Submitted:
22 October 2024
Posted:
23 October 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Results
Discussion
Conclusions
Competing interests
Acknowledgments
List of Abbreviations:
References
- Adair T, Mikkelsen L, Hooper J, et al., 2023, Assessing the policy utility of routine mortality statistics: a global classification of countries. Bull World Health Organ, 101(12): 777–785. [CrossRef]
- Kreuter MW, Thompson T, McQueen A, et al., 2021, Addressing Social Needs in Health Care Settings: Evidence, Challenges, and Opportunities for Public Health. Annu Rev Public Health, 42: 329–344. [CrossRef]
- Mehta NK, Zheng H, Myrskylä M. 2019, How do age and major risk factors for mortality interact over the life-course? Implications for health disparities research and public health policy. SSM Popul Health, 8: 100438. [CrossRef]
- Janssen F. 2018, Advances in mortality forecasting: introduction. Genus, 74(1): 21. [CrossRef]
- Fantini MP, Lenzi J, Franchino G, et al., 2014, Mortality amenable to health care services and health inequalities among Italian Regions. Epidemiol Prev, 38(2): 100–7.
- Nolte E, McKee M. 2003, Measuring the health of nations: analysis of mortality amenable to health care. BMJ, 327(7424): 1129. [CrossRef]
- Mattiuzzi C, Lippi G. 2020, Which lessons shall we learn from the 2019 novel coronavirus outbreak? Ann Transl Med, 8(3): 48.
- Filip R, Gheorghita Puscaselu R, Anchidin-Norocel L, et al. 2022, Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J Pers Med, 12(8): 1295. [CrossRef]
- Foster TB, Fernandez L, Porter SR, et al., 2024, Racial and Ethnic Disparities in Excess All-Cause Mortality in the First Year of the COVID-19 Pandemic. Demography, 61(1): 59–85. [CrossRef]
- Centers for Disease Control and Prevention (CDC). 2024, WISQARS Leading Causes of Death Visualization Tool, viewed June 19, 2024, https://wisqars.cdc.gov/lcd/.
- Pollack Porter KM, Rutkow L, McGinty EE. 2018, The Importance of Policy Change for Addressing Public Health Problems. Public Health Rep, 133(1_suppl): 9S–14S. [CrossRef]
- Ahmad FB, Anderson RN. 2021, The Leading Causes of Death in the US for 2020. JAMA, 325(18): 1829–30. [CrossRef]
- Khalifa SAM, Swilam MM, El-Wahed AAA, et al., 2021, Beyond the Pandemic: COVID-19 Pandemic Changed the Face of Life. Int J Environ Res Public Health, 18(11): 5645. [CrossRef]
- Lippi G, Sanchis-Gomar F, Lavie CJ. 2024, Excess mortality for acute myocardial infarction in the United States during the first two years of the COVID-19 pandemic. Prog Cardiovasc Dis. 2024 Mar 20:S0033-0620(24)00051-3. Epub ahead of print. [CrossRef]
- Keim-Malpass J, Vavolizza RD, Cohn WF, et al., 2023 Cancer Screening and Treatment Delays During the COVID-19 Pandemic and the Role of Health Literacy in Care Re-engagement: Findings from an NCI-Designated Comprehensive Cancer Center sample. J Cancer Educ, 38(5): 1405–1412. [CrossRef]
- Karmali S, Saxena S, Richards O, et al., 2024, What was the impact of COVID-19 restrictions on unintentional injuries, in Canada and globally? A scoping review investigating how lockdown measures impacted the global burden of unintentional injury. Front Public Health, 12: 1385452. [CrossRef]
- Quercioli C, Bosco R, Bova G, et al., 2023, Evaluating the effect of COVID-19 incidence on Emergency Departments admissions. Results from a retrospective study in Central Italy during the first year of pandemic. Ann Ig, 35(5): 572–85. [CrossRef]
- Luo W, Liu X, Bao K, et al., 2022 Ischemic stroke associated with COVID-19: a systematic review and meta-analysis. J Neurol, 269(4): 1731–1740. [CrossRef]
- Sorrell JM. 2021, Losing a Generation: The Impact of COVID-19 on Older Americans. J Psychosoc Nurs Ment Health Serv, 59(4): 9–12. [CrossRef]
- Li R, Shen M, Yang Q, et al., 2023, Global Diabetes Prevalence in COVID-19 Patients and Contribution to COVID-19- Related Severity and Mortality: A Systematic Review and Meta-analysis. Diabetes Care, 46(4): 890–897. [CrossRef]
- Shetty PA, Ayari L, Madry J, et al., 2023, The Relationship Between COVID-19 and the Development of Depression: Implications on Mental Health. Neurosci Insights, 21; 18:26331055231191513. [CrossRef]
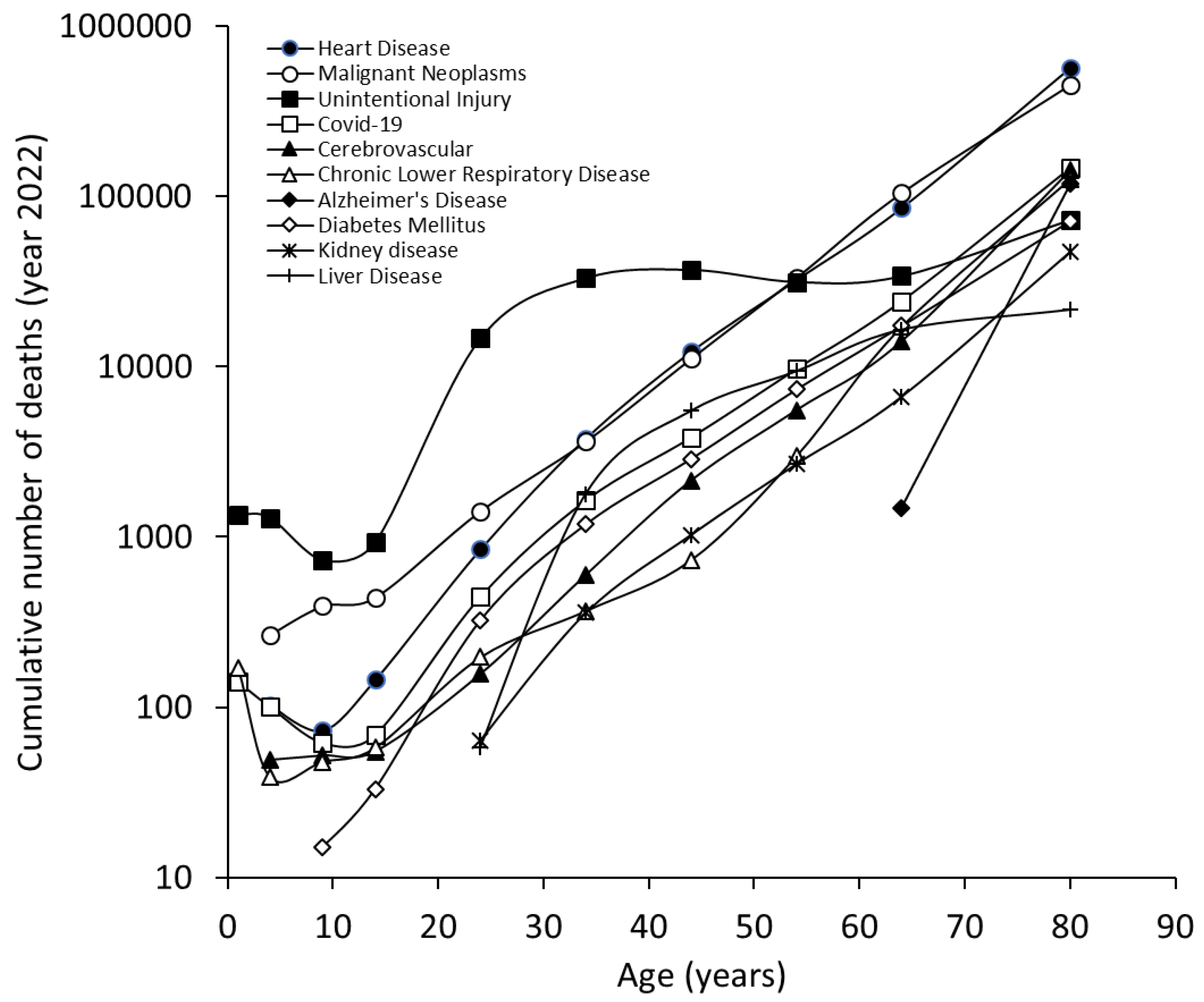
| n. | Cause | Number of deaths | Crude rate | Percentage of all deaths |
|---|---|---|---|---|
| Cumulative | ||||
| 1 | Heart Disease | 702880 | 210.9 | 26.2% |
| 2 | Malignant Neoplasms | 608371 | 182.5 | 22.7% |
| 3 | Unintentional Injury | 227039 | 68.1 | 8.5% |
| 4 | COVID-19 | 186552 | 56 | 6.9% |
| 5 | Stroke | 165393 | 49.6 | 6.2% |
| 6 | Chronic Lower Respiratory Disease | 147382 | 44.2 | 5.5% |
| 7 | Alzheimer's Disease | 120122 | 36 | 4.5% |
| 8 | Diabetes Mellitus | 101209 | 30.4 | 3.8% |
| 9 | Kidney disease | 57937 | 17.4 | 2.2% |
| 10 | Liver Disease | 54803 | 16.4 | 2.0% |
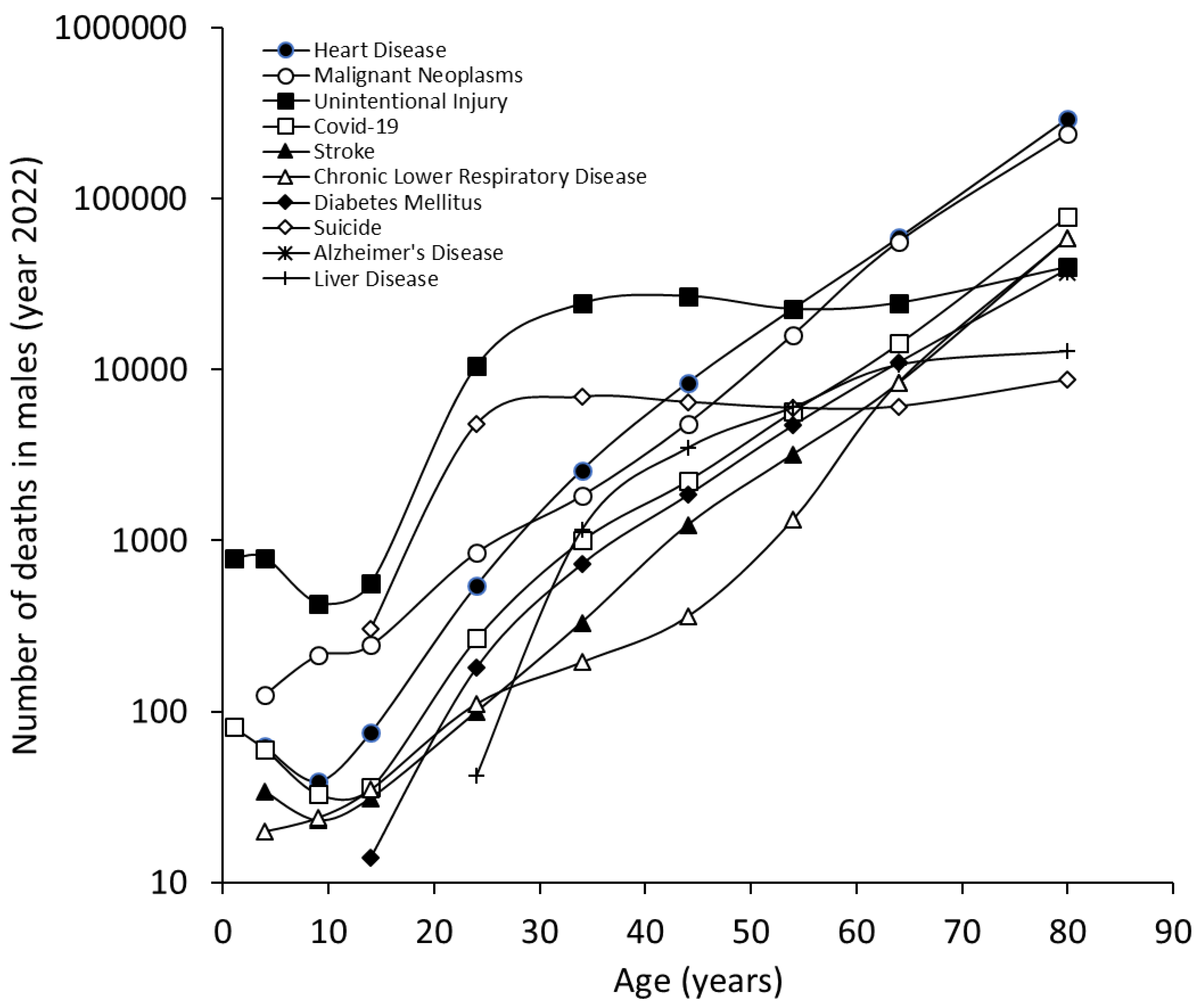
| Males | ||||
| 1 | Heart Disease | 386766 | 234 | 26.8% |
| 2 | Malignant Neoplasms | 319336 | 193.2 | 22.1% |
| 3 | Unintentional Injury | 151629 | 91.7 | 10.5% |
| 4 | COVID-19 | 102660 | 62.1 | 7.1% |
| 5 | Stroke | 71819 | 43.5 | 5.0% |
| 6 | Chronic Lower Respiratory Disease | 69004 | 41.7 | 4.8% |
| 7 | Diabetes Mellitus | 57557 | 34.8 | 4.0% |
| 8 | Suicide | 39273 | 23.8 | 2.7% |
| 9 | Alzheimer's Disease | 37475 | 22.7 | 2.6% |
| 10 | Liver Disease | 34340 | 20.8 | 2.4% |
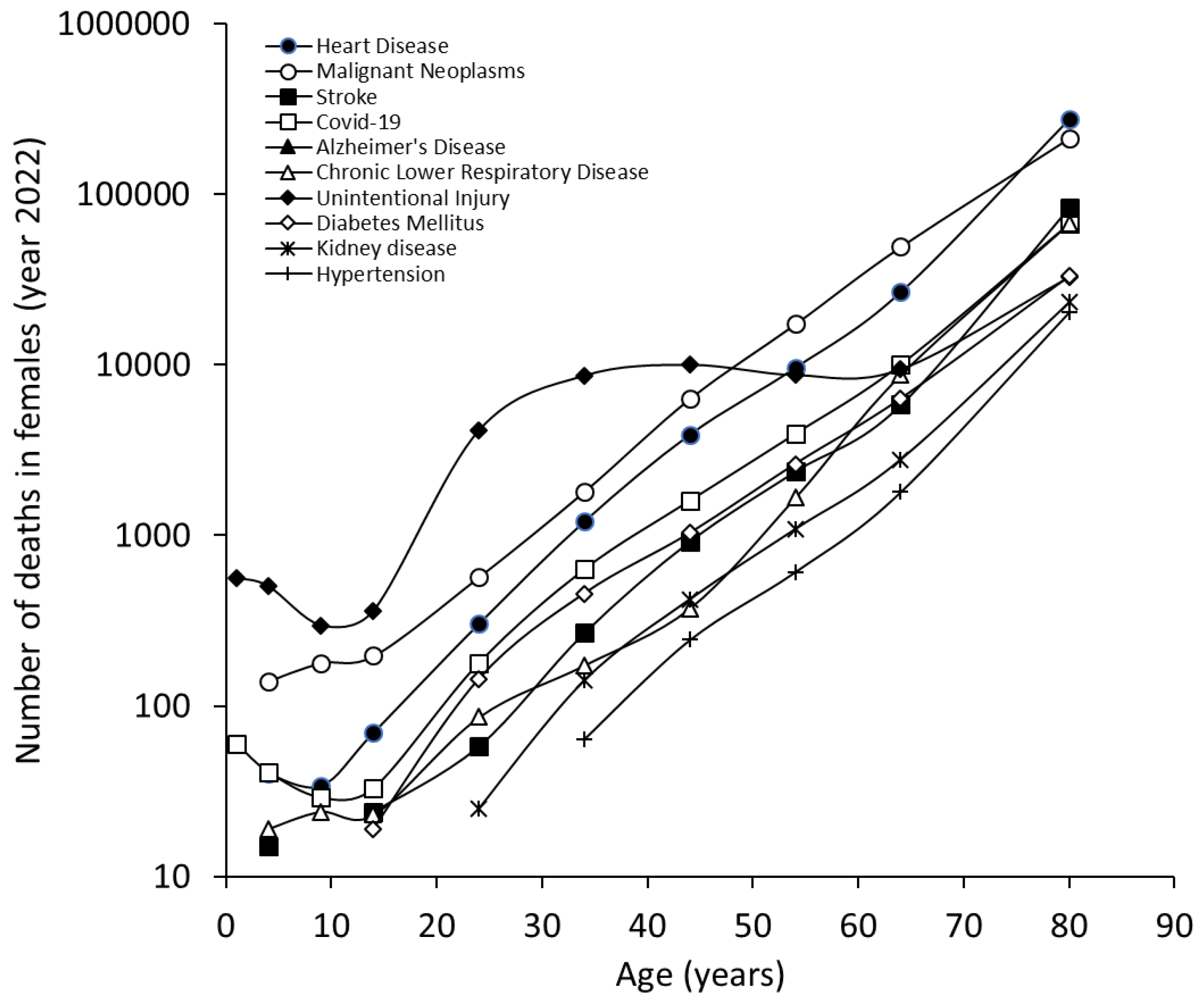
| Females | ||||
| 1 | Heart Disease | 316114 | 188.2 | 25.4% |
| 2 | Malignant Neoplasms | 289035 | 172 | 23.3% |
| 3 | Stroke | 93574 | 55.7 | 7.5% |
| 4 | COVID-19 | 83892 | 49.9 | 6.8% |
| 5 | Alzheimer's Disease | 82647 | 49.2 | 6.7% |
| 6 | Chronic Lower Respiratory Disease | 78378 | 46.7 | 6.3% |
| 7 | Unintentional Injury | 75410 | 44.9 | 6.1% |
| 8 | Diabetes Mellitus | 43652 | 26 | 3.5% |
| 9 | Kidney disease | 27759 | 16.5 | 2.2% |
| 10 | Hypertension | 23056 | 13.7 | 1.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





