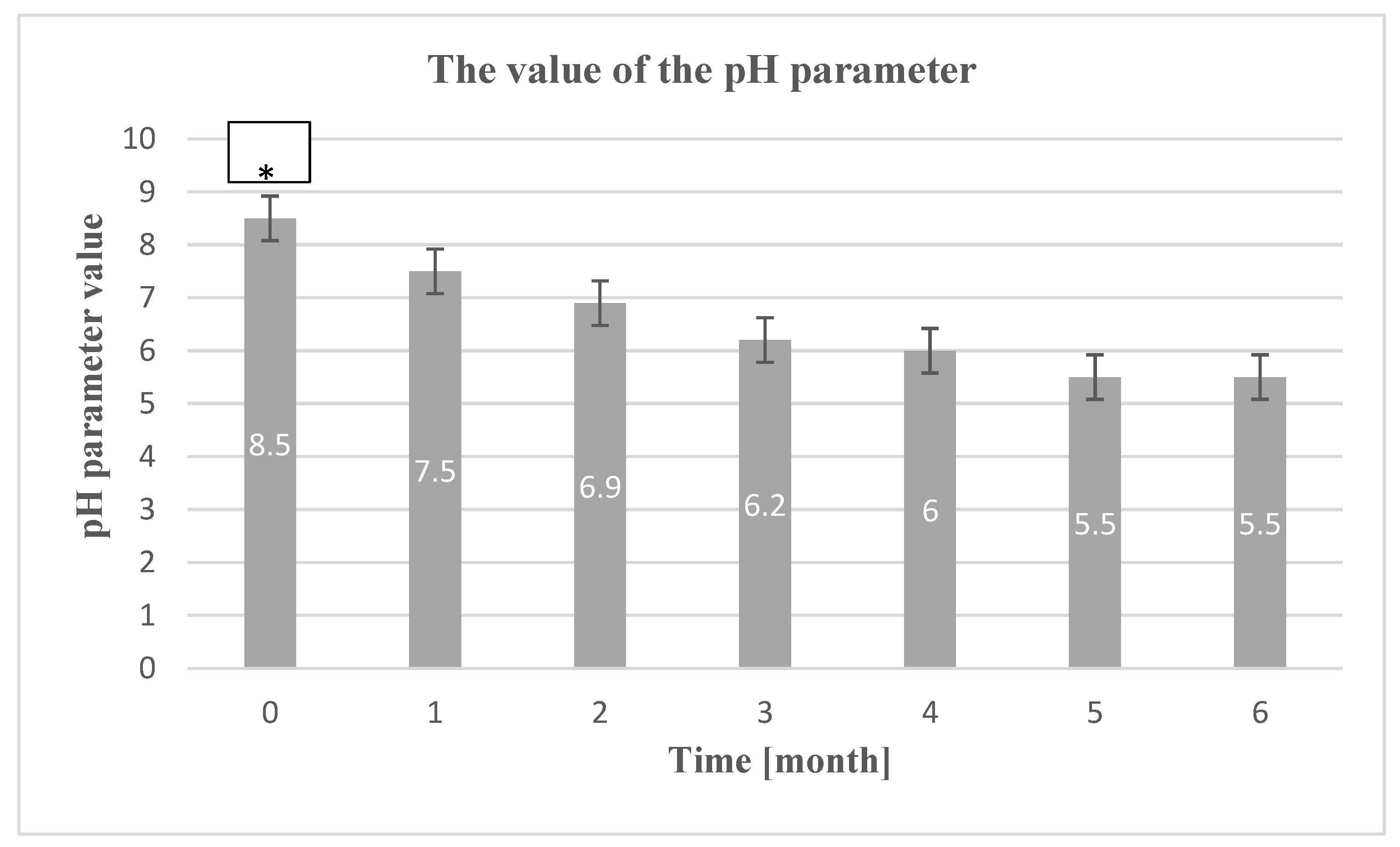
3.1. Hydration Level
The average degree of hydration of the epidermis before laminate application and after 1-6 months is shown in
Figure 1.
Table 1.
Interpretation of epidermal hydration measurement results.
Table 1.
Interpretation of epidermal hydration measurement results.
| The degree of hydration of the epidermis |
Measurement result |
| Very dry skin |
< 30
30 – 45 |
Dry skin
The skin is sufficiently moisturized |
˃ 45 |
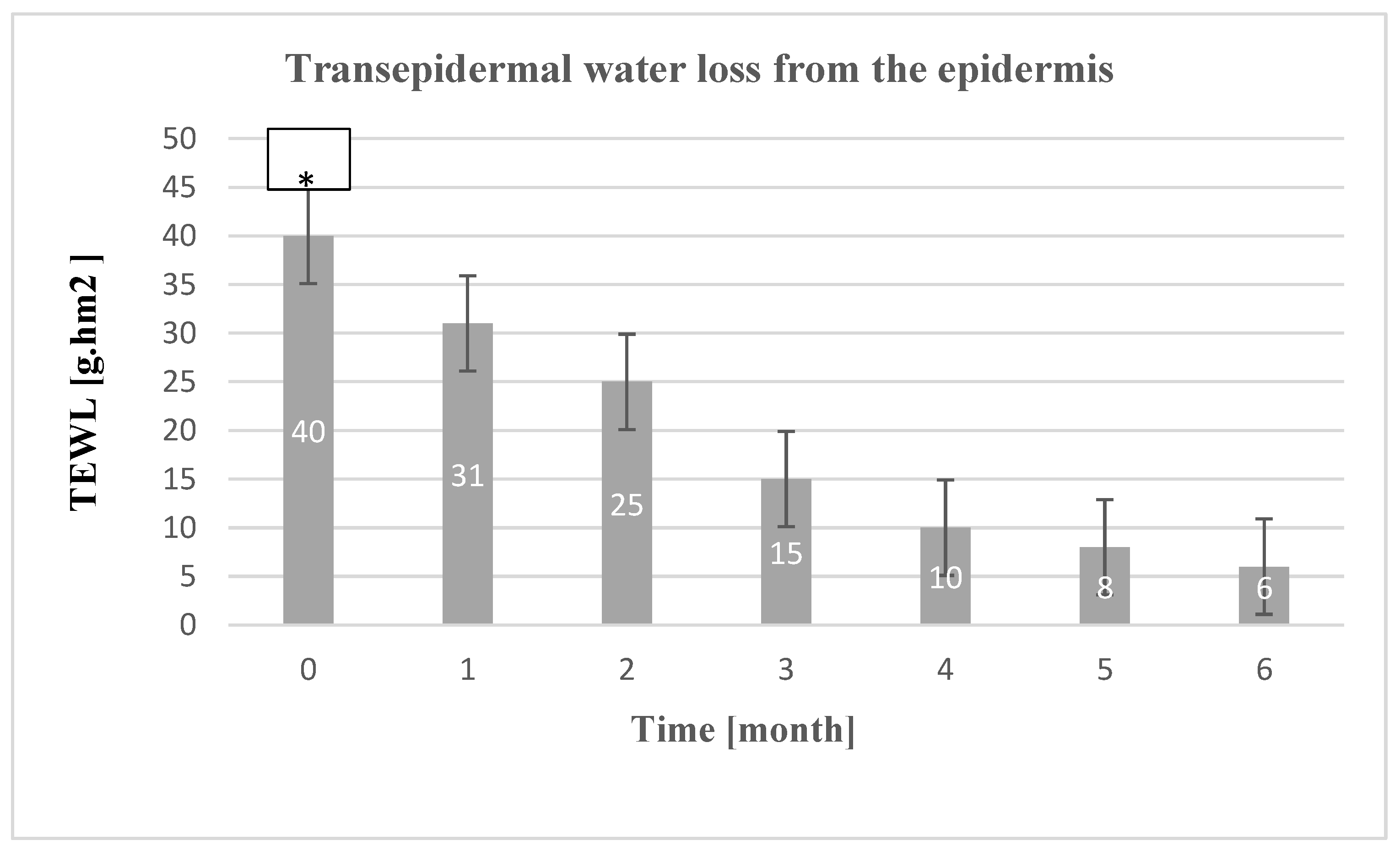
3.2. Transepidermal Water Loss Level from the Epidermis (TEWL)
Figure 2 shows the average level of variation in the transepidermal water loss parameter.
Table 2.
Interpretation of epidermal TEWL measurement results.
Table 2.
Interpretation of epidermal TEWL measurement results.
| Interpretation of the results |
Value TEWL [g/hm2] |
| Very healthy skin |
0 – 10 |
| Healthy skin |
10 – 15 |
| Normal skin |
15 – 25 |
| Leather in poor condition |
25 – 30 |
The results of the epidermal TEWL level were interpreted based on the table below.
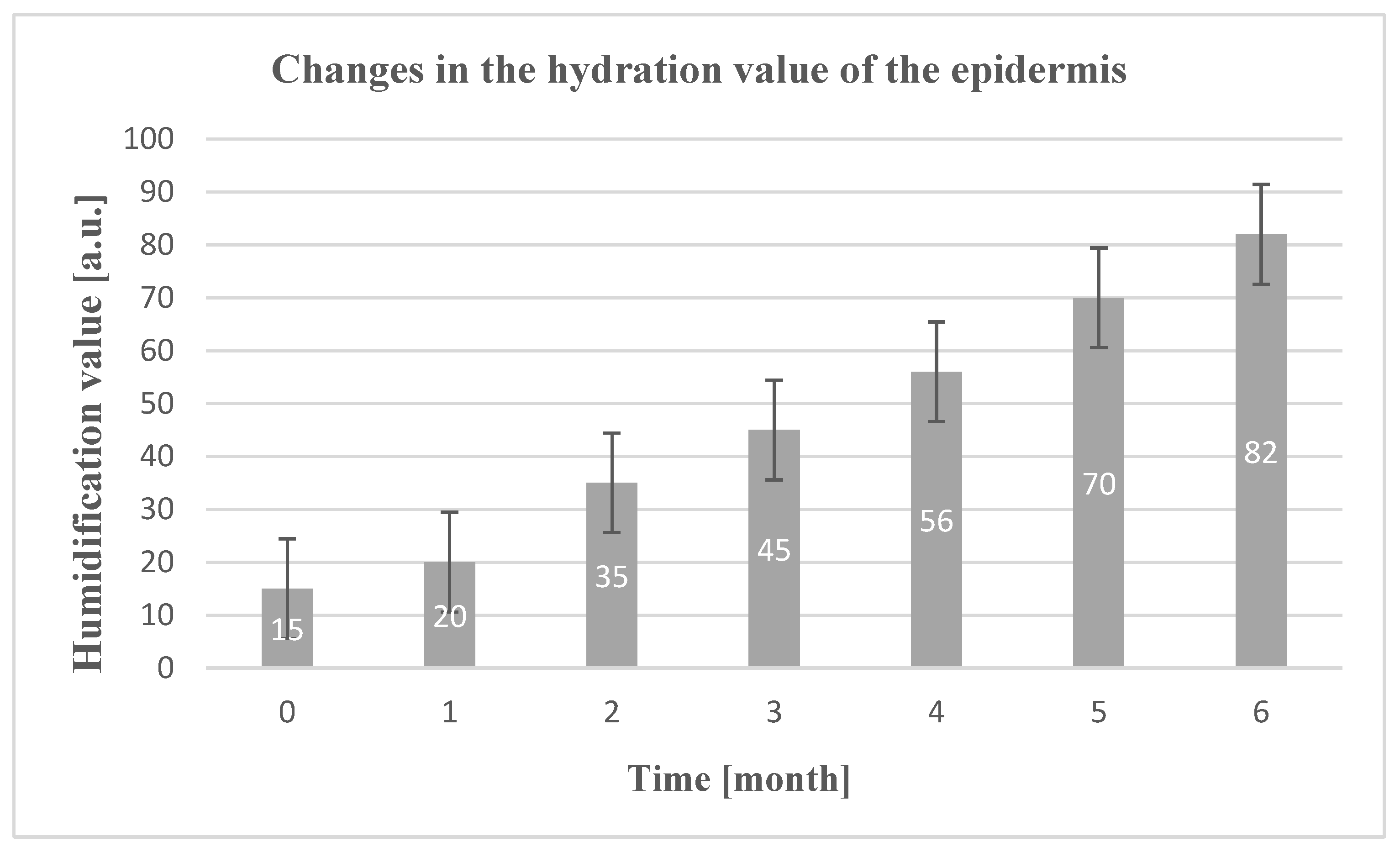
3.3. pH Parameter Value
The normal reaction of human skin is acidic, ranging between 4 and 6 in the outermost layers of the skin. The dermis has a pH value of approximately 7. The slightly acidic pH on the skin has a bacteriostatic effect, prevents excessive colonization of pathogenic bacteria and facilitates the proper course of the skin cell exfoliation process. The hydrolipid coat, sebaceous gland secretions and NMF are responsible for maintaining the appropriate pH level of the skin. Many external factors can affect the pH level, such factors include: too aggressive detergents, UV radiation, atmospheric factors, inadequate skin care, lack of a balanced diet. Each of these factors affects the deficiency of the ingredients that make up the hydrolipid coat and the natural moisturizing factor.
The average change in pH value before laminate application and after 1-6 months is presented in Figure 3.
Figure 2.
Change in the pH value of patients' skin after the first use of the preparation and during its use after radiotherapy **p < 0.01 - significant increase from the 1st to the 6th month (W6) based on the post-hoc test. Group size test (n = 50).
Figure 2.
Change in the pH value of patients' skin after the first use of the preparation and during its use after radiotherapy **p < 0.01 - significant increase from the 1st to the 6th month (W6) based on the post-hoc test. Group size test (n = 50).
3. Discussion
Based on the above graph 1, it can be seen that all people who participated in the study had better results in the hydration parameter as the experiment progressed.
Table 1 presents the interpretation of the results of the discussed parameter. Changes in the hydration parameter ranged on average from 15-82 [a.u.].
Already after the first use, the device's skin hydration level increases by 5 [a.u.]. In the next month it is increased by 15 [a.u.] in the fourth month it increases by 30 [IU]. Staff skin hydration levels increased linearly over time. After 5 parameters enabling 55 [a.u.]. And after 6 a.m., another one until 6 a.m. [a.u.]. During and after radiotherapy, the subjects' skin was hypersensitive, itchy and prone to cracking. The hydrolipid barrier weakened and the body was unable to protect itself against the consequences [
9]. In order to achieve a disease state as a result of treatment, moisturizing preparations should be used. It has been shown that collagen, which is a component of the product but is also detached from our skin, is very harmful to it due to its structure. A long-term state of oxidative stress that is affected by radiation therapy, dysfunction in the role and development of collagen. The form that does not undergo chemical degradation is native collagen. It is obtained from fish skins, isolated from fish skins obtained from fish processing. their existence allows for resource management and is excluded from environmental friendliness. Collagen obtained from marine resources that do not have an allergenic potential, due to its molecular content and biocompatibility with human collagen. The effect of skin regeneration after radiotherapy. Moreover, it's good water-soluble and biodegradable. Increases the resistance of skin cells to environmental factors, including radiation. Hexapeptide-11 Peptide Encapsulated in Yeast (INCI: Saccharomyces Cerevisiae (Yeast Hulls) / Hexapeptide-11 Ferment Lysate) is a substance that is especially beneficial for the condition of the skin. Research results suggest that this compound improves skin hydration by stimulating the production of glycosaminoglycans and collagen, which are responsible for the proper hydration of the deeper layers of the skin. On the surface of the epidermis, they create an impenetrable filter for evaporating water. The hydrophobic active substance penetrates deep into the epidermis, thus replenishing the lipids in the protective layer. Consequently, the emulsion increases the skin's moisturizing parameter [
8,
9,
10]. Pectins from UPCYCLING apple pomace (INCI: Pyrus Malus Fruit Extract/Pectin), which were obtained after juice production. They contain antioxidants that help protect the skin. Pectins support the skin through their moisturizing properties. They act as a moisture-binding agent, which helps maintain the appropriate level of hydration.
The ability of the stratum corneum to retain water is an important parameter that indirectly regulates skin hydration and indicates whether the hydro-lipid barrier is functioning properly. The dermis contains 80% water, while the stratum corneum contains only 13%. The average TEWL value measured in probands after radiotherapy was 40 [g/hm2]. With the duration of the study, the TEWL parameter gradually improved, oscillating after 6 months of study at an average level of 6 [g/hm2] (Fig. 2). As a result of regular use of the preparation, which contained flax extract (INCI: Linum Usitatissimum Seed Extract) rich in fatty acids, vitamins and minerals, as well as alpha-linolenic acid, which has a moisturizing effect and supports the condition of the skin. This ingredient supports the occlusive effect of fatty raw materials and the physicochemical effect on intercellular cement. Lipids are incorporated into cement structures, which allows the properties of the epidermal barrier to change. Free radicals oxidize fatty acids that make up cell membranes and the hydrolipid coat of the skin (this is the process of lipid peroxidation) and damage structural proteins, among others. collagen and enzymatic proteins (aggregation and denaturation process) [
18]. Lipid peroxidation involves the oxidation of unsaturated fatty acids, resulting in the formation of fatty acid peroxides, which, like reactive oxygen species, are characterized by very high chemical reactivity. As a result of this process, excessive water loss may be observed, which is inextricably linked to the dry skin that occurs during and after radiotherapy. In summary, the TEWL value improved after application of the product, also thanks to the phenomenon of merging/gluing irregular epidermal cells [
19,
20].
X-ray therapy also has an adverse effect on the condition of the skin, increasing the normal slightly acidic reaction on the skin surface. Based on the research, it was found that the longer the time passed since the end of the therapy, the less alkaline the pH became Figure 3.
In order to accelerate the return of the appropriate pH reaction and thus the ability to perform protective functions, during the study the subjects were advised not to wash their skin with aggressive detergents, which also contribute to many irritations, excessive evaporation of water from the skin layers and increased sensitivity to external factors. To speed up the process of restoring the appropriate pH value after therapy, the preparation contains glucanolactone (INCI: Gluconolactone), panthenol and citric acid (INCI: Citric Acid). In addition to their pH-restoring properties, these compounds also have soothing and moisturizing properties. They have a soothing effect on irritations. Panthenol (INCI: Panthenol), which is another ingredient of the cosmetic formula tested in our study, accelerates healing, soothes irritations, burns and allergies [
21,
22,
23].
5. Conclusions
It was confirmed that the product tested for an oncological patient has an appropriate level of skin hydration, supports the reconstruction of the skin and its energy barrier by reducing transepidermal water loss and restoring appropriate pH values. Thanks to this, the effects of pathological changes can be removed and the effects of pathological changes can be accelerated. For the emulsion to be more effective in patients exposed to ionized effects, it should be used long-term.
After interviewing the test subjects about their sensory and application experiences, moisturization occurred and the wound healing process was accelerated. The respondents observed that regular use influences better results. The entire group of test subjects agreed that the effect of the product was consistent with the manufacturer's claims.
Maintaining balance on the surface of the skin should be a priority in the equipment, and then it can be used to prepare lubricating and moisturizing preparations.
The new modern methodology, based on obtaining fish skins from the fishing industry, is an innovative method due to the use of the upcycling trend. The formula of the test cosmetic is used to remove CO
2 emissions. They give them a second life. The upcycling trend to a future solution in terms of providing utility functions and additionally gaining access to active ingredients [
24,
25,
26,
27,
28,
29].
Author Contributions
Conceptualization, J.I-K. and J.I-K.; methodology, J.I-K.; software, J.I-K.; validation, J.I-K.; formal analysis, J.I-K.; investigation, J.I-K.; resources, J.I-K.; data curation, J.I-K.; writing—original draft preparation, J.I-K.; writing—review and editing, J.I-K.; visualization, J.I-K.; supervision, J.I-K..; project administration, J.I-K.; funding acquisition, J.I-K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Bioethics Committee consent, resolution number 692/23.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
Support from University of Education and Therapy and Symbiosis Laboratory is acknowledged.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- McKay, J.; Hirano N (Ed). Chemotherapy radiotherapy, 1th ed,; Gdańskie: Wydawnictwo Psychologiczne; Gdansk, Poland; 2002.
- Autier, J.; Mateus, C.; Wechsler, L. Cutaneous side effects of sorafenib and sunitinib. Ann Dermatol Venereol. 2008, 135, 148–53. [Google Scholar] [CrossRef] [PubMed]
- Bergonie, J.; Tribondeau, L.L. Interpretation de quelques resultants de la radiotherapie et essai de fixation d’une technique rationnelle. CR Seances Acad Sci. 1996, 143, 983–985. [Google Scholar]
- McQuestion, M. Evidence-based skin care management in radiation therapy. Semin Oncol Nurses. 2006, 22, 163–73. [Google Scholar] [CrossRef] [PubMed]
- Brzozowska – Mańkowska, S.; Graczyk, M.; Szpinda, M.; Wiśniewski, M. Radiation dermatitis – principles of treatment. PTOP. 2013, 2, 33–47. [Google Scholar]
- Michalewska, J. Radiation reactions in radiotherapy and radiation dermatitis. Letters in Oncology Science. 2017, 14, 104–109. [Google Scholar] [CrossRef]
- Escudier, B.; Eisen, T.; Stadler, W.M. Sorafenib for treatment of renal cell carcinoma: final efficacy and safety results of the phase III treatment approaches in renal cancer global evalu- ation trial. J Clin Oncol. 2009, 27, 3312–8. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.W.; Goldman, B.H.; Lara P.N., Jr. Sorafenib with interferon alfa-2b in first-line treatment of advanced renal carcinoma: a phase II study of the Southwest Oncology Group. J Clin Oncol. 2007, 25, 3296–301. [Google Scholar] [CrossRef]
- Martini, M.C. Cosmetology and skin pharmacology, 1st ed., Warszawa: PZWL Wydawnictwo Lekarskie; Warsov, Poland; 2014.
- Ong, P.Y.; Ohtake, T.; Brandt, C.; Strickland, I.; Boguniewicz, M.; Ganz, T.; et al. Endogenous Antimicrobial Peptides and Skin Infections in Atopic Dermatitis. N Engl J Med. 2002, 347, 1151–1160. [Google Scholar] [CrossRef]
- Tianhong; Roman P. Skin toxicities associated with epidermal growth factor receptor inhibitors. Targ Oncol. 2009, 4, 107–119. [CrossRef]
- Galimont-Collen, AFS.; Vos LE, Lavrijsen, A.P.M.; Ouwerkerkb, J.; Gelderblomb, H. Classification and management of skin, hair and nail and mucosal side-effects of epidermal growth factor receptor (EGFR) inhibitors. Eur J Cancer. 2007, 43, 845–851. [CrossRef]
- Jatoi ,A.; Nguyen, P.L. Do patients die from rashes from epidermal growth factor receptor inhibitors? A systematic review to help counsel patients about holding therapy. Oncologist. 2008, 13, 1201–1204. [CrossRef] [PubMed]
- Wagner, L.I.; Lacouture, M.E. Dermatologic toxicities associated with EGFR inhibitors: the clinical psychologist’s perspective. Impact on health-related quality of life and implications for clinical management of psychological sequelae. Oncology (Williston Park) 2007, 21, 34–36. [Google Scholar] [PubMed]
- Vasquez-Bayo, C.; Rodriguez-Bujaldon, A.L; Jimenez-Puya, R.; Galàn-Gutierrez, M.; Moreno-Gimenez, J.C. Capecitabine induced hyperpigmentation. Actas Dermosifiliogr. 2007, 98, 491–493. [Google Scholar] [CrossRef]
- Milano, G.; Etlenne-Grimaldi, M.C.; Marl, M.; Lasalle,S.; Formento ,J.; Francoual, M. et al. Candidate mechanisms for capecitabine related hand-foot syndrome. Br J Clin Pharmacol. 2008, 66, 188–95. [CrossRef]
- Dave, S.; Thappa, D.M. Peculiar pattern of nail pigmentation following cyclophosphamide therapy. Dermatol Online J. 2003, 9, 13–18. [Google Scholar] [CrossRef]
- Rawlings, A.V.; Matts, P.J.; Anderson, C.F. Roberts MS. Skin biology, xerosis, barrier repair and measurement. Drug Discov Today Dis Mech. 2008, 5, 27–136. [Google Scholar] [CrossRef]
- Tatala, M.; Janowski, K.; Wałachowska, K.; Król, K.; Serej, B. Quality of life in women in the aspect of experiencing breast cancer. Horizons of Psychology. 2013, 3, 163–171. [Google Scholar]
- Lodén, M. The skin barrier and use of moisturizers in atopic dermatitis. Clin Dermatol. 2003, 21, 145–157. [Google Scholar] [CrossRef]
- Darlenski, R.; Sassning, S.; Tsankov, N.; Fluhr, J. W. Non-invasive in vivo methods for investigation of the skin barrier physical properties. Eur J Pharm Biopharm. 2009, 72, 95–303. [Google Scholar] [CrossRef]
- 22 Loden, M.; Maibach, H.I. Dry Skin and Moisturizers. Chemistry and Function, CRC Press: London, New York, Washington; 2009.
- Kacalak-Rzepka, A.; Bielecka-Grzela, S.; Klimowicz, A.; Wesołowska, J, Maleszka R. Dry skin as a dermatological and cosmetic problem. Rocz Pomor Akad Med. 2008, 1, 54–56.
- Igielska-Kalwat, J.; Kilian-Pięta, E. The Use of Dalmatian Tansy and Auxiliary Substances as Natural Substitutes in the Treatmentof Dermatosis. SSRG. 2021, 8, 1–9. [Google Scholar]
- Igielska-Kalwat, J.; Kilian-Pięta, E.; Połoczańska-Godek, S. The use of biodegradable polymers obtained from fish waste in hair. Polymers. 2022, 14, 749. [Google Scholar] [CrossRef] [PubMed]
- Igielska-Kalwat, J.; Połoczańska-Godek, S.; Murawa, D.; Poźniak-Balicka, R.; Wachowiak, M; Demski, G.; Slawomir, Cieśla. Effects of selected cytostatic drugs and ionized air on the skin of oncological patients. Adv Dermatol Allergol. 2022, 39, 47–51.
- Mashaan, N.; Chegenizadeh, A.; Nikraz, H. Laboratory Properties of Waste PET Plastic-Modified Asphalt Mixes. Recycling. 2021, 6, 49–55. [Google Scholar] [CrossRef]
- Enfrin, M.; Myszka, R.; Giustozzi, F. Paving roads with recycled plastics: Microplastic pollution or eco-friendly solution? J. Hazard. Mater. 2022, 437, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Bare, J. TRACI 2.0: The tool for the reduction and assessment of chemical and other environmental impacts 2.0. Clean Technol. Environ. Policy 2011, 13, 687–696. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).