* Coresspondence: todt@gmx.net; Tel.: +49-521-581-3313; Fax: +49-521-581-3303
1. Introduction
Sudden sensorineural hearing loss (SSNHL) is characterized by an acute, mostly unilateral occurring inner ear dysfunction. It is defined as a hearing function decline of at least 30 dB in 3 sequential frequencies [
1]. Frequently but not universally accompanied symptoms can be vertigo, tinnitus, and ear fullness with individual patterns of occurrence [
2].
The incidence of SSNHL is estimated to range from 5 to 400/100000, depending on the sensitivity of observation. Pathophysiological mechanisms include vascular disorders, viral and bacterial infections, rheological dysfunction, neoplasms, and autoimmune diseases, among other etiologies, such as pressure changes of the endolymphatic and perilymphatic systems of the inner ear [
3].
Mostly regarded as idiopathic, SSNHL etiology and pathogenesis remain unclear to date. The treatment of SSNHL remains controversial and highly discussed. According to clinical practice guidelines, treatment options for SSNHL vary, and a „universal“ standard procedure has not yet been established [
4]. Application of systemic and/or intratympanic corticosteroids in various dosages as first-line therapy of SSNHL is a common standard occasionally in combination with histamines and vasodilators, although it is still a matter of debate to what degree these therapy concepts outrun spontaneous recovery [
19].
Although the etiology of SSNHL is mostly considered idiopathic, membrane ruptures of the round and/or oval window with consecutive perilymphatic fistula (PLF) are described as a cause of sudden hearing loss, tinnitus, and vertigo. Membrane ruptures might occur after head trauma due to pressure alterations, iatrogenic procedures, or anatomical malformations. Spontaneous membrane rupture is also described [
5,
6].
The consideration of PLF as a possible cause of SSNHL has been known for decades. Surgical sealing of the round and/or oval window membrane via exploratory tympanotomy as a diagnostic and therapeutic tool has been applied and established since the 1970s but still remains highly discussed [
20,
21,
22]. To date, there is no consensus on performing exploratory tympanotomy and window membrane sealing, although PLF has reached importance in etiology in the case of SSNHL [
7].
So far, no consensus exists on diagnostic criteria for PLF. Intraoperatively diagnostic of PLF whilst performing exploratory tympanotomy can be difficult. Leakage of perilymph from the round or oval window might not be visible when tympanotomy is performed. False fibrous membranes of the round window can make the intraoperative visual interpretation hence PLF difficult to diagnose. Visible fluid might be challenging when distinguishing PLF from intraoperative local fluid injection, such as local anesthesia [
8]. Intraoperative tests such as pressure transmission tests and fistula tests lack of evidence. Reliable noninvasive tests have not yet been established. Objective diagnostic tests with beta-trace protein or fluorescein staining have been described but lack of specificity and are technically ambitious to perform [
9,
10,
11].
Ikezono et al. identified the inner ear-specific cochlin-tomoprotein (CTP), which is specific and sensitive for perilymph. This protein can be used to objectively assess potential PLF using a monoclonal antibody test [
12].
Recent findings show evidence of a 22%/ 47% PLF rate based on the CTP detection test in cases of SSNHL [
13,
14]. Based on this high rate of PLF, SSNHL treatment concepts need to be re-evaluated.
This study aimed to detect CTP in SSNHL patients and compare pre-surgical and post-surgical pure tone hearing thresholds after round and oval window sealing as first-line treatment.
2. Material and Methods
2.1. Sample Collection and Evaluation of CTP Concentration
We collected CTP samples by performing middle ear cavity lavage with 0.3 mL of saline and absorption of the fluid, which is defined as middle ear lavage (MEL). The MEL was centrifuged (6000 rpm for 15 s; Eppendorf Systems, Hamburg, Germany). The supernatant liquid was collected and stored at −20 °C. The samples evaluated for CTP by monoclonal antibody testing ELISA CTP (TECAN/ JBL: 301170068) was performed. Cut-off values for monoclonal antibody ELISA CTP were as follows: <30 ng/mL was no evidence of PLF, 30–60 ng/mL was intermediate evidence of PLF, and >60 ng/mL was evidence of PLF.
2.2. Subjects
Study group:
We prospectively analyzed patients treated for severe to profound unilateral sudden sensorineural hearing loss with tympanotomy and consecutive round and oval window membrane sealing as first-line treatment in our department between November 2022 and October 2023. We defined severe to profound SSNHL as a hearing function decline of 60 dB or more in three consecutive frequencies. Head computed tomography (CT) and magnet resonance tomography imaging (MRI) assessments were performed to exclude other possible reasons for acute hearing loss. The indication for tympanotomy as first-line treatment was SSNHL with a mean PTA/bone conduction of at least 60 dB. Surgical treatment was followed by 3 days iv of steroids (250 mg Prednisolon).
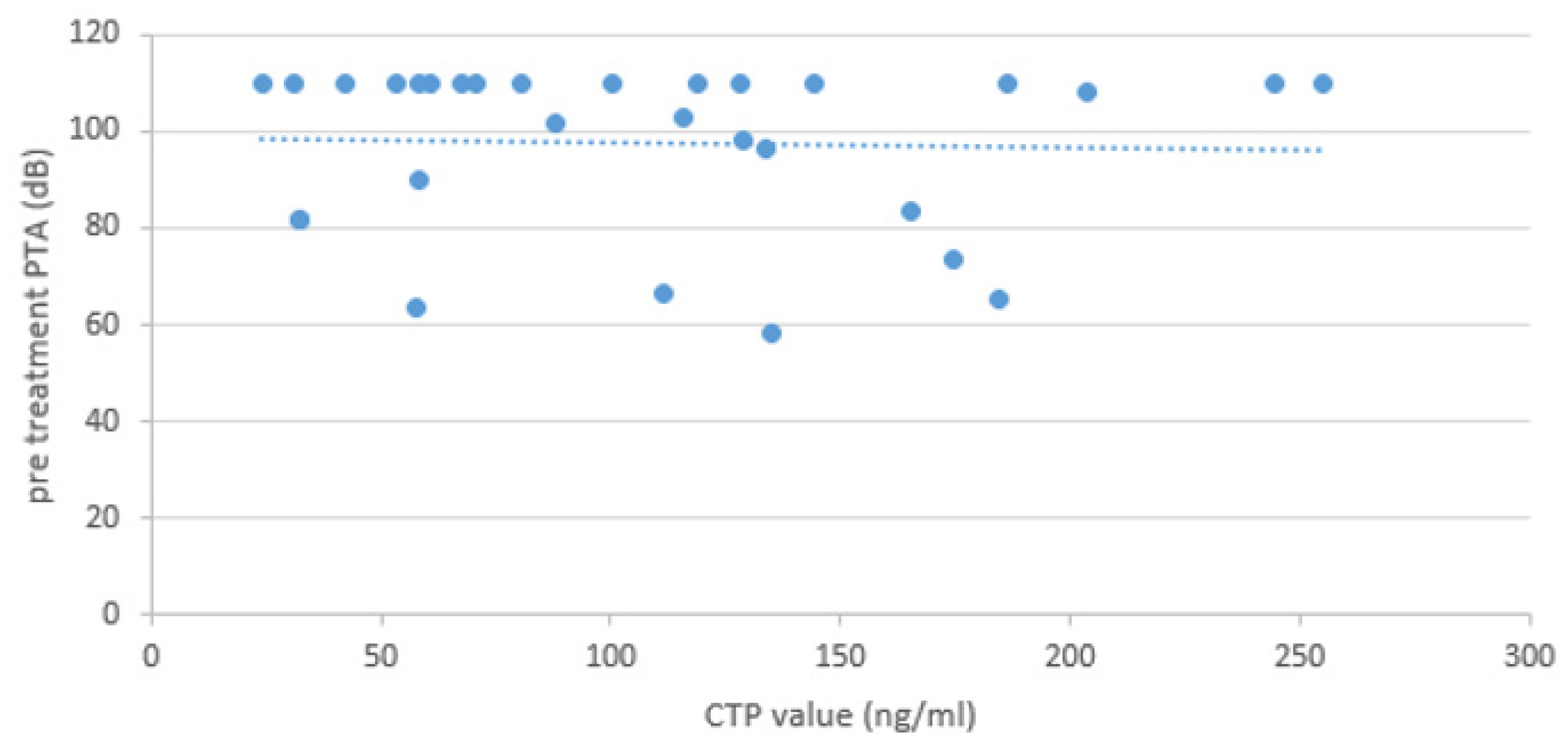
Exclusion criteria were patterns of other diseases explanatory for SSNHL and age of under 18 years. Individual data are collected in
Table 1.
2.3. Surgery
Explorative tympanotomy was performed under general anesthesia. After endaural incision and tympanomeatal flap preparation, middle ear exploration and intraoperative assessment of possible PLF was carried out. Partial bone removal was performed to get a complete overview of the oval window. The round and oval windows were identified. The ossicle chain and stapes footplate were assessed. Via applying pressure, movement of the ossicle chain was provoked, and fluid leaks of the round and oval window membranes were evaluated. All patients immediately obtained middle ear lavage to gain CTP samples for following ELISA-based CTP detection tests. 0.3 mL of saline was applied into the tympanic cavity, absorption via syringe after fluid rinsing three times. Regardless of intraoperative assessment, both oval and round windows were obturated. All patients received first-line treatment with round window and oval window sealing with fascia obtained from tissue from the endaural incision. Additionally, fibrin glue was applied to optimize window sealing. The applied surgical technique was similar in every operation.
2.4. Pure Tone Audiometry
PTA hearing thresholds were analyzed pre-surgical (baseline) and post-surgical 21 days after treatment. We assessed the mean hearing thresholds based on the three most affected contiguous frequencies between 0.5 and 4 kHz (Max 3 Freq 0=110 dB, maximum hearing loss set 0 = 110 dB) and the mean 4-frequency bone conduction at 0.5, 1, 1.5 and 4 kHz (4 Freq 0=130 dB, maximum hearing loss set 0 = 130 dB). Recovery was defined as a mean change in PTA BC of at least 10 dB. Failure to respond was defined as an improvement of BC less than 10 dB—classification of hearing threshold according to WHO hearing impairment 15.
2.5. Vestibular Symptoms
Classification based on absence or presence of vertigo at the onset of hearing impairment
2.6. Intraoperative findings
Visual assessment of ossicular chain, round and oval window membrane at microscopic magnification. Examination regarding integrity and fluid leaks. The ossicle chain and stapes footplate were assessed. The ossicle chain movement was provoked by applying pressure, and fluid leaks of the round and oval window membranes were checked. A positive PLF was classified as findings when a window membrane rupture was detected and/or fluid in the round and oval membrane area and/or dislocation of the stapes was noticed.
3. Results
3.1. Patient Characteristics
Between November 2022 and October 2023, 30 patients with severe to profound unilateral sudden sensorineural hearing loss underwent tympanotomy and consecutive sealing of the round and oval window membrane as first-line treatment. All patients underwent complete ENT examinations, including CT head scans, MRIs, and pure tone audiometry.
Preoperatively age range varied from 18-89 years (mean 55.9 years). 17 patients were male (57%), whilst 13 patients were female (43%). Explorative tympanotomy was performed within a range of 1 to 16 days after onset of symptoms (median 5.0, mean 5.8, standard deviation 4.2 days).
Mostly, evaluation of SSNHL etiology based on patient’s information upon admission indicated an idiopathic origin in 27 out of 30 cases (90%) as patients could not name any reason for hearing impairment in medical history or in-house conducted diagnostic lead to other plausible origins. In only 3 cases (10%) a traumatic event (pressure trauma, head injury) was associated with SSNHL. Vestibular symptoms occurred in 53% (n=16). In 2 out of 3 cases (67%) with traumatic history, vestibular symptoms were present. Idiopathic cases had vestibular symptoms in 14 of 27 cases (52%). (For individual data, see
Table 1).
3.2. Surgery
Surgery was performed after a mean of 5,8 days upon occurrence of symptoms with a range between 1-16 days (median 5.0, mean 5.8, standard deviation 4.2 days). 30 patients underwent explorative tympanotomy with consecutive sealing of the round and oval window membrane as first-line treatment of severe to profound SSNHL. Surgery was performed under general anesthesia.
3.3. Hearing Outcome after Surgery
Hearing recovery was defined as a mean improvement in PTA bone conduction (BC) of at least 10 dB from baseline PTA (preoperative) to PTA on day 21. Failure to respond was an improvement of BC less than 10 dB.
The mean PTA hearing threshold at admission to the hospital was preoperatively 97.7 dB (Max 3 Freq 0=110 dB) and 104.6 dB (4 Freq 0=130 dB) on the affected ear.
After explorative tympanotomy with consecutive sealing of the round and oval window membrane 57% (17 of 30) of patients improved by at least 10 dB in postoperative PTA Max 3 Freq 0=110 dB.
53% (16 of 30) of patients improved by at least 15 dB in postoperative PTA Max 3 Freq 0=110 dB. However, 43% (13 of 30) failed to respond with an improvement of BC less than 10 dB in postoperative PTA Max 3 Freq 0=110 dB.
PTA Max 3 Freq 0=110 dB improvement of 10-20 dB (mean 17,4 dB) was observed in 5 cases. Improvement of 20-30 dB (mean 26,2 dB) occurred in 5 cases. 2 cases improved between 30-40 dB (mean 34,5 dB). Furthermore, 5 cases improved more than 40 dB (mean 69,7 dB) after window coverage.
63% (19 of 30) of patients improved by at least 10 dB in postoperative PTA 4 Freq 0=130 dB, and 60% (18 of 30) improved by at least 15 dB in postoperative PTA 4 Freq 0=130 dB. However, 37% (11 of 30) of patients failed to respond with an improvement of BC less than 10 dB in postoperative PTA 4 Freq 0=130 dB.
A PTA 4 Freq 0=130 dB improvement of 10-20 dB (mean 21,6 dB) was observed in 4 cases. An improvement of 20-30 dB did not occur. 4 cases improved between 30-40 dB (mean 33,4 dB). Furthermore, 11 cases improved more than 40 dB (mean 62,9 dB) after window coverage.
The mean hearing improvement in postoperative PTA 4 Freq 0=130 dB was 27.8 dB, while the mean change in postoperative PTA Max 3 Freq 0=110 dB was 20.3 dB.
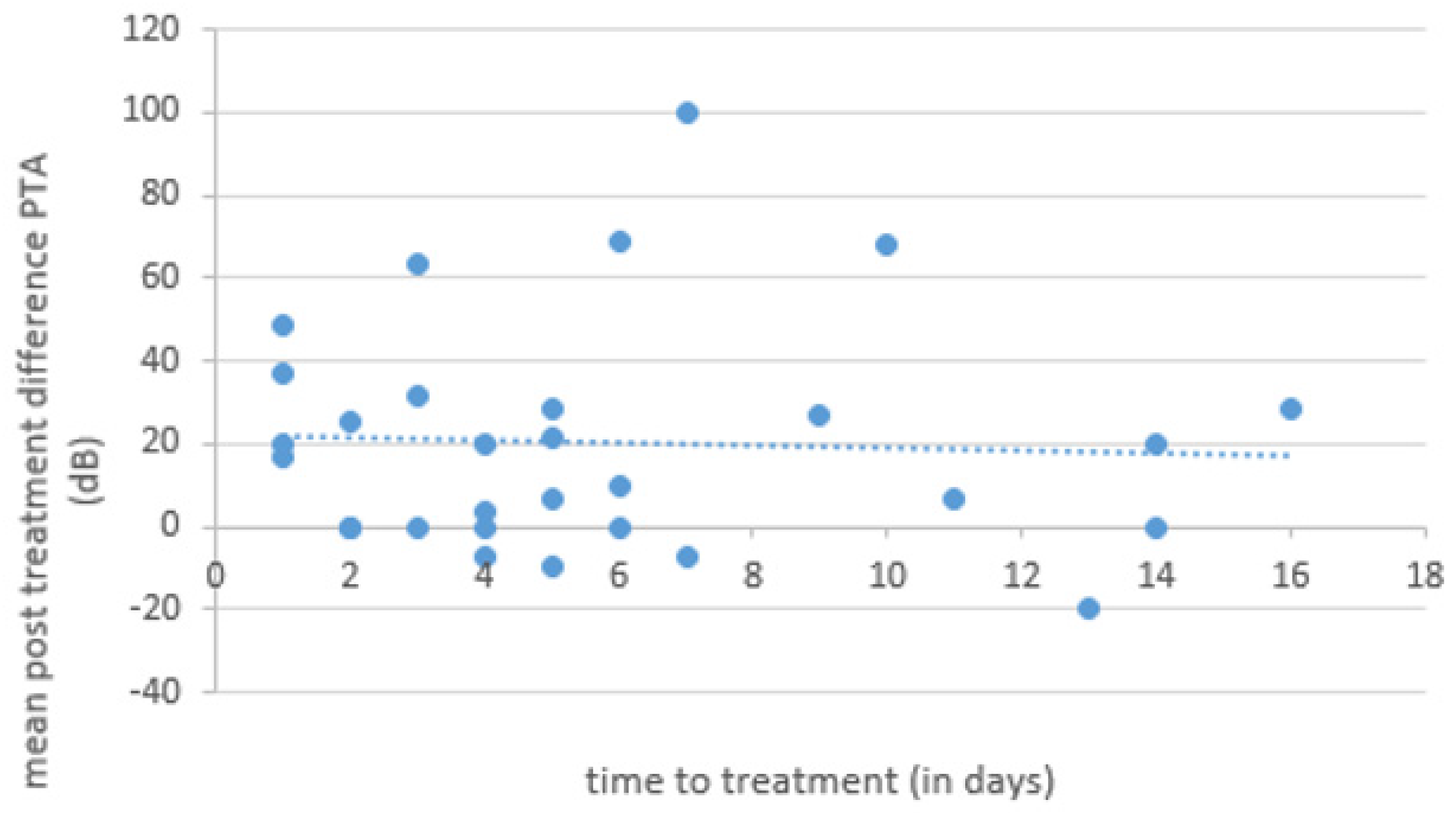
Statistical analysis revealed no statistically significant association between mean postoperative improvement of BC and time to treatment upon occurrence of symptoms (
Figure 1)
3.4. Intraoperative Observation
The intraoperative observation was based on the surgeon’s subjective impression while inspecting the tympanic cavity. In 17 of 30 cases (57%), no abnormal findings were seen. Signs of a lesion of the round and/or oval window (fluid) occurred in 13 cases (43%). Mostly, we did not see an obvious lesion but clear fluid in the area of the window membrane..It is possible that the fluid was not perilymph but rinsing fluid or local anesthesia.
3 out of 13 cases (23%) with intraoperative signs of a PLF had a medical history of a trauma event. In 1 case, the destruction of the footplate was detected. 10 of 13 cases (77%) with intraoperative signs of perilymph leak did not have a trauma medical history and were classified as SSNHL of idiopathic origin.
3.5. CTP Results
70 % (21 of 30) of SSNHL patients were CTP positive according to CTP detection test cutoff criteria. Intermediate CTP was present in 8 cases (27%) while 1 case was CTP negative (3%). We compared the intraoperative subjective PLF evaluation with objective CTP test results. 5 cases were false-positive, and 16 cases were false-negative. These findings can be concluded in a sensitivity of 33,3% and a specificity of 16,7% for intraoperative subjective PLF evaluation.
Based on the enrolled patient’s information upon admission, 27 out of 30 cases (90%) indicated an idiopathic SSNHL origin. Out of the idiopathic origin group, 66,7 % (n=18) were tested CTP positive, 29,6% (n=8) were tested CTP intermediate, and 1 case (3,7%) was classified as CTP negative.
3 patients (10 %) had a trauma etiology. All of the 3 patients (100%) with trauma etiology were tested CTP positive.
In CTP-positive cases, we observed an improvement of BC > 10db (Max 3 Freq 0=110 dB) in 13 out of 21 cases (62%) and BC > 15dB (Max 3 Freq 0=110 dB) in 12 cases (57%). The mean improvement of BC (Max 3 Freq 0=110 dB) in CTP-positive cases was 23.8 dB.
CTP intermediate cases had a mean improvement of 13,6 dB BC (Max 3 Freq 0=110 dB). We observed an improvement of BC > 10db (Max 3 Freq 0=110 dB) in 4 out of 8 cases (50%). These 4 cases (100%) had a BC improvement of > 15dB.
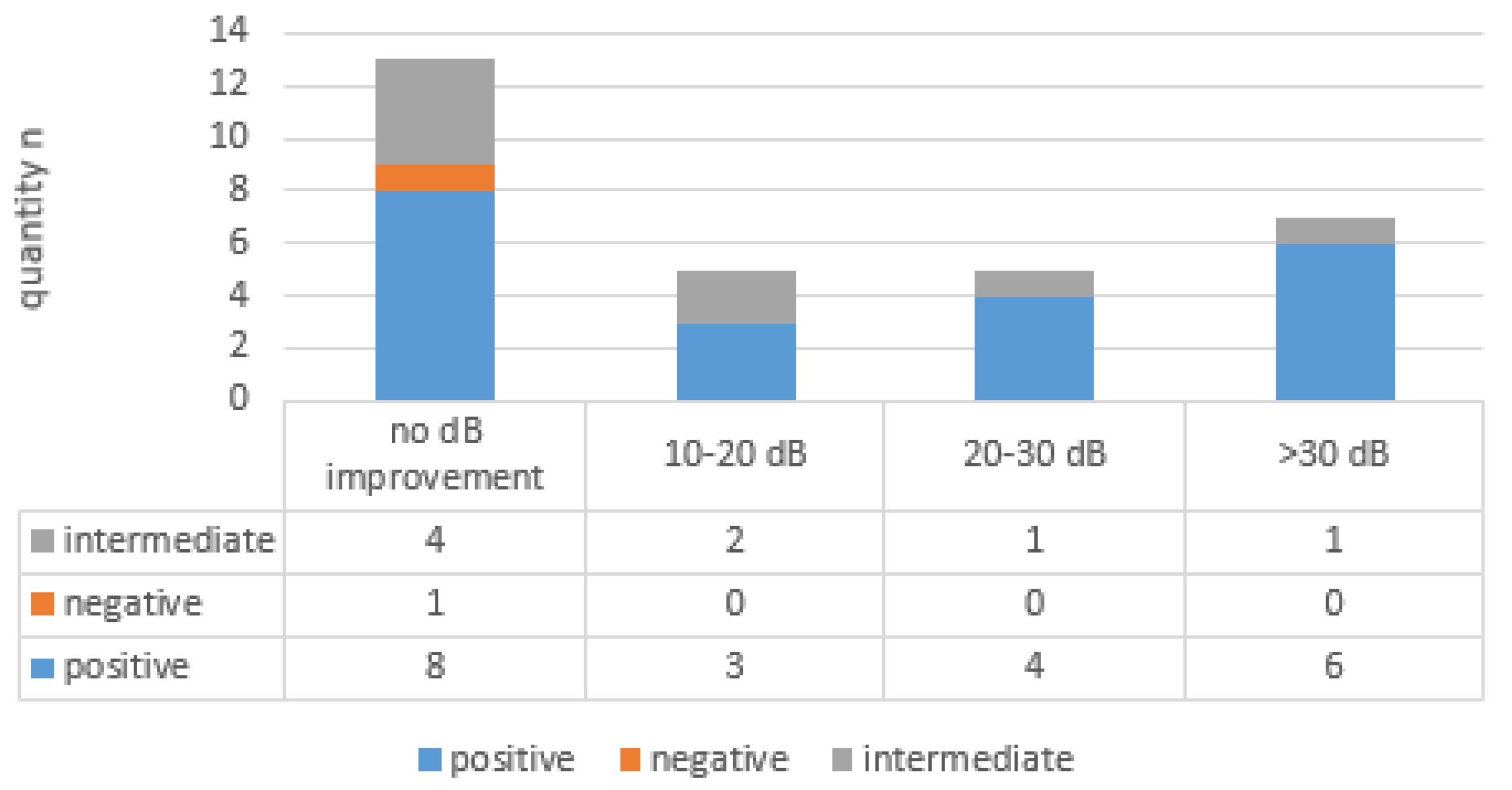
Max 3 Freq
0=110 dB improvement of BC (see
Figure 2) between 10-20 dB was CTP positive in 3 out of 5 cases (60%) and CTP intermediate in 2 out of 5 cases (40%). Improvement of BC between 20-30 dB was CTP positive in 4 out of 5 cases (80%) and in 1 out of 5 cases (20%), CTP intermediate. Improvement of BC > 30 dB was CTP positive in 6 out of 7 cases (86%) and CTP intermediate in 1 out of 7 cases (14%).
No BC improvement occurred in 13 out of 30 cases (43%), with 8 CTP positive cases, 4 CTP intermediate cases, and 1 CTP negative case.
The postoperative PTA 4 Freq 0=130 dB showed an improvement of BC > 10db in 19 out of 30 cases (63%) in CTP positive cases. We observed an improvement of BC > 15db (PTA 4 Freq 0=130 dB) in 18 out of 30 cases (60%). The mean improvement of BC (PTA 4 Freq 0=130 dB) in CTP positive cases was 30.7 dB.
CTP intermediate cases had a mean improvement of 24,0 dB BC (PTA 4 Freq 0=130 dB). An improvement of BC > 10db was observed in 5 out of 8 cases (62,5%). These 5 cases (100%) had a BC improvement of > 15dB.
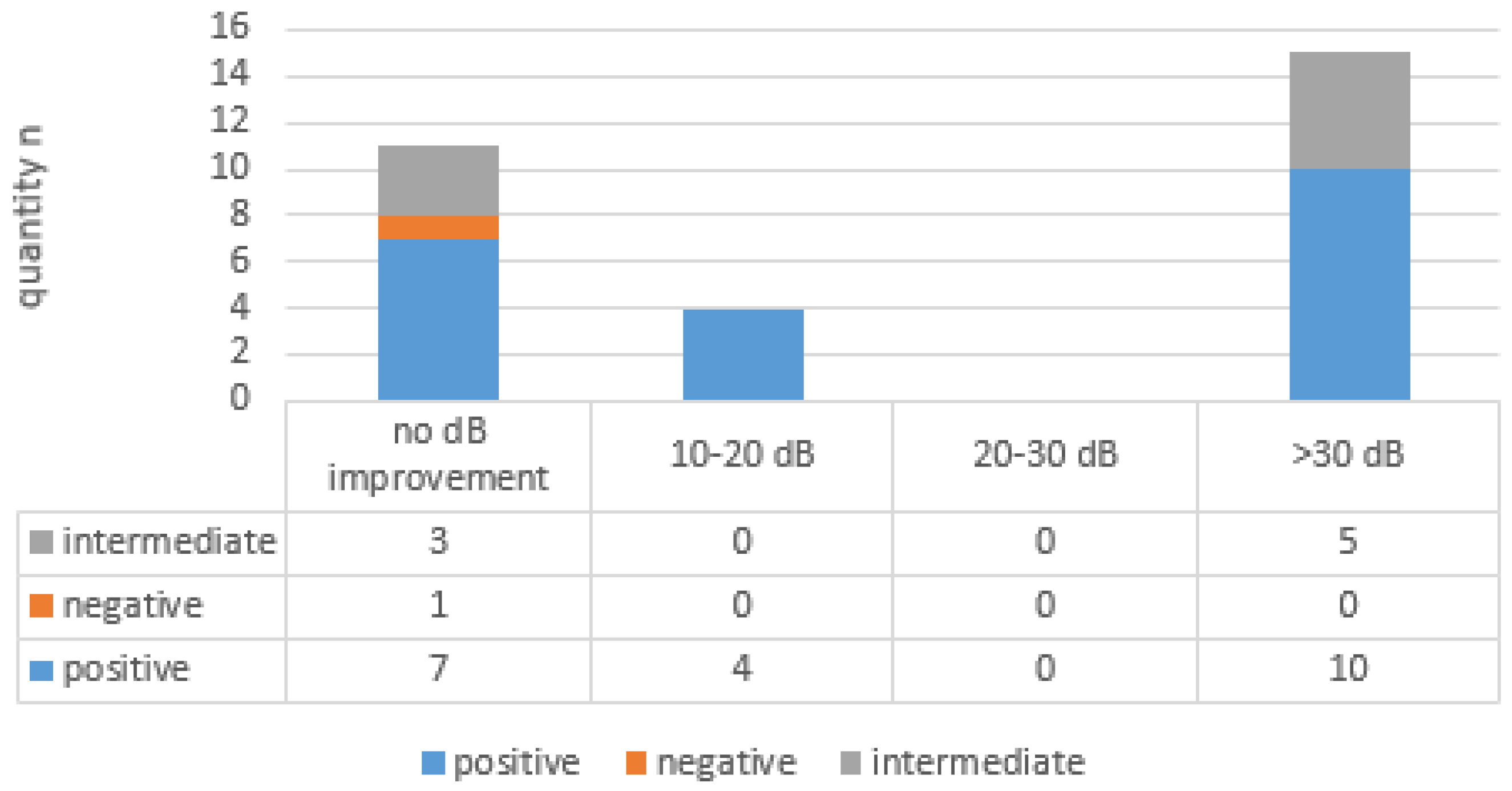
PTA 4 Freq
0=130 dB improvement of BC (see
Figure 3) between 10-20 dB was CTP positive in 4 out of 4 cases (100%). No improvement of BC between 20-30 dB occurred. Improvement of BC > 30 dB was CTP positive in 10 out of 15 cases (67%) and CTP intermediate in 5 out of 15 cases (33%).
No BC improvement occurred in 11 out of 30 cases (37%), with 7 CTP positive cases, 3 CTP intermediate cases and 1 CTP negative case.
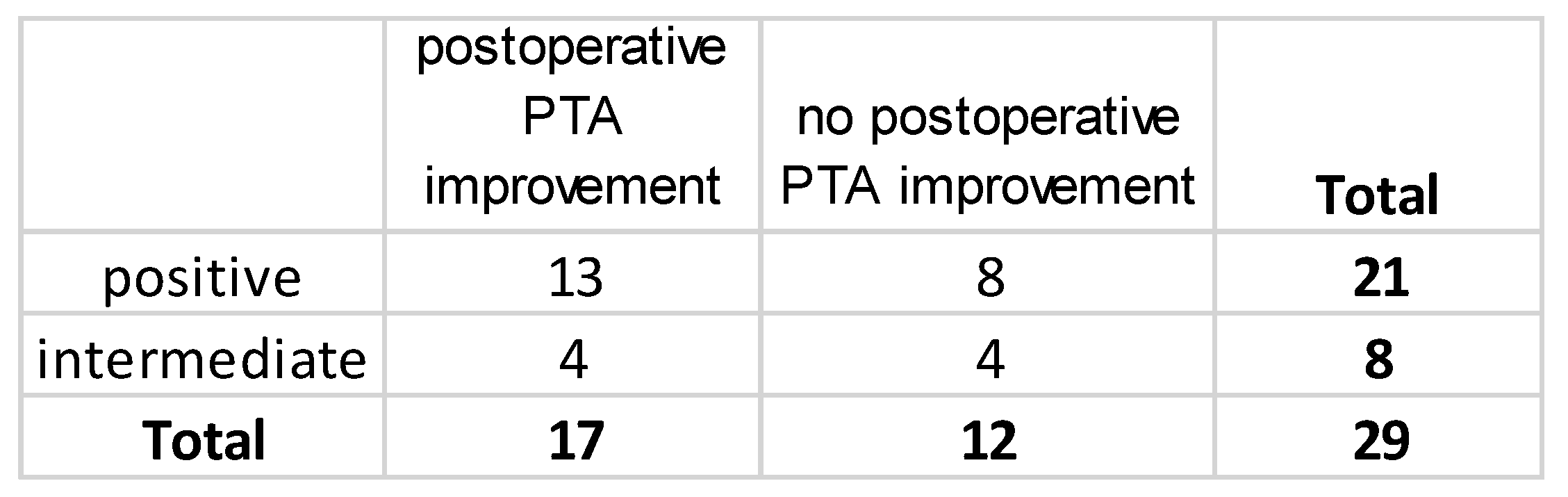
Statistical analysis revealed no statistically significant association between CTP categories (positive/intermediate) and postoperative PTA improvement (
Figure 4)
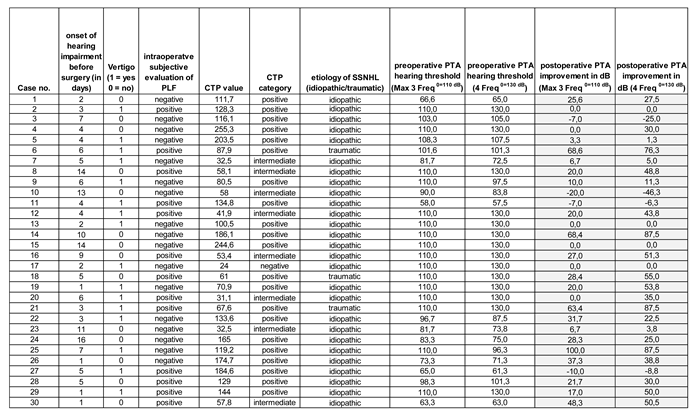
We tested for correlation of CTP value and pre-treatment PTA. Statistical analysis showed no correlation between CTP value and pre-treatment PTA (
Figure 5). CTP values ranged from 24,0 to 255,3 ng/ml. Cut-off values for monoclonal antibody ELISA CTP were as follows: <30 ng/mL was no evidence of PLF, 30–60 ng/mL was intermediate evidence of PLF, and >60 ng/mL was evidence of PLF.
3.6. Vertigo
Vertigo occurred in addition to hearing loss in 16 out of 30 cases (53%). 1 out of 16 cases was CTP negative (6%), 3 out of 16 cases (19%) were associated with intermediate CTP value. 12 out of 16 cases (75%) were CTP-positive. In only 2 out of 12 positive CTP cases (17%), a trauma occurred according to the patient’s medical history.
Vestibular testing was performed in CTP-positive cases. The results indicated that in all CTP-positive cases, there was a vestibular receptor function impairment on the unilateral hearing loss-affected side.
4. Discussion
Membrane ruptures of the round and/or oval window with consecutive perilymphatic fistula (PLF) are described as a cause of sudden hearing loss. Surgical sealing of the round and/or oval window membrane as a diagnostic and therapeutic tool remains highly discussed to date.
Intraoperative diagnostic of PLF while performing exploratory tympanotomy may lack of objective evidence as the visual confirmation might result from the surgeon’s subjective impression. Previous introduced PLF detection tests often lack evidence and are technically ambitious to perform [
9]. Recent studies demonstrated high rates of PLF findings in SSNHL cases using explorative tympanotomy and consecutive objective PLF assessment via inner ear-specific cochlin-tomoprotein (CTP) testing [
13,
14].
We detected a high rate of CTP positive PLF in 70% of the enrolled SSNHL patients. We compared the intraoperative subjective PLF evaluation with objective CTP test results. 5 cases were false-positive and 16 were false-negative underlying CTP testing as the gold standard.
The etiology of the SSNHL patient group study cohort was 90% idiopathic. Only 3 cases (10%) recorded traumatic events were associated with SSNHL. Our intraoperative observation, based on the surgeon’s subjective impression while inspecting the tympanic cavity, indicated normal findings in 57% of the cases.
Mostly, we did not see an obvious lesion, but clear fluid in the area of the window membrane was a possible indicator of a PLF. Despite visual „confirmation“ of fluid as a possible indicator of a lesion of the round and/or oval window in 43% of cases, it is possible that the intraoperative seen fluid was no perilymph but rinsing fluid or local anesthesia and therefore misinterpreted as PLF. As the intraoperative window evaluation during explorative tympanotomy highly depends on the surgeon’s subjective interpretation, there is a high degree of uncertainty.
Micro ruptures of the window membranes might not be visibly detectable as a PLF. Also, a fluctuating PLF due to a valve mechanism might occur. On the other hand, visible fluid from intraoperative local fluid injection, such as local anesthesia, might be misinterpreted as PLF [
8].
We performed two-window sealing of both oval and round windows. This is in line with current literature in cases of severe to profound SSNHL [
16]. After explorative tympanotomy with consecutive sealing of the round and oval window membrane, 57% (PTA Max 3 Freq
0=110 dB) and 63% (PTA 4 Freq
0=130 dB) of our study cohort improved by at least 10 dB.
We observed a 70% CTP positivity according to CTP detection test cutoff criteria in our SSNHL study cohort. In CTP positive cases we observed a postoperative improvement of BC > 10db in 62% (Max 3 Freq 0=110 dB) respectively 63% (PTA 4 Freq 0=130 dB) of cases. Mean improvement of BC in CTP positive cases was 23,8 dB (Max 3 Freq 0=110 dB) respectively 30,7 dB (PTA 4 Freq 0=130 dB). CTP intermediate cases had a mean improvement of 13,6 dB BC (Max 3 Freq 0=110 dB) and 24,0 dB BC (PTA 4 Freq 0=130 dB).
These findings indicate a high evidence of perilymphatic fistula in severe SSNHL and a specific recovery rate after explorative tympanotomy and two window sealing. The difference in BC improvement after window sealing between CTP positive, CTP intermediate and CTP negative cases is logically as a PLF repair through membrane sealing may reduce the negative impact on cochlear function and thereby improve postoperative bone conduction.
The only case of CTP negativity did not show any BC improvement at all. Neither CTP value nor intraoperative findings indicated a PLF. A spontaneous PLF window sealing might explain CTP negativity and normal intraoperative findings. Considered as of idiopathic aetiology it is important to take into account that this one case of CTP negativity already showed a significant acute preoperative hearing loss. Due to the small sample size of one CTP negative patient in our study group, the effect of window sealing in this patient group needs to be evaluated in a larger study cohort.
We observed in 57% of CTP positive cases vertigo additional to the hearing impairment. These observations are in line with the literature which correlated the occurrence of vertigo and the existence of perilymphatic fistula [
18].
No correlation was found between time to surgery and postoperative hearing recovery (
Figure 1). Spontaneous PLF remission of the round and/or oval window in some PLF cases might be a possible explanation. It is important to note that described spontaneous recovery rates in the literature include patients with mild hearing loss, low-degree hearing loss and Ménière’s disease linked low frequency hearing loss with a higher potential of recovery [
16]. These study cohorts differ substantially from our patient characteristics with severe to profound sudden sensorineural hearing loss and a generally significant weaker prognosis regarding hearing recovery according to literature [
15].
PTA hearing thresholds were analysed post-surgical 3 weeks after treatment. As a limitation of this study a post-surgical 3 month evaluation is missing. PTA hearing recovery rates after 3 month evaluation are even expected to be higher considering the positive effects of partial hearing recovery in this study after 3 weeks in > 50% of patients.
The high objective evidence rate of CTP positive PLF in 70 % of SSNHL patients despite the initially recorded 90% idiopathic etiology of SSNHL in our study cohort implies unclear events affecting inner ear structures. These findings imply a need for an early explorative tympanotomy with consecutive window sealing.
5. Conclusions
The combination of early tympanoscopy and inner ear specific cochlin-tomoprotein as detection tool for suspected perilymphatic fistula shows evidence of PLF as a key causative in SSNHL. These findings hold strong implications for the combination of tympanoscopy and inner ear specific cochlin-tomoprotein as detection tool for suspected perilymphatic fistula as a first line treatment for sudden sensorineural hearing loss.
Author Contributions
KA, writing, data collection, statistics, final approval. KR, experimental analysis, data collection, final approval. SLU, data collection, final approval. RC data collection final approval. PC, data collection final approval. SM, experimental analysis, final approval, accountable for all aspects. TI: writing, design, idea, data collection, final approval, accountable for all aspects.
Institutional Review Board Statement
The study is in line with the guidelines for human studies and is ethically following the World Medical Association Declaration of Helsinki. The study was reviewed and positively evaluated by the Ethical Commission of the Wilhelms Universität Münster (2021-597 fS, 11 Sep 2021). All patients gave their written consent for participation in the study.
Data Availability Statement
Upon request to the corresponding author. The data are not publicly available due to containing information that could compromise the privacy of research participants.
References
- National Institute of Health. Sudden deafness (NIH publication 00-4757). Bethesda (MD): National Institutes of Health; 2000.
- Koc A, Sanisoglu O. Sudden sensorineural hearing loss: Literature review on recent studies. J Otolaryngol. 2003;32:308–13.
- Schreiber BE, Agrup C, Haskard DO, Luxon LM. Sudden sensorineural hearing loss. Lancet. 2010 Apr 3;375(9721):1203-11. [CrossRef] [PubMed]
- Clinical Practice Guideline: Sudden Hearing Loss (Update).Otolaryngology–Head and Neck Surgery 2019, Vol. 161(1S) S1–S45.
- Bussieres R, Portmann D, Noyon P. When to suspect a perilymphatic fistula. Rev Laryngol Otol Rhinol (Bord) 2003;124(4):259-64.
- Arndt HJ. Spontaneous perforation of the membrane of the round window—a major cause of sudden deafness. Laryngol Rhinol Otol (Stuttg) 1984;63(9):439-44.
- Maier W, Fradis M, Kimpel S et al. Results of exploratory tympanotomy following sudden unilateral deafness and its effect on hearing restoration.Ear Nose Throat J 2008;87:438-51.
- Arenberg IK,Wu CM. Fluorescein as an easy, low-cost, ind irect, or reverse intraoperative marker to rule out perilymph versus localinjection. Am J OtoI19 96;17(2):259-62.
- LevensonMJ,DeslogeRB,ParisierSc. Beta-2 transferrin:Limitations of use as a clinical marker for perilymph. Laryngoscope 1996;106(2 Pt 1):159-61.
- Arenberg IK,Wu CM. Fluorescein as an easy, low-cost, ind irect, or reverse intraoperative marker to rule out perilymph versus local injection.Am J OtoI19 96;17(2):259-62.
- Bachmann-Harildstad G, Stenklev NC, Myrvoll E, Jablonski G, Klingenberg O. β-trace protein as a diagnostic marker for perilymphatic fluid fistula: a prospective controlled pilot study to test a sample collection technique. Otol Neurotol. 2011;32(1):7-10. [CrossRef]
- Ikezono T, Matsumura T, Matsuda H, Shikaze S, Saitoh S, Shindo S, et al. The diagnostic performance of a novel ELISA for human CTP (Cochlin-tomoprotein) to detect perilymph leakage. PLoS One. (2018) 13:e0191498. [CrossRef]
- Todt I,, Eduardo Martin Sainz, Ikezono T. Perilymphatic fistula, The New Era, CP0005 Journal of Vestibular research, vol. 32, no. s1, pp. SI-S327, 2022, XXXI Bárány Society Meeting, May 9th to May 11th, 2022, Madrid, Spain.
- Sasaki A, Ikezono T, Matsuda H, Araki R, Matsumura T, Saitoh S, Wasano K, Matsubara A. Prevalence of perilymphatic fistula in patients with sudden-onset sensorineural hearing loss as diagnosed by Cochlin-tomoprotein (CTP) biomarker detection: its association with age, hearing severity, and treatment outcomes. Eur Arch Otorhinolaryngol. 2024 May;281(5):2373-2381. Epub 2023 Dec 21. [CrossRef] [PubMed]
- Haile LM, Orji AU, Reavis KM, Briant PS, Lucas KM, Alahdab F, Bärnighausen TW, Bell AW, Cao C, Dai X, Hay SI, Heidari G, Karaye IM, Miller TR, Mokdad AH, Mostafavi E, Natto ZS, Pawar S, Rana J, Seylani A, Singh JA, Wei J, Yang L, Ong KL, Steinmetz JD; GBD 2019 USA Hearing Loss Collaborators. Hearing Loss Prevalence, Years Lived With Disability, and Hearing Aid Use in the United States From 1990 to 2019: Findings From the Global Burden of Disease Study. Ear Hear. 2024 Jan-Feb 01;45(1):257-267. Epub 2023 Sep 15. [CrossRef] [PubMed]
- Prenzler NK, Schwab B, Kaplan DM, El-Saied S. The role of explorative tympanotomy in patients with sudden sensorineural hearing loss with and without perilymphatic fistula. Am J Otolaryngol. 2018 Jan-Feb;39(1):46-49. doi: 10.1016/j.amjoto.2017.10.006. Epub 2017 Oct 9. Epub 2017 Oct 9. [CrossRef]
- Ryosuke Kitoh, Shin-ya Nishio, Kaoru Ogawa, Sho Kanzaki, Naohito Hato, Michihiko Sone, Satoshi Fukuda, Akira Hara, Tetsuo Ikezono, Kotaro Ishikawa, Satoshi Iwasaki, Kimitaka Kaga, Seiji Kakehata, Atsushi Matsubara, Tatsuo Matsunaga, Takaaki Murata, Yasushi Naito, Takashi Nakagawa, Kazunori Nishizaki, Yoshihiro Noguchi, Hajime Sano, Hiroaki Sato, Mikio Suzuki, Hideo Shojaku, Haruo Takahashi, Hidehiko Takeda, Testuya Tono, Hiroshi Yamashita, Tatsuya Yamasoba & Shin-ichi Usami (2017): Nationwide epidemiological survey of idiopathic sudden sensorineural hearing loss in Japan, Acta Oto-Laryngologica. [CrossRef]
- Heiden C, Porzsolt F, Biesinger E, Höing R. Die Spontanheilung des Hörsturzes [Spontaneous remission of sudden deafness]. HNO. 2000 Aug;48(8):621-3. German. [CrossRef] [PubMed]
- Matsuda H, Sakamoto K, Matsumura T, Saito S, Shindo S, Fukushima K, et al. A nationwide multicenter study of the Cochlin Tomo-protein detection test: clinical characteristics of perilymphatic fistula cases. Acta Otolaryngol. (2017) 137:S53–9. [CrossRef]
- Weinaug P: Spontaneous remission in sudden deafness. HNO 1984;32(8):346-351.
- Hornibrook J. Perilymph fistula: fifty years of controversy. ISRN Otolaryngol. 2012 Jul 31;2012:281248. [CrossRef] [PubMed]
- Freeman P (1975) Rupture of the round window membrane. Acta Otolaryngol (Belg) 29(5):783–794.
- Simmons F. The double-membrane break syndrome in sudden hearing loss. Laryngoscope 1979;89:59-66.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).