1. Introduction
Intensive Intensive Care Unit-Acquired Weakness (ICU-AW) is a medium- and long-term complication in critically ill patients that affects quality of life by increasing morbidity and healthcare costs [
1]. It represents a clinically relevant muscle weakness that appears in patients with critical illness and has no underlying cause other than the critical illness itself. It is characterised by symmetrical and predominantly proximal limb weakness, with typical sparing of facial muscles and overall reduction of osteo-tendon reflexes. Respiratory muscles can also be affected [
2]. Depending on the presence of neuropathy or myopathy, a distinction can be made between
critical illness polyneuropathy (
CIP), characterized by axonal damage identified through electrophysiological methods;
critical illness myopathy (
CIM), characterized by visible muscle damage on biopsy or electrophysiology; and finally,
critical illness neuromyopathy (
CINM), which involves elements of both neuropathy and myopathy [
3]. The prevalence of ICU-AW in critically ill patients can reach 50%, with up to 2% of muscle mass lost daily [
4]. The significance of ICU-AW for patients’ quality of life became particularly evident during the COVID-19 pandemic, as muscle dysfunction and reduced mobility were not only more prevalent in patients hospitalized in intensive care units for COVID-19, but could also persist up to six months after discharge [
5,
6]. Furthermore, ICU-AW significantly increases the mortality of patients admitted to the ICU. Although the precise cause in these patients is difficult to determine, most die from irreversible septic shock [
7]. While the exact pathogenesis remains unclear, it is now evident that critical illness, the duration of stay in the intensive care unit, and the devices and therapies used in this setting serve as triggers for a wide range of cellular alterations that compromise nerve and muscle integrity [
4].
2. Risk Factors
It is useful to classify the risk factors for ICU-AW into
modifiable and
non-modifiable, as shown in
Table 1 [
8].
2.1. Premorbid Health Status
The premorbid functional state certainly influences the development of ICU-AW in different ways and for different reasons. The risk of developing ICU-AW is higher in older patients: studies show that the incidence of ICU-AW increases with age [
9]. There is no unanimous consensus among studies regarding gender. While some identify female sex as an independent risk factor [
10,
11], others have found no statistically significant differences in the development of ICU-AW between the sexes [
9,
12]. The frailty of elderly patients prolongs their stay in the ICU and increases the severity of diseases and their mortality. It is also closely related to the development of sarcopenia, which further exacerbates this spiral of complications [
13]. At the same time, obesity appears to be protective against the development of weakness in critically ill patients by reducing muscle mass loss through increased metabolism of fatty acids and glycerol [
14].
2.2. Multiple Organ Failure
Multiple Organ Failure (MOF) has long been considered a crucial risk factor for the development of ICU-AW. It is characterised by sequential failure of two or more organs and, in most ICU patients, is caused by a septic state. Although sepsis is the most frequent cause of MOF, muscle weakness also occurs as a complication of MOF caused by other conditions, such as acute pancreatitis, trauma, and cardiac arrest [
15]. It is now established that also the severity of the underlying pathology predisposes patients to the development of neuromyopathy. The Acute Physiology and Chronic Health Evaluation (APACHE II) score, as well as the Sequential Organ Failure Assessment (SOFA) score, is higher in patients who will develop various forms of ICU-AW [
9,
16]. ICU-AW and MOF seem to exacerbate each other. Multiple organ failure is also the predominant cause of death in ICU-AW patients: a 2020 study showed that MOF caused by irreversible shock was the most common cause of death in this cohort. In most cases, it was septic shock; only in a minority of cases, it was hypovolemic shock [
7].
2.3. Sepsis and Septic Shock
Sepsis, a systemic syndrome characterized by organ damage in the presence of an infection, is a major public health problem, leading to death in up to one third of affected patients [
17]. It is one of the main causes of ICU admissions across all age groups: some statistics estimate that up to 50% of septic patients require intensive care [
18]. The course of patients with sepsis is sometimes complicated by reduced muscle mass and, for those admitted to the ICU, by ICU-AW. Since sepsis coexists with many other clinical conditions, so that determining its role in the development of ICU-AW is challenging. Certainly, septic patients may present nearly all risk factors for ICU-AW described in this article. Additionally, sepsis activates specific mechanisms: studies in cellular, animal, and human models have shown that the main cause of muscle loss during sepsis is an imbalance between increased protein degradation and decreased synthesis of new muscle proteins [
19].
2.4. Immobilization
In hospitalized patients, particularly the elderly, sarcopenia is not uncommon. Muscle atrophy can develop acutely due to reduced muscle use following an illness, or chronically as part of the aging process [
20]. Immobilization is a well-established risk factor for the development of ICU-AW [
2,
13,
15,
21]. A 2014 study on patients following acute lung injury highlighted reduced mobility during hospitalization as a significant risk factor for persistent muscle weakness 24 months after the acute event [
22]. Prolonged stays in intensive care units further increase the risk, as reduced mobilization is compounded by other factors such as infections, potentially muscle-toxic medications, mechanical ventilation, and more [
9].
2.5. Mechanical Ventilation
Mechanical ventilation is one of the main risk factors for ICU-AW in the intensive care setting [
23,
24,
25]. The risk of developing this form of muscle atrophy increases with the duration of mechanical ventilation, although some studies suggest that even a few hours of ventilation can act as a trigger for the process. The mechanism linking ICU length of stay, duration of mechanical ventilation, and the onset of ICU-AW is complex and not yet fully understood, as multiple factors are likely involved, including immobilization, the use of sedatives and muscle relaxants, malnutrition, and hypoxia [
26,
27]. Prolonged mechanical ventilation has also been associated with diaphragmatic weakness and atrophy, which further complicate the process of weaning from ventilation [
28].
2.6. Glycemic Control
Several studies have shown that poor glycaemic control during the acute phase of illness is associated with the development of polyneuropathy and muscle weakness [
10,
29] and appears to worsen the prognosis of ICU patients [
30]. Various mechanisms have been proposed to explain this phenomenon: hyperglycaemia seems to alter neuronal excitability, has toxic effects on neurons, and may impair nerve microcirculation [
27]. For these reasons, maintaining good blood glucose control, through insulin therapy and non-pharmacological approaches such as early mobilization, improves outcomes and reduces the incidence of ICU -AW [
30,
31].
2.7. Drugs
2.7.1. Neuromuscular Blocking Agents
The correlation between the use of neuromuscular blocking agents (NMBA) and the development of ICU-acquired weakness (ICU-AW) has been studied for a long time. Traditionally, NMBA use is considered a risk factor for ICU-AW [
2,
6,
27], although the supporting data are inconsistent and do not provide a definitive answer. A 2016 meta-analysis of 2,254 patients found only a modest association between NMBA use and acquired neuromuscular dysfunction, but the analysis was significantly biased due to the inclusion of studies on critically ill or septic shock patients [
32]. A more recent 2023 meta-analysis suggested a potential association between NMBA use and ICU-AW, although it concluded that the available evidence remains weak, as it is primarily based on heterogeneous observational studies [
33]. An older multicentred study on patients with severe ARDS demonstrated that NMBA use improved mortality rates without increasing the risk of muscle weakness [
34]. The challenge in finding definitive studies on this topic lies in the difficulty of isolating the contribution of NMBA use to the development of ICU-AW from that of other risk factors, which are often present in the studied populations [
35].
2.7.2. Glucocorticoids
Although glucocorticoids are associated with an increased risk of myopathy due to enhanced muscle catabolism [
36,
37], their role in the development of neuromyopathy in the context of ICU-acquired weakness (ICU-AW) remains unclear and controversial. Some studies suggest they may act as an independent risk factor [
10]. A 2018 meta-analysis found a strong correlation between glucocorticoid use and ICU-AW, recommending careful consideration of their use [
38]. However, other studies, particularly those examining low steroid doses, do not confirm this association [
39]. Given that corticosteroids are a key component in the treatment of ARDS and septic shock, this discrepancy may be explained by the benefits of steroids, particularly in controlling systemic inflammation, which is pathologically linked to ICU-AW, and in reducing the duration of mechanical ventilation. According to some authors, these benefits may outweigh the potential and uncertain negative effects on neuromuscular integrity [
40,
41].
3. Pathophysiology
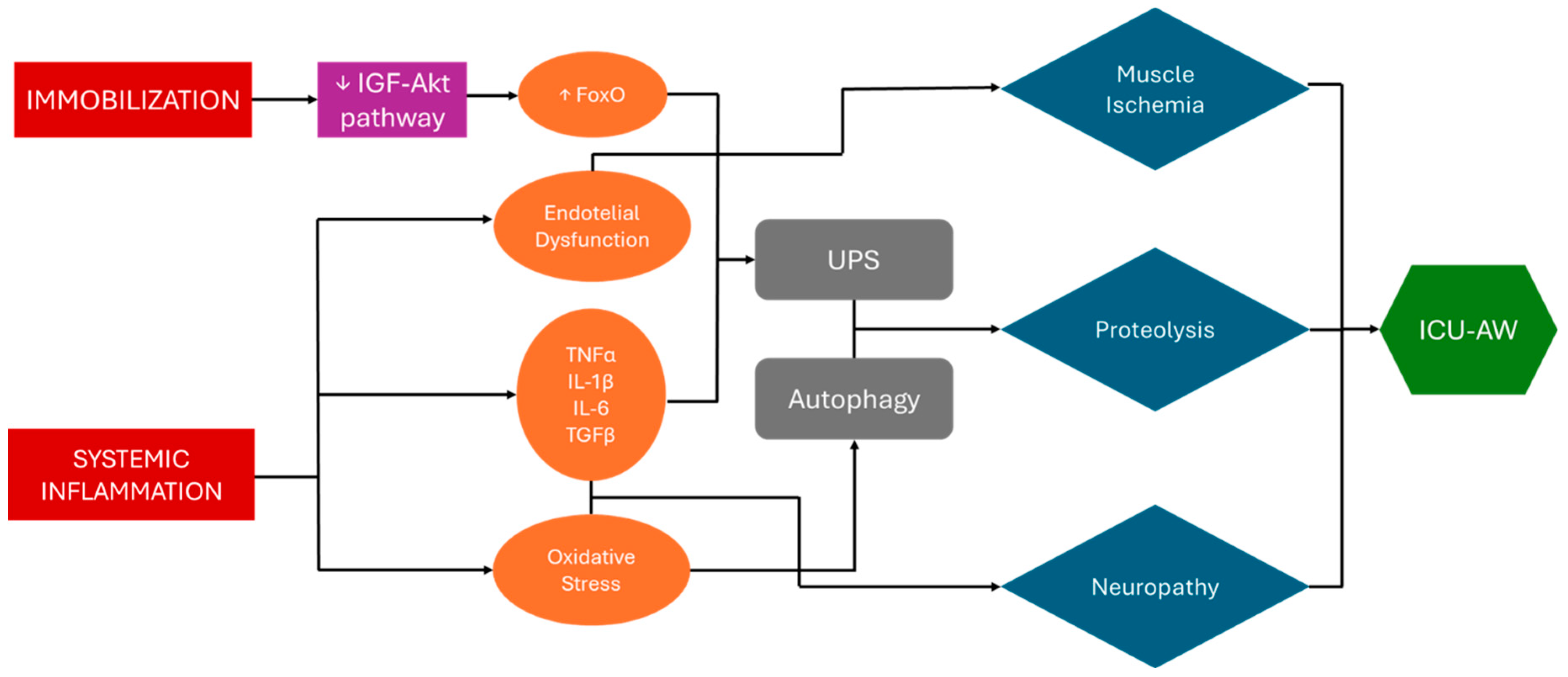
The pathophysiology of ICU-AW is multifactorial, involving a combination of systemic inflammation, bioenergetic failure, oxidative stress and microvascular changes, all contributing to both muscle and nerve dysfunction. The key factor in the pathogenesis is an imbalance between protein synthesis and muscle protein degradation in response to various stimuli. Several mechanism are involved [
23].
One of the mechanisms responsible for protein degradation is the
Ubiquitin-Proteasome System (
UPS). The proteasome, a large protease, recognises and degrades protein tagged with ubiquitin molecules by E3 UB-protein ligase. Two of these ligase, MAFbx and MuRF1, are involved in muscle atrophy as they show increased activity in response to several stimuli [
42].
Another long-studied system involved in cell turnover is the
Autophagy-Lysosome System, which is used in the degradation of cellular components in stressful situations of various kinds or in the event of nutritional deficiency through the formation of organelles called auto-phagolysosomes that are rich in lysosomal proteins. One of the tissues in which this system is most active is skeletal muscle: mitophagy—autophagy that selectively involves mitochondria—plays a role in muscle remodelling in atrophic muscle, in which the mitochondrial make-up is altered and damaged by denervation or fasting. Its uncontrolled and dysregulated action appears to be involved in the protein degradation observed during muscle atrophy [
15,
43].
3.1. Systemic Inflammation and Cytokine Dysregulation
Systemic inflammation is a central factor in the development of ICU-AW. Critical illness, particularly sepsis, triggers a widespread inflammatory response, characterized by the release of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6. These cytokines lead to muscle catabolism by stimulating the UPS, resulting in accelerated muscle protein degradation. Furthermore, these cytokines impair mitochondrial function, promoting oxidative stress and further contributing to muscle atrophy. It also appears that the activation of the TGF-β/MAPK pathway following stress stimuli, in association with the UPS pathway, may play a role in muscle loss [
15,
44].
3.2. Oxidative Stress and Mitochondrial Dysfunction
Mitochondrial dysfunction plays a crucial role in ICU-AW. Critical illness leads to excessive production of reactive oxygen species (ROS) and a concomitant reduction in antioxidant defences. The accumulation of ROS damages cellular components, including proteins, lipids, and mitochondrial DNA, exacerbating muscle wasting [
45]. For instance, oxidative stress triggered by the muscle-specific expression of a mutant superoxide dismutase protein leads to muscle atrophy, primarily through the activation of autophagy [
43]. Moreover, mitochondrial dysfunction impairs ATP production, causing bioenergetic failure and hindering muscle contractility and repair processes [
46].
3.3. Microvascular and Endothelial Dysfunction
Endothelial dysfunction, common in critical illness, reduces blood flow to the muscles, contributing to muscle ischemia and damage. Capillary leakage and microvascular thrombosis impair oxygen and nutrient delivery, exacerbating mitochondrial dysfunction and muscle degradation. Inflammatory mediators and oxidative stress disrupt endothelial nitric oxide production, further impairing vasodilation and microcirculation [
23,
47].
3.4. Immobilization and Muscle Disuse
Prolonged immobilization in ICU patients is another critical contributor to ICU-AW. Immobilization accelerates muscle atrophy by enhancing proteolysis and reducing muscle protein synthesis. Disuse leads to a rapid loss of type II (fast-twitch) muscle fibers, which are particularly vulnerable to atrophy, further impairing muscle strength [
35,
48,
49]. Muscle activity and nutrient availability stimulate another well-studied signaling pathway, the IGF1-Akt pathway. Akt, also known as protein kinase B, responds to several factors, including the growth factor IGF1. This kinase regulates both protein synthesis and protein degradation by acting on specific targets. Specifically, Akt promotes protein synthesis by activating mTOR and simultaneously inhibits protein degradation by suppressing the transcription factor FoxO. When FoxO is active, it promotes muscle degradation by enhancing the expression of muscle-specific ubiquitin ligases, such as Atrogin-1 and MuRF1, which are critical mediators of protein breakdown in muscle tissue [
43].
3.5. Neuromuscular Involvement
In addition to direct muscle injury, ICU-AW can involve peripheral nerve dysfunction, leading to critical illness polyneuropathy (CIP). Nerve injury is driven by factors such as inflammation, oxidative stress, and metabolic disturbances. Axonal degeneration of motor and sensory fibers is commonly observed in CIP, contributing to the overall muscle weakness. Electrophysiological studies reveal reduced nerve conduction velocities and denervation potentials in affected patients [
50,
51].
Figure 1.
Pathogenesis of ICU-AW. Systemic inflammation associated with critical illness and prolonged immobilization are major contributors to ICU-acquired weakness (ICU-AW). Pro-inflammatory cytokines drive an increase in proteolysis via activation of the ubiquitin-proteasome system. Concurrently, oxidative stress from inflammatory processes leads to mitochondrial dysfunction and dysregulated activation of autophagy pathways. Systemic illness further induces endothelial dysfunction, promoting muscle ischemia. Extended immobilization disrupts the IGF-Akt signaling pathway, diminishing its activity and resulting in excessive FoxO activation, which amplifies the ubiquitin-proteasome system's effects. Abbreviations. UPS = Ubiquitin-Proteasome System; ICU-AW = Intensive Care Unit-Acquired Weakness
Figure 1.
Pathogenesis of ICU-AW. Systemic inflammation associated with critical illness and prolonged immobilization are major contributors to ICU-acquired weakness (ICU-AW). Pro-inflammatory cytokines drive an increase in proteolysis via activation of the ubiquitin-proteasome system. Concurrently, oxidative stress from inflammatory processes leads to mitochondrial dysfunction and dysregulated activation of autophagy pathways. Systemic illness further induces endothelial dysfunction, promoting muscle ischemia. Extended immobilization disrupts the IGF-Akt signaling pathway, diminishing its activity and resulting in excessive FoxO activation, which amplifies the ubiquitin-proteasome system's effects. Abbreviations. UPS = Ubiquitin-Proteasome System; ICU-AW = Intensive Care Unit-Acquired Weakness
4. Diagnosis
The diagnosis of ICU-AW is primarily clinical. The main criterion for diagnosing ICU-AW is the presence of symmetrical, progressive muscle weakness affecting all four limbs, while typically sparing the facial muscles. The diaphragm is often involved, which can complicate weaning from mechanical ventilation. Unlike other neuropathies, such as Guillain-Barré Syndrome, the onset of ICU-AW follows the critical illness, rather than preceding it [
52].
4.1. Medical Research Council (MRC) Scale
The first step in the diagnosis of ICU-AW is to assess of muscle strength in critically ill patients who are awake and cooperative. Manual muscle testing using the Medical Research Council (MRC) scale is the most widely accepted bedside tool. A sum score of less than 48 out of a possible 60 points across 12 muscle groups is indicative of ICU-AW. However, the ability to perform a reliable MRC test depends on patient consciousness, cooperation, and the absence of sedation [
53].
4.2. Electrophysiological Studies
ICU-AW can have different pathogenic substrates, including critical illness polyneuropathy (CIP), critical illness myopathy (CIM), a combination of both (CINM), or muscle atrophy due to disuse. It is possible to refer to the set of neuromuscular diseases acquired in the ICU with the acronym CRYMINE (critical illness myopathy and/or neuropathy). To distinguish between CIP and CIM, electrophysiological studies are primarily used, such as nerve conduction studies (NCS) and electromyography (EMG) are valuable adjuncts. By using NCS, it is possible to determine both compound motor action potentials (CMAPs) and sensory nerve action potentials (SNAPs). These measurements allow for the assessment of motor and sensory nerve function, respectively, and are critical in differentiating between neuropathic and myopathic causes of weakness in ICU patients. CMAPs reflect the overall response of the motor nerve and muscle, while SNAPs provide insights into the function of sensory nerves. Electromyography (EMG), on the other hand, assesses motor unit potential (MUP) amplitudes, durations, and fibre recruitment patterns. MUP amplitudes indicate the size and number of muscle fibres innervated by a single motor neuron, while MUP durations reflect the overall temporal profile of the motor unit’s activity. The recruitment patterns assess the ability of the nervous system to activate additional motor units during muscle contraction, providing insights into neuromuscular integrity. CIP has reduced CMAP amplitudes and reduced SNAP amplitudes, while CIM has reduced CMAP amplitudes but normal SNAP amplitudes. Furthermore, on one hand they have spontaneous fibrillation potentials and sharp waves on EMG, but on the other hand CIP has high-amplitude polyphasic MUPs and CIM has low-amplitude MUPs with early recruitment. The peroneal nerve test (PENT) can be used as a simple and standardized electrophysiological method with good accuracy [
51,
52,
53,
54,
55].
Table 2.
Electrophysiological diagnosis.
Table 2.
Electrophysiological diagnosis.
| Condition |
Definition |
ENG |
EMG |
|
CIP [52,54] |
A polyneuropathy characterized by sensory and motor axonal damage, marked by reduced nerve responsiveness and loss of axons, while myelin remains intact. |
Reduced CMAP and SNAP amplitudes and normal nerve conduction velocity. |
Spontaneous fibrillation potentials, sharp waves and long duration, high-amplitude polyphasic MUP. |
|
CIM [52,54] |
An acute primary myopathy characterized by reduced excitability of muscle membranes, loss of myosin filaments, muscle fiber atrophy, and tissue necrosis. |
Reduced CMAP amplitudes, normal SNAP amplitudes and normal conduction velocities. |
Spontaneous fibrillation potentials, sharp waves and short duration, low-amplitude MUP with early recruitment. |
|
CINM [52,54] |
A combination of CIP and CIM |
Reduced CMAP and SNAP amplitudes and normal conduction velocities. |
A combination of CIP and CIM. |
4.3. Neuromuscular Ultrasound (NMUS)
Since the previously described techniques are complex and not easily applied in routine practice, studies are focusing on neuromuscular ultrasound (NMUS) as a tool to support the clinical diagnosis of ICU-AW. Although no reference standards have been established yet, ultrasound allows for the assessment of both the muscle and nerve components. Specifically, ultrasound can evaluate muscle mass reduction and increased muscle echogenicity, which respectively reflect changes in muscle quantity and quality. Target muscles in various studies include the biceps brachii, quadriceps femoris, and tibialis anterior. Similarly, the ultrasound assessment of nerve echogenicity in the transverse section, which will typically be reduced, as well as the nerve's cross-sectional area, can help estimate the presence of polyneuropathy, though it does not differentiate its type [
56,
57].
Additionally, especially in intensive care settings, ultrasound can estimate diaphragmatic function and predict the effectiveness of the patient's ventilatory response. This is primarily achieved by measuring diaphragmatic thickness at the end of expiration and inspiration, followed by calculating the diaphragmatic thickening fraction (TF) [
58].
5. Management and Therapeutic Strategies
In our view, the proper management of ICU-AW and its clinical consequences requires a comprehensive, 360-degree approach to patient care. We emphasize the importance of a multidisciplinary team to effectively integrate the necessary preventive and therapeutic strategies. According to our opinion, the management of ICU-AW can be divided into three fundamental phases, which are not necessarily sequential but often occur simultaneously: prevention, early recognition and effective treatment.
5.1. Prevention
Addressing the risk factors for the development of neuromyopathy is the first essential step in managing this clinical condition. A comprehensive assessment of patients, particularly geriatric patients, can effectively address risk factors for in-hospital death. Considering that frail in-patients are at an increased risk of death and complications, studies have demonstrated that functional assessments of surgical [
59] and COVID-19 [
60] patients can predict the risk of in-hospital death. It can be hypothesized that this approach could be effectively extended to critically ill patients, regardless of the cause.
We believe that effectively treating sepsis is crucial in minimizing the widespread negative effects it has on the body, including multi-organ dysfunction, and in preventing prolonged stays in the ICU, which expose patients to a cascade of risk factors leading to the development of ICU-AW. Additionally, reducing the impact of the cytokine storm that accompanies severe infection can mitigate its detrimental effects on neuromuscular function, based on what was previously said about the role of cytokines in protein degradation [
15,
44].
A key element in preventing ICU-AW is reducing the length of stay in the ICU. Shortening the duration of ICU admission not only decreases patient immobility, but also limits exposure to additional nosocomial infections, which could worsen the clinical condition. Prolonged immobility is a major contributor to the development of muscle atrophy and polyneuropathy. Promoting early mobilization is thus a fundamental strategy, not only for prevention but also therapeutically, as it helps preserve muscle strength and functionality [
2]. To achieve this, reducing the time spent on mechanical ventilation is crucial. Prolonged mechanical ventilation can lead to diaphragmatic dysfunction, further complicating the clinical picture and hindering the patient’s recovery. Reducing ventilation time not only improves diaphragm function, but also facilitates faster recovery and lowers the risk of ICU-AW [
25,
61].
Among the risk factors considered, hyperglycemia is one of the most extensively studied and frequently observed in critically ill patients. Literature shows that maintaining optimal blood glucose levels through insulin therapy has a beneficial effect on both the central and peripheral nervous systems of ICU patients, helping to prevent the development of polyneuropathy and consequently reducing dependence on mechanical ventilation [
31]. Moreover, a study conducted on mechanically ventilated patients highlights that early mobilization not only helps prevent disuse muscle atrophy, but also promotes euglycemia and reduces mechanisms of insulin resistance, presenting a valid alternative to insulin therapy [
30]. Therefore, we believe that the metabolic status of the patient should be considered a priority in the management of critically ill patients.
In the management of ICU-AW, careful attention must be given to the drugs administered, as some medications may potentially contribute to the development of this condition. Although scientific literature is not entirely consistent on this matter, with more recent studies tending to exonerate corticosteroids and neuromuscular blockers as primary risk factors [
34,
39], a prudent approach to pharmacological therapy remains essential. Overtreatment must be avoided, as prolonged and unmonitored use of certain drugs could still negatively impact muscle and neurological function.
In particular, corticosteroids have been linked in earlier studies to an increased risk of myopathy in critically ill patients [
38], although more recent research has questioned this direct association. Similarly, prolonged use of neuromuscular blocking agents, which are sometimes necessary in the clinical management of mechanical ventilation, has been associated with possible muscle function impairment. However, recent evidence has shown conflicting results, highlighting that appropriate management of dose and treatment duration may mitigate these risks [
27,
34]. Thus, the therapeutic approach should always be individualized, avoiding both excessive and unjustified use of these medications, while prioritizing strategies that minimize the negative pharmacological impact on the patient.
5.2. Early Recognition
Prompt recognition of neuromuscular dysfunction in a critically ill patient is a crucial step in subsequent management, as it allows early intervention to halt the pathogenic mechanisms underlying this condition. There is no established gold standard for diagnosing ICU-AW, which often complicates effective identification [
3]. As previously mentioned, validated methods include the MRC scale, which, however, requires active patient participation—a challenge in critical care settings. Electrophysiological studies such as EMG and NCS are also used but can be complex to perform.
Some studies have demonstrated the utility of the peroneal nerve test (PENT) as a screening method for identifying patients affected by ICU-AW. Literature indicates that a reduction in peroneal CMAP amplitude has a sensitivity of 100% and a specificity of 85.2% for identifying CIP or CIM when compared to standard electrophysiological studies [
62] Another study involving septic shock patients in intensive care confirmed the PENT's effectiveness in predicting such conditions and paired it with the measurement of sural sensory nerve action potentials (SNAP) to differentiate between CIM and CIP [
53].
In our opinion, the use of PENT enables early and straightforward detection of ICU-AW, regardless of the patient's consciousness or ability to cooperate. These methods gain additional diagnostic value when combined with more recently applied techniques such as neuromuscular ultrasound, which are equally simple and quick to perform. In cooperative patients, the MRC scale remains a valid alternative.
5.3. Effective Treatment
In this article we analyze and summarize all the key points for the proper prevention and management of this clinical condition. We would like to emphasize that comprehensive patient management is crucial in this clinical process.
Patient mobilization and adequate nutrition are two cornerstones of the treatment of ICU-AW. One without the other is not sufficient; only a proper integration of both improves muscle function in patients [
63]. Prolonged immobilization reduces muscle protein synthesis in response to the ingestion of exogenous proteins, likely due to the development of anabolic resistance to food intake, which appears to be one of the mechanisms underlying muscle atrophy from disuse [
49].
One of the most effective interventions to prevent ICU-AW is early mobilization of patients. Initiating physical therapy and encouraging movement as soon as medically feasible can help maintain muscle strength and function. Patient mobilization not only helps prevent atrophy but also markedly improves patients' glycemic and metabolic compensation [
30]. In ICU, providing patients with physical therapy improves the strength of respiratory muscles, leading to an increase in ventilator-free days [
64]. A 2014 study conducted on a population of septic patients who were ventilated for more than 48 hours and admitted to the ICU for over 4 days suggests that adding functional electrical stimulation (FES)-cycling to traditional physical therapy methods appears to improve muscle performance upon awakening from sedation, while also reducing the incidence of delirium [
65].
Nutritional support plays a vital role in preventing muscle wasting. Ensuring that patients receive adequate protein and caloric intake is crucial for maintaining muscle mass and supporting recovery [
66]. Several studies examine the role of nutrition in these categories of patients, focusing particularly on the methods, timing, and composition of an adequate and effective nutritional approach. The literature is not fully consistent on the optimal nutritional approach regarding energy intake and protein requirements for critically ill patients. It appears that both complete starvation and overfeeding during the early phase of critical illness should be avoided as they can be harmful. A significant focus is on determining the appropriate protein intake. Current guidelines recommend a protein intake of 1.2-1.5 g/kg/day, which has been associated with reduced mortality. However, some studies suggest higher protein doses, exceeding 1.5 g/kg/day.
Nonetheless, caution is advised with high protein intake early in the illness, whether administered enterally or parenterally, as some studies have shown a direct association between increased protein intake and prolonged ICU stays, higher mortality, and even reduced muscle mass. This negative correlation between high protein or amino acid intake and poor patient outcomes may be explained by the suppression of the beneficial effects of autophagy, which helps clear damaged cells [
66,
67,
68]. This effect is particularly evident in septic patients, where autophagy facilitates the clearance of intracellular bacterial products. A 2014 study highlighted that a high protein intake as early as the fourth day of ICU admission (defined as >1.2 g/kg) was associated with lower hospital mortality, but only in non-septic and non-overfed patients. In septic patients, the situation is more complex and further research is needed to provide specific recommendations [
68]. In summary, in the absence of contraindications, it is appropriate to initiate EN within 24-48 hours at a low dose, gradually increasing it to meet the rising metabolic demands for tissue repair [
67]. In animal models, beta-hydroxybutyrate (3-HB), produced from fatty acid metabolism during ketogenesis, has shown a protective effect on muscle. Parenteral supplementation of 3-HB appears to offer muscle protection, suggesting its potential as a preventive strategy against muscle weakness in critically ill human patients [
14]. Among emerging therapies, targeting the ubiquitin-proteasome system seems promising. Developing IGF-1 analogs selective for muscle Akt, which lack the cancer-promoting risks of IGF-1, could combat muscle loss, though it must be noted that inhibiting protein degradation might lead to the accumulation of misfolded proteins [
43].
The management of ICUAW requires a comprehensive, multidisciplinary approach. This involves coordination between intensivists, physiotherapists, nutritionists, and nursing staff to develop and implement individualized care plans for each patient.
6. Conclusions
In conclusion, the management of ICU-AW demands a multifaceted approach that includes early detection, prevention, and effective treatment strategies. ICU-AW arises from a combination of CIP, CIM and muscle atrophy due to disuse, all exacerbated by prolonged immobility and mechanical ventilation. Early diagnosis is pivotal, and employing a variety of tools, such as the MRC scale; electrophysiological studies and neuromuscular ultrasound (NMUS) offers reliable options for recognizing ICU-AW, particularly in unresponsive or non-cooperative patients.
Nutritional support plays a significant role in preserving muscle mass and function. Adequate protein intake and caloric support have been shown to prevent further muscle degradation, particularly when aligned with early mobilization. Implementing a tailored nutrition plan ensures that patients have the necessary nutrients to mitigate muscle waste. Moreover, early and progressive physiotherapy is crucial in both preventing and treating ICU-AW. Regular mobilization exercises, passive or active, reduce immobility-related complications, preserve muscle function, and improve overall outcomes. This combination of physical rehabilitation and nutrition helps counterbalance the muscle loss that occurs during extended ICU stays. Lastly, minimizing pharmacological risks, such as the overuse of corticosteroids and neuromuscular blocking agents, remains essential in preventing ICU-AW.
Altogether, a comprehensive and individualized approach involving early diagnosis, multidisciplinary care, nutrition, physiotherapy, and careful pharmacological management is key to improving outcomes for patients with ICU-AW.
7. Methods
The search was performed between September and November 2024 in the PubMed database. English-language original papers, short communications, clinical trials, randomized controlled trials, meta-analyses, letters, editorials, and articles were evaluated. Emphasis was placed on the selection of original papers and randomized controlled trials filtered for the last five years, whenever possible.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rousseau, A.-F.; Prescott, H.C.; Brett, S.J.; Weiss, B.; Azoulay, E.; Creteur, J.; Latronico, N.; Hough, C.L.; Weber-Carstens, S.; Vincent, J.-L.; et al. Long-Term Outcomes after Critical Illness: Recent Insights. Crit. Care 2021, 25, 108. [Google Scholar] [CrossRef]
- Hermans, G.; Van Den Berghe, G. Clinical Review: Intensive Care Unit Acquired Weakness. Crit. Care 2015, 19, 274. [Google Scholar] [CrossRef]
- Stevens, R.D.; Marshall, S.A.; Cornblath, D.R.; Hoke, A.; Needham, D.M.; De Jonghe, B.; Ali, N.A.; Sharshar, T. A Framework for Diagnosing and Classifying Intensive Care Unit-Acquired Weakness. Crit. Care Med. 2009, 37, S299–S308. [Google Scholar] [CrossRef]
- Fazzini, B.; Märkl, T.; Costas, C.; Blobner, M.; Schaller, S.J.; Prowle, J.; Puthucheary, Z.; Wackerhage, H. The Rate and Assessment of Muscle Wasting during Critical Illness: A Systematic Review and Meta-Analysis. Crit. Care 2023, 27, 2. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, D.; Margarites, A.G.; Alvarenga, L.P.K.B.; Paesi, P.M.; Friedman, G.; Sbruzzi, G. Post-COVID-19 Intensive Care Unit-Acquired Weakness Compromises Long-Term Functional Status. Phys. Ther. 2023, 103, pzad117. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, D.; Piva, T.C.; Glaeser, S.S.; Piekala, D.M.; Berto, P.P.; Friedman, G.; Sbruzzi, G. Intensive Care Unit–Acquired Weakness in Patients With COVID-19: Occurrence and Associated Factors. Phys. Ther. 2022, 102, pzac028. [Google Scholar] [CrossRef] [PubMed]
- Van Wagenberg, L.; Witteveen, E.; Wieske, L.; Horn, J. Causes of Mortality in ICU-Acquired Weakness. J. Intensive Care Med. 2020, 35, 293–296. [Google Scholar] [CrossRef]
- Chen, J.; Huang, M. Intensive Care Unit-Acquired Weakness: Recent Insights. J. Intensive Med. 2024, 4, 73–80. [Google Scholar] [CrossRef]
- Baby, S.; George, C.; Osahan, N.M. Intensive Care Unit-Acquired Neuromuscular Weakness: A Prospective Study on Incidence, Clinical Course, and Outcomes. Indian J. Crit. Care Med. 2021, 25, 1006–1012. [Google Scholar] [CrossRef]
- De Jonghe, B. Paresis Acquired in the Intensive Care UnitA Prospective Multicenter Study. JAMA 2002, 288, 2859. [Google Scholar] [CrossRef]
- Yang, T.; Li, Z.; Jiang, L.; Wang, Y.; Xi, X. Risk Factors for Intensive Care Unit-Acquired Weakness: A Systematic Review and Meta-Analysis. Acta Neurol. Scand. 2018, 138, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Lefaucheur, J.-P. Origin of ICU Acquired Paresis Determined by Direct Muscle Stimulation. J. Neurol. Neurosurg. Psychiatry 2006, 77, 500–506. [Google Scholar] [CrossRef]
- Akan, B. Influence of Sarcopenia Focused on Critically Ill Patients. Acute Crit. Care 2021, 36, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Goossens, C.; Marques, M.B.; Derde, S.; Vander Perre, S.; Dufour, T.; Thiessen, S.E.; Güiza, F.; Janssens, T.; Hermans, G.; Vanhorebeek, I.; et al. Premorbid Obesity, but Not Nutrition, Prevents Critical Illness-induced Muscle Wasting and Weakness. J. Cachexia Sarcopenia Muscle 2017, 8, 89–101. [Google Scholar] [CrossRef]
- Wang, W.; Xu, C.; Ma, X.; Zhang, X.; Xie, P. Intensive Care Unit-Acquired Weakness: A Review of Recent Progress With a Look Toward the Future. Front. Med. 2020, 7, 559789. [Google Scholar] [CrossRef] [PubMed]
- Nanas, S.; Kritikos, K.; Angelopoulos, E.; Siafaka, A.; Tsikriki, S.; Poriazi, M.; Kanaloupiti, D.; Kontogeorgi, M.; Pratikaki, M.; Zervakis, D.; et al. Predisposing Factors for Critical Illness Polyneuromyopathy in a Multidisciplinary Intensive Care Unit. Acta Neurol. Scand. 2008, 118, 175–181. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef]
- Markwart, R.; Saito, H.; Harder, T.; Tomczyk, S.; Cassini, A.; Fleischmann-Struzek, C.; Reichert, F.; Eckmanns, T.; Allegranzi, B. Epidemiology and Burden of Sepsis Acquired in Hospitals and Intensive Care Units: A Systematic Review and Meta-Analysis. Intensive Care Med. 2020, 46, 1536–1551. [Google Scholar] [CrossRef] [PubMed]
- Schefold, J.C.; Bierbrauer, J.; Weber-Carstens, S. Intensive Care Unit—Acquired Weakness (ICUAW) and Muscle Wasting in Critically Ill Patients with Severe Sepsis and Septic Shock. J. Cachexia Sarcopenia Muscle 2010, 1, 147–157. [Google Scholar] [CrossRef]
- Calvani, R.; Joseph, A.-M.; Adhihetty, P.J.; Miccheli, A.; Bossola, M.; Leeuwenburgh, C.; Bernabei, R.; Marzetti, E. Mitochondrial Pathways in Sarcopenia of Aging and Disuse Muscle Atrophy. bchm 2013, 394, 393–414. [Google Scholar] [CrossRef]
- Parry, S.M.; Puthucheary, Z.A. The Impact of Extended Bed Rest on the Musculoskeletal System in the Critical Care Environment. Extreme Physiol. Med. 2015, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Fan, E.; Dowdy, D.W.; Colantuoni, E.; Mendez-Tellez, P.A.; Sevransky, J.E.; Shanholtz, C.; Dennison Himmelfarb, C.R.; Desai, S.V.; Ciesla, N.; Herridge, M.S.; et al. Physical Complications in Acute Lung Injury Survivors: A Two-Year Longitudinal Prospective Study. Crit. Care Med. 2014, 42, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Vanhorebeek, I.; Latronico, N.; Van Den Berghe, G. ICU-Acquired Weakness. Intensive Care Med. 2020, 46, 637–653. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Wenjuan, J. Construction and Evaluation of Acquired Weakness Nomogram Model in Patients with Mechanical Ventilation in Intensive Care Unit. Digit. Health 2024, 10, 20552076241261604. [Google Scholar] [CrossRef]
- Sinha, R.K.; Sinha, S.; Nishant, P.; Morya, A.K. Intensive Care Unit-Acquired Weakness and Mechanical Ventilation: A Reciprocal Relationship. World J. Clin. Cases 2024, 12, 3644–3647. [Google Scholar] [CrossRef]
- Wang, L.; Long, D.-Y. Significant Risk Factors for Intensive Care Unit-Acquired Weakness: A Processing Strategy Based on Repeated Machine Learning. World J. Clin. Cases 2024, 12, 1235–1242. [Google Scholar] [CrossRef]
- Friedrich, O.; Reid, M.B.; Van Den Berghe, G.; Vanhorebeek, I.; Hermans, G.; Rich, M.M.; Larsson, L. The Sick and the Weak: Neuropathies/Myopathies in the Critically Ill. Physiol. Rev. 2015, 95, 1025–1109. [Google Scholar] [CrossRef]
- Jaber, S.; Petrof, B.J.; Jung, B.; Chanques, G.; Berthet, J.-P.; Rabuel, C.; Bouyabrine, H.; Courouble, P.; Koechlin-Ramonatxo, C.; Sebbane, M.; et al. Rapidly Progressive Diaphragmatic Weakness and Injury during Mechanical Ventilation in Humans. Am. J. Respir. Crit. Care Med. 2011, 183, 364–371. [Google Scholar] [CrossRef]
- Bercker, S.; Weber-Carstens, S.; Deja, M.; Grimm, C.; Wolf, S.; Behse, F.; Busch, T.; Falke, K.J.; Kaisers, U. Critical Illness Polyneuropathy and Myopathy in Patients with Acute Respiratory Distress Syndrome*. Crit. Care Med. 2005, 33, 711–715. [Google Scholar] [CrossRef]
- Patel, B.K.; Pohlman, A.S.; Hall, J.B.; Kress, J.P. Impact of Early Mobilization on Glycemic Control and ICU-Acquired Weakness in Critically Ill Patients Who Are Mechanically Ventilated. Chest 2014, 146, 583–589. [Google Scholar] [CrossRef]
- Van Den Berghe, G.; Schoonheydt, K.; Becx, P.; Bruyninckx, F.; Wouters, P.J. Insulin Therapy Protects the Central and Peripheral Nervous System of Intensive Care Patients. Neurology 2005, 64, 1348–1353. [Google Scholar] [CrossRef] [PubMed]
- Price, D.R.; Mikkelsen, M.E.; Umscheid, C.A.; Armstrong, E.J. Neuromuscular Blocking Agents and Neuromuscular Dysfunction Acquired in Critical Illness: A Systematic Review and Meta-Analysis. Crit. Care Med. 2016, 44, 2070–2078. [Google Scholar] [CrossRef] [PubMed]
- Bellaver, P.; Schaeffer, A.F.; Leitao, C.B.; Rech, T.H.; Nedel, W.L. Association between Neuromuscular Blocking Agents and the Development of Intensive Care Unit-Acquired Weakness (ICU-AW): A Systematic Review with Meta-Analysis and Trial Sequential Analysis. Anaesth. Crit. Care Pain Med. 2023, 42, 101202. [Google Scholar] [CrossRef]
- Papazian, L.; Forel, J.-M.; Gacouin, A.; Penot-Ragon, C.; Perrin, G.; Loundou, A.; Jaber, S.; Arnal, J.-M.; Perez, D.; Seghboyan, J.-M.; et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef]
- Puthucheary, Z.; Rawal, J.; Ratnayake, G.; Harridge, S.; Montgomery, H.; Hart, N. Neuromuscular Blockade and Skeletal Muscle Weakness in Critically Ill Patients: Time to Rethink the Evidence? Am. J. Respir. Crit. Care Med. 2012, 185, 911–917. [Google Scholar] [CrossRef]
- Patt, H.; Bandgar, T.; Lila, A.; Shah, N. Management Issues with Exogenous Steroid Therapy. Indian J. Endocrinol. Metab. 2013, 17, 612. [Google Scholar] [CrossRef]
- Pereira, R.M.R.; Freire De Carvalho, J. Glucocorticoid-Induced Myopathy. Joint Bone Spine 2011, 78, 41–44. [Google Scholar] [CrossRef]
- Yang, T.; Li, Z.; Jiang, L.; Xi, X. Corticosteroid Use and Intensive Care Unit-Acquired Weakness: A Systematic Review and Meta-Analysis. Crit. Care 2018, 22, 187. [Google Scholar] [CrossRef] [PubMed]
- Weber-Carstens, S.; Deja, M.; Koch, S.; Spranger, J.; Bubser, F.; Wernecke, K.D.; Spies, C.D.; Spuler, S.; Keh, D. Risk Factors in Critical Illness Myopathy during the Early Course of Critical Illness: A Prospective Observational Study. Crit. Care 2010, 14, R119. [Google Scholar] [CrossRef]
- Efficacy and Safety of Corticosteroids for Persistent Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2006, 354, 1671–1684. [CrossRef]
- Meduri, G.U.; Schwingshackl, A.; Hermans, G. Prolonged Glucocorticoid Treatment in ARDS: Impact on Intensive Care Unit-Acquired Weakness. Front. Pediatr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Lad, H.; Saumur, T.M.; Herridge, M.S.; Dos Santos, C.C.; Mathur, S.; Batt, J.; Gilbert, P.M. Intensive Care Unit-Acquired Weakness: Not Just Another Muscle Atrophying Condition. Int. J. Mol. Sci. 2020, 21, 7840. [Google Scholar] [CrossRef] [PubMed]
- Bonaldo, P.; Sandri, M. Cellular and Molecular Mechanisms of Muscle Atrophy. Dis. Model. Mech. 2013, 6, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Hermans, G.; De Jonghe, B.; Bruyninckx, F.; Berghe, G. Clinical Review: Critical Illness Polyneuropathy and Myopathy. Crit. Care 2008, 12, 238. [Google Scholar] [CrossRef] [PubMed]
- Ayala, J.C.; Grismaldo, A.; Aristizabal-Pachon, A.F.; Mikhaylenko, E.V.; Nikolenko, V.N.; Mikhaleva, L.M.; Somasundaram, S.G.; Kirkland, C.E.; Aliev, G.; Morales, L. Mitochondrial Dysfunction in Intensive Care Unit Patients. Curr. Pharm. Des. 2021, 27, 3074–3081. [Google Scholar] [CrossRef] [PubMed]
- Jiroutková, K.; Krajčová, A.; Ziak, J.; Fric, M.; Waldauf, P.; Džupa, V.; Gojda, J.; Němcova-Fürstová, V.; Kovář, J.; Elkalaf, M.; et al. Mitochondrial Function in Skeletal Muscle of Patients with Protracted Critical Illness and ICU-Acquired Weakness. Crit. Care 2015, 19, 448. [Google Scholar] [CrossRef]
- Raia, L.; Zafrani, L. Endothelial Activation and Microcirculatory Disorders in Sepsis. Front. Med. 2022, 9, 907992. [Google Scholar] [CrossRef]
- Nilwik, R.; Snijders, T.; Leenders, M.; Groen, B.B.L.; Van Kranenburg, J.; Verdijk, L.B.; Van Loon, L.J.C. The Decline in Skeletal Muscle Mass with Aging Is Mainly Attributed to a Reduction in Type II Muscle Fiber Size. Exp. Gerontol. 2013, 48, 492–498. [Google Scholar] [CrossRef]
- Wall, B.T.; Snijders, T.; Senden, J.M.G.; Ottenbros, C.L.P.; Gijsen, A.P.; Verdijk, L.B.; Van Loon, L.J.C. Disuse Impairs the Muscle Protein Synthetic Response to Protein Ingestion in Healthy Men. J. Clin. Endocrinol. Metab. 2013, 98, 4872–4881. [Google Scholar] [CrossRef]
- Latronico, N.; Bolton, C.F. Critical Illness Polyneuropathy and Myopathy: A Major Cause of Muscle Weakness and Paralysis. Lancet Neurol. 2011, 10, 931–941. [Google Scholar] [CrossRef]
- Bolton, C.F. Neuromuscular Manifestations of Critical Illness. Muscle Nerve 2005, 32, 140–163. [Google Scholar] [CrossRef] [PubMed]
- Piva, S.; Fagoni, N.; Latronico, N. Intensive Care Unit–Acquired Weakness: Unanswered Questions and Targets for Future Research. F1000Research 2019, 8, 508. [Google Scholar] [CrossRef] [PubMed]
- Attwell, C.; Sauterel, L.; Jöhr, J.; Piquilloud, L.; Kuntzer, T.; Diserens, K. Early Detection of ICU-Acquired Weakness in Septic Shock Patients Ventilated Longer than 72 h. BMC Pulm. Med. 2022, 22, 466. [Google Scholar] [CrossRef]
- Appleton, R.; Kinsella, J. Intensive Care Unit-Acquired Weakness. Contin. Educ. Anaesth. Crit. Care Pain 2012, 12, 62–66. [Google Scholar] [CrossRef]
- Latronico, N.; Bertolini, G.; Guarneri, B.; Botteri, M.; Peli, E.; Andreoletti, S.; Bera, P.; Luciani, D.; Nardella, A.; Vittorielli, E.; et al. Simplified Electrophysiological Evaluation of Peripheral Nerves in Critically Ill Patients: The Italian Multi-Centre CRIMYNE Study. Crit. Care 2007, 11, R11. [Google Scholar] [CrossRef]
- Klawitter, F.; Walter, U.; Axer, H.; Patejdl, R.; Ehler, J. Neuromuscular Ultrasound in Intensive Care Unit-Acquired Weakness: Current State and Future Directions. Medicina (Mex.) 2023, 59, 844. [Google Scholar] [CrossRef]
- Van Alfen, N.; Mah, J.K. Neuromuscular Ultrasound: A New Tool in Your Toolbox. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2018, 45, 504–515. [Google Scholar] [CrossRef]
- Takahashi, Y.; Morisawa, T.; Okamoto, H.; Nakanishi, N.; Matsumoto, N.; Saitoh, M.; Takahashi, T.; Fujiwara, T. Diaphragm Dysfunction and ICU-Acquired Weakness in Septic Shock Patients with or without Mechanical Ventilation: A Pilot Prospective Observational Study. J. Clin. Med. 2023, 12, 5191. [Google Scholar] [CrossRef]
- Covino, M.; Salini, S.; Russo, A.; De Matteis, G.; Simeoni, B.; Maccauro, G.; Sganga, G.; Landi, F.; Gasbarrini, A.; Franceschi, F. Frailty Assessment in the Emergency Department for Patients ≥80 Years Undergoing Urgent Major Surgical Procedures. J. Am. Med. Dir. Assoc. 2022, 23, 581–588. [Google Scholar] [CrossRef]
- Covino, M.; Russo, A.; Salini, S.; De Matteis, G.; Simeoni, B.; Della Polla, D.; Sandroni, C.; Landi, F.; Gasbarrini, A.; Franceschi, F. Frailty Assessment in the Emergency Department for Risk Stratification of COVID-19 Patients Aged ≥80 Years. J. Am. Med. Dir. Assoc. 2021, 22, 1845–1852.e1. [Google Scholar] [CrossRef]
- Fan, E.; Cheek, F.; Chlan, L.; Gosselink, R.; Hart, N.; Herridge, M.S.; Hopkins, R.O.; Hough, C.L.; Kress, J.P.; Latronico, N.; et al. An Official American Thoracic Society Clinical Practice Guideline: The Diagnosis of Intensive Care Unit–Acquired Weakness in Adults. Am. J. Respir. Crit. Care Med. 2014, 190, 1437–1446. [Google Scholar] [CrossRef] [PubMed]
- Latronico, N.; Nattino, G.; Guarneri, B.; Fagoni, N.; Amantini, A.; Bertolini, G.; GiVITI Study Investigators. Validation of the Peroneal Nerve Test to Diagnose Critical Illness Polyneuropathy and Myopathy in the Intensive Care Unit: The Multicentre Italian CRIMYNE-2 Diagnostic Accuracy Study. F1000Research 2014, 3, 127. [Google Scholar] [CrossRef] [PubMed]
- Anekwe, D.E.; Biswas, S.; Bussières, A.; Spahija, J. Early Rehabilitation Reduces the Likelihood of Developing Intensive Care Unit-Acquired Weakness: A Systematic Review and Meta-Analysis. Physiotherapy 2020, 107, 1–10. [Google Scholar] [CrossRef]
- Kayambu, G.; Boots, R.; Paratz, J. Physical Therapy for the Critically Ill in the ICU: A Systematic Review and Meta-Analysis*. Crit. Care Med. 2013, 41, 1543–1554. [Google Scholar] [CrossRef] [PubMed]
- Parry, S.M.; Berney, S.; Warrillow, S.; El-Ansary, D.; Bryant, A.L.; Hart, N.; Puthucheary, Z.; Koopman, R.; Denehy, L. Functional Electrical Stimulation with Cycling in the Critically Ill: A Pilot Case-Matched Control Study. J. Crit. Care 2014, 29, 695.e1–695.e7. [Google Scholar] [CrossRef]
- Zaragoza-García, I.; Arias-Rivera, S.; Frade-Mera, M.J.; Martí, J.D.; Gallart, E.; San José-Arribas, A.; Velasco-Sanz, T.R.; Blazquez-Martínez, E.; Raurell-Torredà, M. Enteral Nutrition Management in Critically Ill Adult Patients and Its Relationship with Intensive Care Unit-Acquired Muscle Weakness: A National Cohort Study. PLOS ONE 2023, 18, e0286598. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Reintam Blaser, A.; Preiser, J.-C. Less Is More in Nutrition: Critically Ill Patients Are Starving but Not Hungry. Intensive Care Med. 2019, 45, 1629–1631. [Google Scholar] [CrossRef]
- Weijs, P.J.; Looijaard, W.G.; Beishuizen, A.; Girbes, A.R.; Oudemans-van Straaten, H.M. Early High Protein Intake Is Associated with Low Mortality and Energy Overfeeding with High Mortality in Non-Septic Mechanically Ventilated Critically Ill Patients. Crit. Care 2014, 18, 701. [Google Scholar] [CrossRef]
Table 1.
Risk factors for ICU-AW.
Table 1.
Risk factors for ICU-AW.
| Risk factors for ICU-AW |
|---|
| Modifiable |
Non Modifiable |
| Hyperglycaemia |
Premorbid health status |
| Drugs |
Multiple Organ Failure |
| Parenteral nutrition |
Sepsis and septic shock |
| Immobilization |
Mechanical ventilation |
| |
High lactate level |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).