1. Introduction
Neonatal sepsis is a systemic condition caused by any microorganism (bacterial, viral, parasitic or fungal) that is associated with clinical manifestations and results in morbidity and mortality [
1,
2,
3] . Bacterial infectious etiologies are traditionally described as the cause of this neonatal condition, with the most commonly suspected foci being urine, circulatory, pulmonary and even meningeal involvement [
4,
5]. Causing costs to the health system in terms of the need for hospital admission, diagnostic tests and the need for antimicrobial therapy [
6] . This is a major overuse of antimicrobials, with the additional impact known as in the modification of the neonatal microbiota, selection pressure for antibiotic resistance, etc. [
7] .
In 2022, 2.3 million children died in the first 28 days of life, accounting for 47% of under-five deaths. The main causes of neonatal mortality include premature birth, birth complications, neonatal infections and congenital anomalies. Sub-Saharan Africa and South Asia are the most affected regions, with neonatal mortality rates of 27 and 21 per 1000 live births, respectively. Newborns in these regions have a risk of death up to 11 times higher than in countries with the lowest rates, such as Australia and New Zealand [
8,
9] .
Few publications highlight the role of dengue virus as a cause of fever in neonates and cause of neonatal sepsis, even in endemic areas. The expected hematological manifestations in the course of dengue infection commonly described are leukopenia, relative neutropenia, thrombocytopenia, which represents a challenge in the diagnostic and therapeutic approach to neonates with fever given the association described in the literature of the alteration of these hematological parameters with possible association with early and late sepsis of bacterial origin [
10,
11,
12] .
The introduction should briefly place the study in a broad context and highlight why it is important. It should define the purpose of the work and its significance. The current state of the research field should be carefully reviewed and key publications cited. Please highlight controversial and diverging hypotheses when necessary. Finally, briefly mention the main aim of the work and highlight the principal conclusions. As far as possible, please keep the introduction comprehensible to scientists outside your particular field of research. References should be numbered in order of appearance and indicated by a numeral or numerals in square brackets—e.g., [
1] or [
2,
3], or [
4,
5,
6]. See the end of the document for further details on references.
2. Clinical Case
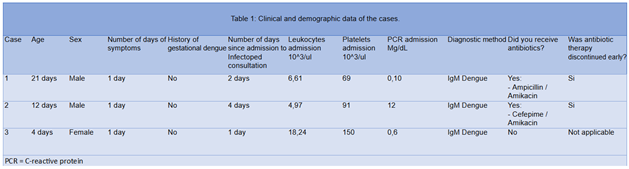
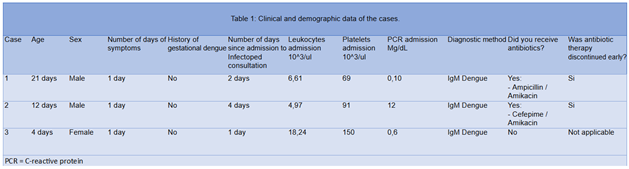
Patient 1: Term newborn admitted at 21 days of life, consulted for 2 days of unquantified thermal rises with no other alteration, no relevant history at delivery, mother asymptomatic 15 days prior to delivery. Admitted for suspicion of late sepsis, normal physical examination, with admission laboratories (Table 1). with thrombocytopenia 69.000/mL, C Reactive protein (CRP) and procalcitonin (PCT) negatives, serial cultures (blood, urine) were taken, urine culture negative, ampicillin / amikacin was started under referred diagnosis. Infection diseases (ID) evaluation was made on 2 of admission, with negative cultures, an IgM for dengue was ordered on the same day, positive report for IgM was reported, antibiotics were suspended and was started on intravenous fluids according to response, he was discharged on day 6 of hospitalization without complications in follow-up and a safe discharge.
Patient 2: Male newborn at term with adequate birth weight, mother 20 years old, first gestation, pregnancy with 6 prenatal controls, cesarean delivery due to cephalopelvic disproportion, with early discharge due to no complications. He was readmitted at 8 days of life due to clinical symptoms of 2 hours of evolution of thermal rises, at admission paraclinics with hemogram without leukocyte or platelet alteration, positive CRP, negative PCT, Considered admission to the intermediate care unit for clinical surveillance, due to persistent thermal rises, started management with cefepime / amikacin. Infectious disease evaluation is indicated. Upon questioning by the infectious diseases service, the mother of the patient was hospitalized for 3 days with a clinical picture of thermal rises associated with myalgias, arthralgias, abdominal pain, hemogram with leukopenia, thrombocytopenia, elevated transaminases, a differential diagnosis with neonatal dengue fever was considered, Dengue IgM was requested with positive report, diagnosis of dengue with alarm signs was confirmed, and suspension of antimicrobial therapy was indicated. The patient was discharged by the infectious disease service, with medical discharge on the eighth day of hospitalization, without complications.
Patient 3: Newborn at term with low birth weight, mother of 19 years, with well-controlled pregnancy, vaginal birth with adequate adaptation, without complications. Admitted at 4 days of life due to feeding problems, evaluated by pediatrics with paraclinics and hemogram with polycythemia, so they indicate management with salinoferesis, in control hemogram evidence of thrombocytopenia 119,000/mL He was evaluated by the infectious diseases service with a report of positive IgM dengue, a diagnosis of neonatal dengue was made and symptomatic management was established. No need to suspend antimicrobial therapy. Mother with no data of gestational dengue infection. Finally, blood cultures were negative, and the patient was discharged on the sixth day of hospitalization without complications.
3. Discussion
Dengue is a neglected infection in neonatal population.
There is a low index of suspicion in vertical cases, that are the most commonly reported, and less suspected in late onset neonatal sepsis, without any guidelines for diagnosis or specific treatment in this age [
13,
14] .
In the literature there are reports of clinical cases of neonatal dengue, Juarez and
colleagues described a series of 5 cases of neonates with dengue in Mexico [
15] Likewise, Romero and collaborators described a series of 7 cases of neonatal dengue [
16] . However, both articles are based on the presentation of vertically transmitted dengue.
This study demonstrates the presence of neonatal dengue not related to vertical transmission, as a differential diagnosis in the approach to late neonatal sepsis in endemic countries in the neonatal population in whom a different viral, bacterial or parasitic etiology cannot be demonstrated, with adequate clinical response, rapid suspension of antibiotics and early discharge. All the diagnoses of neonatal dengue achieved in our experience were diagnosed with positive IgM, which we consider diagnostic in this population since IgM does not cross the placenta. In 1 of the cases it was possible to confirm with IgG seroconversion, which proves our proposal.
An ideal scenario in which molecular testing or NS1 antigen would significantly strengthen the capacity for early detection of dengue in neonates with suspected sepsis in endemic areas. The implementation of these diagnostic tests in the initial phase of the approach would allow rapid identification of the presence of the virus and reduce the need for prolonged empirical antibiotic treatment.
It is important to remember that early discontinuation of antibiotics reduces the consequences of antibiotic use such as changes in the microbiota, a risk factor for the appearance of diseases such as obesity, diabetes, asthma and changes in the immune response, changes in the production of metabolites and amino acids [
17].
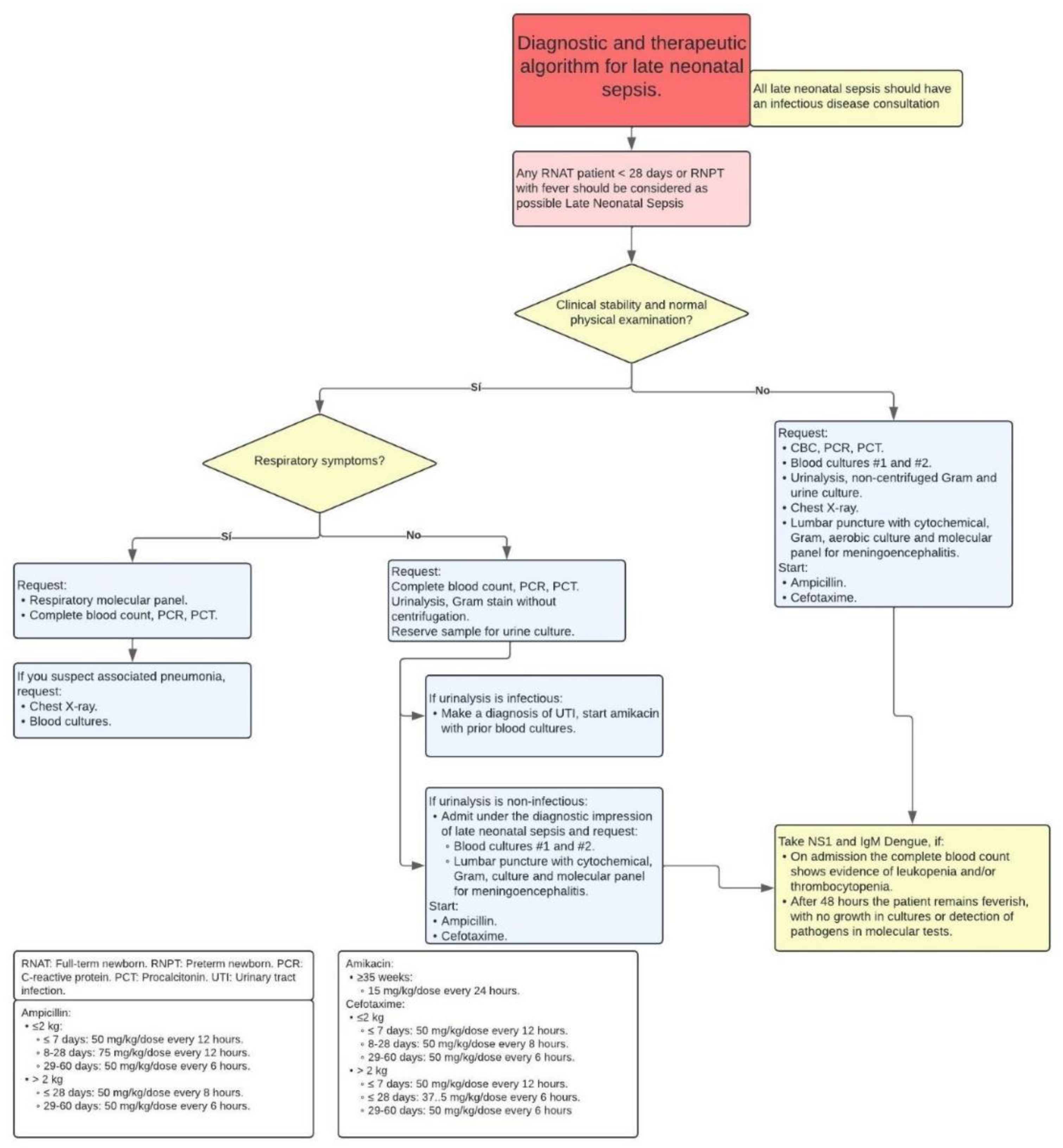
Therefore, we propose the need to establish a diagnostic and therapeutic algorithm of late neonatal sepsis for dengue endemic areas that contemplates the differential diagnosis of infection by these arboviruses, where the addition of NS1 antigen and/or PCR is insisted according to availability. However, insisting that IgA, IgM and IgE antibodies do not cross the blood-placental barrier, therefore, the detection of this type of antibodies can be useful to demonstrate the evidence of current infection of the neonate [
16,
18] (
Figure 1).
It is important to recognize that exposure to the mosquito vector of dengue in endemic areas begins at birth, so neonates are at risk of acquiring this infection early. Despite their young age and the inherent vulnerability of their developing immune system, the cases presented did not show evidence of serious complications, which could suggest a protective effect in this population. This finding opens a relevant line of research on the possible passive transmission of homotypic antibodies from seropositive mothers to their newborns. Future studies could evaluate whether these antibodies, acquired by placental transfer, confer partial or total immunity against dengue at the neonatal stage, this would not only have implications for early prevention but would also contribute to the design of clinical and vaccination strategies in regions with a high prevalence of dengue.
4. Conclusions
Dengue is the most common vector-borne infection in the world. More than 340 million people may be at risk and this includes the neonate, whose route of transmission other than the mother-child route exists and must be recognized.
The manifestations of late neonatal bacterial sepsis overlap with many of the hematologic features of symptomatic dengue in the neonatal period, so it is necessary to propose a comprehensive diagnostic approach algorithm that integrates the most common causes and the proposed workflow for the confirmation and/or exclusion of dengue in endemic countries.
References
- Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Vol. 390, The Lancet. Lancet Publishing Group; 2017. p. 1770–80. [CrossRef]
- Fernández Colomer B, Sastre JL, Coto GD, Aparicio AR, Fernández AI. Sepsis del recién nacido [Internet]. Available from: www.aeped.es/protocolos/.
- Cortés JS, Fernández Cruz LX, Beltrán Zúñiga E, Narváez CF, Fonseca-Becerra CE. Sepsis neonatal: aspectos fisiopatológicos y biomarcadores. Revista Médicas UIS. 2020 Jan 30;32(3):35–47. [CrossRef]
- Bethou A, Bhat BV. Neonatal Sepsis—Newer Insights. Vol. 89, Indian Journal of Pediatrics. Springer; 2022. p. 267–73. [CrossRef]
- León GLD, Valle DIC, Sanchez JDU, Robalino ASA, Stefania MSM, Asencio REO, et al. Revisión bibliográfica: Sepsis neonatal provocado por infección de vías urinarias materna, revisión de protocolos. Brazilian Journal of Health Review. 2023 Aug 25;6(4):18713–25. [CrossRef]
- Cussen A, Guinness L. Cost savings from use of a neonatal sepsis calculator in Australia: A modelled economic analysis. J Paediatr Child Health. 2021 Jul 1;57(7):1037–43. [CrossRef]
- Sturrock S, Sadoo S, Nanyunja C, Le Doare K. Improving the Treatment of Neonatal Sepsis in Resource-Limited Settings: Gaps and Recommendations. Res Rep Trop Med. 2023 Dec;Volume 14:121–34. [CrossRef]
- World Health Organization. WHO. Newborn mortality. WHO. . 2024.
- Rosa-Mangeret F, Benski AC, Golaz A, Zala PZ, Kyokan M, Wagner N, et al. 2.5 Million Annual Deaths—Are Neonates in Low-and Middle-Income Countries Too Small to Be Seen? A Bottom-Up Overview on Neonatal Morbi-Mortality. Vol. 7, Tropical Medicine and Infectious Disease. MDPI; 2022.
- Worku M, Aynalem M, Biset S, Woldu B, Adane T, Tigabu A. Role of complete blood cell count parameters in the diagnosis of neonatal sepsis. BMC Pediatr. 2022 Dec 1;22(1). [CrossRef]
- Adane T, Worku M, Tigabu A, Aynalem M. Hematological Abnormalities in Culture Positive Neonatal Sepsis. Pediatric Health Med Ther. 2022 Jun;Volume 13:217–25. [CrossRef]
- Nguyen TM, Huan VT, Reda A, Morsy S, Nam Giang HT, Tri VD, et al. Clinical features and outcomes of neonatal dengue at the Children’s Hospital 1, Ho Chi Minh, Vietnam. Journal of Clinical Virology. 2021 May 1;138. [CrossRef]
- Yadav B, Gupta N, Gadepalli R, Nag VL. Neonatal dengue: an under-diagnosed entity. BMJ Case Rep. 2021 Aug 16;14(8). [CrossRef]
- World Health Organisation W. Available: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue. 2020. Dengue and severe dengue.
- Juárez Campos CE, Duran Guerra D, Ceja Mejía ÓE, Cortez Comparan D, Baeza Casillas JA, Díaz Santana Bustamante DE, et al. Dengue neonatal: serie de casos**. Revista Latinoamericana de Infectología Pediátrica. 2022;35(2):81–5.
- Romero-Santacruz E, Lira-Canul JJ, Pacheco-Tugores F, Palma-Chan AG. Dengue neonatal. Presentación de casos clínicos. Ginecol Obstet Mex. 2015;83:308–15. [CrossRef]
- Patangia D V., Anthony Ryan C, Dempsey E, Paul Ross R, Stanton C. Impact of antibiotics on the human microbiome and consequences for host health. Vol. 11, MicrobiologyOpen. John Wiley and Sons Inc; 2022. [CrossRef]
- Remington J. Infectious diseases of the fetus and the newborn infant. 7th ed. 2011.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).