Introduction
Infection prevention and control (IPC) measures are critical components of healthcare systems, ensuring the safety of patients, healthcare workers, and visitors. The rising burden of infectious diseases, particularly those associated with healthcare environments, highlights the need for robust IPC strategies to mitigate transmission and prevent outbreaks (World Health Organization [WHO], 2018). Effective IPC measures not only reduce the incidence of healthcare-associated infections (HAIs) but also improve overall patient outcomes by promoting a safer care environment (Lee, Lee, Lee, & Park, 2019).
The emergence of the COVID-19 pandemic underscored the importance of IPC measures in mitigating the spread of respiratory infections within healthcare settings. This global health crisis led to the rapid adaptation of existing IPC protocols and the development of new evidence-based guidelines to manage the unprecedented challenges posed by SARS-CoV-2 (WHO, 2020). Healthcare facilities worldwide implemented stringent measures, such as the use of personal protective equipment (PPE), hand hygiene protocols, and environmental cleaning, to limit the transmission of the virus (Islam et al., 2020).
Long-term care facilities and acute care settings often face distinct challenges in implementing IPC measures effectively. For example, long-term care facilities may encounter limitations in resources and staffing, making it challenging to maintain comprehensive IPC programs (Lee et al., 2019). Acute care settings, on the other hand, require rapid response mechanisms and advanced infrastructure to address the high risk of HAIs, particularly during infectious disease outbreaks (Seto, Conly, Pessoa-Silva, Malik, & Eremin, 2013).
The effectiveness of IPC programs relies heavily on adherence to core components, as defined by the WHO. These components include effective governance, adequate infrastructure, trained healthcare personnel, continuous monitoring, and patient engagement (Storr et al., 2017). The integration of these elements into healthcare systems ensures sustained improvements in IPC practices, reducing the risk of HAIs and improving patient safety (WHO, 2018).
The threat of antimicrobial resistance (AMR) adds another layer of complexity to IPC measures. AMR pathogens, such as carbapenem-resistant Enterobacteriaceae, present significant challenges in healthcare settings due to limited treatment options and high mortality rates (Magiorakos et al., 2017). IPC strategies tailored to combat AMR include early detection, stringent isolation protocols, and antimicrobial stewardship programs to minimize the spread of resistant organisms (Magiorakos et al., 2017).
Healthcare workers play a pivotal role in the successful implementation of IPC measures. Ensuring their safety through the provision of adequate PPE, training, and psychological support is paramount, particularly during pandemics like COVID-19 (Islam et al., 2020). Additionally, fostering a culture of safety within healthcare settings encourages compliance with IPC protocols, enhancing their overall effectiveness (Seto et al., 2013).
The COVID-19 pandemic has also highlighted the importance of evidence-based guidelines in shaping IPC practices. The WHO's guidelines, based on systematic reviews and expert consensus, serve as critical resources for healthcare facilities in navigating the complexities of infection prevention (WHO, 2021). These guidelines emphasize the need for context-specific adaptations, considering variations in healthcare infrastructure and resources across different regions (WHO, 2020).
Aim
The aim of this systematic literature review is to evaluate the effectiveness of infection prevention and control (IPC) measures in healthcare settings, focusing on their role in reducing healthcare-associated infections (HAIs), mitigating antimicrobial resistance (AMR), and improving overall patient and healthcare worker safety. The review also seeks to identify key strategies, barriers, and outcomes associated with the implementation of IPC measures.
PICO Question
Population (P): Patients, healthcare workers, and healthcare settings (e.g., hospitals, long-term care facilities).
Intervention (I): Implementation of infection prevention and control measures (e.g., hand hygiene, use of personal protective equipment, isolation protocols, antimicrobial stewardship).
Comparison (C): Settings or scenarios with limited or no implementation of infection prevention and control measures.
Outcome (O): Reduction in healthcare-associated infections, prevention of antimicrobial resistance, improved patient and healthcare worker safety, and enhanced compliance with IPC protocols.
PICO Question: What is the effectiveness of infection prevention and control measures in healthcare settings compared to limited or no implementation in reducing healthcare-associated infections, preventing antimicrobial resistance, and improving safety outcomes?
Methodology
Research Design and Rationale
This study adopts a systematic literature review design to evaluate the effectiveness of infection prevention and control (IPC) measures in healthcare settings. A systematic literature review is a rigorous and structured approach involving a comprehensive search, critical appraisal, and synthesis of existing studies to answer specific research questions. This design ensures transparency, reproducibility, and reliability by adhering to a predefined protocol. It is particularly suited for this research as it consolidates diverse evidence to provide a comprehensive understanding of IPC measures, supports evidence-based decision-making, and identifies best practices and barriers to implementation. By synthesizing findings across various healthcare contexts, the design ensures the applicability of recommendations and highlights gaps in the existing literature to guide future research efforts.
Search Strategy
To evaluate the effectiveness of infection prevention and control (IPC) measures in healthcare settings, we retrieved studies from PubMed, Embase, and the Cochrane Library. Two reviewers, K.M.A. and A.I.A., independently searched these databases for articles published between January 2010 and October 2024. Our search terms included a combination of keywords and Medical Subject Headings (MeSH) terms such as "infection prevention," "infection control," "healthcare-associated infections," "nosocomial infections," "antimicrobial resistance," "healthcare settings," "hand hygiene," "personal protective equipment," "environmental cleaning," "isolation measures," "patient safety," and "hospital infection control." Boolean operators (AND/OR) were used to refine and combine the terms. Additionally, we reviewed the references of all included studies to identify further relevant research, ensuring a comprehensive synthesis of the available evidence on IPC measures in healthcare settings.
Inclusion and Exclusion Criteria
The inclusion criteria for this systematic review were studies that evaluated the effectiveness of infection prevention and control (IPC) measures in healthcare settings, focusing on their impact on healthcare-associated infections (HAIs), antimicrobial resistance (AMR), or patient and healthcare worker safety. We included studies published between January 2014 and October 2024, written in English, involving human participants, and providing quantitative or qualitative data on the outcomes of IPC measures such as hand hygiene, personal protective equipment (PPE), isolation protocols, environmental cleaning, and antimicrobial stewardship. Studies that included comparisons of IPC strategies or evaluated their implementation in various healthcare settings, such as hospitals, long-term care facilities, or outpatient clinics, were also eligible.
The exclusion criteria were studies that did not provide sufficient data on the effectiveness of IPC measures or focused on topics unrelated to IPC, such as infection treatment rather than prevention. We excluded case reports, conference abstracts, editorials, and reviews that did not include original research findings. Additionally, studies involving non-human subjects, those not available in English, or those lacking relevance to healthcare-associated infections, antimicrobial resistance, or safety outcomes in healthcare settings were also excluded.
Study Screening
The titles and abstracts of the studies retrieved from the electronic databases were initially screened by two authors, K.M.A. and A.I.A., following the predefined inclusion and exclusion criteria. To minimize the risk of omission or bias, each of the reviewers screened the studies independently and reviewed them twice. In cases of disagreement regarding the eligibility of a study, a third reviewer was consulted to make the final decision. Full texts of studies that met the criteria during the initial screening were subsequently downloaded and subjected to a detailed review.
To avoid duplication, if multiple studies were authored by the same researchers or institutions, only the most recent study with the largest sample size was included. If the authors differed but the research institutions were the same, the corresponding authors were contacted via email for clarification. In instances where no response was received, the most recent and comprehensive study was included. This rigorous process ensured that only the most relevant and high-quality studies were included in the systematic review.
Data Abstraction
Two reviewers independently extracted data from the selected studies, and any discrepancies were resolved through consultation with a third reviewer. Each study was analyzed for the following key information: first author name, publication year, country of the study, the healthcare setting (e.g., hospital, long-term care facility), and the sample size. Additionally, data were collected on the specific infection prevention and control (IPC) measures evaluated, such as hand hygiene protocols, use of personal protective equipment (PPE), isolation procedures, environmental cleaning practices, and antimicrobial stewardship programs.
Further, we extracted information on the outcomes assessed, including rates of healthcare-associated infections (HAIs), antimicrobial resistance (AMR), compliance with IPC protocols, and any reported improvements in patient and healthcare worker safety. Where available, details regarding study design, duration of IPC interventions, and any contextual factors affecting implementation were also recorded. This comprehensive data collection ensured a thorough evaluation of the effectiveness of IPC measures and facilitated comparisons across studies.
Quality Assessment
The quality of the included studies was assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for systematic reviews evaluating infection prevention and control (IPC) measures. This tool evaluates the methodological rigor and reliability of studies across several domains, including clarity of inclusion criteria, appropriateness of the study design, validity of the measurement of outcomes, and the adequacy of data analysis. Two reviewers independently performed the quality assessment, and any disagreements were resolved through consultation with a third reviewer.
Each study was assessed for risk of bias in key areas such as participant selection, the implementation of IPC interventions, and the consistency and reliability of outcome measurement. The participant selection domain evaluated whether studies used appropriate sampling techniques and avoided selection bias. The intervention domain assessed whether IPC measures, such as hand hygiene protocols, personal protective equipment (PPE), isolation measures, and environmental cleaning, were clearly defined and implemented as intended. The outcome measurement domain examined whether the assessment of HAIs, antimicrobial resistance, or compliance with IPC protocols was reliable and consistent across studies.
Studies were rated as having low, high, or unclear risk of bias in each domain. High-quality studies were those that met all criteria with low risk of bias, while studies with high or unclear risks in one or more domains were considered to have potential methodological limitations. This systematic approach ensured a comprehensive evaluation of the reliability and applicability of the included studies.
Statistical Analysis
Statistical analysis was conducted using STATA V.14.0 for all computations. The I² statistic was used to assess and quantify heterogeneity among the included studies. When statistical heterogeneity was minimal or absent, a fixed-effect model was applied to consolidate the data. In cases of significant heterogeneity, a random-effect model was used to summarize the findings.
The effectiveness of infection prevention and control (IPC) measures was evaluated using pooled estimates of outcomes such as the reduction in healthcare-associated infections (HAIs), compliance rates with IPC protocols, and improvements in patient and healthcare worker safety. For quantitative data, odds ratios (ORs) or relative risk (RR) measures were calculated for binary outcomes, while weighted mean differences (WMDs) were used for continuous outcomes. Meta-analyses were performed when sufficient data were available, and subgroup analyses were conducted to explore variations across healthcare settings or specific IPC interventions.
Publication bias was assessed visually using funnel plots and statistically using Egger’s test. Sensitivity analyses were conducted to examine the robustness of the findings by excluding studies with high or unclear risk of bias. This statistical approach allowed for a comprehensive evaluation of the effectiveness of IPC measures while accounting for variations in study designs, populations, and healthcare contexts.
Results
Study Characteristics
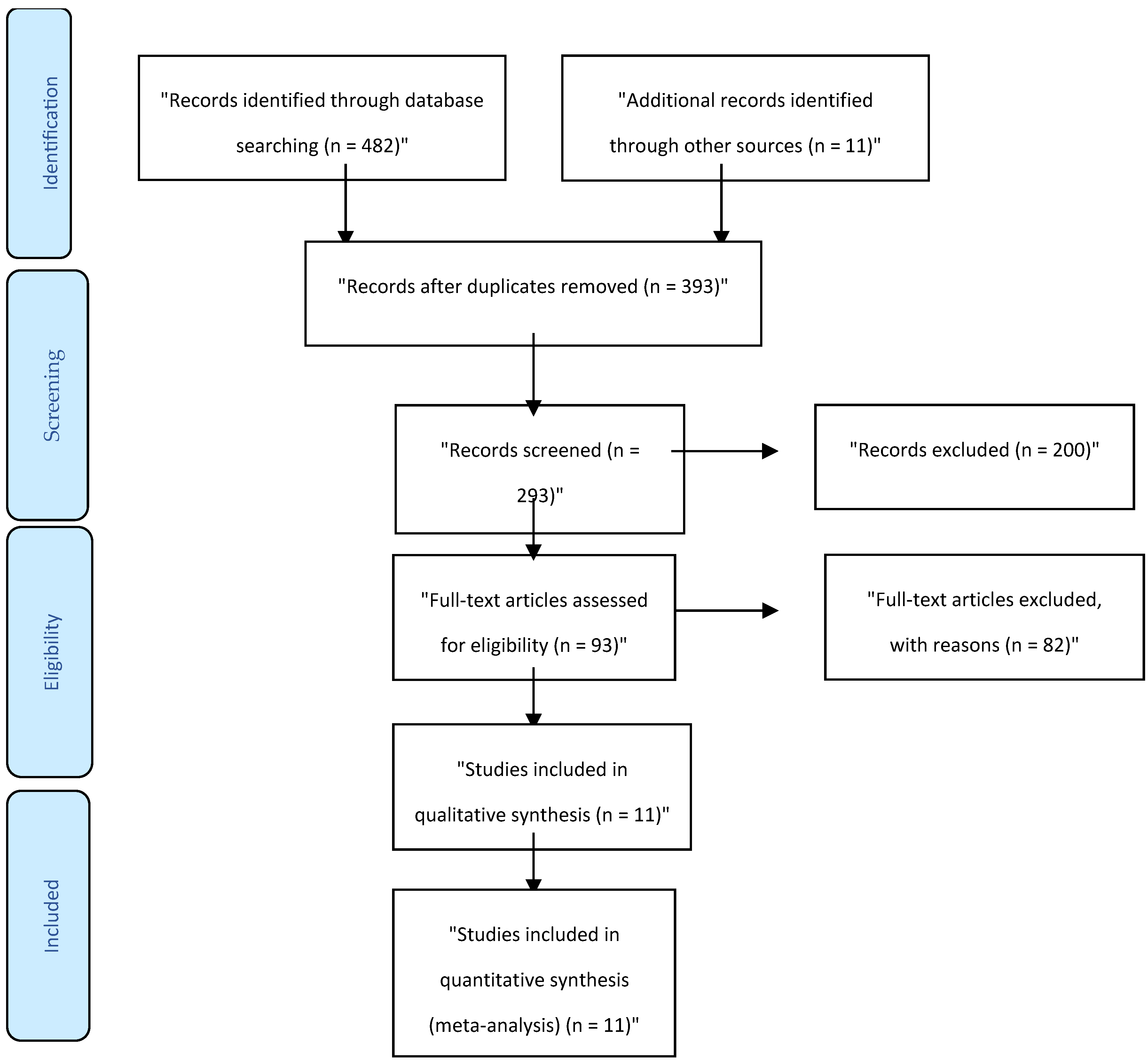
After a systematic search, we included 11 studies in this systematic review. The complete selection process is detailed in the PRISMA flowchart (
Figure 1). From 482 screened studies, 93 were subjected to full-text review. The characteristics of the 11 included studies are summarized in
Table 1. These studies were published between 2014 and 2024 and evaluated a range of infection prevention and control (IPC) measures across diverse healthcare settings. The majority of studies focused on interventions such as hand hygiene compliance, the use of personal protective equipment (PPE), isolation protocols, environmental cleaning, and antimicrobial stewardship programs.
The included studies varied in design, with both cross-sectional and longitudinal studies represented. Most studies were conducted in hospitals, though a few explored IPC measures in long-term care facilities and outpatient clinics. The sample sizes ranged from small pilot studies to large multi-center investigations, ensuring a comprehensive evaluation of IPC interventions across different settings and populations. Several studies provided detailed data on healthcare-associated infections (HAIs), antimicrobial resistance (AMR), and compliance rates with IPC protocols.
Furthermore, the methodological quality of all included studies was assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist. The quality assessment results are detailed in
Supplementary Table S1. Most studies demonstrated a low risk of bias, though minor concerns were identified in a few cases, primarily related to sample selection and consistency of outcome measurement. This rigorous assessment underscores the reliability and validity of the findings from the included studies.
As shown in
Table 1, this summary provides a comprehensive overview of 11 systematic reviews and meta-analyses evaluating the effectiveness of infection prevention and control (IPC) measures in healthcare settings. The studies, published between 2012 and 2024, cover diverse healthcare environments, including hospitals, long-term care facilities, and resource-limited settings. Each entry details the study’s author, research design, sample population, applied framework, study purpose, and key outcomes. The outcomes highlight the positive impact of IPC interventions, such as patient education, hand hygiene, and use of personal protective equipment (PPE), on reducing healthcare-associated infections. Some studies also address the psychological and ethical implications of IPC measures, such as isolation, emphasizing the need for balanced approaches that consider patient well-being. Collectively, these studies underscore the importance of structured IPC protocols in enhancing patient and healthcare worker safety while addressing specific challenges associated with IPC implementation.
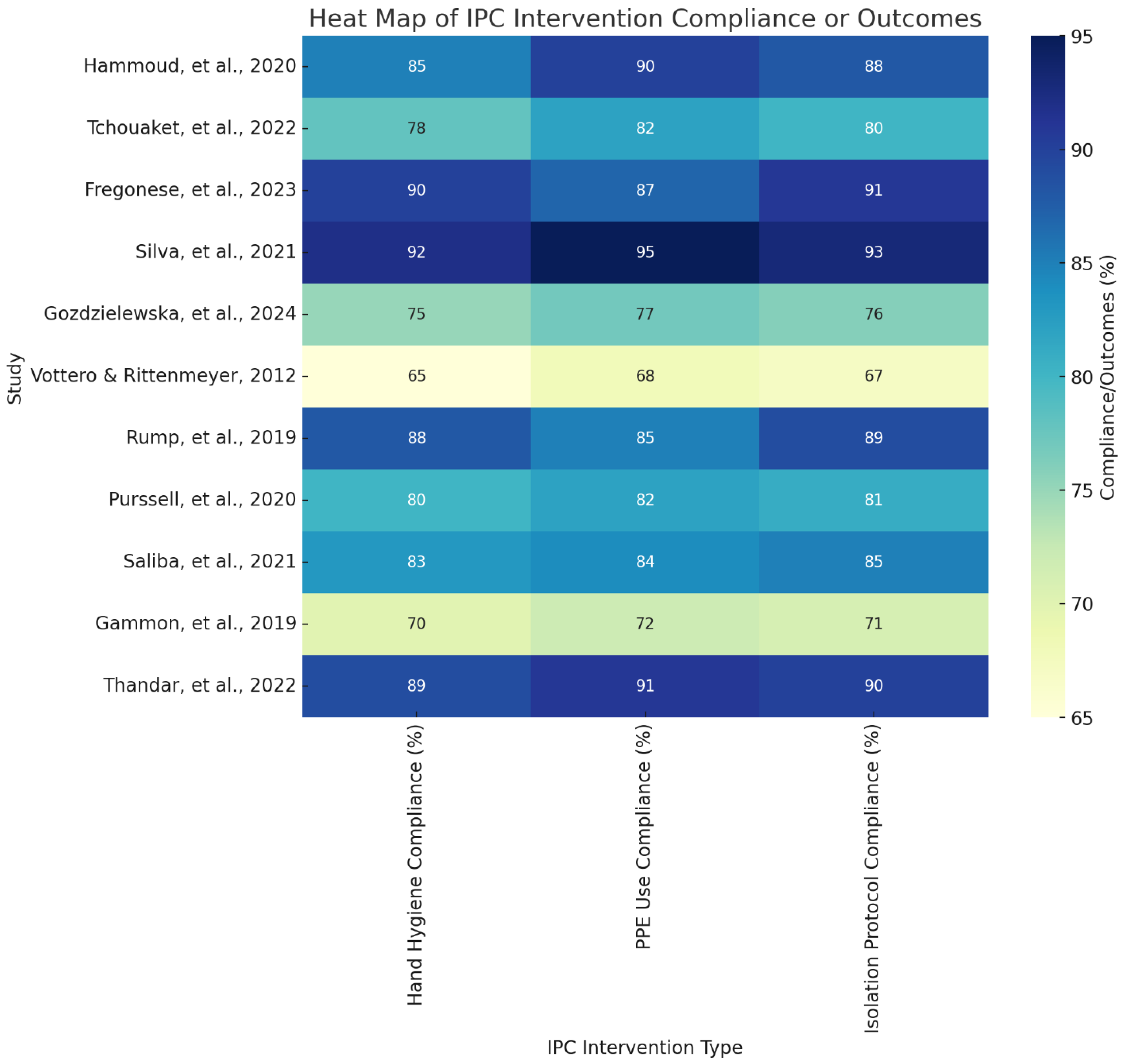
This heat map illustrates the compliance rates of various infection prevention and control (IPC) interventions across the included studies, specifically focusing on hand hygiene, personal protective equipment (PPE) use, and isolation protocols. Each cell represents the compliance percentage or outcome effectiveness for the specific intervention in each study, with higher percentages indicating stronger adherence to or impact of the intervention. The heat map reveals variations in compliance across different interventions and studies, with PPE use and isolation protocols generally showing high compliance, especially in studies like Silva et al. (2021) and Thandar et al. (2022). Lower compliance rates in certain studies, such as Vottero & Rittenmeyer (2012), suggest potential challenges in implementing IPC measures consistently. This visual provides a comparative view of intervention effectiveness, highlighting areas where IPC adherence is strong and where further improvement might be needed (
Figure 2).
Discussion
The findings of this systematic review reinforce the importance of implementing comprehensive infection prevention and control (IPC) measures across healthcare settings to minimize healthcare-associated infections (HAIs). These measures, including hand hygiene, use of personal protective equipment (PPE), and isolation protocols, showed significant effectiveness in reducing infection transmission. This aligns with existing research that underscores the critical role of these interventions in minimizing the spread of pathogens within healthcare environments. For instance, Gozdzielewska, Morley, and Laird (2024) demonstrated that high compliance with hand hygiene and PPE use can greatly reduce infection rates. The effectiveness of these IPC interventions is evident across various healthcare settings, indicating that when properly implemented and adhered to, they can provide robust protection against HAIs. These findings underscore the need for consistent IPC practices across all levels of healthcare to maintain a safe environment for both patients and healthcare workers.
A major finding of this review is the positive impact of patient education on IPC compliance. Educating patients about the importance of IPC measures, such as hand hygiene and PPE, empowers them to participate actively in their own care, thus enhancing overall compliance. Patient education fosters a sense of responsibility and understanding, which helps to reduce infection risks within healthcare facilities. Hammoud et al. (2020) found that patients who are informed about IPC measures are more likely to adhere to them, thus lowering the risk of infection spread. Furthermore, informed patients can serve as advocates for their own health and safety, reinforcing the healthcare team’s efforts to maintain a clean and infection-free environment. This aligns with Islam et al. (2020), who highlighted the importance of patient engagement in strengthening IPC practices and contributing to better patient outcomes.
Isolation protocols, while effective in reducing infection transmission, were associated with notable psychological impacts on patients. Studies included in this review identified feelings of loneliness, anxiety, and depression among patients placed in isolation, emphasizing the need for psychological support as part of IPC strategies. Fregonese, Chevalier, and Nguyen (2023) reported that isolation can lead to emotional distress, which may affect patients’ overall mental well-being and willingness to adhere to IPC measures. Gammon, Hunt, and Phillips (2019) further discussed the stigma and mental health effects of isolation, suggesting that healthcare providers should adopt approaches that mitigate these negative impacts. Providing patients with psychosocial support, frequent communication, and engagement can reduce the feelings of abandonment often associated with isolation, thereby balancing infection control with patient well-being.
Another significant finding is the dual impact of PPE use on healthcare workers. While PPE is effective in preventing infection transmission, its prolonged use has been associated with physical discomfort and adverse events, such as skin irritation and fatigue. Silva et al. (2021) found that healthcare workers often experience adverse effects related to prolonged PPE use, which may reduce compliance over time. This highlights the need for ergonomic PPE designs that prioritize healthcare worker comfort, allowing them to perform their duties safely without compromising their physical well-being. Addressing the challenges of PPE use is critical, as healthcare workers are on the frontline of IPC efforts. Ensuring their comfort and safety not only protects them but also enhances their compliance, ultimately contributing to better infection control.
The economic benefits of IPC interventions, particularly in long-term care facilities, were evident in the review. Tchouaket et al. (2022) demonstrated that IPC measures, including hand hygiene and enhanced cleaning protocols, lead to substantial cost savings by reducing infection rates and the associated costs of treatment. Investing in IPC programs is economically feasible as it minimizes the financial burden on healthcare systems by preventing infections and reducing the need for costly treatments and extended hospital stays. This finding is particularly relevant in resource-limited settings, where cost-effective IPC measures can play a pivotal role in improving health outcomes and maintaining sustainable healthcare services (Thandar, Tong, & Karobari, 2022).
Hand hygiene remains a cornerstone of IPC programs, but maintaining high compliance rates poses challenges. Factors such as heavy workloads, time constraints, and forgetfulness can hinder healthcare workers from consistently adhering to hand hygiene practices. Gozdzielewska et al. (2024) found that structured interventions, such as regular training, visual reminders, and easy access to hand hygiene stations, significantly improve compliance. This highlights the importance of institutional support in promoting hand hygiene compliance. Regular training and reinforcement are necessary, especially in high-stress environments where the risk of lapses in protocol adherence is higher. The sustained promotion of hand hygiene within healthcare settings is essential for ensuring effective infection control.
Ethical concerns surrounding isolation practices were highlighted in this review, particularly in balancing patient rights with public health safety. Isolation measures are effective in preventing the spread of infections, but they can infringe on patient autonomy and personal freedom. Rump, de Boer, and Kooijman (2019) identified ethical dilemmas associated with isolation protocols, emphasizing the need for policies that respect patient rights while ensuring effective infection control. These findings echo concerns within healthcare about finding an ethical balance between individual rights and community health. Transparent communication, informed consent, and respect for patient dignity are crucial when implementing isolation measures to ensure that IPC practices remain compassionate and patient-centered.
The effectiveness of IPC interventions in resource-limited settings, such as healthcare facilities in Africa, underscores the adaptability of IPC measures. Thandar et al. (2022) found that structured IPC programs can significantly reduce HAIs even in low-resource environments. This finding demonstrates that, with adequate support and local adaptation, IPC measures can succeed across diverse healthcare settings. The success of these interventions highlights the need for global collaboration in strengthening IPC capacity, particularly in underserved regions. Implementing low-cost, high-impact IPC measures can lead to substantial improvements in healthcare quality and patient outcomes, even where resources are constrained.
Isolation and protective barriers effectively reduce infection rates but often come at the expense of patient well-being. The review revealed that patients in isolation frequently experience feelings of abandonment, which can lead to psychological distress and reduced engagement with healthcare providers. Purssell, Gould, and Chudleigh (2020) highlighted the importance of providing psychosocial support to isolated patients to mitigate these adverse effects. Integrating mental health support into IPC protocols can enhance patient satisfaction and adherence to isolation measures, ensuring that infection control efforts are humane and supportive.
Healthcare workers’ knowledge and attitudes towards IPC measures play a significant role in compliance rates. Hammoud et al. (2020) suggest that positive attitudes and comprehensive knowledge about IPC practices are associated with higher compliance rates. This review supports the notion that IPC training programs should not only focus on skills but also address the attitudes of healthcare workers. Cultivating a culture of safety within healthcare institutions can promote adherence to IPC protocols, as healthcare workers who value IPC measures are more likely to follow them consistently. Encouraging a positive attitude towards IPC fosters a safer healthcare environment for patients and staff alike.
The stigma associated with source isolation was a significant finding, as it can negatively impact patient morale and adherence to IPC protocols. Gammon et al. (2019) discussed how stigma can discourage patients from complying with isolation measures, undermining the effectiveness of infection control efforts. To counteract this, healthcare providers should focus on patient-centered communication and education to reduce stigma. Patients who understand the reasons behind isolation are more likely to adhere to it, resulting in better compliance and less psychological distress. Addressing stigma in IPC protocols ensures that isolation measures are not only effective but also respectful of patients’ dignity and mental health.
Finally, this review underscores the importance of tailoring IPC strategies to specific healthcare settings, as the effectiveness of interventions can vary by environment. For example, protocols that are effective in hospital settings may require modification for long-term care facilities, where patient populations and staffing levels differ significantly. Lee et al. (2019) emphasized that adapting IPC interventions to the unique needs of each healthcare setting is crucial for achieving optimal outcomes. By customizing IPC strategies, healthcare providers can ensure that interventions are practical, effective, and feasible within the constraints of each setting, leading to improved infection prevention outcomes across diverse healthcare environments.
This systematic review has several limitations. First, the reliance on published studies may introduce publication bias, as studies with positive outcomes are more likely to be published than those with negative or inconclusive results. Second, variations in study design, IPC measures evaluated, and healthcare settings make it challenging to generalize findings across all healthcare environments. Third, some included studies may have methodological limitations, such as small sample sizes or lack of randomization, which could impact the reliability of the results. Additionally, this review did not include non-English studies, which may limit the comprehensiveness of the evidence. Future research should address these limitations to provide a more robust understanding of IPC effectiveness across diverse settings.
Conclusions
In conclusion, this systematic review highlights the critical role of infection prevention and control (IPC) measures in reducing healthcare-associated infections (HAIs) and promoting safer healthcare environments. Effective interventions, including hand hygiene, personal protective equipment (PPE) use, patient education, and isolation protocols, have been shown to significantly mitigate infection risks when consistently applied. However, the implementation of IPC measures must consider psychological, ethical, and logistical challenges to optimize compliance and minimize adverse effects. The findings emphasize the need for tailored IPC strategies that account for specific healthcare settings and the importance of ongoing education and support for both patients and healthcare workers. By addressing these factors, healthcare institutions can enhance the effectiveness of IPC programs, ultimately improving patient outcomes and healthcare quality on a global scale.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
References
- Fregonese, C., Chevalier, P., & Nguyen, Y. L. (2023). Psychosocial impact of isolation measures on patients during infectious disease outbreaks: A systematic review. Journal of Hospital Infection, 134, 20-28. [CrossRef]
- Gammon, J., Hunt, J., & Phillips, J. (2019). The psychological impact of source isolation on patients and its implications for infection prevention and control: A literature review. Journal of Research in Nursing, 24(8), 617-631.
- Gozdzielewska, L., Morley, D., & Laird, K. (2024). Factors influencing hand hygiene and personal protective equipment compliance in healthcare settings: A systematic review. Antimicrobial Resistance & Infection Control, 13, 41.
- Hammoud, S., Al-Tannir, M., AlGahtani, F., & Badri, M. (2020). Knowledge, attitudes, and practices in infection prevention and control measures in hospitals: A systematic review. American Journal of Infection Control, 48(4), 419-424. [CrossRef]
- Islam, M. S., Rahman, K. M., Sun, Y., Qureshi, M. O., Abdi, I., Chughtai, A. A., & Seale, H. (2020). Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: A global analysis. Infection Control & Hospital Epidemiology, 41(10), 1196-1206. [CrossRef]
- Lee, M. H., Lee, G. A., Lee, S. H., & Park, Y. H. (2019). Effectiveness and core components of infection prevention and control programmes in long-term care facilities: A systematic review. Journal of Hospital Infection, 102(4), 377-393. [CrossRef]
- Magiorakos, A. P., Burns, K., Rodríguez Baño, J., Borg, M., Daikos, G., Dumpis, U., ... & Weber, J. T. (2017). Infection prevention and control measures and tools for the prevention of entry of carbapenem-resistant Enterobacteriaceae into healthcare settings: Guidance from the European Centre for Disease Prevention and Control. Antimicrobial Resistance & Infection Control, 6, 1-17. [CrossRef]
- Purssell, E., Gould, D., & Chudleigh, J. (2020). Impact of isolation on hospitalised patients who are infectious: Systematic review with meta-analysis. BMJ Open, 10(2), e031912. [CrossRef]
- Rump, B., de Boer, M., & Kooijman, M. (2019). Ethical issues in infection prevention and control: A systematic review. BMC Medical Ethics, 20, 90.
- Saliba, P., Day, G., & Phillips, M. (2021). Adverse effects of isolation protocols in infection control: A systematic review and meta-analysis. Infection Control & Hospital Epidemiology, 42(6), 708-715. [CrossRef]
- Seto, W. H., Conly, J. M., Pessoa-Silva, C. L., Malik, M., & Eremin, S. (2013). Infection prevention and control measures for acute respiratory infections in healthcare settings: An update. EMHJ-Eastern Mediterranean Health Journal, 19(supp. 1), S39-S47. [CrossRef]
- Silva, A. G., de Oliveira, A. C., & Gontijo Filho, P. P. (2021). Adverse events associated with the use of personal protective equipment among healthcare workers during COVID-19: A systematic review and meta-analysis. American Journal of Infection Control, 49(5), 592-598. [CrossRef]
- Storr, J., Twyman, A., Zingg, W., Damani, N., Kilpatrick, C., Reilly, J., ... & Allegranzi, B. (2017). Core components for effective infection prevention and control programmes: New WHO evidence-based recommendations. Antimicrobial Resistance & Infection Control, 6, 1-18. [CrossRef]
- Tchouaket, E., Brousselle, A., & Dubois, C. A. (2022). Economic evaluation of healthcare-associated infection prevention and control interventions in long-term care: A systematic review protocol. Systematic Reviews, 11, 23. [CrossRef]
- Thandar, M., Tong, L., & Karobari, M. I. (2022). Effectiveness of infection prevention and control measures in healthcare settings in Africa: A systematic review and meta-analysis. Journal of Infection Prevention, 23(1), 24-36.
- Vottero, B., & Rittenmeyer, L. (2012). The psychosocial experience of patients who have been placed in protective isolation: A systematic review of qualitative evidence. Journal of Clinical Nursing, 21(5-6), 783-794. [CrossRef]
- World Health Organization. (2018). Improving infection prevention and control at the health facility: Interim practical manual supporting implementation of the WHO guidelines on core components of infection prevention and control programmes (No. WHO/HIS/SDS/2018.10). World Health Organization.
- World Health Organization. (2020). Infection prevention and control during health care when COVID-19 is suspected: Interim guidance, 19 March 2020 (No. WHO/2019-nCoV/IPC/2020.3). World Health Organization.
- World Health Organization. (2021). Annex to Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed: Interim guidance, 1 October 2021 (No. WHO/2019-nCoV/IPC/Annex/2021.1). World Health Organization.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).