Submitted:
22 October 2024
Posted:
22 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
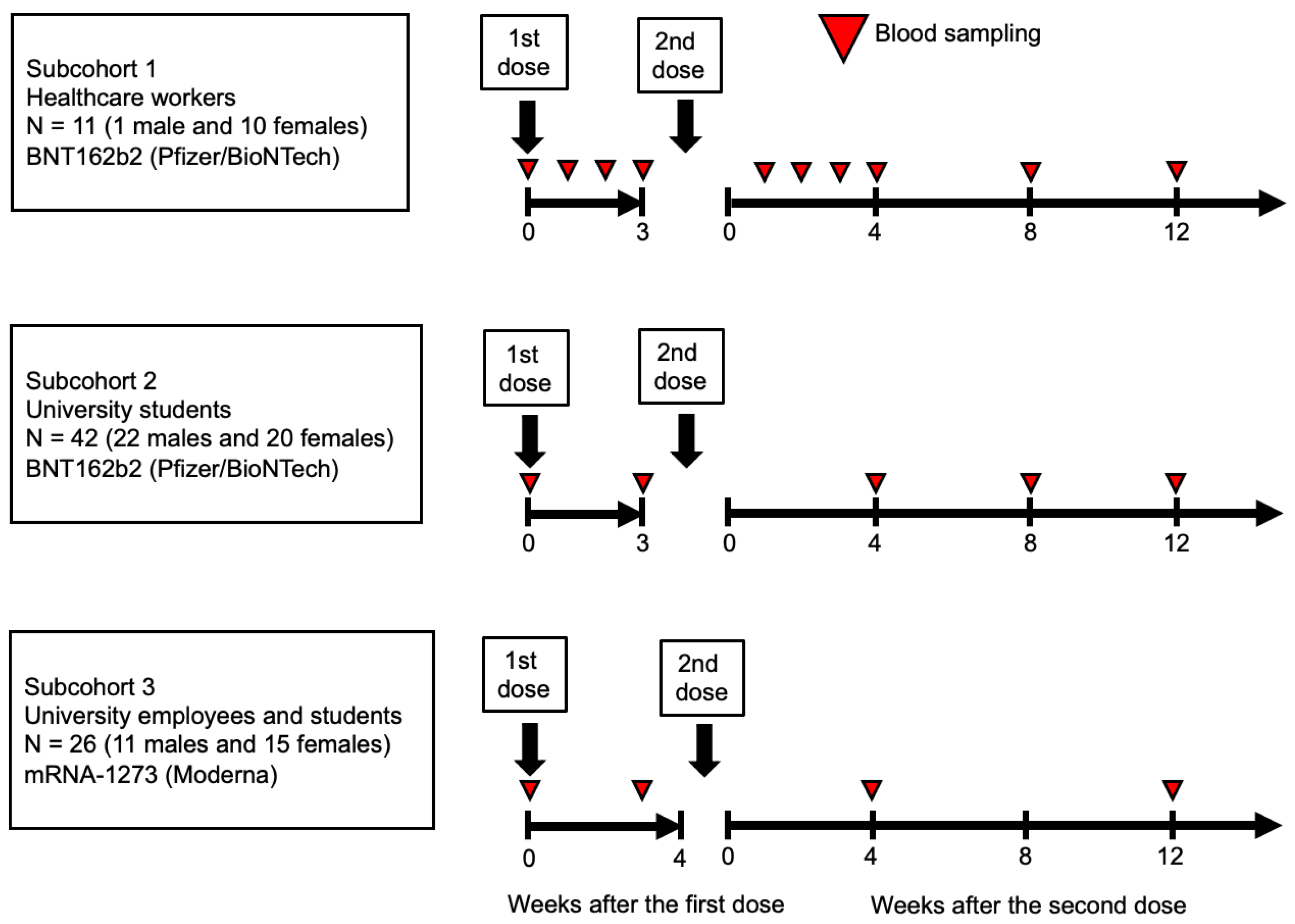
2.1. Study Design and Participants
2.2. Laboratory Testing
2.3. Self-Administered Questionnaire
2.4. Statistical Analyses
2.4.1. Covariates
2.4.2. Mixed Model
2.4.3. Least Squares Geometric Means
2.4.4. Sensitivity Analysis
3. Results
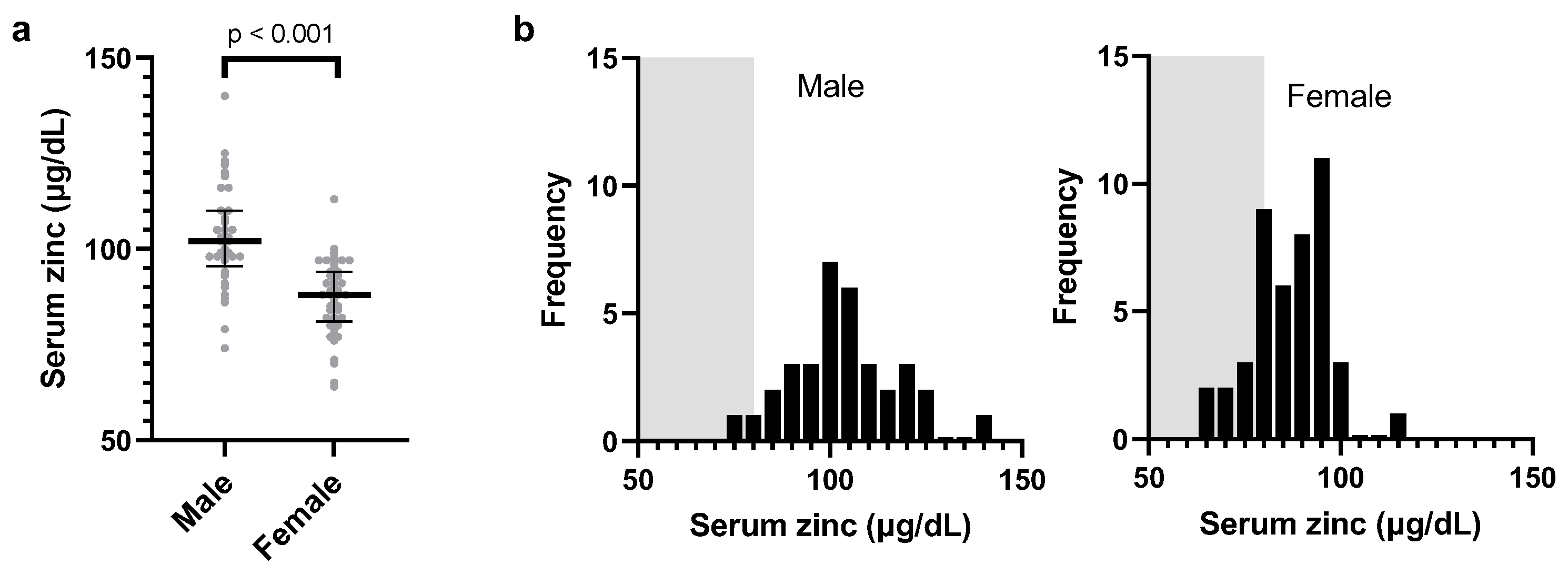
3.1. Baseline Characteristics
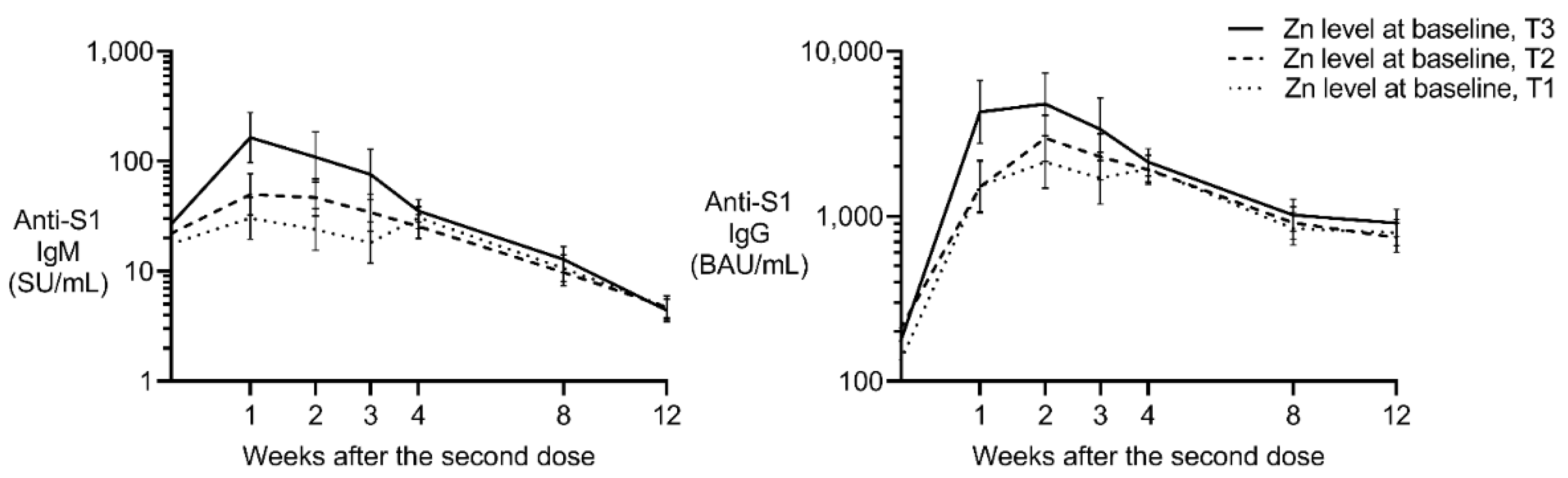
3.2. Effect of Baseline Zinc on Anti-S1 IgM Post-Vaccination
3.3. Effect of Baseline Zinc on Anti-S1 IgG Post-Vaccination
3.4. Sensitivity Analysis
4. Discussion
4.1. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cai, Y.; Kim, D.J.; Takahashi, T.; Broadhurst, D.I.; Ma, S.; Rattray, N.J.W.; Casanovas-Massana, A.; Israelow, B.; Klein, J.; Lucas, C.; et al. Kynurenic acid underlies sex-specific immune responses to COVID-19. medRxiv 2021, 14, eabf8483. [Google Scholar]
- Bechmann, N.; Barthel, A.; Schedl, A.; Herzig, S.; Varga, Z.; Gebhard, C.; Mayr, M.; Hantel, C.; Beuschlein, F.; Wolfrum, C.; et al. Sexual dimorphism in COVID-19: potential clinical and public health implications. Lancet Diabetes Endocrinol. 2022, 10, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.G.; Libby, A.; Vest, A.; Hopkinson, A.; Monte, A.A. Immune mechanisms associated with sex-based differences in severe COVID-19 clinical outcomes. Biol. Sex. Differ. 2022, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Galmes, S.; Serra, F.; Palou, A. Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework. Nutrients 2020, 12, 2738. [Google Scholar] [CrossRef] [PubMed]
- de Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary recommendations during the COVID-19 pandemic. Nutr. Rev. 2021, 79, 382–393. [Google Scholar] [CrossRef]
- Richardson, D.P.; Lovegrove, J.A. Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective. Br. J. Nutr. 2021, 125, 678–684. [Google Scholar] [CrossRef]
- Schubert, C.; Guttek, K.; Reinhold, A.; Grüngreiff, K.; Reinhold, D. The influence of the trace element zinc on the immune system. LaboratoriumsMedizin 2015, 39. [Google Scholar] [CrossRef]
- Maares, M.; Haase, H. Zinc and immunity: An essential interrelation. Arch. Biochem. Biophys. 2016, 611, 58–65. [Google Scholar] [CrossRef]
- Hojyo, S.; Fukada, T. Roles of Zinc Signaling in the Immune System. J. Immunol. Res. 2016, 2016, 6762343. [Google Scholar] [CrossRef]
- Gorji, A.; Khaleghi Ghadiri, M. Potential roles of micronutrient deficiency and immune system dysfunction in the coronavirus disease 2019 (COVID-19) pandemic. Nutrition 2021, 82, 111047. [Google Scholar] [CrossRef]
- Marshall, J.S.; Warrington, R.; Watson, W.; Kim, H.L. An introduction to immunology and immunopathology. Allergy Asthma Clin. Immunol. 2018, 14, 49. [Google Scholar] [CrossRef] [PubMed]
- Meydani, S.N.; Barnett, J.B.; Dallal, G.E.; Fine, B.C.; Jacques, P.F.; Leka, L.S.; Hamer, D.H. Serum zinc and pneumonia in nursing home elderly. Am. J. Clin. Nutr. 2007, 86, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Heller, R.A.; Sun, Q.; Hackler, J.; Seelig, J.; Seibert, L.; Cherkezov, A.; Minich, W.B.; Seemann, P.; Diegmann, J.; Pilz, M.; et al. Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol. 2021, 38, 101764. [Google Scholar] [CrossRef]
- Jothimani, D.; Kailasam, E.; Danielraj, S.; Nallathambi, B.; Ramachandran, H.; Sekar, P.; Manoharan, S.; Ramani, V.; Narasimhan, G.; Kaliamoorthy, I.; et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int. J. Infect. Dis. 2020, 100, 343–349. [Google Scholar] [CrossRef]
- Bagher Pour, O.; Yahyavi, Y.; Karimi, A.; Khamaneh, A.M.; Milani, M.; Khalili, M.; Sharifi, A. Serum trace elements levels and clinical outcomes among Iranian COVID-19 patients. Int. J. Infect. Dis. 2021, 111, 164–168. [Google Scholar] [CrossRef]
- Mossink, J.P. Zinc as nutritional intervention and prevention measure for COVID-19 disease. BMJ Nutr. Prev. Health 2020, 3, 111–117. [Google Scholar] [CrossRef]
- Rahman, M.T.; Idid, S.Z. Can Zn Be a Critical Element in COVID-19 Treatment? Biol. Trace Elem. Res. 2021, 199, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Razzaque, M.S. COVID-19 pandemic: Can zinc supplementation provide an additional shield against the infection? Comput. Struct. Biotechnol. J. 2021, 19, 1371–1378. [Google Scholar] [CrossRef]
- Chillon, T.S.; Maares, M.; Demircan, K.; Hackler, J.; Sun, Q.; Heller, R.A.; Diegmann, J.; Bachmann, M.; Moghaddam, A.; Haase, H.; et al. Serum Free Zinc Is Associated With Vaccination Response to SARS-CoV-2. Front. Immunol. 2022, 13, 2738. [Google Scholar] [CrossRef]
- Lopresti, A.L. The Effects of Psychological and Environmental Stress on Micronutrient Concentrations in the Body: A Review of the Evidence. Adv. Nutr. 2020, 11, 103–112. [Google Scholar] [CrossRef]
- Ashenagar, M.S.; Matsumoto, A.; Sakai, H.; Tokiya, M.; Hara, M.; Hirota, Y. Comparison of CLEIA and ELISA for SARS-CoV-2 Virus Antibodies after First and Second Dose Vaccinations with the BNT162b2 mRNA Vaccine. Vaccines 2022, 10, 487. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, A.; Hara, M.; Ashenagar, M.S.; Tokiya, M.; Sawada, T.; Iwasaka, C.; Furukawa, T.; Kitagawa, K.; Miyake, Y.; Hirota, Y. Variant Allele of ALDH2, rs671, Associates with Attenuated Post-Vaccination Response in Anti-SARS-CoV-2 Spike Protein IgG: A Prospective Study in the Japanese General Population. Vaccines 2022, 10, 1035. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, T.; Ikeda, K.; Tanaka, S.; Taniguchi, T.; Igari, H.; Onouchi, Y.; Kaneda, A.; Matsushita, K.; Hanaoka, H.; Nakada, T.A.; et al. Antibody responses to BNT162b2 mRNA COVID-19 vaccine and their predictors among healthcare workers in a tertiary referral hospital in Japan. Clin. Microbiol. Infect. 2021, 27, e1861. [Google Scholar] [CrossRef]
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int. J. Infect. Dis. 2022, 114, 252–260. [Google Scholar] [CrossRef]
- Deb, P.; Zannat, K.E.; Talukder, S.; Bhuiyan, A.H.; Jilani, M.S.A.; Saif-Ur-Rahman, K.M. Association of HLA gene polymorphism with susceptibility, severity, and mortality of COVID-19: A systematic review. HLA 2022, 99, 281–312. [Google Scholar] [CrossRef] [PubMed]
- Shimanoe, C.; Matsumoto, A.; Hara, M.; Akao, C.; Nishida, Y.; Horita, M.; Nanri, H.; Higaki, Y.; Tanaka, K. Perceived stress, depressive symptoms, and cortisol-to-cortisone ratio in spot urine in 6878 older adults. Psychoneuroendocrinology 2021, 125, 105125. [Google Scholar] [CrossRef]
- Salimans, L.; Liberman, K.; Njemini, R.; Kortekaas Krohn, I.; Gutermuth, J.; Bautmans, I. The effect of resistance exercise on the immune cell function in humans: A systematic review. Exp. Gerontol. 2022, 164, 111822. [Google Scholar] [CrossRef]
- De Spiegeleer, A.; Bronselaer, A.; Teo, J.T.; Byttebier, G.; De Tre, G.; Belmans, L.; Dobson, R.; Wynendaele, E.; Van De Wiele, C.; Vandaele, F.; et al. The Effects of ARBs, ACEis, and Statins on Clinical Outcomes of COVID-19 Infection Among Nursing Home Residents. J. Am. Med. Dir. Assoc. 2020, 21, 909–914 e902. [Google Scholar] [CrossRef]
- Daniels, L.B.; Sitapati, A.M.; Zhang, J.; Zou, J.; Bui, Q.M.; Ren, J.; Longhurst, C.A.; Criqui, M.H.; Messer, K. Relation of Statin Use Prior to Admission to Severity and Recovery Among COVID-19 Inpatients. Am. J. Cardiol. 2020, 136, 149–155. [Google Scholar] [CrossRef]
- Haase, H.; Rink, L. Zinc signals and immune function. Biofactors 2014, 40, 27–40. [Google Scholar] [CrossRef]
- Kawano, Y.; Noma, T. Role of interleukin-2 and interferon-gamma in inducing production of IgG subclasses in lymphocytes of human newborns. Immunology 1996, 88, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Sauerwein, R.W.; Van der Meer, W.G.; Drager, A.; Aarden, L.A. Interleukin 2 induces T cell-dependent IgM production in human B cells. Eur. J. Immunol. 1985, 15, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Mascle, X.; Albagli, O.; Lemercier, C. Point mutations in BCL6 DNA-binding domain reveal distinct roles for the six zinc fingers. Biochem. Biophys. Res. Commun. 2003, 300, 391–396. [Google Scholar] [CrossRef]
| Male | Female | ||||||
| Serum zinc categories | T1 | T2 | T3 | T1 | T2 | T3 | |
| Median (μg/dL) | 90.5 | 103 | 119 | 78.5 | 88.5 | 97 | |
| Interquartile range (μg/dL) | 74–98 | 99–107 | 108–140 | 64–82 | 83–92 | 93–113 | |
| Number | 12 | 11 | 11 | 16 | 14 | 15 | |
| Age, years | |||||||
| Median | 23 | 22 | 23 | 37.7 | 22.2 | 22 | |
| Interquartile range | 20.7–63.0 | 20.5–47.2 | 20.9–46.8 | 22.0–59.0 | 21.3–54.0 | 20.7–59.6 | |
| Occupation | |||||||
| Healthcare worker | 1 | 0 | 0 | 3 | 5 | 2 | |
| Student | 7 | 7 | 8 | 6 | 6 | 8 | |
| University worker | 4 | 4 | 3 | 7 | 3 | 5 | |
| Smoking, yes | 0 | 1 | 0 | 0 | 0 | 0 | |
| Steroid use, yes | 0 | 0 | 2 | 0 | 0 | 0 | |
| Dyslipidemia | 0 | 0 | 0 | 1 | 0 | 0 | |
| Perceived stress* | |||||||
| 0/1/2/3/4 | 3/1/3/5/0 | 5/1/1/3/1 | 5/1/3/2/0 | 2/2/5/5/2 | 4/1/4/4/1 | 6/1/2/5/1 | |
| rs671 variant allele** | |||||||
| 0/1/2 | 8/3/1 | 3/5/3 | 4/5/2 | 10/6/0 | 7/6/1 | 10/4/1 | |
| Ethanol, g/day/weight60kg | |||||||
| <1/ ≥1,<20/ ≥20 | 3/8/1 | 6/4/1 | 6/5/0 | 12/4/0 | 7/5/2 | 11/4/0 | |
| Exercise habit*** | |||||||
| 0/1/2/3 | 2/4/4/2 | 2/5/2/2 | 3/0/5/3 | 7/1/5/3 | 6/0/5/3 | 10/1/3/1 | |
| Allergic disease, yes | 2 | 0 | 2 | 4 | 1 | 1 | |
| Sleep disturbance | 0 | 2 | 0 | 0 | 1 | 1 | |
| Males | Females | ||||||||
| Model 1 | Model 2 | Model 1 | Model 2 | ||||||
| AIC = 427.1 | AIC = 419.6 | AIC = 682 | AIC = 680 | ||||||
| 162 observations | 162 observations | 255 observations | 255 observations | ||||||
| 34 participants | 34 participants | 45 participants | 45 participants | ||||||
| Fixed effect | β | p | β | p | Β | p | β | p | |
| BNT162b2 (reference) | |||||||||
| mRNA-1273 | −0.05036 | 0.7928 | −0.2172 | 0.3295 | 0.251 | 0.1028 | 0.239 | 0.2248 | |
| Age (per year of age) | −0.01927 | 0.0327 | −0.00379 | 0.6982 | −0.00958 | 0.0573 | −0.005 | 0.4755 | |
| Body height (per cm) | −0.01749 | 0.2796 | −0.012 | 0.3177 | |||||
| Steroid use, yes | −1.1015 | 0.0055 | — | — | |||||
| Dyslipidemia, yes | — | — | −1.3556 | 0.0002 | |||||
| Allergic disease, yes | 0.1747 | 0.3552 | 0.005 | 0.9729 | |||||
| Exercise habit (per category) | 0.01473 | 0.8767 | 0.028 | 0.6047 | |||||
| Cigarette smoke, yes | −0.07372 | 0.9281 | — | — | |||||
| Ethanol intake (per category) | −0.5076 | 0.0008 | 0.2721 | 0.0139 | |||||
| Perceived stress (per category) | −0.02271 | 0.7359 | 0.0276 | 0.6176 | |||||
| Sleep disturbance, yes | −0.3611 | 0.5297 | −0.7167 | 0.0124 | |||||
| Log zinc (μg/dL) | −0.7695 | 0.1856 | −0.4191 | 0.4909 | 2.2135 | <0.0001 | 1.5435 | 0.0122 | |
| The effects of baseline characteristics were computed using mixed models to account for repeated measurements and the random effect of the subpopulation. All models include the fixed effects of post-vaccination week as a categorical variable and variables listed in the table. The results are expressed in sysmex unit per mL (SU/mL). β, partial correlation coefficient. | |||||||||
| Males | Females | ||||||||
| Model 1 | Model 2 | Model 1 | Model 2 | ||||||
| AIC = 258 | AIC = 263 | AIC = 529 | AIC = 535 | ||||||
| 162 observations | 162 observations | 255 observations | 255 observations | ||||||
| 34 participants | 34 participants | 45 participants | 45 participants | ||||||
| Fixed effect | β | p | β | p | β | p | β | p | |
| BNT162b2(reference) | |||||||||
| mRNA-1273 | 0.4599 | 0.0062 | 0.3233 | 0.0094 | 0.8347 | <0.0001 | 0.7555 | <0.0001 | |
| Age (per years of age) | −0.012 | 0.017 | −0.005 | 0.3195 | −0.005 | 0.1384 | −0.0038 | 0.4312 | |
| Body height (per cm) | −0.0165 | 0.0659 | −0.002 | 0.8262 | |||||
| Steroid use, yes | −0.4357 | 0.0455 | — | — | |||||
| Dyslipidemia, yes | — | — | −0.6725 | 0.0107 | |||||
| Allergic disease, yes | 0.1581 | 0.131 | −0.2301 | 0.0196 | |||||
| Exercise habit (per category) | 0.0388 | 0.46 | −0.0102 | 0.7973 | |||||
| Cigarette smoke, yes | −1.2462 | 0.0064 | — | — | |||||
| Ethanol intake (per category) | −0.1627 | 0.0487 | −0.0068 | 0.9326 | |||||
| Perceived stress (per category) | 0.07533 | 0.0444 | 0.044 | 0.2769 | |||||
| Sleep disturbance, yes | −0.7196 | 0.0246 | −0.388 | 0.064 | |||||
| Log zinc(μg/dL) | −0.3268 | 0.3113 | −0.056 | 0.8676 | 1.609 | <0.0001 | 1.124 | 0.0131 | |
| The effects of baseline characteristics were computed using mixed models to account for repeated measurements and the random effect of the subpopulation. All models include the fixed effects of post-vaccination week as a categorical variable and variables listed in the table. BAU, binding antibody units, calibrated using the WHO International Standard. β, partial correlation coefficient. | |||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





