1. Introduction
Pediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 / COVID-19 (PIMS-TS) or multisystem inflammatory syndrome in children (MIS-C) is an aftermath of SARS-CoV-2 pandemic [
1,
2,
3]. The cardiovascular system is affected in the majority of patients (typically with left ventricular systolic function deterioration), although cardiac involvement is only temporary in most children.
BMI is known to affect cardiac performance [
4,
5] but its impact on cardiac function recovery in patients after PIMS-TS is still unclear.
The aim of the study was to assess if and how body mass index (BMI) affects the pace of cardiac muscle recovery in children after PIMS-TS.
2. Materials and Methods
A prospective study was conducted in the Department of Pediatric Cardiology between October 2020 and February 2022. Consecutive patients diagnosed with PIMS-TS (according to clinical and laboratory WHO criteria) were followed-up 6 weeks and 6 months after the diagnosis. Patients were divided into normal weight (centile 5th – 85th), overweight and obese (>85th centile) and underweight (<5th centile) groups according to the current CDC criteria.
At control points three-dimensional echocardiography (3D-ECHO) and average global longitudinal strain (GLS) were used to assess ventricular function (Philips, USA, CVx 3D).
Left ventricular ejection fraction (LVEF) was assessed in 3D-ECHO using Philips Dynamic Heart Model (DHM), and right ventricular ejection fraction (RVEF) with 3D Auto RV TomTec algorithm. The average longitudinal strain (GLS Avg) for both ventricles was obtained using TomTec software for two-dimensional apical images.
The study protocol was consistent with the standards of Helsinki Declaration, and was approved by University Bioethical Committee (KB/13/2021). The legal guardians and patients older than 16 years signed informed consent for participation.
Continuous data were expressed as mean and standard deviation (SD) or median and interquartile range. Normal distribution was assessed with the Shapiro-Wilk test. Differences in means between groups were assessed with the paired and unpaired t-test. Categorical data were expressed as percentages. Differences in proportions were compared by means of chi-square analysis (Pearson, with Yates correction when necessary). A 2-sided P value less than 0.05 was considered significant for all tests. Analyses were performed using the statistical package Statistica v. 13.1 software (Dell Inc., Tulsa, OK, USA).
3. Results
The study enrolled 170 consecutive patients aged 1-17 diagnosed with PIMS-TS and controlled in the pediatric cardiology unit. The majority of patients were male (n=115) with the mean age of 8.5+4.43 years. Normal weight children with BMI between 5th and 85th percentile (n=115) accounted for 67.65% of the whole group, while overweight and obese children (n=40) made 23.53% and underweight (n=15) 8.82% of the participants.
At the time of discharge all patients were asymptomatic with normal ventricular systolic function (LVEF and RVEF).
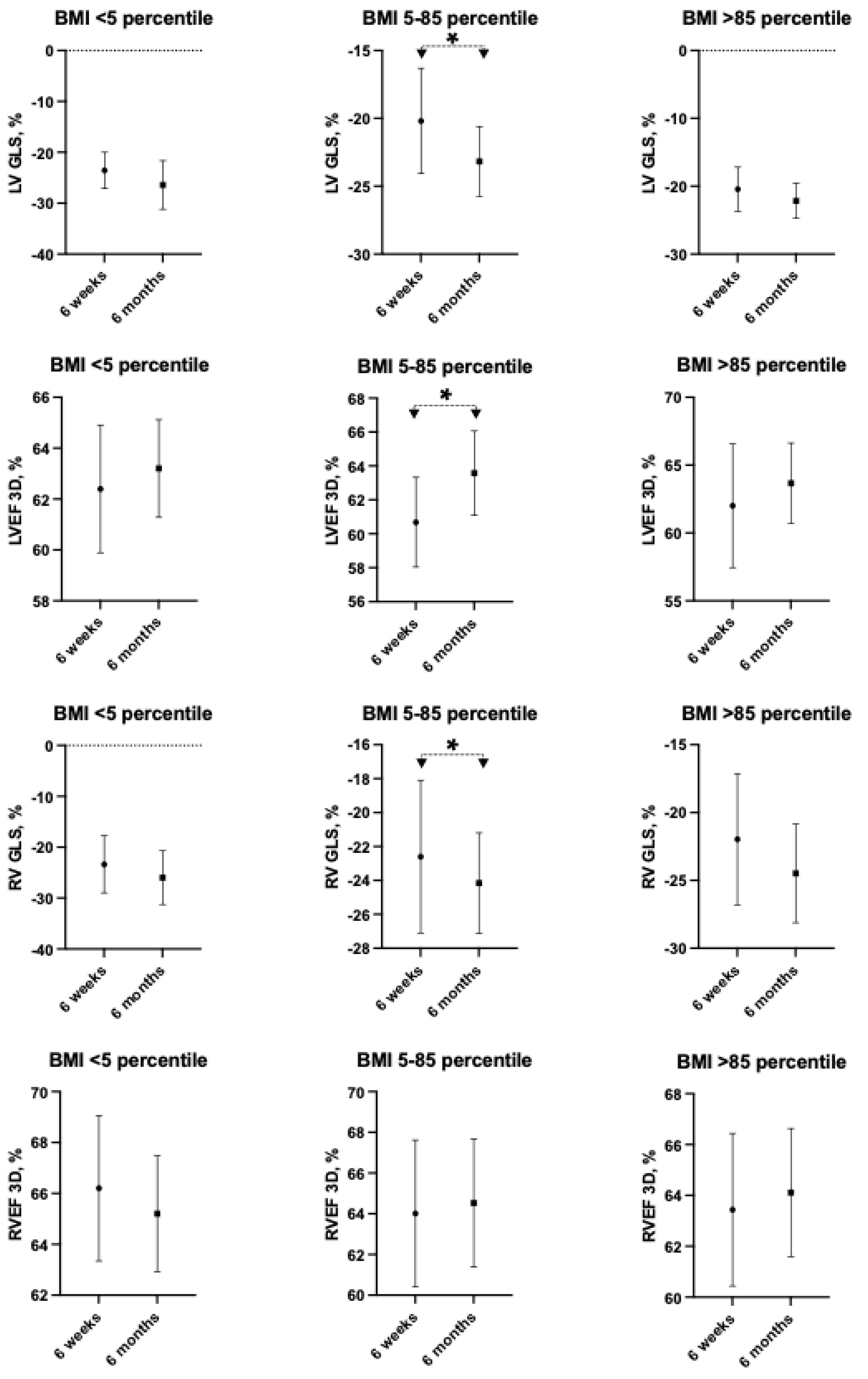
During follow-up 130 children were evaluated after 6 weeks and 72 again after 6 months. For all children, despite their weight status, the means of left and right ventricular ejection fraction (LVEF and RVEF) in 3D-ECHO and average GLS were reported within normal limits at the time of both check-up points. However, in normal weight children the function of left ventricle improved further between 6 weeks and 6 months according to both GLS and LVEF (p<0.05). No significant improvement in left ventricle function was observed in underweight, overweight and obese children between 6 weeks and 6 months according to both GLS and LVEF (
Table 1,
Figure 1).
In patients with BMI >85 percentile the mean of left ventricular GLS after 6 weeks, although in normal range, was significantly lower than in underweight children (respectively: -20.09+2.5% and -23.55+3.55%, p=0.002). Whereas, left ventricle function assessed with 3D-ECHO showed no significant difference in both groups at that time (BMI >85 percentile LVEF 61.15+3.21, BMI <5 percentile LVEF 61.30+2.71, p=0.36).
No significant differences between underweight, normal weight, overweight and obese children were reported after 6 weeks and 6 months for right ventricular function according to both GLS and RVEF. Significant right ventricular function improvement between 6 weeks and 6 months was observed in normal weight children according to GLS (respectively: -22.6+4.51% and -24.16+2.97%, p=0.02), but according to RVEF right ventricular function remained unchanged (p=0.63). In groups of underweight, overweight and obese children right ventricular function presented both as GLS and RVEF showed no significant change after 6 weeks and 6 months.
4. Discussion
In our studied group of 170 patients with PIMS-TS a relatively small portion had abnormal BMI, with only 40 children (less than a quarter) being overweight or obese. This characteristic stays in contrast to other studies involving BMI in analysis, where children with increased BMI represented significantly higher percentage of the population. In the group of children reported by Capone et al. 45% of children were overweight or obese [
6]. In smaller populations from European countries almost half of patients had abnormally high BMI [
7,
8]. Our group’s nutritional status stays in agreement with characteristics of general population of children with PIMS-TS in Poland with 7% of obesity rate [
9,
10] and is consistent with the population of Polish children in general, in which 9.1% of children have excessive BMI [
11].
Interestingly, in the light of current discussion about potential pathophysiological similarity between PIMS-TS with cardiac involvement and myocarditis, Polish population of children suffering from the latter presents with much higher prevalence (45%) of excessive BMI [
12]. The same tendency is also observed in the group of patients with COVID-19-vaccination induced myocarditis [
13].
Due to small percentage of overweight and obese children in our studied population and small ratio/proportion of patients with severe cardiac involvement (also typical for Polish population; only 10 children in our group needed escalated treatment in PICU [
9,
14]) we were not able to establish direct link between excessive BMI and PIMS-TS increased severity or worse outcomes, however this tendency was reported by Khoury et al. in an international cohort study [
8].
In the studied group underweight patients presented significantly higher means of GLS than overweight and obese, therefore the results of the comparison between ventricular mechanics in children with normal and abnormal BMI were similar to those observed and reported for general population by many authors. Kibar et al. [
15] compared a group of 60 obese children aged 10-16 years old (similar to PIMS-TS patients) with healthy controls, noting significantly lower longitudinal strain values in overweight group. Paysal et al. [
5] observed that left ventricular GLS in adolescent girls was affected by BMI with higher values reported in patients with anorexia and lower in obese children (this tendency was not observed for radial and circumferential strain values).
Interestingly, our analysis demonstrated a different pace of ventricular function recovery after PIMS-TS between the children with normal and abnormal (both too low and excessive) BMI, which so far has not been noted in the literature. Even taking into account lower numbers of underweight and overweight children in our group, they demonstrated no tendency to improve ventricular mechanics between 6 weeks and 6 months after the disease, while the means of GLS for both ventricles increased during that time in patients with normal BMI. This tendency may illustrate higher capacity of the muscle for potential improvement in normal weight children, although is visible/noticeable only by GLS and not 3D-ECHO EF. It is worth noting, that the time of observed improvement overlaps with the timing of return to “normal life” and physical activity in most children after PIMS-TS. No marked change in BMI status was apparent in our patients in contrast to the data published by Di Profio et al. [
16], where the means of BMI increased during 6 months of observation after discharge.
In the light of those findings the restrictions of physical activity in children after PIMS-TS should be reconsidered.
As a limitation to our study we must consider that it is a single center study and may not accurately represent trends from general pediatric population. The majority of studied patients had normal BMI which makes this cohort different than in many other countries. We are lacking detailed data on diet and physical activity of underweight and overweight children during the recovery, therefore further prospective observation is required.
Author Contributions
Conceptualization, B.W. and H.K.; methodology, B.W., H.K., A.R.; formal analysis, B.W., H.K.; investigation, H.K, A.R.; data curation, H.K., A.R.; writing—original draft preparation, H.K., A.R.; writing—review and editing, B.W.; supervision, B.W.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Medical University of Warsaw (KB/13/2021, date of approval 18th January 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Felsenstein, S.; Willis, E.; Lythgoe, H.; McCann, L.; Cleary, A.; Mahmood, K.; Porter, D.; Jones, J.; McDonagh, J.; Chieng, A.; et al. Presentation, Treatment Response and Short-Term Outcomes in Paediatric Multisystem Inflammatory Syndrome Temporally Associated with SARS-CoV-2 (PIMS-TS). J. Clin. Med. 2020, 9, 3293. [Google Scholar] [CrossRef] [PubMed]
- Hoste, L.; Van Paemel, R.; Haerynck, F. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur. J. Pediatr. 2021, 180, 2019–2034. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.O.; Goncalves, L.C.; Silva, P.A.N.; Moreira, A.L.E.; Ito, C.R.M.; Peixoto, F.A.O.; Wastowski, I.J.; Carneiro, L.C.; Avelino, M.A.G. Multisystem inflammatory syndrome (MIS-C): a systematic review and meta-analysis of clinical characteristics, treatment, and outcomes. J Pediatr (Rio J) 2022, 98, 338–349. [Google Scholar] [CrossRef] [PubMed]
- Gherbesi, E.; Faggiano, A.; Sala, C.; Carugo, S.; Grassi, G.; Tadic, M.; Cuspidi, C. Left ventricular systolic dysfunction in obesity: a meta-analysis of speckle tracking echocardiographic studies. J. Hypertens. 2024, 42, 1449–1459. [Google Scholar] [CrossRef] [PubMed]
- Paysal, J.; Merlin, E.; Rochette, E.; Terral, D.; Nottin, S. Impact of BMI z-score on left ventricular mechanics in adolescent girls. Front. Pediatr. 2023, 11, 1165851. [Google Scholar] [CrossRef] [PubMed]
- Capone, C.A.; Subramony, A.; Sweberg, T.; Schneider, J.; Shah, S.; Rubin, L.; Schleien, C.; Northwell Health, C.-R.C.; Epstein, S.; Johnson, J.C.; et al. Characteristics, Cardiac Involvement, and Outcomes of Multisystem Inflammatory Syndrome of Childhood Associated with severe acute respiratory syndrome coronavirus 2 Infection. J. Pediatr. 2020, 224, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef] [PubMed]
- Khoury, M.; Harahsheh, A.S.; Raghuveer, G.; Dahdah, N.; Lee, S.; Fabi, M.; Selamet Tierney, E.S.; Portman, M.A.; Choueiter, N.F.; Elias, M.; et al. Obesity and Outcomes of Kawasaki Disease and COVID-19-Related Multisystem Inflammatory Syndrome in Children. JAMA Netw. Open 2023, 6, e2346829. [Google Scholar] [CrossRef] [PubMed]
- Ludwikowska, K.M.; Okarska-Napierała, M.; Dudek, N.; Tracewski, P.; Kusa, J.; Piwoński, K.P.; Afelt, A.; Cysewski, D.; Biela, M.; Werner, B.; et al. Distinct characteristics of multisystem inflammatory syndrome in children in Poland. Sci. Rep. 2021, 11, 23562. [Google Scholar] [CrossRef] [PubMed]
- Okarska-Napierala, M.; Ludwikowska, K.M.; Szenborn, L.; Dudek, N.; Mania, A.; Buda, P.; Ksiazyk, J.; Mazur-Malewska, K.; Figlerowicz, M.; Szczukocki, M.; et al. Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register. J. Clin. Med. 2020, 9, 3386. [Google Scholar] [CrossRef] [PubMed]
- Gajewska, D.; Harton, A. Current nutritional status of the Polish population – focus on body weight status. J. Health Inequalities 2023, 9, 154–160. [Google Scholar] [CrossRef]
- Jarecka, M.; Kamińska, H.; Werner, B. 10 years of myocarditis in children – a single-centre retrospective study. Paediatrcs Fam. Med. 2022, 18, 152–156. [Google Scholar] [CrossRef]
- Puchalski, M.; Kamińska, H.; Bartoszek, M.; Brzewski, M.; Werner, B. COVID-19-Vaccination-Induced Myocarditis in Teenagers: Case Series with Further Follow-Up. Int. J. Env. Res. Public. Health 2022, 19, 3456. [Google Scholar] [CrossRef] [PubMed]
- Kaminska, H.; Roznowska-Wojtowicz, A.; Cacko, A.; Okarska-Napierala, M.; Kuchar, E.; Werner, B. Three-Dimensional Echocardiography and Global Longitudinal Strain in Follow-Up After Multisystem Inflammatory Syndrome in Children: Six-Month, Single-Center, Prospective Study. J. Pediatr. 2023, 260, 113516. [Google Scholar] [CrossRef] [PubMed]
- Kibar, A.E.; Pac, F.A.; Ece, I.; Oflaz, M.B.; Balli, S.; Bas, V.N.; Aycan, Z. Effect of obesity on left ventricular longitudinal myocardial strain by speckle tracking echocardiography in children and adolescents. Balk. Med. J. 2015, 32, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Di Profio, E.; Leone, A.; Vizzuso, S.; Fiore, G.; Pascuzzi, M.C.; Agostinelli, M.; Dilillo, D.; Mannarino, S.; Fiori, L.; D'Auria, E.; et al. Longitudinal Anthropometry and Body Composition in Children With SARS-CoV-2-Associated Multisystem Inflammatory Syndrome. J. Pediatr. Gastroenterol. Nutr. 2023, 76, 505–511. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).