1. Introduction
Cancer is a leading cause of death worldwide, accounting for nearly 10 million deaths in 2020, or nearly one in six deaths [
1]. Melanoma remains a highly malignant type of skin cancer. While less common than basal cell carcinoma (BCC) or squamous cell carcinoma (SCC), melanoma is more dangerous because of its ability to metastasize to other organs more rapidly if it is not treated early [
2]. Furthermore, advanced cutaneous melanoma tends to metastasize to the brain frequently with dismal prognosis [
3].
Radiotherapy is used to treat benign and malignant diseases, and it can be used separately or in combination with immunotherapy, chemotherapy, and surgery. Therapeutic radiation is mostly delivered as low linear energy transfer (LET) photon based radiation termed External Beam Radiation Therapy (EBRT). EBRT therapy is an important treatment for cancer patients, with 50% of patients receiving radiation therapy during their illness, and it is considered to contribute to 40% of the cure of cancer [
4]. External radiation may also use high LET particle-based radiation. The use of high energy protons or heavy ions from different sources (e.g. radionuclides) to the malignant area, can cause more damage than photon-based radiotherapy [
5]. Radiotherapy can also be delivered by placing radioactive sources near or inside the tumor, known as brachytherapy, which allows a higher total dose of radiation than the external beam treatment [
6]. One of the advantages of brachytherapy as compared to EBRT in treating cancer patients is delivering an ablative radiation dose over a short period of time directly to the tumor tissue while sparing the adjacent organs. This method gave brachytherapy a status of standard therapy for a broad spectrum of malignancies [
7].
High-LET alpha-particles interact by coulombic repulsion with the electrons present in the atoms of the target, leading to either excitation or ionization of matter. As the weight of the alpha-particle is very high compared to the weight of an electron, it is not deflected, and the track of the particle is almost linear. The path length in biological material of an alpha particle possessing a LET of about 100 keV/µm is of several cell diameters [
8]. High-LET radiations are known to have greater biological effectiveness per unit dose than those of low-LET, in a wide variety of biological effects [
9]. The signature of high-LET radiations, such as alpha radiation, is the formation of complex DNA damage that comprises of closely spaced DNA lesions forming a cluster of DNA damage [double strand breaks (DSBs) and non-DSB oxidative clustered DNA lesions (OCDL)] [
10,
11,
12]. Theoretical analysis and experimental evidence suggest an increased complexity and severity of complex DNA damage with increasing LET and high mutagenic or carcinogenic potential [
13]. The ‘idea’ of clustered DNA damage was introduced by Milligan [
14] as multiple local damaged sites, i.e., several closely spaced lesions within a short DNA segment [
15]. The radiobiological advantages of alpha particles include short range (typically 30-90 μm), high-LET (for 5,000-8000 keV alpha) [
16] and independence of dose rate, cell cycle during irradiation and oxygen effects [
17]. Unlike photons and beta particles, which are characterized by a low LET and considerable range in the tissue (millimeters for beta particles, centimeters for photons), a single alpha particle hit to the nucleus has a 20-40% probability of killing the cell and only a few hits are required to ensure cell lethality, mostly due to double strand breaks caused to the DNA molecule of the cell by the particle [
18,
19,
20,
21,
22]. Soyland and Hassfjell [
23] provided evidence that particle hits in the cytoplasm did not significantly affect cell survival.
Alpha particle radiation although highly destructive for tumor cells is not used in EBRT due to its short range in tissue and is currently used as a radiopharmaceutical such as Xofigo (Ra-223).
Our laboratories developed an innovative intra-tumoral radiation (brachytherapy) tumor ablation method, known as
Diffusing alpha-emitters Radiation Therapy (Alpha DaRT). The principle of this technology is to introduce into the tumor an array of implantable metal sources that are coated with a low activity of radium-224 (3.7 days half-life). These sources emits by recoil into the tumor Ra-224 daughter atoms that spread inside the tumor by diffusion and convection (vascular and interstitial) over several millimeters around it [
24,
25,
26]. These atoms release alpha particles, causing intensive tumor tissue damage. The extent of radioactive atoms spread in the tumor may be affected by several characteristics, such as, the tumor tissue compactness, disposal of radioactive atoms by the vasculature in the tumor, and cells sensitivity to radiation. There are several beneficial aspects of using alpha particle radiation as treatment against tumor cells: The short range in tissue alpha particles travel is < 100 µm, which keeps most of the radiation inside the tumor, reducing the risk to surroundings tissues and the treating staff; Alpha particles can cause mostly double strand breaks in the DNA in oxygen low environments; Studies showed that only a few hits to the nucleus are required for reproductive cell death [
27]. This treatment modality (alpha DaRT) was already used for the treatment of patients with squamous cell carcinoma with excellent results [
28,
29].
Melanoma is the most common cause of skin-cancer related death [
30]. While surgery remains the main treatment for early, localized melanoma, stage III and IV melanoma require additional systemic therapies, such as
BRAF-targeted and MEK-targeted therapies and checkpoint immunotherapy [
31]
.
Indications of radiotherapy are currently reduced, since melanoma is traditionally considered relatively resistant to conventional photon radiotherapy [
32,
33]
.
The major aim of this study was to investigate the cytotoxic effect of alpha particle radiation on four human-derived melanoma cell lines in vitro and compare and analyze several cell parameters which might affect sensitivity/resistance to alpha radiation. It was also investigated how melanoma derived cells compare to another skin derived tumor, i.e. squamous cell carcinoma (SCC) derived cells.
Firstly, to see the response of human melanoma cells to alpha radiation, and secondly to learn about the variance in response within a group of cells from the same histotype, and thirdly to determine cell characteristics which might correlate with sensitivity/resistance of melanoma cells to alpha radiation. To the best of our knowledge, similar studies of this kind assessing the biological effect of alpha radiation on a battery of human melanoma were not yet reported in the literature.
1.1. Study Aims
The main goal of this study was to investigate the effect of alpha particle radiation on a battery of human derived cutaneous melanoma cell lines and their brain metastatic derivatives.
1.2. Specific Aims
Investigate the direct effect of alpha particle radiation on four cutaneous lines of human derived melanoma and their brain metastatic derivatives.
Look for variations among the variants’ cytotoxic effect.
Compare the response of melanoma cells to alpha radiation to that of squamous cell carcinoma cells.
Investigate the correlation between the cytotoxic effect of alpha radiation and the formation of double strand breaks.
Investigate the correlation between the cytotoxic effect of alpha radiation and the average size of cell nuclei.
Compare the sensitivity of melanoma cells to alpha radiation with their sensitivity to photon radiation (gamma radiation).
Investigate DNA double strand breaks inflicted by alpha radiation in combination with modifiers of DNA repair mechanisms, to enhance cell mortality, such as ATR inhibitors (berzosertib) and topoisomerase 1 inhibitor (irinotecan).
Investigate the cytotoxic effect of alpha radiation on synchronized cell culture after serum starvation to determine the significance of the cell cycle.
2. Materials and Methods
2.1. Cell Lines
Four cutaneous human derived melanoma cells – YDFR.C, DP.C, M12.C, M16.C (C – for cutaneous) and their brain metastatic derivatives, which were obtained from murine models (CB3/CB2 – for brain metastasis).
The development, culturing and maintenance of human cutaneous melanoma variants YDFR.C and DP.C and human MBM variants YDFR.CB3 and DP.CB2 were previously described [
34].
YDFR.C parental cells were kindly provided by Prof. Michael Micksche (Department of Applied and Experimental Oncology, Vienna University, Austria). DP-0574-Me (DP), UCLA-SO-M12 (M12) and UCLA-SO-M16 (M16) were kindly provided by Dr. Dave S.B. Hoon (Department of Translational Molecular Medicine, John Wayne Cancer Institute, Saint John’s Health Center Providence Health Systems, Santa Monica, CA, USA).
The cells were grown in RPMI-1640 medium supplemented with 10% heat-inactivated fetal calf serum (FCS), 2 mmol/ml l-glutamine, 0.01 M HEPES buffered saline, 100 units/ml penicillin, 0.1 mg/ml streptomycin, and 12.5 units/ml nystatin. All cells were routinely cultured in humidified air with 5% CO2 at 37 °C.
The identity of all cell lines used was authenticated using STR.
2.2. Cell Growth Curves
To determine the rate of division of our cell lines, melanoma cells were seeded in 96 wells plates for several periods of incubation. Each well contained 7,000 cells at the beginning. After each period of incubation, cells were fixed with 100% methanol and stained with Hemacolor reagents Color was then extracted with 0.5% of SDS solution and OD measurements were obtained in Emax plate reader [
35].
Division rate of YDFR.C, DP.C, and M12.C was approximately 48 hours and M16.C was approximately 24 hours.
2.3. In Vitro Irradiation with Alpha Particles Using an 241Americium (Am-241) Irradiator
2.3.1. In Vitro Irradiation Apparatus
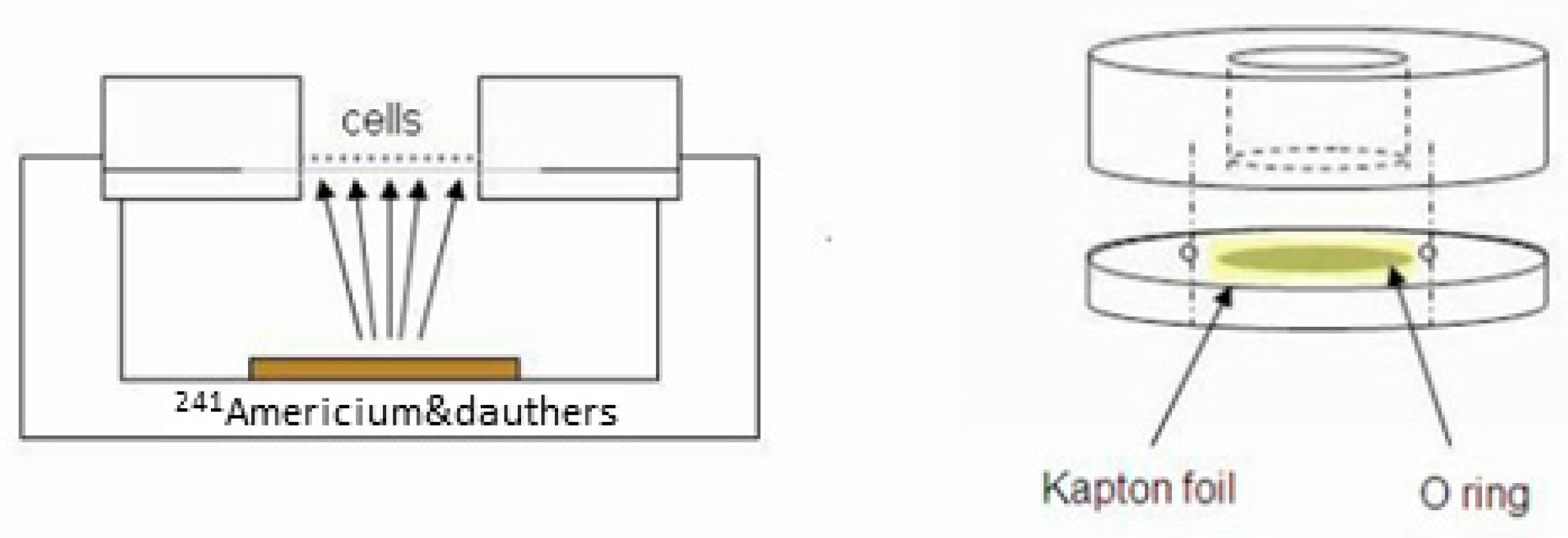
The in vitro irradiation setup (drawn schematically in
Figure 1) consists of an alpha particle source, containing Am-241 (half-life of 432.2 years) in equilibrium with its radioactive daughters [3.8-μCi (140 kBq)]. The Am-241 source, which, due to partial screening, had an alpha emission rate of 50 ± 2.5 kHz. The source irradiates cells seeded on a 7.5-μm thick Kapton foil (polyamide film PRN-IF70, Pornat, Israel), which is thin enough to allow the alpha particles emitted from the source to reach the cells on its other side. The foil is held by an O-ring between two cylindrical stainless-steel parts, forming a well with an inner diameter of 9 mm in which the cells are seeded in culture medium as previously described [
36]. During irradiation, the assembled well is positioned above the alpha particle source, so that the vertical distance between the source and the Kapton foil is 9.8 mm. Thus, the cells are exposed to a controlled flux of alpha particles, at an average dose rate of 0.25 Gy/min. The dose rate was estimated by measuring the spectrum and emission rate of alpha particles from the Am-241 source with an alpha-particle spectrometry system, supplemented by a Monte Carlo simulation of the full setup, using a dedicated MATLAB script utilizing SRIM 2013 [
37]. The calculated mean alpha-particle energy, when passing through the cell layer, was 2.7 MeV, with an LET of 130 ± 3 keV/μm (where the variations reflect the radial position across the foil).
2.3.2. Alpha Radiation In-Vitro Procedure
Four cutaneous human derived melanoma lines and their brain metastatic derivatives were grown in cell culture dishes (corning) in RPMI 1640 Medium (Gibbco), containing 5% FBS, 1% PSN, 1% l-Glutamine until reaching sufficient confluency for seeding in the radiation cell holders.
Cells were harvested with 2 ml trypsin, incubated for 3 minutes, and then neutralized with 2 ml medium. Cells were centrifuged at 1200 RPM for 5 minutes; supernatant was aspirated, and the pellet was mixed with 3 ml medium. Cell concentration was adjusted to 60,000 cells/ml. Radiation cell holders were assembled with Kapton film (irradiation cell holder), washed with ethanol 70% and left to dry out.
Cells were seeded on Kapton in the radiation cell holders, 300 μl per cell holder (18,000 cells per 300 μl) and incubated for 48 hours. After 48 hours of incubation, cells were irradiated and harvested for the viability assay procedure. Cells were seeded in 24 wells plates and left for 5 days of incubation. Each experiment was divided into 5 groups of radiation periods (2 wells per radiation group) as follows: (1) 0 Gy (Control), (2) 0.35 Gy (3.45 minutes), (3) 0.7 Gy (7.5 minutes), (4) 1.4 Gy (15 minutes), (5) 2.8 Gy (30 minutes).
The same procedure was conducted for the CAL 27 cell line, with an exemption of the culture medium. Cells were cultured with DMEM medium (Gibbco) containing 5% FBS, 1% PSN.
2.4. Colorimetric (HemaColor) Viability Assay
The human melanoma cell variants do not form colonies after seeding in plates, and to test cell viability and multiplication after radiation we used the HemaColor colorimetric assay [
35]. After irradiation, 10,000 cells were harvested from the Kapton, centrifuged, counted and seeded in 24 well plates and incubated for up to 5 days. When non-irradiated cells (control) reached 90-100% confluency, incubation was stopped and cell monolayers in all the wells stained with HemaColor reagents (Sigma-Aldrich) as described. After staining plates were rinsed with tap water three times and filled again with water for decolorization for 5 minutes. Plates than left to dry and the color was extracted with 0.7 ml/well of color extraction solution containing 0.5% sodium dodecyl sulfate (SDS) in double distilled water (DDW) for 90 minutes. Three aliquots of 200 µl were removed from each 24 well and added to a 96 wells plate respectively for each group of treatment and respectively for each cell line. Plates were read at 595 nm wavelength in an Emax spectrophotometer reader. The colorimetric assay was repeated 3-5 for each cell line.
2.5. Exposure of Melanoma Cells to γ-Radiation
Melanoma cells were seeded in 24-wells plates (20,000 cells/0.5 ml per well). Cells left for 24 hours to adhere. After 24 hours, cells were irradiated with gamma radiation (BIOBEAM Gamma Irradiator provided by TAU SCIF) with doses of 0, 0.3,0.7,1.4,2.8,4.2,5.6 Gy and left for incubation until control plate (0 Gy) reached full confluency. Cells then were stained with HemaColor reagents and photographed with light microscope. Furthermore, color was extracted as described and triplicates of 200 µl samples for each cell line per radiation doses were transferred into 96 wells plate and optical density was read with an Emax spectrophotometer with wavelength of 595 nm. Data was collected and analyzed manually with Excel. Alpha radiation viability percentage data of our four cell lines from was compared to the extracted data of gamma radiation.
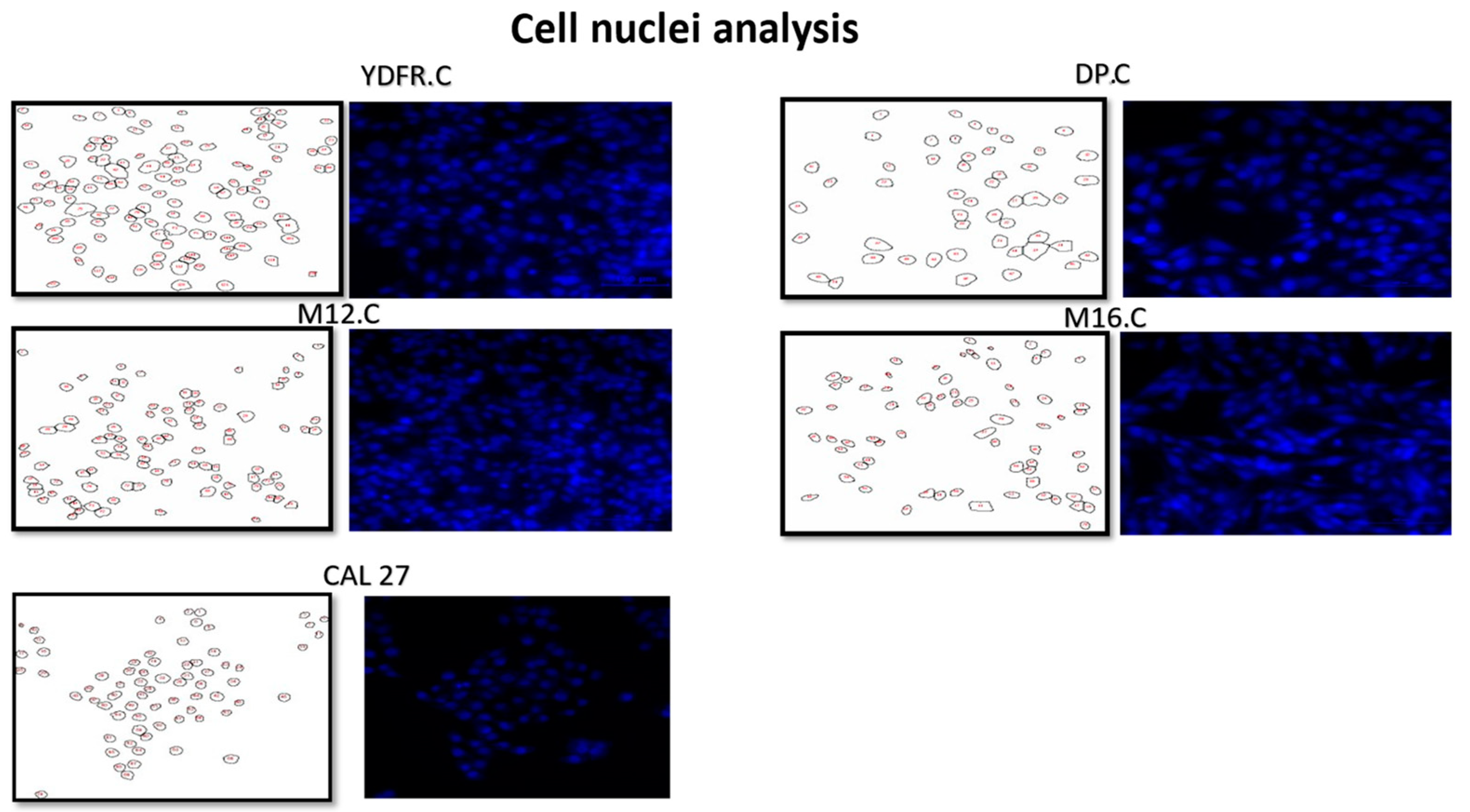
2.6. Cell Nuclei Analysis
Four melanoma cell lines and CAL 27 were incubated in 96 well plates for 24 hours. After 24 hours, medium was removed, and cells were fixed with 4% Paraformaldehyde for 10 minutes. After fixation, wells were washed with PBS once and were incubated with DAPI (Sigma) for 5 minutes (dilution of 1:1000) after incubation with DAPI, wells were washed once with PBS and left to dry in the dark. Images were taken by a fluorescent microscope Nikon Eclipse TI with scale bar of 100 µm ratio. Images were than analyzed with ImageJ/FIJI (ImageJ open-source software) for measurement of the cell nucleus in each of our cell lines.
Average perimeter of the nucleus along with the standard deviation, cell radius, diameter and area were calculated manually with Excel. Comparisons of cutaneous cell lines were presented in radar plots to compare between cells. One way analysis of variance (ANOVA) test was conducted along with Tukey Honestly Significance Difference (HSD) post-hoc analysis on the derived perimeter of each cell variant.
2.7. Double Strand DNA Breaks Signaling
A distinctive marker of the effect of alpha particle radiation is consensually agreed to be double strand breaks (DSB) in the DNA. This breakage in the DNA activates DNA repair pathways. The phosphorylation of the histone gamma - H2Ax (γ-H2aX) and its binding to the DNA is an indicator of the damage to the nucleus [
38]. It has been stated that radioresistant cancers may have acquired an increased proliferative capacity and an upregulation in DNA repair pathways [
3]. To determine the degree of radio resistance/sensitivity in radiated cells, γ-H2aX foci may serve as a convenient comparative marker.
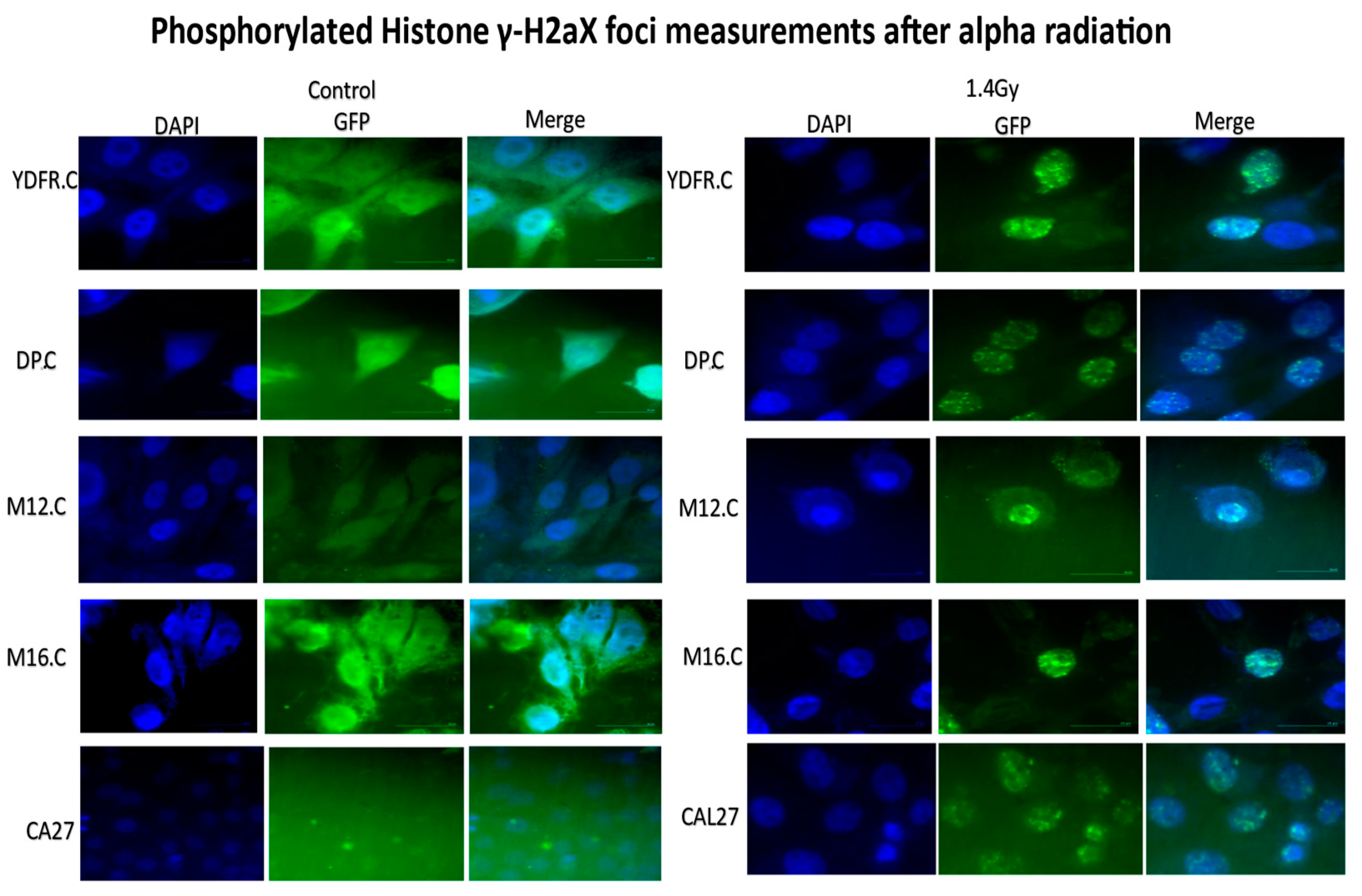
2.8. Immunofluorescence Assay of γ-H2aX Foci
For the immunofluorescence assay, primary Anti-phospho-Histone H2A.X (Ser139) antibody, clone JBW301 was purchased from Merck, Israel. Secondary antibody, Goat Anti-Mouse IgG H&L (Alexa Fluor® Abcam 488) was purchased from Zotal inc., Israel and DAPI reagent was purchased from Sigma. Pictures were taken using a fluorescent microscope Nikon Eclipse TI.
Four human derived melanoma cell lines and CAL 27 cells were seeded on Kapton in the irradiation apparatus at a concentration of 40,000 cells/0.5 ml in each radiation cell holder and left to adhere for 24 hours. After 24 hours, cells were irradiated with 1.4 Gy of alpha radiation (15 minutes of irradiation period). Culture Medium was removed, and cells were fixed with 4% para formaldehyde in PBS (Sigma) for 12 minutes. After fixation, a circular area of kapton, with fixed cells, was cut by a needle, and placed on stretched parafilm paper in 24 well plates. After fixation, cells were washed with PBS three times for 5 minutes each. Cells were then permeabilized with 0.5% triton -X solution in PBS for 10 minutes and washed twice in PBS. For blocking, cells were treated with 10% FBS in PBS solution for 2 hours. Primary antibody diluted 1:250 in blocking solution was added to the cells and left overnight at 40C. after primary antibody was removed, cells were washed with PBS three times, for five minutes each. Secondary antibody diluted 1:200 in PBS was added to the cells and left for 0.5 hour at RT in the dark. After secondary antibody was removed, cells were washed once with PBS for 5 minutes and DAPI, diluted 1:1000 in DDW was added. After DAPI was removed, cells were rinsed with PBS and the circular foils were mounted on glass slides and coverslip and left to dry overnight. Photos were taken and foci were counted manually with ImageJ.
One way analysis of variance (ANOVA) test was conducted along with Tukey HSD post-hoc analysis.
2.9. Viability Assay: D50 Measurements
The D50 calculation is the measure of the radiation dose needed for 50% cytotoxicity/viability for each cell variant. The D50 value was used to compare the relative sensitivity to radiation of the different cells.
The value of D50 was calculated with the linear line formula that was given by the manual calculations of the converted viability percentage.
As data were extracted from the spectrophotometric measurements of remaining cells after radiation. One way analysis of variance (ANOVA) test was conducted along with Fisher’s Least Significant Differences (LSD) post hoc analysis (α=0.05). To compare our variants statistically, we define the dependent variable in the ANOVA test as D50.
2.10. Serum Starvation and Alpha Radiation
Chromatin structure was suggested to affect the extent of DNA damage and repair after ionizing radiation. Although the effects of chromatin structure on the damage are not fully understood several mechanisms have been proposed. Chromatin condensation may have a protective effect against radiation damage. Thus, it was shown that tightly packed chromatin (heterochromatin) is more resistant to DSB in the DNA after ionizing radiation and that dividing cells are more sensitive to photon radiation [
40].
It was suggested that synchronized cell culture induced by serum starvation can induce chromatin condensation in the G0/G1 phase of the cell cycle [
41]. Thus, our intent was to investigate the effect of alpha radiation after serum starvation in a synchronized cell culture.
3. Results
3.1. Sensitivity of Melanoma Cell Lines and Their Brain Metastatic Variants to Alpha Radiation
Alpha particle radiation potential as a cytotoxic agent against human derived tumors was discussed in the literature and reported in previous work from our laboratory [
27,
36,
42,
43,
44]. In this study, we investigated the cytotoxic effect of alpha radiation on human derived melanoma cell variants in vitro. It has been stated that melanoma is a type of skin cancer that is relatively resistant to conventional radiotherapy (photon radiation) in vitro [
45].
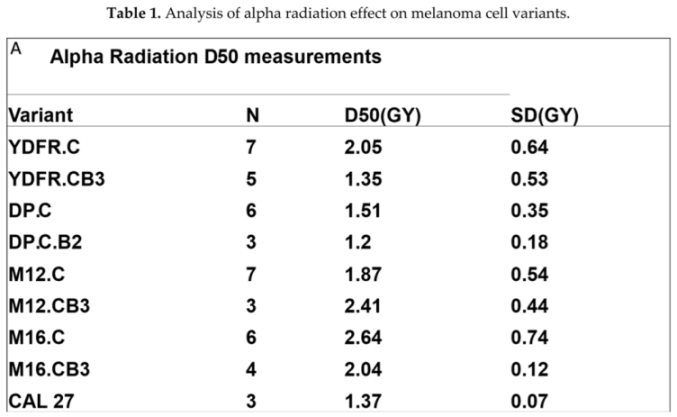
Four cell lines of human derived cutaneous melanoma and their brain metastatic derivatives were irradiated with alpha-particle fluxes in vitro (
Figure 1). The exposure to ongoing doses of alpha radiation revealed that our cell variants were sensitive to the cytotoxic effect of alpha radiation. HemaColor viability assays showed 54%-71% of cytotoxicity at the highest dose (2.8 Gy) of alpha radiation. Comparison of the sufficient dose for killing 50% of cells (D50), using an analysis of variance (ANOVA) test, showed an inter–variant variance among our melanoma cell lines. Furthermore, Tukey HSD post-hoc analysis showed significant inter-variant variance between the cell lines DP.C (the most sensitive, D50=1.51±0.51 Gy) to M16.C (the most resistant, D50 = 2.64±0.74 Gy), and non-significant, yet considerable variance between the cell lines YDFR.C (D50 = 2.05±0.64 Gy) and DP.C to M12.C (D50 = 1.87±0.54 Gy). The brain metastatic variants showed sensitivity very similar to their skin parent cell (Table 1). According to the post - hoc analysis, we continued our research on the cutaneous cell lines, trying to reveal properties of cell biology that may be correlated with this variance.
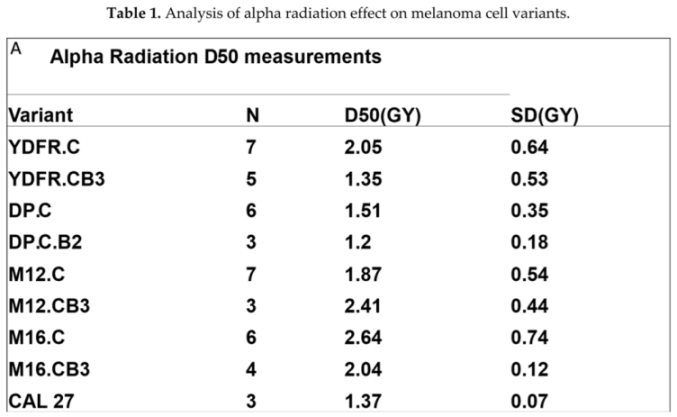
Four cutaneous cell variants and their brain metastatic derivatives were irradiated with ongoing doses of alpha radiation (0-2.8 Gy). (A) summary of the D50 measurement for 50% cell viability/Cytotoxicity for each cell variant with the SD and the number of viability assay repetitions for each cell variant(N). To obtain D50, viability percentages were converted to log10 scale, and the D50 was calculated with linear line formula. ANOVA test showed significant variance (P=0.0126) between all cell lines. Post – Hoc analysis showed significant variance between YDFR.C and DP.C to M12.C (YDFR.C:M12.C, P=0.019; DP.C:M12.C, P=0.029), non-significant yet considerable variance between variants YDFR.C and DP.C to M16.C (YDFR.C:M12.C, P=0.056; DP.C:M16.C, P=0.076) and no variance between YDFR.C:DP.C, (P=0.976) and M12.C:M16.C (P=0.637).
3.2. Comparison of Melanoma Cells with Squamous Cell Carcinoma Cells
The results indicated a variable response to alpha radiation differing between the cell lines. It was interesting to compare the response of the melanoma cells to another skin derived tumor such as squamous cell carcinoma, and the CAL 27 cell line (SCC of the tongue) was used. CAL 27 was irradiated and tested with the same procedure of cell viability assays. D50 measurements and comparison to the cutaneous melanoma cells revealed that CAL 27 was more sensitive (D50=1.37+/-0.07 Gy) than the most sensitive melanoma cell DP.C (Table 1).
3.3. Morphology of the Cell Nucleus as a Determinant of the Cytotoxic Effect of Alpha Particle Radiation
Cells exposed to alpha particles are subjected to a stochastic number of alpha particle traversals through their nuclei. Cell survival studies suggested that only a few numbers of hits in the nucleus are required to induce a lethal effect. Moreover, alpha particles that hit the cytoplasm do not significantly affect cell survival [
23,
46]. Different cell types are characterized by different nuclear morphology in general and with nuclear area in particular, and it was previously shown by Lazarov et al [
27] that there is a correlation between the number of hits of alpha particles and the nuclear area of cells. Thus, the nuclear morphology of human derived melanoma cell variants was assessed and related to the differences in the cytotoxic effect of alpha radiation on these cells and on SCC.
Nuclear area of cell lines was determined by immunohistochemistry assay where nuclei were stained with DAPI. After staining with DAPI, photos were taken with Nikon eclipse TI fluorescent microscope, scale bar- 100 µM and analyzed the photos with ImageJ/FIJI software (
Figure 2).
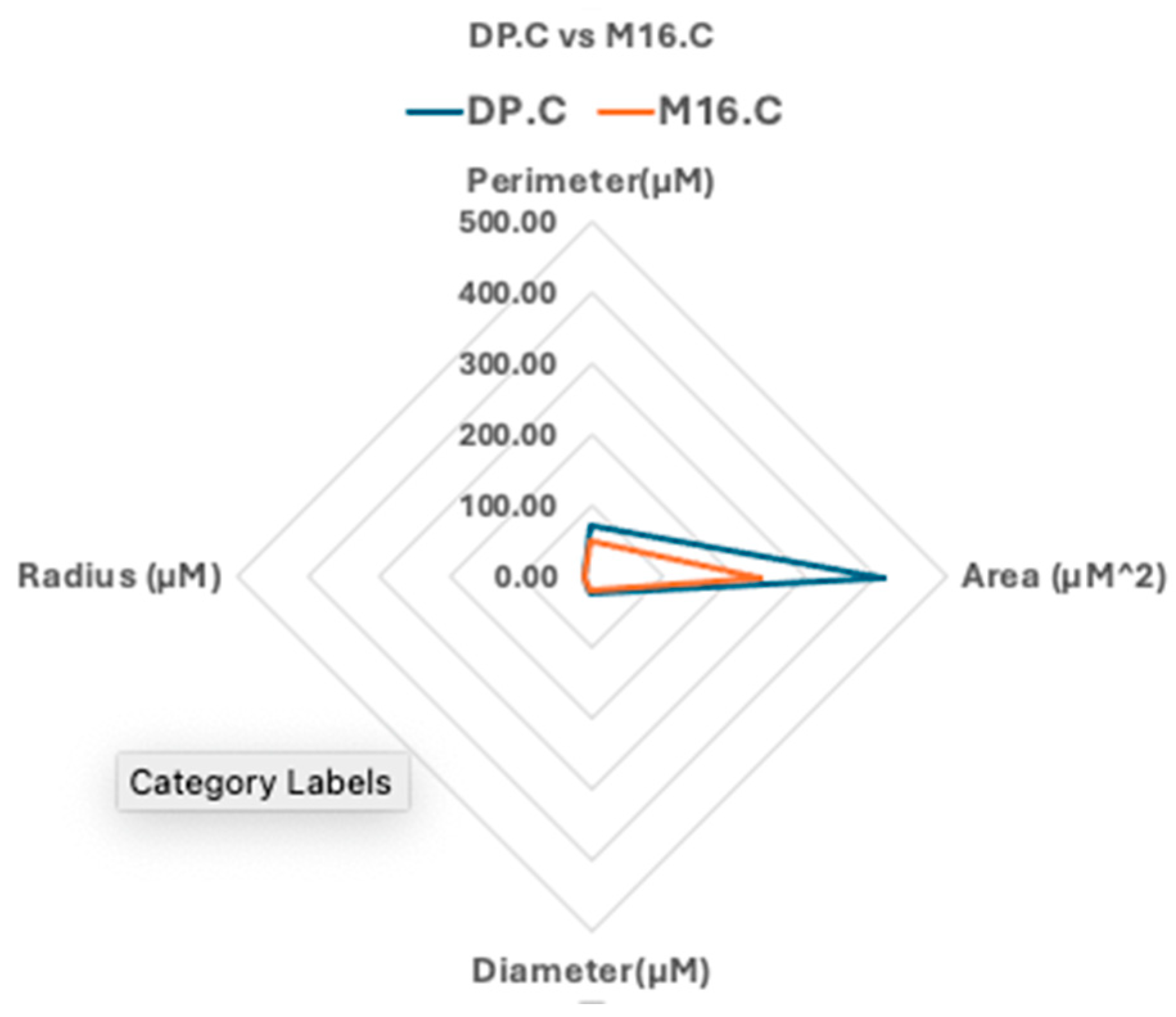
As seen in Table 2, the mean perimeter of each cell line was calculated with the standard deviation and ANOVA test was conducted. Results showed a statistically significant difference between all four cell lines (P=2.00E-26) and post hoc analysis revealed strong significant differences between the pairs YDFR.C:M12.C (P<0.0001); YDFR.C:M16.C (P<0.0001); DP.C:M12.C (P<0.0001) and DP.C:M16.C (P<0.0001). No significance was shown between: YDFR.C:DP.C (P=0.33) and M12.C:M16.C (P=0.85). Other properties of nuclear morphology were calculated according to the derived radius and multi-parametric evaluation of the cell nucleus properties among pairs of cell variants are shown in spider web graphs. According to findings, the most sensitive cell (DP.C) had a larger nucleus compared to the least sensitive cell (M16.C) (
Figure 3). Nuclear area and morphology may be a macroscopic cause for the variance in cytotoxicity of alpha radiation on human derived cutaneous melanoma cell variants.

Mean cell nuclear morphology parameters of the cutaneous melanoma variants and the comparison to CAL 27. ANOVA test of the extracted perimeter of cutaneous cell variants revealed strong significance (P=2E-26) and HSD post hoc reveled significance between pairs of cell variants YDFR.C and DP.C to M12.C and M16.C. Two tailed T-test revealed significance (P<0.0001) between cutaneous melanoma cell lines to CAL 27 calculated nuclear area.
It is important to note that the squamous cell line, CAL 27, which was more sensitive than the most sensitive melanoma cell, DP.C, has a much smaller nucleus size, in the range of the more resistant melanoma cell M16.C (Table 2).
3.4. Exposure of Cells to Alpha Particle Caused DNA Double Strand Breaks (DSB) as Measured by γ-H2aX Foci
DSB in the DNA are one of the main causes for cell death after ionizing radiation [
47]. Thus, it was questioned whether more sensitive cells have more double strand breaks when compared to the more resistant cell lines.
Cutaneous melanoma cell lines and CAL 27 were irradiated with a dose of 1.4 Gy of alpha radiation and stained with the anti-phosphorylated histone γ-H2AX antibody (
Figure 4) and foci per cell were counted and analyzed using ImageJ/FIJI software. The numbers of DSB were 7.68+/-2.12 for YDFR.C, 9.61+/-2.3 for DP.C, 6.17+/-2.23 for M12.C and 6.9+/-1.65 for M16.C. ANOVA test for foci per cell per cell line with confidence interval of 95% showed significant variance between our cells (P=1.06E-8). Post – hoc analysis of the results revealed significant variance among pairs of cell variants: DP.C:M12.C (P=1E-8), DP.C:M16.C (P=5.64E-6), DP.C:YDFR.C (P=0.002), M12.C:YDFR.C (P=0.037). Yet, non-significant differences were obtained in the analysis: M12.C:M16.C (P=0.53) and M16.C:YDFR.C (P=0.49). Concluding the analysis results, the number of DSB in the DNA vary among human-derived cutaneous melanoma, and a higher number of DSB was observed in the more sensitive cell lines. It is interesting to note that the number of DSB in the CAL 27 (SCC) cell line (6.67+/-1.38) was low compared to the melanoma cells and in the range of the more resistant melanoma cells.
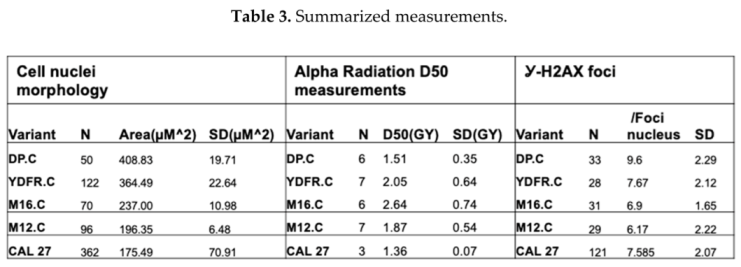
To compare and correlate the sensitivity to alpha radiation, the cell nuclei size and the DSB numbers in the melanoma cells, we include a summary table (Table 3). There is a direct correlation between sensitivity to radiation (D50), number of DSB and the size of the nucleus for the cell lines DP.C, YDFR.C and M16.C. The cells with the larger average nuclei size were observed with more DSB per cell and were more sensitive to alpha particles (lower radioactive dose is needed to kill them). The exception was cell line M12.C, which had the smallest cell size and the lowest number of DSB per cell but was not the most resistant cell line. The comparison of melanoma cells to the SCC cell line CAL 27, showed that this cell line had the smallest nucleus and low DSB but still it was the most sensitive cell.
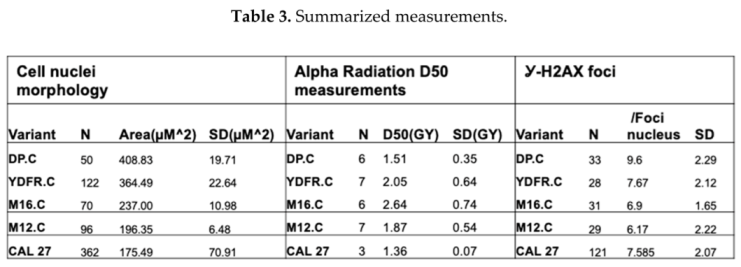
Summarized measurements of four cutaneous melanoma cell variants including the derived D50, nuclear perimeter and the calculated nuclear area according to the derived radius and the mean number of phosphorylated foci per cell variant after alpha radiation.
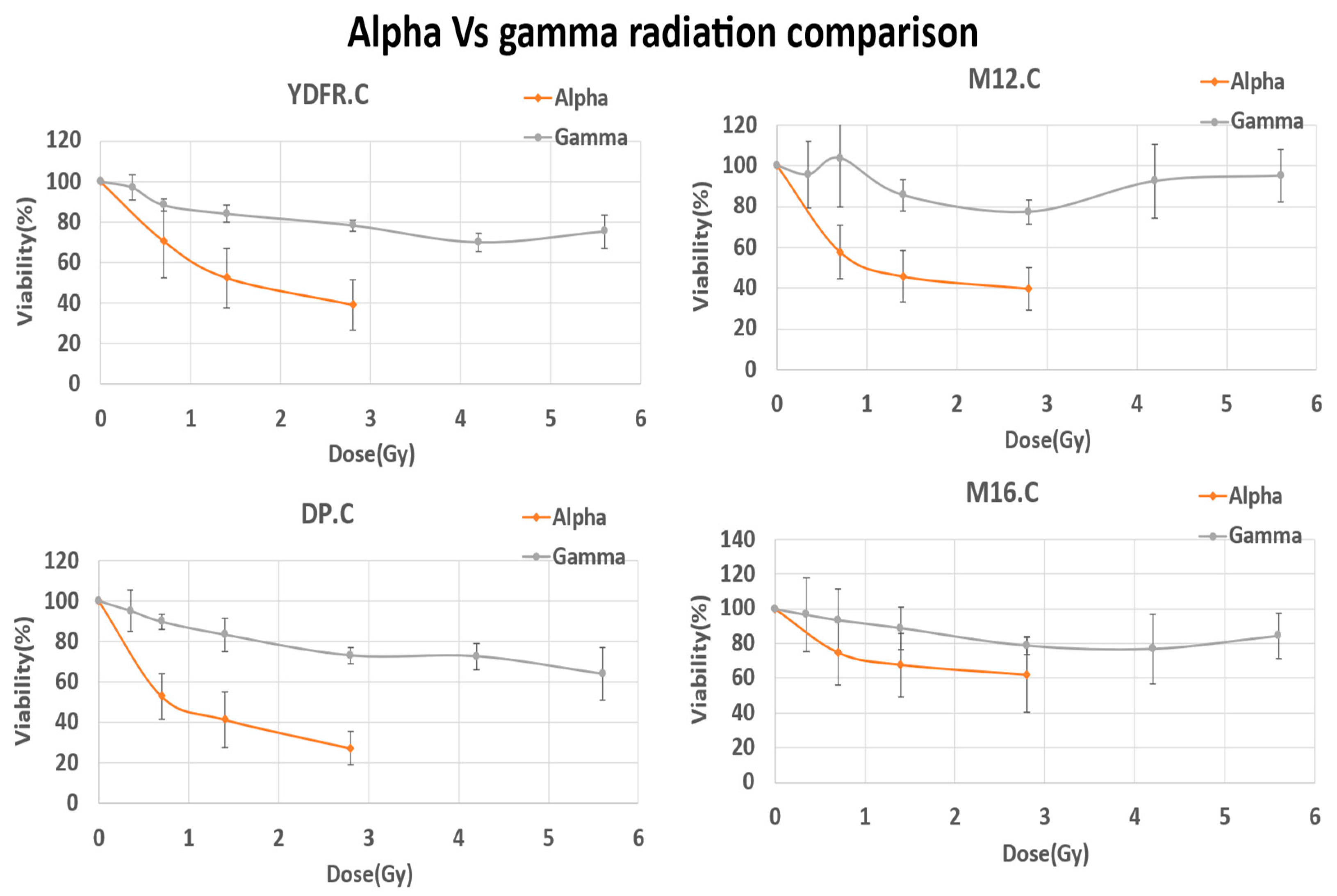
3.5. Alpha Radiation Is More Cytotoxic to Melanoma Cells in Comparison with Gamma Radiation
In a previous study it was observed that the alpha radiation is more lethal for human SCC (FaDU) and pancreatic carcinoma (Panc01) cells than X-rays [
27]. Thus, it was important to make this comparison for the four human melanoma cell lines. The cutaneous cell lines of human derived melanoma were seeded in 24- wells plates (20,000 cells/0.5 ml per well) and left for 24 hours to adhere. After 24 hours, cells were irradiated with gamma radiation (BIOBEAM 8000 Gamma Irradiator provided by TAU, SCIF) with doses of 0, 0.3,0.7,1.4,2.8,4.2,5.6 Gy and further incubated until the cells in the control plate (0 Gy) reached full confluency. Cell viability was assessed with Hemacolor viability assay.
Comparison of the cytotoxic effect of alpha radiation and gamma radiation (
Figure 8) showed that alpha radiation was significantly more cytotoxic than gamma, comparing all four cell lines (P<0.05). The use of higher radiation doses with gamma radiation highlighted alpha particle radiation efficiency destroying the notorious relatively resistant melanoma.
It is interesting to note that the cell line most sensitive to alpha radiation (DP.C) was also more sensitive to photon radiation.
Figure 5.
Effect of Alpha and gamma radiation on melanoma cells. Four cell variants of human derived melanoma were subjected to both alpha and gamma radiation with increasing doses. Percent viability was evaluated with colorimetric assays (HemaColor, N=3 for each variant). Alpha radiation (orange lines) achieved higher cytotoxicity levels than Gamma radiation (blue lines) at the same radiation doses. Paired T-test of the D50 measurements of alpha radiation to gamma suggest significance among all four cell variants (YDFR.C P=0.004, DP.C P=0.001, M12.C P=0.025, M16.C P=0.0063).
Figure 5.
Effect of Alpha and gamma radiation on melanoma cells. Four cell variants of human derived melanoma were subjected to both alpha and gamma radiation with increasing doses. Percent viability was evaluated with colorimetric assays (HemaColor, N=3 for each variant). Alpha radiation (orange lines) achieved higher cytotoxicity levels than Gamma radiation (blue lines) at the same radiation doses. Paired T-test of the D50 measurements of alpha radiation to gamma suggest significance among all four cell variants (YDFR.C P=0.004, DP.C P=0.001, M12.C P=0.025, M16.C P=0.0063).
3.6. Cell Cycle Synchronization and Proliferation Arrest Did Not Affect Cell Killing by Alpha Radiation
In this study serum starvation of cell cultures was used to induce cell cycle synchronization. Serum starved cells can undergo a shift in cell cycle by arresting normal proliferation and entering the G0/G1 phase. It has been suggested in the literature that serum starved cells can undergo chromatin condensation [Shin et al 2008]. Thus, we checked if proliferation arrest and chromatin condensation may affect the cytotoxic effect of alpha particle on irradiated melanoma cells.
3.7. Cell Cycle Analysis
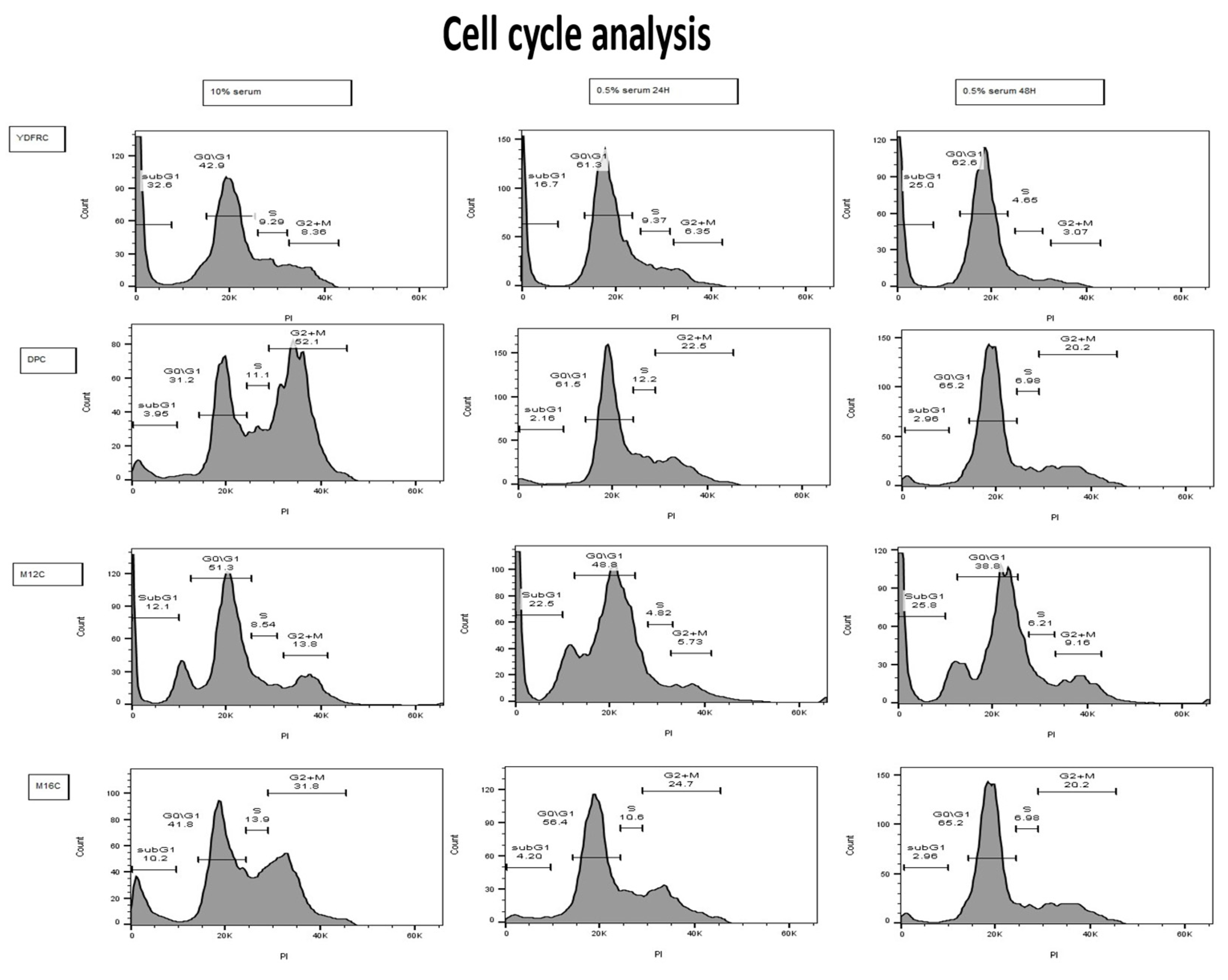
To determine if melanoma cell lines can undergo cell cycle arrest upon serum starvation, cells were seeded in wells, 100,000 cells per well, with RPMI-1640 medium containing 10% FBS serum, 1% PSN solution, and 1% of L-glutamine for 24 hours. After 24 hours, medium was replaced with RPMI -1640 medium (Gibbco) containing 0.5% FBS (Gibbco) serum (starvation medium) for 24 hours and 48 hours. After incubation in starvation serum medium, cells were harvested into 15 ml tubes and centrifuged for 5 minutes at 1200 RPM. Cells were fixed then with 70% ethanol and left at -200 C for 24 hours. Cells then were centrifuged in full medium and collected into FACS tubes in 300-400 mL of PBS (Sigma). Cells were stained with 5 mL of propidium iodide (Sigma) and analyzed in S1000EXi FACS flow cytometer (life science IDRFU).
FACS analysis of the four cell lines revealed coherent cell cycle arrest in three of the four cell variants. The effect was most pronounced in the DP.C cell line which exhibited the highest sensitivity to alpha radiation mediated killing (
Figure 6). As for the M12.C cell line, cell cycle analysis showed an elevation in the sub G1 phase which could imply to contribute to breakage of proliferation (N=6).
3.8. Effect of Cell Starvation on the Killing of Cells by Alpha Radiation
To evaluate the effectiveness of serum starvation on the enhancement of alpha radiation cytotoxicity, we first measured the multiplication rate of our cell lines to determine when to stop the incubation after the combined treatment. Cells were seeded in 96 wells plates for several periods of incubation. Each well contained 7,000 cells at the beginning. After each period of incubation, cells were fixed with 100% methanol and stained with Hemacolor regents. Color was then extracted with 0.5% of SDS solution and OD measurements were obtained in Emax plate reader.
After the determination of each cell line growth rate, the effect of starvation on cell death inflicted by alpha radiation combination treatment was determined. DP.C Cells, the most sensitive cutaneous melanoma, were seeded on Kapton in irradiation holders at a concentration of 20,000 cells per 200 mL for each Kapton and further incubated to adhere for 24 hours. Two groups were obtained: Alpha (treated with full medium) and full starvation pre radiation (S). After 24 hours medium was replaced respectively and left for another 24 hours incubation. Cells were than irradiated and seeded in 96 plate wells at a concentration of 10,000 cells per well and left for a time respectively to one division cycle (24-48 hours, depending on cell line).
Exposure of alpha radiation sensitive starved cells to alpha particles increased non significantly the level of cytotoxicity at the low level of radiation (0.7 Gy), from 12.5% to 29.65%, but not at higher radiation levels. This may indicate that lack of proliferation and probably chromatin condensation does not have a significant effect on alpha particle inflicted cell damage and death.
3.9. Combination Treatment with DNA Damage Repair Modifiers and Alpha Radiation
This part of the study was dedicated to find ways to enhance the cytotoxic effect of alpha radiation. Clinical approaches and literature suggested a combination of chemotherapy with radiation as a multi model approach for better killing malignant cells.
In this study we used two agents, the ATR inhibitor berzosertib, which interferes with the ability of the cells to detect DSB and thus promote cell death, and the topoisomerase I inhibitor, irinotecan, which eventually leads to the inhibition of both DNA replication and transcription.
3.9.1. Drug Calibration Curves
Melanoma cells were incubated until they reached sufficient confluency. Cells were seeded in 96 wells plates at a concentration of 25,000 cells/ml, each well contained 5,000 cells/200 µl and left to adhere for 24. After 24 hours of incubation, culture medium was removed, and berzosertib or irinotecan were added with increasing concentrations of the drug and further incubated for 72 hours.
After incubation, the drug was removed, and plates were stained with HemaColor reagents. Plates were photographed and color was extracted with 0.5% SDS solution in DDW. Plates were read with Emax spectrophotometer, and raw data was obtained and calculated manually with excel.
The results show that all four cell lines are sensitive to berzosertib and irinotecan.
Berzosertib killed fifty percent of DP.C at 356 nM, M12.C at 727 nM, YDFR.C at 953 nM and M16.C at 1012 nM. Irinotecan killed fifty percent of DP.C at 10.4 mM, M12.C at 13.3 mM, YDFR.C at 35.5 mM and M16.C at 8.84 mM. It is interesting to note that there is a difference in the response of the cells to each agent. The sensitivity of the cell lines to berzosertib did not match the sensitivity to irinotecan and was also different from their sensitivity to alpha radiation.
3.9.2. Combination Treatment with Alpha Radiation
Next, we examined if combination treatment with the drugs enhanced alpha radiation mediated killing. Combination treatment of the drugs and alpha radiation was performed with cells seeded in radiation holders upon Kapton (20,000 cells per 300 µl for each Kapton). Cells were left to adhere for 24 hours. After 24 hours Irinotecan or Berzosertib at sublethal concentrations were added respectively and left for another 24 hours incubation. Four groups were used: control (treated with full medium), and 3 concentrations of each berzosertib or irinotecan, according to the drug calibration curves stated earlier. Cells were than irradiated, harvested, and seeded in 24 plate wells at a concentration of 10,000 cells per well and left for incubation until control wells were confluent (approximately 5 days).
Combined treatment with berzosertib – Results of three repetitions of colorimetric viability assay for each cell line were collected and summarized. The results showed that melanoma cell lines had responded to the cytotoxic effect of the ATR inhibitor itself. Yet, the cytotoxic effect of alpha radiation (0.7, 1.4 and 2.8 Gy) was partially, non-significantly, enhanced by berzosertib at the range of 100, 300 and 500 nM.
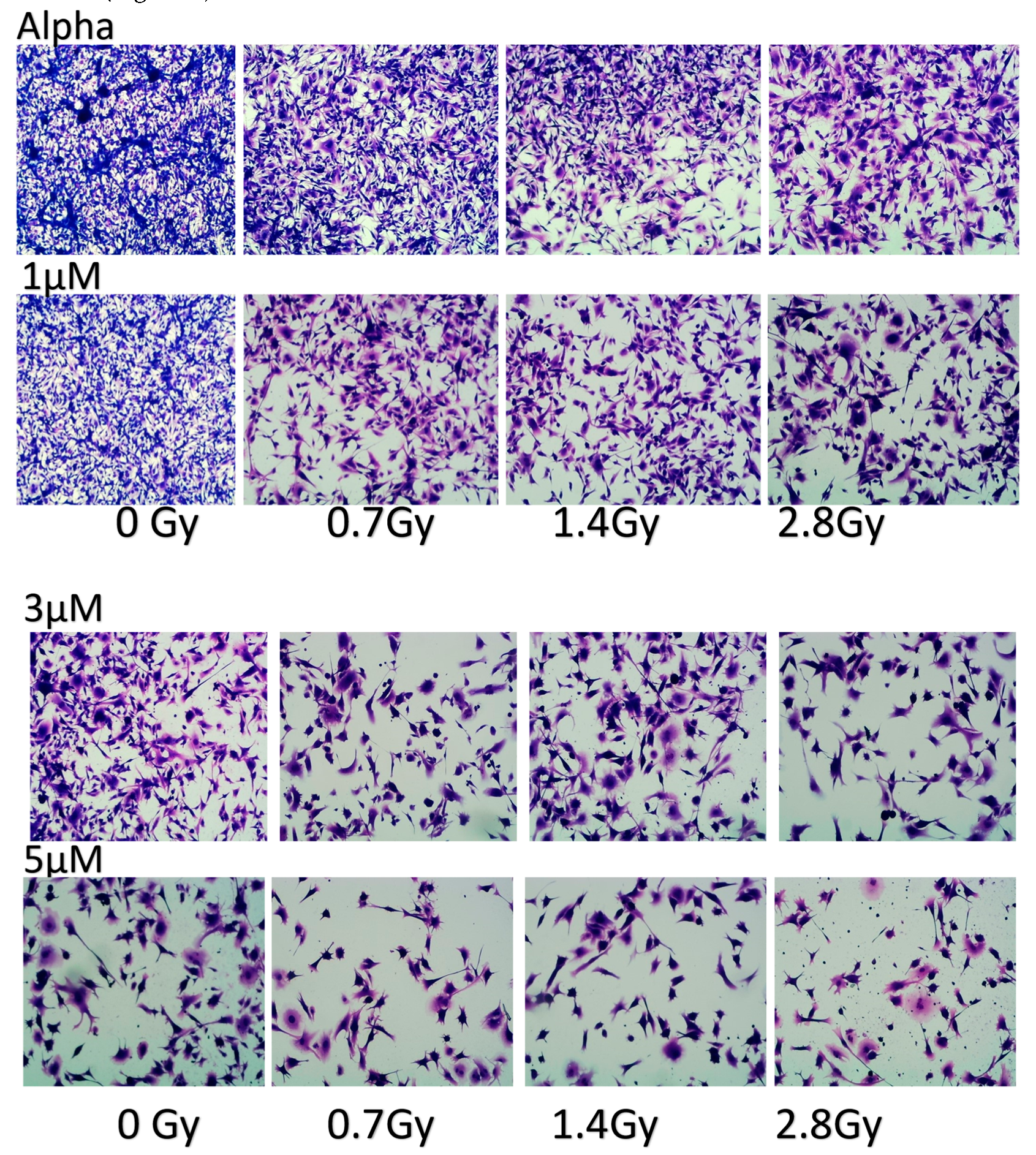
Combined treatment of alpha radiation with irinotecan – colorimetric viability assays with the YDFR.C cell line were performed and showed that low concentration of irinotecan (1 µM) significantly elevated the cytotoxic effect of 0.7 Gy alpha radiation from 20 to 40% (p=0.0233) and at 1.4 Gy cytotoxicity was increased from 38% to 55% (p=0.0008). Photos of the treated cells are presented in (
Figure 7).
3.10. Cell Death Kinetics Analysis
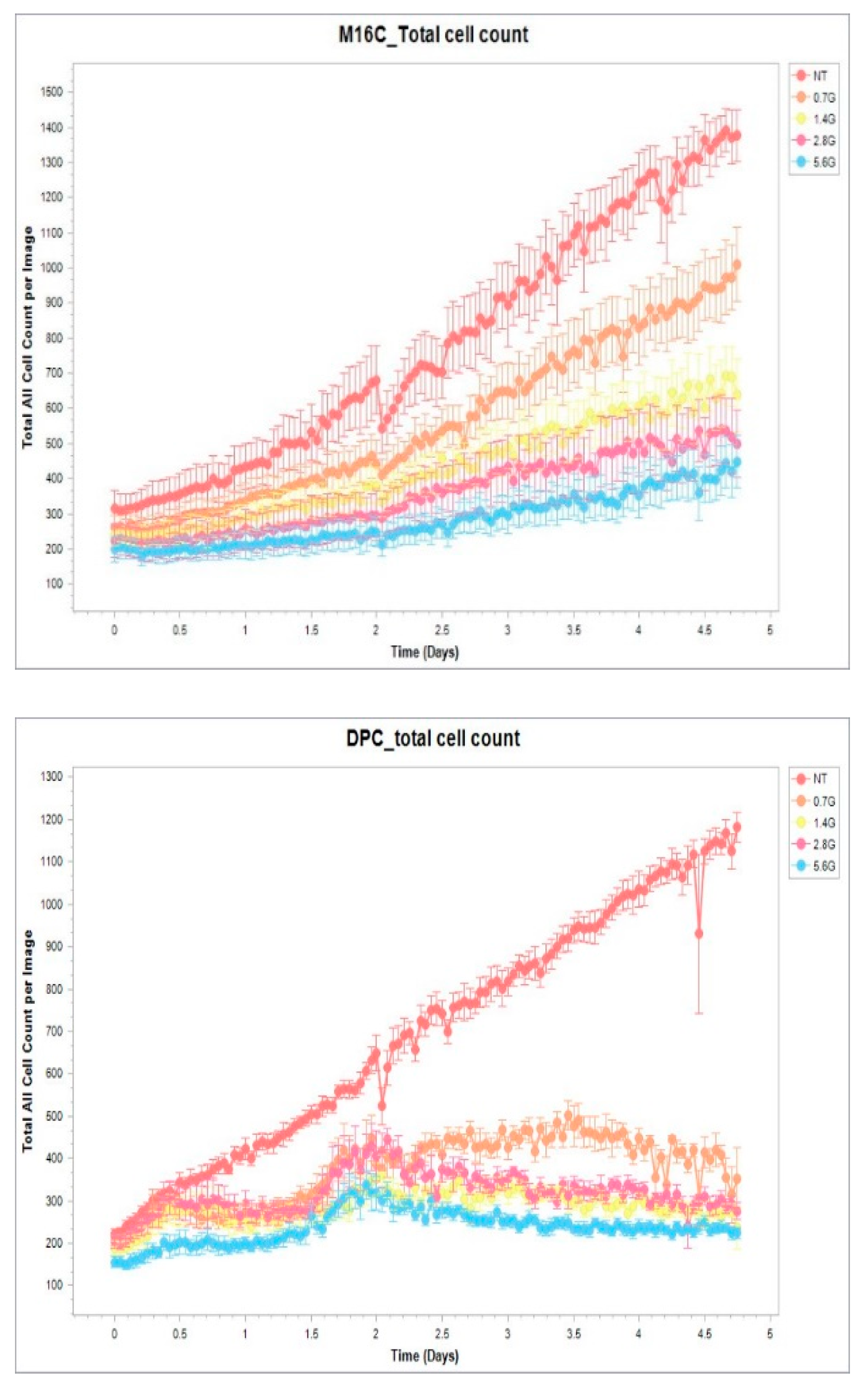
Our results so far showed that although alpha radiation caused cell death in melanoma cells, there is still percentage of viable cells, continuing to grow despite the aggressive nature of the alpha particles hitting their nuclei and breaking their DNA. Thus, we compared cell death kinetics after radiation of the most sensitive cell, DP.C, to the most resistant one, M16.C, to acquire more knowledge about the cytotoxic effect of alpha radiation.
Melanoma cells were seeded in radiation cell holders at a concentration of 100,000 cells per ml (50,000 cells per 500 µl per radiation holder) for 24 hours to adhere and then irradiated with increasing doses of alpha radiation (0-5.6 Gy). Cells were removed from the radiation cell holder and seeded in 96-well plates, triplicates of 10,000 cells per well for each radiation dose. Cell growth and cell death were measured by an ~IncuCyte 2022B Rev2~ Incucyte® SX5 machine, for 5 days with propidium iodide (PI). Analysis of total cell count, and PI positive cells were conducted by ~2022B Rev2~ Incucye2022BRev2 software AI analyses.
Results presented in
Figure 8 show the total cell-count during five days after radiation. It is evident that there is a difference between the behavior of the sensitive DP.C cells and more resistant M16.C cells. Sensitive cells fail to recover even after exposure to a low radiation dose (0.7 Gy) while the resistant M16.C cells start to proliferate within one day and recovery is evident even after the highest dose of 5.6 Gy.
Figure 8.
Total cells count after radiation. DP.C and M16.C cutaneous cells were examined in the IncuCyte machine for five days. Untreated cells were compared to irradiated cells with 0.7, 1.4, 2.8, 5.6 Gy of alpha radiation. Total cell count was analyzed by 2022B Rev2 analyzer.
Figure 8.
Total cells count after radiation. DP.C and M16.C cutaneous cells were examined in the IncuCyte machine for five days. Untreated cells were compared to irradiated cells with 0.7, 1.4, 2.8, 5.6 Gy of alpha radiation. Total cell count was analyzed by 2022B Rev2 analyzer.
4. Discussion
Radiotherapy is a powerful tool against cancer. The treatment of solid tumors with different approaches of radiation therapy is widely discussed in the literature [
48]. Malignant melanoma is a type of skin cancer that is known for its relative resistance to photon radiation [
32,
33,
45]. The need to overcome the radio resistance of melanoma directed our team to investigate the potential use of alpha particles radiation on human melanoma. Our laboratories developed an ablation method using alpha particle radiation (DaRT) as mentioned before. This technique, using alpha radiation, proved to induce effective tumor response in patients with squamous cell carcinoma (SCC) [
28,
29].
The radiobiological advantages of alpha particles include short range in tissue (typically 30-90 μm), high linear energy transfer (high-LET, 5,000-8,000 keV) and independence of the administered dose rate, oxygen effects and the cells state in the cell cycle during the irradiation [
11].
A single alpha particle hit to the nucleus has a 20-40% probability of killing the cell and only a few hits are required to ensure cell lethality [
9,
10,
11], mostly due to DNA double strand breaks (DSBs) [
10]. Densely ionizing radiations induce DSBs that are spatially correlated, more complex (i.e., associated with other lesions), and more difficult to repair than those induced by X or gamma rays [
9,
10,
49]. Using gene expression as an endpoint, it was also shown that stressful effects are transmittable from cells exposed to high LET IR to non-irradiated cells [
50].
These characteristics suggest alpha irradiation as a natural candidate for the treatment of cancerous tissues. Therefore, alpha particle radiation was selected to be researched for its cytotoxic effect on a battery of human derived melanoma cell variants.
It should be mentioned that the melanoma cells used in this study were previously shown to exhibit inter-tumor heterogeneity. Employing xenograft models of human melanomas in nude mice detected differential functional responses of these melanoma cells, from different patients to GM-CSF both in vitro as well as in vivo. Whereas cells of one melanoma acquired pro metastatic features following exposure to GM-CSF, cells from another melanoma either did not respond or became less malignant [
51].
In the current study, firstly, we measured the response of human melanoma cells to alpha radiation, secondly, studied the variance in response within a group of cells from the same histotype, and thirdly looked for cell characteristics which might correlate with sensitivity/resistance of melanoma cells to alpha radiation. To the best of our knowledge, similar studies of this kind assessing the biological effect of alpha radiation on a battery of human melanoma were not yet reported in the literature.
Our study showed that in vitro exposure of human melanoma cells to alpha radiation killed the melanoma cells with variations in sensitivity.
In vivo studies in melanoma bearing mice treated with a peptide conjugated with an alpha emitting radio labeled nuclide, showed a decrease in tumor growth rate, extended mean survival rate of the subjects, and in many cases, complete remission of the disease [
52].
In–vitro examination of the irradiated melanoma cells, in the present study, showed a decrease in proliferation along the dose scale, and cytological staining with HemaColor regents revealed swollen membranes and broken nuclei along with well observed apoptotic bodies. Furthermore, treating with alpha radiation was much more efficient in killing the cells, compared to the irradiation with photon radiation (gamma radiation) (
Figure 5). These results are corroborated by previous studies in which treatment of cells with alpha radiation or x-rays was compared. Interactions of a-particle tracks with the cell may result in an all-or-nothing event, and if there is a hit it is likely to be a severe clustered damage that results in several small fragments. Whereas with the sparser open structure of X-rays a hit may be more likely but can result in just one or a few events, thus reducing the number of small fragments produced compared with a-particles [
53]. From the practical point, the results emphasize the possible role of alpha particle as a suitable treatment for hard shelled tumors as melanoma using a methodology such as alpha DaRT.
The alpha radiation dose required for killing 50% of the cells (D50) was measured as quantitative variable for the comparison of the cytotoxic effect of alpha radiation among all melanoma cell lines. Considerable variations in cytotoxicity levels inflicted by alpha radiation were observed among the four cutaneous cell lines. Post- hoc analysis after ANOVA of cutaneous cell lines revealed that the DP.C cell line was more sensitive than the other three (YDFR.C, M12.C, M16.C) and significantly more sensitive compared to the M16.C cell line. D50 measurements suggest that some cell lines inside the population of cutaneous melanoma needed almost as double dose of radiation to exhibit the same cytotoxicity as the others. In comparison, the melanoma cells showed high resistance to photon radiation with small variation among them, although the DP.C cell line was also the most sensitive to photon radiation. The variance showed with both radiations and in particular the variance in cytotoxicity of alpha radiation emphasized the heterogeneity of human melanoma response after radiation treatment and should be optimized, if used clinically. A detailed study performed with many melanoma cells reported
in – vitro heterogeneity to photon radiation, and the ability to overcome resistance to radiation by Braf inhibition [
54].
As heterogeneity in response to alpha radiation was observed in our viability assays, we further looked for cellular properties, which may contribute to the variance in response to alpha radiation among our cell lines. As alpha particles can penetrate the cell nucleus and break its DNA in different locations, the cell nucleus is determined as a target for these particles. Thus, we looked for a correlation between the nuclear area of the cells and their sensitivity to alpha radiation. Measurements of the cell nuclei, perimeter and the derived radius were performed for each of our cutaneous cell lines. Variance was obtained between the YDFR.C and DP.C compared to M12.C and M16.C cell lines. Comparison of nuclear size and sensitivity to alpha radiation indicated the most sensitive cell to alpha radiation had the largest nucleus (DP.C), while the resistant cell had a smallest nucleus (M16.C) (Table 2). These findings state that when comparing our cutaneous melanoma cell lines, the larger the nucleus, the more sensitive the cell line to alpha radiation, with the exception of line M12.C.
This finding aligns with previous studies. Microdosimetric analysis of other cancer cell lines subjected to alpha radiation showed that the nuclear area of the cells irradiated with alpha radiation is a parameter to be considered when dealing with different tumor cell lines [
27]. Furthermore, it was well discussed
, that considering broad beam using heavy ions radiation, the number of hits is determined by the cell nucleus [
55]. Moreover, a recent paper suggest that the cell and cell nucleus size may impact the biological effect of radiation therapy [
56].
To further elucidate the cause of the variations in cytotoxicity in our cells, we investigated the formation of DNA double strand breaks (DSB) by alpha radiation.
Double stranded breaks in the DNA are deadly to the cell nucleus and accumulation of these can lead to cell death, and in some cases to cell senescence [
57]. It has been stated that alpha radiation, due to its higher LET, is more effective than other ionizing radiation such as gamma radiation in breaking the DNA [
58]. The use of phosphorylated histone γ-H2ax marker to detect DSB in our irradiated cell lines nuclei revealed that all our cutaneous cell lines had phosphorylated foci (
Figure 4, Table 3.) right after uniform radiation with 1.4 Gy. Furthermore, analysis of the number of foci of each cell line confirmed that cells more sensitive to radiation had a larger nucleus (DP.C) and showed more phosphorylated foci than the other cells. Although there are other properties involved in the heterogeneity in response to alpha radiation, we can conclude that nuclear morphology and the mean number of DSB foci can be key properties to determine the variance among our cutaneous melanoma cell lines.
Among all types of damage, clustered lesions present a significant challenge for DNA repair machinery of the cell and explain why high LET ionizing radiation has higher RBE and highly effective, despite not necessarily causing a greater overall number of DSBs compared to low- LET radiation [
59,
60].
Radiation-induced DNA-damage, especially DNA DSBs, triggers activation of the ATM-initiated signaling cascade, to arrest cell division until repairs can be made. This cascade of DNA-damage responses is composed from the following core components: the signals, sensors of signals, transducers and effectors [
61,
62]. The primary transducer of the DSB alarm is the nuclear protein kinase ataxia-telangiectasia mutated (ATM) [
63]. Following ATM activation, the histone H2AX is phosphorylated (to become γ-H2AX), which in turn elicits a sequence of signaling events [
64]. H2AX is one of the most genetically conserved H2A-variants and is present in chromatin at levels that vary between 2-25% of the H2A pool, depending on the cell line and tissue examined [
65,
66]. H2AX turned to be a key-player in the cellular responses to DNA-damage after discovering that it is locally phosphorylated on a conserved serine (Ser139 in mammals), to generate γ-H2AX in the vicinity of DSBs [
64,
67]. The phosphorylation can be rapidly detected after only a few minutes in cells exposed to ionizing radiation (IR) and is implicated in amplifying the DNA-damage signals [
64,
67,
68]. H2AX’s phosphorylation and γ-H2AX foci formation are generally accepted nowadays as consistent and proper quantitative markers of DSBs, applicable even under conditions where only a few DSBs are present [
69]. All three major PIKK (PI3K-like protein kinases) members: ATM, ATR and DNA-PKcs, have the potential of phosphorylating H2AX, and there is numerous evidence that each of them carries out this phosphorylation when others are genetically compromised [
61,
70,
71,
72,
73].
It was important to investigate if the correlation between cell killing by alpha radiation, nuclear morphology and the number of DSB, which was found within the melanoma group of cells, is also applicable for another skin tumor, squamous cell carcinoma. We compared our cutaneous melanoma cell lines to a SCC line (CAL 27) assessing its D50 measurement, nuclear area, and the mean phosphorylated foci after radiation. The SCC cell line, CAL 27, had a similar number of DSB (6.67) and nucleus size (175.49 mM2) as the more resistant melanoma cells. Yet, it was more sensitive to alpha radiation than all melanoma cells. This might indicate that other factors such as DNA damage and repair mechanisms, death related signals, to name a few may also figure importantly in the sensitivity to alpha radiation.
An interesting finding by Lemaitre and coworkers, on DSB and the repair pathways controlling them, revealed that the nuclear position of the DSB dictates the choice of DNA repair pathways. it was suggested that there is a spatial regulation of the DNA damage response to DSB, and that the position of the DSB may be a crucial variable to maintain the response to the damage [
74]. It means that DSB in different cell types may occur at different locations in the nucleus triggering mechanisms of repair or cell death.
Another important observation in our research relates to the death kinetics of the cells after alpha radiation. Live cell imaging, showed in the perspective of time, that the cutaneous melanoma cell lines had different recovery patterns after radiation, which was radiation dose dependent (
Figure 8). Each cell line had a different pattern of growth trend and different time that it started to recover and proliferate. For example, the radiation sensitive cell line, DP.C, with the largest nuclear area and the most phosphorylated foci after radiation hardly recovered at all radiation doses. In contrast, the M16.C cell line, the most resistant cell regained a higher proliferative capacity as compared to DP.C.
Since the state of the DNA and chromatin at the time of radiation might be crucial for the radiation inflicted damage and the function of DNA repair mechanisms we attempted to resolve the issue of chromatin structure in relation to response to alpha particles. The DNA structure is classified into two states: condensed (heterochromatin, HC) and relaxed (euchromatin, EC) [
75]. In condensed chromatin high LET radiation, such as alpha particles, might cause more damage than that in the regular relaxed state. Primarily because alpha radiation doesn’t depend on the oxygenated state of the target, secondly, few alpha particles may cause complexed DNA breaks and higher lethal damage would be achieved, and condensed chromatin might be less favorably for the function of repair mechanisms.
It was reported that the condensed state, restricts DNA DSB repair and damage response signaling, and that ATM signaling enhances heterochromatin relaxation in the DSB vicinity and that this is a prerequisite for HC-DSB repair [
76]. Furthermore, a recent study showed that alpha emitters were more efficient in cancers with heterochromatin states [
77]. Thus, proliferation arrest and chromatin condensation may increase DNA damage and slow down DNA repair mechanisms.
To induce chromatin condensation, cells need in general, to enter the G0/G1 phase of the cell cycle, there the DNA structure is more condensed. To induce this state, it was suggested to use serum starvation to arrest the cell cycle [Shin et al 2008].
Exposure of the alpha radiation sensitive DP.C to alpha particles after proliferation arrest, increased non significantly the level of cytotoxicity at the low level of radiation (0.7 Gy), but not at higher radiation levels. This may indicate that lack of proliferation and probably chromatin condensation is not a significant factor in alpha radiation inflicted cell damage and death. Similar results of radiation after serum starvation were obtained for the YDFR.C, M12.C, and M16.C cell lines (results not shown). We may conclude that condensation of the DNA due to serum starvation marginally increased the cytotoxic effect of alpha radiation. Furthermore, unlike in the case of photon radiation, proliferation arrest did not reduce the cytotoxic effect of alpha radiation on melanoma cell lines.
In this respect, other studies found that cells with maximal chromatin compactness are more resistant to gamma radiation, but the damage is poorly repaired [
78,
79,
80].
More on this aspect was reported in another study which showed that chromatin opening by histone deacetylase inhibitor trichostatin A (TSA) pretreatment reduced clonogenic survival and increased H2AX foci in MDA-MB-231 cells, indicative of increased damage induction by free radicals using gamma radiation. In contrast, TSA pretreatment tended to improve survival after alpha radiation while H2AX foci were similar or lower [
77].
Next, we looked for combinations of chemotherapeutic regents that may enhance the cytotoxic effect of alpha radiation on the cutaneous melanoma cell lines.
Combined treatment of radiotherapy and chemotherapeutic reagents for cancers has advanced significantly in the recent years. The combination was suggested to reduce side effects of treatment, and to overcome radiation resistance it was suggested to target DNA damage repair [
81]. Berzosertib is an example of a reagent that can inhibit the ATR pathway and a potent inhibitor of the ATM pathway as well, which are responsible for sensing DNA damage in dividing cells. The ATM is primarily involved in response to DSB while the ATR involved in wide range of DNA damage [
82]. It has been reported that combining X-ray radiation, and an ATR inhibitor (ATRi) enhanced the effect of radiation in non-small cell lung carcinoma (NSCLC) [
83], and that combining ATRi with radiation is more effective than by themselves in head and neck squamous cell carcinoma [
84]. Moreover, ATRi was found to radio sensitize the triple negative breast cancer cells [
85]. Therefore, we tested if ATR inhibition by berzosertib will enhance the cytotoxic effect of irradiated cutaneous melanoma cell lines. Cells were pretreated by berzosertib (100, 300, 500 nM) for 24 hours, followed by increasing doses of alpha radiation and compared to irradiated only. Results showed that pretreatment of berzosertib 24 hours before radiation marginally enhanced cytotoxicity in all four cutaneous cell lines. It should be mentioned that attempts to sensitize cells to alpha radiation by inhibitors of DNA damage repair (DDR) revealed that some cells can be sensitized by DNA-PK inhibitors while others by ATM inhibition [
86].
Another chemotherapeutic reagent that was used in our study was the semi synthetic compound CPT- 11 (irinotecan) which is an inhibitor of topoisomerase 1, and its potency in enhancing radiosensitivity is known for almost thirty years. Irinotecan radio sensitized human melanoma variant (U1-mel) to X–ray radiation [
87], and the human breast cancer cell line MCF-7 was also radio sensitized by irinotecan [
88]. The combined treatment results of irinotecan and alpha radiation showed evidence for radio sensitization by the drug to alpha radiation. Yet, irinotecan was highly toxic to the melanoma cells and combined effect was observed with sublethal dose of 1 µM for 24 hours pre radiation. Although more research is needed, we can conclude that irinotecan, as a modifier for the inhibition of the Topoisomerase 1, can be considered as a radio sensitization agent for alpha radiation.