1. Introduction
Gallstones are among the most common gastrointestinal disorders worldwide, affecting approximately 10-20% of the population, and their prevalence varies by region and ethnicity, being generally higher in Europe and the United States compared to Asia [
1]. Gallstones impose a substantial economic and resource burden on healthcare systems. In the United States, more than 700,000 cholecystectomies are performed annually, incurring healthcare costs exceeding
$6.5 billion, and total healthcare expenditures for the prevention and treatment of gallstone disease reach up to
$62 billion annually, significantly straining the healthcare infrastructure [
2]. Although most patients with gallstones are asymptomatic, without timely intervention, serious complications such as acute pancreatitis, cholangitis, and acute cholecystitis can occur, and can be life-threatening in severe cases [
3]. Risk factors for gallstones include pregnancy, obesity, metabolic syndrome, a high-fat diet, and rapid weight loss [
4,
5,
6]. Effective clinical indicators to predict or prevent gallstone occurrence are still lacking. Thus, effective management of gallstone-related complications and risk factors is critical to alleviating the growing health and economic burden they pose.
Gallstone formation is closely related to abnormal cholesterol metabolism, changes in bile composition, dysfunctional gallbladder dynamics, and inflammatory responses, with oxidative stress playing a critical role in these processes [
7]. Oxidative stress refers to the imbalance between oxidative and antioxidant systems in the body, leading to the overproduction of free radicals such as reactive oxygen species (ROS) and reactive nitrogen species (RNS), which induces inflammatory responses and causes cellular damage. Cholestasis and gallbladder dysfunction can increase oxidative stress, which alters the components of bile, including cholesterol, bile salts, and phospholipids, facilitating stone formation [
8]. Oxidative stress activates signaling pathways such as NF-κB and Nrf2, causing an imbalance in the expression of inflammatory factors and antioxidant enzymes, which promotes cholesterol crystallization and accelerates stone formation [
9].
The Oxidative Balance Score (OBS) is an index used to comprehensively assess an individual’s oxidative stress status, combining 16 nutrients and 4 lifestyle factors, including 15 antioxidants and 5 pro-oxidants, and reflects oxidative balance through quantitative values [
10]. A higher OBS indicates higher antioxidant levels and lower oxidative stress. Previous studies have shown that OBS is associated with conditions such as non-alcoholic fatty liver disease and kidney stones, and a high OBS is associated with a lower incidence of these diseases [
11,
12]. However, no studies have investigated the relationship between OBS and gallstones or gallbladder surgery.
Based on data from the National Health and Nutrition Examination Survey (NHANES) between 2017 and 2020, this study combines various demographic data, lifestyle factors, and disease characteristics, aiming to explore the potential relationship between OBS and gallstones as well as gallbladder surgery. The findings are expected to provide important evidence for a deeper understanding of the relationship between OBS and the risk of gallstones and surgery, which will help clinicians more accurately identify high-risk populations, develop personalized prevention and treatment strategies, and enhance the health management of gallstone patients.
2. Materials and Methods
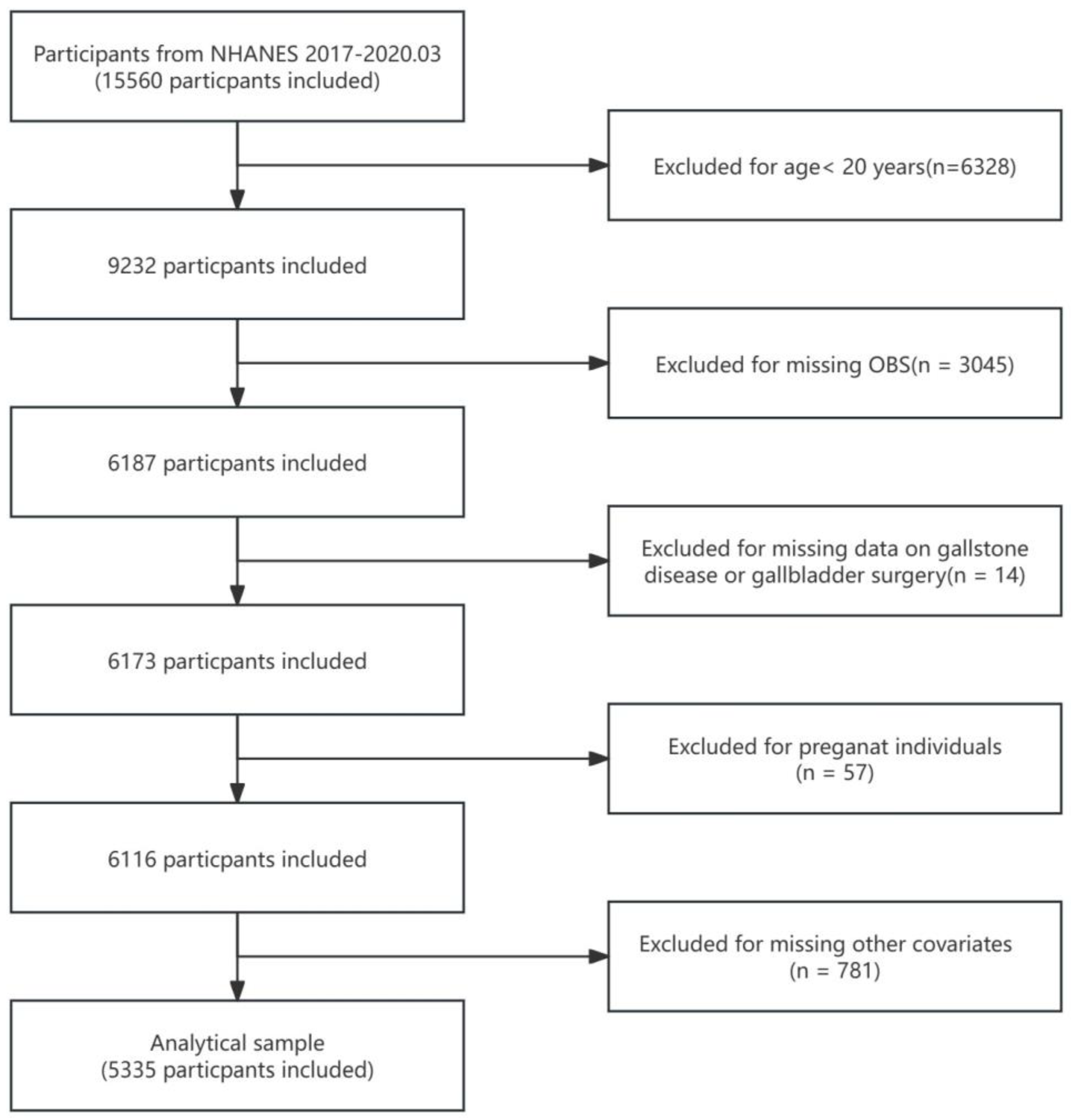
NHANES is a national survey led by the Centers for Disease Control and Prevention (CDC). Since the 1960s, NHANES has helped researchers understand health trends of the U.S. population by collecting and analyzing data on health, nutrition, disease, and physical condition.NHANES strictly follows the principle of informed consent, with all participants signing a written informed consent form prior to their participation, and personal information is strictly anonymized. The data for this study was obtained from NHANES 2017-2020.03 There were 15,560 participants with gallstones exclusion criteria of (1) Age < 20 years (n = 6328) (2) Participants with missing OBS (n = 3045) (3) Participants with lack of data on gallstone prevalence and gallbladder surgery (n = 14). (4) Participants who were pregnant (n = 57) (5) Participants missing other covariates (n = 781) Finally, 5335 participants were included in the final analysis. Of these, 2560 were male and 2775 were female; the detailed screening process is shown in
Figure 1.
Exposure Definition
OBS is a metric used to quantify oxidative stress in the body. The score takes into account the levels of 5 pro-oxidants and 15 antioxidants in the body to reflect an individual's oxidative balance. Specifically, it is calculated from 16 dietary components, such as dietary fiber, carotenoids, riboflavin, niacin, vitamin B6, total folate, vitamin B12, vitamin C, vitamin E, calcium, magnesium, zinc, copper, selenium, total fat, and iron, along with 4 lifestyle factors, including physical activity, alcohol consumption, smoking status, and body mass index (BMI). Of these, total fat, iron, BMI, alcohol consumption, and smoking were considered pro-oxidants, while the other components functioned as antioxidants. Physical activity was measured by calculating the frequency and duration of weekly activity and the corresponding metabolic equivalent (MET) score. Alcohol consumption was categorized into non-drinking, moderate drinking (0-15 g/day for women and 0-30 g/day for men), and heavy drinking (≤15 g/day for women and ≤30 g/day for men), while smoking was assessed by serum cotinine levels. Other components were stratified according to their tertiles in different gender populations, with antioxidants scored 0-2 and pro-oxidants scored 2-0, and all scores were summed to calculate the total OBS score.
Results Definition
Patients with gallstones were defined as those who responded "yes" to the NHANES MCQ questionnaire, "Has a doctor or other health professional ever told you that you have gallstones?" Gallbladder surgery patients were identified by answering "yes" to the question, "Have you had gallbladder surgery?"
Covariates
To avoid the influence of confounding factors, we included relevant covariates in our analysis. The covariates included age, gender, race, education, marital status, poverty-to-income ratio (PIR), stroke, lung disease, heart disease, hypertension, diabetes mellitus, alanine aminotransferase (ALT), alkaline phosphatase (ALP), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), and total energy intake. Race was categorized as Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, and other ethnic groups. Educational attainment was categorized as less than high school, high school graduate, and more than high school education. Marital status was categorized into three groups: married or cohabiting, divorced, separated, or widowed, and never married. PIR was categorized into low-income (<1.3), middle-income (1.3-3.5), and high-income (≥3.5) groups. Stroke diagnosis was based on patient self-report. Patients were categorized as having heart disease if they were diagnosed with any of congestive heart failure, coronary artery disease, myocardial infarction, or angina pectoris, and as having lung disease if diagnosed with any of asthma, chronic obstructive pulmonary disease, or emphysema. Hypertension was defined as meeting any of the following criteria: (1) diagnosed by a physician; (2) having a mean systolic blood pressure of 130 mmHg or more, or a mean diastolic blood pressure of 80 mmHg or more; and (3) receiving antihypertensive medication. Diabetes was defined as (1) a physician-confirmed diagnosis, (2) an HbA1c value of 6.5% or greater, and (3) treatment with diabetes medication or insulin. Energy intake was derived from the mean of two 24-hour dietary recall interviews from NHANES.
Statistical Analysis
Continuous variables were reported as mean ± standard deviation (SD), and categorical variables were reported as percentages. Statistical significance was assessed using the t-test and chi-square test. OBS was divided into four quartile groups using Q1 as the reference group. A multivariate logistic regression analysis was conducted to examine the association between OBS and the prevalence of gallstones, the incidence of gallbladder surgery, and the age at first gallbladder surgery. Model 1 was unadjusted, Model 2 was adjusted for age, gender, and race, while Model 3 was additionally adjusted for age, gender, race, education, marital status, poverty-to-income ratio (PIR), history of stroke, lung disease, heart disease, hypertension, diabetes mellitus, liver function indicators (ALT, ALP, AST, and GGT), and total energy intake. Results were expressed as weighted odds ratios (OR) with 95% confidence intervals (95% CI). The robustness of the results was verified by subgroup analyses, and the dose-response relationship between OBS and gallbladder surgery was assessed using smoothed curve fitting. All statistical analyses were conducted using R software (version 4.4.1,
http://www.R-project.org) and EmpowerStats software (versions 2.0 and 4.2,
http://www.empowerstats.com), and a p-value of <0.05 was considered statistically significant.
3. Results
3.1. Participant Characteristics
This study included 5335 participants aged 20 years or older. As shown in
Table 1, the mean age of the participants was 50.843 ± 17.122 years, and 47.985% of the participants were male. There were 586 participants diagnosed with gallstones and 603 participants who underwent gallbladder surgery. The mean value of OBS was 21.093 ± 7.280. The group with the highest OBS, compared to the group with a lower OBS, had higher ALT, lower ALP, higher AST, lower GGT, higher total energy intake, were more likely to be Mexican American, have education beyond high school, a high PIR, and were less likely to have complications such as stroke, lung disease, heart disease, hypertension, diabetes, gallstones, or gallbladder surgery.
3.2. Association of OBS with Gallstones and Gallbladder Surgery
Table 2 presents the results of multivariate logistic regression analyses between OBS and gallstones as well as gallbladder surgery, with OBS divided into continuous and categorical variables, across multiple models adjusted for different covariates. The results indicate that in the fully adjusted model (model 2), OBS was significantly and negatively associated with both gallstone prevalence and gallbladder surgery. Each one-unit increase in OBS was associated with a 2.6% decrease in the odds of gallstone prevalence (OR = 0.974 [0.958, 0.990]) and a 3.3% decrease in the odds of gallbladder surgery (OR = 0.967 [0.950, 0.983]). The negative association with gallstone prevalence and gallbladder surgery was more pronounced in the highest OBS quartile compared to the lowest. In the fourth quartile group, each one-unit increase in OBS was associated with a 43.3% decrease in the odds of gallstone prevalence (OR = 0.567 [0.406, 0.793]) and a 53.5% decrease in the odds of gallbladder surgery (OR = 0.465 [0.330, 0.655]).
3.3. Subgroup Analysis
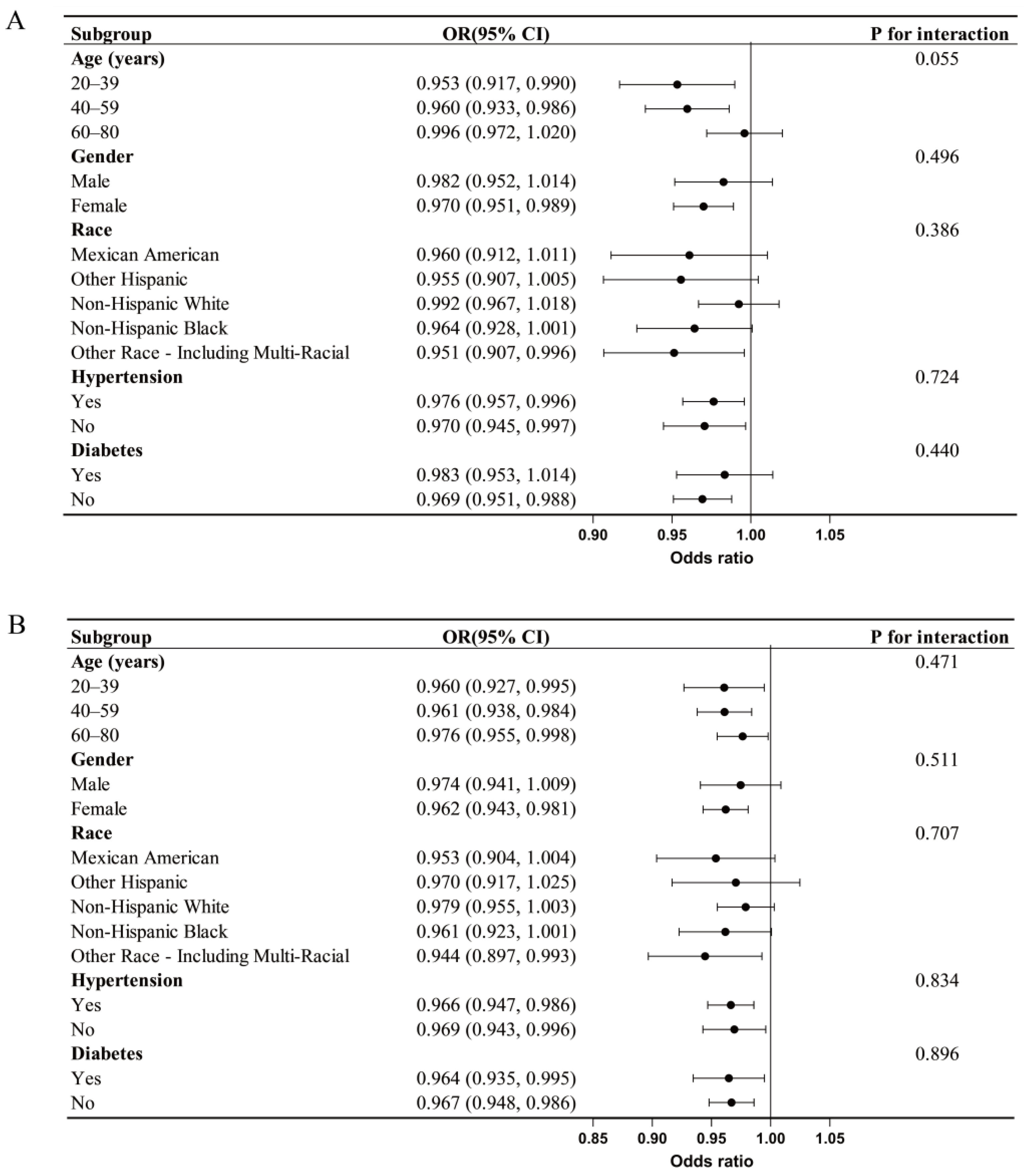
We performed subgroup analyses stratified by age, gender, race, hypertension, and diabetes to determine whether the association between OBS and gallstones, as well as gallbladder surgery, was consistent across subgroups. As shown in the
Figure 2, no significant differences in the associations between OBS and gallstones or gallbladder surgery were observed across the subgroups, suggesting that the negative correlation between OBS and the prevalence of gallstones and gallbladder surgery is consistent.
3.4. Smooth Curve Fitting and Threshold Effect Analysis
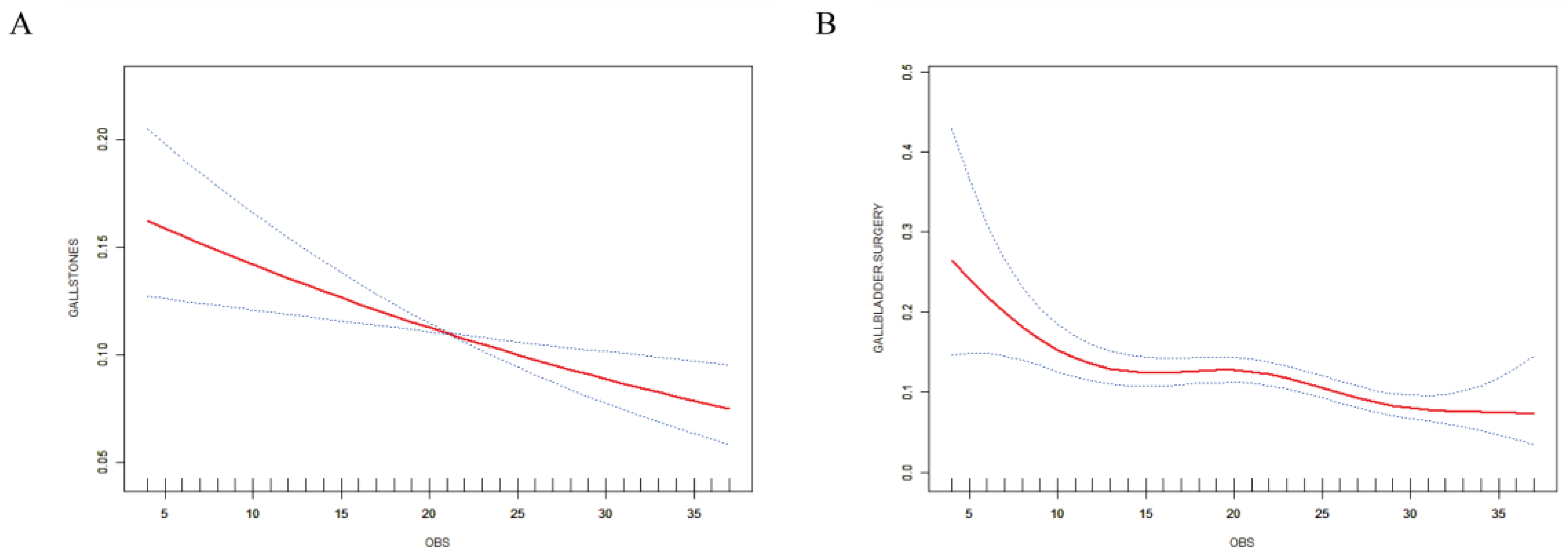
We used smoothed curve fitting to assess the dose-response relationship between OBS and gallstones as well as gallbladder surgery. As shown in
Figure 3, which illustrates that OBS exhibited a linear negative correlation with gallstone prevalence, while a significant nonlinear negative correlation was observed with gallbladder surgery. OBS significantly reduced the risk of gallbladder surgery when OBS values were below 9, and this relationship leveled off when OBS exceeded 9. (
Table 3).
4. Discussion
In this study involving 5335 adult participants from the NHANES database, we observed that OBS was significantly and negatively associated with the prevalence of gallstones and the incidence of gallbladder surgery. Subgroup analyses and interaction tests did not suggest that confounding factors influenced this association. Furthermore, curve-fitting analysis corroborated this negative association and suggested that the risk of gallbladder surgery can be minimized when OBS is raised to at least 9. This result emphasizes the importance of maintaining a robust antioxidant status for the prevention of gallstones and gallbladder surgery.
To the best of our knowledge, this is the first study to explore the association of OBS with the prevalence of gallstones and the incidence of gallbladder surgery. This study highlights the negative association between diet- and lifestyle-induced OBS levels and the prevalence of gallstones and gallbladder surgery, which aligns with previous findings on the relationship between oxidative stress and gallstones. Liu et al. [
13] demonstrated that oxidative stress affects the metabolism of cholesterol and bile acids in bile, and that this metabolic disorder promotes cholesterol crystallization, leading to gallstone formation. Pozo et al. [
14] suggested that oxidative stress may damage gallbladder smooth muscle cells through reactive oxygen species, thereby reducing gallbladder contractility and impairing gallbladder emptying, thereby increasing the risk of stone formation. Another animal study showed that inhibition of superoxide dismutase activity by a stone-promoting diet led to oxidative stress, which activated inflammatory mediators and induced gallbladder inflammation, with the inflammatory milieu further contributing to stone formation and progression [
15].
Evidence from previous studies supports the association between dietary components and gallstone formation. Worthington et al. [
16] analyzed 24 blood samples from gallstone patients and found that dietary antioxidants such as vitamin E, β-carotene, vitamin C, and folic acid were lower compared to controls. This finding was supported by Cikim et al. [
17], who found significantly lower levels of vitamin B12, zinc, and selenium in the sera of 40 female gallstone patients compared to 40 healthy women. However, no significant differences were found between the two groups for copper and folate, possibly due to sampling error. Naumann et al. [
18] found that a hydrophobic interaction may exist between bile acids and dietary fiber, which promotes colonic motility and accelerates the metabolism of stone-promoting bile acids such as deoxycholic acid and lithocholic acid. Different types of fats have differing effects on gallstone formation, with saturated fatty acids elevating cholesterol levels and promoting crystal formation, which can develop into gallstones. High-fat diets may also induce the accumulation of ectopic triacylglycerols, slowing gallbladder emptying and promoting stone formation. On the other hand, unsaturated fatty acids, particularly polyunsaturated omega-3 fatty acids, may reduce cholesterol saturation in bile and protect gallbladder mesenchymal stromal cells, thereby preventing gallstone formation. Interestingly, Tong et al. [
22] showed that calcium, iron, and copper were positively correlated with gallstone formation by promoting inflammatory factor release and increasing reactive oxygen species (ROS) levels, while magnesium and zinc exhibited antioxidant properties and were negatively correlated with gallstone formation. Another controlled study from China suggested that low calcium was positively associated with gallstone development. This discrepancy may be due to the complex mechanisms of metal ions in the body. Calcium plays an important role in cell signaling and regulates many intracellular processes, including apoptosis and oxidative stress. At normal physiological concentrations, calcium helps maintain cellular function and indirectly supports antioxidant defenses, but when calcium ion concentrations are too high, they may promote ROS production, exacerbating oxidative stress. The role of copper is more complex; it can act as a cofactor for antioxidants such as superoxide dismutase, by reducing oxygen radical production. However, copper can also react with hydrogen peroxide to produce hydroxyl radicals, triggering oxidative damage [
27].
In addition to dietary factors, lifestyle is also closely related to gallstones. Regular physical activity promotes normal gallbladder contraction and emptying, prevents cholestasis, and reduces cholesterol and bile pigment deposition. Results from a large European prospective study involving 25,639 participants showed that high levels of physical activity were associated with a reduced risk of symptomatic gallstones in participants older than 70 years. Another study from South Korea suggested that vigorous exercise at least two days per week may reduce the risk of gallstone formation [
28,
29]. Several papers have suggested that BMI is positively associated with the development of gallstones, and a study from the United States suggests that low body weight may be an etiologic factor for gallstones [
30,
31,
32]. Gebhard et al. [
33] suggest that a very low-calorie diet (520 kcal) may lead to gallstone formation due to poor gallbladder emptying and increased bile cholesterol saturation, highlighting the importance of sensible eating habits and healthy weight management in preventing gallstones. A recent large cohort study showed that cotinine is an independent risk factor for gallstones, and nicotine can regulate bile acid metabolism through the FXR-megalin/cubilin pathway, thereby promoting gallstone nucleation, indicating that smoking may be a key factor in gallstone development [
34,
35]. In contrast to smoking, alcohol consumption may act as a protective factor against gallstone disease. A meta-analysis by Wang et al. [
36] found that higher alcohol intake was associated with a significant reduction in the risk of gallstones, with a 12% reduction in risk for each additional 10 grams of alcohol consumed per day. Another cohort study demonstrated that regular alcohol consumption, especially 5-7 days per week, significantly reduced the risk of gallstones, whereas infrequent consumption (1-2 days per week) did not have a significant effect [
37]. A study by Kono et al. [
38] also found that alcohol consumption significantly reduced the incidence of gallstones and post-gallbladder surgery status. However, these results should be interpreted with caution, as sample variations between studies may influence the conclusions. Jayanthi et al. [
39] demonstrated that alcohol consumption significantly increased the relative risk of cirrhosis in South Indian vegetarian women with cirrhosis (RR = 7.03, 95% CI 3.26-15.12). Although moderate alcohol consumption may have a preventive effect on gallstones, the overall health effects of alcohol consumption need to be considered comprehensively.
This study has several strengths; we utilized all currently available data from consecutive NHANES cycles to the fullest extent to ensure the stability and reliability of the results. The study design carefully considered multiple potential confounders and included multivariate adjustments to enhance the scientific validity and credibility of the findings. Compared with earlier studies, our research covered more dietary and lifestyle factors related to oxidative homeostasis, allowing for a more comprehensive assessment of individual oxidative stress levels and providing a stronger scientific basis for the development of personalized health interventions.
There are some limitations to this study. As a cross-sectional study, it can only demonstrate that OBS is associated with gallstone incidence and gallbladder surgery rates, but it cannot establish a causal relationship. Although relevant covariates were included to the fullest extent, some confounding factors may not have been fully accounted for. Moreover, NHANES is based on a US population sample, and gallstone characteristics vary significantly across regions. Future large-scale, prospective studies are needed in multiple regions to further explore the correlation between OBS, gallstone incidence, and gallbladder surgery rates.
5. Conclusions
In summary, we found a negative correlation between OBS and gallstone incidence as well as gallbladder surgery rates, and this negative correlation becomes increasingly significant as OBS levels rise. There is a significant dose-response relationship between OBS and gallbladder surgery rates, and maintaining an OBS of at least 9 may significantly reduce the risk of gallbladder surgery. Additionally, conducting larger prospective studies will help explore the mechanisms between OBS, gallstones, and gallbladder surgery in greater depth, thus providing scientific support for the development of more effective preventive and therapeutic approaches.
Author Contributions
Shouxin Wei and Sijia Yu contributed equally to this work.Conceptualization, Shouxin Wei. and Sijia Yu.; methodology, Shouxin Wei.; software, Shouxin Wei.; validation, Yingdong Jia. and Zhengwen Xu.; formal analysis, Shouxin Wei.; resources,Sijia Yu .; data curation, Shouxin Wei.; writing—original draft preparation, Shouxin Wei.; writing—review and editing, Chuan Qian.; visualization, Shouxin Wei.; supervision, Sijia Yu.; project administration, Yindong Jia.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The NCHS Research Ethics Review Board (ERB) reviewed and approved NHANES study protocols, and all participants provided their written informed consent to participate in this study.
Informed Consent Statement
Not applicable.
Data Availability Statement
Acknowledgments
Our team sincerely appreciates all the staff and participants whose invaluable contributions have greatly enhanced the NHANES data collection.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sun, H.; Warren, J.; Yip, J.; Ji, Y.; Hao, S.; Han, W.; Ding, Y. Factors Influencing Gallstone Formation: A Review of the Literature. Biomolecules 2022, 12, 550. [Google Scholar] [CrossRef] [PubMed]
- Grigor'eva, I.N.; Romanova, T.I. Gallstone Disease and Microbiome. Microorganisms 2020, 8, 835. [Google Scholar] [CrossRef] [PubMed]
- Gutt, C.; Schläfer, S.; Lammert, F. The Treatment of Gallstone Disease. Dtsch. Arztebl. Int. 2020, 117, 148–158. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, L.; Shen, K.; Zhang, J.; Zhu, Y.; Qiao, Q.; Chen, L. Association between metabolically healthy overweight/obesity and gallstones in Chinese adults. Nutr. Metab. 2023, 20, 20. [Google Scholar] [CrossRef]
- Stokes, C.S.; Lammert, F. Excess Body Weight and Gallstone Disease. Visc. Med. 2021, 37, 254–260. [Google Scholar] [CrossRef]
- Hess, E.; Thumbadoo, R.P.; Thorne, E.; McNamee, K. Gallstones in pregnancy. Br. J. Hosp. Med. 2021, 82, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lammert, F.; Gurusamy, K.; Ko, C.W.; Miquel, J.F.; Méndez-Sánchez, N.; Portincasa, P.; et al. Gallstones. Nat. Rev. Dis. Primers 2016, 2, 16024. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Garruti, G.; Frühbeck, G.; De Angelis, M.; de Bari, O.; Wang, D.Q.; Lammert, F.; Portincasa, P. The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Curr. Med. Chem. 2019, 26, 3620–3638. [Google Scholar] [CrossRef]
- Ren, T.; Pang, L.; Dai, W.; Wu, S.; Kong, J. Regulatory mechanisms of the bile salt export pump (BSEP/ABCB11) and its role in related diseases. Clin. Res. Hepatol. Gastroenterol. 2021, 45, 101641. [Google Scholar] [CrossRef]
- Liu, Y.; Han, Y.; Gao, Y.; Yao, N.; Wang, Y.; Wang, F.; Dong, Y.; Wang, S.; Li, B. The association between oxidative balance score and frailty in adults across a wide age spectrum: NHANES 2007-2018. Food Funct. 2024, 15, 5041–5049. [Google Scholar] [CrossRef]
- Li, Y.; Liu, Y. Adherence to an antioxidant diet and lifestyle is associated with reduced risk of cardiovascular disease and mortality among adults with nonalcoholic fatty liver disease: evidence from NHANES 1999-2018. Front. Nutr. 2024, 11, 1361567. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.; Wen, H.; Xu, Z. Higher oxidative balance score is associated with lower kidney stone disease in US adults: a population-based cross-sectional study. World J. Urol. 2024, 42, 222. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.L.; Hekimi, S. The impact of mitochondrial oxidative stress on bile acid-like molecules in C. elegans provides a new perspective on human metabolic diseases. Worm 2013, 2, e21457. [Google Scholar] [CrossRef]
- Pozo, M.J.; Camello, P.J.; Mawe, G.M. Chemical mediators of gallbladder dysmotility. Curr. Med. Chem. 2004, 11, 1801–1812. [Google Scholar] [CrossRef]
- Chen, G.; Wu, S. Role of Baicalin and Liver X Receptor Alpha in the Formation of Cholesterol Gallstones in Mice. Gastroenterol. Res. Pract. 2020, 2020, 1343969. [Google Scholar] [CrossRef]
- Worthington, H.V.; Hunt, L.P.; McCloy, R.F.; Ubbink, J.B.; Braganza, J.M. Dietary antioxidant lack, impaired hepatic glutathione reserve, and cholesterol gallstones. Clin. Chim. Acta; Int. J. Clin. Chem. 2004, 349, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Cikim, G.; Hatipoglu, H.S.; Susam, S. Evaluation of homocysteine, vitamin, and trace element levels in women with gallstones. J. Trace Elem. Med. Biol. : Organ Soc. Miner. Trace Elem. (GMS) 2023, 78, 127177. [Google Scholar] [CrossRef] [PubMed]
- Naumann, S.; Schweiggert-Weisz, U.; Eglmeier, J.; Haller, D.; Eisner, P. In Vitro Interactions of Dietary Fibre Enriched Food Ingredients with Primary and Secondary Bile Acids. Nutrients 2019, 11, 1424. [Google Scholar] [CrossRef]
- Gu, Y.; Yin, J.J.O.M. Saturated fatty acids promote cholesterol biosynthesis: Effects and mechanisms. Obes. Med. 2020, 18, 100201. [Google Scholar] [CrossRef]
- Tharp, K.M.; Khalifeh-Soltani, A.; Park, H.M.; Yurek, D.A.; Falcon, A.; Wong, L.; Feng, R.; Atabai, K.; Stahl, A. Prevention of gallbladder hypomotility via FATP2 inhibition protects from lithogenic diet-induced cholelithiasis. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 310, G855–G864. [Google Scholar] [CrossRef]
- Pasternak, A.; Bugajska, J.; Szura, M.; Walocha, J.A.; Matyja, A.; Gajda, M.; Sztefko, K.; Gil, K. Biliary Polyunsaturated Fatty Acids and Telocytes in Gallstone Disease. Cell Transplant. 2017, 26, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Tong, K.; Jing, C.; Wang, T.; Liu, K.; Guo, W.; Zhang, Z. The roles of metal ions in gallstones formation. Asian J. Surg. 2024. [Google Scholar] [CrossRef]
- Lee, M.H.; Gao, Y.T.; Huang, Y.H.; McGee, E.E.; Lam, T.; Wang, B.; Shen, M.; Rashid, A.; Pfeiffer, R.M.; Hsing, A.W.; et al. A Metallomic Approach to Assess Associations of Serum Metal Levels With Gallstones and Gallbladder Cancer. Hepatology 2020, 71, 917–928. [Google Scholar] [CrossRef]
- Terrell, K.; Choi, S.; Choi, S. Calcium’s Role and Signaling in Aging Muscle, Cellular Senescence, and Mineral Interactions. 2023, 24, 17034. Int. J. Mol. Sci. 2023, 24, 17034. [Google Scholar] [CrossRef]
- Feno, S.; Butera, G.; Vecellio Reane, D.; Rizzuto, R.; Raffaello, A. Crosstalk between Calcium and ROS in Pathophysiological Conditions. Oxidative Med. Cell. Longev. 2019, 2019, 9324018. [Google Scholar] [CrossRef] [PubMed]
- Shim, D.; Han, J. Coordination chemistry of mitochondrial copper metalloenzymes: exploring implications for copper dyshomeostasis in cell death. BMB Rep. 2023, 56, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Vetlényi, E.; Rácz, G. The physiological function of copper, the etiological role of copper excess and deficiency. Orvosi Hetil. 2020, 161, 1488–1496. [Google Scholar] [CrossRef] [PubMed]
- Banim, P.J.; Luben, R.N.; Wareham, N.J.; Sharp, S.J.; Khaw, K.T.; Hart, A.R. Physical activity reduces the risk of symptomatic gallstones: a prospective cohort study. Eur. J. Gastroenterol. Hepatol. 2010, 22, 983–988. [Google Scholar] [CrossRef]
- Wang, H.; So, H.; Ko, S.W.; Jung, S.W.; Bang, S.J.; Park, E.J. Gallstone Is Associated with Metabolic Factors and Exercise in Korea. Healthcare 2022, 10, 1372. [Google Scholar] [CrossRef]
- Zhang, J.; Liang, D.; Xu, L.; Liu, Y.; Jiang, S.; Han, X.; Wu, H.; Jiang, Y. Associations between novel anthropometric indices and the prevalence of gallstones among 6,848 adults: a cross-sectional study. Front. Nutr. 2024, 11, 1428488. [Google Scholar] [CrossRef]
- Scherber, P.R.; Zúniga, S.E.; Glanemann, M.; Lammert, F. Gallstone disease - interdisciplinary treatment. Dtsch. Med. Wochenschr. (1946) 2020, 145, 287–295. [Google Scholar]
- Kata, P.; Kanukuntla, A.K.; Seeburun, S.; Pawa, A.; Burla, K.; Cheriyath, P. S3486 Should Hypoalimentation Cause Concern for Gallstones? Off. J. Am. Coll. Gastroenterol. 2021, 116, S1435. [Google Scholar] [CrossRef]
- Gebhard, R.L.; Prigge, W.F.; Ansel, H.J.; Schlasner, L.; Ketover, S.R.; Sande, D.; Holtmeier, K.; Peterson, F.J. The role of gallbladder emptying in gallstone formation during diet-induced rapid weight loss. Hepatology 1996, 24, 544–548. [Google Scholar] [PubMed]
- Kim, N.H.; Kang, J.H.; Kim, H.J. The Association Between Cotinine-Verified Smoking Status and Risk of Gallstones: A Cohort Study. J. Gastrointest. Liver Dis. JGLD 2024, 33, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Bi, P.; Mi, Q.; Guan, Y.; Jiang, J.; Li, X.; Yang, B. Effect of nicotine on cholesterol gallstone formation in C57BL/6J mice fed on a lithogenic diet. Exp. Ther. Med. 2023, 25, 84. [Google Scholar] [CrossRef]
- Wang, J.; Duan, X.; Li, B.; Jiang, X. Alcohol consumption and risk of gallstone disease: a meta-analysis. Eur. J. Gastroenterol. Hepatol. 2017, 29, e19–e28. [Google Scholar] [CrossRef]
- Leitzmann, M.F.; Giovannucci, E.L.; Stampfer, M.J.; Spiegelman, D.; Colditz, G.A.; Willett, W.C.; Rimm, E.B. Prospective study of alcohol consumption patterns in relation to symptomatic gallstone disease in men. Alcohol. Clin. Exp. Res. 1999, 23, 835–841. [Google Scholar] [CrossRef]
- Kono, S.; Eguchi, H.; Honjo, S.; Todoroki, I.; Oda, T.; Shinchi, K.; Ogawa, S.; Nakagawa, K. Cigarette smoking, alcohol use, and gallstone risk in Japanese men. Digestion 2002, 65, 177–183. [Google Scholar] [CrossRef]
- Jayanthi, V.; Malathi, S.; Ramathilakam, B.; Mathew, S.; Prasanthi, R.; Srinivasan, V. Is vegetarianism a precipitating factor for gallstones in cirrhotics? Trop. Gastroenterol. Off. J. Dig. Dis. Found. 1998, 19, 21–23. [Google Scholar]
Figure 1.
Flowchart of the study.
Figure 1.
Flowchart of the study.
Figure 2.
Stratified analysis of the association between OBS and gallstones and gallbladder surgery. This analysis considered factors such as Age, gender, race, education level, marital status, PIR, stroke, lung disease, heart disease, hypertension, diabetes, and liver function indicators (ALT, ALP, AST, GGT), as well as total energy intake. (A) Stratified analysis of the association between OBS and gallstones. (B) Stratified analysis of the association between OBS and gallbladder surgery..
Figure 2.
Stratified analysis of the association between OBS and gallstones and gallbladder surgery. This analysis considered factors such as Age, gender, race, education level, marital status, PIR, stroke, lung disease, heart disease, hypertension, diabetes, and liver function indicators (ALT, ALP, AST, GGT), as well as total energy intake. (A) Stratified analysis of the association between OBS and gallstones. (B) Stratified analysis of the association between OBS and gallbladder surgery..
Figure 3.
The dose-response relationship between OBS and gallstones and gallbladder surgery.Adjusted for Age, gender, race, education level, marital status, PIR, stroke, lung disease, heart disease, hypertension, diabetes, and liver function indicators (ALT, ALP, AST, GGT), as well as total energy intake. (A) OBS and gallstones. (B) OBS and gallbladder surgery.
Figure 3.
The dose-response relationship between OBS and gallstones and gallbladder surgery.Adjusted for Age, gender, race, education level, marital status, PIR, stroke, lung disease, heart disease, hypertension, diabetes, and liver function indicators (ALT, ALP, AST, GGT), as well as total energy intake. (A) OBS and gallstones. (B) OBS and gallbladder surgery.
Table 1.
Characteristics of the study cohort.
Table 1.
Characteristics of the study cohort.
| Characteristics |
Total (n = 5335) |
Q1 (n = 1189) |
Q2 (n = 1269) |
Q3 (n = 1408) |
Q4 (n = 1469) |
P-value |
| AGE(years) |
50.843 ± 17.122 |
51.511 ± 17.460 |
51.263 ± 17.254 |
50.678 ± 17.329 |
50.098 ± 16.505 |
0.091 |
| Sex, n (%) |
|
|
|
|
|
0.588 |
| Male |
2560 (47.985%) |
557 (46.846%) |
614 (48.385%) |
694 (49.290%) |
695 (47.311%) |
|
| Female |
2775 (52.015%) |
632 (53.154%) |
655 (51.615%) |
714 (50.710%) |
774 (52.689%) |
|
| RACE |
|
|
|
|
|
<0.001 |
| Mexican American |
603 (11.303%) |
84 (7.065%) |
132 (10.402%) |
171 (12.145%) |
216 (14.704%) |
|
| Other Hispanic |
511 (9.578%) |
109 (9.167%) |
122 (9.614%) |
123 (8.736%) |
157 (10.688%) |
|
| Non-Hispanic White |
2048 (38.388%) |
385 (32.380%) |
511 (40.268%) |
569 (40.412%) |
583 (39.687%) |
|
| Non-Hispanic Black |
1376 (25.792%) |
474 (39.865%) |
334 (26.320%) |
307 (21.804%) |
261 (17.767%) |
|
| Other Race - Including Multi-Racial |
797 (14.939%) |
137 (11.522%) |
170 (13.396%) |
238 (16.903%) |
252 (17.155%) |
|
| Education level, n (%) |
|
|
|
|
|
<0.001 |
| Below high school |
825 (15.464%) |
239 (20.101%) |
193 (15.209%) |
205 (14.560%) |
188 (12.798%) |
|
| High school |
1245 (23.336%) |
353 (29.689%) |
332 (26.162%) |
299 (21.236%) |
261 (17.767%) |
|
| Above high school |
3265 (61.200%) |
597 (50.210%) |
744 (58.629%) |
904 (64.205%) |
1020 (69.435%) |
|
| Marital status , n (%) |
|
|
|
|
|
<0.001 |
| Married or living with partner |
3143 (58.913%) |
586 (49.285%) |
735 (57.920%) |
878 (62.358%) |
944 (64.261%) |
|
| Divorced, separated, or widowed |
1204 (22.568%) |
327 (27.502%) |
305 (24.035%) |
286 (20.312%) |
286 (19.469%) |
|
| Never married |
988 (18.519%) |
276 (23.213%) |
229 (18.046%) |
244 (17.330%) |
239 (16.270%) |
|
| Family PIR, n (%) |
|
|
|
|
|
<0.001 |
| <1.3 |
1451 (27.198%) |
468 (39.361%) |
331 (26.084%) |
352 (25.000%) |
300 (20.422%) |
|
| 1.3-3.5 |
2076 (38.913%) |
451 (37.931%) |
537 (42.317%) |
547 (38.849%) |
541 (36.828%) |
|
| ≥3.5 |
1808 (33.889%) |
270 (22.708%) |
401 (31.600%) |
509 (36.151%) |
628 (42.750%) |
|
| Stroke,n (%) |
|
|
|
|
|
<0.001 |
| Yes |
270 (5.061%) |
94 (7.906%) |
68 (5.359%) |
50 (3.551%) |
58 (3.948%) |
|
| NO |
5065 (94.939%) |
1095 (92.094%) |
1201 (94.641%) |
1358 (96.449%) |
1411 (96.052%) |
|
| Pulmonary disease, n (%) |
|
|
|
|
|
<0.001 |
| Yes |
1149 (21.537%) |
327 (27.502%) |
289 (22.774%) |
274 (19.460%) |
259 (17.631%) |
|
| NO |
4186 (78.463%) |
862 (72.498%) |
980 (77.226%) |
1134 (80.540%) |
1210 (82.369%) |
|
| Heart disease, n (%) |
|
|
|
|
|
<0.001 |
| Yes |
499 (9.353%) |
148 (12.447%) |
126 (9.929%) |
119 (8.452%) |
106 (7.216%) |
|
| NO |
4836 (90.647%) |
1041 (87.553%) |
1143 (90.071%) |
1289 (91.548%) |
1363 (92.784%) |
|
| Hypertension, n (%) |
|
|
|
|
|
<0.001 |
| Yes |
3043 (57.038%) |
751 (63.162%) |
742 (58.471%) |
798 (56.676%) |
752 (51.191%) |
|
| NO |
2292 (42.962%) |
438 (36.838%) |
527 (41.529%) |
610 (43.324%) |
717 (48.809%) |
|
| Diabetes, n (%) |
|
|
|
|
|
<0.001 |
| Yes |
1042 (19.531%) |
279 (23.465%) |
268 (21.119%) |
256 (18.182%) |
239 (16.270%) |
|
| NO |
4293 (80.469%) |
910 (76.535%) |
1001 (78.881%) |
1152 (81.818%) |
1230 (83.730%) |
|
| ALT |
22.176 ± 16.879 |
21.672 ± 19.790 |
21.610 ± 17.056 |
22.597 ± 16.302 |
22.671 ± 14.538 |
<0.001 |
| ALP |
78.187 ± 26.892 |
81.170 ± 25.028 |
79.020 ± 27.764 |
77.738 ± 29.432 |
75.484 ± 24.684 |
<0.001 |
| AST |
21.848 ± 13.306 |
21.967 ± 17.995 |
21.222 ± 12.299 |
21.923 ± 12.692 |
22.219 ± 9.784 |
<0.001 |
| GGT |
31.871 ± 43.904 |
35.167 ± 49.391 |
32.426 ± 43.954 |
32.799 ± 51.793 |
27.834 ± 27.636 |
<0.001 |
| Energy intake |
2041.781 ± 839.343 |
1377.419 ± 482.150 |
1803.478 ± 558.697 |
2157.387 ± 671.740 |
2674.563 ± 921.675 |
<0.001 |
| Gallstones |
|
|
|
|
|
0.041 |
| Yes |
586 (10.984%) |
144 (12.111%) |
153 (12.057%) |
155 (11.009%) |
134 (9.122%) |
|
| NO |
4749 (89.016%) |
1045 (87.889%) |
1116 (87.943%) |
1253 (88.991%) |
1335 (90.878%) |
|
| Gallbladder surgery |
|
|
|
|
|
<0.001 |
| Yes |
603 (11.303%) |
156 (13.120%) |
159 (12.530%) |
166 (11.790%) |
122 (8.305%) |
|
| NO |
4732 (88.697%) |
1033 (86.880%) |
1110 (87.470%) |
1242 (88.210%) |
1347 (91.695%) |
|
Table 2.
Association between OBS and gallstones and gallbladder surgery .
Table 2.
Association between OBS and gallstones and gallbladder surgery .
| Characteristics |
Model 1 |
Model 2 |
Model 3 |
| Gallstones |
|
|
|
| OBS continuous |
0.986 (0.974, 0.997) * |
0.981 (0.969, 0.993) ** |
0.974 (0.958, 0.990) ** |
| OBS quartiles |
|
|
|
| Quartile 1 |
1[Reference] |
1[Reference] |
1[Reference] |
| Quartile 2 |
0.995 (0.781, 1.268) |
0.946 (0.736, 1.217) |
0.901 (0.691, 1.174) |
| Quartile 3 |
0.898 (0.705, 1.143) |
0.851 (0.662, 1.094) |
0.784 (0.590, 1.041) |
| Quartile 4 |
0.728 (0.568, 0.934) * |
0.670 (0.517, 0.868) ** |
0.567 (0.406, 0.793) *** |
| P for trend |
0.008 |
0.001 |
<0.001 |
| Gallbladder surgery |
|
|
|
| OBS continuous |
0.978 (0.967, 0.990) *** |
0.970 (0.958, 0.982) *** |
0.967 (0.950, 0.983) *** |
| OBS quartiles |
|
|
|
| Quartile 1 |
1[Reference] |
1[Reference] |
1[Reference] |
| Quartile 2 |
0.949 (0.749, 1.202) |
0.867 (0.676, 1.113) |
0.841 (0.646, 1.096) |
| Quartile 3 |
0.885 (0.701, 1.118) |
0.800 (0.624, 1.024) |
0.773 (0.583, 1.026) |
| Quartile 4 |
0.600 (0.467, 0.770) *** |
0.516 (0.397, 0.672) *** |
0.465 (0.330, 0.655) *** |
| P for trend |
<0.001 |
<0.001 |
<0.001 |
Table 3.
Analysis of threshold effects between OBS and gallbladder surgery.
Table 3.
Analysis of threshold effects between OBS and gallbladder surgery.
| Characteristics |
OR (95% CI) |
| Fitting by standard linear model |
0.967 (0.950, 0.983) |
| Fitting by two-piecewise linear model |
|
| Inflection point |
9 |
| < 9 |
0.769 (0.617, 0.957) |
| > 9 |
0.971 (0.954, 0.988) |
| Log likelihood ratio |
0.047 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).