Submitted:
26 October 2024
Posted:
28 October 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Aims
Methods
Pan-London PCI Registry
Study Population and Procedures
Socio-Economic Status
Clinical Outcomes
Ethics
Statistical Analysis
Results
Baseline Characteristics
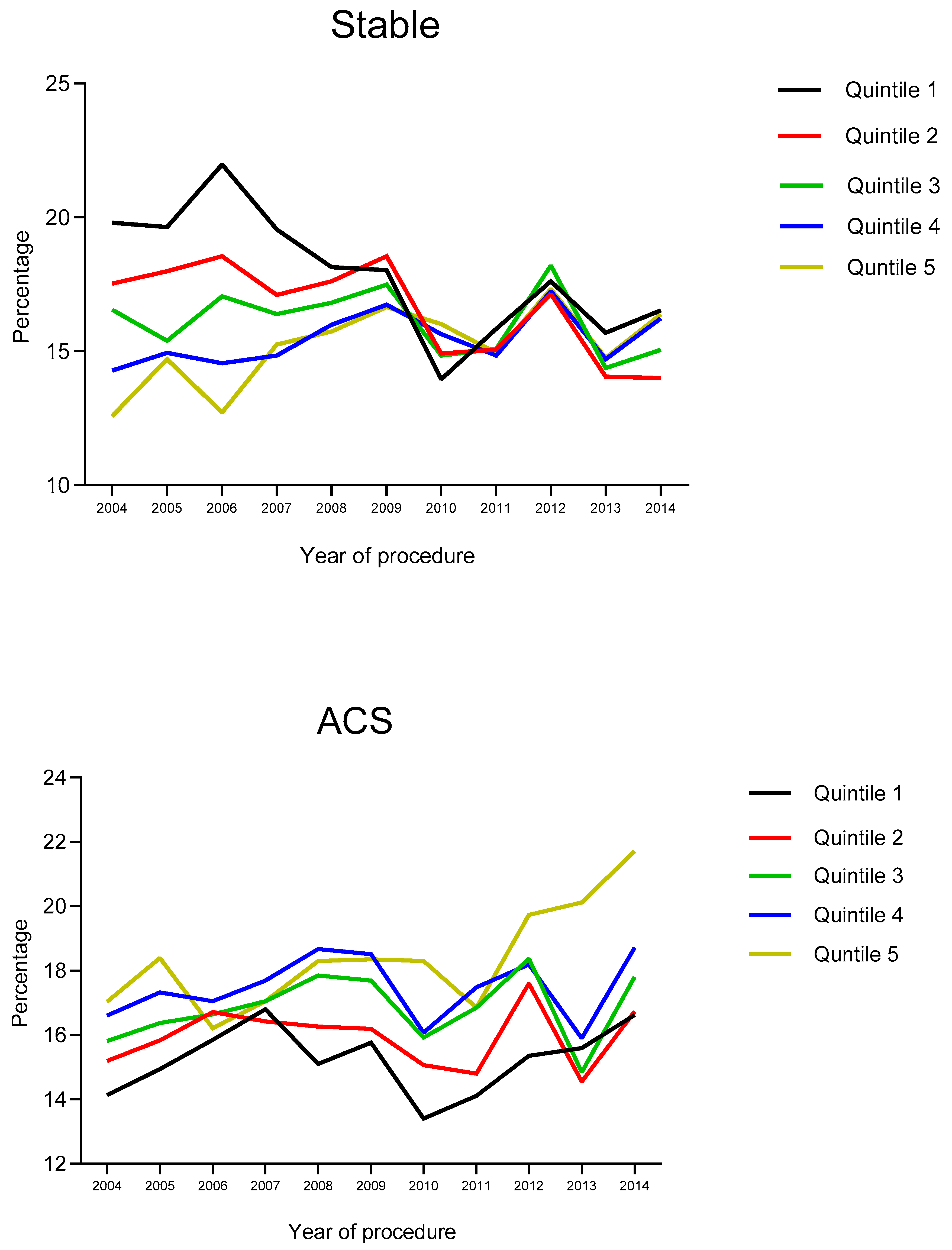
Procedural Characteristics
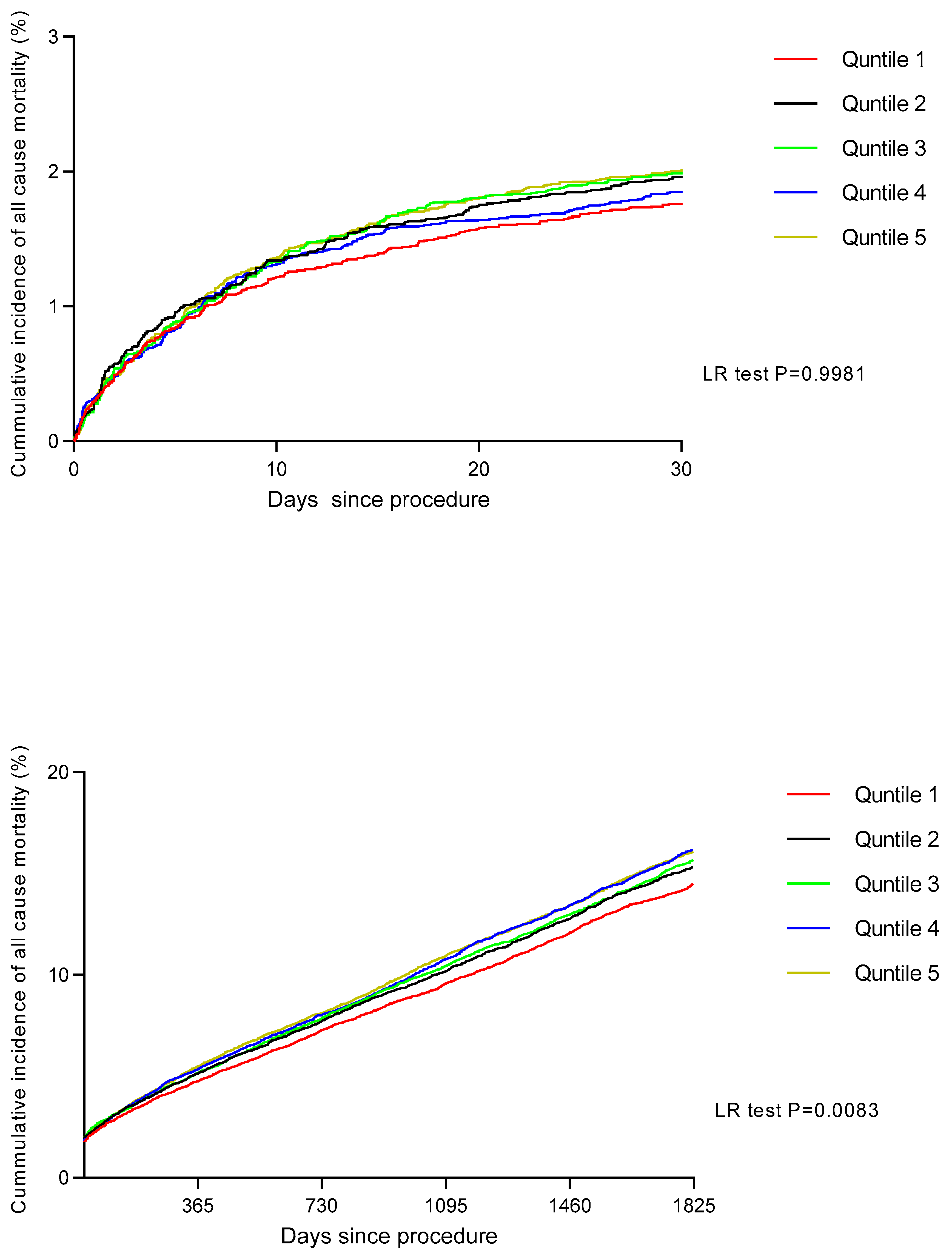
Procedural Outcomes
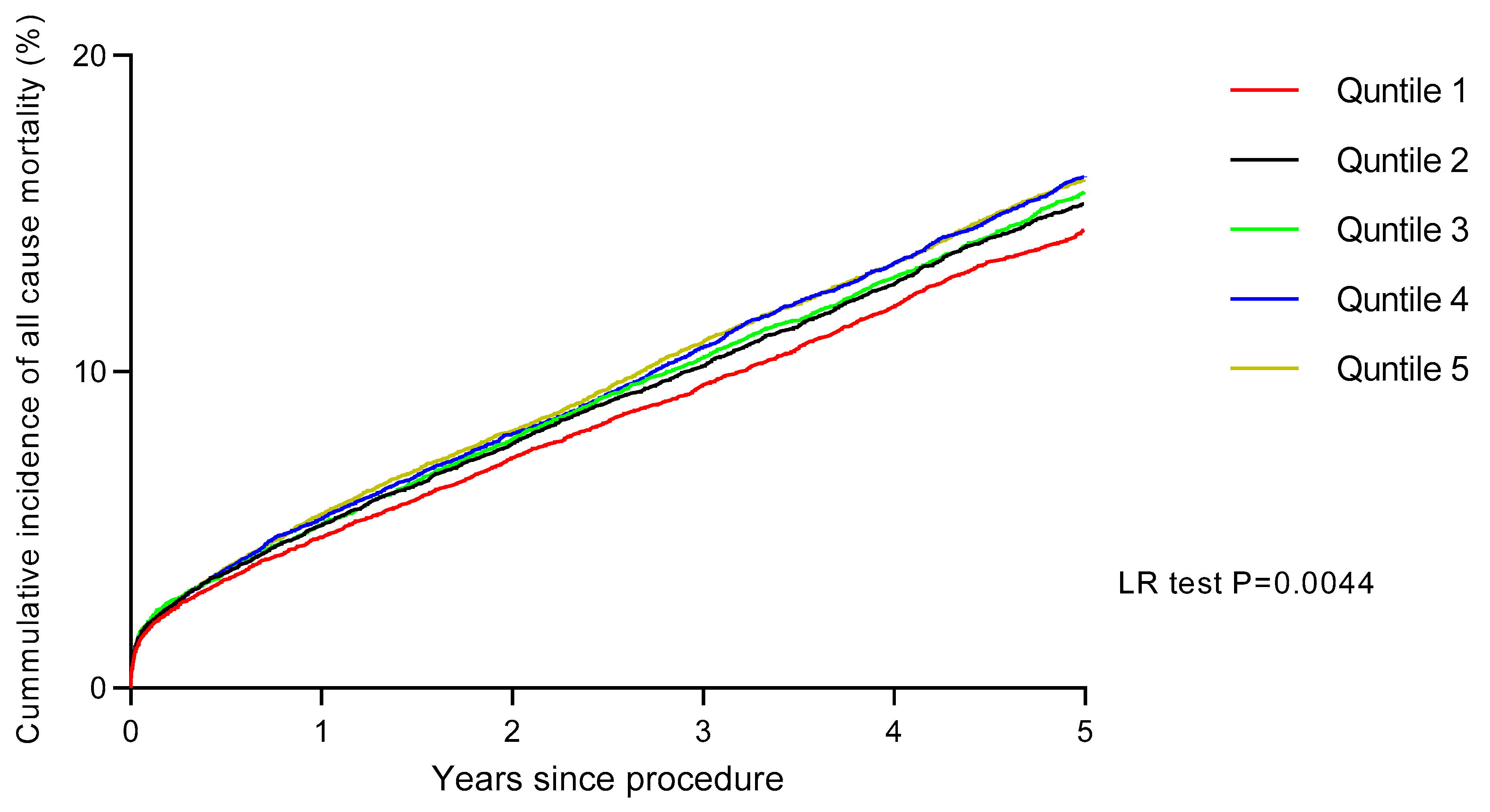
Long-Term Outcomes
Discussion
Limitations
Future Perspectives
Funding
Conflicts of Interest
References
- Davey-Smith G, Dorling D, Mitchell R, Shaw M. Health inequalities in Britain: Continuing increases up to the end of the 20th century. J. Epidemiol. Community Health 2002, 56, 434–435. [Google Scholar] [CrossRef] [PubMed]
- Suadicani P, Hein HO, Gyntelberg F. Socioeconomic status and ischaemic heart disease mortality in middle-aged men: Importance of the duration of follow-up. Cph. Male Study. Int. J. Epidemiol. 2001, 30, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen L, Niemann T, Thorsgaard N, Thuesen L, Lassen JF, Jensen LO; et al. Dimensions of socioeconomic status and clinical outcome after primary percutaneous coronary intervention. Circ. Cardiovasc. Interv. 2012, 5, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Moledina A, Tang KL. Socioeconomic Status, Mortality, and Access to Cardiac Services After Acute Myocardial Infarction in Canada: A Systematic Review and Meta-analysis. CJC open 2021, 3, 950–964.
- Biswas S, Andrianopoulos N, Duffy SJ, Lefkovits J, Brennan A, Walton A; et al. Impact of Socioeconomic Status on Clinical Outcomes in Patients With ST-Segment-Elevation Myocardial Infarction. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e004979. [Google Scholar] [CrossRef]
- Morris RW, Whincup PH, Lampe FC, Walker M, Wannamethee SG, Shaper AG. Geographic variation in incidence of coronary heart disease in Britain: The contribution of established risk factors. Heart (Br. Card. Soc. ) 2001, 86, 277–283. [Google Scholar] [CrossRef]
- Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. New Engl. J. Med. 1999, 341, 1359–1367. [Google Scholar] [CrossRef]
- MacLeod MC, Finlayson AR, Pell JP, Findlay IN. Geographic, demographic, and socioeconomic variations in the investigation and management of coronary heart disease in Scotland. Heart (Br. Card. Soc. ) 1999, 81, 252–256. [Google Scholar]
- Philbin EF, McCullough PA, DiSalvo TG, Dec GW, Jenkins PL, Weaver WD. Socioeconomic status is an important determinant of the use of invasive procedures after acute myocardial infarction in New York State. Circulation 2000, 102 (19 Suppl 3), Iii107–Iii115.
- Pell JP, Pell AC, Norrie J, Ford I, Cobbe SM. Effect of socioeconomic deprivation on waiting time for cardiac surgery: Retrospective cohort study. BMJ (Clin. Res. Ed) 2000, 320, 15–18. [Google Scholar] [CrossRef]
- Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H; et al. Persistence of use of lipid-lowering medications: A cross-national study. Jama 1998, 279, 1458–1462. [Google Scholar] [CrossRef] [PubMed]
- Ward PR, Noyce PR, St Leger AS. Are GP practice prescribing rates for coronary heart disease drugs equitable? A cross sectional analysis in four primary care trusts in England. J. Epidemiol. Community Health 2004, 58, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Gasevic D, Khan NA, Qian H, Karim S, Simkus G, Quan H; et al. Outcomes following percutaneous coronary intervention and coronary artery bypass grafting surgery in Chinese, South Asian and White patients with acute myocardial infarction: Administrative data analysis. BMC cardiovascular disorders. 2013, 13, 121.
- Roth C, Berger R, Kuhn M. The role of the socio-economic environment on medical outcomes after ST-segment elevation myocardial infarction. BMC Public Health 2019, 19, 630. [Google Scholar]
- Ludman, PF. British Cardiovascular Intervention Society Registry for audit and quality assessment of percutaneous coronary interventions in the United Kingdom. Heart (Br. Card. Soc. ) 2011, 97, 1293–1297. [Google Scholar] [CrossRef]
- deprivation DfCaLGIo. Department for Communities and Local Government. Indices of deprivation 2010 [Available from: http://www.communities.gov.uk/communities/research/indicesdeprivation/deprivation10/.
- Bello AK, Peters J, Rigby J, Rahman AA, El Nahas M. Socioeconomic status and chronic kidney disease at presentation to a renal service in the United Kingdom. Clin. J. Am. Soc. Nephrol. 2008, 3, 1316–1323. [Google Scholar] [CrossRef]
- Leigh Y, Seagroatt V, Goldacre M, McCulloch P. Impact of socio-economic deprivation on death rates after surgery for upper gastrointestinal tract cancer. Br. J. Cancer 2006, 95, 940–943. [Google Scholar] [CrossRef]
- Kareem H, Shetty PN, Devasia T, Karkala YR, Paramasivam G, Guddattu V; et al. Impact of socioeconomic status on adverse cardiac events after coronary angioplasty: A cohort study. Heart Asia 2018, 10, e010960. [Google Scholar] [CrossRef]
- Rosvall M, Chaix B, Lynch J, Lindström M, Merlo J. The association between socioeconomic position, use of revascularization procedures and five-year survival after recovery from acute myocardial infarction. BMC public health 2008, 8, 44.
- Rao SV, Schulman KA, Curtis LH, Gersh BJ, Jollis JG. Socioeconomic status and outcome following acute myocardial infarction in elderly patients. Arch. Intern. Med. 2004, 164, 1128–1133. [Google Scholar] [CrossRef]
- Mehta RH, O'Shea JC, Stebbins AL, Granger CB, Armstrong PW, White HD; et al. Association of mortality with years of education in patients with ST-segment elevation myocardial infarction treated with fibrinolysis. J. Am. Coll. Cardiol. 2011, 57, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Pilote L, Tu JV, Humphries K, Behouli H, Belisle P, Austin PC; et al. Socioeconomic status, access to health care, and outcomes after acute myocardial infarction in Canada's universal health care system. Med. Care 2007, 45, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Agarwal S, Garg A, Parashar A, Jaber WA, Menon V. Outcomes and resource utilization in ST-elevation myocardial infarction in the United States: Evidence for socioeconomic disparities. J. Am. Heart Assoc. 2014, 3, e001057. [Google Scholar] [CrossRef] [PubMed]
- Bonow RO, Grant AO, Jacobs AK. The cardiovascular state of the union: Confronting healthcare disparities. Circulation 2005, 111, 1205–1207. [Google Scholar] [CrossRef] [PubMed]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation 2005, 111, 1233–1241. [Google Scholar] [CrossRef]
- Shimony A, Zahger D, Ilia R, Shalev A, Cafri C. Impact of the community's socioeconomic status on characteristics and outcomes of patients undergoing percutaneous coronary intervention. Int. J. Cardiol. 2010, 144, 379–382. [Google Scholar] [CrossRef]
- Damiani G, Federico B, Bianchi CB, Ronconi A, Basso D, Fiorenza S; et al. Socio-economic status and prevention of cardiovascular disease in Italy: Evidence from a national health survey. Eur. J. Public Health 2011, 21, 591–596. [Google Scholar] [CrossRef]
- Lang SJ, Abel GA, Mant J, Mullis R. Impact of socioeconomic deprivation on screening for cardiovascular disease risk in a primary prevention population: A cross-sectional study. BMJ Open 2016, 6, e009984. [Google Scholar] [CrossRef]
- Shishehbor MH, Gordon-Larsen P, Kiefe CI, Litaker D. Association of neighborhood socioeconomic status with physical fitness in healthy young adults: The Coronary Artery Risk Development in Young Adults (CARDIA) study. Am. Heart J. 2008, 155, 699–705. [Google Scholar] [CrossRef]
- Franks AL, May DS, Wenger NK, Blount SB, Eaker ED. Racial differences in the use of invasive coronary procedures after acute myocardial infarction in Medicare beneficiaries. Ethn. Dis. 1993, 3, 213–220. [Google Scholar]
- Kahn KL, Pearson ML, Harrison ER, Desmond KA, Rogers WH, Rubenstein LV; et al. Health care for black and poor hospitalized Medicare patients. Jama 1994, 271, 1169–1174. [Google Scholar] [CrossRef]
- Rathore SS, Berger AK, Weinfurt KP, Feinleib M, Oetgen WJ, Gersh BJ; et al. Race, sex, poverty, and the medical treatment of acute myocardial infarction in the elderly. Circulation 2000, 102, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson H, Rosvall M, Hansen O, Chaix B, Merlo J. Socioeconomic position and secondary preventive therapy after an AMI. Pharmacoepidemiol. Drug Saf. 2010, 19, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ; et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch. Intern. Med. 2006, 166, 1842–1847. [Google Scholar] [CrossRef] [PubMed]
- Bajekal M, Scholes S, O'Flaherty M, Raine R, Norman P, Capewell S. Unequal trends in coronary heart disease mortality by socioeconomic circumstances, England 1982-2006: An analytical study. PLoS ONE 2013, 8, e59608. [Google Scholar]
- Greenland S, Robins J. Invited commentary: Ecologic studies--biases, misconceptions, and counterexamples. Am. J. Epidemiol. 1994, 139, 747–760. [Google Scholar] [CrossRef]
- Inclusion. OCfS. Why the Indices of Deprivation are Still Important in the Open Data Era. 2011 [Available from: https://ocsi.uk/2016/03/24/why-the-imd-is-still-important-in-the-open-data-age/.
- Jones DA, Howard JP, Rathod KS, Gallagher SM, Knight CJ, Jain AK; et al. The impact of socio-economic status on all-cause mortality after percutaneous coronary intervention: An observational cohort study of 13,770 patients. EuroIntervention 2015, 10, e1–e8. [Google Scholar]
- Smith ML, Towne S, Herrera-Venson A, Cameron K, Horel SA, Ory MG; et al. . Delivery of fall prevention interventions for at-risk older adults in rural areas: Findings from a national dissemination. Int. J. Environ. Res. Public Health 2018, 15, 2798. [Google Scholar] [CrossRef]
- Smith ML, Towne SD, Herrera-Venson A, Cameron K, Kulinski KP, Lorig K; et al. . Dissemination of chronic disease self-management education (CDSME) programs in the United States: Intervention delivery by rurality. Int. J. Environ. Res. Public Health 2017, 14, 638. [Google Scholar] [CrossRef]
- Ory MG, Smith ML. Research, practice, and policy perspectives on evidence-based programing for older adults. Front. Public Health 2015, 3, 136. [Google Scholar] [CrossRef]
- Vanassche T, Connolly SJ, Eikelboom JW, Healey JS, Lauw MN, Masiero S, Wang J, Yusuf S. Abstract 18936: Can Biomarkers Improve Risk Stratification of Atrial Fibrillation Patients? Analysis of 3578 Aspirin-treated Patients in ACTIVE and AVERROES. Circulation 2014, 130, A18936. [Google Scholar]
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | p Value | |
|---|---|---|---|---|---|---|
| (n = 18,727) | (n = 18,724) | (n = 18,708) | (n = 18,684) | (n = 18,717) | ||
| Age (yrs) | 66.70 ± 11.45 | 65.55 ± 11.86 | 64.46 ± 12.17 | 63.14 ± 12.24 | 64.32 ± 12.15 | <0.0001 |
| Ethnicity (Caucasian) | 11817 (63.1%) | 10598 (56.6%) | 9092 (48.6%) | 7997 (42.8%) | 6420 (34.3%) | <0.0001 |
| Gender (Male) | 14008 (74.8%) | 14024 (74.9%) | 13975 (74.7%) | 13452 (74.2%) | 13925 (74.4%) | 0.358 |
| Previous MI | 3521 (18.8%) | 3876 (20.7%) | 3779 (20.2%) | 3774 (20.2%) | 3762 (20.1%) | 0.218 |
| Previous CABG | 4232 (22.6%) | 4101 (21.9%) | 3816 (20.4%) | 3606 (19.3%) | 3332 (17.8%) | <0.0001 |
| Previous PCI | 5262 (28.1%) | 5149 (27.5%) | 4958 (26.5%) | 4914 (26.3%) | 4567 (24.4%) | <0.0001 |
| Hypercholesterolaemia | 10993 (58.7%) | 10879 (58.1%) | 10757 (57.7%) | 10818 (57.9%) | 10294 (55.0%) | <0.0001 |
| Diabetes mellitus | 3071 (16.4%) | 3782 (20.2%) | 4434 (23.7%) | 5007 (26.8%) | 5615 (30.0%) | <0.0001 |
| Hypertension | 10487 (56.0%) | 10617 (56.7%) | 10907 (58.3%) | 11080 (59.3%) | 11062 (59.1%) | <0.0001 |
| Smoking History | 10244 (54.7%) | 10785 (57.6%) | 10982 (58.7%) | 11715 (62.7%) | 12072 (64.5%) | <0.0001 |
| PVD | 543 (2.9%) | 618 (3.3%) | 617 (3.3%) | 654 (3.5%) | 674 (3.6%) | 0.002 |
| CKD (Creat >200) | 581 (3.1%) | 749 (4.0%) | 842 (4.5%) | 916 (4.9%) | 880 (4.7%) | <0.0001 |
| Previous CVA | 450 (2.4%) | 487 (2.6%) | 468 (2.5%) | 467 (2.5%) | 487 (2.6%) | 0.894 |
| Poor LV function | 974 (5.2%) | 1723 (9.2%) | 2077 (11.1%) | 1756 (9.4%) | 2059 (11.0%) | <0.0001 |
| Cardiogenic Shock | 412 (2.2%) | 431 (2.3%) | 468 (2.5%) | 486 (2.6%) | 468 (2.5%) | 0.120 |
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | p Value | |
|---|---|---|---|---|---|---|
| (n = 18,727) | (n = 18,724) | (n = 18,708) | (n = 18,684) | (n = 18,717) | ||
| Access for PCI | ||||||
| Radial | 9832 (25.2%) | 4831 (25.8%) | 5126 (27.4%) | 5400 (28.9%) | 5933 (31.7%) | <0.0001 |
| Acute coronary syndrome | ||||||
| Primary PCI for STEMI | 4345 (23.2%) | 4494 (24.0%) | 4602 (24.6%) | 4652 (24.9%) | 4773 (25.5%) | <0.0001 |
| PCI for NSTEMI/UA | 4700 (25.1%) | 5224 (27.9%) | 5519 (29.5%) | 6035 (32.3%) | 6382 (34.1%) | <0.0001 |
| Elective | 9289 (49.6%) | 8688 (46.4%) | 8213 (43.9%) | 7623 (40.8%) | 7637 (40.8%) | <0.0001 |
| CTOs | 1891 (10.1%) | 1741 (9.3%) | 1702 (9.1%) | 1682 (9.0%) | 1479 (7.9%) | <0.0001 |
| Left main coronary artery | 787 (4.2%) | 730 (3.9%) | 655 (3.5%) | 673 (3.6%) | 543 (2.9%) | <0.0001 |
| Right coronary artery | 6798 (36.3%) | 6853 (36.6%) | 7053 (37.7%) | 7119 (38.1%) | 6963 (37.2%) | 0.003 |
| Left anterior descending artery | 9326 (49.8%) | 9175 (49.0%) | 8999 (48.1%) | 9024 (48.3%) | 9096 (48.6%) | 0.020 |
| Left circumflex artery | 4607 (24.6%) | 4775 (25.5%) | 4752 (25.4%) | 4820 (25.8%) | 4923 (26.3%) | 0.004 |
| Vein graft | ||||||
| Multi-vessel PCI | 3521 (18.8%) | 3632 (19.4%) | 3891 (20.8%) | 4017 (21.5%) | 4080 (21.8%) | 0.042 |
| IVUS Use | 1854 (9.9%) | 1760 (9.4%) | 1721 (9.2%) | 1607 (8.6%) | 1348 (7.2%) | <0.0001 |
| DES use | 17060 (91.1%) | 17001 (90.8%) | 16912 (90.4%) | 16760 (89.7%) | 16827 (89.9%) | <0.0001 |
| GP IIb/IIIa inhibitor | 4700 (25.1%) | 4999 (26.7%) | 5145 (27.5%) | 5213 (27.9%) | 5634 (30.1%) | <0.0001 |
| Procedural Success | 18259 (97.5%) | 18237 (97.4%) | 18259 (97.6%) | 18217 (97.5%) | 18237 (97.4%) | 0.215 |
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | p Value | |
|---|---|---|---|---|---|---|
| (n = 18,727) | (n = 18,724) | (n = 18,708) | (n = 18,684) | (n = 18,717) | ||
| MACE | ||||||
| Death | 206 (1.1%) | 243 (1.3%) | 243 (1.3%) | 280 (1.5%) | 299 (1.6%) | 0.048 |
| Q wave MI | 75 (0.4%) | 56 (0.3%) | 94 (0.5%) | 75 (0.4%) | 94 (0.5%) | 0.105 |
| Re-Intervention PCI | 97 (0.5%) | 94 (0.5%) | 75 (0.4%) | 56 (0.3%) | 75 (0.4%) | 0.089 |
| CVA | 19 (0.1%) | 19 (0.1%) | 0 (0.0%) | 19 (0.1%) | 19 (0.1%) | 0.125 |
| Elective CABG | 37 (0.2%) | 19 (0.1%) | 19 (0.1%) | 19 (0.1%) | 19 (0.1%) | 0.101 |
| Emergency CABG | 19 (0.1%) | 19 (0.1%) | 19 (0.1%) | 19 (0.1%) | 19 (0.1%) | 0.201 |
| Bleeding | 150 (0.8%) | 169 (0.9%) | 150 (0.8%) | 131 (0.7%) | 112 (0.6%) | 0.027 |
| Variable | Comparator | Age-adjusted HR | 95%CI |
|---|---|---|---|
| Age | Age | 1.076 | 1.074-1.078 |
| Female | Male | 0.770 | 0.644-1.197 |
| Ethnicity (Asian) | Caucasian | 1.182 | 0.945-1.220 |
| Cardiogenic Shock | No Cardiogenic Shock | 4.643 | 4.329-4.981 |
| Smoking History | No Smoking History | 1.036 | 0.997-1.076 |
| Diabetic | Non diabetic | 1.528 | 1.473-1.586 |
| Previous MI | No previous MI | 1.492 | 0.839-1.546 |
| Previous PCI | No previous PCI | 1.106 | 0.765-1.149 |
| Previous CABG | No previous CABG | 1.666 | 0.992-1.744 |
| Hypertension | No hypertension | 1.403 | 1.354-1.453 |
| Hypercholesterolaemia | No hypercholesterolaemia | 1.013 | 0.957-1.049 |
| Previous CVA | No previous CVA | 2.887 | 1.935-4.309 |
| Peripheral vascular disease | No peripheral vascular disease | 2.934 | 2.750-3.131 |
| eGFR <60 ml/min/1.73m2 | eGFR > 60 | 2.605 | 2.215-3.064 |
| EF < 35% | EF > 35% | 2.179 | 2.042-2.325 |
| GP IIb/IIIa inhibitor use | No GP IIb/IIIa inhibitor use | 0.905 | 0872-0.940 |
| Procedural success | Procedural failure | 0.626 | 0.583-0.673 |
| Access route (Radial) | Femoral | 0.880 | 0.844-0.917 |
| Acute Coronary Syndrome | Elective Procedure | 1.209 | 1.164-1.255 |
| Chronic total occlusions | No chronic total occlusions | 1.043 | 0.987-1.103 |
| Drug-eluting stent use | Bare metal stent use | 0.773 | 0.735-0.812 |
| Multivessel disease | Single vessel disease | 1.428 | 1.380-1.478 |
| Socio-economic status | 1.001 | 1.000-1.012 | |
| Socio-economic quintile 2 | Socio-economic quintile 1 | 1.315 | 1.135-1.523 |
| Socio-economic quintile 3 | Socio-economic quintile 1 | 1.236 | 1.017-1.502 |
| Socio-economic quintile 4 | Socio-economic quintile 1 | 1.260 | 1.054-1.664 |
| Socio-economic quintile 5 | Socio-economic quintile 1 | 1.367 | 1.177-2.130 |
| Variable | Comparator | Age-adjusted HR | 95%CI |
|---|---|---|---|
| Socio-economic status | 1.001 | 1.000-1.002 | |
| Socio-economic quintile 2 | Socio-economic quintile 1 | 1.080 | 1.023-1.140 |
| Socio-economic quintile 3 | Socio-economic quintile 1 | 1.089 | 1.017-1.167 |
| Socio-economic quintile 4 | Socio-economic quintile 1 | 1.124 | 1.021-1.237 |
| Socio-economic quintile 5 | Socio-economic quintile 1 | 1.130 | 1.070-1.316 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





