1. Introduction
Obstructive sleep apnea (OSA) is a prevalent condition affecting between 2% and 34% of adults. It is linked to cardiovascular disorders, cognitive dysfunction, strokes, and increased mortality rates [
1,
2,
3,
4]. The current standard therapy for moderate to severe OSA patients involves continuous positive airway pressure (CPAP) [
5,
6]. Depending on the severity and unique features of the condition, alternative therapeutic options are available. These encompass lifestyle modifications, dietary adjustments, positional therapy, oral appliances, and surgical interventions, which can also be combined for a more comprehensive approach [
7,
8]. Transoral robotic surgery (TORS) has emerged as a minimally invasive surgical approach with promising outcomes. This approach is utilized for patients experiencing obstruction of the airway due to hypertrophy of the lingual tonsils. In such cases, the base of the tongue is reduced, resulting in a broader airway, and reducing the likelihood of collapse [
9].
Post-surgical patients, under general anesthesia and ventilation via an endotracheal tube, necessitate careful management during the awakening and extubation process, typically in an intensive care setting. Extubation is an elective procedure requiring meticulous evaluation and planning, particularly when difficult airway management is anticipated. Complications associated with extubation can lead to increased morbidity and mortality [
10,
11].
Literature highlights common complications following TORS, including tongue edema, tongue and pharyngeal paresthesia, minor and major hemorrhage, dysgeusia, dysphagia with an increased risk of aspiration, and pain. Various devices are suggested to enhance the safety of difficult extubation [
9]. The airway exchange catheter (AEC) for example proves useful for potential reintubation scenarios, where it serves as a guide for tube reinsertion [
12]. Additionally, a high-flow nasal cannula (HFNC) oxygen delivery approach improves ventilation post-extubation, reducing respiratory insufficiency. HFNC application diminishes nasopharyngeal dead space, increases alveolar oxygen fraction, lessens respiratory muscle fatigue, improves secretion management, and decreases upper airway obstruction incidents [
13,
14] These two devices are complementary but non equal in managing difficult airways. While the AEC is a useful guide for reintubation in difficult airway, it does not contribute to oxygenation and ventilation unlike HFNC
Despite the existing literature, there is a notable absence of protocols addressing extubation techniques in the Intensive Care Unit (ICU) following TORS. This retrospective analysis aims to assess the efficacy of different protocols, shedding light on their impact on patient outcomes and complications in this specific clinical context.
2. Materials and Methods
2.1. Study Design and Settings
This study was a single-center retrospective study conducted at hospital “Casa Sollievo della Sofferenza” (San Giovanni Rotondo, Foggia, Italy) from March 2015 and December 2021. The study was approved by the local Ethics Committee (N23/CE). This study adhered to ethical standards as outlined in the Declaration of Helsinki and followed the guidelines set by the Strengthening the Reporting of Observational Studies in Epidemiology checklist. All patients signed informed consent during preoperative assessment.
2.2. Study Participants
Patients scheduled for TORS underwent a comprehensive preoperative assessment, which included polysomnography to evaluate their sleep patterns and respiratory function. The surgical procedures were conducted under a remifentanil propofol-based target-controlled infusion (TCI) general anesthesia monitoring the depth of anesthesia. Curarization was administered only at induction, if necessary, as an alternative to laryngotracheal anesthesia with topical lidocaine (LTA) Following the completion of the surgical intervention, patients were transferred to the ICU for postoperative monitoring and management. The decision to awaken and extubate the patients was made only after a thorough multidisciplinary clinical evaluation, which involved collaboration between anesthesiologists and otolaryngologists. This joint assessment aimed to ensure the patient's readiness for extubation and to mitigate any potential risks or complications associated with the procedure. Patients with incomplete data were excluded from the analysis to maintain the integrity and reliability of the study findings.
2.3. Variables
We collected demographics, preoperative use of CPAP, lowest oxygen saturation (SpO2) at preoperative polysomnography, American Society of Anesthesiologists (ASA) physical status, comorbidities, main diagnosis, and Apnea-Hypopnea Index (AHI). The latter is a measure used in sleep medicine to assess the severity of sleep-disordered breathing, particularly in conditions such as OSA. This index quantifies the frequency and severity of apnea (complete cessation of breathing that lasts for at least 10 seconds) and hypopnea (partial reduction in breathing typically defined as a decrease in airflow of at least 30% accompanied by a reduction in blood oxygen saturation or an arousal from sleep) episodes during sleep. To calculate the AHI, the total number of apneas and hypopneas that occur per hour of sleep is determined. This number is then divided by the total number of hours of sleep to obtain the AHI value. The AHI is considered normal when it is less than 5 events per hour; mild sleep apnea is classified when the score falls within the range of 5 to 15 events per hour, moderate from 15 to 30 events per hour, and severe if it exceeds 30 events per hour. A higher AHI indicates a greater severity of sleep-disordered breathing and may be associated with increased health risks, including cardiovascular problems, daytime sleepiness, and impaired cognitive function [
15].
Regarding the procedure and postoperative management, we considered the type of surgical TORS, operative times, extubation times, hospital and ICU length of stay, the weaning time from HFNC, number of episodes of desaturation (SpO2 < 95% and SpO2 < 92%; continuous desaturation was defined as a period during which blood oxygen saturation levels remain consistently below the specific threshold for at least 5 minutes) in the first 24 hours after extubation, the use of AEC, as well as hemorrhagic and cardiovascular adverse effects in the first 48 hours.
2.4. Outcomes
The main expected outcome of the study was to assess whether the application of a different extubation approach was associated with the absence of major complications and a reduction in the time required to remove the endotracheal tube, expressed in hours. Major complications may include events such as infections, lung or organ damage, bleeding, or other complications requiring additional treatment or prolonged hospital stay.
In addition to the primary outcome, the secondary objective was to assess the duration of stay in the ICU, measured in days, and the number of desaturation episodes, i.e., the reduction in blood oxygen levels below 95%, occurring within the first 24 hours after extubation. These episodes may indicate complications or less effective recovery after tube removal and thus can serve as a measure of the safety and efficacy of the extubation protocol.
2.5. Statistics
The demographic and clinical characteristics of patients at baseline were reported as mean and standard deviation or as median and range for continuous variables, and as frequency and percentage for categorical variables. Comparisons between groups were conducted using the non-parametric Mann-Whitney test for continuous variables and the exact Fisher test for categorical variables. All analyses were performed using the statistical environment R. A p-value <0.05 was considered statistically significant. The balance analysis between the groups (conventional therapy and HFNC) was performed using propensity score (PS) matching with the key variables age, gender, BMI, ASA, AHI, SpO2, CPAP, and duration of intervention in minutes. The missing data was imputed using Random Forest.
3. Results
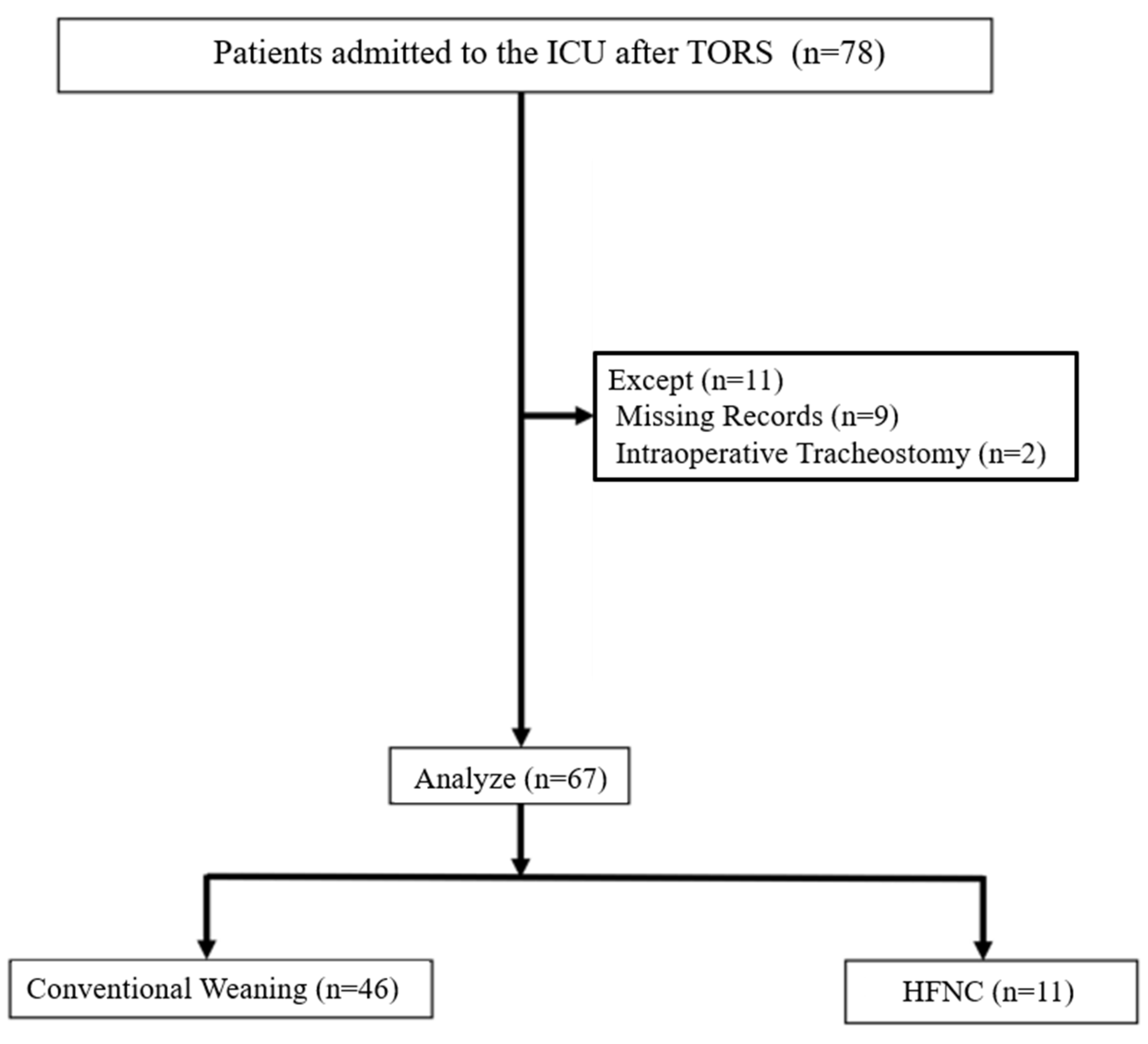
A total of 78 patients were initially considered for the analysis. However, 11 cases were excluded due to incomplete data (n=9) or intraoperative tracheostomy (n=2), resulting in a final sample size of 67 patients included in the analysis. In this sample, 46 patients were included in the conventional weaning group and 21 patients in the HFNC group (
Figure 1). Both medical devices were used in 18 of 21 patients extubated with HFNC. Five patients were extubated only with AEC and they were included in the conventional extubation group. The small sample did not allow analyzing the outcome separately for two groups.
Among the included cases, 54 patients (80.6%) were male. The mean age of the included patients was 28.3 years (SD=3.42), with a median age of 28 years. Demographic and preoperative clinical data are reported in
Table 1.
Data collected on the perioperative course are reported in
Table 2.
Conventional vs HFNC Management
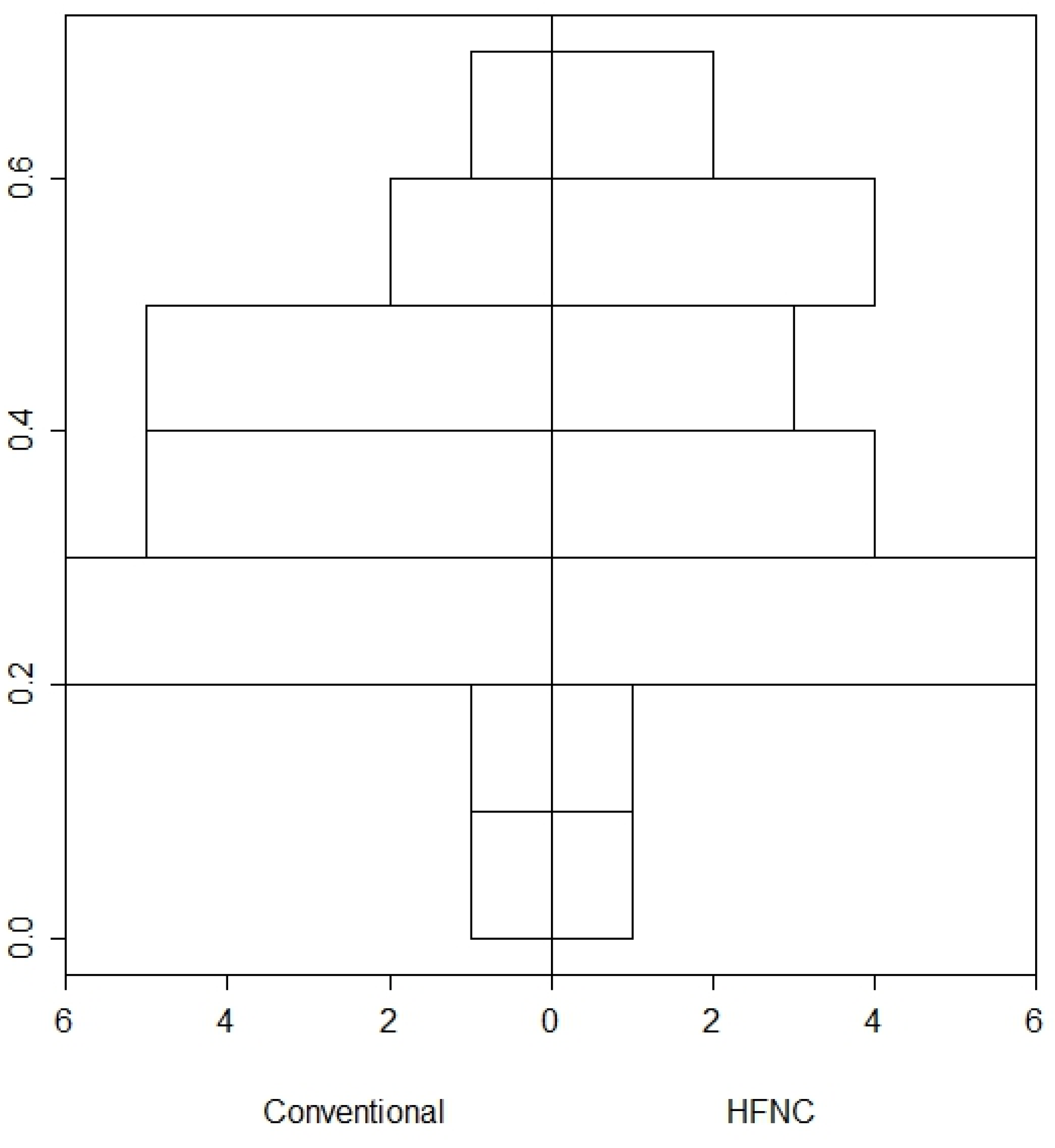
Given the considered variable, a patient-patient matching (n=21) in the conventional and HFNC groups was performed. The analyses of the PS matching achieved its goal of balancing the two groups. Results from the PS after matching are shown in
Figure 2.
In the comparative analysis, involving 46 patients in the Conventional group and 21 patients in the HFNC group, several noteworthy findings emerged. Notably, there was a good homogeneity between groups. There was no statistically significant difference in age (Conventional: 55.3±11.78 years, HFNC: 52.95±11.26 years, p=0.445). Gender distribution was similar in both groups, with approximately 80% male participants in each. Body Mass Index (BMI) also showed no significant difference between groups (Conventional: 28.61±3.59, HFNC: 27.53±2.97, p=0.236). Concerning preoperative characteristics, both groups exhibited comparable AHI scores (Conventional: 25.66±8.76, HFNC: 26.99±10.87, p=0.603). Moreover, preoperative oxygen saturation levels (SPO2) and usage of CPAP were similar across both groups. Furthermore, there were no significant differences in the types of surgeries performed between the groups and although the duration of surgery was slightly longer in the HFNC group, the difference was not statistically significant (p=0.177). (
Table 3).
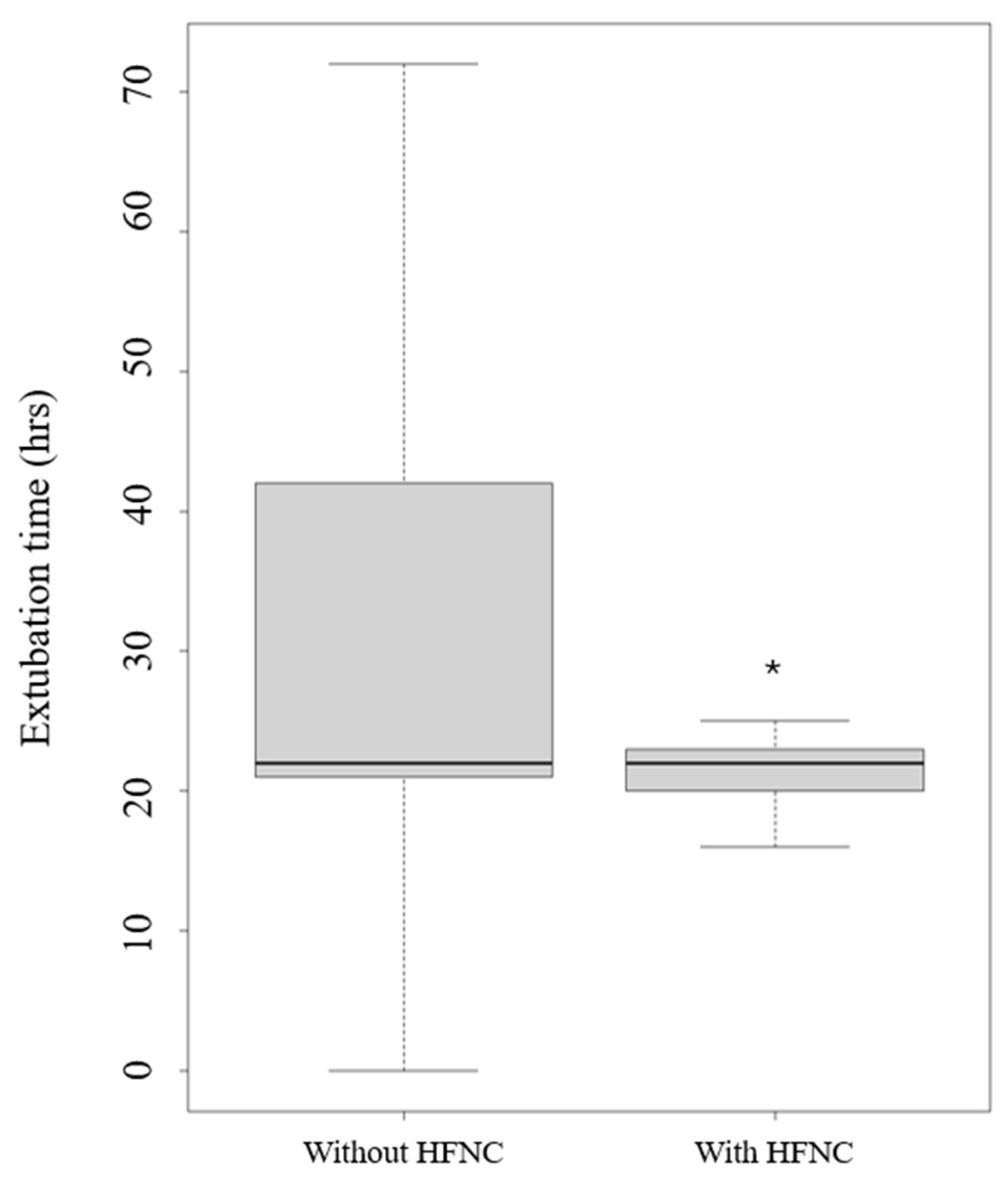
The only application of HFNC use versus conventional oxygen therapy led to a statistical reduction of extubation time (p= 0.024) (
Figure 3).
Moreover, the length of stay in ICU and the episodes of desaturation below 95% were reduced, but data are non-statically significant.
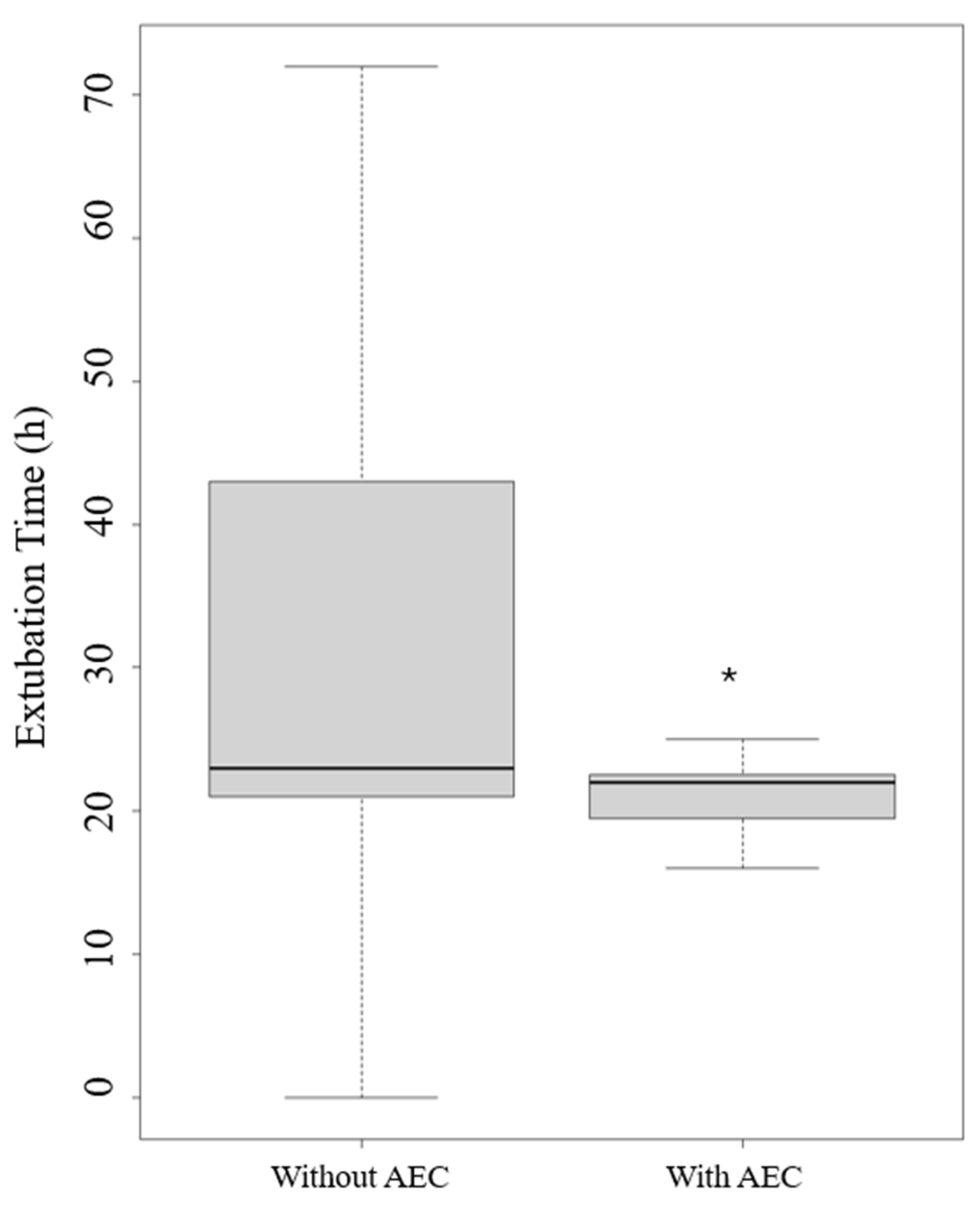
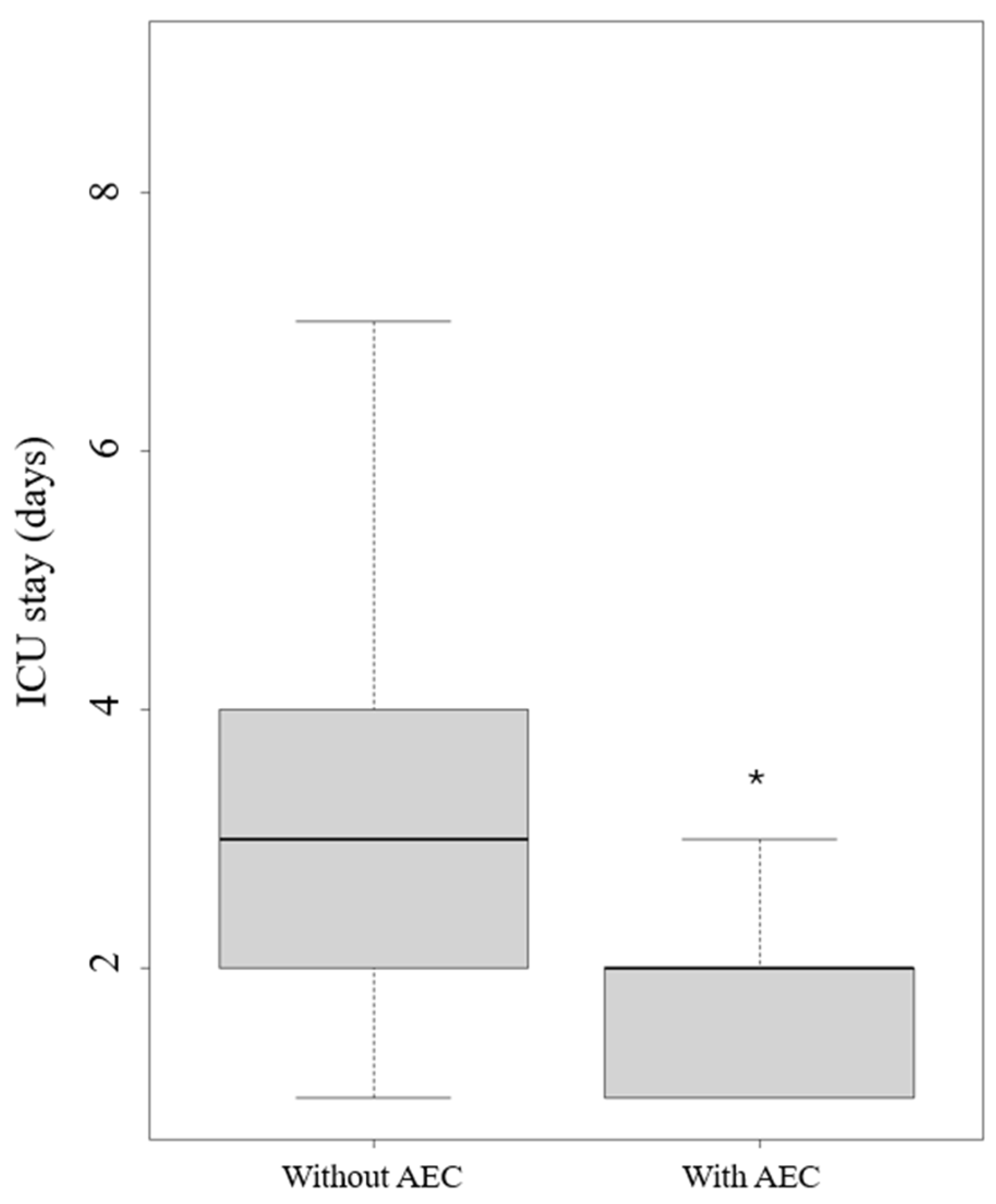
The application of an AEC led to a reduction of extubation time in hours (p= 0.008) (
Figure 4) and length of stay in the ICU (p=0.024) (
Figure 5).
Regarding significant complications, two patients (0.33%) experienced fatal outcomes in the ICU attributable to hemorrhagic and arrhythmic complications, respectively. Both patients were managed with conventional oxygen therapy after the extubation. No hemorrhagic or cardiovascular adverse effects were collected when a protocol of extubation was applied (HFNC or AEC).
4. Discussion
The present study aimed to evaluate the efficacy and safety of extubation protocols following TORS for OSA in patients admitted to the ICU for postoperative care. Our findings suggest that the utilization of HFNC, with or without an AEC, resulted in a significant reduction in extubation time without major adverse events. Additionally, HFNC application may decrease episodes of desaturation during extubation. These results underscore the potential benefits of incorporating HFNC and AEC into extubation protocols in this patient population.
In TORS procedures, the anesthetic approach is typically aimed at minimizing anesthesia recovery duration, reducing postoperative sedation, alleviating severe pain, and mitigating nausea/vomiting [
16]. Nevertheless, due to manipulation of the airway and the potential for lengthy surgery, there is a risk of airway edema, bleeding, and blood clots, which could lead to airway complications and aspiration. The ease of securing the airway, the extent of surgical resection, and the patient's underlying health conditions, such as the severity of obstructive sleep apnea, will determine the level of postoperative monitoring required. Patients who are difficult to intubate, undergo extensive tongue resection, or have high AHI scores may benefit from continued intubation and management in the ICU [
17]. Extubation should only occur after full reversal of anesthesia effects, muscle relaxation, control of surgical bleeding, and resolution of swelling. At our center, we routinely reverse and extubate patients in the ICU for optimal postoperative care.
The reduction in extubation time observed with HFNC and AEC utilization aligns with previous studies demonstrating the efficacy of these interventions in improving respiratory outcomes post-extubation. For example, in chronic obstructive pulmonary disease, HFNC therapy has been shown to enhance ventilation, reduce respiratory muscle fatigue, and improve secretion management, thus facilitating the transition from mechanical ventilation to spontaneous breathing [
18]. Similarly, the use of an AEC may aid in the smooth removal of the endotracheal tube, particularly in cases where difficult airway management is anticipated [
19]. These findings support the notion that combining these interventions can optimize extubation processes and minimize associated complications.
Furthermore, our study highlights the potential role of HFNC in reducing desaturation episodes during extubation. Desaturation, characterized by a decrease in blood oxygen levels, is a common complication following extubation and can lead to respiratory insufficiency and other adverse outcomes [
20]. The ability of HFNC to maintain optimal oxygenation and reduce nasopharyngeal dead space may contribute to the observed reduction in desaturation episodes. However, the non-statistically significant findings regarding desaturation episodes underscore the need for further research to elucidate the precise impact of HFNC on respiratory outcomes in this context.
In our analysis, we calculated that two patients (0.33%) experienced fatal outcomes in the ICU due to hemorrhagic and arrhythmic complications, respectively. However, despite finding that both patients received conventional oxygen therapy after extubation, it is not possible to draw definitive conclusions regarding the link between complications and the weaning technique. There are multiple confounding variables at play, and a large dataset with multivariate analysis would be necessary to elucidate this further. Nonetheless, this surgery is associated with complications, as reported by evidence-based medicine studies. For instance, major hemorrhagic complications can occur in almost 0.9% of procedures [
21]. According to the results of the data analysis, in our centre, the implemented extubation protocol provides HFNC oxygen administration with an AEC in situ. A multidisciplinary clinical evaluation between surgeons and intensivists is performed for addressing stability of vital parameters, presence of airway protective reflexes, and absence of edema or bleeding at the surgical site,
Study Limitations
It is worth noting that our study has several limitations. Firstly, its retrospective nature introduces inherent biases and limitations in data collection. Secondly, the small sample size and single-center design may limit the generalizability of our findings the limited sample size can play a role for small effect sizes. For example, the variable SPO2<95 continuous has a mean equal to 1.00 (SD: 1.62) in the Conventional group and 0.52 (1.57) in the HFNC group, therefore the ex-post power to detect this difference is only 0.20. Additionally, the lack of a standardized extubation protocol and variations in patient management may have influenced the outcomes assessed. Finally, an important source of bias arises from the non-exclusive utilization of the AEC within a single group. However, the two groups significantly differ in terms of device usage (<0.001;
Table 3). Additionally, six patients (8.9%) underwent extubation using both an AEC and conventional oxygen therapy, while three patients (4.4%) were exclusively extubated using HFNC oxygen therapy. Future prospective studies with larger sample sizes and standardized protocols are warranted to validate our findings and further elucidate the optimal approach to extubation in this patient population.
Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
5. Conclusions
In patients affected by OSA and admitted to the ICU after TORS, the application of HFNC with or without an AEC can lead to a significant reduction of extubation time without major adverse events improving the safety of difficult extubation protocols. According to the results of this pilot study, the use of HFNC could reduce desaturation episodes during extubation after TORS. Therefore, oxygen therapy through HFNC combined with AEC seems to be a safety and efficacy strategy for extubation protocols. Nevertheless, further high-quality research is warranted to confirm these results.
Author Contributions
AR: Marco Cascella, ADG conceptualization, methodology, writing, review and editing, and final approval. AM VM AD visualization, review editing, and final approval. AB, GM data curation, methodology and investigation; AI bibliographical review; MC statistical analysis; EGB supervision and final approval. All authors reviewed the manuscript and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Acknowledgment of the ethic committee of the Casa Sollievo Della Sofferenza Foundation Prot N 23/CE (2/82023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Melani, A.S.; Croce, S.; Messina, M.; Bargagli, E. Untreated Obstructive Sleep Apnea in Interstitial Lung Disease and Impact on Interstitial Lung Disease Outcomes. Sleep Med Clin. 2024, 19, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Lui, K.K.; Dave, A.; Sprecher, K.E.; Chappel-Farley, M.G.; Riedner, B.A.; Heston, M.B.; Taylor, C.E.; Carlsson, C.M.; Okonkwo, O.C.; Asthana, S.; Johnson, S.C.; Bendlin, B.B.; Mander, B.A.; Benca, R.M. Older adults at greater risk for Alzheimer's disease show stronger associations between sleep apnea severity in REM sleep and verbal memory. Alzheimers Res Ther. 2024, 16, 102. [Google Scholar] [CrossRef] [PubMed]
- Resende Martinez, A.B.; Barbosa, G.R.; Lopes, M.R.; Barbosa, R.H.A. Sleep apnea and sudden death in the non-cardiac population: A systematic review. Rev Port Cardiol. 2024, 43, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Prechaporn, W.; Hantrakul, P.; Ngamjarus, C.; Sukeepaisarnjaroen, W.; Sawanyawisuth, K.; Khamsai, S. Pooled prevalences of obstructive sleep apnea and heart failure: a systematic review and meta-analysis. Heart Fail Rev. 2024 May 9. [CrossRef]
- Stevens, D.; Title, M.; Spurr, K.; Morrison, D. Positive airway pressure therapy adherence and outcomes in obstructive sleep apnea: An exploratory longitudinal retrospective randomized chart review. Can J Respir Ther. 2024, 60, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Ogbu, I.; Hakobyan, B.; Sossou, C.; Levisman, J.; Obiagwu, C.; Danielian, A. Snoring Survivors: the impact of obstructive sleep apnoea and continuous positive airway pressure use on in-hospital mortality, length of stay and costs among patients hospitalised with acute cardiovascular disease - A retrospective analysis of 2016-2019 National Inpatient Sample Data. BMJ Open. 2024, 14, e073991. [Google Scholar] [CrossRef] [PubMed]
- Cavaliere, M.; De Luca, P.; De Santis, C.; Scarpa, A.; Ralli, M.; Di Stadio, A.; Viola, P.; Chiarella, G.; Cassandro, C.; Cassandro, F. Drug-Induced Sleep Endoscopy (DISE) with Simulation Bite to Predict the Success of Oral Appliance Therapy in Treating Obstructive Sleep Apnea/Hypopnea Syndrome (OSAHS). Transl Med UniSa. 2020, 23, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Kaffenberger, T.M.; Plawecki, A.; Kaki, P.; Boon, M.; Huntley, C. Troubleshooting Upper Airway Stimulation Therapy Using Drug-Induced Sleep Endoscopy. Otolaryngol Head Neck Surg. 2024. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Fakhry, N.; Saussez, S.; Badr, I.; Ayad, T.; Chekkoury-Idrissi, Y.; Melkane, A.E.; Bahgat, A.; Crevier-Buchman, L.; Blumen, M.; Cammaroto, G.; Vicini, C.; Hans, S. Surgical, clinical, and functional outcomes of transoral robotic surgery used in sleep surgery for obstructive sleep apnea syndrome: A systematic review and meta-analysis. Head Neck. 2021, 43, 2216–2239. [Google Scholar] [CrossRef] [PubMed]
- Parotto, M.; Cooper, R.M.; Behringer, E.C. Extubation of the Challenging or Difficult Airway. Curr Anesthesiol Rep. 2020, 10, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Russotto V, Lascarrou JB, Tassistro E, Parotto M, Antolini L, Bauer P, Szułdrzyński K, Camporota L, Putensen C, Pelosi P, Sorbello M, Higgs A, Greif R, Grasselli G, Valsecchi MG, Fumagalli R, Foti G, Caironi P, Bellani G, Laffey JG, Myatra SN; INTUBE Study Investigators. Efficacy and adverse events profile of videolaryngoscopy in critically ill patients: subanalysis of the INTUBE study. Br J Anaesth. 2023, 131, 607–616. [CrossRef]
- Vaithialingam, B.; Arun, B.G. High-flow Tracheal Oxygenation with Airway Exchange Catheter: A Novel Approach. Indian J Crit Care Med. 2023, 27, 456. [Google Scholar] [CrossRef] [PubMed]
- Rochwerg, B.; Einav, S.; Chaudhuri, D.; Mancebo, J.; Mauri, T.; Helviz, Y.; Goligher, E.C.; Jaber, S.; Ricard, J.D.; Rittayamai, N.; Roca, O.; Antonelli, M.; Maggiore, S.M.; Demoule, A.; Hodgson, C.L.; Mercat, A.; Wilcox, M.E.; Granton, D.; Wang, D.; Azoulay, E.; Ouanes-Besbes, L.; Cinnella, G.; Rauseo, M.; Carvalho, C.; Dessap-Mekontso, A.; Fraser, J.; Frat, J.P.; Gomersall, C.; Grasselli, G.; Hernandez, G.; Jog, S.; Pesenti, A.; Riviello, E.D.; Slutsky, A.S.; Stapleton, R.D.; Talmor, D.; Thille, A.W.; Brochard, L.; Burns, K.E.A. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 2020, 46, 2226–2237. [Google Scholar] [CrossRef] [PubMed]
- Du, F.; Gu, Y.H.; He, Y.C.; Deng, W.F.; Liu, Z.Z. High-flow nasal cannula therapy for pediatric obstructive sleep apnea: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2022, 26, 4583–4591. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Chi JJ, Mandel JE, Weinstein GS, O'Malley BW Jr. Anesthetic considerations for transoral robotic surgery. Anesthesiol Clin. 2010, 28, 411–422. [CrossRef]
- Chi JJ, Mandel JE, Weinstein GS, O’Malley BW Jr. Anesthetic considerations for transoral robotic surgery. Anesthesiol Clin 2010, 28, 411–422.
- Tan, D.; Walline, J.H.; Ling, B.; Xu, Y.; Sun, J.; Wang, B.; Shan, X.; Wang, Y.; Cao, P.; Zhu, Q.; Geng, P.; Xu, J. High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care. 2020, 24, 489. [Google Scholar] [CrossRef] [PubMed]
- Thakore, S.; Kundra, P.; Garg, R. A descriptive survey of tracheal extubation practices among Indian anaesthesiologists. Indian J Anaesth. 2021, 65, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Seet, E.; Waseem, R.; Chan, M.T.V.; Wang, C.Y.; Liao, V.; Suen, C.; Chung, F. Characteristics of Patients with Unrecognized Sleep Apnea Requiring Postoperative Oxygen Therapy. J Pers Med. 2022, 12, 1543. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Henriquez, C.; Boronat-Catala, B.; Rivero-Fernández, I.; Cammaroto, G.; Ibrahim, B.; Lechien, J.R.; Martínez-Capoccioni, G.; Carrasco-Llatas, M.; Capasso, R.; Martin-Martin, C. Safety of tongue base procedures for sleep apnoea in adults: A systematic review and metanalysis from the YO-IFOS study group. Acta Otorrinolaringol Esp (Engl Ed). 2022, 73, 384–393. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).