Submitted:
30 October 2024
Posted:
31 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection and Data Extraction
2.3. Assessment of Methodological Quality
2.4. Main and Subgroup Analyses
2.5. Statistical Analysis
3. Results
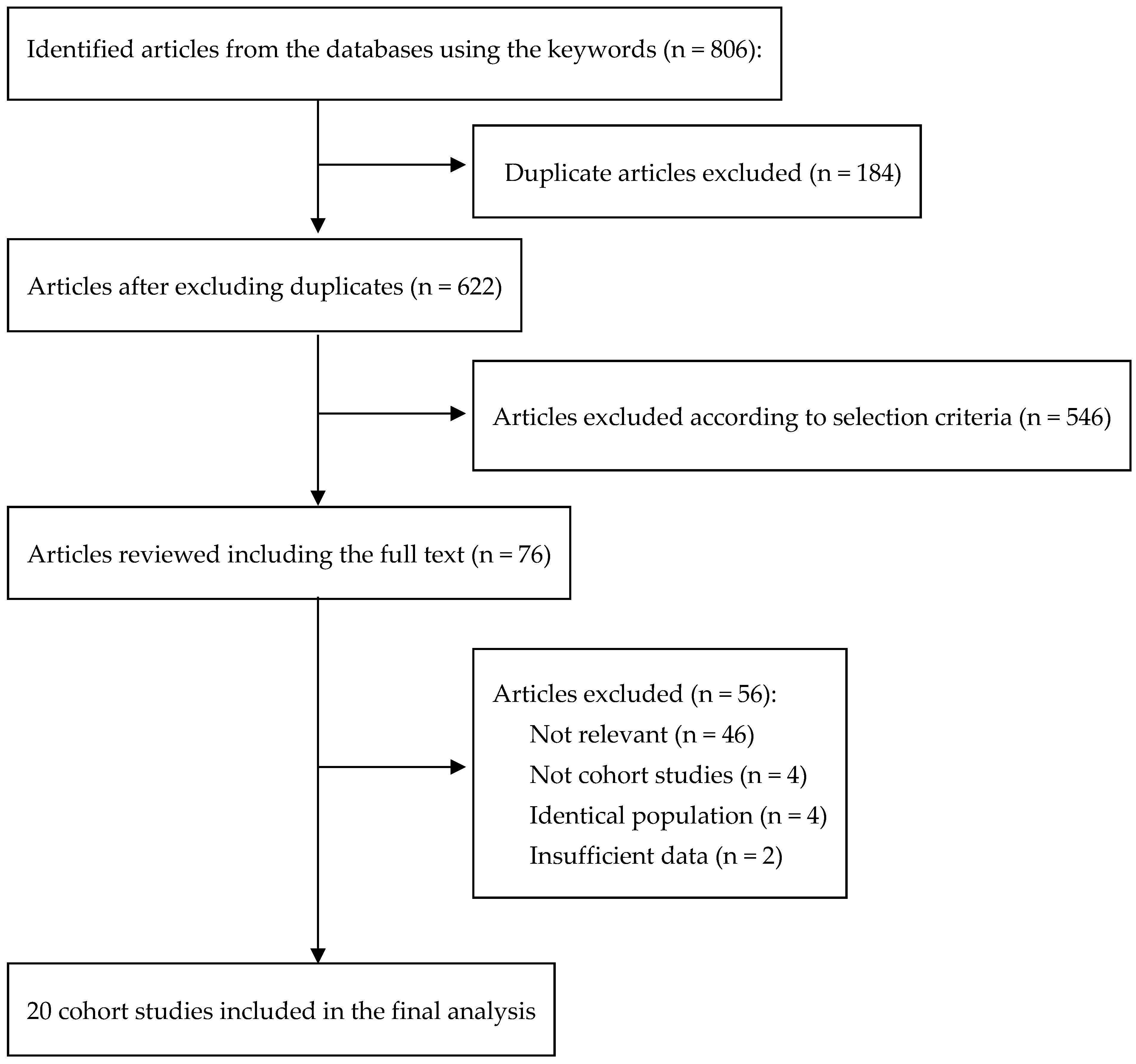
3.1. Study Selection
3.2. General Characteristics of Included Studies
3.3. Methodological Quality of Studies
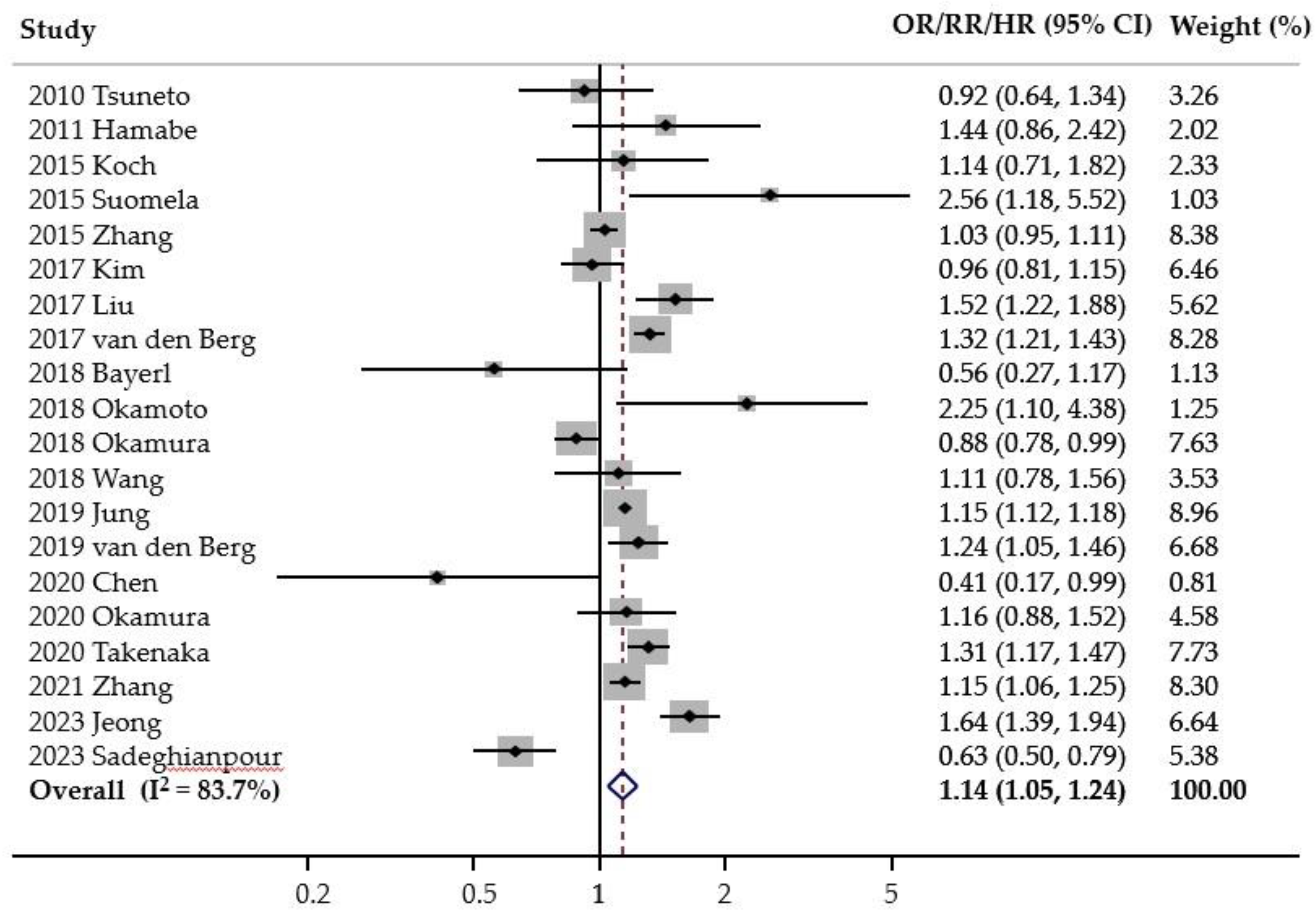
3.4. Association Between Smoking and Risk of FLD
3.5. Subgroup Meta-Analyses
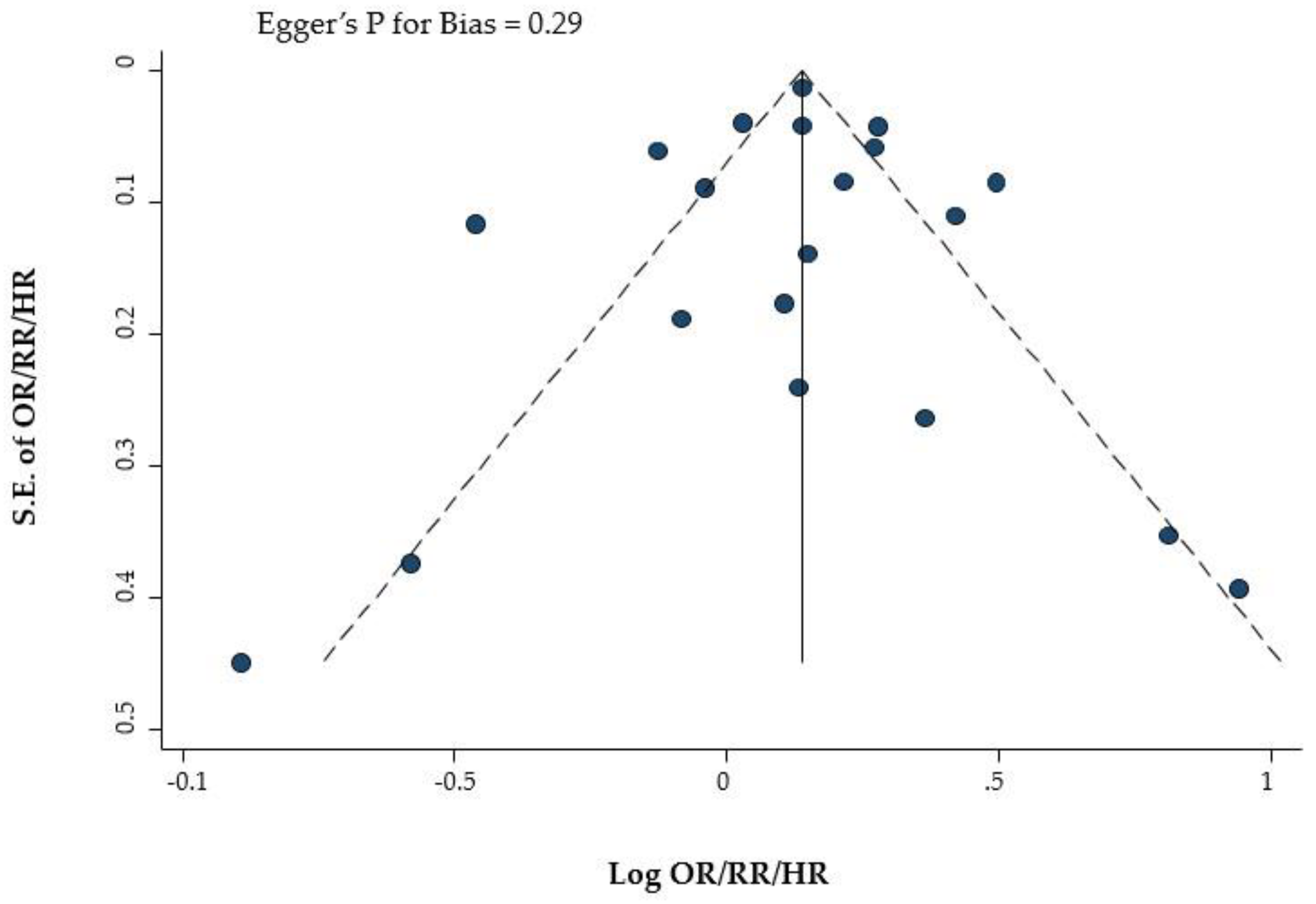
3.6. Publication Bias
4. Discussion
Author Contributions
Funding Support
Data Availability Statement
Conflict of Interest
Ethics Statement
References
- Adams, L.A.; Lymp, J.F.; St Sauver, J.; Sanderson, S.O.; Lindor, K.D.; Feldstein, A.; Angulo, P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005, 129, 113-121. [CrossRef]
- Nascimbeni, F.; Pais, R.; Bellentani, S.; Day, C.P.; Ratziu, V.; Loria, P.; Lonardo, A. From NAFLD in clinical practice to answers from guidelines. J. Hepatol. 2013, 59, 859-871. [CrossRef]
- Crabb, D.W.; Galli, A.; Fischer, M.; You, M. Molecular mechanisms of alcoholic fatty liver: role of peroxisome proliferator-activated receptor alpha. Alcohol 2004, 34, 35-38. [CrossRef]
- Machado, M.; Cortez-Pinto, H. Non-alcoholic steatohepatitis and metabolic syndrome. Curr. Opin. Clin. Nutr. Metab. Care 2006, 9, 637-642. [CrossRef]
- Machado, M.V.; Cortez-Pinto, H. Management of fatty liver disease with the metabolic syndrome. Expert Rev. Gastroenterol. Hepatol. 2014, 8, 487-500. [CrossRef]
- Riazi, K.; Azhari, H.; Charette, J.H.; Underwood, F.E.; King, J.A.; Afshar, E.E.; Swain, M.G.; Congly, S.E.; Kaplan, G.G.; Shaheen, A.A. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 851-861. [CrossRef]
- Browning, J.D.; Szczepaniak, L.S.; Dobbins, R.; Nuremberg, P.; Horton, J.D.; Cohen, J.C.; Grundy, S.M.; Hobbs, H.H. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 2004, 40, 1387-1395. [CrossRef]
- Ko, E.; Yoon, E.L.; Jun, D.W. Risk factors in nonalcoholic fatty liver disease. Clin. Mol. Hepatol. 2023, 29, S79-s85. [CrossRef]
- Yuan, H.; Shyy, J.Y.; Martins-Green, M. Second-hand smoke stimulates lipid accumulation in the liver by modulating AMPK and SREBP-1. J. Hepatol. 2009, 51, 535-547. [CrossRef]
- Azzalini, L.; Ferrer, E.; Ramalho, L.N.; Moreno, M.; Domínguez, M.; Colmenero, J.; Peinado, V.I.; Barberà, J.A.; Arroyo, V.; Ginès, P., et al. Cigarette smoking exacerbates nonalcoholic fatty liver disease in obese rats. Hepatology 2010, 51, 1567-1576. [CrossRef]
- Tsuneto, A.; Hida, A.; Sera, N.; Imaizumi, M.; Ichimaru, S.; Nakashima, E.; Seto, S.; Maemura, K.; Akahoshi, M. Fatty liver incidence and predictive variables. Hypertens. Res. 2010, 33, 638-643. [CrossRef]
- Hamabe, A.; Uto, H.; Imamura, Y.; Kusano, K.; Mawatari, S.; Kumagai, K.; Kure, T.; Tamai, T.; Moriuchi, A.; Sakiyama, T., et al. Impact of cigarette smoking on onset of nonalcoholic fatty liver disease over a 10-year period. J. Gastroenterol. 2011, 46, 769-778. [CrossRef]
- Koch, M.; Borggrefe, J.; Schlesinger, S.; Barbaresko, J.; Groth, G.; Jacobs, G.; Lieb, W.; Laudes, M.; Müller, M.J.; Bosy-Westphal, A., et al. Association of a lifestyle index with MRI-determined liver fat content in a general population study. J. Epidemiol. Community Health 2015, 69, 732-737. [CrossRef]
- Suomela, E.; Oikonen, M.; Virtanen, J.; Parkkola, R.; Jokinen, E.; Laitinen, T.; Hutri-Kähönen, N.; Kähönen, M.; Lehtimäki, T.; Taittonen, L., et al. Prevalence and determinants of fatty liver in normal-weight and overweight young adults. The Cardiovascular Risk in Young Finns Study. Ann. Med. 2015, 47, 40-46. [CrossRef]
- Zhang, T.; Zhang, C.; Zhang, Y.; Tang, F.; Li, H.; Zhang, Q.; Lin, H.; Wu, S.; Liu, Y.; Xue, F. Metabolic syndrome and its components as predictors of nonalcoholic fatty liver disease in a northern urban Han Chinese population: a prospective cohort study. Atherosclerosis 2015, 240, 144-148. [CrossRef]
- Kim, T.J.; Sinn, D.H.; Min, Y.W.; Son, H.J.; Kim, J.J.; Chang, Y.; Baek, S.Y.; Ahn, S.H.; Lee, H.; Ryu, S. A cohort study on Helicobacter pylori infection associated with nonalcoholic fatty liver disease. J. Gastroenterol. 2017, 52, 1201-1210. [CrossRef]
- Liu, P.; Xu, Y.; Tang, Y.; Du, M.; Yu, X.; Sun, J.; Xiao, L.; He, M.; Wei, S.; Yuan, J., et al. Independent and joint effects of moderate alcohol consumption and smoking on the risks of non-alcoholic fatty liver disease in elderly Chinese men. PLoS One 2017, 12, e0181497. [CrossRef]
- van den Berg, E.H.; Amini, M.; Schreuder, T.C.; Dullaart, R.P.; Faber, K.N.; Alizadeh, B.Z.; Blokzijl, H. Prevalence and determinants of non-alcoholic fatty liver disease in lifelines: A large Dutch population cohort. PLoS One 2017, 12, e0171502. [CrossRef]
- Bayerl, C.; Lorbeer, R.; Heier, M.; Meisinger, C.; Rospleszcz, S.; Schafnitzel, A.; Patscheider, H.; Auweter, S.; Peters, A.; Ertl-Wagner, B., et al. Alcohol consumption, but not smoking is associated with higher MR-derived liver fat in an asymptomatic study population. PLoS One 2018, 13, e0192448. [CrossRef]
- Okamoto, M.; Miyake, T.; Kitai, K.; Furukawa, S.; Yamamoto, S.; Senba, H.; Kanzaki, S.; Deguchi, A.; Koizumi, M.; Ishihara, T., et al. Cigarette smoking is a risk factor for the onset of fatty liver disease in nondrinkers: A longitudinal cohort study. PLoS One 2018, 13, e0195147. [CrossRef]
- Okamura, T.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. Low urine pH is a risk for non-alcoholic fatty liver disease: A population-based longitudinal study. Clin. Res. Hepatol. Gastroenterol. 2018, 42, 570-576. [CrossRef]
- Wang, L.; Li, M.; Zhao, Z.; Xu, M.; Lu, J.; Wang, T.; Chen, Y.; Wang, S.; Dai, M.; Hou, Y., et al. Ideal Cardiovascular Health Is Inversely Associated with Nonalcoholic Fatty Liver Disease: A Prospective Analysis. Am. J. Med. 2018, 131, 1515.e1511-1515.e1510. [CrossRef]
- Jung, H.S.; Chang, Y.; Kwon, M.J.; Sung, E.; Yun, K.E.; Cho, Y.K.; Shin, H.; Ryu, S. Smoking and the Risk of Non-Alcoholic Fatty Liver Disease: A Cohort Study. Am. J. Gastroenterol. 2019, 114, 453-463. [CrossRef]
- van den Berg, E.H.; Gruppen, E.G.; Blokzijl, H.; Bakker, S.J.L.; Dullaart, R.P.F. Higher Sodium Intake Assessed by 24 Hour Urinary Sodium Excretion Is Associated with Non-Alcoholic Fatty Liver Disease: The PREVEND Cohort Study. J. Clin. Med. 2019, 8, 2157. [CrossRef]
- Chen, X.; Ma, T.; Yip, R.; Perumalswami, P.V.; Branch, A.D.; Lewis, S.; Crane, M.; Yankelevitz, D.F.; Henschke, C.I. Elevated prevalence of moderate-to-severe hepatic steatosis in World Trade Center General Responder Cohort in a program of CT lung screening. Clin. Imaging 2020, 60, 237-243. [CrossRef]
- Okamura, T.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. Creatinine-to-bodyweight ratio is a predictor of incident non-alcoholic fatty liver disease: A population-based longitudinal study. Hepatol. Res. 2020, 50, 57-66. [CrossRef]
- Takenaka, H.; Fujita, T.; Masuda, A.; Yano, Y.; Watanabe, A.; Kodama, Y. Non-Alcoholic Fatty Liver Disease Is Strongly Associated with Smoking Status and Is Improved by Smoking Cessation in Japanese Males: A Retrospective Study. Kobe J. Med. Sci. 2020, 66, E102-e112.
- Zhang, Q.; Ma, X.; Xing, J.; Shi, H.; Yang, R.; Jiao, Y.; Chen, S.; Wu, S.; Zhang, S.; Sun, X. Serum Uric Acid Is a Mediator of the Association Between Obesity and Incident Nonalcoholic Fatty Liver Disease: A Prospective Cohort Study. Front. Endocrinol. (Lausanne) 2021, 12, 657856. [CrossRef]
- Jeong, S.; Oh, Y.H.; Choi, S.; Chang, J.; Kim, S.M.; Park, S.J.; Cho, Y.; Son, J.S.; Lee, G.; Park, S.M. Association of Change in Smoking Status and Subsequent Weight Change with Risk of Nonalcoholic Fatty Liver Disease. Gut Liver 2023, 17, 150-158. [CrossRef]
- Sadeghianpour, Z.; Cheraghian, B.; Farshchi, H.R.; Asadi-Lari, M. Non-alcoholic fatty liver disease and socioeconomic determinants in an Iranian cohort study. BMC Gastroenterol. 2023, 23, 350. [CrossRef]
- Akhavan Rezayat, A.; Dadgar Moghadam, M.; Ghasemi Nour, M.; Shirazinia, M.; Ghodsi, H.; Rouhbakhsh Zahmatkesh, M.R.; Tavakolizadeh Noghabi, M.; Hoseini, B.; Akhavan Rezayat, K. Association between smoking and non-alcoholic fatty liver disease: A systematic review and meta-analysis. SAGE Open Med. 2018, 6, 2050312117745223. [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539-1558. [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97-111. [CrossRef]
- Artese, A.; Stamford, B.A.; Moffatt, R.J. Cigarette Smoking: An Accessory to the Development of Insulin Resistance. Am. J. Lifestyle Med. 2017, 13, 602-605. [CrossRef]
- Cetin, E.G.; Demir, N.; Sen, I. The Relationship between Insulin Resistance and Liver Damage in non-alcoholic Fatty Liver Patients. Sisli Etfal Hastan. Tıp Bul. 2020, 54, 411-415. [CrossRef]
- Eliasson, B.; Attvall, S.; Taskinen, M.R.; Smith, U. The insulin resistance syndrome in smokers is related to smoking habits. Arterioscler. Thromb. 1994, 14, 1946-1950. [CrossRef]
- Utzschneider, K.M.; Kahn, S.E. Review: The role of insulin resistance in nonalcoholic fatty liver disease. J. Clin. Endocrinol. Metab. 2006, 91, 4753-4761. [CrossRef]
- Jia, W.P. The impact of cigarette smoking on metabolic syndrome. Biomed. Environ. Sci. 2013, 26, 947-952. [CrossRef]
- Zhang, C.X.; Guo, L.K.; Qin, Y.M.; Li, G.Y. Association of polymorphisms of adiponectin gene promoter-11377C/G, glutathione peroxidase-1 gene C594T, and cigarette smoking in nonalcoholic fatty liver disease. J. Chin. Med. Assoc. 2016, 79, 195-204. [CrossRef]
- Myung, S.K. How to review and assess a systematic review and meta-analysis article: a methodological study (secondary publication). J. Educ. Eval. Health Prof. 2023, 20, 24. [CrossRef]
- Mackay, J.; Eriksen, M.P.; Shafey, O.; American Cancer Society. The tobacco atlas. 2nd ed.; American Cancer Society: Atlanta, Ga., 2006; pp 1 atlas (128 pages) : color illustrations, color maps ; 125 cm.
- Jung-Choi, K.H.; Khang, Y.H.; Cho, H.J. Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob. Control 2012, 21, 536-542. [CrossRef]
- Hwang, J.-e.; Choi, Y.; Yang, Y.-s.; Oh, Y. Gender differences in the perceived effectiveness of female-focused graphic health warnings against smoking in South Korea. Health Educ. J. 2020, 79, 58-72. [CrossRef]
- Seo, D.C.; Torabi, M.R.; Kim, N.; Lee, C.G.; Choe, S. Smoking among East Asian college students: prevalence and correlates. Am. J. Health Behav. 2013, 37, 199-207. [CrossRef]
- Nakhaee, N.; Divsalar, K.; Bahreinifar, S. Prevalence of and factors associated with cigarette smoking among university students: a study from Iran. Asia Pac. J. Public Health 2011, 23, 151-156. [CrossRef]
| Study | Region | Type of study | Gender | Study participants (% of men) | Comparison | Odds ratio, relative Risk, or hazard ratio, and 95% confidence interval | Outcomes | Adjusted variables |
|---|---|---|---|---|---|---|---|---|
| 2010 Tsuneto [11] | Asia | Prospective | Both | 1,635 atomic bomb survivors who underwent biennial examinations in Nagasaki without NAFLD at baseline |
Ex-smoker or current smoker vs. none | 0.92 (0.64-13.4) | FLD | Age, sex, BMI, DM, HTN, dyslipidemia, drinking habits, and atomic radiation dose |
| 2011 Hamabe [12] | Asia | Retrospective | Both | 1,560 subjects without NAFLD who underwent a complete medical health checkup at the Kagoshima Kouseiren Medical Healthcare Center | Cigarette smoking vs. no smoking | 1.44 (0.86-2.42) | NAFLD | Age, sex, obesity, HTN, dyslipidemia, dysglycemia, and alcohol intake |
| 2015 Koch [13] | Europe | Cross-sectional | Both | 747 official population registeries in Kiel | Cigarette smoking vs. no smoking | 1.14 (0.71-1.82) | FLD | Age, sex, years of education, total energy intake, physical activity, and waist circumference |
| 2015 Suomela [14] | Europe | Cross-sectional | Both | 3,592 Young Finns | Current smoker vs. none | 2.56 (1.18-5.52) | FLD | Age, sex, BMI, and waist circumference |
| 2015 Zhang [15] | Asia | Prospective | Both | 15,791 health check-up participants at the Center for Health Management of Shandong Provincial Qianfoshan Hospital and Shandong Provincial Hospital |
Current smoker vs. none | 1.03 (0.95-1.11) | NAFLD | Baseline Mets status, sex, age, diet, smoking status, and regular exercise |
| 2017 Kim [16] | Asia | Retrospective | Both | 17,028 health-screening exam participants at the Center for Health Promotion of the Samsung Medical Center, South Korea | Current smoker vs. none | 0.96 (0.81-1.15) | NAFLD | Age, sex, body mass index, year of screening exam, alcohol intake, regular exercise, and education level |
| 2017 Liu [17] | Asia | Cross-sectional | Male | 9,432 DFTJ cohort study among retirees of Dong feng Motor corporation | Current smoker vs. none | 1.52 (1.22-1.88) | NAFLD | Age, body mass index, waist circumference alcohol intake, DM, HTN, dyslipidemia, and past history of CHD |
| 2017 van den Berg [18] | Europe | Cross-sectional | Both | 37,496 Framework of the Lifelines Cohort Study | Current smoker vs. none | 1.32 (1.21-1.43) | FLD | Age, sex, Hemoglobin, ALT/ALP/Albumin, HBA1c, Type 2 DM, dyslipidemia, and past history of CHD |
| 2018 Bayerl [19] | Europe | Cross-sectional | Both | 1,282 persons from Cooperative Health Research in German region | Ex-smoker or current smoker vs. none | 0.56 (0.27-1.17) | FLD | Age, sex, DM, and alcohol intake |
| 2018 Okamoto [20] | Asia | Retrospective | Both | 7,905 persons who underwent health checkup at Ehime General Health Care Association | Current smoker vs. none | 2.25 (1.10-4.38) | FLD | Age, sex, BMI, DM, HTN, CVD, dyslipidemia, and snacking habit |
| 2018 Okamura [21] | Asia | Retrospective | Both | 29,555 medical examination program at Murakami Memorial Hospital using the NAGALA (NAFLD in the Gifu Area, Longitudinal Analysis) database |
Current smoker vs. none | 0.88 (0.78-0.99) | NAFLD | Age, sex, BMI, ALT, triglycerides, exercise habit, alcohol consumption, systolic blood pressure, fasting plasma glucose, and uric acid |
| 2018 Wang [22] | Asia | Prospective | Both | 10,375 participants from community residents in the Jiading District of Shangia | Current smoker or quit<12mo vs. none | 1.11 (0.78-1.56) | NAFLD | Age, sex, alcohol consumption, education, and HOMA-IR |
| 2019 Jung [23] | Asia | Prospective | Both | 199,468 persons who underwent health checkup at Kangbuk Samsung Health Study | Ex-smoker or current smoker vs. none | Men: 1.15 (1.12-1.18) Women: 1.14 (1.03-1.27) |
FLD | Age, sex, BMI, DM, HTN, dyslipidemia, alcohol drinking, education level, physical activity, waist circumference, and laboratory test |
| 2019 van den Berg [24] | Europe | Cross-sectional | Both | 6,132 participants of the prevention of Renal and Vascular End-stage Disease cohort study | Current smoker vs. none | 1.24 (1.05-1.46) | NAFLD | Age, sex, BMI, DM, HTN, dyslipidemia, alcohol drinking, estimated GFR, urine albumin excretion, use of antihypertensive medication, glucose lowering drugs, lipid lowering drugs, and HOMA-IR |
| 2020 Chen [25] | US | Cross-sectional | Both | 154 World Trade Center participants in NIOSH | Current smoker vs. none | 0.41 (0.17-0.99) | FLD | Age, sex , Ethnicity, BMI, DM,HTN,COPD, and membership in the WTC |
| 2020 Okamura [26] | Asia | Retrospective | Both | 13,728 population-based longitudinal study of participants in a medical checkup program at Asahi University Hospital |
Current smoker vs. none | 1.16 (0.88-1.52) | NAFLD | Age, aspartate aminotransferase, fasting plasma glucose, triglyceride to high-density lipoprotein cholesterol ratio, systolic blood pressure, alcohol consumption, and exercise. |
| 2020 Takenaka [27] | Asia | Cross-sectional | Both | 8,297 health check-up participants at Yodogawa Christian Hospital |
Current smoker vs. none | 1.31 (1.17-1.47) | NAFLD | Age, sex, presence of metabolic syndrome, and light alcohol consumption |
| 2021 Zhang [28] | Asia | Prospective | Both | 16,839 participants who received the Kailuan Group’s detailed and thorough medical examination at Tangshan City, China |
Current smoker vs. none | 1.15 (1.06-1.25) | NAFLD | Age, sex, marital status, working type, education level, physical activity, systolic blood pressure , lipid profile, CRP, and Cr |
| 2023 Jeong [29] | Asia | Retrospective | Both | 296,033 in NHIS of Korea | Current smoker vs. none | 1.64 (1.39-1.94) | FLD | Age, sex, household income, BMI, HTN, DM, HL, physical activity, and Charlson comorbidity index |
| 2023 Sadeghianpour [30] | Asia | Cross-sectional | Both | 180,000 Iranian adults in Hoveyzeh Cohort Study | Current smoker vs. none | 0.63 (0.50-0.79) | FLD | Age, sex, area, physical activity, Energy intake Household income, DM, HL, Education level, wealth status, and skill level |
| Studies | Selection | Comparability | Exposure | Total score | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 1 | 1 | 2 | 3 | ||
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Outcome of interest not present at start of the study | Comparability of cohorts | Assessment of outcome | Adequate follow-up period for outcome of interest | Adequacy of follow-up of cohorts | ||
| 2010 Tsuneto | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 7 |
| 2011 Hamabe | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| 2015 Zhang | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 2017 Kim | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 2018 Okamoto | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 2018 Okamura | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| 2018 Wang | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| 2019 Jung | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| 2020 Okamura | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| 2021 Zhang | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| 2023 Jeong | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| Factor | No. of studies | RR (95%CI) | Heterogeneity I2 (%) |
|---|---|---|---|
| All studies | 20 | 1.14 (1.05-1.24)* | 83.7 |
| Type of cohort study | |||
| Prospective | 5 | 1.15 (1.05-1.18)* | 51.7 |
| Retrospective | 6 | 1.23 (0.94-1.62) | 88.4 |
| Cross-sectional | 9 | 1.12 (0.92-1.36) | 85.2 |
| Region | |||
| Europe | 8 | 1.32 (1.16-1.50)* | 82.1 |
| Asia | 10 | 1.03 (0.91-1.18) | 83.5 |
| US | 2 | 0.75 (0.28-2.06) | 79.5 |
| Type of fatty liver disease | |||
| Fatty liver disease | 6 | 1.27 (1.01-1.59)* | 72.7 |
| Non-alcoholic fatty liver disease | 14 | 1.09 (1.00-1.19)* | 83.2 |
| Gender (All from Asia) | |||
| Men | 4 | 1.15 (1.06-1.25)* | 71.2 |
| Women | 4 | 1.12 (0.94-1.34) | 47.8 |
| Follow-up period | |||
| <5 years | 3 | 1.44 (0.95-2.13) | 93.0 |
| >5 years | 7 | 1.08 (0.98-1.19) | 70.9 |
| Quality of study† | |||
| High | 6 | 1.16 (0.94-1.42) | 85.3 |
| Low | 5 | 1.07 (0.95-1.20) | 67.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





