Introduction
The diaphragm is a crucial skeletal muscle that separates the thoracic and abdominal cavities (1) and plays an essential role in respiration, as well as in activities like defecation and vomiting by regulating intra-thoracic and intra-abdominal pressure gradients (2). Embryologically, it develops from the septum transversum during week four of gestation and assumes a domelike appearance with a central tendinous part upon development (2). Anatomically, it attaches to the sternum, the sixth to twelfth ribs, the last thoracic vertebra, and the first three lumbar vertebrae (2). Despite its protection within the thoracic cage, the diaphragm can sustain traumatic injuries, either blunt or penetrating injury, through the thoracoabdominal region. Blunt injuries often result from motor vehicle accidents, falls from a height, or pedestrian strikes, whereas penetrating injuries include gunshot wounds, stab wounds, or sharp objects with the capacity to penetrate the thoracoabdominal partition. Injury to the diaphragm can also arise at birth, a term called congenital diaphragmatic hernia, which occurs due to a defect in the diaphragm during its development (3).
Traumatic diaphragmatic injuries (TDI) are not common, with blunt TDI occurring in 1 to 7% of cases and penetrating injuries occurring in 15% of cases (2, 4). Patients may present with chest pain and respiratory symptoms, raising suspicion of diaphragmatic injury. Blunt trauma can lead to diaphragm rupture due to an increase in kinetic energy transferred to the diaphragm (5). The left hemidiaphragm is more commonly affected due to its congenital weakness during development (5), whereas the right is less vulnerable to injury due to the liver acting as a protective mechanism. Although it is rare, right-sided diaphragmatic injury carries an increased risk of mortality due to association with other abdominal injuries (6). Penetrating injuries typically follow the path of the foreign object and are relatively small in extent (2). Studies show that motor vehicle collisions are the most common cause of blunt TDI (63.4%), while gunshot wounds are the predominant cause of penetrating TDI (66.5%) (7).
Chest X-ray and computed tomography (CT) are the primary imaging techniques for diagnosing TDI (8). However, CT is preferred due to its ability to detect herniated intraabdominal content and provide detailed visualization of air or fluid in the thoracic cavity when the diaphragm is ruptured (11). Management usually involves thoracotomy, laparotomy, or a combination of both if necessary. Other interventions are thoracoscopy and laparoscopy, but in patients who are hemodynamically stable (14, 15) or in cases where traumatic diaphragmatic rupture is detected early, exploratory laparotomy is recommended (9). This is because exploratory laparotomy allows for a broad examination of the abdominal cavity to exclude any other intra-abdominal injuries that were missed on CT imaging.
Here, we examine the cases of nine patients with blunt TDI, including their demographics, injury mechanisms, modes of detection, injury severity score (ISS), and outcomes.
Cases Presentation
Case 1
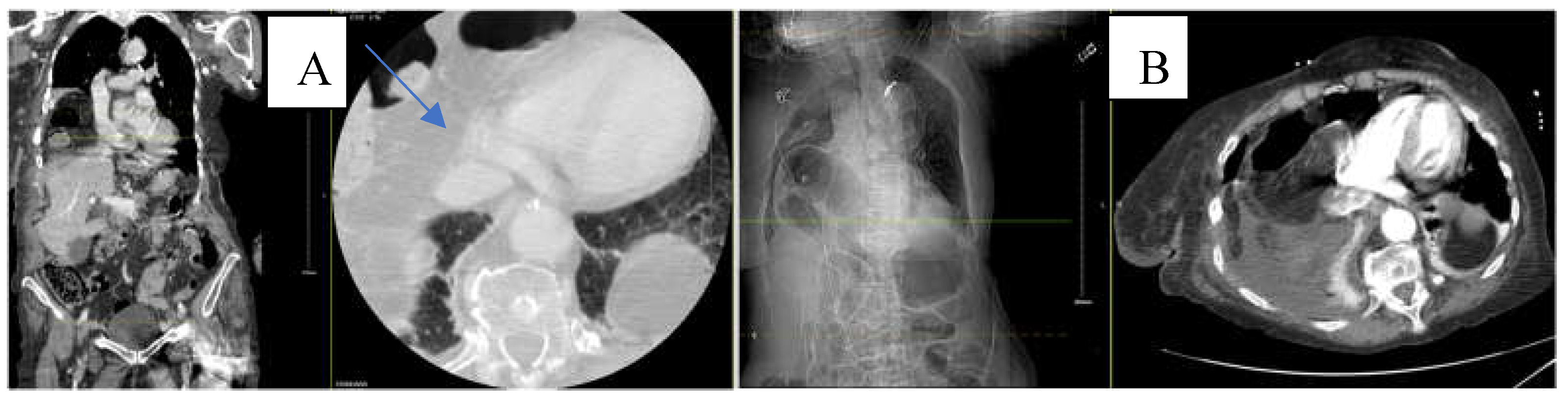
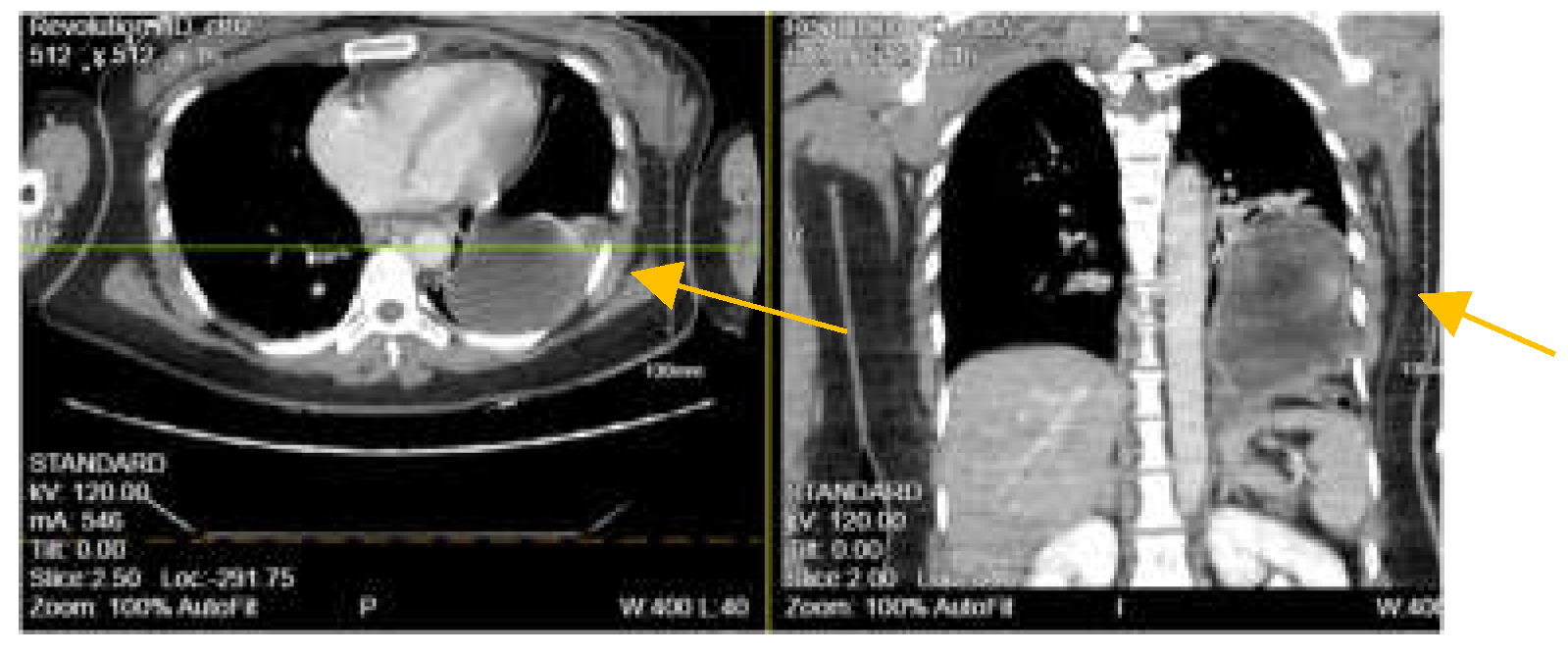
An 88-year-old White American woman with a past medical history of hypertension, hyperlipidemia, and hip fracture with repair (4 years ago) presented to our emergency department (ED) with complaints of pain in her right forearm, left hand, lower back, and on the chest bilaterally with trouble breathing. According to the patient, she fell at home 2-days ago. She did not remember how she fell or the precise location but believed she tripped. The patient admitted to an extensive smoking history and likely has undiagnosed chronic obstructive pulmonary disease (COPD). Denied any loss of consciousness, dizziness, or hitting her head. The electrocardiogram (EKG) finding was significant for rapid atrial fibrillation (no prior history) which was managed with an anti-arrhythmic medication throughout her hospital course. The patient was tachycardic, tachypneic, hypotensive with blood pressure (BP) of 96/62 mmHg, and hypoxic to 88% for which she was placed on supplemental oxygen but afebrile in the ED. Physical examination noted tenderness to the right lateral chest with bruising to the right breast and right forearm with an overlying laceration. The abdomen was soft and non-tender. No sign of labored breathing. Chest X-ray (CXR) revealed right pleural effusion and areas of atelectasis with several right and lower fractured ribs. Contrast-enhanced computed tomography (CT) of the chest showed a perforated right hemidiaphragm with gastrointestinal content in the thorax (
Figure 1A). CT abdomen and pelvis revealed no acute findings. The patient refused surgical intervention. Two days after admission to the surgical intensive care unit (SICU), the patient experienced respiratory distress with the use of accessory muscles to breathe and became hypotensive for which she responded to fluid resuscitation. CT angiogram (CTA) was performed which showed herniation of the bowel into the right anterior chest significantly compromising the right lung volume, pleural effusion, and small pneumothorax (
Figure 1B). The patient again refused surgical management and signed a do not intubate and do not resuscitate (DNI/DNR) order. The patient requested comfort care only and died the next day from her condition. Injury Severity Score (ISS) was 29.
Case 2
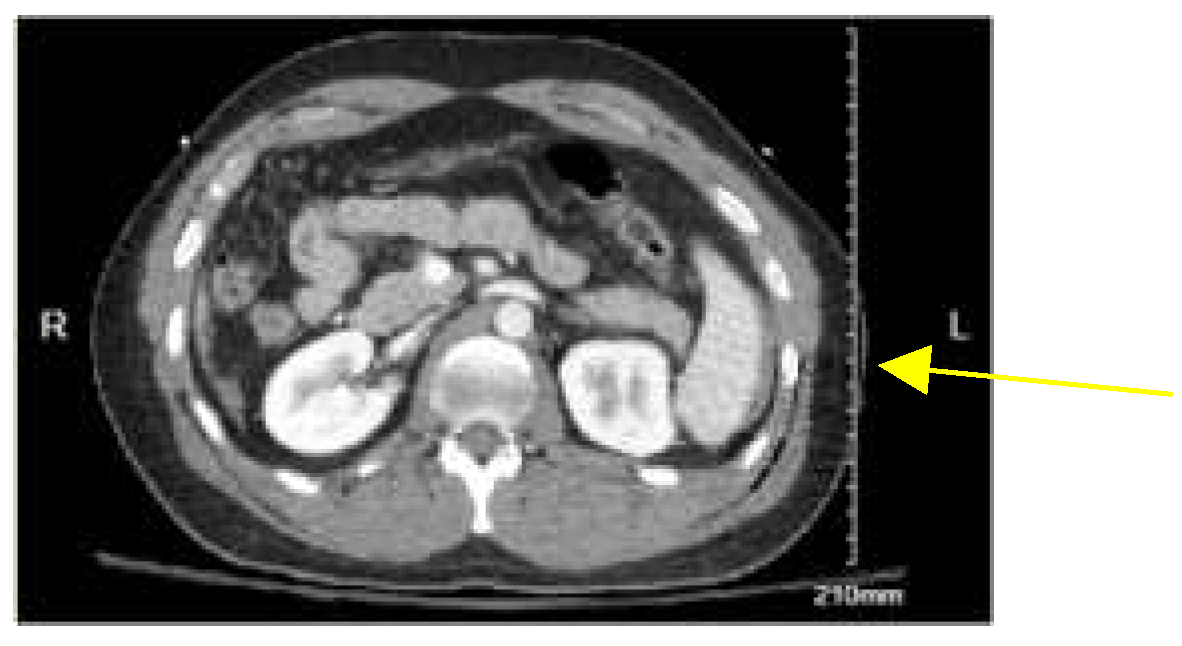
A 30-year-old non-Hispanic male with no past medical history was brought to the emergency department (ED) by the emergency medical services (EMS) after being involved in a motor vehicle accident. The patient was riding his motorcycle when he got struck on his left side by a car traveling at 30 miles per hour (mph). Per the patient, he had a helmet on which remained intact after the collision. Denies losing consciousness but was not ambulating at the scene. The patient was hemodynamically stable at the time of presentation with a BP of 110/77 mmHg. The primary survey was remarkable for mild crepitus on the left lateral chest, a major deep laceration on the left chin, a deep wound on the right knee, and an abrasion to the left flank. Extended Focused Assessment with Sonography in Trauma (eFAST) was negative for any pericardial fluid. CXR showed a rib fracture on the left without pneumothorax. CT chest revealed mildly displaced fractures of the left sixth through 12
th ribs posteriorly, contusion along the left lateral chest wall, and subcutaneous emphysema. CT abdomen and pelvis (CTAP) showed grade 2 or 3 splenic laceration with a small amount of perisplenic (
Figure 2) fluid for which the patient underwent embolization of the splenic artery. Due to CT chest findings of traumatic fractures of left 6
th -12
th ribs, the patient was taken to the operating room for left Video-Assisted Thoracic Surgery (VATS), left thoracotomy, and plating of left 7
th-10
th ribs. During thoracotomy exploration, it was discovered that the 10
th rib had torn the diaphragm, and this was repaired with 0-ethibond running stitch and a 28French chest tube was placed on the left. The patient was discharged on postoperative day 4 with pain medication and in stable condition. ISS was 22.
Case 3
A 27-year-old Hispanic male with no significant past medical history presented to the ED by EMS after sustaining a stab injury to the chest and flank region by an approximate 4-inch-long knife. Per the patient, he had an altercation with an unknown individual and was seen by bystanders running after sustaining the injury. The patient denies trauma to the head, loss of consciousness, nausea, or vomiting. On arrival at the ED, the patient was tachycardic initially but stabilized after fluid administration. BP was 137/77 mmHg. All other vitals were unremarkable. The alcohol level was elevated at 241mg/dL. On physical examination, there was no sign of labored breathing, and the abdomen was non-tender. There was a 2-inch laceration and 2-inch deep, actively bleeding on the left chest lateral and inferior to the nipple; a 2-inch deep laceration actively bleeding on the left flank (Image 1). Lacerations were cleaned and sutured at the bedside. CXR and eFAST showed no rib fracture, pneumothorax, or pericardial fluid. Contrast-enhanced CT radiograph of the chest showed trace left pleural effusion with no evidence of fractures or pneumothorax. CT abdomen and pelvis report revealed no acute intraabdominal injury. The patient was admitted to SICU for 24-hour monitoring. After 24 hours, the patient was noted to have a benign abdominal exam without signs of peritonitis or abdominal pain but remained hemodynamically stable. He was taken to the operating room for a diagnostic laparoscopy where a laceration was noted on the dome of the left diaphragm. The patient became bradycardic and hypotensive intraoperatively with concern for tension pneumothorax which was decompressed and placement of a 24French chest tube on the left. The procedure was then converted to an exploratory laparotomy for repair of the diaphragmatic injury. On exploration, a laceration of 2 cm was in the mid portion of the left diaphragm. It was repaired with a single figure of eight 0-proline sutures. The patient tolerated the procedure well and was discharged on postoperative day 4. ISS was 9
Image 1.
Left- showed a 2-inch laceration on the left anterior chest. The right image revealed a 2-inch laceration on the left flank/left posterior chest.
Image 1.
Left- showed a 2-inch laceration on the left anterior chest. The right image revealed a 2-inch laceration on the left flank/left posterior chest.
Case 4
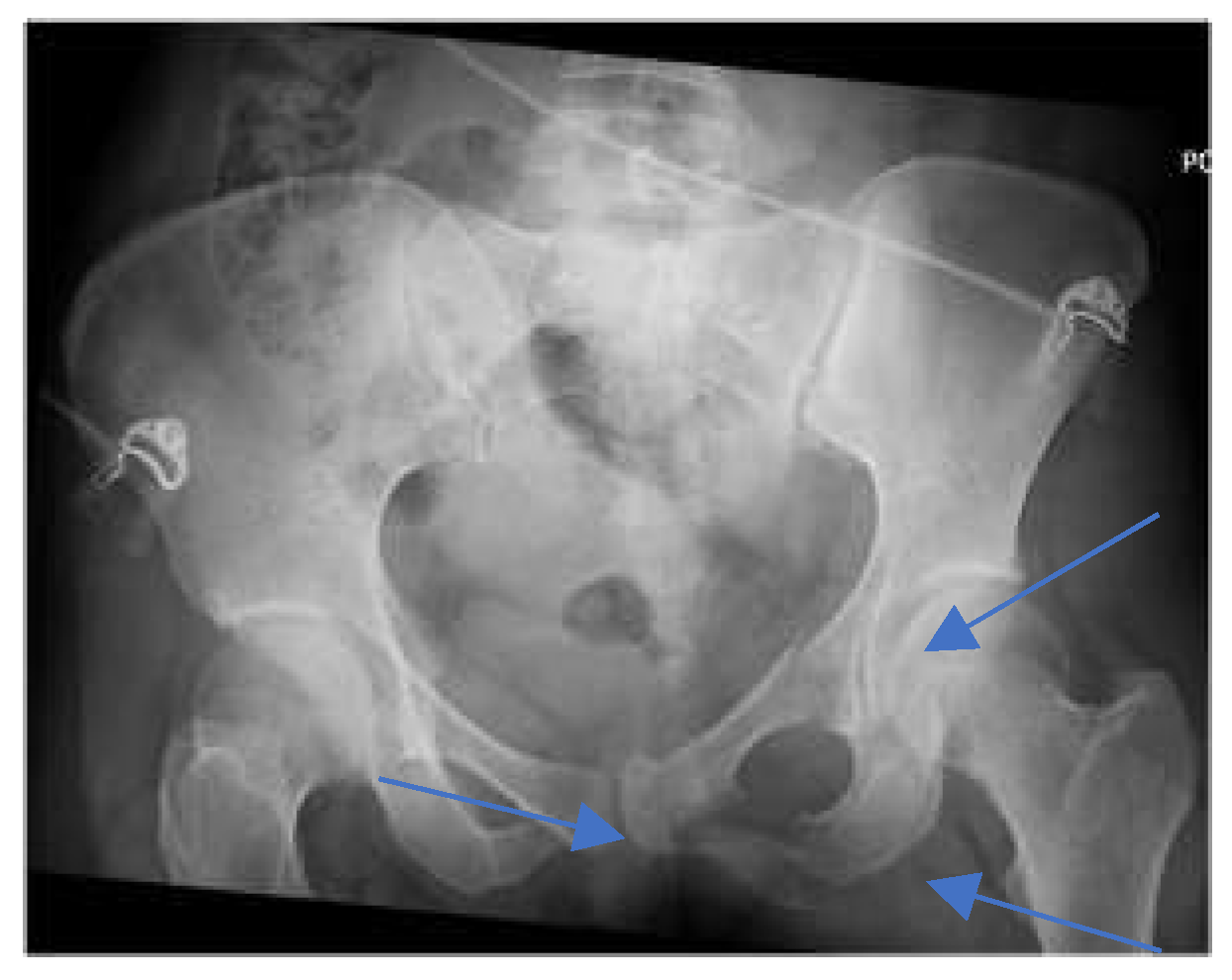
A 28-year-old Asian female with an unknown past medical history was brought by EMS as a pedestrian struck vs jumped in front of a car at a high rate of speed. She was thrown onto her left side. The initial Glasgow Coma Scale (GCS) was 10. On arrival at the ED, the patient was spontaneously moving but mumbling incoherently. Vitals were remarkable for tachycardia, tachypneic, and hypoxia. BP was 136/107 mmHg. The primary survey was notable for deformity of the left forearm and dilated unreactive left pupil. A portable pelvic ultrasound (
Figure 3) revealed pelvic fracture. Chest ultrasound showed elevation of the left hemidiaphragm and comminuted diaphyseal fracture of the left humerus with major fragments. CTA of the neck showed C5-C6 with 3 mm posterior subluxation, irregular narrowing of the right vertebral artery extending from C5-7, and nondisplaced coracoid fracture of the left scapula. CT chest with contrast (
Figure 4) revealed a distended stomach with air-fluid in the left hemithorax concerning a closed loop obstruction. eFAST was negative for pericardial fluid. CTAP was consistent with CT chest findings including grade 4 splenic injury with contrast extravasation, grade 3 left renal injury with perinephric collection, and multiple pelvic fractures. The patient became hemodynamically unstable and was emergently taken to the operating room (OR) for exploratory laparotomy. The stomach was successfully reduced into the abdominal cavity from the thorax and on exploration, the diaphragm was noted to have a 6 cm defect, which was repaired with 2-0 ethibond in interrupted fashion with a total of 8 stitches. The patient also underwent splenectomy due to pulsatile red blood extravasation. On the same admission, neurosurgery performed anterior cervical discectomy and fusion and open reduction internal fixation (ORIF) of open humerus fracture and pelvic fracture. Two days after admission, she was taken back to the OR for repair of liver capsular laceration and facial closure. The patient was discharged on postoperative day 47 in stable condition. ISS was 41.
Case 5
A 74-year-old Hispanic female with a past medical history of diabetes mellitus and hyperlipidemia presents to the ED as a transfer from another facility with a complaint of right-sided rib cage pain and right arm pain. According to the patient, she fell earlier today at home. The patient reported falling 7-8 steps while walking up the stairs in her home. She mentioned feeling dizzy before falling and hitting the right side of her body. Denied head trauma or loss of consciousness. Her vitals were stable in the ED with a BP of 140/88 mmHg. On examination, there was tenderness on the chest wall and right upper arm, abrasions, and bruising to the right side of the rib cage. CT chest without contrast (
Figure 5) showed acute displaced lateral right 7
th and 8
th rib fractures and comminuted scapular fractures. Moderate right hemidiaphragm elevation. The patient underwent exploratory laparoscopy, and no diaphragmatic injury was identified. ISS 9.
Case 6
A 36-year-old Hispanic female was brought by EMS after a pedestrian struck her. Initially had pulses on the scene but lost en route to the ED with 6 minutes of cardiopulmonary resuscitation (CPR) pre-hospital. Vitals were not accessible in the ED. Physical examination noted abrasion to the face, left leg deformity, and distended abdomen. The patient was intubated upon arrival and resuscitative thoracotomy was performed with no blood return, numerous rib fractures and contused lungs were noted, the diaphragm was significantly distended, and minimal cardiac activity. GCS was 3. There was no return of spontaneous circulation and the patient was pronounced dead in the ED. No images were taken before death. ISS 43.
Case 7
A 68-year-old Asian female was brought in by EMS for traumatic arrest. The patient was struck by a motor vehicle on city streets. According to EMS, the patient was unresponsive and pulseless upon their arrival. The patient returned a pulse after a couple of rounds of CPR. Upon arrival at our emergency room, she was bagged with a bag valve mask but no response. Initial vitals were suggestive of hypovolemic shock with the absence of a pulse. Portable CXR showed multiple right-sided acute rib fractures and the possibility of impacted distal left clavicular fracture without pneumothorax. Portable pelvis ultrasound revealed a dislocated right femoral head (
Figure 6). The patient did not respond to resuscitative efforts and was pronounced dead in the ED. No CT images were obtained before death. ISS 54.
Case 8
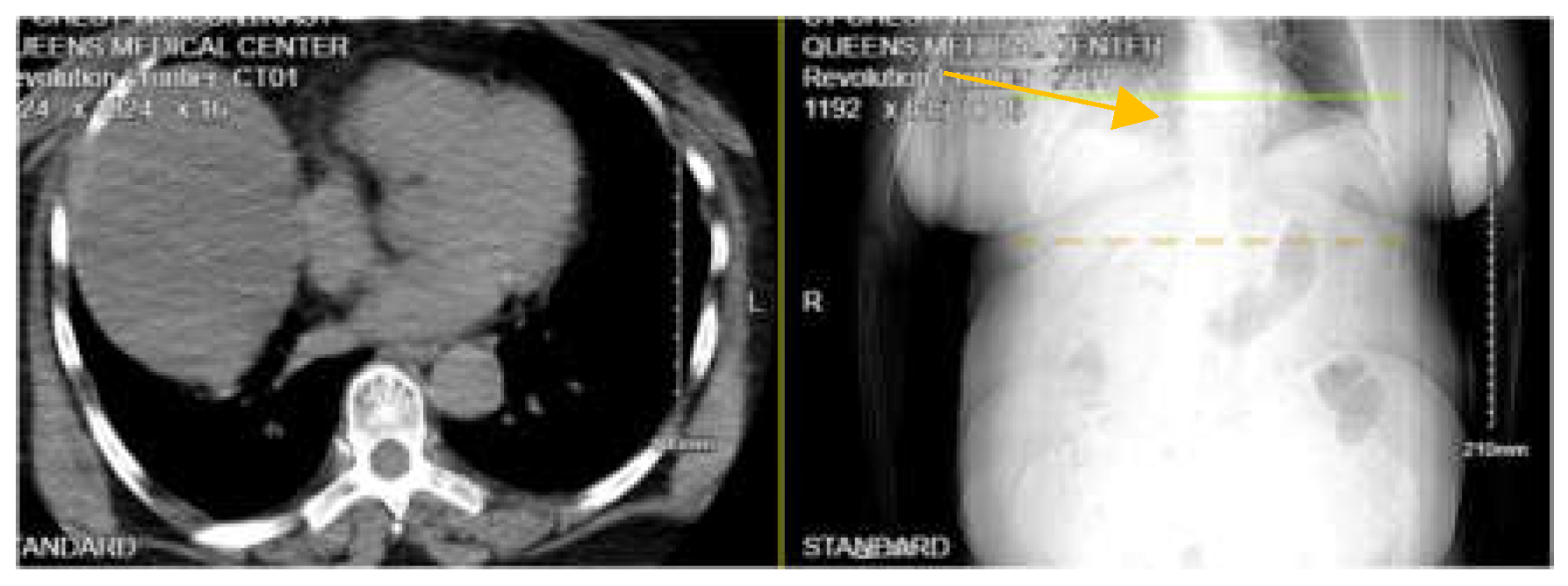
A 48-year-old Hispanic male with an unknown past medical history was brought by EMS after a motorcycle accident. Per EMS, the patient was riding his motorcycle without a helmet and weaving through traffic before hitting a pole. EMS arrived about 15-20 minutes to the scene when the patient still had a weak pulse. eFAST was negative and no cardiac activity on Point of Care Ultrasound (POCUS). CPR was in progress in the ED. There was no pulse for more than 20 minutes and the patient was pronounced dead in the trauma bay. No vitals or labs were taken, and no CT images of the chest abdomen, and pelvis were on file. ISS 75.
Case 9
A 32-year-old Black male was brought by EMS in traumatic arrest. The patient was pinned between the subway platform and the oncoming train. He suffered massive crush injuries to his torso, neck, and face. The patient was in cardiac arrest at the time of the paramedic’s arrival on the scene. Paramedics attempted to intubate but were unable to due to neck trauma. The patient was asystole on the scene and arrived at our ED without a pulse. Physical examination noted gross deformity to the right arm, right shoulder, pelvis, and ribs. No cardiac activity on ultrasound (US) and the patient was pronounced dead in the ED. No scans were obtained before death. ISS 75.
Management and Outcome
Diagnosing a blunt diaphragmatic injury can be challenging because of its potential to remain undetected in a few cases, leading to delayed presentation with abdominal pain and respiratory symptoms several months after the acute event (9). Early diagnosis is important to prevent complications. Contrast-enhanced computed tomography (CT) is the preferred imaging modality for the diagnosis of blunt diaphragmatic injury. Although chest X-rays are initially preferred, some review studies have shown that they are diagnostic in only one-third of cases, compared to chest CT, which has a sensitivity of 71% and a specificity of 100% (10) for detecting diaphragmatic injuries. Chest radiography can identify herniation of abdominal contents into the thoracic cavity (11). Thus, it is mandatory to obtain a CT scan of the chest to accurately detect diaphragmatic injuries. While there are no set guidelines for when to perform surgery (12), management decisions are made based on the severity of symptoms and the presence of bowel contents protruding into the chest wall, which can result in complications such as strangulation and perforation (12, 13). Laparotomy, thoracotomy, or a combination of both are commonly utilized surgical interventions (13). Rubikas Romaldas in his studies found that urgent surgical intervention improved survival rates (14). Furthermore, Zarour et al., in their study discovered that operative interventions and young age are associated with favorable outcomes (6).
In our study, cases 1 and 5 had diaphragmatic injury detected on a chest CT scan. Of these two patients, case 5 underwent diagnostic laparoscopy but no injury to the diaphragm was identified. In case 2, the patient underwent video-assisted thoracotomy surgery (VATS) for rib repair, and a diaphragmatic injury was noted on the left, which was repaired with a 0-ethibond stitch, leading to a favorable outcome. Case 3 had a diaphragmatic injury that was noted on diagnostic laparoscopy, converted to open laparotomy, and was repaired with 0-proline suture. The patient survived as well. In case 4, the diaphragmatic injury was detected on exploratory laparotomy with repair using a 2-0 ethibond suture. The patient survived. In case 6, resuscitative thoracotomy in the trauma bay revealed a distended diaphragm, but the patient succumbed to his injuries. Cases 7,8 and 9 died from traumatic arrest either before arriving at the ED or were pronounced dead in the trauma bay without any CT imaging to indicate diaphragmatic injury before their death.
Discussion
Diagnosing diaphragmatic injury after a blunt trauma can be challenging due to its potential to remain undetected leading to delayed presentation years after the initial injury (9). Our case series aimed to analyze the methods of detecting blunt TDI, the mechanism of injury, and the role of the Injury Severity Score (ISS) in patient outcomes. We also reviewed patient demographics.
This case series included 9 patients from 2016 to 2023 with blunt TDI. The demographic breakdown included 1 White American, 1 Black American, 3 Asians, and 4 from other racial backgrounds, with ages ranging from 27 to 88 years old. Of the patients, 4 were male, and 5 females. Two patients sustained diaphragmatic injuries from mechanical falls at home (cases 1 and 5). Both patients were elderly, in their 70s to 80s. Case 1 CT imaging revealed abdominal contents in the right hemidiaphragm, but the patient declined surgical intervention opting for comfort care and passing away the following day. This finding is consistent with literature indicating that right hemidiaphragm injury has an increased risk of mortality (6). Case 5 had a CT scan without contrast showing right hemidiaphragm elevation without evidence of intraabdominal contents in the thorax. Although the patient was hemodynamically stable, a diagnostic laparoscopy revealed no injury. This aligns with Al-Jehani et al., who mentioned a preference for the use of diagnostic laparoscopy in stable patients (15).
Two patients (cases 2 and 8) sustained blunt TDI from motor vehicle accidents, with ages ranging from 30 to 48 years. Case 2 had a CT scan that failed to detect injury to the diaphragm, but during VATS and thoracotomy for rib repair, a torn diaphragm was discovered and repaired with a 0-ethibond running stich. The patient survived. This finding aligns with the literature indicating that CT may miss injuries that have no bowel contents protrusion into the thoracic cavity (2). A high index suspicion should be held for injury to the 6th to 12th ribs because the diaphragm also attaches to the ribs at this region.
Four patients (cases 4, 6, 7, and 9) had pedestrian strikes, aged 28 to 68 years. Three of these patients died spontaneously. Case 4 survived her injury after repair of a 6 cm diaphragmatic injury with a 2-0 ethibond stitch on exploratory laparotomy. Case 6, 7, and 9, involved in high-impact energy collision, did not have imaging performed and died shortly after the presentation to the ED. Although the patient in case 6 already lost pulse en route to the hospital, she underwent resuscitative thoracotomy in the trauma bay, which revealed an elevated diaphragm but did not survive her injury.
Case 3 injury was a Hispanic male who sustained his injury from a knife stab. His initial examination and imaging revealed benign findings. Due to injury sustained to the thoracoabdominal region and also benign abdominal exam findings after 24 hours of monitoring in SICU, the patient underwent diagnostic laparoscopic that was converted to open surgery. Tension pneumothorax was encountered intraoperatively and successfully managed. A 2 cm diaphragmatic injury was also noted and repaired with 0-proline suture. The patient survived and was discharged in stable condition.
All patients who underwent immediate surgical intervention following the CT finding of a herniated bowel in the thorax from a ruptured diaphragm had a favorable outcome compared to patients who refused surgery. This finding is consistent with the literature reviewed (6, 14).
Regarding ISS, a retrospective review study conducted on 103 patients with diaphragmatic injuries in a trauma center by Cardoso et al., found that mortality was higher among the patients with ISS greater than 24 (16). In our case series, three patients with ISS less than 24 had favorable outcomes, while six patients with ISS greater than 24 had poor outcomes. Five of the six patients died. One patient with ISS of 41 survived likely due to timely surgical intervention. We have summarized various findings in
Table 1 of this case series.
Conclusion
In conclusion, our study highlights the importance of high suspicion for diaphragmatic injury in cases with rib fractures from the 6th to 12th ribs or high-energy trauma. Patients with ISS greater than 24 had poorer outcomes regardless of the mode of mechanism, except in one case where the patient survived likely due to timely operative intervention. CT radiography helped detect diaphragmatic injury in a few cases but its failure to detect a diaphragmatic injury in one patient highlights the need for timely surgical management, particularly in the setting of high clinical suspicion or severe ISS. Our case series is limited by its sample size which may limit the generalizability of our findings.
Funding
No funding was received for this work.
Informed consent
Retrospective analysis was performed on anonymized data and informed consent was not applicable.
Acknowledgments
Not applicable
Declaration of conflicting interests
The authors declare no conflict of interest.
Ethics approval
This retrospective study was approved by the IRB at Elmhurst Facility on July 5, 2024, with IRB number 24-12-183-05G(HHC)
References
- Merrell, A.J.; Kardon, G. 2014. Development of the diaphragm, a skeletal muscle essential for mammalian respiration. FEBS Journal. PMCID: PMC3879042. [CrossRef] [PubMed]
- Sekusky, A.L.; Lopez, R.A. 2023. Diaphragm Trauma. StatePearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK557647.
- Pober, B.R. 2007. Overview of epidemiology, genetics, birth defects, and chromosome abnormalities associated with CDH. PMCID: PMC2891729. [CrossRef] [PubMed]
- Thiam, O.; Konate, I.; Gueye, M.L.; Toure, A.O.; Seck, M.; Cisse, M.; Diop, B.; Dirie, E.S.; Ka, O.; Thiam, M.; Dieng, M.; Dia, A.; Toure, C.T. Traumatic diaphragmatic injuries: epidemiological, diagnostic and therapeutic aspects. SpringerPlus. 2016, 5, 1614. [Google Scholar] [CrossRef] [PubMed]
- Petrone, P.; Asensio, J.A.; Marini, C.P. Diaphragmatic injuries and post-traumatic diaphragmatic hernias. Curr Probl Surg. 2017, 54, 11–32. [Google Scholar] [CrossRef] [PubMed]
- Zarour, A.M.; El-Menyar, A.; Al-Thani, H.; Scalea, T.M.; Chiu, W.C. Presentations and outcomes in patients with traumatic diaphragmatic injury: a 15-year experience. Journal of Trauma Acute Care Surgery 2013, 74, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Amy, M.A.; Bryce, R.R.H.; Louis, A.; Patrick, B.L.; Heath, D.; Elliott, H.R.; Jeremy, J.; Firas, M.; Srinivas, R.; Patricia, W.; John, C.J. Evaluation and management of traumatic diaphragmatic injuries: A Practice Management Guideline from the Eastern Association for the Surgery of Trauma. Journal of Trauma and Acute Care Surgery 2018, 85, 198–207. [Google Scholar] [CrossRef]
- Matsuda, Y.; Hoshikawa, Y. Traumatic Diaphragmatic Injury. Kyobu Geka 2022, 75, 872–877. [Google Scholar] [PubMed]
- Al-Nouri, O.; Hartman, B.; Freedman, R.; Thomas, C.; Esposito, T. 2012. Diaphragmatic rupture: is management with biological mesh feasible? International Journal of Surgical Case Report 2012, 3, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Pace, M.; Vallati, D.; Belloni, E.; Cavallini, M.; Ibrahim, M.; Rendina, E.A.; Nigri, G. 2021. Blunt Trauma Associated with Bilateral Diaphragmatic Rupture: A Case Report. Frontiers in Surgery. PMCID: PMC8671305. [CrossRef] [PubMed]
- Bonatti, M.; Lombardo, F.; Vezzali, N.; Zamboni, G.A.; Bonatti, G. Blunt diaphragmatic lesions: imaging findings and pitfalls. World Journal of Radiology 2016, 8, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Ercan, M.; Aziret, M.; Karaman, K.; Bostanci, B.; Akoglu, M. Dual mesh repair for a large diaphragmatic hernia defect: an unusual case report. International Journal of Surgical Case Report 2016, 28, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Gwely, N.N. Outcome of blunt diaphragmatic rupture. Analysis of 44 cases. Asian Cardiovascular and Thoracic Annals 2010, 18, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Romaldas, R. Diaphragmatic injuries. European Journal of Cardiothoracic Surgery 2001, 20, 53–57. [Google Scholar] [CrossRef]
- Al-Jehani, Y.; Salah, A.; El-Ghoneimy, Y. Bilateral blunt diaphragmatic rupture. Lung India. 2011, 28, 212. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cardoso, L.F.; Goncalves, M.V.C.; Machado, C.J.; Resende, V.; Fernandes, M.P.; Pastore-Neto, M.; Campanati, R.G.; Reis, G.V.O.P. Retrospective analysis of 103 diaphragmatic injuries in patients operated in a trauma center. Rev Col Bras Cir. 2017, 44, 245–251. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).